Special care nursery vs nicu
Special care nursery (SCN) | Pregnancy Birth and Baby
Special care nursery (SCN) | Pregnancy Birth and Baby beginning of content5-minute read
Listen
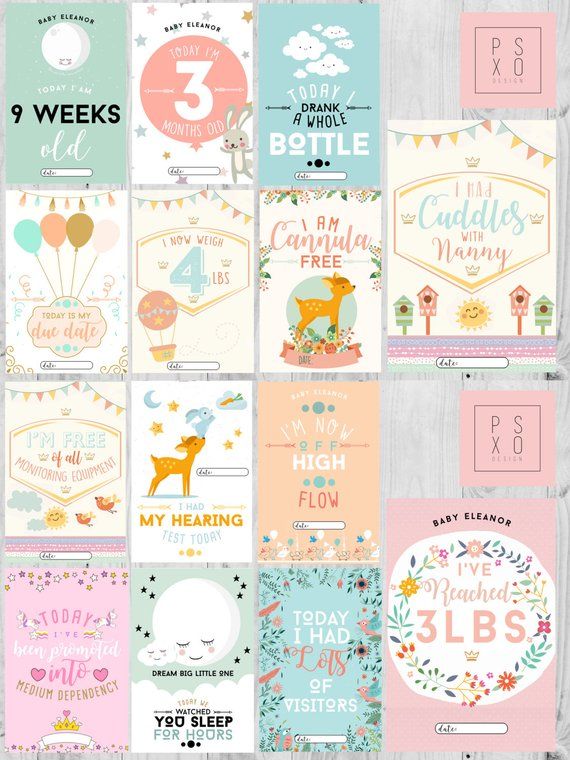
Some babies will need to spend time in a special care nursery, or ‘SCN’, after they are born. They may be admitted to an SCN for several reasons, but it’s important to know that even if your baby can't leave hospital straight away, they are on the road to becoming stronger.
What is a special care nursery?
Babies are admitted to a special care nursery (SCN) when they need extra care from specially trained staff. Your baby may need this care even if they can maintain their own body temperature and generally breathe on their own.
An SCN is different from a neonatal intensive care unit (NICU), where the babies are more seriously ill or premature, and need closer observation and care. If your baby is in an SCN, their health is more stable and they are stronger than babies who are in a NICU.
Babies may need to be in a special care nursery because:
- they were born prematurely and need extra care
- they may have health issues such as jaundice, low blood sugar or temporary breathing problems
- they were born with a low birth weight
- they were moved from a NICU as their health improved
In an SCN, you will often receive help with feeding and preparing to take your baby home.
Special care nursery staff
There may be different types of trained staff in a special care nursery:
- neonatologists, who specialise in looking after premature or ill newborns
- paediatricians
- nurses and midwives with special training in neonatal care
- lactation consultants
- allied healthcare providers such as physiotherapists, speech pathologists and occupational therapists
- other medical specialists such as anaesthetists or surgeons, if your baby needs them
And as a parent, you are of course considered an important part of your baby’s healthcare team.
What you can expect to see in a special care nursery
If your baby has been moved from a NICU, you will notice that much of the specialised equipment that you saw there is not in the special care nursery.
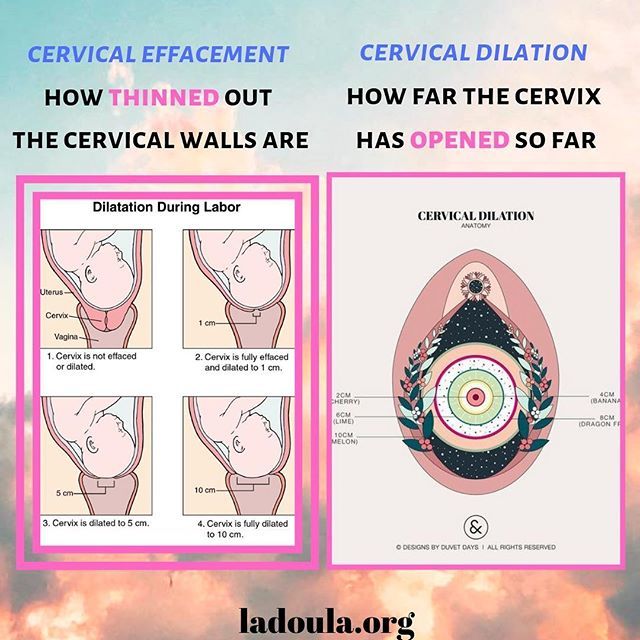
In an SCN, your baby may start off sleeping in an incubator (also known as a 'humidicrib') then move into an open cot. There may be equipment in the room that monitors your baby’s oxygen level, heart rate and breathing, or to treat jaundice. Nursery staff will explain any equipment or procedures that your baby will need.
The environment in a special care nursery is likely to be quiet, and you will be asked to whisper or talk quietly. This is because a low noise level is important for your baby’s brain development and to keep them calm. There may be a quiet ‘baby rest’ period during the day, when your baby can sleep undisturbed, with little noise or handling.
Contact with your baby
You can see your baby as often and for as long as you like in the SCN, and staff will encourage you to have plenty of hands-on contact. This includes holding, feeding ,changing nappies and bathing your baby.
This includes holding, feeding ,changing nappies and bathing your baby.
Other members of your family, such as grandparents or your other children, can visit – although you may be restricted to 2 or 3 people visiting at any one time.
Hygiene in the SCN
It’s important that your baby’s environment is clean and free of germs since babies in a special care nursery are more prone to catching infections. Visitors will need to use the nursery’s hand washing and sanitising facilities.
People should also avoid visiting your baby if they are unwell – for example, if they have a cold, diarrhoea or are vomiting. If you’re not sure about the health of a visitor – or yourself – speak with your baby’s doctor or a staff member in the nursery.
Feeding your baby
Your baby may need to be fed using a tube before they are strong enough to take milk from your breast or a bottle. You will be encouraged to give your baby breastmilk if you want to, and a lactation specialist may be available to support you. You may be shown how to express milk by hand or by using a breast pump.
You may be shown how to express milk by hand or by using a breast pump.
When will my baby be discharged?
Your baby is likely to be discharged when:
- they have reached their due date
- they can regulate their own body temperature, in a cot
- they are a suitable weight
- feeding has been established
- they have finished any intravenous medications
How you might be feeling
You may have mixed feelings about your baby being in a special care nursery. These feelings may range from being overwhelmed by the equipment to being happy and excited that your baby has moved from the NICU. You may, in fact, be anxious that they are receiving less intensive care than in the NICU.
It’s possible that you may need to go home before your baby does, or your baby may be transported to a special care nursery in a hospital closer to your home. But you can ask the SCN staff any questions at any time, as well as talk to them about how you are feeling.
For more help and information
- Speak with your baby’s doctor or midwife.
- Speak with other staff in your baby’s special care nursery.
- Call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.
Sources:
Raising Children Network (Special care nursery - life after the NCIU), ACT Health (Neonatal Intensive Care Unit NICU and Special Care Nursery SCN), North Shore Private Hospital (Special care nursery), NSW Health (NSW Maternity and Neonatal Service Capability Framework Guideline), Better Health Channel (Specialised care for your baby), Queensland Health (Baby - Special care nursery), The Wesley Hospital (Special care nursery)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Baby's first 24 hours
- Choosing where to give birth
- Health professionals involved in your pregnancy
- Premature baby
- Neonatal intensive care unit (NICU)
- Birth trauma (emotional)
- Birth injury (to the baby)
Need more information?
Special care nursery: life after the NICU | Raising Children Network
If your baby is moving from the NICU to the special care nursery, it helps to know what to expect. Read how special care nursery is different from the NICU.
Read more on raisingchildren.net.au website
Going Home - Miracle Babies
Congratulations on your miracle baby's graduation from NICU/ SCN
Read more on Miracle Babies Foundation website
In Hospital - Miracle Babies
Having a baby born premature or sick is usually a very different path than what you had expected
Read more on Miracle Babies Foundation website
8 things I wish I knew as a NICU Dad - Miracle Babies
Read more on Miracle Babies Foundation website
Specialised care for your baby - Better Health Channel
If your baby is sick at birth or born too early (premature) they will be cared for in a Neonatal Intensive Care Unit (NICU) or Special Care Nursery (SCN) by highly experienced medical and nursing staff.
Read more on Better Health Channel website
Premature baby
Preterm labour is when you go in to labour before your pregnancy reaches 37 weeks. Here's what to expect when you have your baby prematurely.
Read more on Pregnancy, Birth & Baby website
Premature birth: coping with your feelings | Raising Children Network
After a premature birth and while caring for a premature baby, it’s normal to have powerful and mixed feelings. Here’s how to cope with your feelings.
Read more on raisingchildren.net.au website
Pregnancy care & birth at birth centres | Raising Children Network
Birth centres support healthy women with low-risk pregnancies to give birth in a home-like environment. Pregnancy care at birth centres is led by midwives.
Pregnancy care at birth centres is led by midwives.
Read more on raisingchildren.net.au website
Pregnancy care & birth: private hospitals | Raising Children Network
Private hospitals offer comfortable, caring birth environments. Private obstetricians look after pregnancy care for women having a private hospital births.
Read more on raisingchildren.net.au website
Neonatal Care - Miracle Babies
As parents, you eagerly look forward to welcoming your baby into the world and bringing your new family member home
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Specialised care for your baby
Newborn babies need close observation and care when they are sick at birth or born too early (premature). Neonatal Intensive Care Units (NICUs) and Special Care Nurseries (SCNs) provide extra care for these babies in the first weeks, and sometimes months, of their lives.
Learning that your baby needs to be admitted to a special care unit is stressful, especially after a difficult birth. It will be strange at first, but for a while this will be your newborn baby’s home and you will be an important part of their healthcare team.
Your baby will be cared for by highly experienced medical and neonatal nursing staff with specialist skills to support feeding, breathing and early development.
Types of specialised care for babies
If your baby needs specialised care that cannot be provided in the maternity ward, or in the hospital where they were born, they may need to be transferred to a higher level of care, either in a Neonatal Intensive Care Unit or a Special Care Nursery.
Neonatal Intensive Care Units
Neonatal Intensive Care Units (NICUs) provide services to newborn babies who need special treatment for critical illnesses straight after birth. NICUs are in larger, metropolitan hospitals. In Victoria, these hospitals are:
- Mercy Hospital for Women, Heidelberg
- Monash Medical Centre, Clayton
- Royal Children’s Hospital, Parkville
- Royal Women’s Hospital, Parkville.
Special Care Nurseries
A Special Care Nursery (SCN) looks after babies who are healthier and stronger than the babies in the NICU, but still need extra care. They may be premature babies, or have a low birth weight or need specific care for neonatal health issues.
Emergency transfer to specialised care
If the level of care for your baby needs to change, this can sometimes mean moving hospitals. At such times, Paediatric Infant Perinatal Emergency Retrieval (PIPER) coordinates expert advice, referral and transport to specialised services in Victoria and interstate, 24 hours, 7 days a week. This includes both urgent transfer and non-urgent and ‘back transfer’ to special care nurseries.
The emergency transfer service for newborn babies in Victoria is known as NETS (Newborn Emergency Transport Service).
Find more information about NETS.
Equipment and monitoring in the NICU
You may be worried at first by the amount of equipment, cords and monitors on or near your baby when they are in the NICU.
It is very important to keep your baby warm and comfortable. To keep them at their ideal temperature they will either be in an incubator, which looks like a see-through plastic box on wheels, or in a heated open cot with overhead heaters or mattress heating.
Depending on what they need, your baby may have:
- leads on their chest to monitor their heart and lungs
- breathing support through a ventilator machine
- a narrow tube and needle in their hand or foot to provide intravenous (IV) fluids
- sensors on their foot or hand to monitor oxygen
- a catheter in the umbilical cord
- feeding tubes and a pump.
A nurse will explain the equipment, what it is doing and how you can help.
Your baby’s healthcare team
Your baby and your family will be looked after by a team that could include:
- specialist doctors (neonatologists and paediatric specialists)
- specialist nurses
- technicians (laboratory, echocardiogram and x-ray)
- care managers
- physiotherapists, speech pathologists and occupational therapists
- lactation consultants
- social workers, mental health professionals and pastoral care workers.
Each member of the healthcare team will have different skills and expertise. A care manager will usually look after the ‘big picture’ and help coordinate the team.
A care manager will usually look after the ‘big picture’ and help coordinate the team.
You will meet your care manager soon after you arrive at the specialised care unit. They will help you to settle in, show you around and explain how things work.
Sharing information about your baby’s health
You are an important member of your baby’s healthcare team. You can usually call the ward at any time to check on your baby and ask questions.
Each hospital will have a different system for communication. Often there are whiteboards near your baby’s cot for messages.
In the NICU, each baby will have an individual bedside nurse, who will know most things about your baby’s medical condition and will be able to bring you up to date about recent test results, or any changes in your baby’s care.
A neonatologist will also be on duty at all times.
Medical staff will share information during daily medical rounds where they discuss each baby’s status and progress. You can ask questions and share information during these rounds. More complex discussions are better suited to a dedicated family meeting with a healthcare professional.
You can ask questions and share information during these rounds. More complex discussions are better suited to a dedicated family meeting with a healthcare professional.
Visiting the specialised care unit
Parents can usually visit their baby at any time. Sometimes you will have a swipe card that will give 24-hour access. The space around your baby's cot is yours. You may like to bring in things like photos, toys and cards to make the space more personal.
Overnight stays
Each hospital will have different arrangements for parents to stay overnight if needed. Sometimes there is accommodation nearby, or a family room where you can sleep for a night. Ask your care manager or nurse about the options.
Limits on visitors
Often there is a period every day where there are limits on visitors. This may be during ward rounds or during a ‘baby rest time’.
Hospitals usually limit the number of visitors who can be near the baby’s bed. Most hospitals allow a maximum of three (one parent and two others) at any one time. If you have a larger group to look after, ask the nurses if there is a family room nearby where you can meet.
If you have a larger group to look after, ask the nurses if there is a family room nearby where you can meet.
Children under 12 years old, other than your own, are usually not allowed to visit.
Illness and risk
If someone is unwell or has an infection, they should not visit your baby in the special care nursery. This includes colds, fever, diarrhoea and vomiting. If you are not sure about the risks or symptoms, talk to your care manager or your baby's doctor.
Food and drink
Hospitals will usually not let you bring your own food and drink into a special care unit for hygiene and safety reasons. Often there is a family room nearby where you can eat, drink and store food.
Infection control
Infection control is especially important in neonatal and special care units. Hand washing is a good way to limit the spread of germs. Hospital staff will show you how to wash up to the elbows for best results.
Immunisation against common infectious diseases such as whooping cough, influenza, chicken pox and measles can also reduce the risk of infection to babies in a special care unit.
Immunisation of a premature baby
All of the routine immunisations are safe for immature and low birth weight babies and should be administered according to the Australian National Immunisation Program Schedule. Some preterm babies may require extra doses due to the immaturity of their immune system at birth but most babies develop full immune maturity in the third trimester. Reactions to immunisation may occur but the risk is similar for all infants regardless of their birth weight, their gestation or how old they are when they receive the immunisation. Premature babies are at higher risk of developing infections than babies born at term. They are also more likely to suffer serious complications form these illnesses.
Feeding your baby in specialised care
At first, your baby may not be able to breastfeed when they are in neonatal intensive care or special care. A tube may be used to feed your baby until they are stronger and can be fed by mouth.
Expressing milk after delivery
Breastmilk contains all the nutrients your baby needs, and can help to protect them from infection. For this reason, whether your baby is being tube-fed or can feed by mouth, you will be encouraged to provide breastmilk.
For this reason, whether your baby is being tube-fed or can feed by mouth, you will be encouraged to provide breastmilk.
After your baby is delivered, your breasts produce colostrum. This first milk will be collected in syringes and fed to your baby. Even small amounts of colostrum have great benefits for your baby.
A nurse or lactation consultant will show you how to express by hand soon after your baby is born. They will also show you how to use a breast pump to express larger amounts. Expressing milk every few hours will not only provide food for your baby while in specialised care, but will help to keep up a good supply for when they are able to breastfeed directly.
Excess breastmilk can be stored and used later. This can be useful for times when you are not able to be at the specialised care unit.
Formula feeds
If you choose not to breastfeed your baby, the healthcare team will discuss artificial feeding using formula. Sometimes, even when you are breastfeeding, there is not enough milk available for your baby.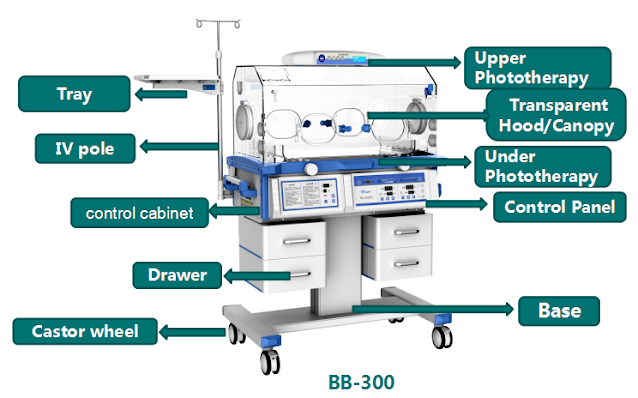 A nurse or lactation consultant will talk to you about adding formula feeds and ways to increase your milk supply.
A nurse or lactation consultant will talk to you about adding formula feeds and ways to increase your milk supply.
Emotional support for families with babies in specialised care
Extended time in hospital for your baby can place a great strain not only on parents but also on extended family. A social worker will talk to you and your family about what type of support can help while your baby is in hospital and after you return home.
Social workers can provide:
- counselling
- emotional support
- referrals to internal and external services
- information on topics such as parenting, bonding with your baby and coping strategies.
Leaving the specialised care unit
Finding out that your baby can move from intensive or special care is exciting news. Often this means you can take your baby home. Sometimes it will mean that your baby can be moved to a hospital closer to home because they are more stable and healthy.
Decisions about discharge
Leaving the security of the hospital can be daunting. The healthcare team will not arrange for discharge until they feel that your baby is well enough to stay healthy in a home environment and that you are capable of giving your baby the care they need.
The healthcare team will not arrange for discharge until they feel that your baby is well enough to stay healthy in a home environment and that you are capable of giving your baby the care they need.
Your baby’s healthcare team will look at a range of issues before discharging your baby. Often, babies are ready when they:
- reach their original due date
- can maintain a normal temperature in an open cot
- have gained enough weight
- can take all or most feedings by breast or bottle
- no longer need intravenous medications.
The healthcare team will explain how to access services in your community that will help you to look after your baby when you return home. Your hospital may also have a home visiting service if you live within a certain distance.
Some babies will go home needing extra care and will require additional support. If you have to use any special equipment, you will get training and detailed instructions. If the unit has the facilities, they will also give you the chance to sleep in the hospital with your baby for a short period to get used to caring for them without the healthcare team.
Community support groups can help you to connect with other parents and families who have had similar experiences.
Where to get help
- Your baby’s doctor (neonatologist)
- Neonatal intensive care and special care nurses
- Counsellor
- Social worker
- ParentLine, call 13 22 89
- Maternal and Child Health Line (24 hours) Tel. 13 22 29
Neonatal Resuscitation and Intensive Care Unit
Home / Maternity Hospital / Our departments/
Neonatal Intensive Care Unit is a structural subdivision of maternity hospital No. 10, consists of an intensive care unit and an intensive care unit and is designed for 20 beds.
The main mission and goal of the intensive care unit specialists is to save the life of the baby with the least negative consequences for his health. Children with various perinatal pathologies are admitted to the resuscitation and intensive care unit. Usually they require mechanical ventilation, parenteral nutrition, infusion therapy, correction and restoration of important body functions. Very premature babies with low body weight, who often have severe health disorders, are also transferred here. Parents are regularly provided with full information about the state of health of the newborn, about the characteristics of the disease and the tactics of its treatment.
Very premature babies with low body weight, who often have severe health disorders, are also transferred here. Parents are regularly provided with full information about the state of health of the newborn, about the characteristics of the disease and the tactics of its treatment.
If your baby has been transferred to the intensive care unit, do not panic and despair. The department staff will teach you how to care for your baby, introduce you to new medical technologies, medical language, rules and procedures that are designed to help your child. Our specialists make every effort to ensure that parents get used to it as soon as possible and begin to understand the needs of their baby. This is very important, because the correct care of the child in these difficult first days depends on how quickly he will be able to adapt to new living conditions outside the mother's body. Only after the baby's health improves and does not cause concern, when he is ready for a full life under normal conditions, can we talk about discharge from the department.
Resuscitation unit
This includes babies who need extra attention and resuscitation.
Children who have serious neurological problems, who cannot breathe on their own or who were born with very low birth weight are treated here. The resuscitation unit has everything for intensive treatment of the child and constant monitoring of his condition: incubators, monitor monitoring and, of course, qualified personnel.
Intensive care unit.
Rehabilitation treatment takes place here. Children are transferred here from the intensive care unit when adequate spontaneous breathing is restored, there is no need for continuous monitoring of vital functions, premature babies or babies with newborn jaundice.
The resuscitation and intensive care unit is equipped with modern medical equipment, which allows creating comfortable conditions for babies: modern incubators protect from noise and bright light, conditions are created for severely premature babies that are as close as possible to intrauterine conditions. For children who cannot feed on their own, nutrient solutions are introduced through a special probe. Also, if necessary, drugs are used to regulate the heart rate, stimulate breathing, blood pressure, ultrasound. In the premises of the department, the level of humidity and air temperature is constantly monitored.
For children who cannot feed on their own, nutrient solutions are introduced through a special probe. Also, if necessary, drugs are used to regulate the heart rate, stimulate breathing, blood pressure, ultrasound. In the premises of the department, the level of humidity and air temperature is constantly monitored.
Resuscitation and intensive care unit equipment:
- Incubators to maintain optimal temperature and humidity for the child;
- Open resuscitation systems for infusion, oxygen therapy with a heating system;
- Non-invasive ventilation apparatus for spontaneously breathing patients;
- ventilators for artificial lung ventilation;
- Monitors for round-the-clock monitoring of vital body functions (pulse rate, respiration, blood oxygen saturation, hemoglobin, pressure).
- Infusomats - devices for the dosed administration of medicines intravenously;
- Airway sanitation apparatus;
- Phototherapy lamps.

All devices used are certified and connected to a stand-alone station, which guarantees their trouble-free operation.
The medical staff of the intensive care unit is one of the most highly qualified. The team includes a medical unit, middle and junior medical personnel. The department is headed by the head, who is the chief of the doctors, and the senior nurse manages the sisters and junior staff.
The junior staff consists of assistant nurses and nurses who keep the department clean. Their work is very responsible, since the sanitary and hygienic requirements for treatment units are close to those established in operating rooms.
Nurses spend the most time with babies. They are around the clock with little patients, care for them, perform medical appointments, monitor the slightest changes in the condition of children, monitor readings, report on the dynamics of the condition of patients during medical rounds. Each sister is responsible for a certain number of newborns, and if the baby's condition is very serious, then there is only one patient per sister (and at the same time she is constantly busy, since the instability of the condition dictates a constant change in treatment).
Since the department's nurses work in shifts, the parents of severely premature babies have time to get to know many of them. Without a doubt, the nurse is the central figure in the nursing of premature babies, his "mother" for the period of his stay in the department. Good sisters "feel" babies and have not only a kind heart, skillful hands, intuition, but are also extremely observant. They will always point out to the doctor about problems in the condition of the newborn, everyone feels good and calm with them - both patients and doctors.
There are also nurses who provide fluid therapy and therapeutic nutrition for newborns. They monitor the condition of intravascular catheters and infusion systems, the condition of medical equipment, and are responsible for the sterilization of instruments.
The main doctors of the department are anesthesiologists-resuscitators and neonatologists, there are fewer of them than nurses. Their task is to make a diagnosis, develop an intensive care program, monitor and adjust treatment.
Every day the doctor conducts a general examination, listens to the child's heartbeat and breathing patterns. The condition of patients is monitored by equipment and nurses, as well as during medical rounds, which are carried out day and night every 3 hours.
At each round, the doctor evaluates the child's condition: breathing stability, heart function, nutritional adequacy. The doctor of the department determines what tests are needed and with what frequency, what treatment is required. The doctor assesses the need and amount of medical support for cardiac activity, the advisability of prescribing antibiotics to protect against infections, develops a therapeutic nutrition program, and finally decides when the child can be disconnected from the ventilator and when he can be transferred from the intensive care unit to the intensive care unit.
In addition, on-call doctors assist premature babies in the delivery room, transfer them to the department, carry out primary stabilization and treatment until the end of their shift, as well as monitor and treat patients in the evening, at night and on weekends. The duties of the doctors on duty also include registering the child in the intensive care and advisory bureau in order to transport the patient, if necessary, to other hospitals ( According to order No. examinations, children are transferred to specialized departments for newborns of city hospitals in a regulated time frame).
The duties of the doctors on duty also include registering the child in the intensive care and advisory bureau in order to transport the patient, if necessary, to other hospitals ( According to order No. examinations, children are transferred to specialized departments for newborns of city hospitals in a regulated time frame).
All doctors of the department have undergone the necessary training and improvement to provide resuscitation care to newborn children at the bases of the leading medical centers in Moscow and St. Petersburg.
Interaction of parents with department staff
According to the Health Law, the legal representatives of a newborn child are his parents (Article 18), to whom the attending physician provides information about the patient's condition (Article 17). The most complete information is provided in a personal conversation at a specially allotted time (over the phone it is impossible to make sure that the patient's mother or father is really on the other end). The attending doctor has the most complete picture of the diagnosis, changes in the condition, data of laboratory and instrumental studies of his patients, so it makes sense to ask him all the detailed questions. You can also inquire about the condition of the baby by phone.
The attending doctor has the most complete picture of the diagnosis, changes in the condition, data of laboratory and instrumental studies of his patients, so it makes sense to ask him all the detailed questions. You can also inquire about the condition of the baby by phone.
It is important for us that parents receive the most complete and accurate information, do not hesitate to ask even those questions that seem stupid, uncomfortable or inappropriate. We recommend that you write down questions as they arise, so that you can ask them later without forgetting anything.
What to ask your doctor:
- What is my child's condition?
- What is the severity of the condition?
- How is the baby treated (what does the intensive care program consist of)?
- What examinations are planned?
- What is the probability of normal development and possible complications?
- How do I get information about a change in condition and when can I visit my baby?
- Is it possible to perform the sacrament (rite) of baptism?
- How can I help my child get well?
Often, intensive care physicians have to tell relatives things that no one would like to hear, but objectively informing parents about the health of their children is part of our daily work. During meetings with doctors, parents have the opportunity to see and communicate with their children.
During meetings with doctors, parents have the opportunity to see and communicate with their children.
Maternity hospital No. 10 participates in the state program to support breastfeeding, and our specialists do their best to help maintain it. Regardless of the severity of the child's condition, we welcome the communication of parents with the newborn, we consider it necessary for the baby and contribute to his speedy recovery. Visits are limited only during SARS and influenza epidemics in order to protect seriously ill newborns from infection, which can worsen their condition.
6 intensive care unit
PHONES
Appointment for a consultation: +7(812) 670-01-11
Vaccination department: +7(812) 234-57-59
Reception department: +7(812) 234-16-70
More contacts...
Address
197022, St. Petersburg, st. Professor Popov, d.9. Show on map- Home
- Structure
- 6th branch
Phones: 812 2343310
The Department of Resuscitation and Intensive Care of the Federal State Budgetary Institution NIIDI FMBA of Russia At the origins of the creation of the ICU was MD. Professor E.K. Tsybulkin. The overhaul of the department with re-equipment with resuscitation modules and optimization of energy and gas supply was carried out in 2010. Department for 12 beds, has 7 Meltzer boxes, designed for 1-2 patients
Professor E.K. Tsybulkin. The overhaul of the department with re-equipment with resuscitation modules and optimization of energy and gas supply was carried out in 2010. Department for 12 beds, has 7 Meltzer boxes, designed for 1-2 patients
MAIN DIRECTIONS OF WORK OF THE DEPARTMENT:
- Provision of emergency care in emergency conditions at the Clinic for Infectious Diseases
- Intensive care, intensive observation and intensive care for all categories of patients in need with infectious diseases of the central nervous system, respiratory system, gastrointestinal tract
- Provision of anesthesia for diagnostic and surgical interventions
- Provision of resuscitation protection and all types of resuscitation measures to all categories of patients in need
EQUIPMENT
The equipment of the intensive care unit complies with the Federal Procedures for the provision of care. The department is equipped with the most modern equipment: Dräger FABIUS anesthesia and respiratory devices, a monitoring system (Philips) with a central station that allows you to measure blood pressure, heart rate, respiratory rate, the degree of blood oxygen saturation (StO2) in round-the-clock monitoring, a monitor depth of anesthesia "BIS", cerebral oximeter "INVOS", expert class ventilators Puritan-Bennett-840, "Draeger EVITA" 4 and Dräger XL, transport ventilator Dräger Oxylog 2000, defibrillators (Nichon Conden), infusion stations, infusion pumps and BBraun perfusors, medical electric and vacuum aspirators, radiant heat sources and a patient heating system, Dräger open resuscitation systems for patients in the first year of life.
All resuscitation places of patients are equipped with resuscitation modules with centralized supply of medical oxygen and compressed air, bedside monitors with a touch color display (Philips), which allow monitoring the main vital body functions around the clock: ECG, respiratory rate, heart rate, blood oxygen saturation. temperature. Express diagnostics is provided by a round-the-clock laboratory service, which makes it possible to conduct an emergency examination in a short time, including an analysis of the acid-base state and blood gases. The department is provided with all the necessary most modern and effective medicines, infusions and blood substitutes, anesthesia and consumables; during intensive care, syringes, needles, systems for intravenous infusion, enteral nutrition, catheters, sets for catheterization of the main veins, endotracheal tubes and other disposable consumables from leading world manufacturers are used.
DIAGNOSTIC EXAMINATIONS UNDER ANESTHESIA
Doctors of the department, if indicated, provide general anesthesia for diagnostic examinations, such as endoscopy (fibrogastroduodenoscopy, colonoscopy). It is possible to carry out inhalation (mask) anesthesia or intravenous anesthesia. After anesthesia and examination, children are under the supervision of qualified staff of the intensive care unit and IT.
It is possible to carry out inhalation (mask) anesthesia or intravenous anesthesia. After anesthesia and examination, children are under the supervision of qualified staff of the intensive care unit and IT.
INTENSIVE CARE
The Intensive Care Unit (ICU) provides emergency care for all emergency conditions at the Clinic for Infectious Diseases and provides intensive care, intensive monitoring and intensive care for all categories of patients in need with infectious diseases of the central and peripheral nervous system (meningitis , encephalitis, demyelinating diseases), infectious diseases of the respiratory system (acute respiratory diseases, bronchitis, pneumonia, broncho-obstructive syndrome), infectious diseases of the gastrointestinal tract (viral and bacterial diarrhea), combined infectious pathology.
EMPLOYEES
The Intensive Care Unit (ICU) of the Institute's Clinic employs a team of highly qualified doctors and nurses. These are employees who have devoted more than one year to their specialty and retained their devotion to the chosen business - medicine of critical conditions, treatment and nursing of seriously ill patients.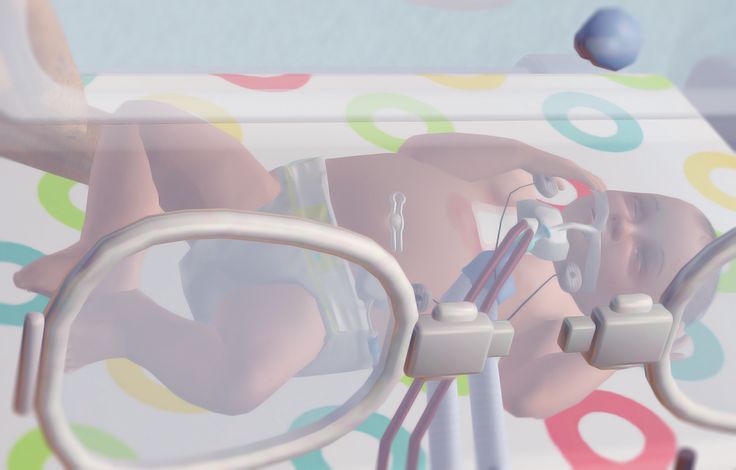 The department's doctors maintain close scientific and practical ties with leading methodological and clinical bases both in St. Petersburg and Moscow, as well as in the regions of the Russian Federation and beyond.
The department's doctors maintain close scientific and practical ties with leading methodological and clinical bases both in St. Petersburg and Moscow, as well as in the regions of the Russian Federation and beyond.
Konev Alexander Ivanovich
- Position:
- Head of the intensive care unit
- Specialty:
- Anesthesiologist-resuscitator
- Category:
- highest qualification category
- Work experience:
- 25 years
- Academic title:
- Assistant of the Department of Anesthesiology, Resuscitation and Emergency Pediatrics of AF and FVE of St. Petersburg State Pediatric Medical University (SPbSPMU)
- Awards:
- Honored Worker of the Komi Republic, winner of the All-Russian competition for the title "The Best Doctor of Russia in 2005" in the nomination "the best anesthesiologist-resuscitator"
- Certificates:
- "Transfusiology", "Health Organization";
- Area of professional interests:
- Organization of resuscitation care, sepsis and septic shock, cerebral and multiple organ failure in neuroinfections, infusion and nutritional support in the clinic of infectious diseases
Vysochenko Lyubov Sergeevna
- Certificates:
- "Anesthesiology and Resuscitation", "Organization of Nursing", "Nursing", "Nursing in Pediatrics"
Ioffe Mikhail Yakovlevich
- Specialty:
- Anesthesiologist-resuscitator
- Category:
- highest qualification category
- Work experience:
- 23 years
- Academic title:
- Associate Professor of the Department of Anesthesiology, Intensive Care and Emergency Pediatrics, St.
 Petersburg State Pediatric Medical University (SPbSPMU)
Petersburg State Pediatric Medical University (SPbSPMU) - Degree:
- PhD
- Area of professional interest:
- Sepsis and septic shock, multiple organ failure, cerebral edema, intracranial hypertension syndrome and cerebral insufficiency in neuroinfections, infusion support in the clinic of infectious diseases
Kurochkina Anna Vladimirovna
- Specialty:
- Anesthesiologist-resuscitator
- Category:
- second qualification category
- Work experience:
- 14 years
- Area of professional interest:
- Intensive care at the clinic for infectious diseases
Rydnik Tatyana Aleksandrovna
- Specialty:
- Anesthesiologist-resuscitator
- Work experience:
- 18 years
- Area of professional interest:
- Intensive care at the clinic for infectious diseases
Gordeev Vladimir Ilyich
- Position:
- Department consultant
- Specialty:
- Anesthesiologist-resuscitator
- Category:
- highest qualification category
- Academic title:
- Professor, Head of the Department of Anesthesiology, Intensive Care and Emergency Pediatrics, St.