Blood pressure 140 90 pregnant
High Blood Pressure in Pregnancy | Preeclampsia
On this page
Basics
- Summary
- Start Here
- Symptoms
- Diagnosis and Tests
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- Videos and Tutorials
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
What is high blood pressure in pregnancy?
Blood pressure is the force of your blood pushing against the walls of your arteries as your heart pumps blood. High blood pressure, or hypertension, is when this force against your artery walls is too high. There are different types of high blood pressure in pregnancy:
- Gestational hypertension is high blood pressure that you develop while you are pregnant. It starts after you are 20 weeks pregnant. You usually don't have any other symptoms. In many cases, it does not harm you or your baby, and it goes away within 12 weeks after childbirth. But it does raise your risk of high blood pressure in the future. It sometimes can be severe, which may lead to low birth weight or preterm birth. Some women with gestational hypertension do go on to develop preeclampsia.
- Chronic hypertension is high blood pressure that started before the 20th week of pregnancy or before you became pregnant. Some women may have had it long before becoming pregnant but didn't know it until they got their blood pressure checked at their prenatal visit. Sometimes chronic hypertension can also lead to preeclampsia.

- Preeclampsia is a sudden increase in blood pressure after the 20th week of pregnancy. It usually happens in the last trimester. In rare cases, symptoms may not start until after delivery. This is called postpartum preeclampsia. Preeclampsia also includes signs of damage to some of your organs, such as your liver or kidney. The signs may include protein in the urine and very high blood pressure. Preeclampsia can be serious or even life-threatening for both you and your baby.
What causes preeclampsia?
The cause of preeclampsia is unknown.
Who is at risk for preeclampsia?
You are at higher risk of preeclampsia if you:
- Had chronic high blood pressure or chronic kidney disease before pregnancy
- Had high blood pressure or preeclampsia in a previous pregnancy
- Have obesity
- Are over age 40
- Are pregnant with more than one baby
- Are African American
- Have a family history of preeclampsia
- Have certain health conditions, such as diabetes, lupus, or thrombophilia (a disorder which raises your risk of blood clots)
- Used in vitro fertilization, egg donation, or donor insemination
What problems can preeclampsia cause?
Preeclampsia can cause:
- Placental abruption, where the placenta separates from the uterus
- Poor fetal growth, caused by a lack of nutrients and oxygen
- Preterm birth
- A low birth weight baby
- Stillbirth
- Damage to your kidneys, liver, brain, and other organ and blood systems
- A higher risk of heart disease for you
- Eclampsia, which happens when preeclampsia is severe enough to affect brain function, causing seizures or coma
- HELLP syndrome, which happens when a woman with preeclampsia or eclampsia has damage to the liver and blood cells.
 It is rare, but very serious.
It is rare, but very serious.
What are the symptoms of preeclampsia?
Possible symptoms of preeclampsia include:
- High blood pressure
- Too much protein in your urine (called proteinuria)
- Swelling in your face and hands. Your feet may also swell, but many women have swollen feet during pregnancy. So swollen feet by themselves may not be a sign of a problem.
- Headache that does not go away
- Vision problems, including blurred vision or seeing spots
- Pain in your upper right abdomen
- Trouble breathing
Eclampsia can also cause seizures, nausea and/or vomiting, and low urine output. If you go on to develop HELLP syndrome, you may also have bleeding or bruising easily, extreme fatigue, and liver failure.
How is preeclampsia diagnosed?
Your health care provider will check your blood pressure and urine at each prenatal visit. If your blood pressure reading is high (140/90 or higher), especially after the 20th week of pregnancy, your provider will likely want to run some tests. They may include blood tests other lab tests to look for extra protein in the urine as well as other symptoms.
They may include blood tests other lab tests to look for extra protein in the urine as well as other symptoms.
What are the treatments for preeclampsia?
Delivering the baby can often cure preeclampsia. When making a decision about treatment, your provider take into account several factors. They include how severe it is, how many weeks pregnant you are, and what the potential risks to you and your baby are:
- If you are more than 37 weeks pregnant, your provider will likely want to deliver the baby.
- If you are less than 37 weeks pregnant, your health care provider will closely monitor you and your baby. This includes blood and urine tests for you. Monitoring for the baby often involves ultrasound, heart rate monitoring, and checking on the baby's growth. You may need to take medicines, to control your blood pressure and to prevent seizures. Some women also get steroid injections, to help the baby's lungs mature faster. If the preeclampsia is severe, you provider may want you to deliver the baby early.

The symptoms usually go away within 6 weeks of delivery. In rare cases, symptoms may not go away, or they may not start until after delivery (postpartum preeclampsia). This can be very serious, and it needs to be treated right away.
- About Preeclampsia and Eclampsia (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- High Blood Pressure and Pregnancy (Mayo Foundation for Medical Education and Research) Also in Spanish
- High Blood Pressure during Pregnancy (American Academy of Family Physicians) Also in Spanish
- High Blood Pressure during Pregnancy (March of Dimes Birth Defects Foundation)
- What Are the Symptoms of Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- How Do Health Care Providers Diagnose Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Magnesium Blood Test (National Library of Medicine) Also in Spanish
- What Are the Treatments for Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- HELLP Syndrome (American Academy of Family Physicians) Also in Spanish
- What Are the Risks of Preeclampsia and Eclampsia to the Fetus? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Risks of Preeclampsia and Eclampsia to the Mother? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Postpartum Preeclampsia (American Academy of Family Physicians) Also in Spanish
- High Blood Pressure During Pregnancy Fact Sheet (Centers for Disease Control and Prevention)
- Who Is at Risk of Preeclampsia? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Hypertension, Pregnancy-Induced (National Institutes of Health)
gov: Hypertension, Pregnancy-Induced (National Institutes of Health) - ClinicalTrials.gov: Pre-Eclampsia (National Institutes of Health)
- Article: The presence of hypertension during pregnancy determines the future risk of.
 ..
.. - Article: Maternal hypertensive disorder of pregnancy and mortality in offspring from birth...
- Article: Hypertensive disorders during pregnancy and polycystic ovary syndrome are associated with.
 ..
.. - High Blood Pressure in Pregnancy -- see more articles
- Find an Ob-Gyn (American College of Obstetricians and Gynecologists)
- National Heart, Lung, and Blood Institute
Preeclampsia and High Blood Pressure During Pregnancy
-
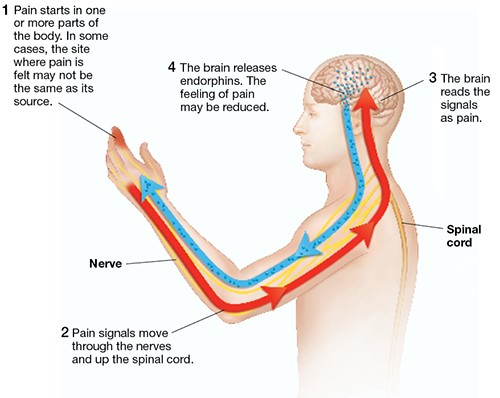
Blood pressure is the force of blood pushing against the walls of blood vessels called arteries.
 The arteries bring blood from the heart to your lungs, where it picks up oxygen and then moves to your organs and tissues. The organs and tissues use the oxygen to power their activities. Blood vessels called veins return the blood to the heart.
The arteries bring blood from the heart to your lungs, where it picks up oxygen and then moves to your organs and tissues. The organs and tissues use the oxygen to power their activities. Blood vessels called veins return the blood to the heart. -
High blood pressure (also called hypertension) can lead to health problems at any time in life. High blood pressure usually does not cause symptoms. During pregnancy, severe or uncontrolled high blood pressure can cause problems for you and your fetus.
Some women have high blood pressure before they get pregnant. Others develop it for the first time during pregnancy. A serious high blood pressure disorder called preeclampsia can also happen during pregnancy or soon after childbirth.
-
A blood pressure reading has two numbers separated by a slash.
 A blood pressure reading of 110/80 mm Hg, for example, is referred to as “110 over 80.” The first number is the pressure against the artery walls when the heart contracts. This is called the systolic blood pressure. The second number is the pressure against the artery walls when the heart relaxes between contractions. This is called the diastolic blood pressure.
A blood pressure reading of 110/80 mm Hg, for example, is referred to as “110 over 80.” The first number is the pressure against the artery walls when the heart contracts. This is called the systolic blood pressure. The second number is the pressure against the artery walls when the heart relaxes between contractions. This is called the diastolic blood pressure. -
-
Normal: Less than 120/80 mm Hg
-
Elevated: Systolic between 120 and 129 mm Hg and diastolic less than 80 mm Hg
-
Stage 1 hypertension: Systolic between 130 and 139 mm Hg or diastolic between 80 and 89 mm Hg
-
Stage 2 hypertension: Systolic at least 140 mm Hg or diastolic at least 90 mm Hg
-
-
Your obstetrician–gynecologist (ob-gyn) should check your blood pressure at each prenatal care visit.
 Blood pressure changes often during the day. If you have one high reading, another reading may be taken later during your office visit.
Blood pressure changes often during the day. If you have one high reading, another reading may be taken later during your office visit.
-
Chronic hypertension is high blood pressure that a woman has before getting pregnant or that develops in the first half of pregnancy (before 20 weeks of pregnancy). If you were taking blood pressure medication before you got pregnant—even if your blood pressure is currently normal—you have been diagnosed with chronic hypertension.
-
When you are pregnant, your body makes more blood to support the fetus’s growth. If blood pressure goes up during pregnancy, it can place extra stress on your heart and kidneys. This can lead to heart disease, kidney disease, and stroke. High blood pressure during pregnancy also increases the risk of preeclampsia, preterm birth, placental abruption, and cesarean birth.

-
High blood pressure may reduce blood flow to the placenta. As a result, the fetus may not get enough of the nutrients and oxygen needed to grow.
-
In the first half of pregnancy, blood pressure normally goes down. If your hypertension is mild, your blood pressure may stay that way or even return to normal during pregnancy. But if your blood pressure is 140/90 mm Hg or higher, your ob-gyn may recommend that you start or continue taking blood pressure medication during pregnancy.
-
Your blood pressure should be checked at every prenatal care visit. You may also need to monitor your blood pressure at home. Ultrasound exams may be done throughout pregnancy to track the growth of the fetus.
 If growth problems are suspected, you may have other tests that monitor the health of the fetus. This testing usually begins in the third trimester of pregnancy.
If growth problems are suspected, you may have other tests that monitor the health of the fetus. This testing usually begins in the third trimester of pregnancy. -
If your condition remains stable, delivery 1 to 3 weeks before your due date (about 37 weeks to 39 weeks of pregnancy) generally is recommended. If you or the fetus develop complications, delivery may be needed even earlier.
-
After delivery, you will need to keep monitoring your blood pressure at home for 1 to 2 weeks. Blood pressure often goes up in the weeks after childbirth. You may need to resume taking medication, or your medication dosage may need to be adjusted.
Talk with your ob-gyn about blood pressure medications that are safe to take if you plan to breastfeed. Do not stop any medications without talking with your ob-gyn.

-
You have gestational hypertension when:
-
You have a systolic blood pressure of 140 mm Hg or higher and/or a diastolic blood pressure of 90 mm Hg or higher.
-
The high blood pressure first happens after 20 weeks of pregnancy.
-
You had normal blood pressure before pregnancy.
Most women with gestational hypertension have only a small increase in blood pressure. But some women develop severe hypertension (defined as systolic blood pressure of 160 mm Hg or higher and/or diastolic blood pressure of 110 mm Hg or higher). These women are at risk of very serious complications.
-
-
All women with gestational hypertension are monitored often (usually weekly) for signs of preeclampsia and to make sure that their blood pressure does not go too high.

-
Although gestational hypertension usually goes away after childbirth, it may increase the risk of developing high blood pressure in the future. If you had gestational hypertension, keep this risk in mind as you take care of your health. Healthy eating, weight loss, and regular exercise may help prevent high blood pressure in the future.
-
Preeclampsia is a serious disorder that can affect all the organs in your body. It usually develops after 20 weeks of pregnancy, often in the third trimester. When it develops before 34 weeks of pregnancy, it is called early-onset preeclampsia. It can also develop in the weeks after childbirth.
-
It is not clear why some women develop preeclampsia.
 Doctors refer to "high risk" and "moderate risk" of preeclampsia.
Doctors refer to "high risk" and "moderate risk" of preeclampsia. Factors that may put you in the “high risk” category include
-
preeclampsia in a past pregnancy
-
carrying more than one fetus (twins, triplets, or more)
-
chronic hypertension
-
kidney disease
-
diabetes mellitus
-
autoimmune conditions, such as lupus (systemic lupus erythematosus or SLE)
-
having multiple moderate risk factors (see below)
Factors that may put you in the “moderate risk” category include
-
being pregnant for the first time
-
being pregnant more than 10 years after your previous pregnancy
-
body mass index (BMI) over 30
-
family history of preeclampsia (mother or sister)
-
being age 35 or older
-
complications in previous pregnancies, such as having a baby with a low birth weight
-
in vitro fertilization (IVF)
-
Black race (because of racism and inequities that increase risk of illness)
-
lower income (because of inequities that increase risk of illness)
-
-
-
Preeclampsia can lead to a condition that causes seizures and stroke.

-
Preeclampsia can cause HELLP syndrome. HELLP stands for hemolysis, elevated liver enzymes, and low platelet count. HELLP syndrome damages or destroys red blood cells and interferes with blood clotting. It can also cause chest pain, abdominal pain, and bleeding in the liver. HELLP syndrome is a medical emergency. Women can die from HELLP syndrome. They can also have lifelong health problems from the condition.
-
-
For women with preeclampsia, early delivery may be needed in some cases. Preterm babies have an increased risk of problems with breathing, eating, staying warm, hearing, and vision. Some preterm complications last a lifetime and require ongoing medical care.
-
Women who have had preeclampsia—especially those whose babies were born preterm—have an increased risk later in life of kidney disease, heart attack, stroke, and high blood pressure.
 Also, having preeclampsia once increases the risk of having it again in a future pregnancy.
Also, having preeclampsia once increases the risk of having it again in a future pregnancy. -
Preeclampsia can develop quietly without you being aware of it. Symptoms can include
-
swelling of face or hands
-
headache that will not go away
-
seeing spots or changes in eyesight
-
pain in the upper abdomen or shoulder
-
nausea and vomiting (in the second half of pregnancy)
-
sudden weight gain
-
difficulty breathing
If you have any of these symptoms, especially if they develop in the second half of pregnancy, call your ob-gyn right away.
A woman with preeclampsia whose condition is worsening will develop “severe features.” Severe features include
-
low number of platelets in the blood
-
abnormal kidney or liver function
-
pain in the upper abdomen
-
changes in vision
-
fluid in the lungs
-
severe headache
-
systolic pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or higher
-
-
A high blood pressure reading may be the first sign of preeclampsia.
 If your blood pressure reading is high, it may be checked again to confirm the results. You may have a urine test to check for protein. You may also have tests to check how your liver and kidneys are working and to measure the number of platelets in your blood.
If your blood pressure reading is high, it may be checked again to confirm the results. You may have a urine test to check for protein. You may also have tests to check how your liver and kidneys are working and to measure the number of platelets in your blood. -
You and your ob-gyn should talk about how your condition will be managed. The goal is to limit complications for you and to deliver the healthiest baby possible.
-
Women who have gestational hypertension or preeclampsia without severe features may be treated in a hospital or as an outpatient. Being an outpatient means you can stay at home with close monitoring by your ob-gyn. You may need to keep track of your fetus’s movement by doing a daily kick count. You may also need to measure your blood pressure at home. Visits to your ob-gyn may be once or twice a week.

At 37 weeks of pregnancy, you and your ob-gyn may talk about delivery. Labor may be induced (started with medications). If test results show that the fetus is not doing well, you may need to have the baby earlier. Women with preeclampsia can have vaginal deliveries, but if there are problems during labor, cesarean birth may be needed.
-
If you have preeclampsia with severe features, you may be treated in the hospital. If you are at least 34 weeks pregnant, you and your ob-gyn may talk about having your baby as soon as your condition is stable.
If you are less than 34 weeks pregnant and your condition is stable, it may be possible to wait to deliver your baby. Delaying delivery for just a few days may be helpful in some cases. It allows time to give corticosteroids, which can help the fetus’s lungs mature. Delaying can also give you time to take medications to reduce your blood pressure and help prevent seizures.
.jpg) If your health or the fetus’s health worsens, you and your ob-gyn should discuss immediate delivery.
If your health or the fetus’s health worsens, you and your ob-gyn should discuss immediate delivery.Read Preterm Labor and Birth or Extremely Preterm Birth to learn more.
-
Prevention involves identifying whether you have risk factors for preeclampsia and taking steps to address them.
-
Low-dose aspirin may reduce the risk of preeclampsia in some women. Your ob-gyn may recommend that you take low-dose aspirin if
Low-dose aspirin may also be considered if you are Black or if you have a low income, even if you have no other risk factors.
Talk with your ob-gyn about whether you should take aspirin. Do not start taking aspirin on your own without talking with your ob-gyn.
-
If you have high blood pressure and want to get pregnant, see your ob-gyn for a check-up.
 Your ob-gyn will want to know if your high blood pressure is under control and if it has affected your health.
Your ob-gyn will want to know if your high blood pressure is under control and if it has affected your health. You may have tests to check how your heart and kidneys are working. Your medications should be reviewed to see if you need to switch to others that are safer during pregnancy. You should also talk about the signs and symptoms of preeclampsia.
-
Arteries: Blood vessels that carry oxygen-rich blood from the heart to the rest of the body.
Body Mass Index (BMI): A number calculated from height and weight. BMI is used to determine whether a person is underweight, normal weight, overweight, or obese.
Cesarean Birth: Birth of a fetus from the uterus through an incision (cut) made in the woman’s abdomen.
Chronic Hypertension: Blood pressure that is higher than normal for a person’s age, sex, and physical condition.

Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Corticosteroids: Drugs given for arthritis or other medical conditions. These drugs also are given to help fetal lungs mature before birth.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Diastolic Blood Pressure: The force of the blood in the arteries when the heart is relaxed. It is the lower reading when blood pressure is taken.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gestational Hypertension: High blood pressure that is diagnosed after 20 weeks of pregnancy.
HELLP Syndrome: A severe type of preeclampsia.
 HELLP stands for hemolysis, elevated liver enzymes, and low platelet count.
HELLP stands for hemolysis, elevated liver enzymes, and low platelet count.High Blood Pressure: Blood pressure above the normal level. Also called hypertension.
Hypertension: High blood pressure.
In Vitro Fertilization (IVF): A procedure in which an egg is removed from a woman’s ovary, fertilized in a laboratory with the man’s sperm, and then transferred to the woman’s uterus to achieve a pregnancy.
Kick Count: A record kept during late pregnancy of the number of times a fetus moves over a certain period.
Kidneys: Organs that filter the blood to remove waste that becomes urine.
Lupus: An autoimmune disorder that affects the connective tissues in the body. The disorder can cause arthritis, kidney disease, heart disease, blood disorders, and complications during pregnancy.
 Also called systemic lupus erythematosus or SLE.
Also called systemic lupus erythematosus or SLE.Nutrients: Nourishing substances found in food, such as vitamins and minerals.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Oxygen: An element that we breathe in to sustain life.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Placental Abruption: A condition in which the placenta has begun to separate from the uterus before the fetus is born.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain in the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.

Preterm: Less than 37 weeks of pregnancy.
Stroke: A sudden interruption of blood flow to all or part of the brain, caused by blockage or bursting of a blood vessel in the brain. A stroke often results in loss of consciousness and temporary or permanent paralysis.
Systolic Blood Pressure: The force of the blood in the arteries when the heart is contracting. It is the higher reading when blood pressure is taken.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Veins: Blood vessels that carry blood from various parts of the body back to the heart.
Don't have an ob-gyn? Search for doctors near you.
FAQ034
Last updated: April 2022
Last reviewed: April 2022
Copyright 2022 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
High blood pressure during pregnancy
But its meaning is not always correctly controlled and interpreted. Let's figure out how to properly control blood pressure during pregnancy, which blood pressure is considered elevated, why it can rise and what should be done and what should not be done.
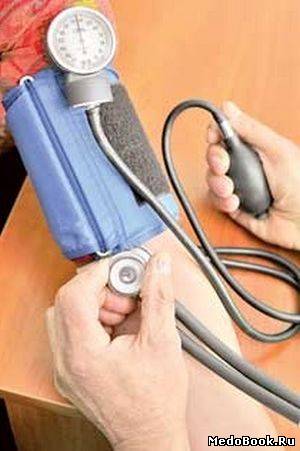
Blood pressure measurement
Blood pressure is monitored using a tonometer: electronic, semi-automatic or mechanical. You can buy any that you can handle and the cuff of which suits you in diameter. The only thing to consider is that the blood pressure cuff should be worn on the upper arm, carpal blood pressure monitors are too inaccurate and cannot be relied upon.
Measurement of blood pressure is best done in a sitting position, and after you have spent about fifteen minutes in this position, in a state of physical and emotional rest, you do not need to talk while measuring blood pressure.
The cuff is worn on the shoulder freed from clothing, its lower edge should be a few centimeters above the elbow. The arm on which blood pressure is measured should be in a relaxed position, the cuff should be located approximately at the level of the heart. Measurement is performed on one arm, measurement on two arms, which was previously required for all pregnant women, is now excluded from all clinical recommendations.
When measuring with a mechanical sphygmomanometer , air is inflated into the cuff to the digits, approximately twenty to thirty mm. rt. Art. higher than expected blood pressure. The air from the cuff is released slowly, the appearance of sound marks the numbers of systolic blood pressure, the disappearance of the sound - diastolic.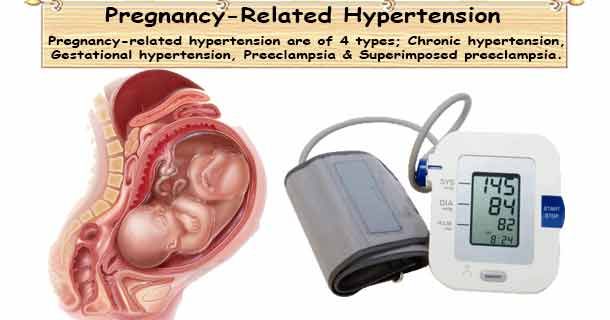 This is not "cardiac" and "renal" pressure, but - systolic and diastolic.
This is not "cardiac" and "renal" pressure, but - systolic and diastolic.
Measurement of blood pressure is carried out at each visit to the obstetrician-gynecologist - office measurement of blood pressure, at home of the pregnant woman or her relative - outpatient measurement of blood pressure. If necessary, the doctor may recommend that the patient keep a blood pressure diary - measure blood pressure several times a day for some time, writing down the numbers. Ceteris paribus, more reliable information is obtained from outpatient (at home) measurements.
If there is doubt about the correctness of the patient's blood pressure measurement or if there is a suspicion of an increase in blood pressure at night, the doctor may prescribe the patient 24-hour blood pressure monitoring (ABPM), in which blood pressure is measured automatically at certain intervals within one day.
In general, during pregnancy, blood pressure in the first trimester is lower than normal for the patient, in the second or third it returns to her usual numbers, by the third trimester it may be slightly higher, but within the normal range. Blood pressure below 140/9 is considered normal during pregnancy.0 mm. rt. Art.
Blood pressure below 140/9 is considered normal during pregnancy.0 mm. rt. Art.
If the patient is prone to arterial hypotension (low blood pressure), elevated blood pressure is still considered to be blood pressure above 140/90 mm. rt. Art., lower figures do not require any additional examination or treatment, even if they are higher than usual for the patient. None of the clinical guidelines for the treatment of arterial hypertension during pregnancy indicate the need for treatment with higher blood pressure than usual, but not reaching a value of 140/90 mm. rt. Art.
AD 140/90 mm. rt. Art. and above must be recorded 2 or more times with an interval between measurements of at least 4 hours to be considered hypertension.
Causes of high blood pressure
There are three causes of high blood pressure during pregnancy: chronic arterial hypertension, gestational arterial hypertension and preeclampsia.
Chronic arterial hypertension is the general name for all cases of high blood pressure that existed before pregnancy. Chronic arterial hypertension is not divided into primary (due to unknown causes) and secondary (resulting from a disease), in contrast to arterial hypertension detected outside of pregnancy. Also, chronic arterial hypertension includes situations when a woman did not control blood pressure before pregnancy, and for the first time an increase in blood pressure was detected only in the first half (up to 20 weeks) of pregnancy.
Chronic arterial hypertension is not divided into primary (due to unknown causes) and secondary (resulting from a disease), in contrast to arterial hypertension detected outside of pregnancy. Also, chronic arterial hypertension includes situations when a woman did not control blood pressure before pregnancy, and for the first time an increase in blood pressure was detected only in the first half (up to 20 weeks) of pregnancy.
Gestational hypertension occurs from the twentieth week until the end of the term, and is not accompanied by the excretion of protein in the urine.
Pre-eclampsia, in contrast to gestational hypertension, also develops after the 20th week of pregnancy, and is accompanied by the release of protein into the urine (proteinuria). Preeclampsia can also occur after delivery. Signs of an increase in the severity of preeclampsia are the appearance of a headache, dizziness, visual disturbances, pain in the solar plexus and / or in the right hypochondrium, pain under the right shoulder blade, respiratory failure, and some changes in blood tests. These signs require urgent hospitalization.
These signs require urgent hospitalization.
The extreme case of preeclampsia - eclampsia - is characterized by the occurrence of convulsions and threatens the life of both the mother and the child, therefore, it requires an emergency delivery, regardless of the gestational age, only in this way it becomes possible to save the life of the mother and child.
Since an increase in blood pressure may occur before proteinuria in preeclampsia, it is only possible to distinguish gestational arterial hypertension from preeclampsia in retrospect - if blood pressure increased, and protein did not appear in the daily urine, it can be said with certainty that this increase in blood pressure was due to specifically gestational hypertension.
Pre-eclampsia may be associated with chronic arterial hypertension that existed before pregnancy.
Treatment of Hypertensive Disorders
Hypertensive disorders are an important cause of maternal and perinatal death, increase the incidence of preterm birth, and are indeed a serious problem and should not be ignored.
The only one to date proven effective in preventing preeclampsia drug is acetylsalicylic acid. It is prescribed starting from the 13th week of pregnancy at a low dose and at this dosage does not lead to impaired fetal development, unlike high doses.
Treatment of any arterial hypertension during pregnancy is prescribed only by a doctor.
In chronic arterial hypertension uncomplicated by damage to other organs, treatment is started at BP 150/90 mm. rt. Art. and more, with gestational arterial hypertension and preeclampsia - with blood pressure 140/90 mm. rt. Art. and more.
During treatment, it is necessary to maintain blood pressure at the level of 130-150/80/95 mmHg. rt. Art., since a more radical decrease in blood pressure is fraught with impaired blood supply to the fetus and is not recommended.
There are several groups of antihypertensive drugs, the use of which during pregnancy can lead to impaired fetal development or death, so they should not be used during pregnancy. These are angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Do not use during pregnancy and diuretics (drugs with a diuretic effect).
These are angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Do not use during pregnancy and diuretics (drugs with a diuretic effect).
Usually, treatment is started with methyldopa, but it is also possible to use certain drugs from the group of beta-blockers and some drugs from the group of calcium antagonists, which are best studied from the point of view of safety in pregnancy. It is possible to use combinations of these drugs.
Separately, a few words need to be said about magnesium sulfate (magnesium sulphate). This drug has practically no antihypertensive effect, and its use during pregnancy is limited only to preeclampsia, which threatens the development of eclampsia. It is needed to prevent the development of seizures (neuroprotective effect). It should not be used to influence elevated blood pressure.
Delivery for hypertension during pregnancy, is usually performed through the natural birth canal, except in cases of severe pre-eclampsia, eclampsia and their complications, requiring emergency delivery by caesarean section, regardless of the gestational age for health reasons.
Chronic arterial hypertension that persists during lactation and is not complicated by damage to other organs does not require medical treatment for blood pressure less than 150/95 mm. rt. Art. Arterial hypertension after childbirth does not require stopping breastfeeding; on the contrary, the protective effect of lactation in arterial hypertension has been proven.
If it is necessary to prescribe drug therapy , drugs are selected that are least able to be excreted into breast milk, the use of which has not been recorded serious side effects in the child.
Make an appointment with a gynecologist
For more details, consult a qualified specialist at the Semeynaya clinic.
For prices for gynecological appointments or other questions, please follow the link below:
Arterial hypertension during pregnancy | Shchelkovsky perinatal center
Arterial hypertension during pregnancy
Rise in blood pressure during pregnancy. What is preeclampsia?
What is preeclampsia?
Pre-eclampsia is one of the most common complications of pregnancy, affecting both the mother and the unborn child. This condition occurs in 5-8% of pregnant women, is diagnosed based on the rise in blood pressure (BP) and the appearance of protein in the urine. That is why at every prenatal visit to the doctor in a pregnant woman, blood pressure is measured and urine is evaluated for the presence of protein.
In most cases, preeclampsia is relatively mild, occurs closer to full-term pregnancy, and ends with favorable outcomes. At the same time, some cases of preeclampsia progress or develop rapidly and can be extremely dangerous for a woman and her child.
What is "toxemia"?
During visits to the doctor or in the literature, you may come across other terms that define the rise in blood pressure during pregnancy: toxemia, preeclampsia, OPG-preeclampsia (edema, proteinuria, hypertension).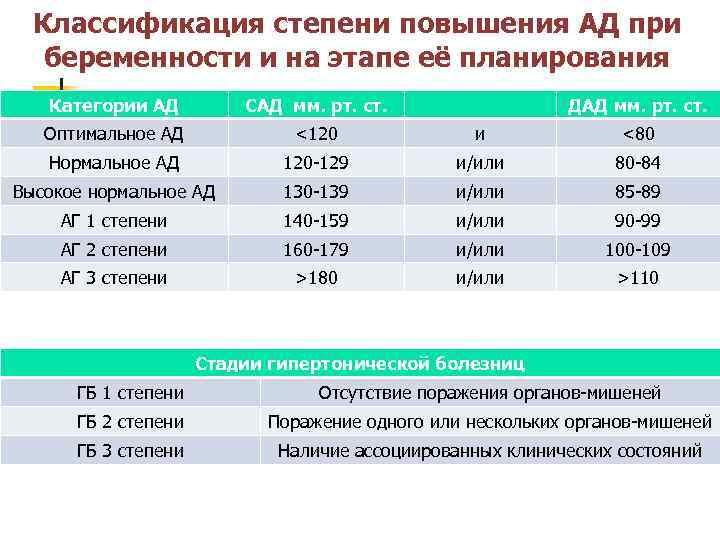 However, the definition of "preeclampsia" is now accepted.
However, the definition of "preeclampsia" is now accepted.
How is preeclampsia related to eclampsia or HELLP syndrome?
Eclampsia and HELLP syndrome are clinical variants of preeclampsia. The hallmark of eclampsia is seizures, which usually occur as a late complication of severe preeclampsia. However, seizures can also develop without any previous signs of severe illness.
HELLP syndrome is one of the most severe forms of preeclampsia and occurs in approximately 15% of patients with preeclampsia. This condition is sometimes confused with a cold or gallbladder problems. HELLP syndrome can lead to significant liver damage in the mother, the breakdown of red blood cells (erythrocytes), and a decrease in platelets.
What are the causes of preeclampsia? Can it be prevented?
The causes of preeclampsia are not fully understood, so there is currently no reliable way to prevent this condition. Many theories have been proposed that describe various strategies for the prevention of preeclampsia, but none of them is completely successful.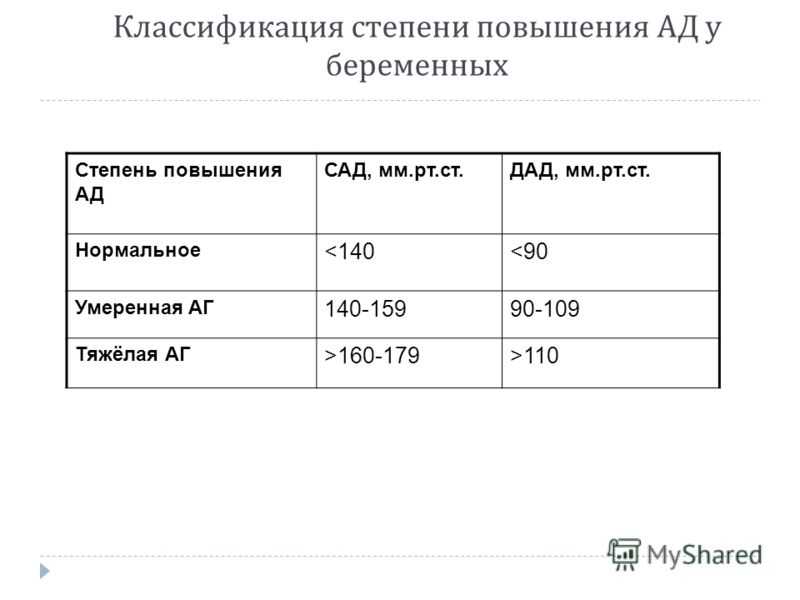
The use of aspirin, calcium, and other therapeutic agents may be beneficial in some settings, but studies do not recommend their widespread use. At the same time, there is a widespread belief that the placenta plays a key role in the development of preeclampsia, and that women with chronic hypertension and other risk factors are predisposed to developing preeclampsia. It is important to know the alarming symptoms, trust your feelings, visit the doctor regularly and strictly follow his recommendations.
When does preeclampsia develop?
In most cases, preeclampsia develops after 20 weeks of pregnancy and usually stops with the birth of the baby. Sometimes preeclampsia continues for up to 6 weeks after delivery. Therefore, you should carefully monitor the symptoms even after childbirth.
Preeclampsia may progress slowly. But sometimes it comes suddenly. This usually happens in cases where a woman does not attach due importance to the manifestations and symptoms of the disease, as a result of which they remain unrecognized for a long time.
Signs and symptoms of pre-eclampsia:
- High blood pressure. 140/90 mm. rt. Art. and higher. An increase in blood pressure during pregnancy that is 30 or more units above your baseline is a cause for concern and requires medical attention.
- Protein in urine. 0.3 g in a 24 hour sample or mark 1+ on a paper test strip.
- Swelling of hands, feet or face. Particularly around the eyes, if there are impressions from thumb pressure, or if these symptoms come on suddenly.
- Headache, which does not go away even after taking medication for it.
- Visual disturbances. Double vision, glow, "flies", aura (a special condition preceding an attack).
- Nausea or pain in the upper abdomen (epigastrium). Sometimes confused with indigestion, gallbladder pain, or the flu, however, nausea in the second half of pregnancy is not a normal condition.

- Sudden weight gain, more than 500 g per week.
Risk factors
Personal history
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- High blood pressure before pregnancy
- Diabetes before or during pregnancy
- Multiple pregnancy
- Obesity
- Systemic lupus erythematosus or other autoimmune diseases
- Polycystic ovary syndrome
- Long interval between pregnancies
- Pregnancy after IVF
- Sickle cell disease
Family history
- Maternal or paternal preeclampsia in the family
- High blood pressure or heart disease
- Diabetes
Risk factors for premature babies include lung immaturity and many other potential problems. In severe cases, preeclampsia can cause fetal death.
What is the treatment for preeclampsia?
Professionals need to consider many factors when deciding how to manage preeclampsia and when to deliver, including the condition of the baby, the condition and age of the mother, and the exact course of the disease. These include monitoring blood pressure, evaluating the results of laboratory tests that characterize the condition of the mother's kidneys, liver, or the ability of her blood to clot. Other tests monitor how the fetus grows and whether it is endangered while in the womb. Therapeutic agents include magnesium sulfate to prevent seizures, as well as medications to lower blood pressure. Sometimes a wait-and-see approach is used, both with and without medication. When the health of the mother or child is in serious danger, the only acceptable treatment for preeclampsia at any stage of pregnancy is delivery.
Can medicines harm me or my baby?
Blood pressure medication rarely causes any side effects for the mother.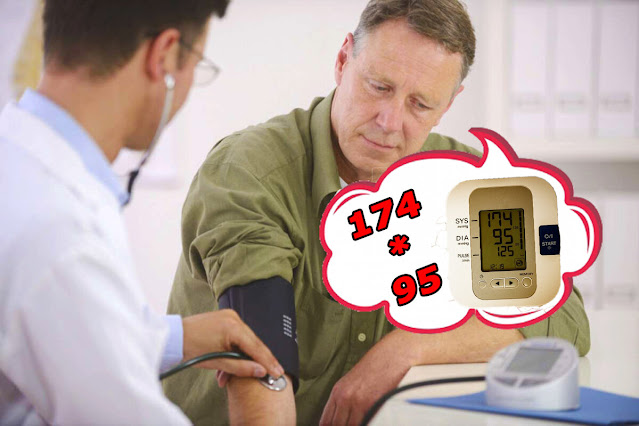 And if the doctor prescribed them for you, then this means that your pressure is high enough, and that the risk for you or your child from raising the pressure is much higher than from taking medication. Magnesium sulfate is generally safe for the baby, but can cause hot flashes, sweating, thirst, visual disturbances, drowsiness, mild confusion, muscle weakness, and shortness of breath in the mother. These side effects should completely disappear when the administration of the drug ends.
And if the doctor prescribed them for you, then this means that your pressure is high enough, and that the risk for you or your child from raising the pressure is much higher than from taking medication. Magnesium sulfate is generally safe for the baby, but can cause hot flashes, sweating, thirst, visual disturbances, drowsiness, mild confusion, muscle weakness, and shortness of breath in the mother. These side effects should completely disappear when the administration of the drug ends.
Can I stay at home?
Sometimes women with mild preeclampsia stay at home. In this case, more frequent visits to a specialist, monitoring of blood pressure and urine tests are necessary in order to timely identify signs of a progressive condition and prevent the adverse effects of preeclampsia on your health and the health of your child. The well-being of the child should be assessed by monitoring the nature of changes in heart rate, fetal growth and weight, blood flow in the vessels using ultrasound.