What to expect during labor
What to Expect During Your First Childbirth
As your expected due date approaches, you might be wondering what to expect during childbirth. While each labor and birth is unique, the process of a vaginal delivery follows four stages: First Stage (early labor, active labor and transition), Second Stage (pushing and birth), Third Stage (delivery of the placenta), and Fourth Stage (uterus returns to original size).
Attending childbirth classes at Cedars-Sinai is another way to help ease your labor fears.
View Childbirth Classes
First Stage (early labor, active labor and transition)
During Early Labor
What to Expect: You will begin to notice tightening sensations in your abdomen called contractions. These contractions can last up to 60 seconds and can be between 5 to 30 minutes apart. Contractions will increase in strength and frequency as your labor progresses. At this time, your cervix will start to dilate (open) and will reach 6 centimeters by the end of this phase.
How Long It Will Last: Early labor is the longest part of labor and can last 12 to 24 hours or longer if this is your first baby. Because of this, it is important to be patient and try to rest as much as possible.
Tips for Coping With Early Labor
- Pace yourself: Balance rest and activity to conserve your energy
- Distraction: Ignore labor until you can’t ignore it anymore
- Reading, cooking, puzzles, neighborhood walks, watching TV
- Comfort measures: massage, shower, music
- Eat light snacks and stay hydrated
- You and/or your partner can time your contractions: how long they last and how often they happen
Arriving to Labor and Delivery
If you are at least 37 weeks, expecting a single baby and have no medical complications, you should continue to stay at home until it is difficult to breathe through or talk through contractions.
If you arrive at Labor and Delivery in early labor, after careful evaluation of you and your baby, your doctor may recommend that you return when you are further along in labor. The earlier you are admitted in your labor process, the longer your hospital stay.
When to Call Your Doctor
Not all labor is the same; follow your doctor’s or midwife’s advice. If you experience any of the following, call your provider or come to the hospital:
- Your water breaks/membranes rupture
- You experience vaginal bleeding that is more than spotting
- You have regular, painful contractions that are less than 5 minutes apart for several hours
- You are concerned that your baby is moving less
During Active Labor
What to Expect: Your contractions are stronger, longer and closer together. Contractions can last up to 60 to 90 seconds and are approximately 2 to 5 minutes apart. Dilation typically happens more rapidly in active labor than in early labor, your cervix dilates to 6 to 8 centimeters.
Dilation typically happens more rapidly in active labor than in early labor, your cervix dilates to 6 to 8 centimeters.
How Long It Will Last: For many people giving birth for the first time, active labor typically lasts 4 to 8 hours.
During Transition
What to Expect: Your contractions are the strongest, longest and closest together. Contractions can last 60 to 120 seconds and are usually 2 to 3 minutes apart. Your cervix dilates from 8 to 10 centimeters and when you reach 10 centimeters, you begin the second stage.
How Long It Will Last: This is usually the shortest part of the first stage of labor.
Tips for Coping With Active Labor and Transition
- Walking, changing positions, slow or rhythmic breathing during contractions
- Visualizations or aromatherapy
- Massage, counter-pressure or other hands-on techniques
- Pain medication (epidural analgesia) is available if you desire
- Utilize your support person for coaching and encouragement
Second Stage (pushing and birth)
What to Expect: Your cervix has fully dilated to 10 centimeters. You may feel pressure and the urge to push. Your doctor or midwife will let you know when to start pushing.
You may feel pressure and the urge to push. Your doctor or midwife will let you know when to start pushing.
How Long It Will Last: On average this stage can last 1 ½ to 2 hours with your first baby. However, you only push when you are having a contraction and you can rest in between.
Third and Fourth Stages (after delivery)
What to Expect: Your placenta is delivered. You may experience chills or shakiness during this time. This stage can take up to 30 minutes. Once the placenta is delivered, you enter the fourth stage of labor as your uterus returns to its original size. Many people feel light cramping during this period.
Pain Management During Labor and Childbirth
Pain during childbirth is unique to each person’s expectations and goals. This can be due to beliefs about pain in labor, pain tolerance, support in labor and delivery, and previous injury or trauma. There are both medicated and nonmedicated options available. Discuss with your provider the pain management options available to you during your labor and childbirth.
There are both medicated and nonmedicated options available. Discuss with your provider the pain management options available to you during your labor and childbirth.
Tips for Dealing With Labor Pains
Watch this video to learn how to manage labor pains that begin at home and explore your pain-management choices once you get to the hospital.
If Your Baby Is Breech
In the final weeks before birth, most babies move in the womb so their head faces down toward the birth canal. When a baby's bottom or feet point down, it's called breech presentation. If that happens, many birthing people will have a planned cesarean delivery. In some cases, you may still be able to have a vaginal birth—especially if your doctor is able to perform an "external version," which helps turn your baby in the right direction.
Turning your breech baby (PDF)
If You Need A Cesarean Delivery
Most birth plans include having a vaginal delivery, however, there are times where an unscheduled, or even an emergency, cesarean delivery is necessary. A cesarean delivery is a procedure where a baby is delivered through a surgical incision in the birthing person’s stomach and uterus. Your doctor may require you to have an unplanned cesarean delivery for several reasons - labor is not progressing, contractions are too weak, the umbilical cord is pinched or wrapped, abnormal heart beat is detected in the fetus, there is an issue with the placenta, the baby is too large, or the baby is breech. Understanding what to expect with a cesarean birth will help you better prepare in the event you require this procedure.
A cesarean delivery is a procedure where a baby is delivered through a surgical incision in the birthing person’s stomach and uterus. Your doctor may require you to have an unplanned cesarean delivery for several reasons - labor is not progressing, contractions are too weak, the umbilical cord is pinched or wrapped, abnormal heart beat is detected in the fetus, there is an issue with the placenta, the baby is too large, or the baby is breech. Understanding what to expect with a cesarean birth will help you better prepare in the event you require this procedure.
To learn more about the risks and benefits of a cesarean delivery, watch the Elective Primary Cesarean video.
You can also sign up for these classes:
- The Elective Cesarean Option
- Cesarean Birth
Pre-Admission
You can save time on delivery day by filling out forms in advance. Find out how to pre-register for admission to Cedars-Sinai.
LEARN MORE
Labor & Delivery Tips from an OBGYN for First-Time Moms
Giving birth can be both exciting and terrifying for first-time moms.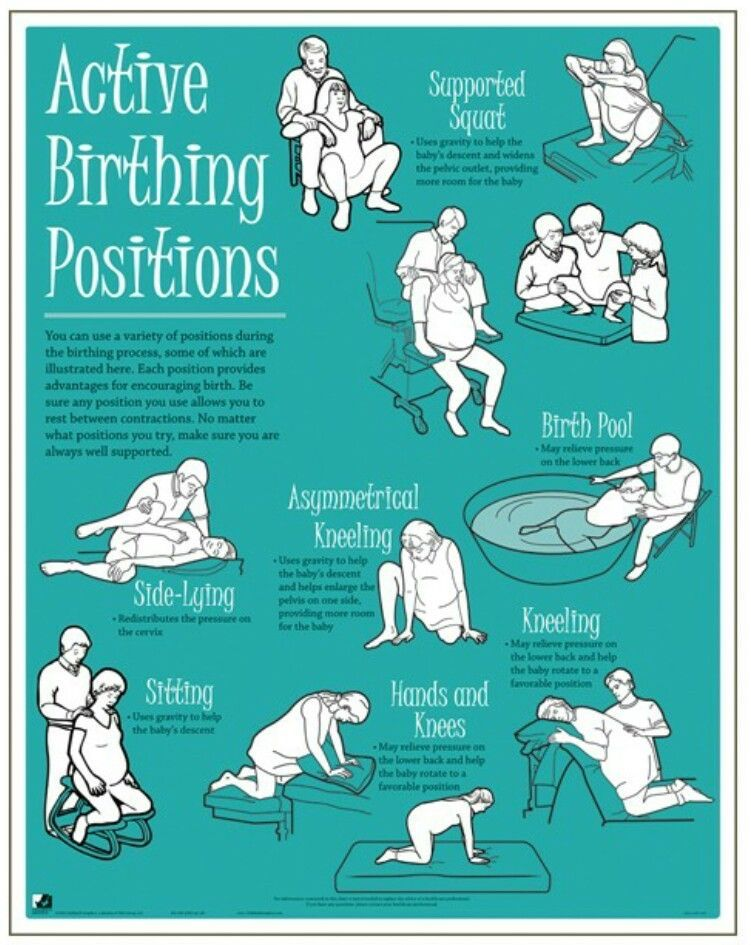 Just as the rest of your pregnancy has differed from others’, your birth experience will be unique to you and your baby. As you think about the big day when you’ll finally meet your little one, you probably have questions about what to expect!
Just as the rest of your pregnancy has differed from others’, your birth experience will be unique to you and your baby. As you think about the big day when you’ll finally meet your little one, you probably have questions about what to expect!
Here are some of the most common questions I’ve been asked about giving birth for the first time.
Getting Ready for Baby
How important are birthing classes?
Prenatal classes or birthing classes can help you understand what to expect during your labor and delivery. You’ll learn about creating a birth plan, common things that happen in a hospital, and how to manage pain. At Madison Women’s Health, we refer our patients to Unity Point Meriter for prenatal classes. You can begin taking prenatal classes at the start of your second trimester. We recommend completing them before your 37th week of pregnancy.
Prenatal classes can be online or in person. Check with the hospital to see what they currently offer. Prenatal classes typically include a birth center tour. There are classes for singletons and multiples. They are helpful in understanding various things that can happen in labor and delivery that are not common things you see on TV (like ways to monitor your baby’s heart rate and the use of forceps or a vacuum if needed to safely deliver your baby).
There are classes for singletons and multiples. They are helpful in understanding various things that can happen in labor and delivery that are not common things you see on TV (like ways to monitor your baby’s heart rate and the use of forceps or a vacuum if needed to safely deliver your baby).
Tip: Prenatal classes will help you think of questions you may want to ask your OB during your prenatal check-ups. Keep a list! Classes are a good supplement to your 10-15 minute prenatal visits.
Who can be with me at the birth?
Before the COVID-19 pandemic, there were no restrictions on how many people could be with you during the birth. During any Public Health Emergency, guidelines may change. It’s always a good idea to verify how many people can be there with you.
At the time this article was written, Meriter allowed one support person (in addition to a doula) to be with you. This person can be anyone — your partner, a friend, or a relative. Choose someone who will be supportive and encouraging. Currently, your support person must be the same person throughout the birthing experience. In other words, your support person cannot be your spouse for a few hours, then your mother, and then your sister.
Currently, your support person must be the same person throughout the birthing experience. In other words, your support person cannot be your spouse for a few hours, then your mother, and then your sister.
Tip: A doula is considered part of the medical team and is therefore allowed to be involved in your care during the pandemic.
What is the difference between a midwife and a doula?
Midwives have been trained in obstetric procedures. They can interpret fetal monitoring, make recommendations on labor management, and recommend a C-section if it is needed.
Doulas have been trained in the emotional, psychological, and physical support of moms throughout pregnancy, delivery. and postpartum. They have not been medically trained, but their attention and focus on the mom has been shown to improve birth outcomes. Women who use a doula are more likely to have a delivery without pain medications and their labors tend to be shorter.
Tip: A doula does not make medical recommendations or replace your midwife or doctor, but rather they offer extra services and individualized prenatal and labor support
What will the labor and delivery room or birthing room look like?
Our patients deliver their babies at Meriter Hospital, which has large birthing rooms. You’ll appreciate having more space to walk around in early labor or sit on a birthing ball. You’ll be able to control the temperature and dim the lighting. Your room will have a couch, perfect for your support person to nap on if needed.
You’ll appreciate having more space to walk around in early labor or sit on a birthing ball. You’ll be able to control the temperature and dim the lighting. Your room will have a couch, perfect for your support person to nap on if needed.
Tip: Meriter’s birth rooms also include a comfortable tub. While we don’t offer water births (in accordance with ACOG recommendations), water immersion during labor can help with relaxation and easing labor pain.
What should I pack in my hospital bag?
If you have to drop what you’re doing and immediately go to the hospital, they will have all the essentials. I usually tell patients, however, that it’s a good idea to have a bag ready to go around 36 weeks. There are things you will want to help make your stay more comfortable.
Here are some ideas for your hospital bag:
-
- Toiletries: Shampoo, conditioner, soap, toothbrush and toothpaste, hair brush, deodorant. While we have these things at the hospital, you’ll probably prefer your own.
- Comfy clothes for you.
- Slippers, socks, or flip-flops.
- Robe and/or nightgown. If you plan to breastfeed, choose a nightgown that opens in the front (although the hospital ones are great for this!)
- Clothes to wear home. Comfortable maternity clothes are usually your best bet. Include a nursing bra if you plan on breastfeeding.
- Going home outfit for your baby. Your baby will be swaddled and diapered during the hospital stay, but most parents want a photo-worthy outfit for the big trip home.l
- Snacks for your partner / your support person. The hospital has a cafeteria (open during the day) and vending machines, but your partner may want to consider anything special they want. Sometimes light snacks are okay in early labor, but we recommend against eating in active labor for safety reasons (and you usually won’t feel like it!).

- Toiletries: Shampoo, conditioner, soap, toothbrush and toothpaste, hair brush, deodorant. While we have these things at the hospital, you’ll probably prefer your own.
- Phone charger. Family and friends will want frequent updates and you will fill up your camera roll quickly.
It’s Time!
At what point do I need to go to the hospital? How long should I labor at home?
Most women can spend time in early labor at home. We recommend calling if you have painful contractions every 5 minutes for 1-2 hours to keep us in the loop. Call sooner if your doctor has given you more specific instructions due to medical conditions. If you have had a more complicated pregnancy or if you live far from the hospital, you may be asked to come in sooner. If you think your water has broken, we recommend calling to discuss the best time to come in, which is usually early for safety reasons.
Tip: Everyone has a different pain threshold. A good measure of “painful contractions” means you need to stop and breathe through them without focusing on anything else.
How long is labor for first-time moms?
There are three stages of labor and how long each lasts is very unpredictable for first-time moms. The whole event can last hours or days. Your first labor will be the most unpredictable, while second labors are generally faster.
The whole event can last hours or days. Your first labor will be the most unpredictable, while second labors are generally faster.
What are the stages of labor?
Stage 1a: Latent Labor
Contractions during early labor will feel mild, like deep menstrual cramps, and will be irregular. Early labor helps soften, shorten, and thin your cervix. It can start a few days or a few hours before birth.
Stage 1b: Active Labor
During active labor, your contractions become more frequent, regular, and painful. You are considered to be in active labor when your cervix has dilated to 6 cm. The rate of cervical change is more consistent and predictable from this point to “complete” dilation (10 cm). Your doctor will check your cervix to let you know when it’s ok to begin pushing. If you push too soon, before your cervix has fully dilated, you are at risk of tearing your cervix and having significant bleeding.
Stage 2: Pushing Stage / Birth
The second stage is the pushing stage. This stage can last a few minutes or many hours (up to 4 or more if the baby is making progress through the birth canal).
This stage can last a few minutes or many hours (up to 4 or more if the baby is making progress through the birth canal).
You may think, “how will I know when to push?” If you don’t have an epidural during labor, the urge to push is often very strong. If you have an epidural, you may not notice the urge to push in the same way. We will help you know how and when to push with your contractions.
Stage 3: Placenta Delivery
The placenta generally delivers within 30 minutes of giving birth. We sometimes massage your uterus to help with this (although we say massage, this can be uncomfortable). We strongly recommend every woman receive oxytocin as well. These steps are important to decrease the risk of excess bleeding following delivery.
What should my partner do during labor?
Talk about this with your support person ahead of time so expectations are clear. Some women prefer their partner help with coping with labor pain. Others prefer a more hands off approach. Talk together ahead of time to determine what you are comfortable with.
Talk together ahead of time to determine what you are comfortable with.
Tip: Your support person can be supportive in many ways. This can be giving you sips of water and ice chips, holding your hand, being responsible for music, rubbing your back, etc. Do what works best for both of you.
Can I eat and drink while I’m in labor?
If you are undergoing an induction or are at the hospital in early labor, sometimes light snacks are reasonable. A lot of women get nauseous and throw up in labor and are at risk for aspiration, a serious complication. We therefore recommend against eating in active labor. If there’s a possibility of needing a C-section, it is safest to have not had food recently. Most women are not hungry anyway! Water, clear juice, and ice chips are satisfying.
Tip: If you have an I/V, you will be properly hydrated. If your lips get dry from your breathing exercises, ask for some chapstick.
Pain Management
What does giving birth feel like?
Labor pain feels different for everyone, but some general principles include:
- Braxton Hicks contractions — These are common, even as early as the second trimester.
 You’ll feel your uterus gradually tighten and get soft. This is not painful.
You’ll feel your uterus gradually tighten and get soft. This is not painful. - Early labor — Contractions can feel like strong menstrual cramps lasting 30 to 60 seconds (like a charley Horse in your uterus). Some women feel these contractions in their back.
- Active labor — These are cramps that can’t be described by words. You may feel intense pelvic pressure as you “transition” to 10 cm and your baby descends into the birth canal.
- Pushing stage — Along with the muscle pain of contractions, you will feel stretching and pressure in your vagina.
What are my options to treat labor pain?
Non-Pharmacologic Pain Control:
- Changing positions: You may feel better standing up, resting on your hands and knees, or sitting on a birthing ball. Your body will tell you what is working!
- Taking a warm shower or bath: The warm water can relax tense muscles.
 Water immersion has been shown to lower pain scores.
Water immersion has been shown to lower pain scores. - Massage: Your support person, nurse, or doula can massage your back and provide counter pressure during contractions
- Breathing techniques: You’ll learn breathing techniques during your prenatal classes. Staying relaxed and calm helps with pain control.
Pharmacologic Pain Control:
- I/V Narcotic: Some women have good pain relief with an IV or subcutaneous injection of a narcotic medication. We don’t recommend this option if we suspect you will deliver within an hour. This is to let the medication clear from you and your baby’s system before delivery. .
- Epidural: You can request an epidural at any time you are in pain in labor. Some women request an epidural almost immediately, while others choose to have it done later. Medication from an epidural does not transfer to the baby.
 Learn more FAQs about epidurals for labor pain.
Learn more FAQs about epidurals for labor pain.
Tip: Each woman has different anatomy and experiences pain differently, so please be careful not to put pressure on yourself to make decisions about your labor based on others experiences. Women who give birth with an epidural have no less of a “natural birth” than someone who did not use pain medication. Each birth is equally as beautiful!
Special Circumstances & Preparing for Unexpected
What about giving birth to twins? How is labor different?
If you’re pregnant with twins, we recommend that you deliver in an operating room instead of the birth room, even if delivered vaginally. While it may not feel as cozy as a birth room, an operating room allows for more room to meet these babies safely. Your OBGYN will counsel prenatally on the safest way to meet your twins, as having two babies at one time comes with more risk than one.
In the United States, the primary Cesarean section (C-section) rate is just over 30%.
At Madison Women’s Health, the C-section rate for first-time moms is well under 20%.
What is the likelihood I will need a C-Section?
In the United States, the primary Cesarean section (C-section) rate is just over 30%. At Madison Women’s Health, the C-section rate for first-time moms is well under 20%.
In the United States, the most common reason a woman delivers by C-section is that labor does not progress. In most cases, this is due to cephalopelvic disproportion (when a baby does not fit). The second most common reason is because we see signs a baby is in distress in labor. The recommendation for C-section is made when the benefit of meeting a baby by surgery outweighs the risks.
Tip: Our primary goal in caring for you is a healthy mom and a healthy baby and we will explain our recommendations for that each step of the way. We also want you to have a vaginal birth! We only recommend C-sections if we think the benefit is greater than the risk.
What is an episiotomy? Will I need one?
An episiotomy is a rarely performed medical procedure that involves cutting the perineum to help the baby deliver. Historically, an episiotomy was thought to decrease severity of tearing with delivery. We know through research that letting tearing happen naturally is more beneficial to the mom.
Historically, an episiotomy was thought to decrease severity of tearing with delivery. We know through research that letting tearing happen naturally is more beneficial to the mom.
Tip: Episiotomies are only performed in emergency situations, with your consent, when it will help the baby deliver more quickly (a rare occurrence).
Will I tear? How is it treated?
Approximately 90% of women have a vaginal/perineal tear with delivery. Tears are graded as 1st through 4th degree, with 1st as the least amount of tearing. We recommend suturing tears to help them heal appropriately. We do this with stitches that dissolve.
Tip: A new technique, called perineal massage, has been proven to decrease the amount of tearing with delivery.
What about the embarrassing things….like pooping and pubic hair?
Most worry or feel embarrassed about these things, but we don’t even notice!
If you like to wax, I don’t recommend this past the 37th week. We don’t recommend shaving before delivery because it increases your risk of infection. Trust us, we are not paying attention to grooming!
Trust us, we are not paying attention to grooming!
Most women will have a bowel movement in labor or with pushing. This is good! it means you are pushing correctly.
Tip: Trust us. We really don’t care or remember!
Recovery
How long does it take to recover from giving birth?
Every woman is different in how she recovers, too. Postpartum is an awesome time, but also stressful! It is often referred to as the 4th trimester. Your sleep schedule changes, your body changes, and your interpersonal relationships change. If you choose to breastfeed, read up on our breastfeeding tips for new moms.
Vaginal Birth:
Many moms are surprised to know there is still a recovery period. You may have cramping, tailbone pain, and pain as a tear heals. Sometimes sitting and walking are tricky! There are no true lifting restrictions after a vaginal delivery, but I recommend avoiding heavy lifting for about two weeks, especially from the ground. This puts a lot of stress on your pelvic floor as it heals. Helpful tips for going home include sitting on soft surfaces, using a spray bottle after you void, using ice pads, taking ibuprofen and Tylenol, and keeping an area of all the things you will need most to care for you and baby in your home.
Helpful tips for going home include sitting on soft surfaces, using a spray bottle after you void, using ice pads, taking ibuprofen and Tylenol, and keeping an area of all the things you will need most to care for you and baby in your home.
C-section:
The recovery from a C-section is longer because it is a major surgery. Wait six weeks before lifting anything greater than 10-15 lbs. We will teach you how to care for your incision in the hospital and will send you home with pain medication.
Final Recommendations
What are your recommendations about giving birth at home?
Home births double your risk of complications, with two times the risk of perinatal mortality and three times the risk of neonatal seizures. We, along with the American Academy of Pediatrics and ACOG, believe the hospital is the safest place to give birth. If you decide to give birth at home, you should have a low-risk pregnancy, the help of a certified midwife, and be reasonably close to a hospital.
Tip: Our first priorities are the health and safety of you and your baby. We will give you information and recommendations about safety and labor so you can make informed decisions throughout the process.
Bring a list of questions to your next OB visit!
Dr. Ashley Durward has been providing healthcare to women in Madison since 2015 and joined Madison Women’s Health in 2019, specializing in high and low risk obstetrics, contraception and preconception counseling, management of abnormal uterine bleeding, pelvic floor disorders, and minimally invasive gynecologic surgery.
How to behave in childbirth? Learning to give birth quickly and with problems
Childbirth is a natural process, laid down by nature. The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
Childbirth is the final and most important stage of pregnancy. How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions.
How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions.
1. When is it time to go to the maternity hospital?
Childbirth is a natural result of hormonal changes that occur in your body during the final stages of pregnancy. The sagging belly and heaviness in its lower part and the lumbar region speak of the imminent denouement of the story. Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity.
The signal to call an ambulance should be sufficiently strong contractions that are repeated at regular intervals, the appearance of mucous secretions from the genital tract, slightly stained with blood, or the outflow of amniotic fluid.
2. First stage of childbirth: we breathe for two!
From the moment the contractions become regular, the first stage of labor begins, during which the strength, frequency and duration of uterine spasms increases and the cervix opens.
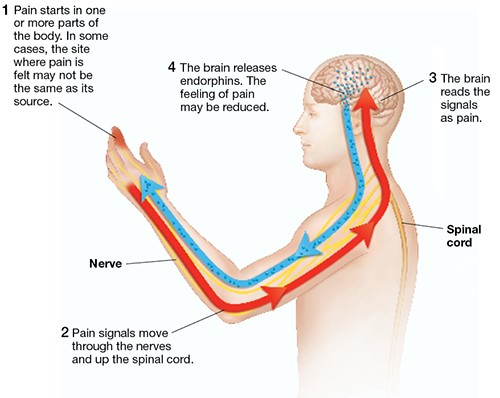
During spastic contraction of the uterine muscle fibers, the blood vessels that carry arterial blood to the placenta and fetus are compressed. The fetus begins to experience a lack of oxygen, and this involuntarily makes you breathe deeper. The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
In the first stage of labor, during each contraction, you need to breathe calmly and deeply, trying not to hold your breath while inhaling. At the same time, the air should fill the upper sections of the lungs, as if raising the chest. You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
3. Auto-training in the prenatal ward
To speed up the opening of the cervix, you need to walk more, but sitting is not recommended, while blood flow in the limbs is disturbed and venous blood stagnation occurs in the pelvis. From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby."
4. To relieve pain
Acupressure of the lower back can help relieve pain. Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Monitor the frequency and duration of contractions and if they weaken or sharply increase, immediately inform your doctor. In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
If dilatation of the cervix causes reflex vomiting, rinse the mouth with water and then drink a few sips to replace the lost fluid. Do not drink a lot, this can provoke a recurrence of vomiting.
5. The maternity ward is not a place for tantrums
They say that difficult childbirth is a person's retribution for walking upright. Childbirth is actually a painful process, but the presence of reason allows us, representatives of the genus Homo sapiens, to control our emotions. Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome.
6. Second stage of labor - pushing and expulsion of the fetus
After the baby's head slips through the dilated cervix and finds itself on the bottom of the pelvis, the pushing period of labor begins. At this time, there is a desire to push, as it usually happens during a bowel movement, but at the same time many times stronger. At first, the attempts are controllable, they can be "breathed", but by the beginning of the third stage of labor, the expulsion of the fetus, they become unbearable.
With the beginning of the straining period, you will be transferred to the delivery room. Having settled down on the delivery table, rest your feet on the special steps, firmly grasp the handrails and wait for the midwife's command.
While pushing, inhale deeply, close your mouth, clench your lips tightly, pull the handrails of the delivery table towards you and direct all the exhalation energy down, squeezing the fetus out of you. When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
7. Third stage of labor and final
Third stage of labor - afterbirth. At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
About 10 minutes after your baby is born, your midwife will ask you to push again to deliver your afterbirth. The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures.
You will have to spend another couple of hours in the delivery room with an ice-filled bladder on your stomach. To quickly contract the uterus, you will be given injections of special drugs. When the threat of postpartum hemorrhage has passed, you will be transferred to the postpartum ward to the baby.
Childbirth completed. Ahead of the postpartum period, during which your body will recover after pregnancy.
More details on Medkrug.RU: http://www.medkrug.ru/article/show/kak_pravilno_vesti_sebja_v_rodah_uchimsja_rozhat_bystro_i_problem
Source: http://www.medkrug.ru/
Childbirth - what to expect really? | Libresse
So you're getting ready to give birth
Becoming a mother is a truly special experience full of excitement and happiness. But you can also experience stress and fear – especially at a time like this.
Your body is changing, emotions are changing quickly - and this is easy to understand, because you are preparing for childbirth during a global pandemic. All this (and more!) when you know your life is about to change forever. It's not hard to see how frightening this can be.
All this (and more!) when you know your life is about to change forever. It's not hard to see how frightening this can be.
Even in a situation where social distancing has to be maintained, which has created a whole host of new challenges, you can still have a positive experience of having a baby. In the end, you are still in control of your choices.
Fortunately, you are not alone. Every woman who experiences pregnancy and childbirth today is going through changes and emotions like yours.
Your body changes during pregnancy
The obvious changes in your body during pregnancy are hard to miss. But a lot goes on behind the scenes. From the moment you conceive, your uterus, vagina, and vulva prepare for the birth of your baby.
Many women notice that their labia changes color and size during pregnancy. Others feel changes in the size of their vagina. It's just the way your body prepares for childbirth. All this is quite natural and normal.
If your delivery is vaginal, there may be other changes. Women's bodies are designed to make childbirth possible, the vagina is structurally capable of stretching, but some tears during childbirth are still common. As one mom told us in our project #StoriesVinsideUs: "It's like a cozy garden full of beautiful flowers that suddenly changed forever." If you've had a rupture - or had an episiotomy (an incision made to reduce the damage that a natural tear might cause) - you can get stitches, and they can change the look of your vulva and how you feel during sex.
Women's bodies are designed to make childbirth possible, the vagina is structurally capable of stretching, but some tears during childbirth are still common. As one mom told us in our project #StoriesVinsideUs: "It's like a cozy garden full of beautiful flowers that suddenly changed forever." If you've had a rupture - or had an episiotomy (an incision made to reduce the damage that a natural tear might cause) - you can get stitches, and they can change the look of your vulva and how you feel during sex.
Pain or dryness is common but luckily improves over time and lubricants can help. Many women also experience weakening of the pelvic floor, which can affect the ability to regulate excretory functions. Indeed, vaginal delivery increases the chances of incontinence by 2-3 times [1].
Treat your body with love after childbirth
Society puts a lot of pressure on women to "return to shape" after birth. As one woman told us, "I was surrounded by diet and fitness advice, it felt like I had all these expectations of my body. "
"
But as any mother who has recently given birth will tell you, "getting back into shape" is a ridiculous expectation. Your body has done an incredible job of carrying and delivering a baby, and now it needs time to heal itself.
In time your body will recover and change again. Not to the same shape that was before the baby was born, but to a new, normal one for you. This may mean that your vulva will look different. Or your vagina will feel different. Or something completely different. All of these changes are part of having a baby, which can ultimately also change who you are and how you see the world at the deepest level.
So even though you may be pressured to look a certain way after giving birth, remember that you have had a baby. This is your time to take care of yourself and nurture your body, accepting all the changes that come with your creation of a small life.
As one mother told us: “Being a mother is wonderful. Why look at stretch marks as what we are “left with”? This is what we have acquired.