What is the swab test at 37 weeks pregnant
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
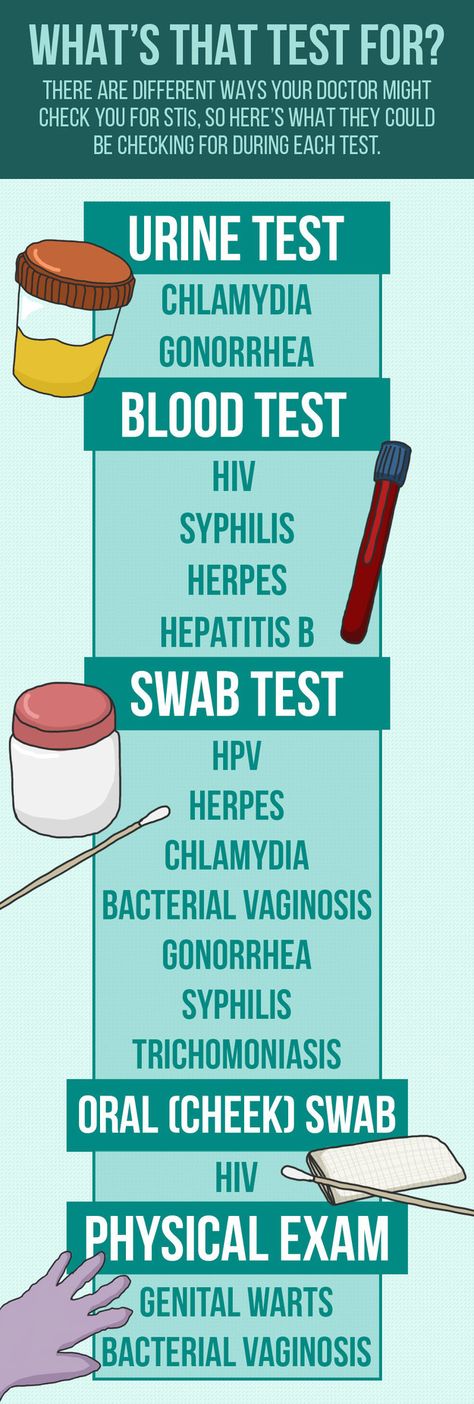
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
Doctors will test a pregnant woman to see if she has GBS. If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Group B strep test | Pregnancy Birth and Baby
Group B strep test | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you’re pregnant, one of the routine antenatal tests you’ll probably have is for group B streptococcus (also known as ‘group B strep’ or ‘GBS’). This page explains what the test is for, which babies are at risk of infection and how group B strep is treated.
This page explains what the test is for, which babies are at risk of infection and how group B strep is treated.
What is group B strep?
Group B strep is a type of bacteria commonly found in the intestines, rectum, urethra or vagina. Many women have it, and it usually causes no health concerns or symptoms. Some women infected with group B strep get a urinary tract infection, and it increases the risk of a miscarriage only very slightly.
The main concern is passing it on to the baby before or during a vaginal birth. While many babies who get infected stay healthy, a small proportion (about 1 in 200) become very sick within the first few days of life. They get serious infections such as pneumonia and blood poisoning, or meningitis, which is an infection around the brain.
These seriously ill babies are treated with intravenous antibiotics. Most recover with no side-effects, but some don't survive.
Group B strep test
The group B strep test is a routine antenatal test. It involves taking a swab of the inside of the vagina. Your doctor or midwife will do this, or you may be able to do it yourself. The swab is taken at 35 to 37 weeks' pregnancy. Tests done earlier in your pregnancy aren't a good guide to your condition at birth because the bacteria can come and go.
It involves taking a swab of the inside of the vagina. Your doctor or midwife will do this, or you may be able to do it yourself. The swab is taken at 35 to 37 weeks' pregnancy. Tests done earlier in your pregnancy aren't a good guide to your condition at birth because the bacteria can come and go.
Who has the group B strep test?
Some hospital and doctors recommend that every pregnant woman has a group B strep test.
But others ask only some women to have the test if they are at higher-than-average risk because they go into labour early, or their waters break early.
Even if you're planning a caesarean, you can think about having the test in case your waters break early or you go into labour unexpectedly early.
Talk about the risks and benefits of the group B strep test with your midwife or doctor.
Risk factors for infection with group B strep
Babies are more likely to be infected with group B strep if:
- they are born, or your waters break, before 37 weeks
- you give birth more than 18 hours after your waters break
- you have a fever (over 38°C) while in labour
- you've had a previous child with severe group B strep infection
- a urine test during pregnancy detected group B strep
- a swab taken no more than 5 weeks earlier detected group B strep
Preventing group B strep from infecting your baby
If your group B test at 35 to 37 weeks was positive, or if you have the risk factors listed above, your doctor or midwife will probably recommend that you have intravenous antibiotics when your waters break or labour starts.
Often this is penicillin, but alternatives are available if you are allergic to penicillin. The antibiotics pass through the placenta and into the baby. This greatly reduces your baby's chances of becoming ill.
There's no need for antibiotics before a planned caesarean because the baby will not pass through the vagina. You can't pass the bacteria to your baby through the placenta.
After the birth
If you had antibiotics during labour, your baby will be monitored for the first couple of days for signs of infection. The chance of your baby being infected is low.
Late-onset group B strep
There is a very small group of babies that develop group B strep infection weeks or months after birth (called ‘late onset group B strep'). They become seriously ill quite quickly, with fevers and vomiting and difficulty feeding. Unfortunately, the group B strep test and use of antibiotics doesn’t prevent a baby developing late-onset group B strep infection.
If your child's condition deteriorates quickly, call triple zero (000) and ask for an ambulance, or go to the nearest hospital emergency department.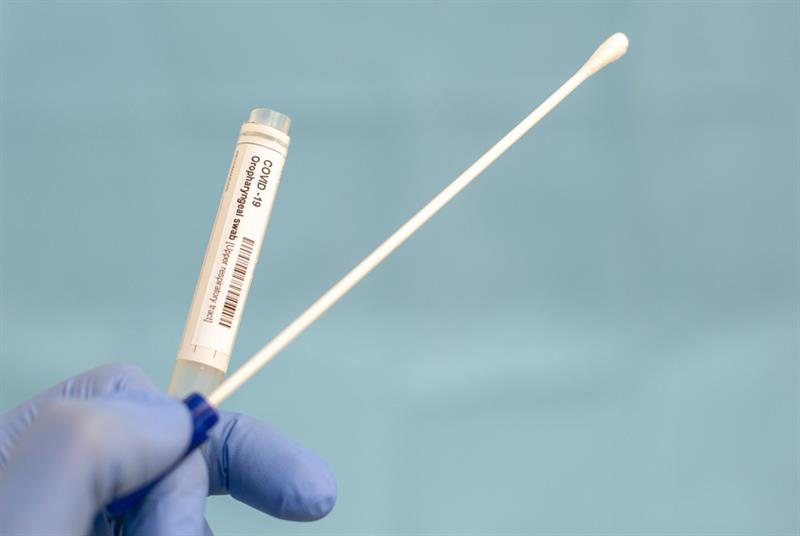
When to seek help
If you want more information about group B strep, or if you have any concerns about your baby, call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse, or talk to your midwife or doctor.
Sources:
RANZCOG (Group B Streptococcus), RANZCOG (Maternal Group B Streptococcus in pregnancy), Cochrane Database of Systematic Reviews (Vaginal chlorhexidine during labour to prevent early-onset neonatal group B streptococcal infection), Cochrane Database of Systematic Reviews (Intrapartum antibiotics for known maternal Group B streptococcal colonization), Department of Health (Pregnancy Care Guidelines, Group B streptococcus)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Pregnancy checkups, screenings and scans
Need more information?
Group B Streptococcus
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Pregnancy screening Group B Streptococcus (GBS) - Maternal, child and family health
The Pregnancy screening for Group B Streptococcus (GBS) consumer brochure provides information to all pregnant women on screening and recommended treatment for GBS.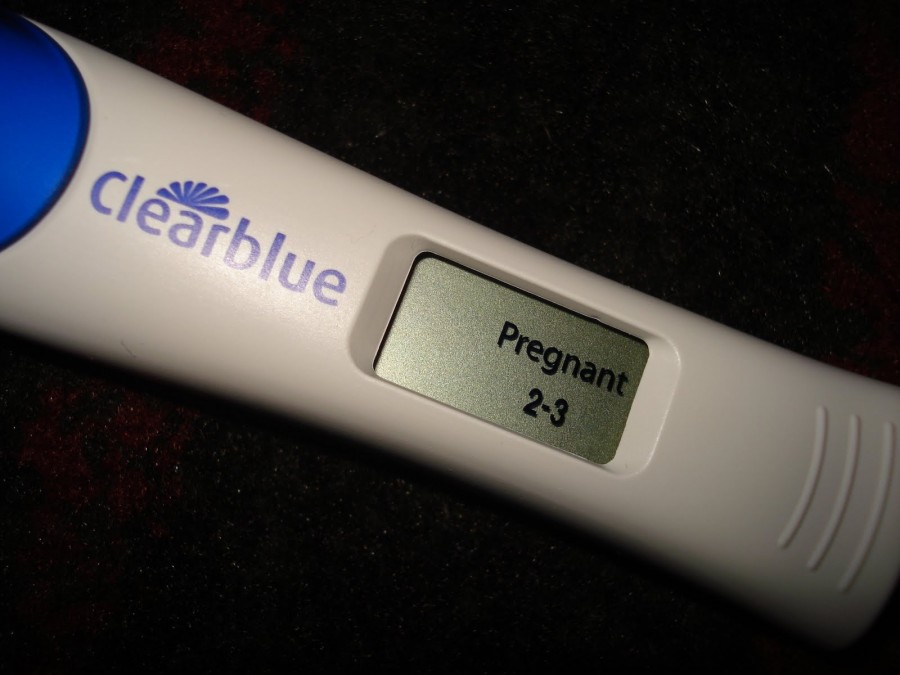
Read more on NSW Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Flora smear during pregnancy - when and why to take it
- When to take a flora smear
- What a flora smear shows
- Flora smear preparation rules
The flora smear is the most common test prescribed by an obstetrician-gynecologist. To conduct this study, the doctor, while examining a woman in a gynecological chair, takes the contents of the vagina from the posterior fornix (this is the space that is located between the back wall of the vagina and the cervix), the cervical canal and the discharged urethra, applies the material to the glass slide and directs him to the lab.
Smear examination for flora in the laboratory is carried out by a doctor of laboratory diagnostics under a microscope. This study allows you to determine the nature of the microflora (types of microorganisms) of the vagina, cervical canal and urethra, to identify the inflammatory process in the genitals of a woman, in some cases it also allows you to determine the causative agent of this inflammatory process (for example, gonococcus, Trichomonas).
When to take a smear for flora
It is mandatory for all pregnant women to take a swab twice - at registration and at 30 weeks of pregnancy, often another swab for flora is taken at 36-37 weeks to assess the state of the vaginal microflora before childbirth. During these periods, the analysis is given even in cases where the patient is not bothered by anything. This is carried out in order to identify a hidden inflammatory process that can lead to serious complications during pregnancy. During pregnancy, due to changes in hormonal levels and a decrease in immunity, exacerbation of chronic infections, as well as candidiasis (thrush), is much more likely.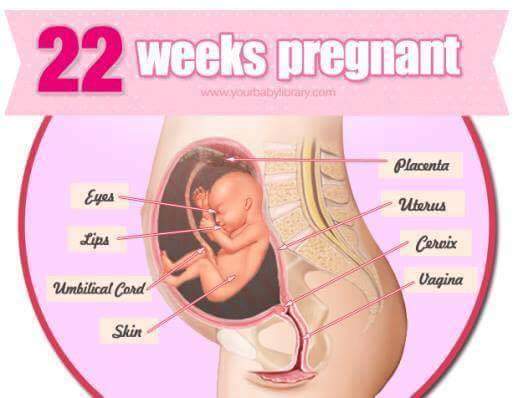 Any inflammatory process in the vagina during pregnancy can lead to serious complications of pregnancy - premature rupture of amniotic fluid, premature birth, oligohydramnios or polyhydramnios, intrauterine growth retardation and others.
Any inflammatory process in the vagina during pregnancy can lead to serious complications of pregnancy - premature rupture of amniotic fluid, premature birth, oligohydramnios or polyhydramnios, intrauterine growth retardation and others.
If a pregnant woman has complaints - the appearance of copious discharge from the genital tract, itching, burning or discomfort in the genital area, a swab for flora is also taken. In some pathological conditions, for example, in the presence of past miscarriages associated with infectious complications of pregnancy, cervical incompetence, a smear for flora is taken once a month, and after 30 weeks once every two weeks. Smear sampling is an absolutely safe procedure and does not lead to any complications, therefore it can be performed at any stage of pregnancy.
What a flora smear shows
A flora smear is evaluated according to the following indicators:
Epithelium
Squamous epithelium is the cells of the surface layer of the mucous membrane of the vagina and cervix. The presence of a large amount of squamous epithelium in a smear may indicate an inflammatory process. The absence of epithelium in the smear indicates a violation of the hormonal background.
The presence of a large amount of squamous epithelium in a smear may indicate an inflammatory process. The absence of epithelium in the smear indicates a violation of the hormonal background.
Leukocytes
These are blood cells involved in the destruction of pathogenic bacteria. Leukocytes are able to actively penetrate through the wall of blood vessels into the tissues of the body and participate in the fight against infectious agents. Normally, no more than 10 leukocytes are present in a smear for flora from the vagina, no more than 15 leukocytes per field of view from the cervical canal, and up to 2 leukocytes per field of view from the urethra. An increase in the content of leukocytes in a smear is a sign of inflammation, while the higher the content of leukocytes in a smear, the more pronounced the inflammatory process.
Red blood cells
These are red blood cells. Normally, single erythrocytes (1-2 in the field of view) can be found in a flora smear.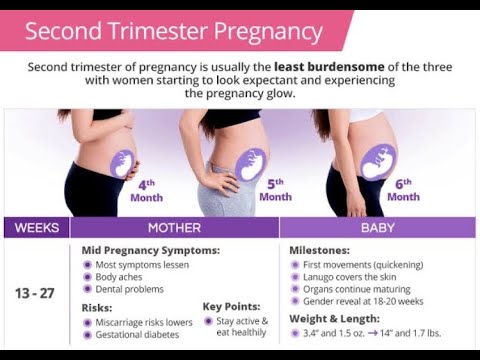 An increase in the number of red blood cells indicates the presence of a chronic inflammatory process, and also be a sign of injury or occult bleeding, for example, in the presence of cervical ectopia (the so-called erosion, when the vaginal part of the cervix is covered with a cylindrical epithelium normally lining the inside of the cervix).
An increase in the number of red blood cells indicates the presence of a chronic inflammatory process, and also be a sign of injury or occult bleeding, for example, in the presence of cervical ectopia (the so-called erosion, when the vaginal part of the cervix is covered with a cylindrical epithelium normally lining the inside of the cervix).
Slime
Normally, there is no mucus in the urethra, a moderate amount of mucus is detected in the vagina, and there may be a large amount of mucus in the cervix. An increase in the amount of mucus may be a sign of an inflammatory process, but this criterion does not have great diagnostic value, and doctors rarely rely on it when making a diagnosis.
Bacteria
Normally, flora should not be detected in the urethra, rod flora is detected in a moderate amount in the vagina and cervix. Rod flora is most often lactobacilli, which are 95% are normal vaginal biocenosis. Lactobacilli actively colonize the vagina and create an acidic environment in it, thereby preventing the growth and reproduction of pathogenic bacteria.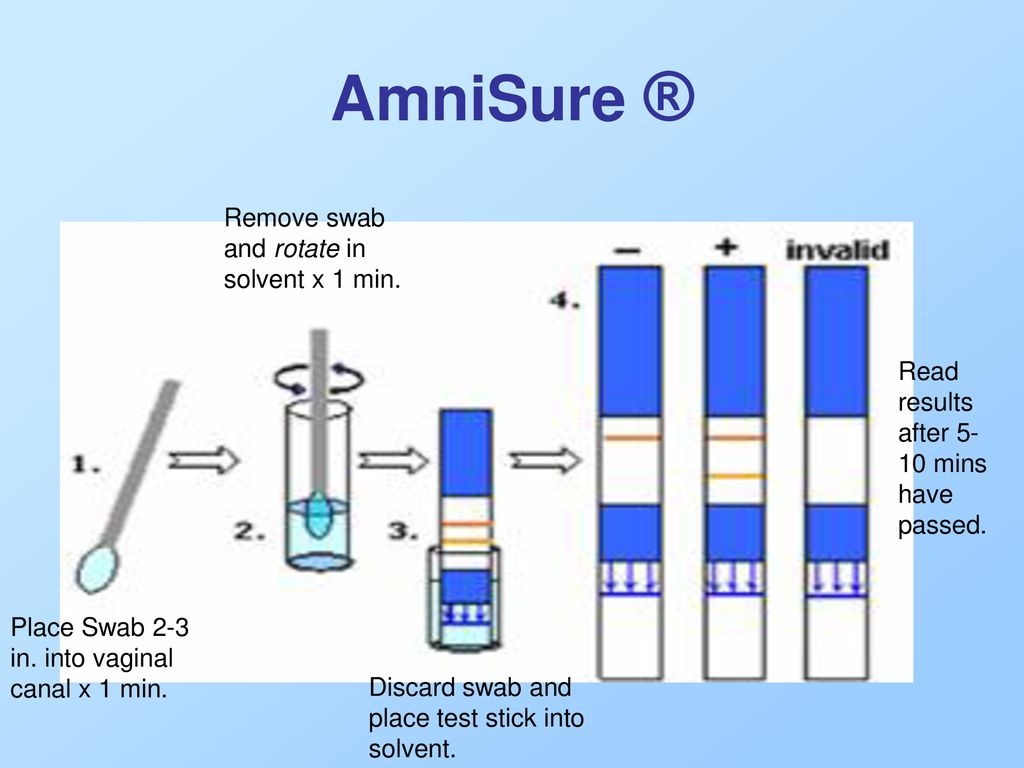
In addition to lactobacilli, other rod bacteria, such as E. coli, bacteroids, and various cocci, may also be present in the vagina. These are bacteria that, under microscopy, have the shape of balls. This group of bacteria includes streptococci, staphylococci, enterococci. In a small amount, they are normally present in the vagina. If their number increases sharply against the background of the death of normal lactobacilli, this can lead to the development of an inflammatory process. Unfortunately, according to the results of a routine smear on the flora, it is impossible to determine which specific bacteria and in what quantity are present in the vagina. Therefore, with a pronounced inflammatory process, as well as when a large amount of coccal flora is found in a smear on the flora, the doctor prescribes an additional analysis to make the correct diagnosis - sowing on the flora with the determination of sensitivity to antibiotics.
Opportunistic flora
These are micro-organisms that live in the human body in small numbers, without causing harm, but under certain conditions can lead to an inflammatory process. Such microorganisms found in a smear on the flora include fungi of the genus Candida and gardnerella.
Such microorganisms found in a smear on the flora include fungi of the genus Candida and gardnerella.
Gardnerella ("key cells")
Gardnerella and other bacteria living in anoxic conditions (so-called anaerobic bacteria) normally live in the vagina in small numbers, without causing symptoms of an inflammatory process. With a decrease in local immunity, which is quite common during pregnancy, there is an increase in the proportion of these bacteria in the vaginal microflora, a disease occurs - bacterial vaginosis (vaginal dysbiosis). At the same time, “key” cells are found in a smear on the flora - these are cells of the vaginal mucosa, covered with gardnerella and other anaerobic bacteria. The gardnerella themselves are not visible in a normal unstained smear. They can only be detected by staining smears with special dyes.
Mushrooms
Microorganisms of the genus Candida are part of the normal microflora of the mouth, vagina and colon of most healthy people. Normally, the number of these microorganisms is small and they do not cause an inflammatory process. Normally, in some women, a small amount of spores of the fungus may be detected in a vaginal smear. In the absence of an inflammatory reaction and complaints of the patient, the treatment of this condition is not carried out. The detection of a large number of spores or mycelium of a yeast-like fungus of the genus Candida in a smear on the flora makes it possible to diagnose candidiasis (or thrush)
Normally, the number of these microorganisms is small and they do not cause an inflammatory process. Normally, in some women, a small amount of spores of the fungus may be detected in a vaginal smear. In the absence of an inflammatory reaction and complaints of the patient, the treatment of this condition is not carried out. The detection of a large number of spores or mycelium of a yeast-like fungus of the genus Candida in a smear on the flora makes it possible to diagnose candidiasis (or thrush)
Pathogenic flora
There are microorganisms that should not normally be present in the vagina of a healthy woman and the detection of which in a flora smear indicates the presence of a serious sexually transmitted disease. Of these infections in the smear, Trichomonas and gonococci are most often detected.
Trichomonas
These are the simplest microorganisms that have a flagellum and are capable of movement. Detection in a smear on the flora of Trichomonas indicates the presence of a sexually transmitted disease - trichomoniasis. Trichomoniasis in a pregnant woman increases the risk of preterm birth, premature rupture of amniotic fluid, intrauterine growth retardation. In addition, there is a risk of infection of the baby when passing through the birth canal, therefore, if Trichomonas is found in a smear, antibacterial treatment is mandatory during pregnancy.
Trichomoniasis in a pregnant woman increases the risk of preterm birth, premature rupture of amniotic fluid, intrauterine growth retardation. In addition, there is a risk of infection of the baby when passing through the birth canal, therefore, if Trichomonas is found in a smear, antibacterial treatment is mandatory during pregnancy.
Gonococci
These are bacteria that look like double bean-shaped balls in the smear, adjacent to each other with a concave side. Detection of gonococci in a smear allows the doctor to make a diagnosis - gonorrhea. This is a sexually transmitted disease, which must also be cured during pregnancy. The inflammatory process caused by gonococcus significantly complicates the course of pregnancy, can lead to miscarriage, premature birth, premature rupture of amniotic fluid, infection of the placenta and membranes, and in addition, when the baby passes through the birth canal, the eyes of the newborn are affected by gonococcus.
Detection of pathogens of other sexually transmitted infections in a smear on the flora is very difficult. Therefore, in the presence of an inflammatory process according to the smear, the doctor usually recommends testing for sexual infections by another, more sensitive method - a PCR smear.
Therefore, in the presence of an inflammatory process according to the smear, the doctor usually recommends testing for sexual infections by another, more sensitive method - a PCR smear.
Rules for preparation for taking a smear for flora
In order for the result of a smear for flora to be reliable, a number of important conditions must be observed before taking this analysis. Within 2-3 days, you can not use any vaginal suppositories or creams, douching with any solutions is contraindicated, since they change the composition of the vaginal microflora, making it difficult to identify the causative agent of inflammation. In addition, within 2 days it is desirable to refrain from sexual intercourse. This is also due to the fact that spermatozoa and residual semen in the vagina can lead to an incorrect smear result for flora. 9Pregnancy it is recommended to visit an obstetrician-gynecologist every 4 weeks up to 30 weeks, every 2 weeks after 30–32 weeks, and once a week after 37 weeks and until childbirth. For each visit to the doctor, the expectant mother should have the results of certain tests on hand. This allows you to monitor the health status of both the woman and the unborn baby, which means predicting the risk of developing complications and diseases, if necessary, prescribing and adjusting treatment in time. What are the deadlines and what needs to be submitted?
For each visit to the doctor, the expectant mother should have the results of certain tests on hand. This allows you to monitor the health status of both the woman and the unborn baby, which means predicting the risk of developing complications and diseases, if necessary, prescribing and adjusting treatment in time. What are the deadlines and what needs to be submitted?
6-10 weeks
This is usually the time a woman sees her doctor for the first time about her pregnancy and many tests are ordered right away. Very important clinical analysis of urine. The results must be presented at every visit to the doctor, as they show how the body copes with the load.
The main indicators of this study are the levels of protein, bilirubin and glucose. The words “traces of protein or glucose” indicate that there are very few of them and the analysis must be repeated. The detection of these substances in significant amounts may be a symptom of pregnancy complications.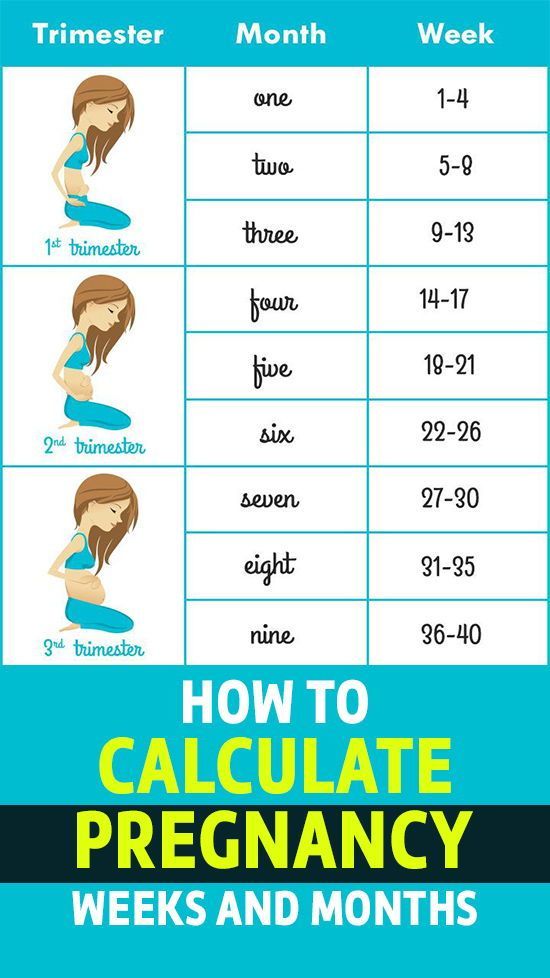 Their risk increases as the duration of pregnancy increases. Because the further, the more closely the doctors monitor these parameters.
Their risk increases as the duration of pregnancy increases. Because the further, the more closely the doctors monitor these parameters.
The presence of ketone bodies is a signal that the body lacks fluid and needs to drink more. Single erythrocytes and cylinders, epithelium, up to 3-4 leukocytes per field of view, the presence of salts is also a variant of the norm. An excess of white blood cells can indicate a malfunction of the kidneys and inflammation in the urinary tract. Normal urine is clear; if it is cloudy, there is a suspicion of incipient inflammation. Its acidity (pH) should be 5–5.5. Otherwise, disinfectant properties are reduced, and the doctor will advise you to drink acidic drinks - for example, cranberry juice.
Also donate urine for inoculation for sterility. This study allows you to notice in time the asymptomatic excretion of bacteria that provokes the inflammatory process. If the results differ from the norm, treatment is prescribed.
- Photo
- Getty Images/iStockphoto
Special conditions
In order for the results of urine tests to be reliable, certain conditions must be met when they are submitted. On the eve, fruits and vegetables that stain urine, such as carrots and beets, should be discarded. Immediately before collection, it is necessary to conduct a thorough toilet of the external genital organs. Urine should be morning, the container should be clean. Since secretions from the genital tract increase during pregnancy, and when urinating, they can get into the container and affect the results, it is recommended to plug the vagina with a regular cotton swab before urinating. For analysis, you need to collect at least 70–100 ml of an average portion of urine. The material intended for research should be in the laboratory no later than 1.5–2 hours after collection.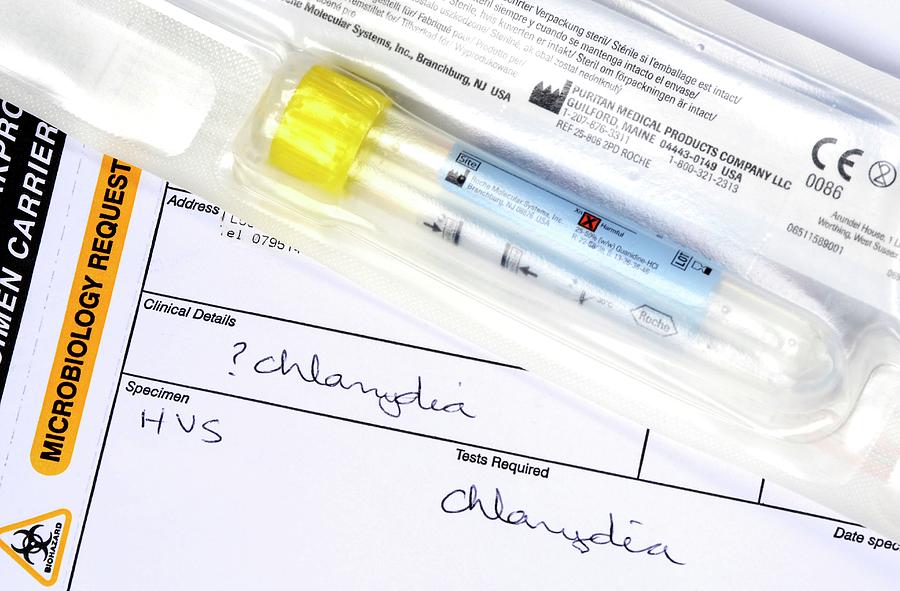 During long-term transportation, the physical properties of urine may change, bacteria multiply, etc.
During long-term transportation, the physical properties of urine may change, bacteria multiply, etc.
Strictly fasted blood tests - clinical, biochemical, coagulogram, antibodies to HIV, syphilis, hepatitis B, C and TORCH infections. In addition, blood type and Rh factor are determined. This is done at once, in one visit.
Clinical blood test is taken every 4 weeks until delivery. Attention is drawn to the level of hemoglobin, erythrocytes, leukocytes, platelets. The hemoglobin level can decrease to 110 g / l, the number of red blood cells - up to 3 x 1012 - 4 x 1012 / l. The number of leukocytes, on the contrary, increases to 12 x 109- 14 x 109 / l. Platelets are not affected by a normal pregnancy. Their decrease may indicate complications that have arisen.
Biochemical blood test allows you to monitor the functioning of the liver, kidneys and other internal organs. Liver function is indicated by the levels of bilirubin, ALT and AST. The work of the kidneys is judged by the amount of creatinine, urea and uric acid. Anxiety in both cases should cause an excess of the norm, which indicates that the organs cannot cope with the load and additional research is needed. They also control glucose levels. High readings are a signal that there is a possible risk of gestational diabetes.
The work of the kidneys is judged by the amount of creatinine, urea and uric acid. Anxiety in both cases should cause an excess of the norm, which indicates that the organs cannot cope with the load and additional research is needed. They also control glucose levels. High readings are a signal that there is a possible risk of gestational diabetes.
Coagulogram characterizes the work of the blood coagulation system. Preparing for childbirth, the body accumulates a supply of coagulation components. Doctors monitor this process and, in case of deviations from the norm, prescribe treatment.
Interpretation of the coagulogram during pregnancy should only be a doctor observing the expectant mother. Even if the indicators do not fit within the normal range, you should not take this as a disaster. Often these are simply individual fluctuations in levels.
- Photo
- Getty Images
Test results for antibodies to HIV, syphilis, hepatitis B and C must be negative. Otherwise, preventive treatment is prescribed to avoid intrauterine infection of the unborn child with dangerous infections.
Otherwise, preventive treatment is prescribed to avoid intrauterine infection of the unborn child with dangerous infections.
But with TORCH infections (toxoplasmosis, rubella, cytomegalovirus and herpes), the situation is different. According to the level of antibodies, immunoglobulins of classes G and M, doctors monitor whether the expectant mother is a carrier of the infection and at what stage the process is - chronic or acute. If there are no antibodies, the woman is at risk and should repeat this test every trimester. She is likely to get infected for the first time during pregnancy, and these infections can adversely affect the development of the internal organs of the unborn baby. This turn of events is indicated by the presence of class M immunoglobulins. The expectant mother must be prescribed additional studies, clarify the diagnosis and carry out treatment. If serious deviations in the development of the baby are detected, it may be proposed to terminate the pregnancy. If only class G immunoglobulins are detected, there is no danger to the child.
If only class G immunoglobulins are detected, there is no danger to the child.
At the same time, blood is taken to determine Rh factor . With a negative Rh, the titer of Rh antibodies is immediately determined, and this study is repeated every 4 weeks. The analysis allows diagnosing and tracking the development of the Rhesus conflict between the expectant mother and the child to be born. If there are no Rh antibodies, anti-Rhesus immunoglobulin is administered prophylactically at 28–30 weeks, and the analysis is not given until the end of pregnancy.
A swab is also taken from the cervix to detect atypical cells, as well as a swab from the vagina, cervical and urethra for microscopic examination. This allows you to identify inflammation and detect pathogens of gonorrhea, trichomoniasis and chlamydia, which can be dangerous for the baby.
The expectant mother is not required to take tests that are not included in the standard of pregnancy management.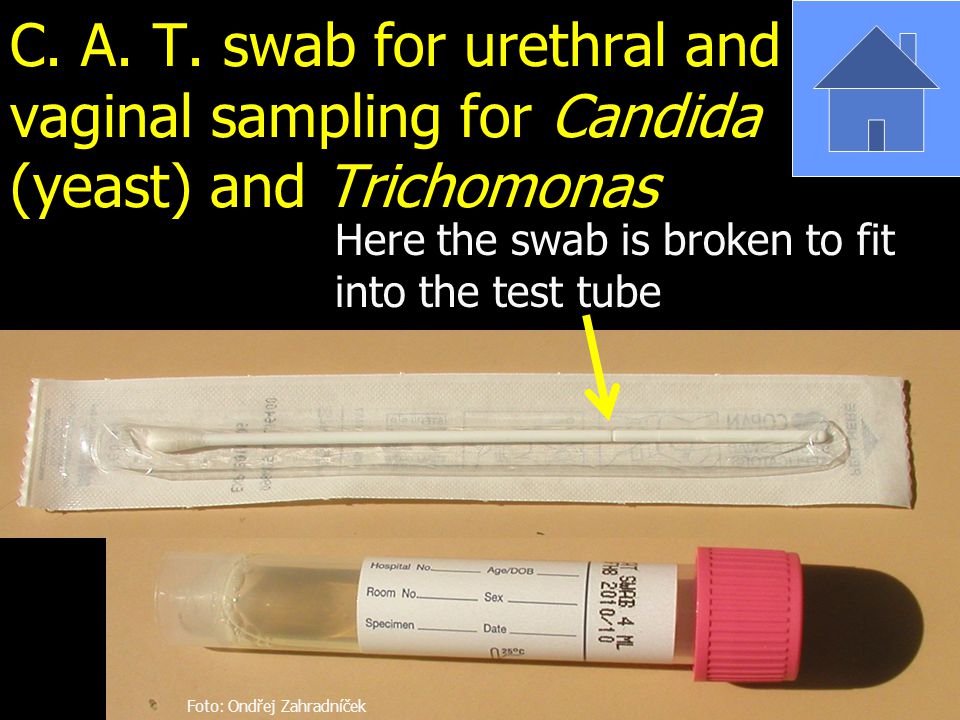 These include, for example, PCR studies for ureaplasma, mycoplasma and other pathogens. An analysis for the detection of these microorganisms is indicated only if a woman complains of discomfort, itching in the vagina, a change in the color of discharge from it, etc.
These include, for example, PCR studies for ureaplasma, mycoplasma and other pathogens. An analysis for the detection of these microorganisms is indicated only if a woman complains of discomfort, itching in the vagina, a change in the color of discharge from it, etc.
- Photo
- Getty Images
10-12 weeks
In addition to the mentioned clinical blood and urine tests, the expectant mother must pass a combined double test. This genetic screening allows you to determine whether a woman is at risk for the possibility of having a child with chromosomal diseases. In a blood test taken on an empty stomach from a vein, biochemical markers are determined - human chorionic gonadotropin (hCG) and pregnancy-associated plasma protein-A (PAPP-A). The first is a pregnancy hormone, the second is a blood plasma protein. The results are considered only together with the ultrasound data performed at the same time. That is why the test is called combined.
That is why the test is called combined.
14-20 weeks
If for some reason a double test was not taken, at 16-20 weeks the woman will be asked to take a triple combined test. The levels of alpha-fetoprotein (AFP), human chorionic gonadotropin and free estriol are being studied. The results are also considered together with the ultrasound data. Screening data is not a diagnosis, but only a calculation of the degree of risk. If necessary, it is recommended to visit a geneticist.
24-28 weeks
Pregnant women are encouraged to take a glucose tolerance test. With its help, diabetes mellitus caused by pregnancy is detected. It is important to meet the deadlines: after 30 weeks, the study should not be carried out, since the glucose load becomes dangerous for the unborn child. Strictly on an empty stomach, a blood test for sugar is taken. If its level is exceeded, the test is canceled and the woman is referred for a consultation with an endocrinologist. When the fasting glucose level is normal, 75 g of glucose dissolved in water is drunk and the pregnant woman is at rest for 2 hours. After that, the blood sugar content is again determined. Based on the results, one can judge how the body metabolizes glucose, whether consultation with an endocrinologist and, accordingly, treatment is needed.
When the fasting glucose level is normal, 75 g of glucose dissolved in water is drunk and the pregnant woman is at rest for 2 hours. After that, the blood sugar content is again determined. Based on the results, one can judge how the body metabolizes glucose, whether consultation with an endocrinologist and, accordingly, treatment is needed.
30-32 weeks
The second time they take a biochemical blood test, a coagulogram, blood tests for HIV, syphilis, hepatitis B and C, as well as a smear from the vagina, cervical and urethra for microscopic examination. You should be wary if the protein level in the results of a biochemical blood test is below 60-65 g / l: this can lead to edema. In this case, the woman may be assigned additional studies and give recommendations on nutrition and lifestyle. As for the coagulogram, the coagulation indicators, especially the level of fibrinogen, should increase compared to the first analysis, but up to certain limits. With deviations in one direction or another, an examination is prescribed to exclude the risk of thrombosis and DIC. Repeated infectious screening is done because a woman can become infected with microorganisms that are dangerous for the unborn child at any time, and it is possible to detect antibodies to the virus in the blood not immediately after the latter enters the body. After all, there is an incubation period - different for each infection.
Repeated infectious screening is done because a woman can become infected with microorganisms that are dangerous for the unborn child at any time, and it is possible to detect antibodies to the virus in the blood not immediately after the latter enters the body. After all, there is an incubation period - different for each infection.
35–37 weeks
A third vaginal, cervical and urethral swab and culture of vaginal discharge is recommended. If something is found, treatment can be carried out before delivery. Please note that primary infection with the genital herpes virus a month or less before delivery is an indication for caesarean section. At 36–37 weeks, clinical blood and urine tests, a biochemical blood test, a coagulogram are again done, and blood is also taken to detect antibodies to HIV, syphilis, hepatitis B and C, if the last study was conducted more than 3 months ago. It is not recommended to neglect this analysis: with overdue data, a woman in labor can be hospitalized in the observational department of the maternity hospital.