Wetting during pregnancy
Tips to prevent involuntary urine leakage (incontinence) during and after pregnancy | Women's Health | Your Pregnancy Matters
Instructions on how to locate pelvic muscles and exercises to strengthen them can help prevent incontinence during and after pregnancy.Friends and family describe stress urinary incontinence (SUI) to pregnant women as if it’s just a fact of life: "After you have a baby, you won't be able to cough, sneeze, or exercise without peeing a little."
SUI is the most common type of urinary incontinence associated with pregnancy. More than a third of pregnant women experience involuntary urine leakage during the second and third trimesters, and a third leak during the first three months after delivery.
But you don’t have to just live with urinary incontinence. There are steps you can take to prevent and reduce leakage before, during, and after pregnancy. Interventions can include lifestyle modifications and strengthening your pelvic floor muscles through Kegel exercises.
Unfortunately, not all health care providers make such recommendations. Or they might suggest performing Kegels, but they don't show patients how to do them correctly. There's a lot going on in the pelvic region during pregnancy, and many women don't know how to locate or engage their pelvic floor muscles.
UT Southwestern has one of the largest Female Pelvic Medicine and Reconstructive Surgery divisions in the country. We help patients at all stages of life with strategies and therapies to prevent or treat urinary incontinence.
The first step in prevention is education.
Why does urinary incontinence occur with pregnancy?
Pregnancy and childbirth can cause incontinence in several ways:
- Your growing baby takes up a lot of room. As the uterus expands, it puts increased pressure on the bladder, urethra, and pelvic floor muscles. This can lead to leakage.
- Changing progesterone levels during pregnancy can weaken the pelvic floor.
 Increases in this hormone loosen up your ligaments and joints so the belly can expand and so you can deliver. But it can also loosen ligaments in the pelvis that help you hold in urine.
Increases in this hormone loosen up your ligaments and joints so the belly can expand and so you can deliver. But it can also loosen ligaments in the pelvis that help you hold in urine. - Childbirth, particularly vaginal delivery, can stretch and weaken the pelvic floor muscles. This can lead to pelvic organ prolapse, in which your bladder, uterus, or rectum droops into the vaginal canal. Prolapse can be associated with urinary incontinence.
- Vaginal delivery also can result in pelvic muscle and nerve injury, which can result in bladder control problems.
If you experience urinary incontinence during pregnancy, you are at higher risk of having a persistent problem after birth. Tell your health care provider about urinary incontinence symptoms as soon as you notice them during pregnancy or at your first postnatal visit.
More than 80% of postpartum women who experience SUI symptoms during pregnancy may continue to experience stress incontinence without treatment.
Related reading: Body after birth: Treating post-pregnancy problems
Where are the pelvic floor muscles?
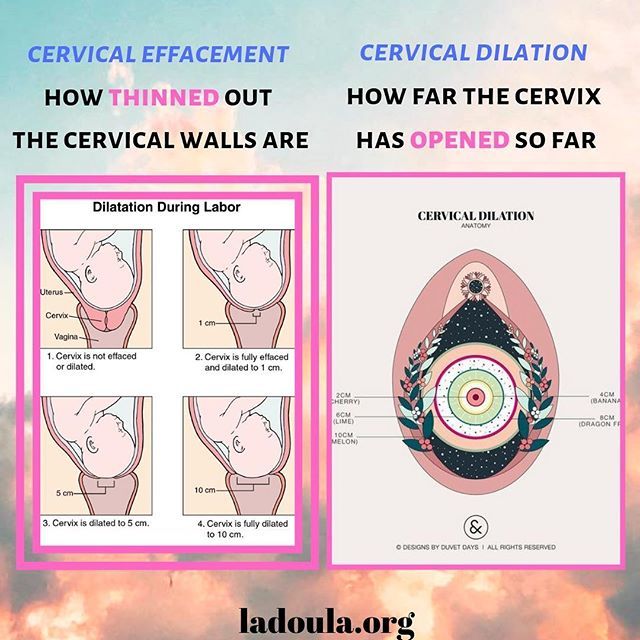
During initial exam, I often use a clock visual to help women know where their pelvic floor muscles can be palpated. If you lie on your back, imagine the top of the opening of your vagina is 12 o’clock and the bottom of the opening is 6 o’clock.
The pelvic floor muscles are easiest to palpate at the 5 o’clock and 7 o’clock positions– about even with where your legs meet your hips and approximately 3 to 4 centimeters above the vaginal opening.
These are the same muscles you contract when you try to stop the flow of urine midstream or if you were to tighten your vagina around a tampon. And these are the muscles you contract to do Kegel exercises. These pelvic floor muscle exercises were named after Dr. Arnold Kegel, who described them in the 1940s to help patients strengthen their pelvic floor muscles to treat urinary incontinence.
The proper way to Kegel
Verbal or written instructions alone don't necessarily help patients know whether they're doing Kegel exercises properly.
When we see patients for urinary incontinence, we provide education and instruction. We often recommend one to six sessions of supervised Kegel exercises with a female pelvic medicine and reconstructive surgery doctor, a pelvic floor physical therapist, or another provider who has expertise in pelvic floor disorders. While physical therapy or other medical visits usually are not covered by insurance for preventive purposes, they usually are once a problem develops.
In these appointments, your provider will describe how to locate and engage the pelvic floor muscles. The provider will gently press on the pelvic floor muscles with a gloved exam finger inside your vagina and ask you to squeeze the muscles. The muscles will be identified as described. Make sure you’re not squeezing your stomach, legs, or gluteal muscles at the same time, and don’t hold your breath.
Some patients benefit from holding a mirror between the legs to visualize the external anatomy during the exercise. When done properly, you should see the area between your vagina and anus lift toward your upper body.
When done properly, you should see the area between your vagina and anus lift toward your upper body.
Doing Kegel exercises regularly is key to strengthening the pelvic floor. We recommend women do 10 repetitions, holding each squeeze for 5 to 10 seconds, three times each day.
You can do the exercises while lying down, sitting, or standing. Many patients find it easier to remember to do Kegels if the exercises become part of a daily routine. Maybe do a set while lying in bed right after you wake up, another as you eat lunch, and another at bedtime.
Most women see less frequent urine leakage within a few weeks or months after maintaining a Kegel exercise routine.
Before your big day arrives, get a preview of the accommodations for new moms at UT Southwestern's Clements University Hospital. From the chef-prepared meals to the roomy, high-tech labor and delivery suites, we want to make sure that you, your baby, and your family have the opportunity to bond in a safe and soothing environment.
Lifestyle changes to reduce urinary incontinence
Along with Kegel exercises, there are a few other noninvasive methods to eliminate or reduce the risk of urinary incontinence:
- Lose weight. Excess body weight puts pressure on the bladder. Even a 10% reduction in weight can significantly help with urinary incontinence. Work with your doctor to manage your weight gain during pregnancy, and after the birth of your little one, returning to your pre-pregnancy weight will help relieve the pressure on your bladder and pelvic floor.
- Quit smoking. Smoking has been shown to increase the risk of urinary incontinence as it leads to bladder irritation and chronic coughing.
- Make dietary changes. Some foods and beverages can make incontinence worse. These include caffeine, alcohol, and spicy and acidic foods. This is especially important if you experience urinary frequency and urgency and have trouble making it to the bathroom once you have the urge to urinate.
 Constipation can worsen symptoms of urine leakage. Stool in the rectum can put pressure on the bladder, urethra, and pelvic floor, so include plenty of higher-fiber foods and fluids in your daily diet.
Constipation can worsen symptoms of urine leakage. Stool in the rectum can put pressure on the bladder, urethra, and pelvic floor, so include plenty of higher-fiber foods and fluids in your daily diet.
Other treatments for urinary incontinence
Your doctor may recommend alternative treatment options, such as:
- Electrical stimulation: This therapy can help rehabilitate weak pelvic floor muscles and can be done in conjunction with Kegel exercises.
- Medications: Certain drugs can be used to treat urgency urinary incontinence (UUI) that does not respond to diet and behavioral modification, such as timed voiding to avoid overfilling of the bladder. UUI is associated with a sudden, intense urge to urinate followed by involuntary loss of urine. It is often associated with urinary frequency and urgency. Medications to treat UUI allow the bladder to fill up with more urine before giving the body a signal that it needs to use the bathroom.
- Pessary: This is a plastic insert that supports the vaginal walls.
 It can be removed, replaced, and cleaned at home.
It can be removed, replaced, and cleaned at home. - Surgical procedures: There are several surgical procedures that can be performed for the treatment of stress urinary incontinence that does not respond to the conservative measures described above. One of the most common and effective surgeries involves placing a synthetic mesh sling between the vagina and the middle portion of the urethra. This supports the urethra like a hammock and helps control urine leakage during activities such as coughing, sneezing, laughing, exercise. Other effective surgeries for SUI that do not involve mesh include the Burch colposuspension and the traditional pubovaginal sling with graft material procured from the patient’s own body. Urethral bulking injection is an office procedure that may provide relieve of symptoms in patients who have contraindications for surgery.
If you are experiencing urinary incontinence during or after pregnancy, know that you’re not alone. Talk with your doctor – we can help you get back to exercising, laughing, and sneezing without worrying about a accidental urine leakage.
To visit with an incontinence expert, call 214-645-8300 or request an appointment online.
Frequent Urination During Pregnancy | Pampers
You may be wondering whether peeing a lot is a sign of pregnancy or whether this urge to pee so often will ever go away. Frequent urination is a common early pregnancy symptom, but it can also reappear later on during pregnancy as your uterus and baby grow, putting pressure on your bladder. Although it can definitely be annoying, in most cases, it's nothing to worry about. Read on to find out what causes frequent urination during pregnancy, get some tips to help you manage it, and learn the signs that indicate it may be linked to another condition, like a urinary tract infection.
What Causes Frequent Urination During Pregnancy?
What makes you need to pee more is often the increased amount of blood in your body. To process this blood flow, your kidneys need to produce extra fluids, which then end up in your bladder. Although peeing often during pregnancy is annoying, it's also a normal and common pregnancy symptom. Here are some frequently asked questions about this symptom:
Although peeing often during pregnancy is annoying, it's also a normal and common pregnancy symptom. Here are some frequently asked questions about this symptom:
What is considered frequent urination in pregnancy? There's no set number of visits to the bathroom – it's simply needing to go more often than you usually would.
When does frequent urination start during pregnancy? How soon it may start differs for each woman, but you may find yourself needing to pee more often from around six to eight weeks of pregnancy.
Will I need to pee this often the whole pregnancy? It may ease up for a while after you enter the second trimester, but you may find the increased urge to pee returns later on, as your growing baby places more pressure on your bladder. Toward the end of the third trimester, when your baby “drops," the extra pressure on your pelvis and bladder might have you rushing to pee even more frequently.
How often should you pee? Whenever you have to! It's better not to hold it in.

Tips to Manage Peeing Often While Pregnant
You can't really avoid more frequent urination, and you really wouldn't want to, as it's a natural consequence of drinking lots of fluids to stay well hydrated and healthy during pregnancy. Here are some tips that might help make your life easier:
Lean forward when you pee so that you properly empty your bladder
To prevent increased urination at night, try not to drink too much water just before going to bed
Avoid beverages and foods containing caffeine, which can make you need to pee more often. (Read our article to find out more about what not to eat or drink while you're pregnant.)
Practice Kegel exercises to strengthen your pelvic floor muscles, as this can help prevent leaking when you cough, sneeze, or laugh, both before and after giving birth. (If you do find yourself peeing when you sneeze, consider wearing a panty liner.
 )
)If your urine is dark yellow or orange, this may be a sign of dehydration − try to increase your fluid intake until your urine is back to a normal pale yellow
If you're heading out the door, or you know you're going into a long meeting, consider one more dash to the toilet beforehand. You can also try to scout out where the nearest bathroom so you're not caught off guard.
Can Pregnancy Peeing Be a Sign of a Problem?
More frequent urination is usually a normal pregnancy symptom. However, sometimes it can be a sign of a medical condition that may require treatment by your healthcare provider. These conditions include:
Urinary tract infection (UTI). Many women wonder whether frequent urination is part of pregnancy or a UTI. If it's a UTI, you may notice a painful, burning sensation while peeing, have a fever, notice cloudy urine, or see blood in the toilet.
 You may also feel the strong urge to pee, but then only a few drops will come out. Pregnant women face an increased risk of UTI from week 6 to week 24, because the growing uterus can place pressure on the urinary tract, increasing the chance of bacterial infections. If you suspect you have a UTI, consult your healthcare provider, as this infection requires treatment – often antibiotics.
You may also feel the strong urge to pee, but then only a few drops will come out. Pregnant women face an increased risk of UTI from week 6 to week 24, because the growing uterus can place pressure on the urinary tract, increasing the chance of bacterial infections. If you suspect you have a UTI, consult your healthcare provider, as this infection requires treatment – often antibiotics.Gestational diabetes. Frequent urination can sometimes be a sign of gestational diabetes, generally a temporary form of diabetes that affects a small percentage of moms-to-be. Healthcare providers usually test for gestational diabetes between 24 and 28 weeks of pregnancy. If gestational diabetes is treated, then the baby's health isn't adversely impacted, and the diabetes will usually go away after you give birth. If you notice symptoms like frequent urination combined with persistent thirst, nausea, or fatigue, consult your healthcare provider.
Frequent urination during early pregnancy is common and usually nothing to worry about. Although it may feel as if you are peeing all the time, keep in mind that it may ease up for a time, before returning later on. Once your baby is born, your urge to pee more often should go away, and you'll only have your newborn's pee to worry about!
Although it may feel as if you are peeing all the time, keep in mind that it may ease up for a time, before returning later on. Once your baby is born, your urge to pee more often should go away, and you'll only have your newborn's pee to worry about!
Home - Seni
Home - Seni- Seni Club
- Where to buy
- Request a free sample
- Contacts
- Change country
- menu
Urological pads for women with mild to moderate urinary incontinence
More details
Urological pads for women with mild to moderate urinary incontinence
Urological inserts for men with mild to moderate urinary incontinence
More details
Urological inserts for men with mild to moderate urinary incontinence
A wide range of absorbent products for people in need of reliable protection.
More
A wide range of absorbent products for people in need of reliable protection.
Absorbent briefs
Absorbent briefs for active people who need comfortable protection.
More
Absorbent briefs for active people who need comfortable protection.
skin care
Daily skin care products
More details
Cosmetics for daily skin care
A well-chosen product not only ensures the comfort of the person who uses it, but also avoids unnecessary costs.
Find product
It is important to choose the correct size of the product. An incorrectly selected size can lead not only to leakage, but even harm to health. Use the special "form" to select the correct size.
Find size
Seni care products have been helping to properly care for skin that needs especially delicate care for many years. Depending on the purpose, conditions of use and individual characteristics of the skin, seni care cosmetics are conventionally divided into 2 areas: for specialized care and for the care of dry and sensitive skin. Informative packaging design, convenient color identification with special symbols make it easy to choose the right cosmetic product.
Read more
Menopause
Menopause (menopause, menopause) is a natural stage in the life of every woman, at which menstruation stops as a result of a weakening of the hormonal function of the ovaries.
Read more
Prevention of bedsores
Pressure sores never occur in healthy people who control their muscles and are able to respond to the discomfort caused by pressure.
Read more
MoreThe SeniControl mobile app is a handy tool with which you can easily monitor your urinary incontinence. The application will assess the degree of urinary incontinence and recommend the best urological product that will suit your needs.
Read more
Application available at:
What causes urinary incontinence in pregnant women
One of the signs of pregnancy is frequent urination. In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women. The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor.
The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor.
Types of urinary incontinence during pregnancy
Most often, 3 types of urinary incontinence in a pregnant woman appear, and in each case there are characteristic signs.
- Stress. It manifests itself with the tension of the abdominal muscles and fluctuations of the diaphragm. That is, it is enough to sneeze, cough or laugh so that a couple of drops of urine appear on the linen. The condition is typical for the first trimester.

- Urgent. Symptoms are sudden urge to urinate. They arise so unexpectedly that the expectant mother simply does not have enough time to run to the bathroom. One of the causes of the condition lies in the irritation of the urinary canal. You can also blame the failure of the nervous system and overstretching of the muscles in the pelvis. The condition is typical for the last trimester, but also occurs after childbirth.
- Full bladder syndrome. The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.
Regardless of the cause of urinary incontinence in a pregnant woman, the condition causes discomfort and stress. This is not a reason to panic, in fact, the situation is not so critical - most often, not the entire volume of urine from the bladder is released, but only a small amount. To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary.
To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary.
Main causes of urinary incontinence in pregnancy
Given that it is not difficult to find an explanation for urinary incontinence in a pregnant woman, it should not cause much concern. It is only necessary to identify the causes and make sure that this is due to physiology, and not diseases of the genitourinary system. The doctor who leads the pregnancy will help dispel fears.
The main cause is weakened muscles in the pelvic area. Excessive stretching of muscle tissue leads to loss of tone. As a result, the sphincter that holds urine, the walls of the bladder, and other muscles are weakened. This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often.
Another cause of urinary incontinence in a woman during pregnancy is the impact of a baby's foot on the bladder. This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
The number of previous pregnancies and births is also thought to increase the risk of urinary incontinence. Especially if the pregnancies go one after another, and the woman's muscles simply do not have time to recover.
Other factors associated with urinary incontinence during pregnancy are overweight and a sedentary lifestyle. A protracted birth process provokes a problem already in the postpartum period.
Healthy urinary retention occurs when the following conditions are met:
- when the bladder is in a normal position;
- immobility of the urethra;
- good work of the muscles surrounding the bladder and pelvic floor muscles;
- with the functional and anatomical integrity of the urethra and bladder closure apparatus.
What to do to deal with the problem
As mentioned above, urinary incontinence in women during pregnancy is most often associated with physiological changes, so no treatment is required. However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.
However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.
If the tests do not show deviations, it remains only to calm down and practice hygiene more often. The doctor will give recommendations on hygiene products - their choice and the frequency of changing underwear. But even without a specialist, we can say that the replacement of pads and panties is carried out as needed. Lingerie should fit the size, and it is better to choose a special cut for expectant mothers so that it does not press anywhere. Decorative details on underwear are not welcome, you should give preference to simple panties made of natural fabric.
If there is a problem, you will often have to wash yourself, go to the toilet on time. Doctors advise you to lean forward slightly when urinating. This will allow the urethra to open completely. At the end, you need to push slightly (without fanaticism) to completely empty the bubble.
At the end, you need to push slightly (without fanaticism) to completely empty the bubble.
Reducing the pressure on the diaphragm can help reduce the risk of urine leakage when sneezing and coughing. To do this, you need to open your mouth, normalizing the pressure.
Examination and treatment
Before dealing with incontinence, it is imperative to establish its cause by contacting a doctor. The doctor, in turn, will prescribe the necessary examination. It usually consists of several stages:
- Urodynamic examination. With the help of it, the work of the upper and lower urinary tract is evaluated.
- Clinical examination. It includes a routine urine test and urine culture for flora, as well as a study in a gynecological chair - during an external examination, the doctor can assess the mobility of the bladder neck during a cough test or straining, assess the condition of the vaginal mucosa and skin, and also identify a possible genital prolapse.

- Ultrasound examination. It is carried out to study the functioning of the renal system, the urethrovesical segment, the condition of the urethra in a pregnant woman with stress urinary incontinence, as well as to confirm the presence or absence of pathologies of the genitals.
In addition to tests and examinations, you will most likely be asked to keep a special diary in which for several days you will record several parameters of urination, such as the amount of urine released per urination, the number of urination per day, all cases of urinary incontinence, the number of used during the day pads and physical activity.
Only after the examination, conclusions are drawn about the methods of treatment, which are often necessary only in extreme cases. If no pathology or inflammatory processes are detected, then most likely no special treatment will be carried out, since after childbirth, incontinence most often goes away on its own or occurs less and less.
If incontinence is due to weakening of the pelvic floor muscles, then the situation can be significantly improved with the help of special exercises. Currently, there are a large number of complexes for intimate gymnastics. One of the most popular was developed by the American gynecologist and MD Arnold Kegel. The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay).
It is important to know that if you have never strengthened intimate muscles before pregnancy, you need to do this with caution, in no case overdo it.
It is possible that the doctor will prescribe you some herbal preparation that supports the functioning of the bladder and has an antispasmodic, anti-inflammatory and antimicrobial effect.
Treatment with decoctions of herbs (rose hips, sage, dill, lingonberries) may also be recommended. They have not only preventive, but also curative properties.
Pelvic (intimate) muscle training
To reduce the risk of urinary incontinence in a pregnant woman at night and during the day, doctors recommend doing special exercises. These are Kegel exercises that are useful not only for expectant mothers, but for all women, without exception, regardless of age. The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article.
How to ensure your comfort and peace of mind
So that urinary incontinence in pregnant women in the early, and especially in the later stages (38-39 weeks), does not cause increased discomfort, manufacturers of hygiene products produce special pads. One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
- anatomically shaped to prevent leakage of urine;
- absorbent layer that instantly absorbs liquids and odors;
- secure fit on underwear;
- small thickness so that the pad is not visible under clothing;
- safe even for sensitive skin;
- the ability to choose a product based on the amount of discharge.
If you need help choosing the right hygiene products, the PAUL HARTMANN Sp. z o.o. hotline will advise you.
How else can you help yourself
Go to the toilet as often as possible during the day. At the same time, you should not reduce your fluid intake. The expectant mother should drink as much as she wants. But you need to try not to drink large amounts of liquid an hour before bedtime.
Many women use disposable pads to avoid trouble.