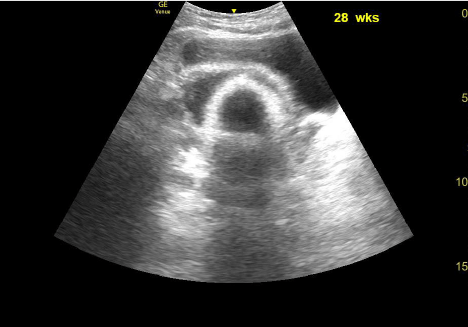
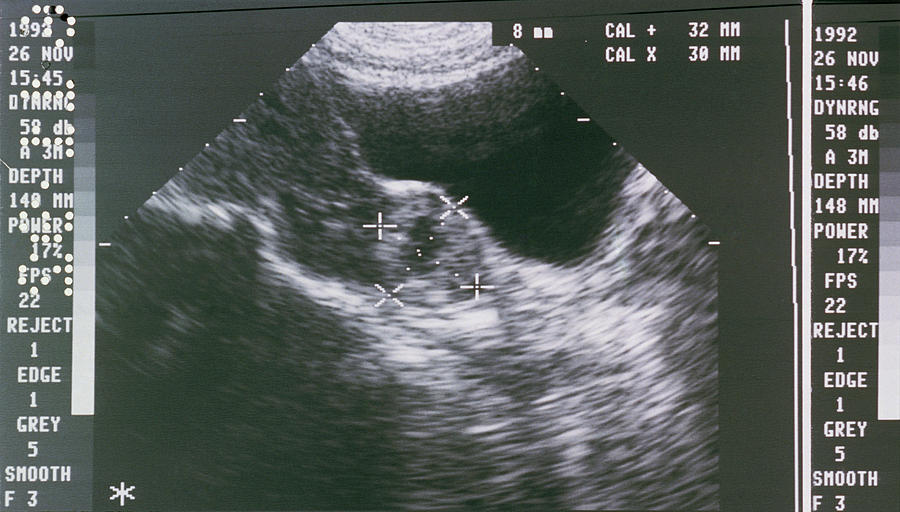
10 weeks transabdominal ultrasound
10 Week Ultrasound: Procedure, Abnormalities and More
At FirstCry Parenting, our aim is to give you the most elevant, accurate and up to date information.
Every article that we publish, confirms to stringent guidelines & involves several levels of reviews, both from our Editorial team & Experts. We welcome your suggestions in making this platform more useful for all our users. Write in to us at [email protected]
- Why Should You Have an Ultrasound at 10 Weeks?
- How to Prepare for Your 10th Week Pregnancy Scan
- How Long Does It Take to Perform an Ultrasound Scan?
- How Is an Ultrasound Scan Performed?
- What Will You See on the Scan at the Tenth Week of Your Pregnancy?
- No Movement at the 10th-week Ultrasound – Is this Normal?
- What If Some Abnormalities Are Discovered in the Scan?
Last Updated on
If you are reading this, we take it that you are 10 weeks pregnant. Congratulations! Now that you are 10 weeks pregnant, you can stop worrying when you’ll start looking pregnant because you have reached that phase where your pregnancy bump will start showing. Your doctor may suggest an ultrasound scan around this time to make sure that your baby is healthy and is developing normally. An ultrasound, also called a sonogram, will help create a picture of your baby on a monitor with the help of sound waves. Read on to know why you need an ultrasound scan at 10 weeks of your pregnancy and how it is performed.
Why Should You Have an Ultrasound at 10 Weeks?
Following are the reasons for performing an ultrasound scan at 10 weeks of pregnancy.
1. To check the baby’s growth.
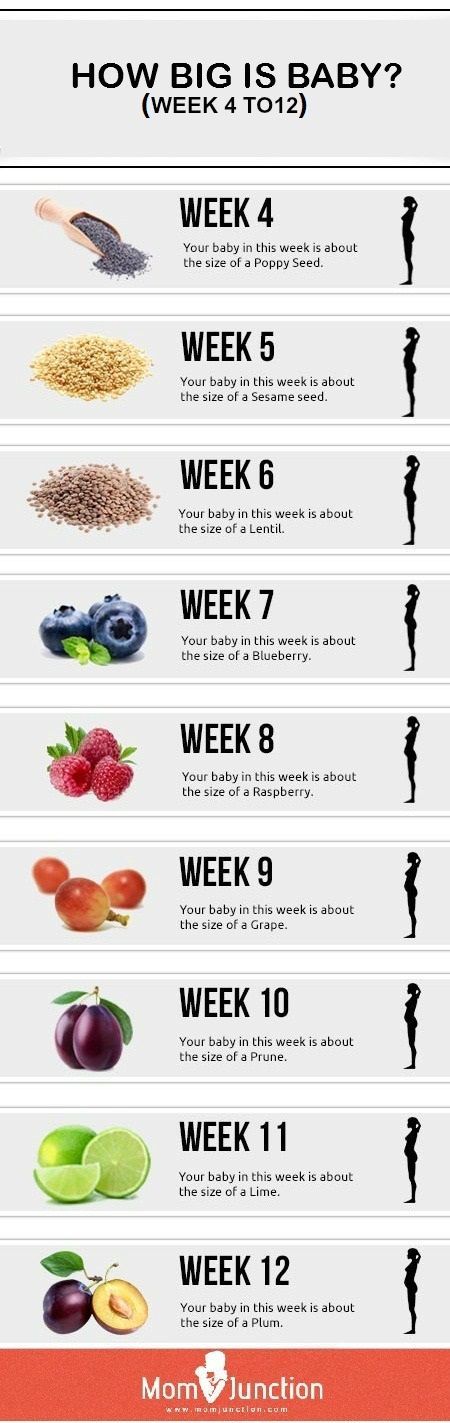
Your doctor may suggest an ultrasound scan at 10 weeks of your pregnancy to check the progress or growth of your baby. By conducting a scan, she will be able to identify whether or not your baby is developing normally. At 10 weeks of pregnancy, the foetus weighs about 4gm and measures around 3.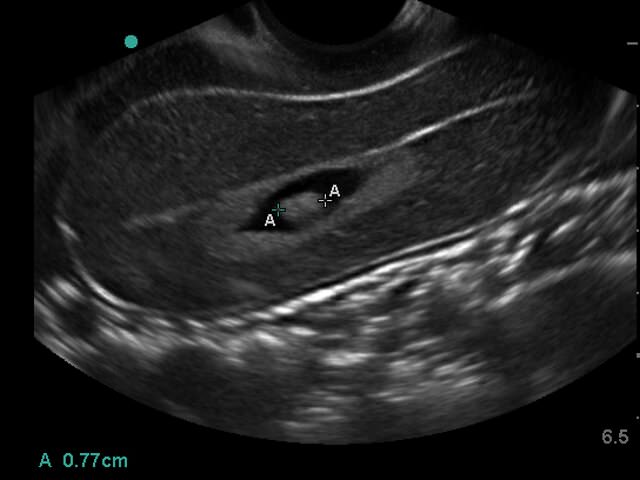 1cm from crown to rump. An ultrasound will make it clear how your baby is developing. She will also calculate the baby’s gestational age based on these measurements and predict a due date.
1cm from crown to rump. An ultrasound will make it clear how your baby is developing. She will also calculate the baby’s gestational age based on these measurements and predict a due date.
2. To check for any abnormalities.
Between 10 and 14 weeks of your pregnancy, nuchal translucency scan (NTS) will be performed to test the foetus for the risk of Down syndrome and other chromosomal abnormalities. In this, the unborn baby’s nuchal fold, which is the transparent back of the neck, will be measured to test for any abnormalities. This test is usually conducted in the 12th week of pregnancy.
3. To hear the baby’s heartbeat.
You must have heard your baby’s heartbeat through an ultrasound scan at around 8 weeks of your pregnancy itself. But you can hear it during the 10th week as well. Your doctor will perform this test to ensure that your baby’s heart functions normally.
4. To ensure that the baby’s organs are functioning normally.

In the 10th week of pregnancy, the skin of the foetus is translucent. This means that all the internal organs will be visible on the ultrasound scan. Thus your doctor will be able to gauge whether all the organs are developing normally and functioning properly or not.
5. To see how the spine is developing.
The spine should be visible by the 10th week of pregnancy. The doctor will conduct an ultrasound to check if the spine is developing normally.
6. To determine the position of the baby.
If this is your first ultrasound, then the doctor will tell you about the location of the pregnancy, i.e., the position of your baby. An ultrasound will help rule out an ectopic pregnancy.
How to Prepare for Your 10th Week Pregnancy Scan
To prepare for your 10-week ultrasound scan, you will need to have a full bladder. Going for the scan with a full bladder will help the ultrasound technician to get a clear image of the baby, the placenta, uterus, ovaries, and cervix. You will need to drink 3 glasses of water an hour before you have the ultrasound so that your bladder is full.
You will need to drink 3 glasses of water an hour before you have the ultrasound so that your bladder is full.
How Long Does It Take to Perform an Ultrasound Scan?
A typical ultrasound scan can take between 15 to 30 minutes to perform. The sonographer has to get a good image of the baby and also examine your uterus, placenta, and ovaries. If the baby is very active and moves around or is in an awkward position, the sonographer might take longer to capture clear images. And if clear images are not obtained, the scan may have to be rescheduled for some other time.
How Is an Ultrasound Scan Performed?
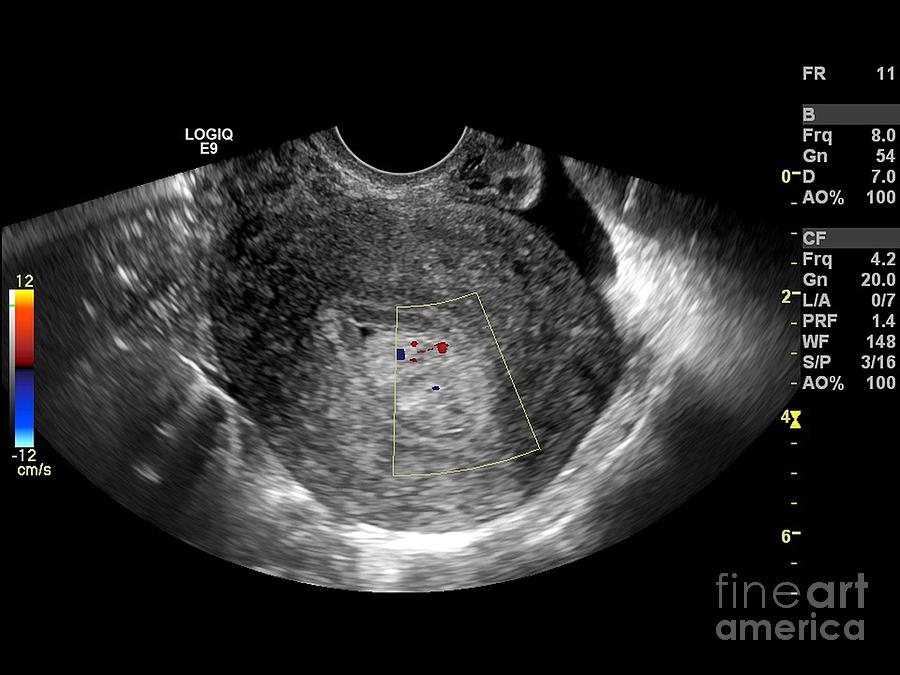
In order to perform an ultrasound, the sonographer will ask you to lie down on the examination table and expose your belly and abdomen. She will then apply some gel over your belly and press a wand called a transducer on the skin. This wand will send ultrasound waves that will form an image of your baby on the monitor. The technician will apply some pressure on your belly with the wand to get a clear view of the baby.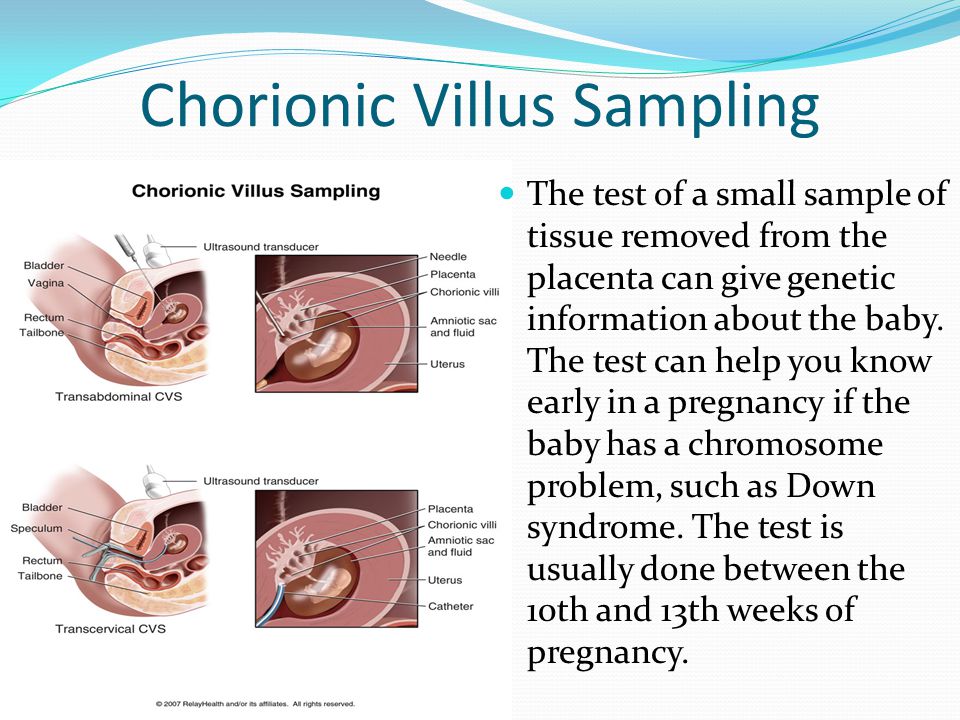 The scan is not painful and is non-invasive. In some cases, the scan may be done vaginally if the abdominal scan fails to produce clear images. But you don’t have to worry – the vaginal probe is also not painful.
The scan is not painful and is non-invasive. In some cases, the scan may be done vaginally if the abdominal scan fails to produce clear images. But you don’t have to worry – the vaginal probe is also not painful.
What Will You See on the Scan at the Tenth Week of Your Pregnancy?
Here is what you can expect to see in your 10-week ultrasound scan.
- You might see your baby moving at the 10-week ultrasound. You can also expect to see your baby’s hands, feet, and head clearly.
- As your little one’s skin will be transparent, you may also see the internal organs.
- On the monitor, you will also see your baby’s heart beating and you will be able to hear it too.
- You might see your baby’s forehead bulged. It is usually bulged to accommodate the growing brain. However, the forehead will flatten gradually.
- You might also see your baby’s fingers and toes. You can also expect to see his nose and ears. You will see your baby’s eyelids but they will be closed.

- Baby’s skeleton is complete, and the framework of the spine can be seen.
No Movement at the 10th-week Ultrasound – Is this Normal?
If you do not see your baby moving at the 10th-week of your ultrasound, don’t worry. Chances are your little one might be sleeping in the womb. As long as your sonographer assures you that the baby’s growth, development, and heartbeat are normal, you need not worry.
What If Some Abnormalities Are Discovered in the Scan?
If any abnormalities are spotted in the 10-week ultrasound pictures, your sonographer or doctor will inform you about it. In such cases, the doctor may recommend further testing such as Chorionic Villi Sampling, blood tests, and amniocentesis to be certain. Based on the findings, the doctor will speak to you about the further course of action to be taken and may even refer you to a specialist.
The 10-week ultrasound scan is also called a dating scan, as it is used to determine the gestational age of the baby and predict the due date. The nuchal translucency test is part of this scan. Some parents may choose to get a printed picture of the scan to preserve as a memento. In some countries, the technician may be able to determine the gender of the baby. However, sex determination is illegal in India. The 10-week ultrasound is done to ensure that the foetal development is normal and the baby is healthy. So don’t miss this ultrasound if your doctor has suggested it. Go for regular tests and have a healthy pregnancy!
The nuchal translucency test is part of this scan. Some parents may choose to get a printed picture of the scan to preserve as a memento. In some countries, the technician may be able to determine the gender of the baby. However, sex determination is illegal in India. The 10-week ultrasound is done to ensure that the foetal development is normal and the baby is healthy. So don’t miss this ultrasound if your doctor has suggested it. Go for regular tests and have a healthy pregnancy!
Previous Week: 9 Weeks Pregnant Ultrasound
Next Week: 11 Weeks Pregnant Ultrasound
ADVERTISEMENT
POPULAR POSTS
ADVERTISEMENT
LATEST
What Do Breastfeeding Moms Really Want?
Ruchelle Fernandes -
Hands up if you thought breastfeeding would be easy – but then struggled! To mark World Breastfeeding Week in August this year, Australian breastfeeding. ..
..
Pregnancy Ultrasound Evaluation - StatPearls
Continuing Education Activity
The use of ultrasound in pregnancy is vast and has become the standard of care during pregnancy. This activity describes different applications of ultrasound in the setting of pregnancy, focusing on the importance of recognizing critical findings in the acute and routine settings along with the associated management strategies. In addition, the role of the interprofessional healthcare team involved in the intricate management of the pregnant patient is discussed.
Objectives:
Identify the indications and contraindications of ultrasound in pregnancy.
Describe the equipment and technique in regards to ultrasound in pregnancy.
Summarize different uses of ultrasound in pregnancy in routine versus emergent settings.
Explain the importance of improving care coordination amongst the interprofessional team to enhance the delivery of care for pregnant patients.

Access free multiple choice questions on this topic.
Introduction
The use of ultrasound in the setting of pregnancy is vast and has become the standard of care in the evaluation of pregnant women. The average number of ultrasounds performed during pregnancy has increased from 1.5 in 1995 to 1997 to 2.7 in 2005 to 2006, with even higher numbers of ultrasound studies obtained for high-risk pregnancies.[1] The use of ultrasound during pregnancy is growing and is utilized in both routine monitoring as well as in an acute setting of trauma or pregnancy complications.
Anatomy and Physiology
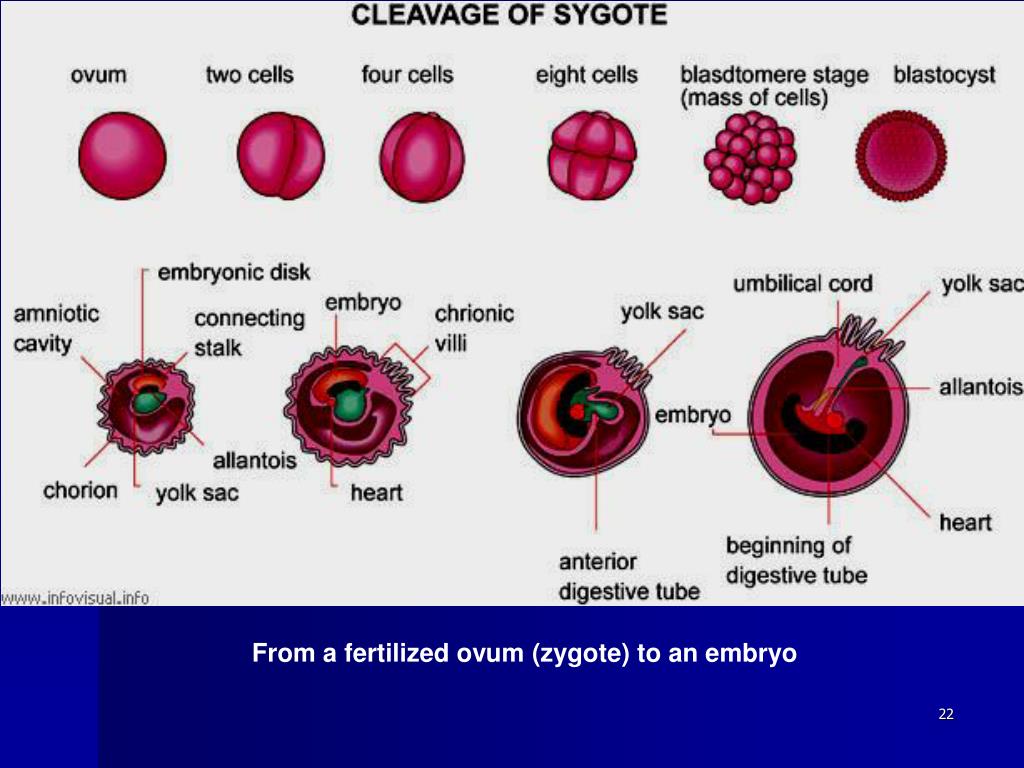
Ultrasound can be used transvaginally or transabdominally to view the female reproductive anatomy, with a transvaginal approach allowing for better visualization of structures. The uterus is located posterior to the bladder and anterior to the colon. The three parts of the uterus can be visualized with the use of transvaginal ultrasound, beginning most caudal: cervix, body, and then the fundus.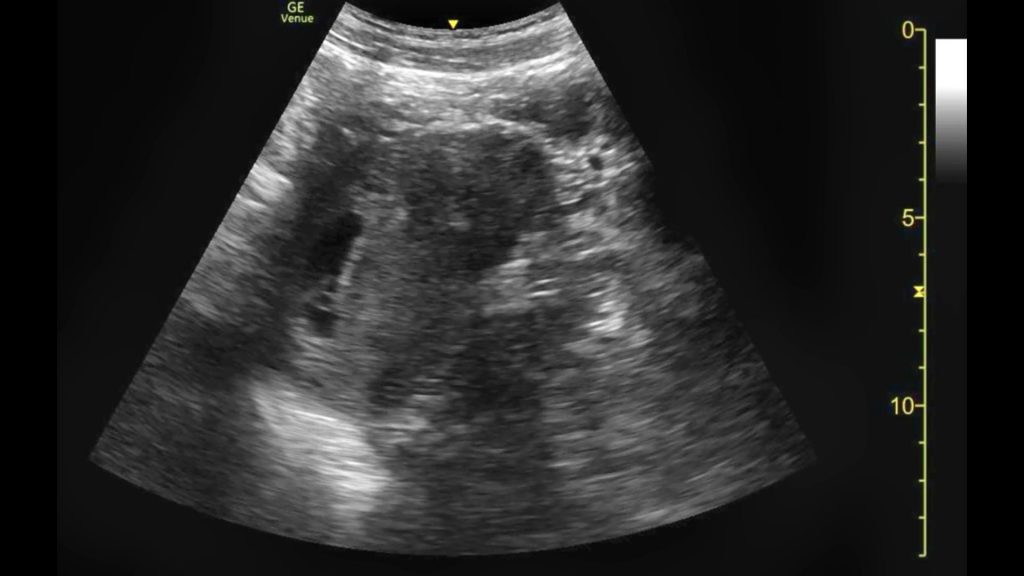 The uterus contains the gestational sac during pregnancy which is typically visualized in the center of the uterine body at 4.5 to 5 weeks of gestation and is the first structure visualized in pregnancy.[2][3] The ovaries and Fallopian tubes are paired female reproductive organs that can be found lateral to the uterus. The fetal heartbeat becomes detectable at 6 weeks of gestational age and is described initially as a “flickering” structure. The placenta is visible by 10 weeks gestational age with a transabdominal ultrasound. It appears as a uniformly echogenic structure with rounded margins, usually located along the anterior or posterior uterine wall, where it is seen as a thickened echogenic rim of tissue surrounding the gestational sac.[4]
The uterus contains the gestational sac during pregnancy which is typically visualized in the center of the uterine body at 4.5 to 5 weeks of gestation and is the first structure visualized in pregnancy.[2][3] The ovaries and Fallopian tubes are paired female reproductive organs that can be found lateral to the uterus. The fetal heartbeat becomes detectable at 6 weeks of gestational age and is described initially as a “flickering” structure. The placenta is visible by 10 weeks gestational age with a transabdominal ultrasound. It appears as a uniformly echogenic structure with rounded margins, usually located along the anterior or posterior uterine wall, where it is seen as a thickened echogenic rim of tissue surrounding the gestational sac.[4]
Indications
If there are no concerning symptoms in pregnancy, a routine ultrasound should be performed at 10 to 13 weeks gestational age to establish accurate gestational age, determine viability, and determine the number of fetuses [5].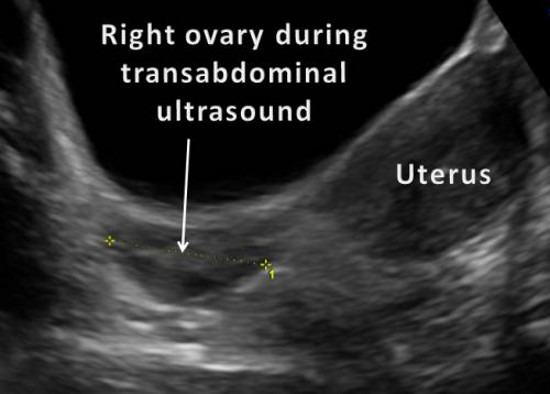 However, in the presence of concerning symptoms such as vaginal bleeding, abdominal or pelvic pain in a female with a positive pregnancy test, an emergent pelvic ultrasound must be performed to rule out an ectopic pregnancy.
However, in the presence of concerning symptoms such as vaginal bleeding, abdominal or pelvic pain in a female with a positive pregnancy test, an emergent pelvic ultrasound must be performed to rule out an ectopic pregnancy.
In the setting where a female of reproductive age presents with minor or major trauma, pregnancy is automatically assumed until it is ruled out with serum or urine pregnancy tests. [6] During the FAST (Focused Assessment with Sonography in Trauma) exam, a transabdominal ultrasound is performed to assess for free fluid in the abdomen and to investigate the potential presence of intrauterine pregnancy (IUP). If IUP is identified, further assessment should include fetal heart rate, the amount of amniotic fluid, fetal movement, and the placenta. In cases of traumatic injury in females with confirmed or estimated pregnancy greater than 20 weeks gestation, OBGYN expert consultation should be sought as soon as possible, and a transabdominal ultrasound must be performed to evaluate fetal well-being as soon as the mother is stabilized.
Contraindications
While the only absolute contraindication to transabdominal and transvaginal ultrasound is patient refusal, the use of transvaginal ultrasound may be relatively contraindicated late into pregnancy term or in the high-risk patient population.[7] Special consideration should be made in the acute setting with a pregnant patient with vaginal bleeding and an unknown past medical history. In this case, a transabdominal ultrasound should be performed first to evaluate the placenta, followed by transvaginal ultrasound and speculum examination if it is deemed safe. However, transvaginal ultrasound is relatively safe in the setting of placenta previa as the angle between the cervix and the vaginal probe is adequate to prevent the probe from slipping into the cervix and disrupting the placenta.[8]
Equipment
The equipment needed to perform a 2-D prenatal ultrasound includes two ultrasound probes. A High-frequency transvaginal probe (7.5-10 MHz) is used for a transvaginal portion of the examination, and the curvilinear probe (1-6 MHz) is used in the transabdominal approach.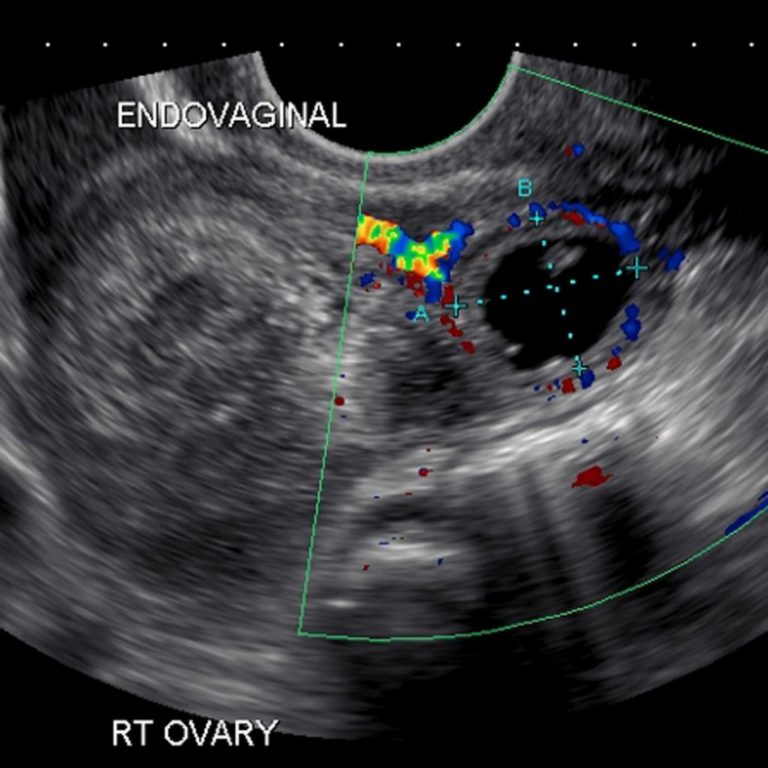 [9]
[9]
Technique
The overall technique for transabdominal and transvaginal ultrasound is the same for all pregnancies, but it differs in the setting of the initial evaluation of pregnancy with trauma.
The transabdominal view in pregnancy is obtained using the curvilinear probe with the patient in a supine position. The probe is placed with the indicator to the head of the patient above the pubis symphysis in the midline. An adequate view of the uterus includes having the length of the uterus in addition to the cervix and part of the vagina visualized.[10] It is important to distinguish the endometrial stripe in the transverse view as a dot or oval and the vaginal as a stripe going across the screen. For transabdominal assessment, it is best to obtain imagining in both longitudinal and transverse views.
During a transvaginal examination, the tactile indicator that is located on the handle of the probe is pointed up towards the ceiling, and the probe is inserted approximately 4 to 5 cm in the sagittal plane.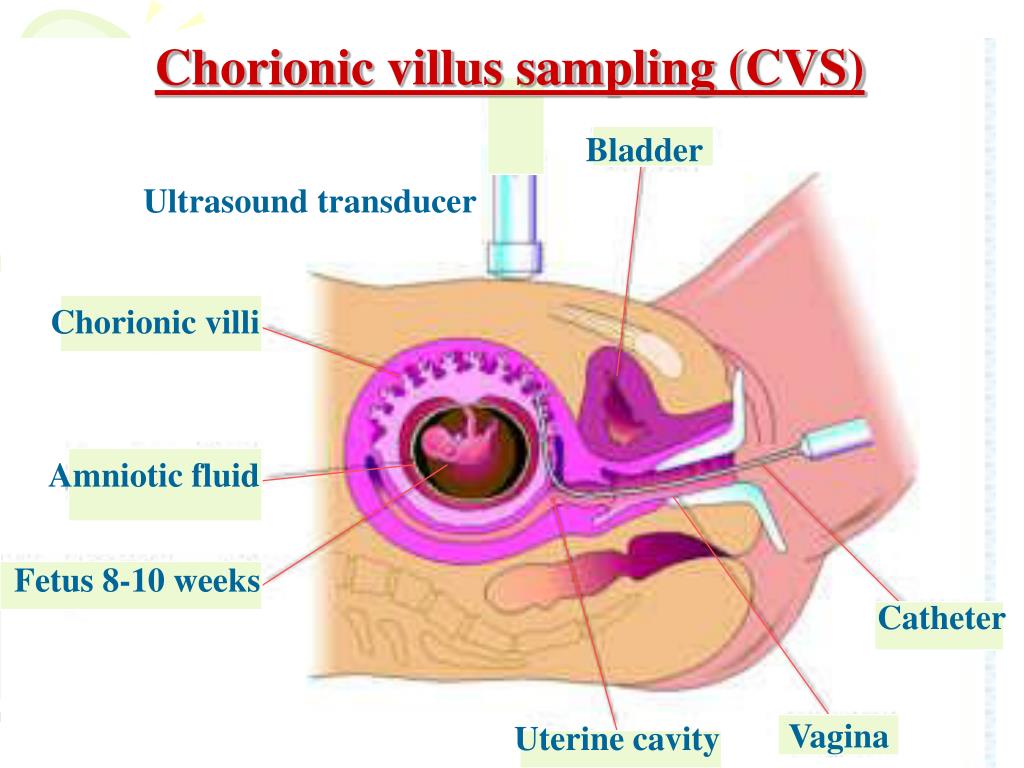 The first and critical step is the determination of landmarks in which the bladder is identified, and subsequently, the juxtaposition between the bladder and the uterus is recognized, which makes it less likely that the exam is being performed in the adnexa.[10] Next, the ovaries and Fallopian tubes must be investigated when suspicion is high for ectopic pregnancy; the most common location for an ectopic pregnancy being the ampulla of the fallopian tube.[11]
The first and critical step is the determination of landmarks in which the bladder is identified, and subsequently, the juxtaposition between the bladder and the uterus is recognized, which makes it less likely that the exam is being performed in the adnexa.[10] Next, the ovaries and Fallopian tubes must be investigated when suspicion is high for ectopic pregnancy; the most common location for an ectopic pregnancy being the ampulla of the fallopian tube.[11]
In the setting of trauma, the patient should undergo an assessment with an ultrasound of the abdomen with a FAST exam to evaluate for free fluid in the peritoneal cavity and pericardium. The FAST exam is performed with a curvilinear probe and evaluates the right upper quadrant (Morrison pouch), left upper quadrant, subxiphoid, and suprapubic with additional attention spent evaluating the uterus for intrauterine pregnancy (IUP) while in this position.
Complications
The overall risk of complications with ultrasound is low; however, a transvaginal ultrasound may cause complications such as anxiety, pain, or vaginal bleeding.
Clinical Significance
Ultrasound is the most commonly used diagnostic procedure in obstetrics. The use of ultrasound is a convenient, painless procedure that yields immediate results and is considered widely safe.[12] Ultrasound has uses in both routine care and in the acute or emergent setting. The goal of ultrasound during routine prenatal care is to establish viability, determine gestational age, and to assess the number of fetuses.[13]
Fetal viability is confirmed by the presence of an embryo that has cardiac activity. Cardiac activity is often present when the embryo itself measures 2 mm or greater during the 6th week of gestation.[5] If cardiac activity is not evident, other sonographic features of early pregnancy can predict viability. Since the first sonographic evidence of pregnancy is the gestational sac (which can be visualized at 4.5 to 5 weeks), its growth and progression are used to assess viability in early pregnancy. The gestational sac should increase by 1. 13 mm a day in normal pregnancy.[2][14] To obtain gestational sac diameter with ultrasound, the caliper function is used and then placed from the inner to the outer wall of the gestational sac. The mean sac diameter (MSD) is calculated by added the longitudinal, anteroposterior, and transverse dimensions of the chorionic space and then taking the sum of these 3 measurements and dividing the sum by 3 to obtain the MSD.[15] Tracking the progression of the MSD through early pregnancy helps predict potential pregnancy failure. An MSD of 25 mm with no embryo indicates pregnancy failure, while MSD between 16 and 25 mm without an embryo is suggestive of a possible pregnancy failure.[16][17] Another predictor of non-viability is the absence of cardiac activity in an embryo with a crown-rump length (CRL) greater than 7 mm. CRL is measured by taking the average of 3 measurements of the longest fetal length.[18] CRL is taken by placing the calipers on the measurement setting and measuring the maximum straight-line length of the embryo in the longitudinal axis.
13 mm a day in normal pregnancy.[2][14] To obtain gestational sac diameter with ultrasound, the caliper function is used and then placed from the inner to the outer wall of the gestational sac. The mean sac diameter (MSD) is calculated by added the longitudinal, anteroposterior, and transverse dimensions of the chorionic space and then taking the sum of these 3 measurements and dividing the sum by 3 to obtain the MSD.[15] Tracking the progression of the MSD through early pregnancy helps predict potential pregnancy failure. An MSD of 25 mm with no embryo indicates pregnancy failure, while MSD between 16 and 25 mm without an embryo is suggestive of a possible pregnancy failure.[16][17] Another predictor of non-viability is the absence of cardiac activity in an embryo with a crown-rump length (CRL) greater than 7 mm. CRL is measured by taking the average of 3 measurements of the longest fetal length.[18] CRL is taken by placing the calipers on the measurement setting and measuring the maximum straight-line length of the embryo in the longitudinal axis. It is important to ensure that when measuring CRL that the embryo isn't too flexed or too extended.[15]
It is important to ensure that when measuring CRL that the embryo isn't too flexed or too extended.[15]
The yolk sac size and shape can be used to predict viability. The yolk sac can be evaluated as early as 5 weeks. Abnormal yolk sac shape (non-round or oval) predicts poor pregnancy outcomes with a sensitivity of 29% and a specificity of 95%.[19] Other characteristics of the yolk sac associated with poor outcomes include the size (smaller than 2 mm or larger than 5 mm in diameter) and the presence of a hyperechoic or hypoechoic rim, hyperechoic yolk sac center, or a number of yolk sacs unequal to the number of embryos. Abnormal yolk sac size and shape are associated with statistically significant higher abortion rates.[20]
Subchorionic hemorrhage is another condition associated with poor pregnancy outcomes that can be assessed with ultrasound. The overall spontaneous abortion rate is doubled in pregnancy cases in which the separation between the uterine wall and the chorionic membrane is considered large compared to small or moderate. A large separation is found to be associated with an approximate 3 fold increase in spontaneous abortion rates.[21] In addition to the size of the hemorrhage, the identification of subchorionic hemorrhage earlier in pregnancy is associated with higher rates of subsequent pregnancy failure.[22]
A large separation is found to be associated with an approximate 3 fold increase in spontaneous abortion rates.[21] In addition to the size of the hemorrhage, the identification of subchorionic hemorrhage earlier in pregnancy is associated with higher rates of subsequent pregnancy failure.[22]
Fetal bradycardia during the first trimester is another important predictor for potential fetal demise. Fetal bradycardia in the early first trimester below 80 bpm is an ominous sign, and physicians should prepare their patients for likely poor outcomes such as spontaneous abortion and potential intrauterine fetal demise. Follow-up scans are done weekly until the heart rate is no longer present or until it becomes normal.[23]
It is recommended that all pregnant women undergo a routine ultrasound at 10 to 13 weeks of gestation to determine an accurate gestational age. Getting an accurate gestational age is highly important and pertinent for the optimal assessment of fetal growth later in pregnancy.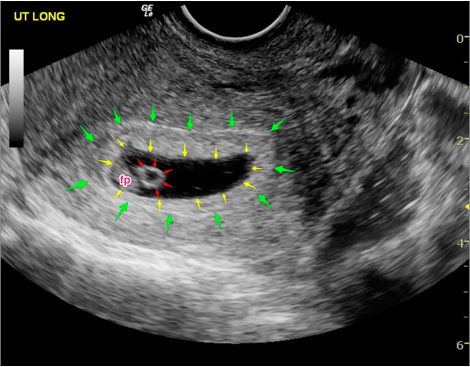 Ultrasound is the most reliable method for establishing a true gestational age by measurement of crown-rump length, which can be measured either transabdominally or transvaginally. CRL allows for an accurate determination of the day of conception +/- 5 days in 95% of pregnancies. Between 11 and 13.6 weeks gestation, it is recommended that CRL be used to determine gestational age unless it is >84 mm, then head circumference (HC) should be used as it is slightly more precise when compared to biparietal diameter (BPD). Head circumference is measured around the outer table of the fetal skull. The technique of BPD measurement depends on the nomogram used. If the nomogram uses outer-to-outer measurements of the fetal skull, then the same should be done during a fetal ultrasound. However, the outer edge of the skull to the inner edge of the skull nomograms are available as well. In order to obtain reliable information, the largest symmetric axial view of the fetal head must be used to visualize the choroid plexus, the third ventricle, or thalamus.
Ultrasound is the most reliable method for establishing a true gestational age by measurement of crown-rump length, which can be measured either transabdominally or transvaginally. CRL allows for an accurate determination of the day of conception +/- 5 days in 95% of pregnancies. Between 11 and 13.6 weeks gestation, it is recommended that CRL be used to determine gestational age unless it is >84 mm, then head circumference (HC) should be used as it is slightly more precise when compared to biparietal diameter (BPD). Head circumference is measured around the outer table of the fetal skull. The technique of BPD measurement depends on the nomogram used. If the nomogram uses outer-to-outer measurements of the fetal skull, then the same should be done during a fetal ultrasound. However, the outer edge of the skull to the inner edge of the skull nomograms are available as well. In order to obtain reliable information, the largest symmetric axial view of the fetal head must be used to visualize the choroid plexus, the third ventricle, or thalamus.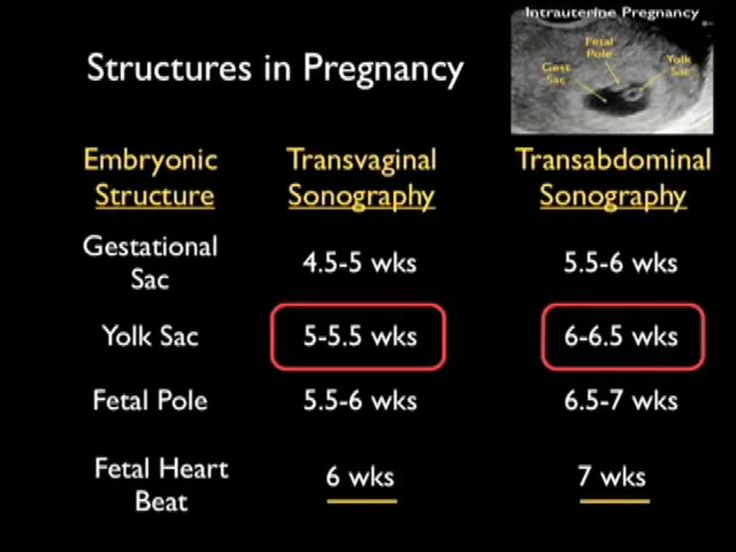 [5]
[5]
Towards the end of the first trimester, a routine scan offers the opportunity to detect any visible gross fetal abnormalities. Measuring nuchal translucency in the first trimester has been associated with having both high sensitivity and specificity for identifying pregnancies that are at risk for chromosomal anomalies, the cut-off being 3 mm or greater.[24] It is important to note that not all fetal abnormalities manifest in the first trimester; thus, it is important to undergo standard transabdominal ultrasound during the second trimester.[25]
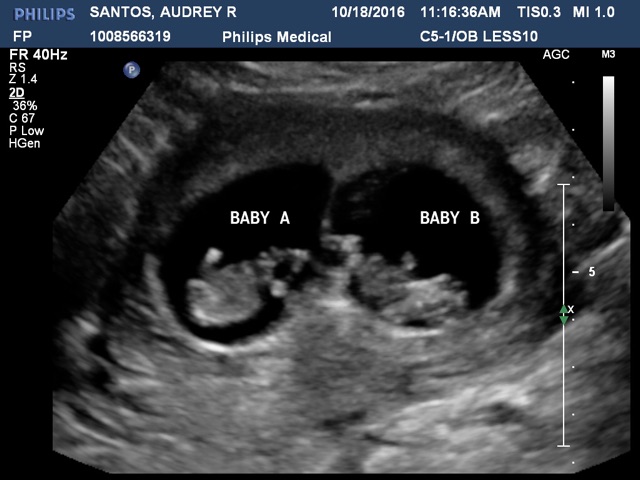
Another important goal of the routine obstetric ultrasound at 10 to 13 weeks of gestation is the determination of the number of fetuses as well as amnionicity and chorionicity in twin gestations. Amnionicity is determined by the absence or presence of the intertwin membrane (ITM). If no ITM is identified, pregnancy is described as "mono-amniotic and mono-chorionic," and it implies the highest potential rate of complications (cord entanglement and fetal death). [26] Chorionicity describes different types of placentation and also predicts risks in twin pregnancies. If ITM is identified, monochorionic or dichorionic placentation is investigated next. Monochorionic placentation has a single placenta, while dichorionic placentation describes two separate placentas in twin pregnancies. In order to determine chorionicity, chorionic membrane base and thickness are evaluated. The presence of the lambda sign (a thick, Y-shaped base of the chorion) is used to predict chorionicity with greater than 95% accuracy, but only if it's used before 14 weeks of gestation. If the lambda sign is identified, a dichorionic pregnancy is diagnosed.[27]
[26] Chorionicity describes different types of placentation and also predicts risks in twin pregnancies. If ITM is identified, monochorionic or dichorionic placentation is investigated next. Monochorionic placentation has a single placenta, while dichorionic placentation describes two separate placentas in twin pregnancies. In order to determine chorionicity, chorionic membrane base and thickness are evaluated. The presence of the lambda sign (a thick, Y-shaped base of the chorion) is used to predict chorionicity with greater than 95% accuracy, but only if it's used before 14 weeks of gestation. If the lambda sign is identified, a dichorionic pregnancy is diagnosed.[27]
In the second trimester, the goal of routine ultrasound examination, typically performed between 18 and 22 weeks, is to assess the fetal anatomy and further evaluate the placenta.[28] The reported advantages of routine ultrasound include early detection of many major anomalies, earlier determination of genetic diagnosis, and easier pregnancy termination if appropriate.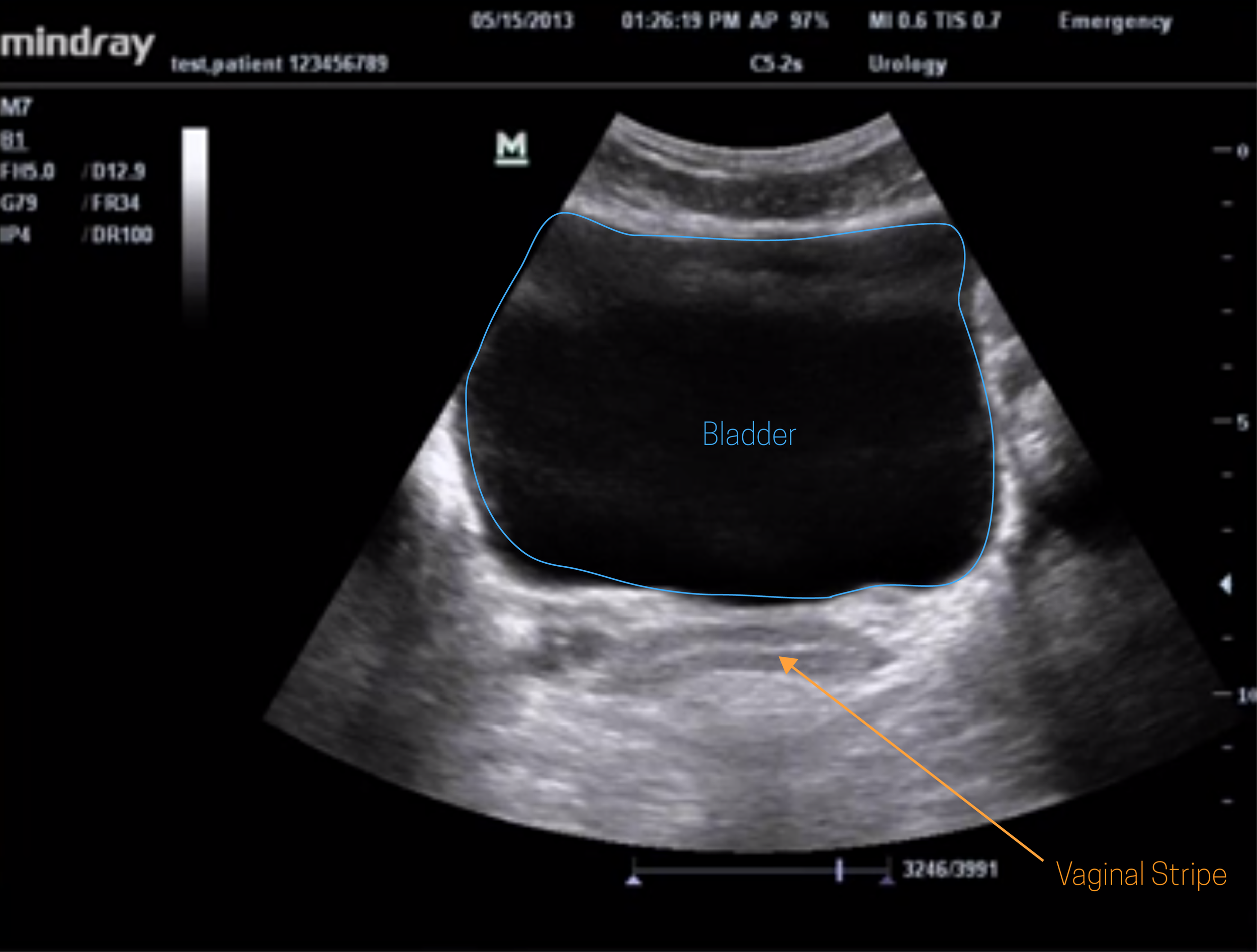 [5] Ultrasound evaluation of the placenta can confirm that the placenta has implanted in the correct anatomical position and help recognize variations of placenta previa or placenta accreta. During the second trimester, the placental volume can be measured and calculated using volume organ computer-aided analysis. This measurement of placental volume aids in predicting neonatal birth weights. Women who have lower mean second-trimester placental volume have higher rates of neonates that were born small for gestational age (SGA) compared to women with normal placental volumes in the appropriate gestational age (AGA) group. Placental volumes for the AGA group typically measured with ultrasound to be 213.5 ± 75.8 versus the SGA group measured at 170.6 ± 49.8.[29]
[5] Ultrasound evaluation of the placenta can confirm that the placenta has implanted in the correct anatomical position and help recognize variations of placenta previa or placenta accreta. During the second trimester, the placental volume can be measured and calculated using volume organ computer-aided analysis. This measurement of placental volume aids in predicting neonatal birth weights. Women who have lower mean second-trimester placental volume have higher rates of neonates that were born small for gestational age (SGA) compared to women with normal placental volumes in the appropriate gestational age (AGA) group. Placental volumes for the AGA group typically measured with ultrasound to be 213.5 ± 75.8 versus the SGA group measured at 170.6 ± 49.8.[29]
As opposed to asymptomatic pregnant patients undergoing routine obstetric ultrasound imaging, pregnant patients with concerning symptoms must be evaluated on an emergent basis. In cases in which a stable patient presents for an evaluation of pelvic pain, abdominal pain, or vaginal bleeding early in suspected pregnancy, it is important first to establish a diagnosis of an IUP.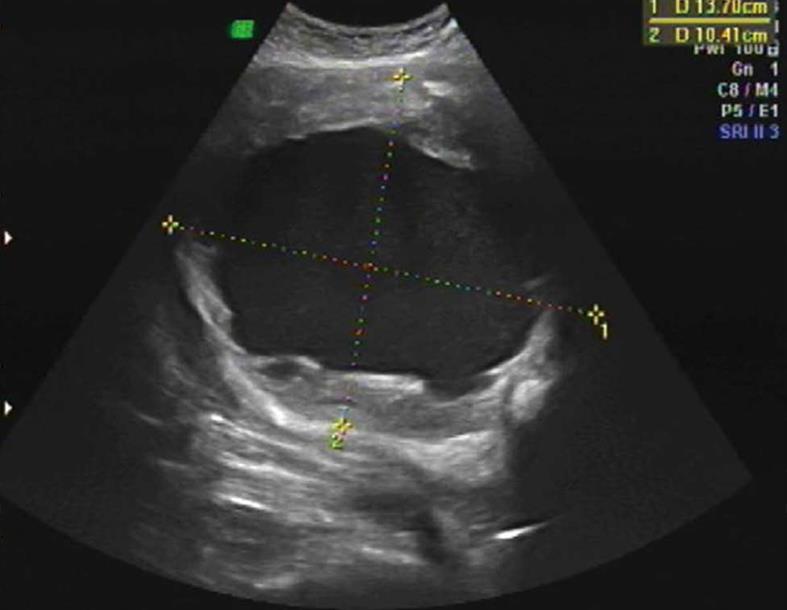 If pelvic ultrasound reveals an IUP, it can be assumed that the cause of symptoms is unlikely to be secondary to an ectopic pregnancy.[30] However, it is important to consider heterotopic pregnancy, which is defined as the simultaneous presence of intrauterine and ectopic pregnancies; this condition is more common in women undergoing in-vitro fertilization (IVF) or women that have a history of tubal disease. The incidence of ectopic pregnancy is 0.006 to 0.001% in spontaneous cases, while in assisted reproductive techniques, such as IVF, it is 1 to 3%.[31] Once ectopic pregnancy is ruled out, other causes of vaginal bleeding or pelvic pain may be considered, such as spontaneous abortion, threatened abortion, gestational trophoblastic neoplasm, trauma, or most commonly normal pregnancy. Management of a stable patient with minimal bleeding in early pregnancy includes outpatient follow-up within 1 to 2 days and strict return precautions. It must be noted that for pelvic pain or vaginal bleeding complaints that occur later in pregnancy (>23 weeks), a speculum or digital vaginal exam should be held until placenta previa is ruled out by ultrasound.
If pelvic ultrasound reveals an IUP, it can be assumed that the cause of symptoms is unlikely to be secondary to an ectopic pregnancy.[30] However, it is important to consider heterotopic pregnancy, which is defined as the simultaneous presence of intrauterine and ectopic pregnancies; this condition is more common in women undergoing in-vitro fertilization (IVF) or women that have a history of tubal disease. The incidence of ectopic pregnancy is 0.006 to 0.001% in spontaneous cases, while in assisted reproductive techniques, such as IVF, it is 1 to 3%.[31] Once ectopic pregnancy is ruled out, other causes of vaginal bleeding or pelvic pain may be considered, such as spontaneous abortion, threatened abortion, gestational trophoblastic neoplasm, trauma, or most commonly normal pregnancy. Management of a stable patient with minimal bleeding in early pregnancy includes outpatient follow-up within 1 to 2 days and strict return precautions. It must be noted that for pelvic pain or vaginal bleeding complaints that occur later in pregnancy (>23 weeks), a speculum or digital vaginal exam should be held until placenta previa is ruled out by ultrasound.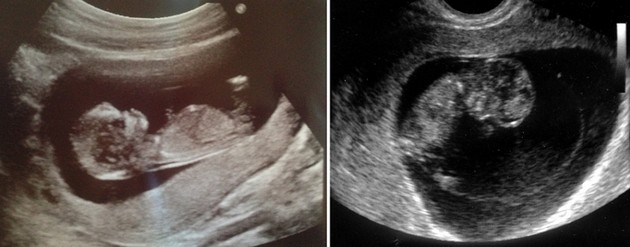 [6] Placenta previa accounts for 13 percent of maternal deaths secondary to hemorrhage in the United States in a recent report. It is associated with other complications, including the need for blood transfusion, organ injury, need for hysterectomy, venous thromboembolism, and increased infection risk, making identification of placenta previa an important part of obstetric ultrasound.[32]
[6] Placenta previa accounts for 13 percent of maternal deaths secondary to hemorrhage in the United States in a recent report. It is associated with other complications, including the need for blood transfusion, organ injury, need for hysterectomy, venous thromboembolism, and increased infection risk, making identification of placenta previa an important part of obstetric ultrasound.[32]
Trauma in pregnancy is the leading cause of non-obstetric maternal mortality. Non-lethal injuries during pregnancy most commonly occur from motor vehicle accidents and domestic/intimate partner violence. Although most injuries during pregnancy are classified as minor, fetal losses that are associated with minor trauma range from 60 to 70%. Importantly, any female of reproductive age with minor or major injury should be assumed pregnant until proven otherwise. The immediate focus is always on stabilizing the patient. Once successfully stabilized, all female patients of reproductive age should undergo a definitive pregnancy test or an ultrasound scan. In the setting of trauma, the patient may not be conscious or able to report their pregnancy status or gestational age; thus, estimating gestational age with bedside ultrasound can be a useful tool. Identifying pregnancy and estimating gestational age can help anticipate the need for prompt delivery. Ultrasound can assist in the evaluation of fetal cardiac rate and rhythm, amniotic fluid volume, placental localization, exclusion of previa, delineating possible fetal injury, and confirming fetal demise. If a patient is estimated to be >20 weeks gestation, fetal monitoring should be initiated as soon as possible in a stable patient. In the setting of trauma in pregnancy, a critical concern is placental abruption, a condition that occurs most commonly in trauma in which the patient experiences intense and severe uterine pain, in addition to uterine contractions and vaginal bleeding. It is important to note that the use of ultrasound for detecting placental abruption has a poor sensitivity; however, it is very specific if identified; resulting in a positive predictive value of 88% if seen and a negative predictive value of 53% if not identified.
In the setting of trauma, the patient may not be conscious or able to report their pregnancy status or gestational age; thus, estimating gestational age with bedside ultrasound can be a useful tool. Identifying pregnancy and estimating gestational age can help anticipate the need for prompt delivery. Ultrasound can assist in the evaluation of fetal cardiac rate and rhythm, amniotic fluid volume, placental localization, exclusion of previa, delineating possible fetal injury, and confirming fetal demise. If a patient is estimated to be >20 weeks gestation, fetal monitoring should be initiated as soon as possible in a stable patient. In the setting of trauma in pregnancy, a critical concern is placental abruption, a condition that occurs most commonly in trauma in which the patient experiences intense and severe uterine pain, in addition to uterine contractions and vaginal bleeding. It is important to note that the use of ultrasound for detecting placental abruption has a poor sensitivity; however, it is very specific if identified; resulting in a positive predictive value of 88% if seen and a negative predictive value of 53% if not identified. Thus fetal prolonged monitoring is advised in pregnant patients with trauma. A follow-up obstetric ultrasound and examination should be done 2 weeks after any hospital admission for either maternal or fetal factors (regardless of the gestational age) to document and assess normalcy after the traumatic event.[6][33]
Thus fetal prolonged monitoring is advised in pregnant patients with trauma. A follow-up obstetric ultrasound and examination should be done 2 weeks after any hospital admission for either maternal or fetal factors (regardless of the gestational age) to document and assess normalcy after the traumatic event.[6][33]
Enhancing Healthcare Team Outcomes
The care of a pregnant patient requires coordination between an interprofessional team comprised of physicians, nurses, pharmacists, and other healthcare professionals. Not every complaint in pregnancy is an obstetric emergency; however, it is important to recognize and promptly diagnose the conditions that have been discussed above (ectopic pregnancy, placental abruption, etc.). The use of rapid bedside ultrasound by emergency department providers improves patient outcomes and allows for rapid assessment of both mother and baby, which in turn aids in the ability to communicate more rapidly with the obstetrical specialists in the setting of surgical obstetric emergencies. Ultrasound reduces maternal and neonatal mortality in primary care facilities and should be included in the assessment by all providers routinely caring for pregnant patients.[33]
Ultrasound reduces maternal and neonatal mortality in primary care facilities and should be included in the assessment by all providers routinely caring for pregnant patients.[33]
Nursing, Allied Health, and Interprofessional Team Interventions
When a stable pregnant patient presents for an evaluation with complaints of pelvic pain, vaginal bleeding, or trauma, the initial action is to get the patient on a monitor and obtain a full set of vital signs. Vital signs must be monitored closely in the pregnant patient to ensure shock is promptly recognized. In addition to cardiac monitoring and continuous pulse oximetry, 2 large-bore intravenous (IV) lines must be established, coordinating care between the physician and nursing staff of paramount importance.
In cases when an unstable female patient presents for an evaluation in an acute setting (e.g., the emergency department), staff must work together to ensure that portable bedside ultrasound is available and ready for use by trauma or emergency medicine providers (preferably before the unstable patient arrives). While the primary assessment is being performed, nursing staff should obtain a full set of vital signs and establish at least 2 large-bore IVs. In cases of known pregnancy or if bedside ultrasound reveals pregnancy, emergent consultation with obstetrical specialists must be requested. Nursing should be prepared and plan for a prompt sign-out to obstetrical services in the setting of a pregnant patient.[33]
While the primary assessment is being performed, nursing staff should obtain a full set of vital signs and establish at least 2 large-bore IVs. In cases of known pregnancy or if bedside ultrasound reveals pregnancy, emergent consultation with obstetrical specialists must be requested. Nursing should be prepared and plan for a prompt sign-out to obstetrical services in the setting of a pregnant patient.[33]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Siddique J, Lauderdale DS, VanderWeele TJ, Lantos JD. Trends in prenatal ultrasound use in the United States: 1995 to 2006. Med Care. 2009 Nov;47(11):1129-35. [PubMed: 19786915]
- 2.
Doubilet PM. Ultrasound evaluation of the first trimester. Radiol Clin North Am. 2014 Nov;52(6):1191-9. [PubMed: 25444100]
- 3.
Richardson A, Gallos I, Dobson S, Campbell BK, Coomarasamy A, Raine-Fenning N.
 Accuracy of first-trimester ultrasound in diagnosis of intrauterine pregnancy prior to visualization of the yolk sac: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015 Aug;46(2):142-9. [PubMed: 25393076]
Accuracy of first-trimester ultrasound in diagnosis of intrauterine pregnancy prior to visualization of the yolk sac: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015 Aug;46(2):142-9. [PubMed: 25393076]- 4.
Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental Imaging: Normal Appearance with Review of Pathologic Findings. Radiographics. 2017 May-Jun;37(3):979-998. [PubMed: 28493802]
- 5.
Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, Lau TK, Papageorghiou AT, Raine-Fenning NJ, Stirnemann J, Suresh S, Tabor A, Timor-Tritsch IE, Toi A, Yeo G. ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol. 2013 Jan;41(1):102-13. [PubMed: 23280739]
- 6.
Jain V, Chari R, Maslovitz S, Farine D, Maternal Fetal Medicine Committee. Bujold E, Gagnon R, Basso M, Bos H, Brown R, Cooper S, Gouin K, McLeod NL, Menticoglou S, Mundle W, Pylypjuk C, Roggensack A, Sanderson F.
 Guidelines for the Management of a Pregnant Trauma Patient. J Obstet Gynaecol Can. 2015 Jun;37(6):553-74. [PubMed: 26334607]
Guidelines for the Management of a Pregnant Trauma Patient. J Obstet Gynaecol Can. 2015 Jun;37(6):553-74. [PubMed: 26334607]- 7.
Narayanan M, Tafti D, Cohen HL. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 5, 2022. Pelvic Ultrasound. [PubMed: 29262064]
- 8.
Timor-Tritsch IE, Yunis RA. Confirming the safety of transvaginal sonography in patients suspected of placenta previa. Obstet Gynecol. 1993 May;81(5 ( Pt 1)):742-4. [PubMed: 8469465]
- 9.
Mausner Geffen E, Slywotzky C, Bennett G. Pitfalls and tips in the diagnosis of ectopic pregnancy. Abdom Radiol (NY). 2017 May;42(5):1524-1542. [PubMed: 28144719]
- 10.
Baker M, dela Cruz J. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 21, 2022. Ectopic Pregnancy, Ultrasound. [PubMed: 29489174]
- 11.
Chukus A, Tirada N, Restrepo R, Reddy NI. Uncommon Implantation Sites of Ectopic Pregnancy: Thinking beyond the Complex Adnexal Mass.
 Radiographics. 2015 May-Jun;35(3):946-59. [PubMed: 25860721]
Radiographics. 2015 May-Jun;35(3):946-59. [PubMed: 25860721]- 12.
Abramowicz JS. Benefits and risks of ultrasound in pregnancy. Semin Perinatol. 2013 Oct;37(5):295-300. [PubMed: 24176149]
- 13.
Elson J, Salim R, Tailor A, Banerjee S, Zosmer N, Jurkovic D. Prediction of early pregnancy viability in the absence of an ultrasonically detectable embryo. Ultrasound Obstet Gynecol. 2003 Jan;21(1):57-61. [PubMed: 12528163]
- 14.
Blaas HG. Detection of structural abnormalities in the first trimester using ultrasound. Best Pract Res Clin Obstet Gynaecol. 2014 Apr;28(3):341-53. [PubMed: 24355991]
- 15.
Ali S, Byanyima RK, Ononge S, Ictho J, Nyamwiza J, Loro ELE, Mukisa J, Musewa A, Nalutaaya A, Ssenyonga R, Kawooya I, Temper B, Katamba A, Kalyango J, Karamagi C. Measurement error of mean sac diameter and crown-rump length among pregnant women at Mulago hospital, Uganda. BMC Pregnancy Childbirth. 2018 May 04;18(1):129.
 [PMC free article: PMC5935951] [PubMed: 29728143]
[PMC free article: PMC5935951] [PubMed: 29728143]- 16.
Doubilet PM, Benson CB, Bourne T, Blaivas M, Society of Radiologists in Ultrasound Multispecialty Panel on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy. Barnhart KT, Benacerraf BR, Brown DL, Filly RA, Fox JC, Goldstein SR, Kendall JL, Lyons EA, Porter MB, Pretorius DH, Timor-Tritsch IE. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013 Oct 10;369(15):1443-51. [PubMed: 24106937]
- 17.
Preisler J, Kopeika J, Ismail L, Vathanan V, Farren J, Abdallah Y, Battacharjee P, Van Holsbeke C, Bottomley C, Gould D, Johnson S, Stalder C, Van Calster B, Hamilton J, Timmerman D, Bourne T. Defining safe criteria to diagnose miscarriage: prospective observational multicentre study. BMJ. 2015 Sep 23;351:h5579. [PMC free article: PMC4580727] [PubMed: 26400869]
- 18.
Kapfhamer JD, Palaniappan S, Summers K, Kassel K, Mancuso AC, Ryan GL, Shah DK.
 Difference between mean gestational sac diameter and crown-rump length as a marker of first-trimester pregnancy loss after in vitro fertilization. Fertil Steril. 2018 Jan;109(1):130-136. [PMC free article: PMC6248327] [PubMed: 29175064]
Difference between mean gestational sac diameter and crown-rump length as a marker of first-trimester pregnancy loss after in vitro fertilization. Fertil Steril. 2018 Jan;109(1):130-136. [PMC free article: PMC6248327] [PubMed: 29175064]- 19.
Küçük T, Duru NK, Yenen MC, Dede M, Ergün A, Başer I. Yolk sac size and shape as predictors of poor pregnancy outcome. J Perinat Med. 1999;27(4):316-20. [PubMed: 10560085]
- 20.
Moradan S, Forouzeshfar M. Are abnormal yolk sac characteristics important factors in abortion rates? Int J Fertil Steril. 2012 Jul;6(2):127-30. [PMC free article: PMC4258241] [PubMed: 25493170]
- 21.
Bennett GL, Bromley B, Lieberman E, Benacerraf BR. Subchorionic hemorrhage in first-trimester pregnancies: prediction of pregnancy outcome with sonography. Radiology. 1996 Sep;200(3):803-6. [PubMed: 8756935]
- 22.
Heller HT, Asch EA, Durfee SM, Goldenson RP, Peters HE, Ginsburg ES, Doubilet PM, Benson CB.
 Subchorionic Hematoma: Correlation of Grading Techniques With First-Trimester Pregnancy Outcome. J Ultrasound Med. 2018 Jul;37(7):1725-1732. [PubMed: 29341210]
Subchorionic Hematoma: Correlation of Grading Techniques With First-Trimester Pregnancy Outcome. J Ultrasound Med. 2018 Jul;37(7):1725-1732. [PubMed: 29341210]- 23.
Laboda LA, Estroff JA, Benacerraf BR. First trimester bradycardia. A sign of impending fetal loss. J Ultrasound Med. 1989 Oct;8(10):561-3. [PubMed: 2681826]
- 24.
Conner SN, Longman RE, Cahill AG. The role of ultrasound in the diagnosis of fetal genetic syndromes. Best Pract Res Clin Obstet Gynaecol. 2014 Apr;28(3):417-28. [PMC free article: PMC4079588] [PubMed: 24534428]
- 25.
Achiron R, Tadmor O. Screening for fetal anomalies during the first trimester of pregnancy: transvaginal versus transabdominal sonography. Ultrasound Obstet Gynecol. 1991 May 01;1(3):186-91. [PubMed: 12797070]
- 26.
Killion MM. Twins: The Importance of Chorionicity in Planning Care and Timing of Birth. MCN Am J Matern Child Nurs. 2019 Mar/Apr;44(2):115. [PubMed: 30807329]
- 27.
Maruotti GM, Saccone G, Morlando M, Martinelli P. First-trimester ultrasound determination of chorionicity in twin gestations using the lambda sign: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016 Jul;202:66-70. [PubMed: 27180271]
- 28.
Bethune M, Alibrahim E, Davies B, Yong E. A pictorial guide for the second trimester ultrasound. Australas J Ultrasound Med. 2013 Aug;16(3):98-113. [PMC free article: PMC5029995] [PubMed: 28191183]
- 29.
Fang SW, Ou CY, Tsai CC, Fu HC, Cheng HH, Cheng BH, Chang MS, Hsu TY. Second-trimester placental volume and vascular indices in the prediction of small-for-gestational-age neonates. Fetal Diagn Ther. 2015;37(2):123-8. [PubMed: 25359105]
- 30.
Varner C, Balaban D, McLeod S, Carver S, Borgundvaag B. Fetal outcomes following emergency department point-of-care ultrasound for vaginal bleeding in early pregnancy. Can Fam Physician. 2016 Jul;62(7):572-578. [PMC free article: PMC4955088] [PubMed: 27829074]
- 31.

Nabi U, Yousaf A, Ghaffar F, Sajid S, Ahmed MMH. Heterotopic Pregnancy - A Diagnostic Challenge. Six Case Reports and Literature Review. Cureus. 2019 Nov 05;11(11):e6080. [PMC free article: PMC6894893] [PubMed: 31853431]
- 32.
Wortman AC, Schaefer SL, McIntire DD, Sheffield JS, Twickler DM. Complete Placenta Previa: Ultrasound Biometry and Surgical Outcomes. AJP Rep. 2018 Apr;8(2):e74-e78. [PMC free article: PMC5910059] [PubMed: 29686936]
- 33.
Murphy NJ, Quinlan JD. Trauma in pregnancy: assessment, management, and prevention. Am Fam Physician. 2014 Nov 15;90(10):717-22. [PubMed: 25403036]
prices for tests for pregnant women
During the development of the fetus, ultrasound is one of the key methods of examination. There is no exact schedule for ultrasound, so the doctor focuses primarily on the condition of the patient, the condition of the fetus, the presence of somatic pathology. If we take a physiologically occurring pregnancy, then ultrasound is performed in each of the trimesters.
Ultrasound at 8 weeks is the first time that this study is recommended. The eighth week is the first critical period, therefore, it is most rational to carry out diagnostics during this period.
Since it is the 8th week of pregnancy, a transvaginal examination is performed more often, which is more reliable. At this time, transabdominal ultrasound is used less and less. The transvaginal method does not pose any threat to either the mother or the fetus.
Ultrasound at 8 weeks can confirm
- Normal uterine pregnancy;
- Dimensions of the gestational sac;
- Whether the pregnancy is multiple;
- Place of attachment of the fetus;
- Exclude the presence of malformations;
- Exclude various obstetric complications.
If the doctor confirms a physiologically proceeding pregnancy on an ultrasound examination, does not reveal complications, the fetus develops according to age norms, then the next ultrasound is prescribed at 12 weeks. This period is another critical period when it is necessary to assess the condition of the woman and the unborn baby.
This period is another critical period when it is necessary to assess the condition of the woman and the unborn baby.
If the first two critical periods are mainly related to hormonal changes, then the next period - 22 weeks, is most often associated with sexual infections. Therefore, we also perform an ultrasound at 22 weeks. Pregnancy can provoke the development of latent infections, which, in turn, can lead to certain complications.
Tests at 8 weeks of pregnancy
There are no exact recommendations for registering pregnant women, but doctors recommend starting monitoring at the antenatal clinic before 12 weeks. There is a mandatory list of tests in accordance with the order of the Ministry of Health of the Russian Federation, and an additional one, which is appointed by the gynecologist individually.
Tests at 8 weeks of gestation:
- CBC;
- OAM;
- Swab;
- Determination of blood group and Rh factor;
- Tests for major venereal diseases.

In addition, the 8th week of pregnancy is the period of visiting the following doctors:
- Therapist;
- Optometrist;
- ENT;
- Dentist.
Accordingly, if any pathology is detected, any of these specialists has the right to prescribe an additional analysis in their direction. If this pregnancy proceeds with complications, or if there are previous complications in the anamnesis, then the laboratory and instrumental complex may expand.
You will have to take tests regularly, so you should prepare in advance for the next tests at week 12.
Ultrasound at 12 weeks pregnant
As we mentioned earlier, the next critical period is the 12th week of pregnancy. Therefore, the next ultrasound is performed at this time. Here we are not talking about a simple study, but about screening, which allows you to identify intrauterine malformations of the fetus.
In contrast to the ultrasound at 8 weeks, this is predominantly a transabdominal examination.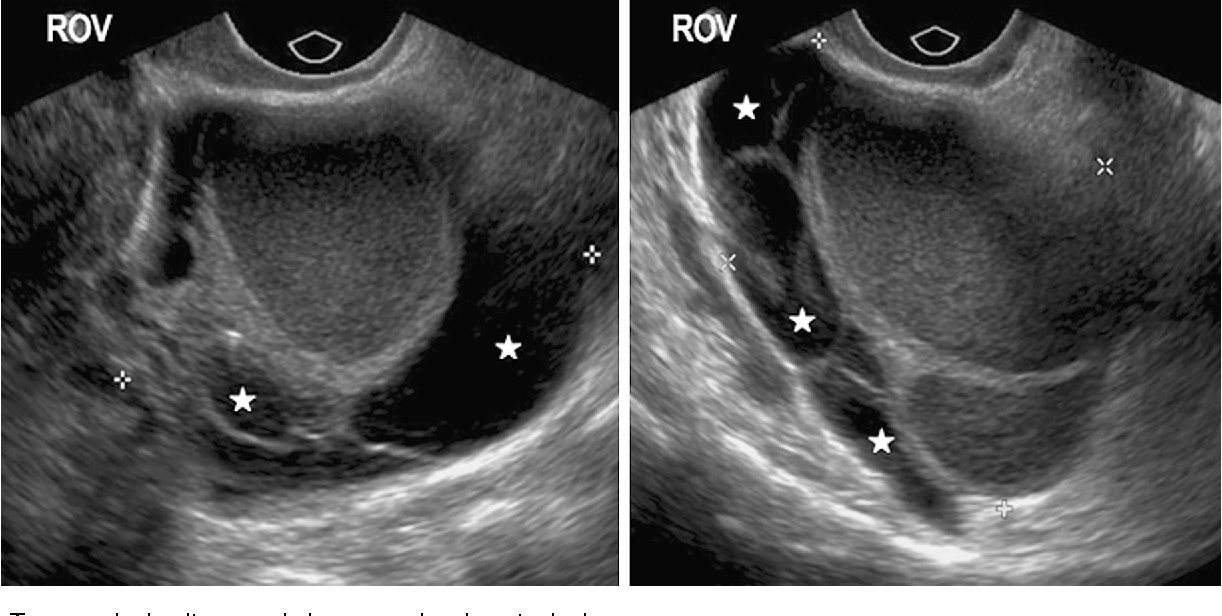 Transvaginal ultrasound is performed only for certain indications:
Transvaginal ultrasound is performed only for certain indications:
- Low insertion of the placenta;
- Isthmic-cervical insufficiency;
- Pelvic inflammation;
- Atypical location of myomatous nodes;
- Malposition of the fetus, in which transabdominal ultrasound at 12 weeks of gestation is uninformative.
So, what information does an ultrasound give a gynecologist?
- Detection of deviations in the growth and development of the fetus;
- Possibility to suspect congenital anomalies;
- Exact gestational age;
- Palpitation;
- Cord entanglement;
- Characteristics of amniotic fluid;
- Condition of the placenta.
It must be clearly understood that ultrasound during pregnancy is only one of the methods of examination, therefore, if there are any deviations in the indicators, you should not panic, you should consult a specialist. The doctor, interpreting the results, always relies on many factors, which allows him to adequately assess the true state of the future mother and fetus.
The doctor, interpreting the results, always relies on many factors, which allows him to adequately assess the true state of the future mother and fetus.
Even if deviations in some indicators are confirmed, doctors still only talk about a certain probability of developing a particular pathology. In this case, a second screening may be prescribed, or a similar study is carried out at a later date. In any case, the final decision regarding the continuation of the pregnancy is made exclusively by a specialist.
Tests at 12 weeks of pregnancy
As we have already said, 12 weeks is the time for screening. For this, an ultrasound examination is prescribed, the external indicators of the woman are evaluated, and a blood test is performed.
Particular attention is paid to two coefficients: β-hCG and PAPP-A. It is believed that in the presence of deviations according to these parameters, one can judge the presence of fetal pathologies. According to the level of hCG, doctors predict the further management of pregnancy and the possibility of miscarriage or premature birth.
Accordingly, according to the screening results, it is possible to identify:
- The baby has Down syndrome;
- Multiple pregnancy;
- Specify term;
- Detect toxicosis;
- Determine the risk of miscarriage;
- Check for other chromosomal abnormalities.
Thus, tests at the 12th week of pregnancy are decisive for solving a number of issues related to the further development of the fetus. It should be clearly understood that screening is not 100% reliable, therefore, if you receive any deviations from normal results, you should immediately contact a specialist who can correctly assess such changes in indicators.
Ultrasound at 22 weeks gestation
The next scheduled ultrasound is performed at 22 weeks of gestation. Here, for the doctor, it is not the condition of the mother or the size of the fetus that is important, but the assessment of the formation of various organs and systems, as well as bones.
So, the 22nd week - the fetus has already formed all the main organs and systems, and on the monitor screen the child acquires the outlines familiar to future parents. Accordingly, the following indicators come to the fore:
- All internal organs should form. During an ultrasound, the doctor evaluates their location, how they function;
- The spine is also studied, the presence of bones and their sizes are determined;
- Assessing the brain and its activity;
- Assess the condition of the placenta, umbilical cord vessels;
- Composition of amniotic fluid;
- Condition of the cervix.
Unlike ultrasound at 8 weeks, ultrasound at this time is performed transabdominally. 22 weeks is already the second trimester, and right now the question is being decided whether there are serious deviations in the development of the fetus, and further actions of obstetricians. The question of whether to continue a further pregnancy is decided not by one doctor, but by a whole council, based on numerous research results.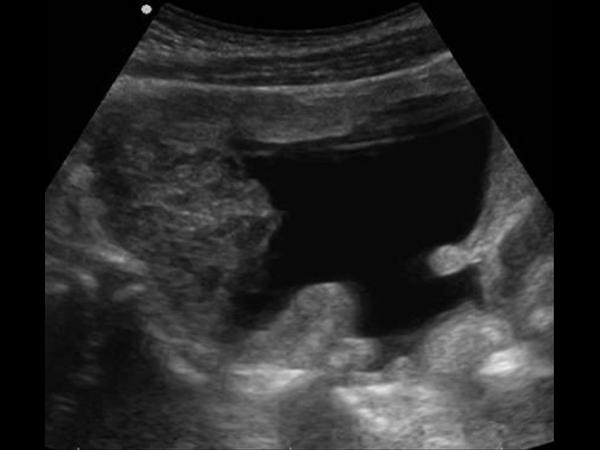
Tests at 22 weeks pregnant
Week 22 is when the second screening is more common. This analysis is prescribed in the period from 18 to 24 weeks, but this time is considered optimal. Accordingly, during repeated screening, the doctor already makes final conclusions about the condition and development of the fetus, the presence of deviations.
In addition to ultrasound, the doctor prescribes mandatory tests to monitor the woman's health. The expectant mother again takes a general blood and urine test, where the most important are a number of indicators: hemoglobin, erythrocytes, leukocytes, ESR, protein in the urine.
During the examination, the gynecologist necessarily measures the woman's height, weight, blood pressure level, and measures the abdomen. Tests at 22 weeks of gestation are designed to assess the likelihood of developing preeclampsia. Here, the role is played not by hormonal changes, but by the exacerbation of chronic pathology. Therefore, timely screening and assessment of the woman's condition allows you to plan further tactics for managing pregnancy.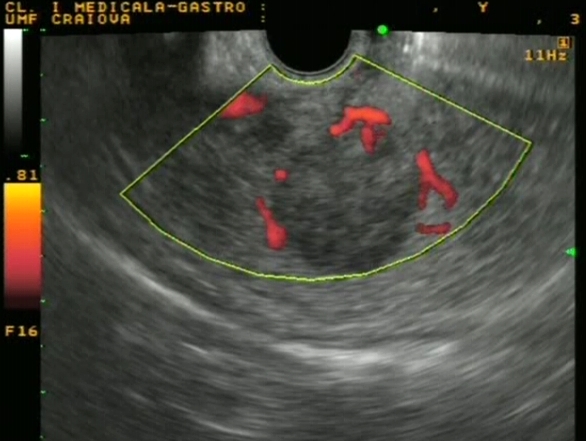
You can find out the cost of an appointment with a gynecologist by phone number +7 495 478 10 03. Also during the planning of pregnancy in our center there is an opportunity to undergo a comprehensive examination of the body for women, and for future fathers - a comprehensive examination of men.
Author of the text: Sokolov Alexander Alexandrovich
Position: Doctor of ultrasound diagnostics
Total experience: 6 years
Ultrasound of pregnant women up to 11 weeks of pregnancy
The expectant mother during the entire pregnancy should be observed by an obstetrician-gynecologist and regularly undergo scheduled diagnostic examinations. Ultrasound is considered the most informative and safe way to monitor the development of the fetus. As part of prenatal screening, the first procedure is usually carried out at 10-11 weeks of pregnancy. It is during this period that one can track the presence or absence of abnormalities and defects in the development of the embryo, as well as assess the state of the woman's reproductive system.
Ultrasound of pregnant women up to 11 weeks of pregnancy in Novokuznetsk:
Clinic "Mother and Child" Novokuznetsk
Why do ultrasound before 11 weeks of pregnancy?
From an obstetric point of view, the first weeks of pregnancy are a special stage, and examination during this period allows doctors to get an objective picture of the development of the embryo. A certain time has already passed since the moment of conception, and every day significant changes occur in the child's body: organs and vital systems are formed, features of physical development are laid, and gender is manifested.
The main task of ultrasound is to identify possible pathologies of fetal development, including chromosomal ones (Down, Cornelia de Lange, Turner, Patau syndromes). During the examination, the specialist determines the date of conception with high accuracy, makes predictions regarding the further course of pregnancy, as well as the risks of complications and the possibility of miscarriage.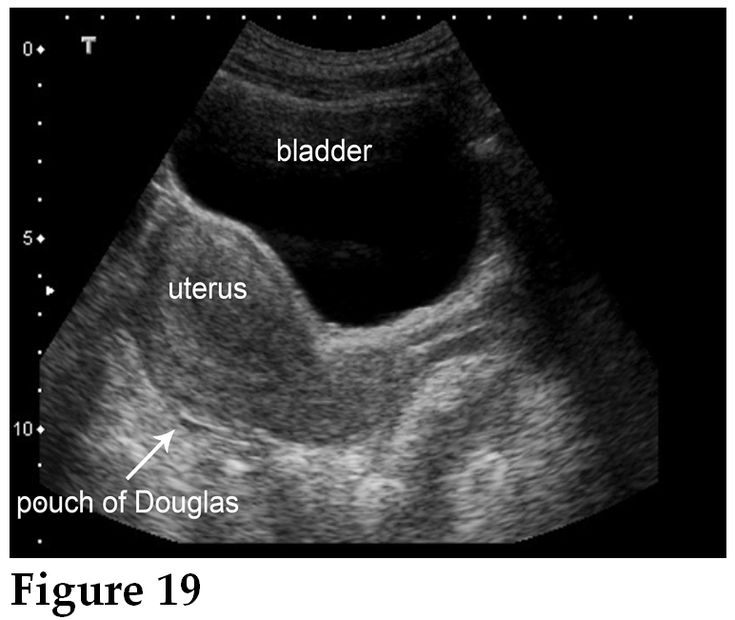 To get a complete picture in the first trimester, a comprehensive examination is carried out, including two procedures:
To get a complete picture in the first trimester, a comprehensive examination is carried out, including two procedures:
- ultrasound procedure;
- blood chemistry.
Indications for examination
Ultrasound before the 11th week of pregnancy is prescribed for all women; but there are patients for whom this procedure is of particular importance. We are talking about expectant mothers from the risk group, namely:
- over the age of 35;
- with hereditary genetic pathologies;
- who have already given birth to children with chromosomal abnormalities;
- taking strong medications in early pregnancy;
- transferred infectious diseases;
- suffered miscarriages and premature births.

The age of the patient's partner also matters: if a man is over 40 years old at the time of conception, then this is also an indication for an ultrasound scan.
Ultrasound examination is absolutely safe and has no contraindications.
Preparation for the procedure
No special preparation is required before the procedure. In order for the picture during the study to have a clear outline and not be distorted, three days before the ultrasound, foods that promote increased gas formation should be excluded from the diet: legumes, cabbage, bakery products, fatty foods, milk, carbonated drinks. If possible, it is better to come to the examination on an empty stomach.
Examination procedure
Ultrasound during pregnancy can be performed in two ways: transabdominally or transvaginally. In the first case, the study is carried out through a sensor that is in contact with the woman's stomach. But due to the fact that in the first trimester the uterine cavity is not yet located close to the abdominal wall, and the fatty layers prevent an objective assessment of the fetal condition, transvaginal ultrasound is more often prescribed at week 11.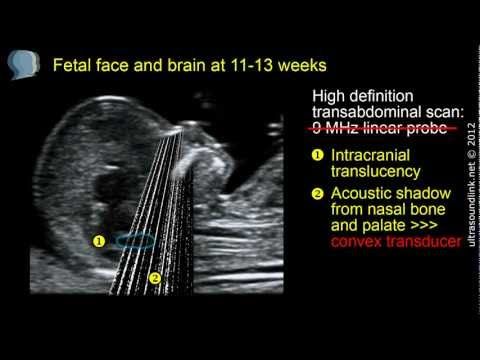
During the examination, the woman is located on the couch, lying on her back, her legs should be bent at the knees. The sensor, on which the condom is previously put on, is inserted into the vagina.
Interpretation of results
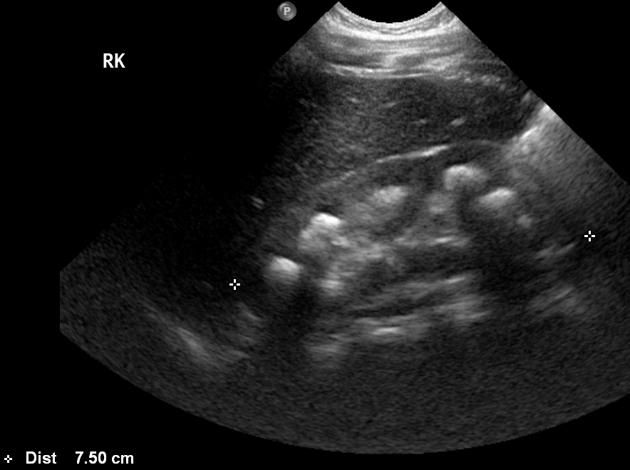
With an ultrasound at the 11th week of pregnancy, you can see how the fetus develops. The torso, head, limbs and even facial features are already distinguishable. The heart, spine, liver are visible. The doctor evaluates the main indicators:
- coccyx-parietal size;
- hip length;
- biparietal head size;
- the length of the nasal bone;
- heart rate;
- collar space thickness;
- the structure of the yolk sac;
- location of the placenta.