What causes stillbirth at 20 weeks
Stillbirth: Definition, Causes & Prevention
Overview
What is a stillbirth?
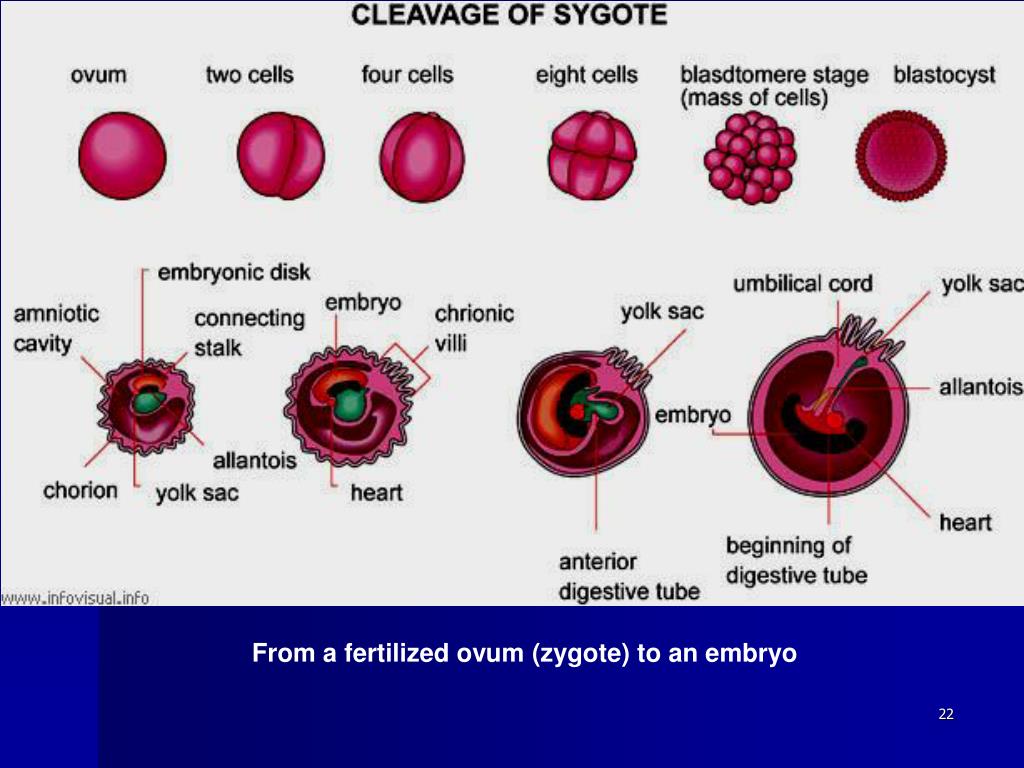
A stillbirth is when a fetus dies after the mother’s 20th week of pregnancy. The fetus may have died in the uterus weeks or hours before labor. Rarely, the fetus may die during labor. Although prenatal care has drastically improved over the years, the reality is stillbirths still happen and often go unexplained.
A stillbirth is classified as either an early stillbirth, a late stillbirth, or a term stillbirth. Those types are determined by the number of weeks of pregnancy:
- Early stillbirth: The fetus dies between 20 and 27 weeks.
- Late stillbirth: The fetus dies between 28 and 36 weeks.
- Term stillbirth: The fetus dies the 37th week or after.
How common are stillbirths?
A stillbirth occurs in about one of 160 births (about 24,000 babies per year in the United States).
Who is at risk of having a stillbirth?
A stillbirth can happen to pregnant people of any age, background, or ethnicity. They can be unpredictable — 1 in 3 cases go unexplained. There are some ways you can reduce your risk, though. You’re more likely to have a stillbirth if you:
- Smoke, drink alcohol, or use recreational drugs.
- Are over the age of 35.
- Have poor prenatal care.
- Are malnourished.
- Are Black.
- Are having multiple births (twins or more).
- Have a preexisting health condition.
- Have obesity (body mass index above 30).
What’s the difference between a stillbirth and a miscarriage?
Like a stillbirth, a miscarriage is also a pregnancy loss. However, while a stillbirth is the loss of a fetus after 20 weeks of pregnancy, a miscarriage happens before the 20th week.
Symptoms and Causes
What causes a stillbirth?
The cause of the stillbirth is vital not only for the healthcare providers to know, but for the parents to help with the grieving process. The cause is not always known (1 in 3 stillbirths cannot be explained), but the most likely causes include:
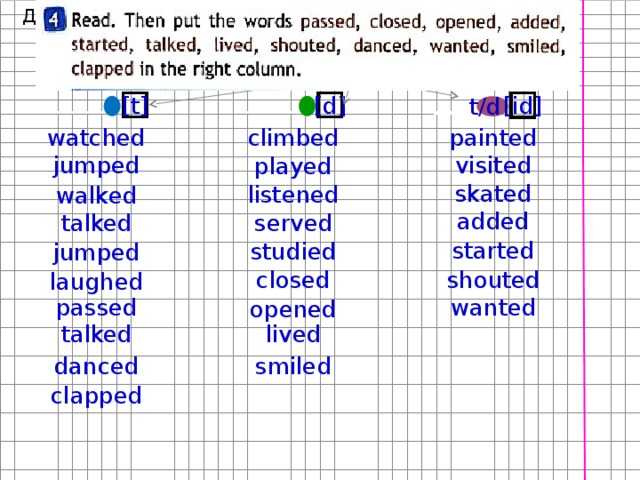
- Problems with the placenta and/or the umbilical cord.
 Your placenta is an organ that lines your uterus when you’re pregnant. Through it and the umbilical cord, the fetus gets blood, oxygen and nutrients. Any problems with your placenta or umbilical cord and the fetus will not develop properly.
Your placenta is an organ that lines your uterus when you’re pregnant. Through it and the umbilical cord, the fetus gets blood, oxygen and nutrients. Any problems with your placenta or umbilical cord and the fetus will not develop properly. - Preeclampsia. Preeclampsia is high blood pressure and swelling that often happens late in pregnancy. If you have preeclampsia, you have twice the risk of placental abruption or stillbirth.
- Lupus. A person who has lupus is at risk of having a stillbirth.
- Clotting disorders. A person with a blood clotting disorder like hemophilia is at a high risk.
- The pregnant person's medical conditions. Other illnesses can sometimes cause stillbirths. The list includes diabetes, heart disease, thyroid disease, or a viral or bacterial infection.
- Lifestyle choices. If your lifestyle includes drinking, using recreational drugs and/or smoking, you’re more likely to have a stillbirth.

- Birth defects. One or more birth defects cause about 25% of stillbirths. Birth defects are rarely discovered without a thorough examination of the fetus, including an autopsy.
- Infection. An infection between week 24 and week 27 can cause fetal death. Usually, it’s a bacterial infection that travels from your vagina to your uterus. Common bacteria include Group B Streptococcus, E. coli, klebsiella, enterococcus, Haemophilus influenza, chlamydia and mycoplasma or ureaplasma. Additional problems include rubella, the flu, herpes, Lyme disease and malaria, among others. Some infections go unnoticed until there are serious complications.
- Trauma. Trauma such as a car crash can result in a stillbirth.
- Intrahepatic cholestasis of pregnancy (ICP). Also known as obstetric cholestasis, this is a liver disorder that includes severe itching.
What physical symptoms does the mother have after stillbirth?
If you have a fever, bleeding, chills, or pain, be sure to contact your healthcare provider right away because these may be signs of an infection.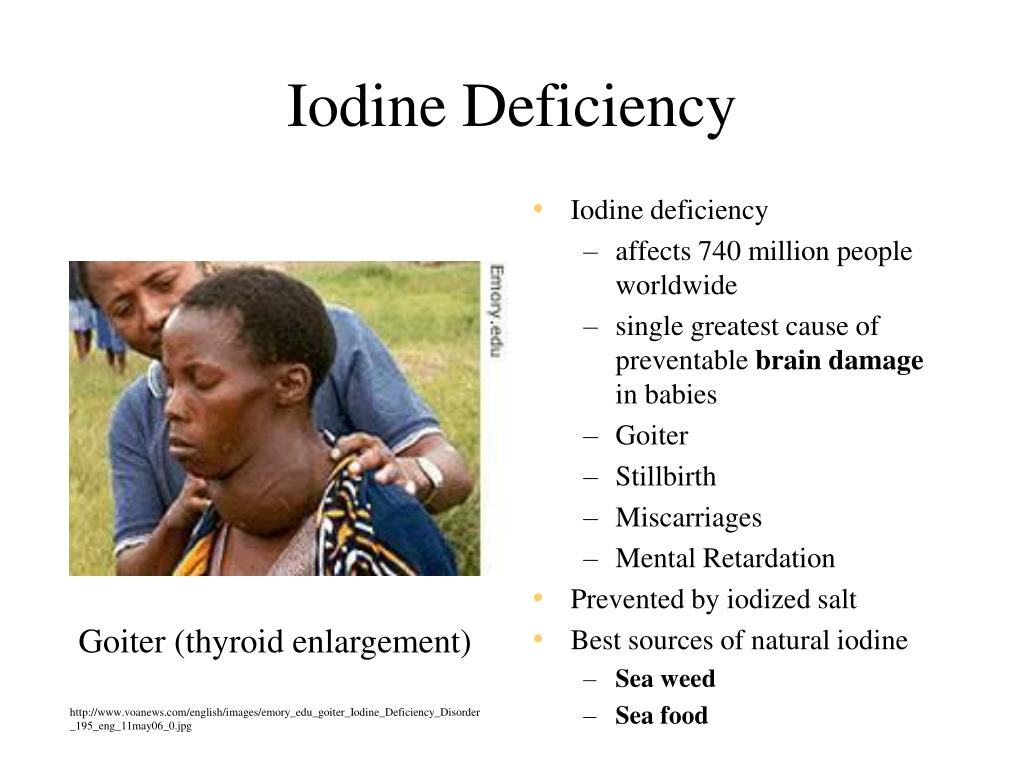
Will I lactate after a stillbirth?
After the delivery of the placenta, the milk-producing hormones may be activated (lactation). You might start to produce breast milk. Unless you have preeclampsia, you can take medicines called dopamine agonists that may stop your breasts from producing milk. You can also choose to let the lactation stop naturally.
Does stillbirth cause infertility?
No. A stillbirth does not cause infertility and it doesn’t indicate that there is a problem with it.
Diagnosis and Tests
How is the diagnosis made?
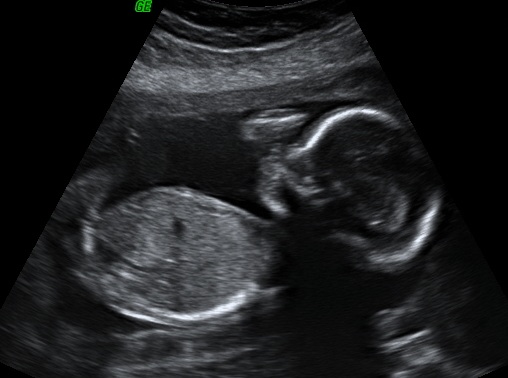
Usually, you’ll notice that the fetus isn’t as active as it used to be. An ultrasound will confirm if the fetus has passed.
How can I find out what caused my stillbirth?
To discover the cause, your healthcare provider will perform one or more of the following tests:
- Blood Tests. Blood tests will show if you have preeclampsia, obstetric cholestasis or diabetes.
- Examination of the umbilical cord, membranes and placenta.
 These tissues attach to your fetus. An abnormality could prevent the fetus from receiving oxygen, blood and nutrients.
These tissues attach to your fetus. An abnormality could prevent the fetus from receiving oxygen, blood and nutrients. - Tests for infection. Healthcare providers will take a sample of your urine, blood, or cells from your vagina or cervix to test for infection.
- Thyroid function test. This test will determine if there’s something wrong with your thyroid gland.
- Genetic tests. Your healthcare provider will take a sample of the umbilical cord to determine if the fetus had genetic problems such as Down’s syndrome.
Your healthcare provider will also review medical records and the circumstances surrounding the stillbirth. With your consent, an autopsy can be performed to determine the cause of fetal death. An autopsy is a surgical procedure performed by a skilled pathologist. Incisions are made carefully to avoid disfigurement, and the incisions are surgically repaired afterward. You have the right to limit the autopsy to eliminate any incisions on your baby that are uncomfortable for you. Be sure to write these requests on the autopsy permission form.
Be sure to write these requests on the autopsy permission form.
Some hospitals don't perform autopsies, so your baby may have to be transported to another hospital. Be sure you feel comfortable with where your child is being taken. You also have the right to deny an autopsy, if that is your wish.
An autopsy may be legally required in some cases, including when:
- A baby died within 24 hours of a surgical operation.
- A healthcare provider can't certify the cause of death.
- A baby was alive and then died suddenly.
Management and Treatment
What happens after a stillborn baby passes away?
If the fetus passes away before you’re in labor, you have three options:
- Induced labor.
- Natural birth.
- Cesarean section.
Induced labor. Healthcare providers recommend induced labor as the best option after a stillbirth. It should be done immediately if you:
- Have severe preeclampsia (high blood pressure).
- Have a serious infection.
- Have a broken amniotic sac (the bag of water around the fetus).
- Have any clotting disorder.
The labor is induced using medicine dispensed in one of five ways:
- A tablet inserted into your vagina.
- A gel inserted into your vagina.
- A swallowed tablet.
- A drip into a vein.
- A Foley bulb. A mechanical balloon that widens the cervix.
Natural birth. Waiting for birth to happen naturally is an option but, as time goes by, the fetal body may deteriorate in your uterus. The fetus may look different than you expect. The deterioration also makes it more difficult to determine the cause of death.
Cesarean section. A cesarean section is not recommended because it’s not as safe as a natural birth or induced labor.
What happens after a stillborn baby is delivered?
You'll be able to hold your baby, and your healthcare providers will allow you as much time as you need to spend with your child. You may feel uncomfortable with this idea at first.
You may feel uncomfortable with this idea at first.
You may want to ask for any mementos and keepsakes of your child, such as a blanket, a lock of your child’s hair, the hospital ID bracelet, etc. You can take pictures. This may also be uncomfortable, but it may be a cherished possession at a later time and may help you during your grieving process. Most hospitals will issue the family a birth certificate, but make sure you ask and request that it include the baby's handprints and footprints.
Prevention
Can a stillbirth be prevented?
Usually, a stillbirth can't be prevented. It often occurs because the fetus wasn't developing normally. Generally, improving your health, including managing preexisting conditions and lifestyle choices, increases your chances of a successful pregnancy. You’re also less likely to have a stillbirth if, when you know you’re high-risk, you’re carefully monitored through routine ultrasounds and/or fetal heart rate monitoring. If your healthcare provider finds a problem, they can have your baby delivered early if necessary.
How can I reduce my risk of having a stillbirth?
Because the reason why a stillbirth happens isn't always understood, it is difficult to prevent. However, there are some steps you can take to increase your chances of having a healthy baby:
- Avoid recreational drugs, smoking and drinking alcohol.
- Contact your healthcare provider if there’s any bleeding during the second half of your pregnancy.
- Do what’s called a daily “kick count.” Around 26-28 weeks, familiarize yourself with fetal movements. Figure out what’s normal for the fetus. Then, if they stop acting normally, contact your healthcare provider.
- Before you get pregnant, work toward a weight that's healthy for you. If you’re already pregnant, talk with your healthcare provider about diet and exercise options.
- Protect yourself against infections.
- Avoid certain foods including some types of fish and some types of cheese. Also, double-check to make sure that any meat or poultry you eat is thoroughly cooked.
- Report any stomach pain, itching, or vaginal bleeding immediately.
- Sleep on your side, not your back. If you’ve been pregnant for 28 weeks or more, sleeping on your back can double the risk of stillbirth. It’s not completely clear why that makes a difference, but experts suspect that it has something to do with the flow of blood and oxygen to the fetus.
- Get routine tests, including your blood pressure and urine. These will help your healthcare provider see if there are any illnesses or conditions that may affect the health of your baby.
Can the food I eat prevent stillbirth?
Unfortunately, eating or avoiding a specific food can’t guarantee you won’t have a stillbirth. However, there are some foods you should stay away from to improve the chances of a healthy pregnancy in general. Avoid the following:
- Mold-ripened soft cheeses and soft blue cheeses.
- Unpasteurized milk and unpasteurized milk products.
- Raw or undercooked meat.

- Liver products.
- Pâté.
- Game meats.
- Raw or partially cooked eggs.
- Duck, goose or quail eggs.
- Swordfish, marlin, shark and raw shellfish.
- Limit caffeinated drinks and herbal teas.
Outlook / Prognosis
When should I see my healthcare provider after the natural birth or induced labor?
You’ll likely have a follow-up appointment with your healthcare provider a few weeks later. At that time the post-mortem and test results will be discussed and you can voice concerns about future pregnancies.
Can I get pregnant after I've delivered a stillborn baby?
Yes. Most people who deliver stillborn babies go on to have normal pregnancies and births. If the stillbirth was caused by a birth defect or umbilical cord problem, the chances of another stillbirth is slight. If the cause was an illness the pregnant person has or a genetic disorder, the risk is somewhat higher. The chance that your next pregnancy will result in stillbirth is about 3%, which means that most post-stillbirth pregnancies result in healthy babies.
How long after a stillbirth should I get pregnant again?
Discuss the timing of your next pregnancy with your healthcare provider to make sure you are physically ready to begin a new pregnancy. Some healthcare providers recommend waiting a certain amount of time (from six months to one year) before trying to conceive again. Some studies have shown that people who wait at least one year to conceive may have less depression and anxiety during a later pregnancy.
Statistics show that about 60% of couples take up to six months to conceive after delivery of a stillborn baby, and another 30% take up to 12 months. Don't be surprised if things don't happen quickly.
Living With
Is a funeral necessary after a stillbirth?
After the death of your baby, one of the first decisions you will be faced with is whether or not to need to arrange a funeral.
The type of arrangements you make may play an important role in the grieving process. It is a decision that only you and the other parent can make together. You may find that you need time to make your decisions and arrangements. It is quite common for families to take up to a week (and sometimes longer) to make arrangements. This is okay.
You may find that you need time to make your decisions and arrangements. It is quite common for families to take up to a week (and sometimes longer) to make arrangements. This is okay.
No matter what your choice is, you have the right to change your mind. Be sure you ask whoever is carrying out your arrangements about how long you have to make any changes.
How should I communicate with my other children after a stillbirth?
You may find your children are a comfort, a worry, or just too hard to deal with. These are normal reactions. Take time to grieve and say goodbye to the child you lost. You will eventually feel normal feelings for your living children again, and the bond you have with them may possibly become stronger.
No matter how much you may want to shelter your children from pain, they can sense the emotion around them. Honesty is the best way to help your children cope with this painful experience. Children have a different understanding of death at different developmental stages.
What can I do to cope with a stillbirth?
Take as much time as you need to heal physically and emotionally after a stillbirth. Regardless of the stage of pregnancy during which your loss occurred, you are still a parent and the life you nurtured was real. It is completely normal for you to experience depression and post-traumatic stress disorder (PTSD). Above all, don't blame yourself. Give yourself time to cope, grieve and accept your devastating loss.
Counseling is available. Pregnancy loss support groups may also be a good resource for both parents. Ask your healthcare provider for more information about counseling and support groups.
What questions should I ask my healthcare provider after a stillbirth?- What was the cause of the stillbirth?
- Is there anything else I can do to prevent a stillbirth in the future?
- Do you recommend a psychiatrist?
- Do you recommend a counselor?
- Do you recommend a support group?
- How soon do you recommend I get pregnant again?
- Does this hospital keep records of stillbirths?
- Can I get a copy of the records/birth certificate?
- When should I return for another appointment?
- How will I be cared for in the next pregnancy?
A note from Cleveland Clinic
A stillbirth can be devastating. It can be overwhelming and depressing for the parents, their children, the grandparents, and other family members and friends. The grieving can be even worse when a stillbirth happens for no known reason. Remember that it’s normal to have difficulty coping. Access mental health professionals if you need help.
It can be overwhelming and depressing for the parents, their children, the grandparents, and other family members and friends. The grieving can be even worse when a stillbirth happens for no known reason. Remember that it’s normal to have difficulty coping. Access mental health professionals if you need help.
Stay in contact with your healthcare providers before, during and after your pregnancy. Share your worries and ask questions. Do your best to avoid risk factors such as smoking and drinking. Also, remember that if you’ve had a stillbirth, you can get pregnant again. There is a 3% chance of another stillbirth.
Stillbirth
What is stillbirth?
Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy. Most stillbirths happen before a pregnant person goes into labor, but a small number happen during labor and birth. Stillbirth affects about 1 in 160 pregnancies each year in the United States.
Who is at risk for stillbirth?
Stillbirth can happen in any family. We don’t always know why stillbirth affects certain families more than others. Researchers are working to learn more about risk factors for stillbirth.
We don’t always know why stillbirth affects certain families more than others. Researchers are working to learn more about risk factors for stillbirth.
Risk factors are things that make you at risk for (more likely than others to have) a condition. Having a risk factor for stillbirth doesn’t mean for sure that you will have a stillbirth. But knowing about and reducing your risk factors may help prevent a stillbirth from happening to your baby. Some risk factors are things you can’t change, such as having a stillbirth in a previous pregnancy. Other risk factors are things you can do something about, like quitting smoking. Talk to your health care provider about what you can do to help reduce your risk factors for stillbirth.
According to the Centers for Disease Control and Prevention (also called CDC) and other experts, risk factors for stillbirth include:
Medical conditions
- Being obese. If you’re obese, you have an excess amount of body fat and your body mass index (also called BMI) is 30 or higher.
 BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi.
BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi. - Diabetes. Diabetes is a condition in which your body has too much sugar (called glucose) in the blood.
- High blood pressure. Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body.
- Substance abuse. Using certain harmful substances increase the risk of having a stillbirth. For example, smoking, drinking alcohol or using street drugs or prescription painkillers, such as opioids.
Pregnancy conditions and pregnancy history
- You’re pregnant with multiples (twins, triplets or more).
- You have intrahepatic cholestasis of pregnancy (also called ICP). This is the most common liver condition that happens during pregnancy.
- You had complications in a previous pregnancy, like premature birth, preeclampsia or fetal growth restriction.
 Preterm birth is a birth that happens too early, before 37 weeks of pregnancy. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant person has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Fetal growth restriction is when a baby doesn’t gain enough weight in the womb before birth.
Preterm birth is a birth that happens too early, before 37 weeks of pregnancy. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant person has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Fetal growth restriction is when a baby doesn’t gain enough weight in the womb before birth. - You’ve never given birth before.
- You had a miscarriage or stillbirth in a previous pregnancy. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
- You’re pregnant after the age of 35. According to the American College of Obstetricians and Gynecologists (ACOG), studies show that a large number of stillbirths that happen among pregnant people 35 or older are related to congenital or chromosomal conditions.
- You have little social support. Many unmarried people have strong social networks of families and friends who help them.
 However, some studies have reported a higher risk of stillbirth among unmarried people. Researchers think that this may be because they have less social support.
However, some studies have reported a higher risk of stillbirth among unmarried people. Researchers think that this may be because they have less social support.
Health Disparities and Racism
We do not know exactly why, but stillbirth happens more often in some groups compared with others. We call this a health disparity (difference). To understand why these groups are at a higher risk of having a stillbirth we need to look at the social factors affecting them, this is what we call social determinants of health. These are the conditions in which you are born, grow, work, live and age. These conditions affect your health throughout your life. In many cases, social determinants of health and health disparities are related to racism.
Racism refers to the false belief that certain groups of people are born with qualities that make them better than other groups of people.
Racism isn’t limited to personal attacks such as ethnic slurs, bullying, or physical assault. In a racist culture, one group of people has more power than other groups. People in the dominant racial or ethnic group make important decisions that affects everyone’s lives. For example, they have a lot of control over the way that schools, health care, housing, laws and law enforcement work. This control means that people in the dominant group are more likely to:
In a racist culture, one group of people has more power than other groups. People in the dominant racial or ethnic group make important decisions that affects everyone’s lives. For example, they have a lot of control over the way that schools, health care, housing, laws and law enforcement work. This control means that people in the dominant group are more likely to:
- Have better education and job opportunities
- Live in safer environmental conditions
- Be shown in a positive light by media, such as television shows, movies, and news programs.
- Be treated with respect by law enforcement
- Better access to health care
In contrast, people from racial or ethnic minority groups who live in a racist society are more likely to:
- Experience chronic stress
- Live in an unsafe neighborhood
- Live in areas that have higher amounts of environmental toxins, such as air, water, and soil pollution
- Go to a low-performing school
- Have limited access to healthy foods
- Have little or no access to health insurance and quality medical care
- Have less access to well-paying jobs
The Role of Chronic Stress
Studies have shown that the chronic stress caused by living in a racist culture is a factor in many health conditions, including having a preterm or low-birthweight baby. While some studies and statistics mention race as a risk factor for these conditions, we can’t say that race itself the cause. More research is needed to understand the connections between racism, stress, and health problems.
While some studies and statistics mention race as a risk factor for these conditions, we can’t say that race itself the cause. More research is needed to understand the connections between racism, stress, and health problems.
Rates of Stillbirth
According to data from the CDC (2017), there are there are major differences in stillbirth rates among different groups. For Black people, the stillbirth rate is more than double the rate than other groups, except when compared with American Indian/Alaskan Native people. These are rates per 1,000 live births and stillbirths. See the data below:
- Non-Hispanic Black, 10.32
- American Indian/Alaska Native people, 7.22
- Hispanic, 5.01
- Non-Hispanic white, 4.89
- Asian or Pacific Islander, 4.29
Being a person of color is not a cause for having a stillbirth. However, communities of color are disproportionately affected by racism. Racism and unequal living conditions affect their health and well-being and puts them at higher risk of pregnancy complications, such as stillbirth.
March of Dimes recognizes that racism and its effects are factors in the health disparities in pregnancy outcomes and babies’ health. We must work together to bring fair, just and full access to health care for all moms and babies.
How do you know if your baby is stillborn?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
The most common symptom of stillbirth is when you stop feeling your baby moving and kicking. Others include cramps, pain or bleeding from the vagina. Call your health care provider right away or go to the emergency room if you have any of these conditions.
Your provider uses ultrasound to see if your baby’s heart has stopped beating. An ultrasound uses sound waves and a computer screen to show a picture of your baby in the womb.
What are your options for giving birth if your baby is stillborn?
If your baby is stillborn, your provider talks with you about options for giving birth. When and how you give birth depends on how far along you are in your pregnancy, your medical condition and what you think is best for you and your family. Some women need to give birth right away for medical reasons, but it’s often safe to wait until you go into labor on your own. Labor usually starts within 2 weeks after a baby dies in the womb.
When and how you give birth depends on how far along you are in your pregnancy, your medical condition and what you think is best for you and your family. Some women need to give birth right away for medical reasons, but it’s often safe to wait until you go into labor on your own. Labor usually starts within 2 weeks after a baby dies in the womb.
Your provider may recommend:
- Dilation and evacuation (also called D&E). During this surgical procedure, your provider dilates (opens) the cervix to remove tissue from the lining of the uterus. The cervix is the opening to the uterus (womb) that sits at the top of the vagina. Having a D&E may limit the information your provider can get about your baby’s condition. For example, if you have a D&E, your baby’s provider can’t do an autopsy on your baby.
- Inducing labor. This is when your provider gives you medicine or breaks your water (amniotic sac) to make your labor start. Most pregnant people with a stillbirth have their providers induce labor soon after they learn of their baby’s death.
 If you decide to wait to go into labor on your own and it doesn’t happen by 2 weeks after your baby’s death, your provider may induce labor to help prevent dangerous blood clots from developing.
If you decide to wait to go into labor on your own and it doesn’t happen by 2 weeks after your baby’s death, your provider may induce labor to help prevent dangerous blood clots from developing. - Cesarean birth (also called c-section). This is surgery in which your doctor makes a cut in your belly and uterus to deliver your baby.
What tests do you get after a stillbirth?
Your provider checks your baby, the placenta and the umbilical cord to try to find out why your baby died. The placenta grows in your uterus and supplies the baby with food and oxygen through the umbilical cord. Your provider may ask to do certain tests to try find out what caused the stillbirth. Tests may include:
- Amniocentesis (also called amnio). In this test, your provider takes some amniotic fluid from around your baby in the uterus. If your provider thinks a genetic condition or an infection in your baby may have caused the stillbirth, she may recommend an amnio before you give birth.
 Genetic conditions are health conditions that are passed from parents to children through genes.
Genetic conditions are health conditions that are passed from parents to children through genes. - Autopsy. This is a physical exam of your baby’s body after death. During an autopsy, a provider checks your baby’s organs for signs of birth defects or other conditions. This may help your provider find out what caused your baby’s death and if you may be at risk of having another stillbirth in the future. It’s common for a provider not to find a cause for stillbirth. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
- Genetic tests. Genetic tests to check for genetic conditions in your baby
- Tests for infections on your baby or on the placenta
In addition to checking your baby for medical and genetic conditions, your provider reviews your family health history and any problems or illnesses you had during pregnancy. Your family health history is a record of any health conditions you, your partner and members of both your families have had. Your provider may want to test you for infections, genetic conditions and other medical conditions, like lupus or thyroid problems.
Your family health history is a record of any health conditions you, your partner and members of both your families have had. Your provider may want to test you for infections, genetic conditions and other medical conditions, like lupus or thyroid problems.
Information from tests on you and your baby may help you if you’re thinking about getting pregnant again. Test results may help your provider find out if there’s a chance that you could have another stillbirth. Even if your provider doesn’t find out what caused your stillbirth, having the tests may help you better understand and cope with your baby’s death. If you have questions about the tests, including their cost, talk to your health care provider.
If you’ve had a stillbirth, can you have a healthy baby in another pregnancy?
Yes. For most women, the chances of having another stillbirth are very low. Less than 1 in 100 women (less than 1 percent) who’ve had a stillbirth go on to have another stillbirth.
If you had a stillbirth and are thinking about having another baby, give yourself time to heal physically and emotionally. Your provider may recommend that you have medical tests to try to find out more about what caused your stillbirth. You may need to wait until after you’ve had these tests to try to get pregnant again.
Your provider may recommend that you have medical tests to try to find out more about what caused your stillbirth. You may need to wait until after you’ve had these tests to try to get pregnant again.
If you had a stillbirth that was caused by a genetic condition, a genetic counselor can help you understand the condition and the chances of you having another stillbirth. A genetic counselor is a person who is trained to help you understand about how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby’s health. Your health care provider can help you find a genetic counselor.
Here’s what you can do help to lower your risk of having a stillbirth in another pregnancy:
- Get a preconception checkup. This is a medical checkup you get before pregnancy. It helps make sure you’re healthy when you get pregnant.
- Get treatment for any medical conditions you have.
- Get to a healthy weight before getting pregnant.
 Your provider can recommend ways to get to a weight that’s right for you.
Your provider can recommend ways to get to a weight that’s right for you. - Don’t smoke, drink alcohol, use marijuana or other drugs that can be harmful to your pregnancy. Tell your provider if you need help to quit.
- If you have any pain or bleeding from the vagina during pregnancy, call your provider right away.
If you get pregnant again, your provider monitors you and your baby closely. At around 32 weeks of pregnancy, she may ask you to do kick counts to help you keep track of how often your baby moves. Your provider also may do medical tests to check your baby’s heart rate and movements.
What causes stillbirth?
We don’t know what causes many stillbirths, but common causes include:
Infections in the mother or baby. Some infections may not cause signs or symptoms and may not be diagnosed until they cause serious complications, like premature birth or stillbirth. Infections that can cause stillbirth include:
- Cytomegalovirus (also called CMV).
 This is a kind of herpes virus that you can get by coming in contact with body fluid (like saliva, semen, mucus, urine or blood) from a person who carries the virus. It’s a common infection in young children, but if you get it during pregnancy, it can cause serious problems, like stillbirth.
This is a kind of herpes virus that you can get by coming in contact with body fluid (like saliva, semen, mucus, urine or blood) from a person who carries the virus. It’s a common infection in young children, but if you get it during pregnancy, it can cause serious problems, like stillbirth. - Fifth disease. This is a common childhood illness that’s caused by a virus called parvovirus B19. It usually spreads through the air from an infected person’s cough or sneeze.
- Genital and urinary tract infections. These infections affect the urinary tract and genitals (also called sex organs), like the vagina or ovaries. The urinary tract is the system of organs (like the kidneys and bladder) that helps your body get rid of waste and extra fluids. Getting infected with genital herpes for the first time during pregnancy can lead to stillbirth. Genital herpes is a sexually transmitted infection (also called STI) you can get from having sex with someone who’s infected.
- Listeriosis.
 This is a type of food poisoning.
This is a type of food poisoning. - Syphilis. This is an STI.
- Toxoplasmosis. This is an infection you can get from eating undercooked meat or touching cat poop.
Problems with the placenta or umbilical cord. Placental problems include infections, blood clots, inflammation (redness, pain and swelling), problems with blood vessels and other conditions, like placental abruption. Placental abruption is a serious condition in which the placenta separates from the wall of the uterus before birth. Placental problems cause about 24 in 100 stillbirths (24 percent). Problems with the umbilical cord include having a knot in the cord or the cord being pinched so that your baby doesn’t get enough oxygen. Problems with the umbilical cord may lead to about 10 in 100 stillbirths (10 percent).
Complications during pregnancy, including:
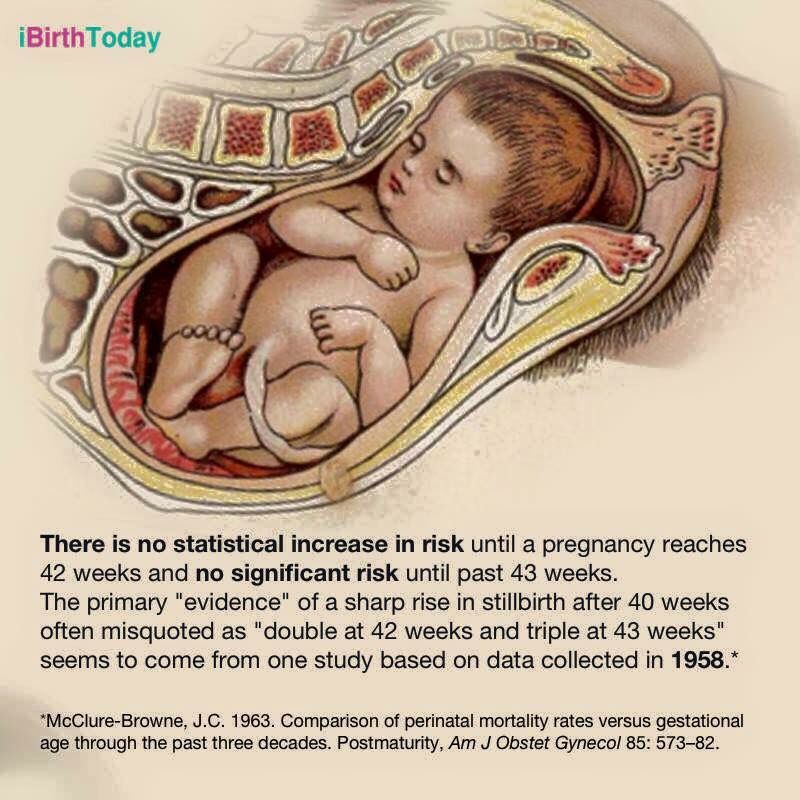
- Being pregnant longer than 42 weeks
- Diabetes, obesity, high blood pressure and preeclampsia
- Health conditions like lupus, thrombophilias and thyroid disorders.
 Lupus is an autoimmune disorder. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue just about anywhere in the body by mistake. Thyroid disorders affect your thyroid, a gland in your neck that makes hormones that help your body store and use energy from food. Thrombophilias increase your chances of making abnormal blood clots.
Lupus is an autoimmune disorder. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue just about anywhere in the body by mistake. Thyroid disorders affect your thyroid, a gland in your neck that makes hormones that help your body store and use energy from food. Thrombophilias increase your chances of making abnormal blood clots. - Preterm labor and preterm premature rupture of the membranes (also called PPROM). Preterm labor is labor that begins early, before 37 weeks of pregnancy. PPROM is when the sac around the baby breaks early, causing labor to start.
- Fetomaternal hemorrhage. This is when your baby’s blood mixes with your blood during pregnancy or birth.
- Trauma or injuries (like from a car accident)
Conditions in the baby, including:
- Birth defects and genetic conditions. About 14 in 100 stillborn babies (14 percent) have one or more birth defects, including genetic conditions like Down syndrome.

- Fetal growth restriction
- Not getting enough oxygen during labor and birth
- Rh disease. Rh factor is a protein on the surface of red blood cells. Rh disease happens when a woman who doesn’t have the protein (called Rh-negative) is pregnant with a baby who does have the protein (called Rh-positive). Rh disease can be prevented.
How can you deal with feelings of grief after a stillbirth?
Grief is all the feelings you have when someone close to you dies. Having a stillborn baby is a painful loss for a family. But there are things you can do to help you grieve, heal and remember your baby.
After birth, do what feels right for you and your family. You may want to spend time alone with your baby and other family members. You can name your baby, hold your baby, bathe and clothe her and take part in cultural or religious traditions, like baptism. Some families take pictures of their baby, make footprints or save locks of hair. You may be able to keep things from the hospital, like blankets, that were used with your baby. Keepsakes like these can help you and your family remember your baby.
Keepsakes like these can help you and your family remember your baby.
Parents who have a stillbirth need time to grieve. You and your partner may cope with grief in different ways, and you may need help dealing with others as you grieve.
After you leave the hospital, certain things, like hearing names you were thinking of for your baby, seeing the baby’s nursery at home or having your breast milk come in can be painful reminders of your loss. You may need help learning how to deal with these situations and the feelings they create. Ask your health care provider to help you find a grief counselor to help you cope with your baby’s death. Or your hospital may have a loss and grief program for families. Getting counseling can be really helpful to you and your family.
Talking about your feelings with other parents who have had a stillbirth may help you deal with your grief. Visit shareyourstory.org, the March of Dimes online community where families who have lost a baby can talk to and support each other.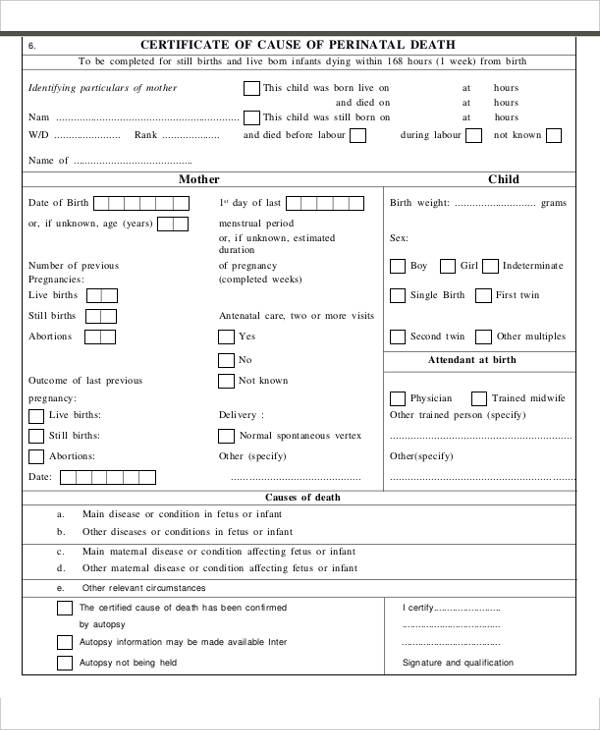 Sharing your story may ease your pain and help you heal.
Sharing your story may ease your pain and help you heal.
Having a stillbirth may make you at risk for postpartum depression (also called PPD). PPD is a kind of depression that some women get after having a baby. Tell your provider if you have signs or symptoms of PPD, like feeling depressed most of the day every day, having little interest in things you normally like to do, or having trouble eating or sleeping.
More information
- From hurt to healing (free booklet from the March of Dimes for grieving parents)
- Share Your Story (March of Dimes online community for families to share experiences with prematurity, birth defects or loss)
- Centering Corporation (grief information and resources)
- Compassionate Friends (support for families after the death of a child)
- First Candle (support for families with children who died of SIDS or preventable stillbirth)
- International Stillbirth Alliance
- Journey Program of Seattle Children’s Hospital (support for families after the death of a child)
- Now I Lay Me Down to Sleep (remembrance photography)
- Perinatal Hospice & Palliative Care (resources for parents who find out during pregnancy that their baby has a life-limiting condition
- Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
- Star Legacy Foundation (support for families who have had a stillbirth)
Last reviewed: October, 2020
“A baby died in my stomach”
In February 2019, Canadian resident Allison Harley-Queen gave birth to twins Gwen and Clara. They were born at the 25th week of pregnancy already dead - the sisters had intrauterine circulatory disorders. The fact that her girls had died, Allison found out before the birth and planned a farewell in advance.
They were born at the 25th week of pregnancy already dead - the sisters had intrauterine circulatory disorders. The fact that her girls had died, Allison found out before the birth and planned a farewell in advance.
She went to the hospital with her husband and a photographer friend. Pictures of babies and a touching story titled “A stillbirth is still a birth” was published on social networks and collected more than 8 thousand comments of support. “I’m sorry for your loss!”, “I pray for you”, “You are so brave that you share this experience with the world” - these are just a few of the thousands and thousands of replies from users.
Under the post of Muscovite Yana Yatskovskaya, who lost her son Alexander in the fall of 2018 at the 27th week of pregnancy due to a true knot in the umbilical cord, a scandal erupted. The story got into the press with the headlines “The model posted a photo with a dead child on the network,” and some of Yana’s followers wrote: “Why publish such pictures? It's disgusting!" As a result, Yatskovskaya simply closed the comments in her account.
We are talking to doctors, psychologists and representatives of charitable foundations that work with perinatal loss about why the conversation about the death of a baby is so painful in Russia.
How to cope with the death of a child?
"Doctors don't like to talk about it"
Stillbirth is not uncommon. WHO gives statistics: up to 3.2 million annually around the world. In Russia, the statistics are not obvious, since in our country all deaths of a child under the age of one are considered infant mortality. However, there is data for 2010, when more than 8,000 episodes of intrauterine death of a child were recorded at terms of 20 weeks of pregnancy.
When I was looking for a doctor willing to comment on this topic, I came across refusals or silence. “Why are you digging into medical details? Women don’t need to know how a dead baby is born,” an experienced obstetrician-gynecologist, an employee of one of Moscow’s private clinics, told me.
“Nobody likes to talk about this topic. And no one likes to take such births either. This is a closed topic, ”anonymous confession of the deputy chief physician of one of the major metropolitan maternity hospitals.
Quite a whisper and with a request “just not for print!” doctors said: it's all about the statistics. No one wants to see infant mortality rates rise in the maternity hospital - they spoil the reputation and can cost the hospital a reduction in funding, and the head doctor's job.
“Our society still treats a pregnant woman as a kind of vessel that should give out the contents. And if the “product” turns out to be of inadequate quality, they look at her as if she were plagued. There is an order for healthy, pink, successful children. Everything else should be forgotten,” says the doctor of the Center for Traditional Obstetrics and Family Medicine Veronika Nazarova.
“It is better for such women in labor not to meet mothers of healthy children”
At the moment, childbirth with intrauterine death of the fetus takes place strictly in those maternity hospitals that have the so-called 2nd obstetric department, or observation. This is a kind of “maternity hospital in a maternity hospital” with stricter sanitary rules, regular disinfection, wards for one, maximum two people. Usually, women in labor come here with various kinds of infections - from the commonplace SARS to HIV. Give birth in separate boxes.
This is a kind of “maternity hospital in a maternity hospital” with stricter sanitary rules, regular disinfection, wards for one, maximum two people. Usually, women in labor come here with various kinds of infections - from the commonplace SARS to HIV. Give birth in separate boxes.
“This happens for only one reason - that women in labor have the opportunity not to meet other women who have given birth to healthy children. This is for their own peace of mind,” explains Roman Getmanov , an obstetrician-gynecologist at the Moscow City Clinical Hospital No. 70.
Childbirth with a dead baby is still childbirth. Protocols in the vast majority of situations forbid a caesarean section, because there is a risk of blood poisoning. On condition of anonymity, an obstetrician-gynecologist of one of the private clinics in Moscow explains that in such a situation, doctors are constantly waiting for complications, they are afraid of sepsis, so they usually stimulate the patient without waiting for the birth to begin on their own.
Russian doctors prefer to act quickly when they learn that a baby is dead in the womb, she says. So, if the diagnosis is established in the antenatal clinic during an ultrasound scan, an ambulance is called, the woman is taken to the hospital and given an emergency delivery, most likely with anesthesia.
In foreign practice, on the contrary, expectant tactics are possible - of course, if the pregnant woman has no complications, for example, bleeding, and with the control of blood tests, pressure, heart rate. For example, a Canadian study cites the following figures: more than three-quarters of women give birth spontaneously within two weeks after the death of the fetus, most of the rest within four weeks of the death of the child. At the same time, the earlier during pregnancy the child died in the womb, the later childbirth can begin, and the more mature the fetus, the less time it will take for the body to reject it.
“It's not about sepsis, it's about fear”
So far, waiting tactics are hardly possible in Russia, for a number of reasons.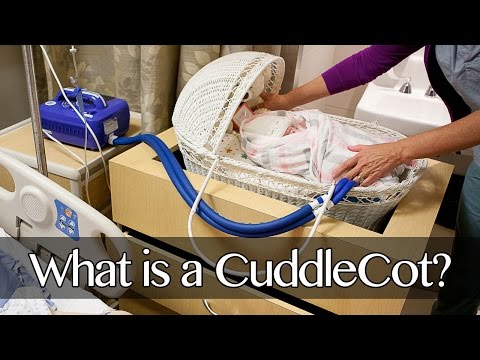
“The difficult situation is not around the problem of blood poisoning - after all, in obstetric practice there is an approach when one of the twins dies, and the pregnancy is kept in order to bring the second child. Sepsis does not start immediately. But such a speed of delivery, which we often observe in Russia, is associated more with psychological reasons than with medical ones,” says the coordinator of the perinatal program of the Children’s Hospice “House with a lighthouse” Ksenia Popova, former obstetrician-gynecologist.
According to her, the whole point is the desire of doctors to protect the woman, and themselves too, from worries. “Midwives are those who welcome life. And suddenly, death. How to meet a dead child, how to help? Almost no one here knows about it."
“Well, who wants to do this when a person works in a maternity hospital, accepts living children? And suddenly a child who died in utero. We are all living people, everyone understands that this is a misfortune,” Roman Getmanov confirms her opinion.
“In residency, I happened to attend such births,” recalls Ksenia Popova. – I really sympathized with this mother, I wanted to come to her room and console her. But I did not know how to do it - we were not taught this at the institute. I was afraid and she was afraid too. We both did not know how to talk about it, and preferred to remain silent.
Sometimes a woman herself demands that everything be left behind as soon as possible, and doctors are accustomed to this course of events, they willingly meet the wishes of the patient.
“Mothers think that if the child is dead, nothing can be done. In fact, a lot can be done. Look at the child or touch him, say something, mourn, give a name, bury. Mom needs to find a way to survive this grief, how to say goodbye to the child, how to remember him and pray,” says Ksenia Popova.
“You have time to wait and think about everything”
Foreign practice regarding stillbirth is different. Mom has time: to comprehend what happened, talk with her loved ones, find support and prepare for a sad but important event in her life. Yes, at least - take clothes for the baby with you to the hospital, solve the issue of photography, if necessary, and take into account many more important, in her opinion, little things.
Mom has time: to comprehend what happened, talk with her loved ones, find support and prepare for a sad but important event in her life. Yes, at least - take clothes for the baby with you to the hospital, solve the issue of photography, if necessary, and take into account many more important, in her opinion, little things.
There are quite a few articles on stillbirth in English on the Internet. All these are quite user-friendly materials that describe in detail and calmly what awaits the mother in the maternity hospital, how the birth will go, and how to organize a farewell later. They discuss the possibility of using epidural anesthesia, describe the pros and cons of different ways to stimulate labor. The obligatory advice is to take an accompanying person with you to the birth: a husband, mother, girlfriend or doula, so as not to be left alone.
Books for pregnant women include such information in a special section. “In one of the Australian publications that I came across, there is a chapter on what to do if the child died, in utero or during childbirth. The author warns readers: “I understand that you are now preparing to become happy parents. You do not need to read this chapter in advance. Just know that it is in the book, and you can get information if something goes wrong,” says Veronika Nazarova.
The author warns readers: “I understand that you are now preparing to become happy parents. You do not need to read this chapter in advance. Just know that it is in the book, and you can get information if something goes wrong,” says Veronika Nazarova.
The death of a child: how to talk about the worst
If you want to say goodbye, get ready to defend this right
“I teach childbirth preparation courses, and there I also communicate with women with such a sad experience. From their cautious reservations, you can roughly guess what they have to go through. It happens that there is rudeness, especially on the part of middle and junior medical personnel, - says Elizaveta Novoselova, obstetrician-gynecologist, perinatal psychologist, author and teacher of the educational project "School for Parents".
– The very moment of childbirth is perceived as unnatural, because you are giving birth, but in fact there is no one to give birth. And you are still reminded of this, not embarrassed in expressions.
And you are still reminded of this, not embarrassed in expressions.
The situation can definitely be corrected by the presence of an escort - a husband, mother or someone else you trust. At one time, I was present at such births in this capacity, and I can say that the attitude towards the woman in labor was excellent: everyone felt sorry for her, sympathized and communicated with her extremely politely. But who knows what it would be like if she were alone?
Lawyer and human rights activist Ruslan Trofimov informs that much of what could protect women in such a difficult situation is already written into the law. You just need to know your rights.
So, in the law "On the protection of the health of citizens in the Russian Federation" there is Article 6, which speaks of respecting the priority of the patient. This means that the interests of the woman (and not doctors) are at the forefront, and not only the issues of her health and life, but also the observance of cultural and religious traditions. In other words, in the case of a stillborn child, the mother has the right to say goodbye to him and observe all the rituals that she considers necessary.
In other words, in the case of a stillborn child, the mother has the right to say goodbye to him and observe all the rituals that she considers necessary.
The law regulates the creation of comfortable conditions for the patient. On the basis of it, one can demand that a woman in labor who has experienced the loss of a child be placed separately from other mothers and their babies, allowed visits from relatives who could provide her with moral support.
Part 2 of article 51 of the federal law says that the child's father may be present at the birth. It does not specify which child will appear in such childbirth - living or dead.
“Look at him anyway”
Often the main question for a woman giving birth to a baby who died in the womb is the dilemma: is it worth looking at?
According to Alexandra Feshina, director of the Light in Hands Charitable Foundation , there is no single correct answer to this question.
“We have parent support groups after a loss, and we've noticed this. Parents who did not see their baby, did not look at him, most often regret it. But there are situations when for women who saw the baby, it became a severe injury, mainly because of the appearance. The best thing to do in this case is to listen to yourself.”
Parents who did not see their baby, did not look at him, most often regret it. But there are situations when for women who saw the baby, it became a severe injury, mainly because of the appearance. The best thing to do in this case is to listen to yourself.”
Obstetrician-gynecologist Roman Getmanov , on the contrary, I am sure that it is not worth looking at a dead child. “I have been in the profession for 35 years, and I can hardly look at it. If the child died a few days ago, it's decomposed flesh. What is there to show mothers? On the contrary, we try to take it away as quickly as possible, otherwise she will later associate it with children.”
According to the coordinator of perinatal programs of the Children's Hospice "House with a lighthouse" Ksenia Popova , fencing off the problem, we do not solve it.
“It seems to doctors that by their silence, by the fact that they take away and immediately take away the child without showing it, they protect the mother from worries, help her “start living on” as soon as possible. But because of this silence, mother with her grief and horror is left all alone. The memory remains haste, averted glances, silence, as if something shameful had happened.
But because of this silence, mother with her grief and horror is left all alone. The memory remains haste, averted glances, silence, as if something shameful had happened.
It is difficult to say in advance in what form her dead baby will appear before her mother. It depends on many different factors - how long ago the child died, what was the cause of his death, how the birth went, and so on. But Ksenia is sure: the mother should have the opportunity to think about whether she wants to say goodbye to the child, and if so, how.
“It is important to discuss this with your mother before giving birth. She may not see the whole baby, but only the arm or leg, while the body is covered with a sheet. In foreign practice, it happens that the midwife describes to the mother what the child looks like, and then the mother decides whether she wants to see him or not. You may not look, but touch, stroke through the fabric of the diaper. In our country, it is not sometimes offered to take the body of a child and bury it, although the family has the right to do so. Everyone tries to pretend that there was no child. But for my mother, he was and always will be.
Everyone tries to pretend that there was no child. But for my mother, he was and always will be.
In foreign practice, there are options that can be used even in extremely ambiguous situations and have a therapeutic effect. “In Britain, a midwife Sally Kelly practices, which fundamentally deals only with complex cases - the birth of non-viable children, babies with severe pathologies and intrauterine death. Even if the mother does not have the opportunity to show the body of the child for aesthetic reasons, Sally Kelly takes a photograph for her as a souvenir - for example, a tiny hand hugs a teddy bear, ”says Veronika Nazarova.
“Maternity hospitals are not ready to give such mothers boxes of memory”
“Last year we tried to launch the “Box of Memory” project,” says Alexandra Feshina. - She could become in Moscow an alternative to a gift box from the mayor, which women in labor receive.
The idea is not new, it is widely practiced in the West. Usually two soft toys are placed in such boxes - one is buried with a child, the second is left as a keepsake. Carbon paper or special clay to make a cast or imprint of a hand and foot. Photo frame. A postcard on which a mother can write words of love to a child. A small blanket that covers the baby when they are buried.
Usually two soft toys are placed in such boxes - one is buried with a child, the second is left as a keepsake. Carbon paper or special clay to make a cast or imprint of a hand and foot. Photo frame. A postcard on which a mother can write words of love to a child. A small blanket that covers the baby when they are buried.
Unfortunately, we have not yet found the chief physicians who are ready to take part and support the distribution of such boxes to mothers. Today, maternity hospitals give out brochures developed by our foundation with information for mothers and their loved ones who are experiencing loss. Thank you anyway. Not so long ago, it didn't even exist."
There are also difficulties with the farewell ceremony. It happens that heartbroken parents do not even have time to realize what they really want, how they plan to spend their child, and no one simply provides them with information and possible options.
“There should be an opportunity to say goodbye to a dead child and bury him, because this is an important part of living and experiencing grief and loss,” explains Natalia Perevoznyuk, a psychologist at the House with a Lighthouse Children's Hospice .
- Alas, avoiding feelings and grief is one of the communication strategies with parents adopted in Russian society. Meanwhile, the woman and her family are alarmed by the "suddenness" of the stillbirth, they are in shock and cannot immediately "figure out" what they would like or what else they could do for their dead child.
If parents initially refuse to take and bury the child, they should be able to do so later. Simply because the importance of preserving the memory of a dead child becomes clear to most mothers at a later stage of mourning.
“We have cases when parents managed to get the ashes of their child more than six months after death and still buried him,” says Alexandra Feshina . For them it was important.
Illustrations: Oksana Romanova
Toxoplasmosis – Family Doctor clinic.
Pregnancy is an important period in the life of every woman. And, of course, it is very important to properly prepare for the bearing and birth of a healthy baby. During pregnancy, many factors can affect the development of the fetus and the health of the woman. Infections are among the most common causes that can cause pregnancy complications. There is a whole complex of infectious diseases that negatively affect the fetus (TORCH-complex). One such infection is toxoplasmosis.
During pregnancy, many factors can affect the development of the fetus and the health of the woman. Infections are among the most common causes that can cause pregnancy complications. There is a whole complex of infectious diseases that negatively affect the fetus (TORCH-complex). One such infection is toxoplasmosis.
Toxoplasmosis is a fairly common parasitic disease caused by protozoa (Toxoplasmagondii). Reproduction of Toxoplasma occurs in the body of cats. At the end of the reproduction cycle, oocysts are formed, which enter the soil with faeces and can remain there for up to 2 years. In the future, getting into the body of other animals or humans, they cause their infection.
There are two main ways that humans can become infected with toxoplasmosis:
1. Alimentary: consumption of undercooked meat, dirty hands, consumption of contaminated vegetables and berries;
2. Contact: direct contact with sick animals, often found in veterinarians and meat-packing workers (in the presence of microdamages on the surface of the skin and mucous membranes).
Toxoplasmosis is very dangerous for pregnant women. Depending on the time of infection, it can cause early termination of pregnancy, stillbirth, and the birth of children with severe malformations. The main symptoms of the disease are: headache, fever, lethargy, muscle pain, swollen lymph nodes, inflammatory changes in the general blood test. These signs are also found in influenza and many viral infections, so a person is not always aware of the illness.
In the diagnosis of toxoplasmosis, an important role is played by the detection of antibodies in the venous blood: immunoglobulins M and G . By their titers (that is, the number), as well as by avidity (an indicator of the strength of the bond between antibodies and the pathogen), it is possible to determine the stage of the disease and the approximate time of infection. These studies are included in the mandatory program for the examination of pregnant women and, by order of the Ministry of Health, are carried out when registering and before taking maternity leave. When planning a pregnancy, it is also necessary to be examined for the presence of antibodies to toxoplasmosis, since a woman's primary contact with the infection during pregnancy and 6 weeks before conception can lead to the birth of a child with congenital toxoplasmosis. With repeated pregnancies, the transmission of toxoplasmosis to the fetus does not occur.
When planning a pregnancy, it is also necessary to be examined for the presence of antibodies to toxoplasmosis, since a woman's primary contact with the infection during pregnancy and 6 weeks before conception can lead to the birth of a child with congenital toxoplasmosis. With repeated pregnancies, the transmission of toxoplasmosis to the fetus does not occur.
The most severe lesions of the fetus are detected during infection in the first trimester of pregnancy. Signs of congenital toxoplasmosis in the fetus can be detected by ultrasound (usually at the second screening study at 18-20 weeks). These include: microcephaly, hydrocephalus, detection of calcifications in the fetal brain tissue, enlargement of the liver and spleen, accumulation of fluid in the abdominal and pleural cavities).
Treatment of patients with signs of toxoplasmosis is selected individually, according to examination data and depending on the clinical picture and the duration of pregnancy. In case of detection of gross defects in the fetus, the question of termination of pregnancy is raised.