Epidural pregnancy shot
Epidural block - pregnancy: MedlinePlus Medical Encyclopedia
An epidural block is a numbing medicine given by injection (shot) in the back. It numbs or causes a loss of feeling in the lower half of your body. This lessens the pain of contractions during childbirth. An epidural block may also be used to reduce pain during surgery on the lower extremities. This article focuses on epidural blocks during childbirth.
The block or shot is given into an area over your lower back or spine.
- You may be asked to lie on your side, or you may sit up.
- Either way, you will be asked to pull your stomach inward and hunch your back outward.
Your health care provider will wash the area of your back and inject a little medicine to numb the spot where the epidural needle is placed:
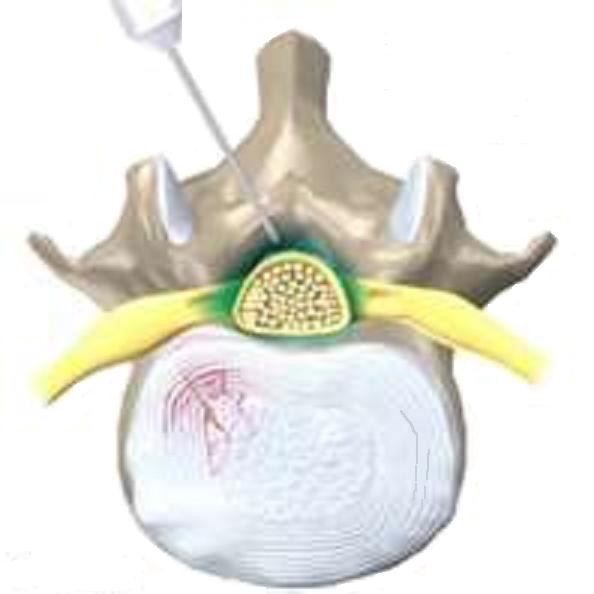
- The provider inserts a needle into your lower back.
- The needle is placed into a small space outside your spinal cord.
- A small soft tube (catheter) is placed into your back, next to your spine.
- The needle is removed.
The numbing medicine is given through the tube for as long as it is needed.
In most cases, you will receive a low dose because it is safer for you and baby. Once the medicine takes effect (10 to 20 minutes), you should feel better. You may still feel some back or rectal pressure during contractions.
You may shiver after an epidural, but this is common. Many women shiver during labor even without an epidural.
Many studies have shown that an epidural is a safe way to manage pain during childbirth. While rare, there are some risks.
Your blood pressure may drop for a short while. This might cause the baby's heart rate to slow down.
- To avoid this, you will receive fluids through an intravenous (IV) line to help keep your blood pressure stable.
- If your blood pressure shows a drop, you may need to lie on your side to keep the blood moving throughout your body.
- Your provider may also give you medicine to raise your blood pressure.

An epidural block may change or alter labor and delivery.
- If you are very numb from the block, you may have a harder time bearing down to push your baby through the birth canal.
- Contractions may lessen or slow down for a little while, but labor will still move along as it should. In some cases, it may even go faster. If your labor slows down, your doctor can give you medicine to speed up your contractions. It is best to wait until you are in active labor to have the epidural placed.
Other rare side effects are:
- You may get a headache after your epidural but this is rare.
- Medicine could enter your spinal fluid. For a short while, it could make you feel dizzy, or you might have a hard time breathing. You could also have a seizure. This is also rare.
There are 2 types:
- "Walking" epidural block. This type of epidural will lessen your pain, but you will still be able to move your legs. Most women are not really able to walk around, but they can move their legs.

- Combined spinal epidural block. This combines both a spinal and epidural block. It provides pain relief much faster. The combined block is used when women are in very active labor and want relief right away.
Delivery - epidural; Labor - epidural
- Epidural - series
Hawkins JL, Bucklin BA. Obstetric anesthesia. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Nathan N, Wong CA. Spinal, epidural, and caudal anesthesia: anatomy, physiology, and technique. In: Chestnut DH, Wong CA, Tsen LC, et al, eds. Chestnut's Obstetric Anesthesia: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Sharpe EE, Arendt KW. Anesthesia for obstetrics. In: Gropper MA, ed. Miller's Anesthesia. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 62.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
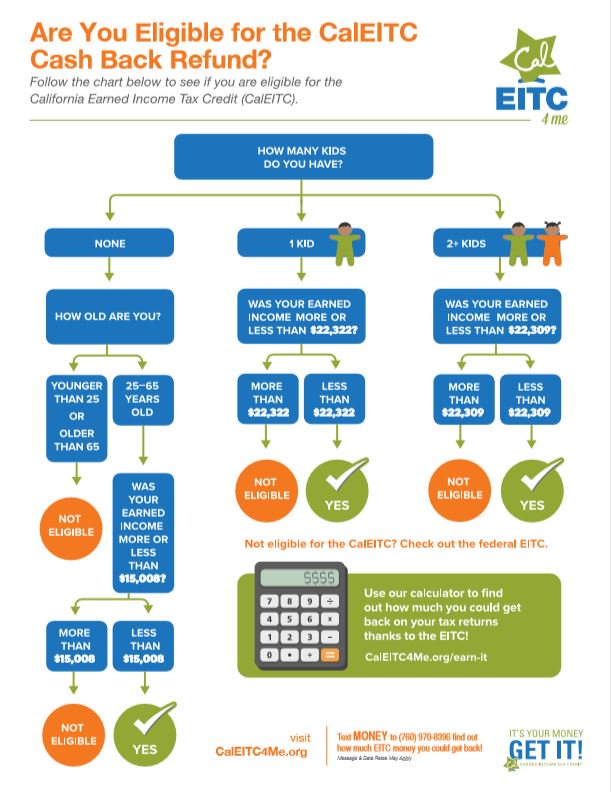
What is an Epidural | American Pregnancy Association
Epidural anesthesia is the most popular method of pain relief during labor. Women request an epidural by name more than any other method of pain relief. More than 50% of women giving birth at hospitals use epidural anesthesia.
As you prepare yourself for “labor day,” try to learn as much as possible about pain relief options so that you will be better prepared to make decisions during the labor and birth process. Understanding the different types of epidurals, how they are administered, and their benefits and risks will help you in your decision-making during the course of labor and delivery.
Epidural anesthesia is regional anesthesia that blocks pain in a particular region of the body. The goal of an epidural is to provide analgesia, or pain relief, rather than anesthesia, which leads to a total lack of feeling. Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body.
Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body.
Epidural medications fall into a class of drugs called local anesthetics, such as bupivacaine, chloroprocaine, or lidocaine. They are often delivered in combination with opioids or narcotics such as fentanyl and sufentanil in order to decrease the required dose of local anesthetic.
This produces pain relief with minimal effects. These medications may be used in combination with epinephrine, fentanyl, morphine, or clonidine to prolong the epidural’s effect or to stabilize the mother’s blood pressure.
How is an epidural given?
Intravenous (IV) fluids will be started before active labor begins and prior to the procedure of placing the epidural. You can expect to receive 1-2 liters of IV fluids throughout labor and delivery. An anesthesiologist (specialize in administering anesthesia), an obstetrician or nurse anesthetist will administer your epidural.
You will be asked to arch your back and remain still while lying on your left side or sitting up. This position is vital for preventing problems and increasing epidural effectiveness.
- An antiseptic solution will be used to wipe the waistline area of your mid-back to minimize the chance of infection. A small area on your back will be injected with a local anesthetic to numb it. A needle is then inserted into the numbed area surrounding the spinal cord in the lower back.
- After that, a small tube or catheter is threaded through the needle into the epidural space. The needle is then carefully removed, leaving the catheter in place to provide medication either through periodic injections or by continuous infusion. The catheter is taped to the back to prevent it from slipping out.
- You’ll start to notice the numbing effect about 10 to 20 minutes after the first dose of medication, though the nerves in your uterus will begin to go numb within a few minutes. You’ll receive continuous doses of medication through the catheter for the rest of your labor.

What are the different types?
There are two basic epidurals in use today. Hospitals and anesthesiologists will differ on the dosages and combinations of medication. You should ask your care providers at the hospital about their practices in this regard.
Regular Epidural
After the catheter is in place, a combination of narcotic and anesthesia is administered either by a pump or by periodic injections into the epidural space. A narcotic such as fentanyl or morphine is given to replace some of the higher doses of anesthetic, like bupivacaine, chloroprocaine, or lidocaine.
This helps reduce some of the adverse effects of the anesthesia. You will want to ask about your hospital’s policies about staying in bed and eating.
Combined Spinal-Epidural (CSE) or “Walking Epidural”
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back. While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
What are the benefits of epidural anesthesia?
- An epidural provides a route for very effective pain relief that can be used throughout your labor.
- The anesthesiologist can control the effects by adjusting the type, amount, and strength of the medication. This is important because as your labor progresses and your baby moves down into your birth canal, the dose you’ve been getting might no longer be adequate, or you might suddenly have pain in a different area.
- The medication only affects a specific area, so you’ll be awake and alert during labor and birth. And because you’re pain-free, you can rest (or even sleep!) as your cervix dilates and conserve your energy for when it comes time to push.

- Unlike with systemic narcotics, only a tiny amount of medication reaches your baby.
- Once the epidural is in place, it can be used to provide anesthesia if you need a c-section or if you’re having your tubes tied after delivery.
What are the risks of epidural anesthesia?
- You have to stay still for 10 to 15 minutes while the epidural is put in, and then wait up to 20 minutes before the medication takes full effect.
- Epidurals may cause your blood pressure to suddenly drop. For this reason, your blood pressure will be routinely checked to help ensure adequate blood flow to your baby. If there is a sudden drop in blood pressure, you may need to be treated with IV fluids, medications, and oxygen.
- You may experience a severe headache caused by leakage of spinal fluid. Less than 1% of women experience this side effect. If symptoms persist, a procedure called a “blood patch”, which is an injection of your blood into the epidural space can be performed to relieve a headache.

- After your epidural is placed, you will need to alternate sides while lying in bed and have continuous monitoring for changes in fetal heart rate. Lying in one position can sometimes cause labor to slow down or stop.
- You might experience the following side effects: shivering, a ringing of the ears, backache, soreness where the needle is inserted, nausea, or difficulty urinating.
- You might find that your epidural makes pushing more difficult and additional medications or interventions may be needed, such as forceps or cesarean. Talk to your doctor when creating your birth plan about what interventions he or she generally uses in such cases.
- For a few hours after the birth, the lower half of your body may feel numb. Numbness will require you to walk with assistance.
In rare instances, permanent nerve damage may result in the area where the catheter was inserted. - Though research is somewhat ambiguous, most studies suggest that some babies will have trouble “latching on” causing breastfeeding difficulties.
 Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
How Long Does an Epidural Last?
Once the catheter is in place, the anaesthetist can set up an epidural pump. The pump feeds the epidural solution into the catheter continuously, providing pain relief for as long as needed.
The type, amount and strength of the anaesthetic can be adjusted, as necessary. You might also be given the option of having control of the medication pump. This is called patient controlled analgesia. The amount of painkiller is still regulated, so you can’t accidentally overdose.
You can have the dose lowered for second stage pushing, but it takes some time for the pain relief and numbness to wear off, so if this is important to you, discuss it with your care provider early on.
Common Questions About Epidurals
Does the placement of epidural anesthesia hurt?The answer depends on who you ask. Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Typically epidurals are placed when the cervix is dilated to 4-5 centimeters and you are in true active labor.
Can an epidural slow labor or lead to a cesarean delivery (C-section)?There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues. With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
How can an epidural affect my baby?As previously stated, research on the effects of epidurals on newborns is somewhat ambiguous, and many factors can affect the health of a newborn. How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
Since dosages and medications can vary, concrete information from research is currently unavailable. One possible side effect of an epidural with some babies is a struggle with “latching on” in breastfeeding. Another is that while in-utero, a baby might also become lethargic and have trouble getting into position for delivery.
These medications have also been known to cause respiratory depression and decreased fetal heart rate in newborns. Though the medication might not harm these babies, they may have subtle effects on the newborn.
How will I feel after the placement of an epidural?The nerves of the uterus should begin to numb within a few minutes after the initial dose. You will probably feel the entire numbing effect after 10-20 minutes. As the anesthetic dose begins to wear off, more doses will be given–usually every one to two hours.
Depending on the type of epidural and dosage administered, you can be confined to your bed and not allowed to get up and move around.
If labor continues for more than a few hours you will probably need urinary catheterization, because your abdomen will be numb, making urinating difficult. After your baby is born, the catheter is removed and the effects of the anesthesia will usually disappear within one or two hours.
Some women report experiencing an uncomfortable burning sensation around the birth canal as the medication wears off.
Will I be able to push?You might not be able to tell that you are having a contraction because of your epidural anesthesia. If you can not feel your contractions, then pushing may be difficult to control. For this reason, your baby might need additional help coming down the birth canal. This is usually done by the use of forceps.
Does an epidural always work?For the most part, epidurals are effective in relieving pain during labor. Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
An epidural may not be an option to relieve pain during labor if any of the following apply:
- You use blood thinners
- Have low platelet counts
- Are hemorrhaging or in shock
- Have an infection on or in your back
- Have a blood infection
- If you are not at least 4 cm dilated
- Epidural space cannot be located by the physician
- If labor is moving too fast and there is not enough time to administer the d
Questions to ask your healthcare providers now and at the time of delivery in the hospital:
- What combination and dosage of drugs will be used?
- How could the medications affect my baby?
- Will I be able to get up and walk around?
- What liquids and solid foods will I be able to consume?
Want to Know More?
- Nitrous Oxide During Labor
- Stages of Labor: Stage 1
- Inducing Labor
- Cord Blood Banking: Your Three Choices Explained
Compiled using information from the following sources:
1. American Academy of Family Physicians
American Academy of Family Physicians
https://www.aafp.org
2. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 19.
3. Mayo Clinic Guide To A Healthy Pregnancy Harms Roger W., M.D., et al, Part 2.
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
Do you know which doctor you want to see
You know the service you want to sign up for
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022.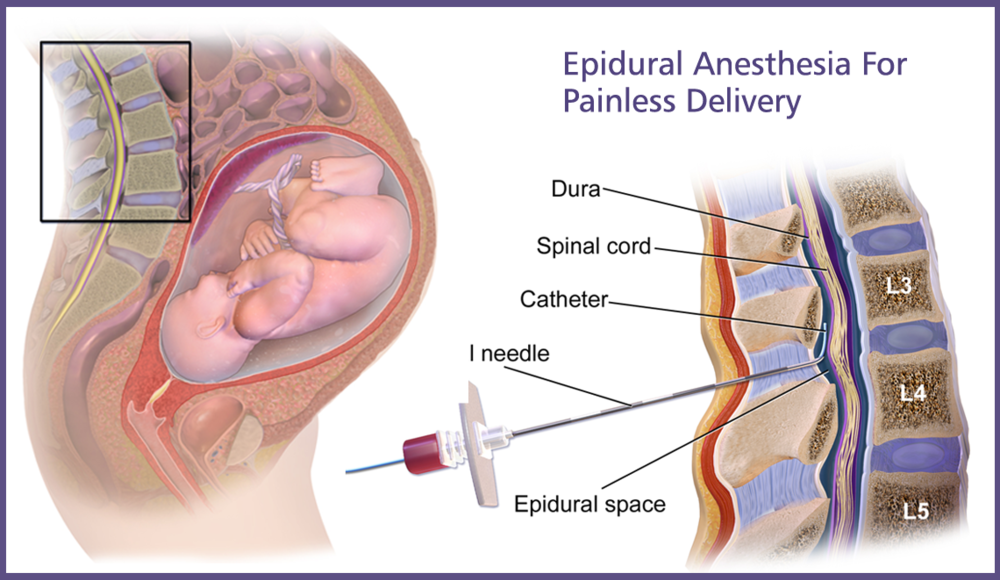 N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.
Thus, if the taxpayer submits to the tax authority a Certificate of payment for medical services, the taxpayer's failure to submit the relevant contract for the provision of medical services and (or) documents confirming payment cannot be grounds for refusing to provide such a deduction.
The amounts are based on payment data. Therefore, checks, an agreement and a clinic license are not needed to make a deduction.
Sample certificate attached.
Help Sample
Your application has been accepted, our specialists will contact you shortly!
Telephone
Comment
Epidural anesthesia for childbirth
Perinatal center
For an experienced anesthesiologist, this procedure is quite easy to perform. Epidural anesthesia greatly facilitates the course of childbirth, improves the well-being of the woman in labor and allows you to save strength and mood for the most crucial moments in childbirth. Up to 60% of women in labor worldwide prefer to give birth after epidural anesthesia.
Epidural anesthesia greatly facilitates the course of childbirth, improves the well-being of the woman in labor and allows you to save strength and mood for the most crucial moments in childbirth. Up to 60% of women in labor worldwide prefer to give birth after epidural anesthesia.
What is epidural anesthesia?
Epidural anesthesia refers to regional methods of pain relief, relieving pain only in a specific area of the body. The anesthetist places a thin catheter near the nerve roots between the lumbar vertebrae and injects a local anesthetic. The lower part of the abdomen and sometimes the legs “freeze”. Pain disappears, and the woman in labor can relax, and even sleep.
Pros and cons of epidural anesthesia for childbirth
Pain relief during childbirth with epidural anesthesia has several advantages over other methods:
- Clarity of consciousness. The woman in labor remains conscious, can control the course of childbirth, and after the baby is born, put him to the breast, hug and get incomparable emotions from the first meeting with the child.

- Security. Properly performed anesthesia does not affect the course of childbirth. The effect of epidural anesthesia on the child during childbirth is also absent.
- Flexibility of anesthesia. The presence of an epidural catheter allows you to control both the duration and depth of anesthesia.
- Maintains mobility in the first stage of labor. At the beginning of labor, when the contractions are not yet intense, a weakly concentrated solution of local anesthetic can be injected into the epidural catheter, while maintaining the sensitivity and mobility of the legs.
- Helps childbirth. After anesthesia, the contractility of the uterus normalizes, the opening of the cervix accelerates and the muscles of the pelvis relax a little.
- Fast conversion. If an emergency caesarean delivery becomes necessary during childbirth, a highly concentrated local anesthetic is sufficient to obtain complete anesthesia and immediately begin the operation.
Epidural anesthesia has some disadvantages:
- Lack of feeling or movement in the legs during intense contractions.
 With increasing intensity of contractions, large doses of pain medication may be required. This often leads to the fact that the woman in labor does not feel her legs. The effect is temporary, disappears a few hours after the cessation of the administration of the anesthetic.
With increasing intensity of contractions, large doses of pain medication may be required. This often leads to the fact that the woman in labor does not feel her legs. The effect is temporary, disappears a few hours after the cessation of the administration of the anesthetic. - Excludes alternative genders. Due to the lack of mobility in the legs, a bathtub or vertical birth becomes almost impossible.
- Violation of urination. Sometimes the help of a midwife is required to empty the bladder using a catheter. The problem disappears with the end of the anesthesia.
- Violation of thermoregulation and chills. In comfortable maternity boxes, this happens extremely rarely.
Contraindications for epidural anesthesia in childbirth
- Low blood clotting.
- Allergy to local anesthetics.
- Bacterial or viral infection of the skin at the insertion site of the catheter.
- Severe diseases and heart defects (the possibility of epidural anesthesia is discussed together with a cardiologist or cardiac surgeon).

- Severe liver disease causing decreased blood clotting and metabolism (destruction) of local anesthetics in the liver.
- Severe pathologies of the nervous system (demyelinating diseases and peripheral neuropathies).
- Tattoo at the puncture site. Tattooed skin is considered conditionally clean, prone to infection. This point is discussed individually at the consultation with the anesthesiologist.
- Patient's unwillingness. If there are no strict medical indications, then the refusal of a woman from epidural anesthesia for a doctor is also a contraindication to its implementation.
If epidural anesthesia is not possible, an experienced anesthesiologist will always suggest alternative methods of labor pain relief.
Consequences and complications after epidural anesthesia in childbirth
Possible complications may be associated either with a violation of the execution technique, or with the anatomical or physiological characteristics of the expectant mother.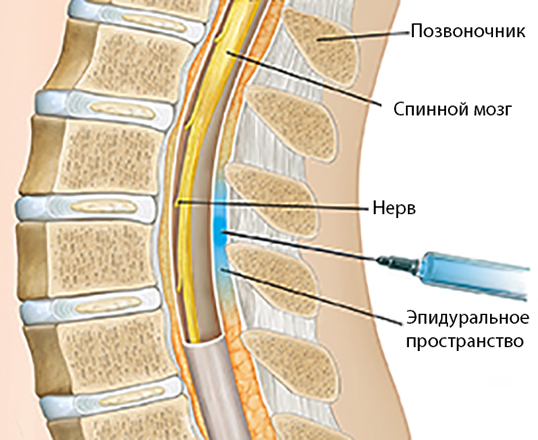
- Back pain (if the vertebrae or ligaments have been injured due to involuntary movement of the patient or unintentional mishandling by the anesthesiologist).
- Headache (if due to involuntary movement of the patient or inadvertent violation of technique, the dura mater has been affected).
- Longer urinary difficulty (after anesthesia wears off) if the woman is hypersensitive to local anesthetics.
- Sensitivity disorders due to traumatization of the nerve roots (due to involuntary movement of the patient or in the presence of anatomical features (scoliosis, disc herniation, fixed spinal cord syndrome).
- Decreased blood pressure when the patient is dehydrated (often occurs if the woman in labor independently restricts herself in the use of liquids).
- Pruritus with the use of opioid analgesics to enhance pain relief.
Discussing these complications with your anesthesiologist will help you avoid most problems.
Epidural anesthesia for childbirth in the maternity hospital EMC
Childbirth is the long-awaited end of pregnancy and the bright beginning of a new life. Therefore, we treat patients in the EMC maternity hospital with care, warmth and care. With state-of-the-art equipment and medicines, high professionalism and extensive experience, EMC anesthesiologists, together with your obstetrician-gynecologist and neonatologist, develop an individual plan for labor pain relief from the standpoint of safety and the concept of openness in anesthesia.
Many people ask what is the cost of epidural anesthesia during childbirth. At the EMC maternity hospital, pain relief does not need to be paid for separately, regardless of what contract you have.
Follow our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.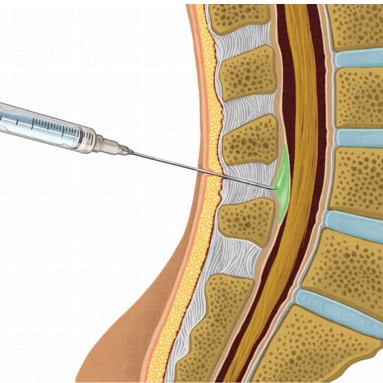 com/roddompravda/
com/roddompravda/
Cost of services
* Prices in the Price List are indicated in conventional units (unless otherwise specified by the Parties, 1 conventional unit is equal to 1 euro), all settlements under the Agreement are carried out in ruble terms. Payment under the Agreement is carried out by the Customer at the exchange rate of the Central Bank of the Russian Federation in force on the day of payment, if the rate of the Central Bank of the Russian Federation does not exceed the internal rate of the Clinic on the day of payment, indicated by posting on the Internet, on the official website of the medical centers of the Clinic, and on information stands in medical centers. If the exchange rate of the Central Bank of the Russian Federation exceeds the internal exchange rate of the Clinic on the day of payment, payment is made at the internal exchange rate of the Clinic.
| Designation | PRICE, USD* | Price, ₽ | Code |
| BIRTH PROGRAMS | |||
| Childbirth management program. VIP | 7 500 USD | 458 496 ₽ | The code: PRG87 |
| Childbirth management program. SUITE | 10 000 USD | 611 328 ₽ | The code: PRG88 |
Childbirth management program. EXCLUSIVE EXCLUSIVE | 12 000 USD | 733 594 ₽ | The code: PRG89 |
Specialists of the direction
All doctors
Perinatal center
Write to WhatsApp
Review of childbirth at the European Medical Center
October 30
All videos
Only the warmest and most pleasant memories of the maternity hospital remain!
Only the warmest and most pleasant memories of the maternity hospital remain! Real professionals work here, to whom you want to return with smiles and gratitude! First of all, I would like to note the people who played the most significant role in the birth of my son: The wonderful doctor Sharova Marina Lvovna, thanks to whom a very difficult and lengthy birth ended easily and without complications! Marina Lvovna is a doctor who pays great attention to the wishes and feelings of the patient regarding the process of childbirth, and she really did everything possible to make everything go exactly as I wanted.