Why do nipples bleed
Causes With and Without Breastfeeding
Is this cause for concern?
Oftentimes, bleeding nipples aren’t cause for concern. They’re usually the result of some sort of trauma or friction, like your nipple rubbing against a scratchy bra or shirt material.
Bloody or otherwise, abnormal nipple discharge is relatively common, regardless of whether you’re breastfeeding. About 5 percent of women who seek treatment for breast-related symptoms go to the doctor because of abnormal nipple discharge.
Keep reading to learn more about what may be causing your nipples to bleed, what you can do to find relief, and when to see your doctor.
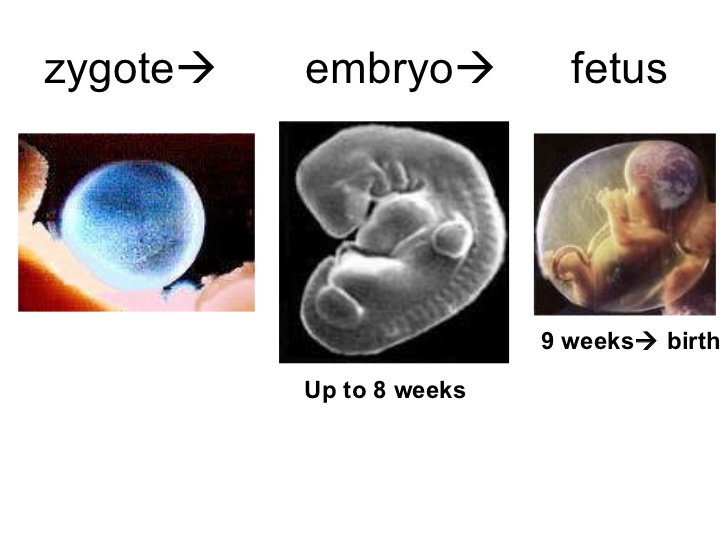
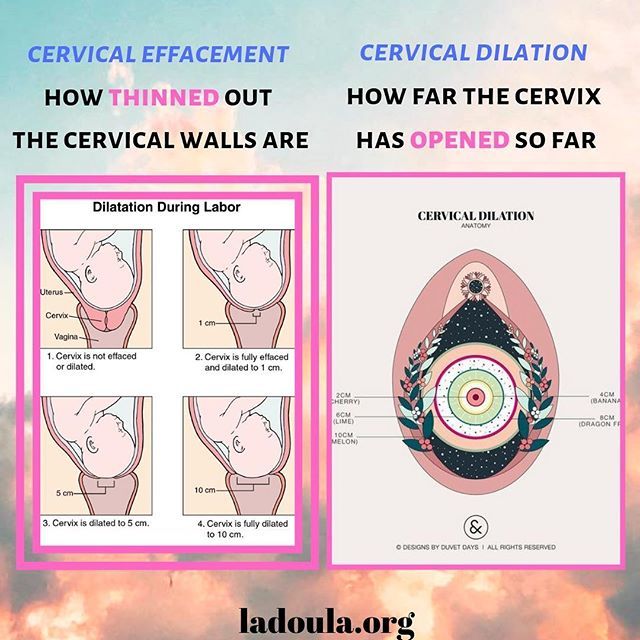
For first-time moms, breastfeeding can take some time to master. In the first few days, your nipples may become sore and cracked. There might be bleeding cuts on the nipple or the colored area around the nipple (areola).
But breastfeeding shouldn’t be painful or cause bleeding. If your nipples continue to bleed during the first few days or weeks of breastfeeding, it may be because your baby isn’t latching properly.
Other signs of a poor latch include:
- flat, wedged, or white nipples at the end of a feed
- severe pain throughout a feed
- your baby seems unsettled or still hungry after a feed
- the bottom part of your areola isn’t in the baby’s mouth
If you’ve been breastfeeding for a few months and suddenly develop pain, it could be a sign of infection. About 10 percent of women who breastfeed develop an infection at some point.
What you can do
If you have pain during breastfeeding, try putting a finger in your baby’s mouth to break the seal, and then reposition your child. A deeper latch ensures that the nipple is deep in the mouth where the baby’s palate is softer.
A baby latched on to the nipple only will do damage quickly, so you want the baby fully latched on to the breast, with the nipple centered and deep in the baby’s mouth.
It may also be helpful to talk to a lactation specialist about effective latching techniques. The hospital where you gave birth should have one available.
You can also join La Leche League’s online peer support group to talk with other breastfeeding moms about their experiences. You baby, and your breasts, will thank you.
Bleeding can also result from skin conditions that cause dryness and cracking, such as contact dermatitis or dry skin.
Contact dermatitis happens when your skin comes into contact with an irritating substance. This could be a new soap, laundry detergent, or an industrial cleaner on a new bra.
Dry skin often results from exposure to cold and heat. For example, your nipples may be dry and cracked because of exposure to hot water in the shower. This irritation can be made worse by tight-fitting clothing.
Other symptoms may include:
- itchiness
- rashes
- scaly skin
- blisters
What you can do
Try to identify what’s causing your nipple irritation and avoid it. In general, fragrance-free products tend to be gentler on sensitive skin. Warm showers are also better than hot.
When skin cracks, it’s important to prevent infection. Keep the area clean with soap and water and apply an antibiotic ointment, such as Neosporin, until it heals. If the condition continues, see your health care provider for prescription creams.
A new nipple piercing takes two to four months to heal, during which time, it may bleed. Infections, which can develop both during and after healing, can also cause a collection of pus (an abscess) to form inside the nipple or areola.
Anything that breaks the skin can cause bleeding and lead to infection. Most nipple piercings are done under sterile conditions, but other nipple trauma may introduce bacteria. This can happen during rough nipple stimulation, especially when the skin is broken by bites, nipple clamps, or other sex toys.
Symptoms of infection include:
- redness and inflammation
- pain or tenderness to the touch
- pus or abnormal discharge
What you can do
Keep the area around your piercing or wound as clean as possible. Wash with soap and warm water or an antiseptic wash, such as Bactine. Soaking your piercing in a solution of warm water and salt several times per day can also help treat and prevent infection.
Wash with soap and warm water or an antiseptic wash, such as Bactine. Soaking your piercing in a solution of warm water and salt several times per day can also help treat and prevent infection.
If you develop an abscess or experience severe pain, you should go to your doctor immediately. Your doctor can drain the wound and prescribe a course of oral antibiotics.
Mastitis is a breast infection that causes pain and redness. It’s most common in women who are breastfeeding, but it can happen to anyone. It often occurs within three months of giving birth.
Mastitis usually doesn’t cause nipple bleeding. It’s often the other way around; cracked, damaged, bleeding nipples provide an entry point for bacteria, which can lead to a mastitis infection.
Symptoms of mastitis include:
- breast pain or tenderness
- warm to the touch
- general flu-like feeling
- breast swelling or lump
- pain or burning while breastfeeding
- breast redness
- fever and chills
What you can do
If you suspect you have mastitis, see your doctor. Most cases are treated with 10 to 14 days of oral antibiotics. You should feel better within a few days, but take it easy for the next week or two.
Most cases are treated with 10 to 14 days of oral antibiotics. You should feel better within a few days, but take it easy for the next week or two.
The doctor will prescribe an antibiotic safe for breastfeeding, and breastfeeding should continue. Engorgement can make the problem worse when you are breastfeeding.
If an abscess develops near the nipple, it may need to be drained. With your doctor’s permission, you can treat pain and fever with over-the-counter (OTC) pain relievers that help reduce swelling. Popular options include ibuprofen (Advil) and naproxen (Aleve).
Intraductal papillomas are one of the most common causes of a bleeding nipple, especially if blood is flowing out of the nipple, similar to milk. They’re benign (noncancerous) tumors that grow inside the milk ducts.
These tumors are small and wart-like. You may be able to feel one behind or next to the nipple. They’re usually quite close to the nipple, which is why they cause bleeding and discharge.
Other possible symptoms include:
- clear, white, or bloody nipple discharge
- pain or tenderness
What you can do
If blood is flowing directly out of your nipple, see your doctor. Your doctor can diagnose your symptoms and advise you on next steps. If you’re dealing with an intraductal papilloma, they may recommend surgically removing the affected ducts.
Nipple discharge is traditionally regarded as a symptom of breast cancer, but this symptom isn’t that common.
About 3 to 9 percent of women treated at breast cancer clinics present with nipple discharge. It isn’t clear whether this includes bloody discharge. However, a lump or mass is usually present in these cases.
Current research is exploring the potential relationship between nipple discharge color and cancer severity. Although one 2016 study suggests that blood-colored discharge may be associated with malignant (invasive) breast cancers, more research is needed to confirm these findings.
Intraductal carcinoma
The type of breast cancer that someone has is determined by the specific area where it starts:
- Carcinomas are tumors that can grow in organs and tissues throughout the body.
- Ductal carcinomas are tumors that start inside the milk ducts.
- Intraductal carcinoma, also called ductal carcinoma in situ (DCIS), is the most common type of noninvasive breast cancer. About one in five new breast cancers are DCIS.
DCIS is noninvasive because it hasn’t spread beyond the milk duct to the rest of the breast. But DCIS is considered pre-cancer because it could eventually become invasive, though this is unlikely. DCIS usually doesn’t cause symptoms. It’s typically discovered during a mammogram.
Lobular carcinoma
The lobules are the glands in the breast responsible for producing milk.
- Lobular carcinoma in situ is another type of pre-cancer that doesn’t spread to the rest of the breast.
- Invasive lobular carcinoma is cancer that has spread beyond the lobule, potentially to the lymph nodes and other parts of the body.

Invasive lobular carcinoma is relatively rare. About 8 out of 10 invasive breast cancers begin in the milk ducts (invasive ductal carcinoma), not the glands.
Early lobular carcinoma has few symptoms. Later, it may cause:
- an area of thickening in the breast
- an unusual area of fullness or swelling in the breast
- a change in the texture or appearance of breast skin (dimpling or thickening)
- a newly inverted nipple
Paget’s disease
Paget’s disease of the breast is a rare type of breast cancer that starts on the nipple and extends to the areola. It most often affects women of age 50 or older.
Paget’s disease most often occurs in conjunction with another form of breast cancer, usually ductal cancer in situ (DCIS) or invasive ductal carcinoma.
Symptoms of Paget’s disease include:
- crusted, scaly, and red nipple and areola
- bleeding nipple
- yellow nipple discharge
- flat or inverted nipple
- burning or itching nipple
How breast cancers are treated
Doctors consider many different factors before recommending a certain breast cancer treatment. This includes:
This includes:
- the type of breast cancer
- its stage and grade
- its size
- whether the cancer cells are sensitive to hormones
Many women choose to undergo surgery for breast cancer. Depending on the size and grade of your tumor, surgery may involve removing the lump (lumpectomy) or removing the entire breast (mastectomy).
Surgery is often combined with additional treatments, such as chemotherapy, hormone therapy, or radiation. In its early stages, some breast cancers can be treated with radiation alone.
If bloody nipple discharge lasts for more than a day, make an appointment to see your doctor. Your doctor will run imaging tests to look for anything abnormal inside the breast. This may include an ultrasound, MRI, or mammogram.
See your doctor immediately if you notice any of the following:
- a new lump or bump
- dimpling or other texture changes
- newly inverted or flat nipple
- peeling, scaling, crusting, or flaking of the areola
- redness or pitting of the skin on the breast
- changes in the size, shape, or appearance of the breast
Cuts, cracks, or other damages to the skin on your breast don’t necessarily require immediate treatment. If symptoms don’t improve or if you notice signs of an infection, call your doctor. Signs of infection include:
If symptoms don’t improve or if you notice signs of an infection, call your doctor. Signs of infection include:
- fever and chills
- redness
- breast hot to the touch
- pain or severe tenderness
Causes and when to see a doctor
Causes of bleeding nipples vary. While it is more common in females, males can also experience bleeding nipples.
Some causes of bleeding nipples relate to breastfeeding or the milk ducts. Other causes include irritation, infection, and less frequently, specific diseases.
In this article, we examine several causes of bleeding nipples and the symptoms that may occur alongside them. We also look at when a person should see a doctor, and what treatment approaches may be available.
Breastfeeding is a common cause of nipple pain. Some women experience severe irritation when breastfeeding, which can sometimes result in bleeding nipples.
Not all nipple pain occurs immediately after giving birth. One study found that over one-third of women were still having difficulties with nipple pain at 2 weeks and 1 month after birth.
Despite being a common problem for people who breastfeed, there is a lack of research into treatments for nipple pain as a result of breastfeeding.
Some experts believe that nipple pain occurs as a result of poor positioning during breastfeeding or babies latching incorrectly to the nipple. One study indicated that teaching babies between 4 days and 12 months old how to latch correctly stopped the breast pain in 65% of cases.
However, researchers still need to do more investigations into how positioning affects nipple pain.
Nipple pain while breastfeeding can also occur due to the following:
- flat or inverted nipples
- friction-causing or overly strong sucking from the baby
- differences in the baby’s mouth, such as palatal anomalies including ankyloglossia, or tongue tie
- milk blisters
- infections
- psoriasis
- dermatitis
- Raynaud’s phenomenon
Where friction causes nipple pain, applying vitamin A ointment or highly-purified anhydrous lanolin may alleviate the pain.
One small study highlights that it might be beneficial to lie down when breastfeeding a baby with palatal anomalies, such as cleft palate. However, scientists need to carry out more studies, as the researchers only found this indication in one case.
Thrush, or oral candida infection, is an oral infection that some infants might transfer to people via breastfeeding. It is the most common oral fungal infection in infants, making it a widespread problem for people who breastfeed. Severe irritation could result in bleeding nipples.
Babies that have an oral candida infection will have white patches and painful, shiny red patches in their mouth.
A person with nipple thrush can experience symptoms, such as:
- severe, burning nipple pain
- flaking nipple or areola skin
- sharp pains in the breast
- painful breast without lumps
Treatment for a thrush infection includes practicing proper hygiene, changing the diet to eliminate sugars and refined carbohydrates that feed candida infections, and eating a variety of vegetables and nutrients. In some cases, a doctor may prescribe medication.
In some cases, a doctor may prescribe medication.
Mastitis is an infection caused by ectasia, or the widening of the breast milk ducts. Mastitis is most common in women who are breastfeeding, but it can occur in women who are not breastfeeding and also in men.
Risk factors include:
- obesity
- diabetes
- smoking
- having given birth recently
Treating mastitis in women who are breastfeeding may involve:
- treatments to drain the breast, such as continued breastfeeding
- antibiotics
- painkillers, such as ibuprofen
- applying warm compresses before and after feeding
- resting and avoiding stress
- changing feeding positions
Sometimes, problems with the milk ducts cause bleeding nipples.
Conditions include:
Duct ectasia
Share on PinterestDuct ectasia is most common in women in their late 40s and 50s.
Ectasia is a noncancerous condition that occurs when the breast milk ducts become wider. Milk ducts sometimes become blocked, and this can lead to infection.
Milk ducts sometimes become blocked, and this can lead to infection.
Ectasia is most common in women in their late 40s and 50s.
Other potential symptoms include:
- tender or painful breasts
- nipples that go inward
- sticky nipple discharge
- a lump behind the nipple
- an abscess or fistula
People can sometimes treat ectasia with warm compresses. Ectasia can also occur due to an infection, such as mastitis. If this is the cause, a doctor may prescribe antibiotics.
Dermatitis can also cause bleeding nipples. This refers to inflammation of the skin. Dermatitis may appear as an itchy, scaly, red rash on either the nipple or the darker area surrounding the nipple, the areola.
Irritation, infection, or allergy can also cause dermatitis.
Objects that can trigger dermatitis include irritating fabrics, detergents, and soaps. Avoiding scented products and choosing hypoallergenic products without chemicals, perfumes, and dyes can help prevent symptoms of nipple dermatitis.
Many forms of dermatitis fall under the category of eczema. Nipple eczema most often occurs in people who have a history of eczema. People who are breastfeeding can also develop this condition.
Learn more about ways to treat eczema here.
Intraductal papilloma
These harmless tumors found in the breast milk ducts are a common cause of bleeding from one or both nipples.
Often, intraductal papilloma will appear as either one lump near the nipple or several smaller lumps spread out across the breast.
These tumors can appear in people of any age but are most common in women aged between 35 and 55 years old. They can also occur in men but are much less common.
Intraductal tumors are more likely to develop according to individual risk factors, such as:
- contraceptive use
- hormone therapy
- estrogen exposure
- family history of breast tumors
Share on PinterestBleeding nipples can be a symptom of cancer, but they are rarely the only symptom.
While uncommon if bleeding nipples are the only symptom, sometimes bleeding nipples can be a symptom of cancer.
Other symptoms that might suggest cancer include:
- a lump occurring alongside discharge
- nipple discharge that does not improve with hygiene and cleanliness measures
- breast pain
- swelling of some or all of the breast
A rare condition associated with breast cancer, Paget’s disease has symptoms that are similar to eczema or psoriasis. A red, scaly rash will appear on the nipple, and bleeding may occur. The nipple may be sore and can become scabby. This condition appears in 1–4% of breast cancer cases.
If a doctor suspects that a person has Paget’s disease, they will order a biopsy.
Anyone experiencing new symptoms should see a doctor, particularly if they come on quickly. When a person has bleeding nipples, they should see a doctor, especially if the symptoms are painful or if they have other symptoms, such as a lump in the breast. While lumps are not usually serious, it is important to see a doctor for an examination.
While lumps are not usually serious, it is important to see a doctor for an examination.
A few different underlying conditions can cause bleeding nipples. These include breastfeeding, irritation, allergy, infection, and tumors.
If breastfeeding causes bleeding nipples, try to find a way to improve latching or speak to a doctor.
If an allergy is causing the problem, a doctor may recommend a steroid cream. In the case of an infection, doctors typically prescribe antibiotics.
Cracked nipples | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs A. et al., "Recommendations S -3 for the management of inflammatory breast disease during breastfeeding: guidelines AWMF , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs A. et al., "Recommendations S -3 for the management of inflammatory breast disease during breastfeeding: guidelines AWMF , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
- Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent sore nipples in the mother", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012).
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma. J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).
J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).
Hale, T.W., & Rowe H.E., Medications and mothers' Milk 2014 (Hale Publishing, Plano, 2014). - Hale T . and Row X . and ., " medicinal Preparations in Maternal milk ". Publishing Hale
Nipple fissure: Methods of treatment - ProMedicina Ufa
Nipple fissure - a defect, damage to the integrity of the skin on the nipples of the mammary glands. It is manifested by a sharp soreness with irradiation to the shoulder blade when feeding a child. It can be complicated by infection of wounds, the development of candidiasis on the nipple, mastitis. If cracks become infected, there is a risk of infection of the child during feeding.
It can be complicated by infection of wounds, the development of candidiasis on the nipple, mastitis. If cracks become infected, there is a risk of infection of the child during feeding.
Treatment of cracked nipples begins with the elimination of their cause. In parallel, they carry out the prevention of their infection, use means that promote the speedy healing.
Causes
The main reason for the appearance of cracks is the lack of breastfeeding during feeding. When properly applied to the breast, the nipple rests against the baby's palate in a fixed motionless position, the child squeezes the areola with its jaws, contributing to the outflow of milk. In this case, the lower lip of the child is tucked up. If the nipple is not inserted to the proper depth, then it ends up on the tongue, gaining mobility, the lower lip injures the nipple and areola, and the jaws compress the breast in the most sensitive and easily damaged place. As a result of constant irritation of the nipple and areola areas, damage to the skin occurs - cracks form.
The second most common cause of cracked nipples can be improper weaning. Often, when feeding, mothers do not support the child's head, and also place his stomach not towards himself, but up. As a result, at the end of feeding, the child turns away from the breast, pinching the nipple in the jaws. There is pressure on areas of the nipple that are not intended for this.
Another common cause is washing your nipples too often. Modern medicine does not support the need to wash the breast after each feeding. With frequent washing, the nipples are washed off their natural lubricant, which is secreted by special glands in the skin of the areola (Montgomery's glands) and the nipples lose one of their natural protective mechanisms.
Fissures can also develop when feeding older children as a result of bites from erupted teeth.
The development of thrush contributes to the occurrence of cracked nipples.
Symptoms
Symptoms that may appear both in the early periods of feeding and later:
- single or multiple lesions of the skin of the breast, nipples and areals;
- surface cracks that will show up on contact with underwear;
- subcutaneous fissures, characterized by severe pain;
- bleeding;
- slight suppuration;
- increased sensitivity and soreness of the nipples;
- Excessively dry skin around the nipples and areolas.

Even if you notice that at least one of the above symptoms appears from time to time and then disappears, this can also be an important signal of a possible infection or the presence of any other disease.
Treatment of cracked nipples
If it is a small cracked nipple, treatment can be started at home. The first step is to prevent infection. Change your underwear every day, iron your bra after washing with a hot iron. Put disposable sterile pads inside the bra and change them when they become damp.
Do not wash your breasts after each feeding, so as not to violate the natural protection. Mother's milk itself is a good antiseptic, so it can be used as a cream for cracked nipples, squeezing a few drops after feeding. Be sure to let the milk dry, hold your chest open for a few minutes.
Previously, when nipple cracks appeared, treatment was started with brilliant green. You should not do this, as it has been proven that brilliant green is quite toxic. It is better to use a methylene blue aqueous or alcohol solution as an antiseptic, this antiseptic will also serve to prevent thrush in a child. It should be noted that antiseptics cannot solve the problem of how to treat nipple cracks, they only prevent infection.
Cracked nipples can be lubricated with castor oil to soften the skin and heal quickly. It can be replaced with sea buckthorn or rosehip oil. Oil is applied to cracked nipples after feeding. Be sure to wait until it dries, and only then put on a bra.
Compresses for cracked nipples can be made from butter and applesauce. Apples need to be rubbed on a grater, add butter to them in a ratio of 1: 1 and attach to the chest. Hold the compress for 2-3 hours.
Kalanchoe or aloe juice has an excellent healing effect. The leaves of the plants are cut in half and smeared with pulp on the cracks in the nipples. Juice can be squeezed out and compresses can be made from it.
Cracked nipples during feeding can also be treated with products from a pharmacy.