Feeling depressed when pregnant
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Psycho-emotional state of a woman during pregnancy, childbirth and the postpartum period
Expecting a child, childbirth and caring for a newborn are the most important period in the life of every woman, which should be accompanied by feelings of joy and satisfaction. At the same time, the emotional, hormonal and physical changes in a woman's body that occur during this period can cause sadness, confusion, fear, and possibly even anger and aggressiveness. Young mothers are often confused by these opposing feelings, especially when confronted with the idealized public understanding of motherhood. The discrepancy between one's own feelings and idealized social expectations causes a feeling of guilt and shame. Most women cope with these emotional problems over time, but for some, they not only do not go away, but even intensify, acquiring forms of maternal depression.
The discrepancy between one's own feelings and idealized social expectations causes a feeling of guilt and shame. Most women cope with these emotional problems over time, but for some, they not only do not go away, but even intensify, acquiring forms of maternal depression.
Depression can be caused by unwanted pregnancy, memories of sexual abuse, childhood abuse. Although it has been proven that depression can happen to almost any woman both during and after pregnancy, one should pay attention to these prerequisites and risk factors in order to prevent or prepare in advance for possible manifestations of depression.
A mother who is in a depressed state cannot have a positive emotional impact on the child and sufficiently stimulate his development, which is fraught with a delay in the development of the child.
Some women who suffer from depression stop taking care of themselves. They begin to eat poorly, suffer from constant fatigue and insomnia, do not visit a doctor, do not follow medical prescriptions, and may begin to abuse harmful substances such as tobacco, alcohol and drugs.
Depression can seriously affect a woman's ability to perform her maternal functions. Loss of interest in the child, irritability and fatigue can prevent the mother from giving the child the necessary love, tenderness and caress and providing him with proper care. As a result, a woman develops a sense of guilt, she loses self-confidence as a mother, which further aggravates her depressive state.
During pregnancy and after childbirth, every second woman may have some manifestations of maternal depression, which includes a whole range of physical and emotional changes. These conditions can have a negative impact on a woman's mental health, her maternal qualities, family life and child development
Antenatal depression occurs during pregnancy, when biological and hormonal changes occur in a woman's body. Depressive symptoms include frequent mood swings, bouts of bad mood, tearfulness, irritability, and insomnia. But all pregnant women have such manifestations from time to time. Therefore, it is very important to recognize depression in time, because. many women who have experienced prenatal depression continue to suffer from it after childbirth. Timely consultation (doctors and psychologists) would be appropriate here.
But all pregnant women have such manifestations from time to time. Therefore, it is very important to recognize depression in time, because. many women who have experienced prenatal depression continue to suffer from it after childbirth. Timely consultation (doctors and psychologists) would be appropriate here.
Postpartum sadness is considered normal. 50-80% of women go through this condition after childbirth. A woman can cry long and disappointingly for no apparent reason, feel tired and irritated, suffer from insomnia. Such symptoms usually begin on the fifth day after the birth of the child and last 7-10 days. These symptoms resolve and do not harm the mother or prevent her from caring for the baby. There is no need to treat postpartum sadness. The main thing is that a woman and her entourage know and understand what is happening with a young mother, what to expect and, if necessary, could seek qualified help.
Postpartum depression is a clinically defined condition that requires the attention of a healthcare professional. During pregnancy, the amount of hormones (progesterone and estrogen) in a woman's body increases dramatically, and during the first 24 hours after childbirth, it rapidly drops to their normal "non-pregnant" level. Scientists believe that the rapid change in hormone levels can cause depression. Another cause of postpartum depression may be the level of hormones produced by the thyroid gland. Low thyroid hormone levels can cause low mood, loss of interest in the world around you, irritability, weakness, difficulty concentrating, trouble sleeping, and weight gain. A blood test for thyroid hormones helps to reveal a reliable picture of the disorder.
During pregnancy, the amount of hormones (progesterone and estrogen) in a woman's body increases dramatically, and during the first 24 hours after childbirth, it rapidly drops to their normal "non-pregnant" level. Scientists believe that the rapid change in hormone levels can cause depression. Another cause of postpartum depression may be the level of hormones produced by the thyroid gland. Low thyroid hormone levels can cause low mood, loss of interest in the world around you, irritability, weakness, difficulty concentrating, trouble sleeping, and weight gain. A blood test for thyroid hormones helps to reveal a reliable picture of the disorder.
Symptoms of postpartum depression:
- Long periods of poor mood,
- irritability,
- sleep disorders,
- appetite disorders,
- fatigue,
- loss of interest in life,
22222222 - inability to cope with the rhythm of life,
- feeling of guilt and despair,
- feeling of underestimation of others,
- indecision,
- decrease in concentration,
- thoughts about harming yourself and the child.
This condition can last from a few weeks to a year or even more. Approximately 8-15% of women who give birth experience postpartum depression. A woman with these symptoms requires the immediate help of specialists, especially doctors.
Postpartum psychosis is the most complex of all conditions associated with maternal depression. It includes symptoms of hallucinations and obsessions, as well as suicide attempts and child murder. Because of its complexity, postpartum psychosis is considered a psychiatric emergency. This condition occurs in 1-3 women per thousand, but it deserves the closest attention, since the development of symptoms can be rapid.
Psychologists and physicians agree that for a sedentary lifestyle during pregnancy, women pay with complications during childbirth and the health of the child.
Improving the emotional and physical condition of women during pregnancy, preparing women for childbirth has a positive effect on medical indicators - it contributes to a favorable course of pregnancy and childbirth; reducing the number of birth injuries; reducing pain during childbirth; the number of complications and surgical interventions - a woman becomes an active participant in the process of childbirth, the level of postpartum depression decreases; adaptation to the appearance of a new family member is accelerated, etc.
Today, both domestic and foreign methods of preparing for childbirth are widely used. A large number of existing studies and developed programs are devoted to finding the most effective ways of non-drug pain relief in childbirth, teaching women using auto-training.
Recently, when preparing pregnant women for childbirth , more and more emphasis is placed on the mental characteristics of pregnant women, their emotional state, creating positive emotions and providing an optimal psychophysical environment for the birth of a child.
At present, all components of preparation for childbirth are taken into account in preventive work: the formation of a maternal dominant, a positive emotional mood of a woman for childbirth; learning to master stable skills of self-control in childbirth, breathing, muscle and general psycho-emotional relaxation.
Maternal and child health, Mental and physical well-being of the future generation is one of the priorities of our state.
REMEMBER!
Your health and health
Your baby is in your hands!
Take care of him!
Head of antenatal clinic O.S. Mikulich L.A.
Depression and Pregnancy - Phoenix Center
Women today suffer from depression more than previous generations
Studies show that 1 in 7 women experience prenatal depression or0019 pregnancy .
According to an open study, modern women are more likely than their mothers to experience prenatal depression or depression during pregnancy. Prenatal depression is quite common and affects 10 to 15% of pregnant women.
Depression is a mental disorder that affects the entire body during pregnancy.
Signs of depression during pregnancy can range from loss of interest in enjoyable activities and feelings of worthlessness to changes in appetite and fatigue.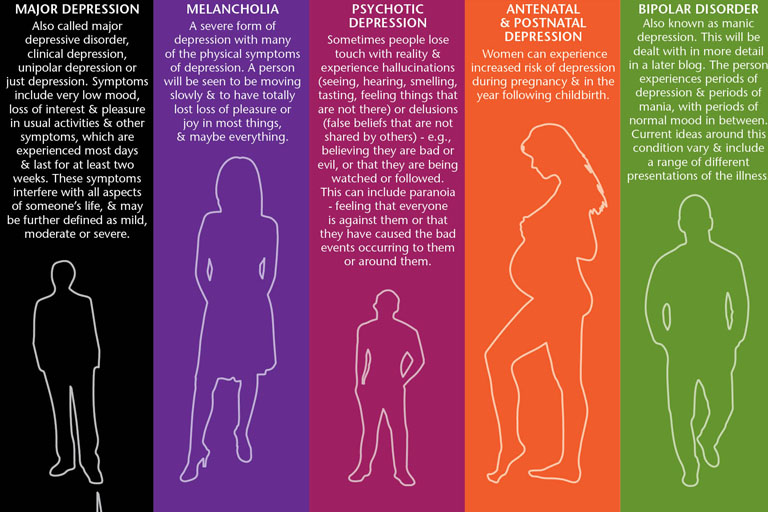
Symptoms of depression during pregnancy are very similar to depression that occurs at other times in life. A pregnant woman may also worry about the birth of her child or about her inferiority and failure as a mother.
Pregnant women who have anxiety problems, who have an unplanned pregnancy, or who are stressed about the baby's well-being are at increased risk of depression during pregnancy. Women who receive fertility treatment are also at increased risk. They may worry about the effect of treatment on pregnancy.
About 17% of mothers reported experiencing severe symptoms of depression, while 25% of mothers reported experiencing depression during pregnancy. The mothers in both groups were between the ages of 19 and 24 when they were interviewed.
Why should young mothers, such as those in an open study, be depressed? We know that financial stress and lack of support increase the risk of depression, and new moms may be less likely to access these financial and interpersonal resources. However, depression during pregnancy can affect women of all ages.
However, depression during pregnancy can affect women of all ages.
Can maternal depression affect the unborn child?
If left untreated, a mother's depression can negatively affect her baby. There are risks to the developing fetus. When a mother is under stress, cortisol is released, which can negatively affect the development of the baby. According to research, the baby of a depressed mother may be born too small or too early.
Experts say pregnant women with depression should know there are effective treatments available to help them learn how to deal with depression.
The network's open study states that depression rates in young pregnant women are higher than in the 1990s and steps need to be taken to support these mothers-to-be. The results of the study highlight the need to expand screening and resources to support young pregnant women and minimize the potentially far-reaching effects of depression on mothers, their children, and future generations.
Is there an effective treatment?
Both medication and psychotherapy are effective treatments for depression during pregnancy, experts say. Psychiatrists say what usually happens is that when a woman finds out she's pregnant, she stops taking her psychiatric medication. Unfortunately, this is not necessarily specified.
There are risks associated with both medication and untreated depression. Pregnant women should always consult a psychiatrist, but often, especially in cases of severe depression, the benefits of antidepressants may outweigh the risks.
In addition to medication, social support is critical for a pregnant woman who is experiencing depression. A formal support group can help, or just connecting with peers and hanging out with friends can help the mom-to-be not feel isolated. Therapies such as Interpersonal Psychotherapy and Cognitive Behavioral Therapy (CBT) have also been shown to be helpful.
To determine which course of treatment is best for you, discuss it with your healthcare provider to discuss the benefits and risks.