Shallow hip sockets in babies
Hip Dysplasia | Boston Children's Hospital
What is hip dysplasia?
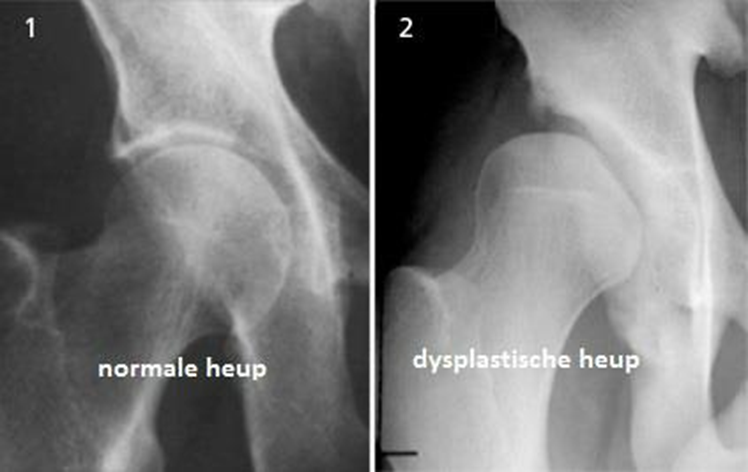
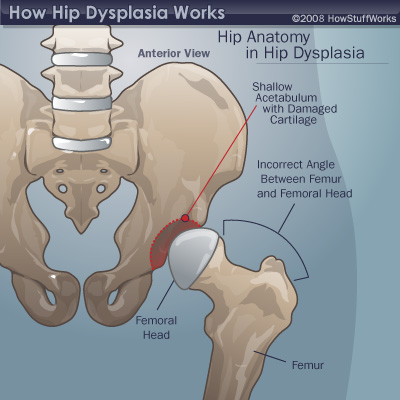
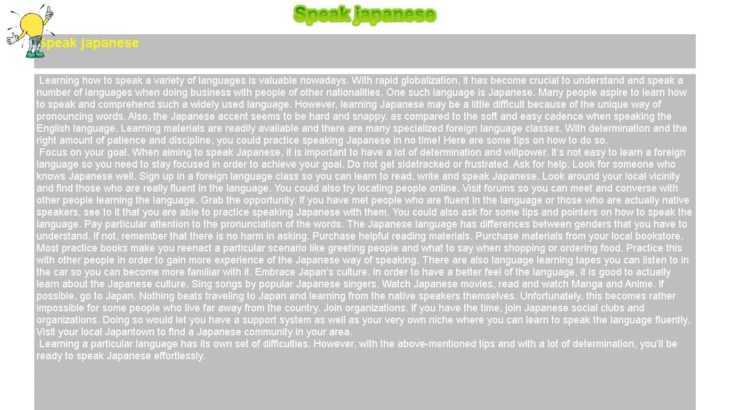
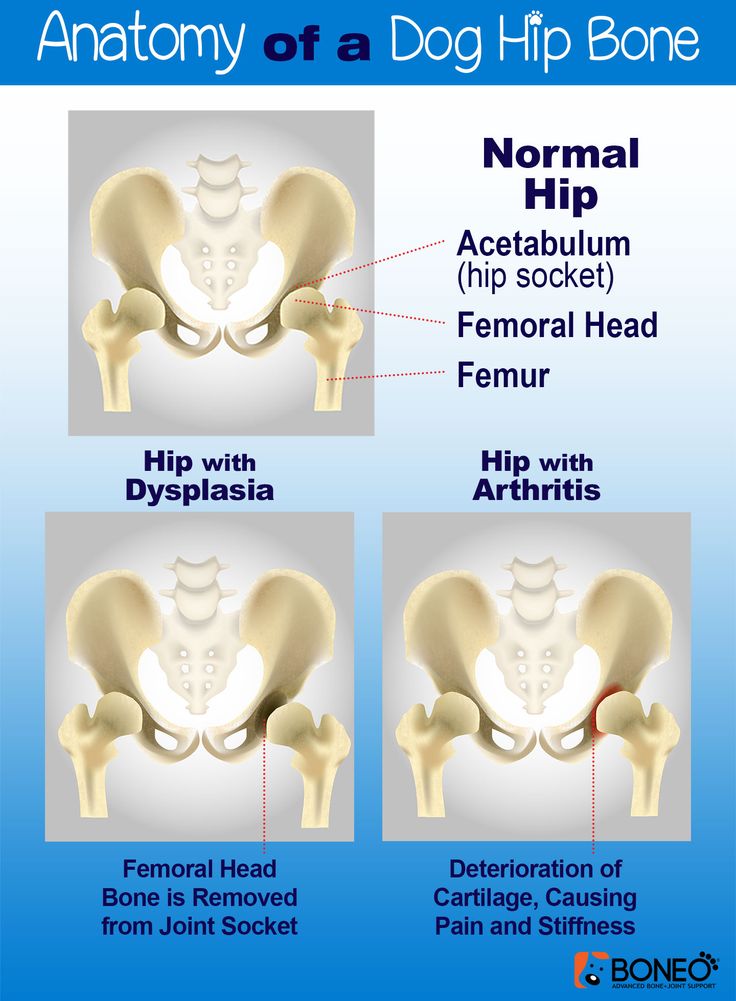
The hip is a ball-and-socket joint. Normally, the ball at the top of the thigh bone fits into the hip socket. Hip dysplasia occurs when the hip joint has not developed properly and the socket (acetabulum) is too shallow. This allows the ball (femoral head) to slip partially or completely out of the joint. Hip dysplasia ranges from a mild abnormality to a complete dislocation of the hip.
Severe cases of hip dysplasia are usually diagnosed during a routine screening within the first few months of a baby’s life. Other times, the problem may only become noticeable as a child grows and becomes more active.
Hip dysplasia is a treatable condition. However, if left untreated, it can cause irreversible damage that will cause pain and loss of function later in life. It is the leading cause of early arthritis of the hip before the age of 60. The severity of the condition and catching it late increase the risk of arthritis. Therefore, monitoring and early intervention are both important to reduce a child’s risk of pain and disability in adulthood.
Who is affected?
Hip dysplasia can affect anyone at any age. Although it is believed to develop around birth, a child with mild dysplasia may not have symptoms for years, or even decades.
- Hip dysplasia in babies is known as infant developmental dysplasia of the hip (DDH).
- When diagnosed in adolescents and young adults, it is sometimes called acetabular dysplasia.
The age at which older kids and young adults with hip dysplasia begin to notice symptoms depend on the severity of the condition and their activity level. Athletes who place a lot of load on their hips by participating in dance, hockey, football, soccer, or track and field may experience symptoms sooner.
Meet Louise
Undiagnosed hip dysplasia caused such severe knee pain, this former track star sometimes had trouble walking after competitions. With surgery behind her, and a degree in medicine in the works, she has returned to the sport she loves.
With surgery behind her, and a degree in medicine in the works, she has returned to the sport she loves.
Read her story
Girls and women are two to four times more likely than boys to have hip dysplasia. It also tends to affect first-born children and those who have a close family member with hip problems. Some people with hip dysplasia are affected in only one hip while others have it in both hips.
In boys, the condition tends to be accompanied by other hip problems. These include acetabular retroversion (when the hip socket grows too far over the head of the femur) or CAM lesions (extra bone growth on the surface of the bone that causes extra friction and joint damage).
Hip dysplasia is sometimes confused with hip impingement, which occurs when extra bone grow on the acetabulum or femoral head. The irregular shape creates friction within the joint and wears down cartilage. Some patients have both conditions, both of which cause hip pain and are easy to confuse. However, they are different issues that require different treatments.
However, they are different issues that require different treatments.
Image
Image
Generally speaking, treating hip dysplasia as early as possible can minimize joint damage and reduce the chance of early onset arthritis.
How we care for hip dysplasia
The Child and Young Adult Hip Preservation Program at Boston Children’s Hospital is at the forefront of research and innovation. We combine specialized expertise in non-surgical and surgical treatments with structured physical therapy to help children, adolescents, and young adults live healthy, active lives.
Our team has treated thousands of children with every level of complexity and severity of hip deformity. Our hip specialists have pioneered minimally invasive procedures as well as open surgical techniques to help treat patients of all ages. We perform more periacetabular osteotomy (PAO) procedures every year than any other hospital in the country and have helped hundreds of athletes return to the activities they love.
We have the experience to treat you or your child. Our goal is the same as yours: to help you get better so you can return to being healthy and pain-free.
Patient resources
Download these fact sheets to learn more about hip dysplasia and treatment options.
- fact sheet: developmental dysplasia of the hip (DDH)
- fact sheet: Pavlik harness
- fact sheet: hip dysplasia in adolescents and young adults
Hip Dysplasia | Hip Dysplasia in Adolescents
What is hip dysplasia in adolescents?
Hip dysplasia occurs when the hip socket (acetabulum) doesn't develop properly and is too shallow to cover the head of the thigh bone (femoral head) completely. Many adolescents and young adults with the condition were born with developmental dysplasia of the hip (DDH). In others, previously healthy hips did not develop properly as their bones and bodies grew.
Meet Alana and Nicole
A year and a half after hip surgery, Nicole still questioned her physical capabilities.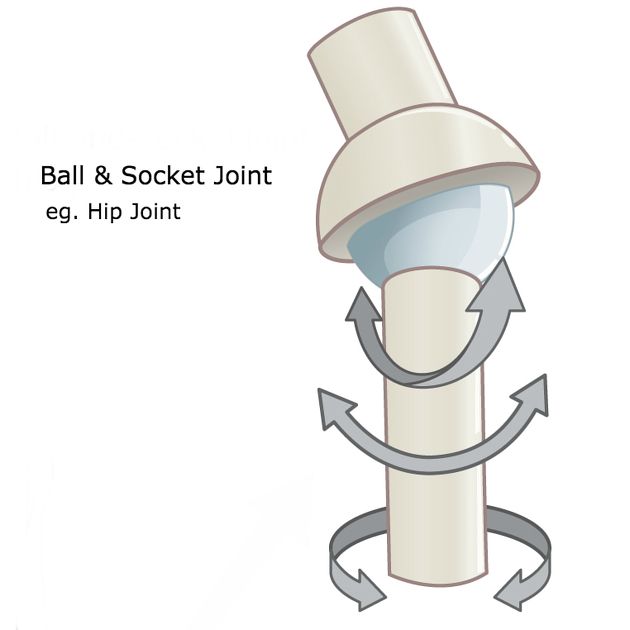 That changed when she met Alana, another dancer who’d had the same surgery. This chance meeting became a turning point in both dancers' healing.
That changed when she met Alana, another dancer who’d had the same surgery. This chance meeting became a turning point in both dancers' healing.
Read their story
The condition ranges from a mild abnormality of the hip socket to a complete dislocation of the hip. As children become more active and demand more of their legs, the ill-fitting hip joint becomes unstable. The instability damages cartilage inside the joint that becomes increasingly painful over time.
It is important not to ignore hip pain. Hip dysplasia is a treatable condition but early diagnosis and treatment are critical to preventing irreversible damage.
What are the symptoms of hip dysplasia in adolescents and young adults?
Teens or young adults may develop a limp or have hip pain in the front of the hip or groin. For others, the first sign is knee pain. You might hear a clicking sound in your hip. As the damage progresses, you may find it more and more painful to participate in sports and other activities. Without treatment, the pain will continue to become worse.
Without treatment, the pain will continue to become worse.
What causes hip dysplasia in adolescents and young adults?
Some teens and young adults are born with mild DDH that becomes symptomatic as they grow. However, the hip joint continues to develop throughout the teen years and sometimes does not develop properly, even if you were not born with DDH. Doctors are not sure why this happens but they do know that the condition affects girls two to four times as often as boys. People with a close relative with hip problems are also at higher risk.
Image
Image
How is hip dysplasia diagnosed in adolescents and young adults?
Doctors typically use variety of tests to determine if dysplasia is the source of hip pain in adolescents and young adults.
The first step is a thorough patient history and physical exam. The doctor will check your hip for range of motion. They may order imaging studies such as an x-ray, MRI, or CT scan to confirm the diagnosis. Ultrasound-guided diagnostic injection can help your doctor determine the location of your hip pain with greater precision.
Ultrasound-guided diagnostic injection can help your doctor determine the location of your hip pain with greater precision.
How is hip dysplasia treated in adolescents and young adults?
The goal of treatment is to restore normal hip function and eliminate pain. Your treatment will depend on the severity of your condition.
Non-surgical treatment options for adolescents and young adults
Mild to moderate cases of hip dysplasia are often treated with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs). If you continue to be in pain after these treatments, your physician may suggest surgery.
Surgical options for adolescents and young adults
Periacetabular osteotomy (PAO) is the main surgical treatment for adolescents and young adults with hip dysplasia. PAO may serve as a lifelong treatment if performed before serious damage occurs within the joint.
The goals of PAO are to:
- reduce or eliminate pain
- maximize the function of your hip
- enable you to return to sport or other activity
Hip Dysplasia | Hip Dysplasia in Babies
What is hip dysplasia in babies?
Hip dysplasia in babies, also known as developmental dysplasia of the hip (DDH), occurs when a baby’s hip socket (acetabulum) is too shallow to cover the head of the thighbone (femoral head) to fit properly. DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
Image
What are the symptoms of hip dysplasia in babies?
Many babies with DDH are diagnosed during their first few months of life.
Common symptoms of DDH in infants may include:
- The leg on the side of the affected hip may appear shorter.
- The folds in the skin of the thigh or buttocks may appear uneven.
- There may be a popping sensation with movement of the hip.
What causes hip dysplasia in babies?
The exact cause is unknown, but doctors believe several factors increase a child’s risk of hip dysplasia:
- a family history of DDH in a parent or other close relative
- gender — girls are two to four times more likely to have the condition
- first-born babies, whose fit in the uterus is tighter than in later babies
- breech position during pregnancy
- tight swaddling with legs extended
Breech position: Babies whose bottoms are below their heads while their mother is pregnant with them often end up with one or both legs extended in a partially straight position rather than folded in a fetal position. Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Tight swaddling: Wrapping a baby’s legs in a straight position may interfere with healthy development of the joint. If you swaddle your baby, you can wrap their arms and torso snugly, but be sure to leave room for their legs to bend and move.
Angela's story
Angela was 5 when her parents brought her to Boston Children’s Hospital, where she was diagnosed with hip dysplasia in both hips.
How is hip dysplasia diagnosed?
Infants in the U.S. are routinely screened for hip dysplasia. During the exam, the doctor will ask about your child’s history, including their position during pregnancy. They’ll also ask if there is any history of hip problems on either parent’s side.
The doctor will do a physical exam and order diagnostic tests to get detailed images of your child’s hip. Typical tests can include:
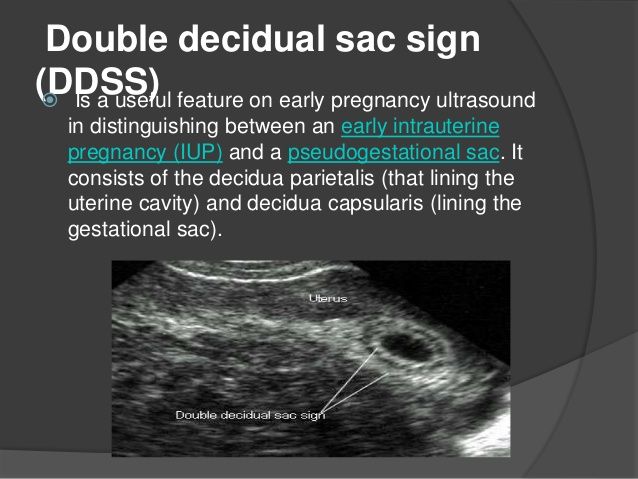
- Ultrasound (sonogram): Ultrasound uses high-frequency sound waves to create pictures of the femoral head (ball) and the acetabulum (socket).
 It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age.
It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age. - X-ray: After a child is 6 months old and bone starts to form on the head of the femur, x-rays are more reliable than ultrasounds.
How is hip dysplasia treated?
Your child’s treatment will depend on the severity of their condition. The goal of treatment is to restore normal hip function by correcting the position or structure of the joint.
Non-surgical treatment options
Observation
If your child is 3 months or younger and their hip is reasonably stable, their doctor may observe the acetabulum and femoral head as they develop. There’s a good possibility the joint will form normally on its own as your child grows.
Pavlik harness
If your child’s hip is unstable or sufficiently shallow, their doctor may recommend a Pavlik harness. The Pavlik harness is used on babies up to four months old to hold their hip in place while allowing their legs some movement. The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
Image
While your child is wearing the harness, their doctor will frequently examine the hip and use imaging tests to monitor its development. After successful treatment, your child will need to continue to see the doctor regularly for the next few years to monitor the development and growth of their hip joint.
Typically, infants’ hips are successfully treated with the Pavlik harness. But some babies’ hips continue to be partially or completely dislocated. If this is the case, your child’s doctor may recommend another type of brace called an abduction brace. The abduction brace is made of lightweight material that supports your child’s hips and pelvis. If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
Image
Surgical treatment options for babies
Closed reduction
If your child’s hip continues to be partially or completely dislocated despite the use of the Pavlik harness and bracing, they may need surgery. Under anesthesia, the doctor will insert a very fine needle in the baby’s hip and inject contrast so they can clearly view the ball and the socket. This test is called an arthrogram.
The process of setting the ball back into the socket after the arthrogram is known as a closed reduction. Once the hip is set in place, technicians will put your child in a spica cast. This cast extends from slightly below the armpits to the legs and holds the hip in place. Different casts cover differing amounts of the child’s legs, based on the condition of their hips. Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Open reduction
If a closed reduction does not work, your child’s doctor may recommend open-reduction surgery. For this, the surgeon makes an incision and repositions the hip so it can grow and function normally. The specifics of the procedure depend on your child’s condition but it may include reshaping the hip socket, redirecting the femoral head, or repairing a dislocation. After the surgery, your child will need to wear a spica cast while they heal.
Follow-up care
Any infant treated surgically for hip dysplasia must be followed periodically by an orthopedist until they have reached physical maturity. At regular visits, their orthopedic doctor will monitor their hip to ensure it develops normally as they grow. Diagnosing and treating any new abnormality early will increase the chance your child will grow up to be active free from hip pain throughout their childhood, the teen years, and adulthood.
Will treatment affect my child’s ability to walk?
Depending on their age during treatment, your child may start walking later than other kids. However, after successful treatment, children typically start walking as well as other kids. By contrast, children with untreated hip dysplasia often start walking later, and many walk with a limp.
Hip Dysplasia | Programs & Services
Departments
Centers
Programs
Hip Dysplasia | Contact Us
Developmental Dysplasia of the Hip (for Parents)
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows. It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around. This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together. Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint.
 This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray. - An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.
Bracing
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.

- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the cartilagepart of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.
- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.

- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.
Childhood hip dysplasia
Contents
Introduction
- Definition
- Epidemiology
- Etiology and pathogenesis
- Risk factors
- Clinical stages
- ICD-10 classification
- Diagnostics
- Treatment
- Forecast
- Output
“Your child was born with hip dysplasia” - this news in the maternity hospital can shock unprepared parents, because a lot of questions immediately arise: “Why does our child have?”, “And this is now forever?”, “What should we do now ? etc. The first thing to do is stop panicking. Hip dysplasia has always existed, in the medical literature it was first described by Hippocrates in the 300s BC. In most cases, the situation is resolved on its own, in others, this will only require the use of special fixing splints, and only a small number of children may require more serious intervention - plastering or surgical treatment.
The first thing to do is stop panicking. Hip dysplasia has always existed, in the medical literature it was first described by Hippocrates in the 300s BC. In most cases, the situation is resolved on its own, in others, this will only require the use of special fixing splints, and only a small number of children may require more serious intervention - plastering or surgical treatment.
Hip dysplasia describes a spectrum of different pathologies in newborns and young children. This includes abnormal development of the acetabulum and proximal femur, as well as mechanical instability of the hip joint. As information accumulated, the terminology changed. Initially, they often talked about congenital dislocation of the hip, but the pathology is not always identified at birth, developing in early childhood, so the definition of "congenital" was abandoned. Further, it turned out that not only dislocation, but also a number of other conditions can be a manifestation of pathology, so that the modern term “hip (or hip) joint dysplasia” was formed as a result.
Estimates of the incidence of hip dysplasia are quite variable and depend on the means of detection, the age of the child, and diagnostic criteria. It is estimated that dislocation of the hip or hips with severe or persistent dysplasia occurs in 3 to 5 children per 1000. Historically, the incidence of hip dysplasia with dislocation has been 1 to 2 per 1000 children. Mild hip instability is more common in neonates, with a reported incidence of up to 40%. However, mild instability and/or mild dysplasia in the neonatal period often resolves on its own without intervention from specialists. Infants with mild instability and/or mild dysplasia during the neonatal period, according to modern concepts, should not be included in the assessment of general morbidity, otherwise there is a distortion that significantly overstates the overall assessment of the prevalence of pathology.
In a prospective study published in the journal Pediatrics, 9,030 infants (18,060 hips) were routinely screened for hip dysplasia by physical examination and ultrasound during the first to third days of life. Ultrasound anomalies were found in 995 joints, the incidence was 5.5%. However, when re-examined at 2 to 6 weeks of age without prior treatment, residual anomalies were found in only 90 hip joints, which ultimately corresponds to the true incidence of dysplasia of 0.5%. It was these children who needed further treatment. In other words, 90% of newborns with clinical or ultrasound evidence of hip dysplasia improved spontaneously between two and six weeks of age to the point where they did not require medical intervention.
Ultrasound anomalies were found in 995 joints, the incidence was 5.5%. However, when re-examined at 2 to 6 weeks of age without prior treatment, residual anomalies were found in only 90 hip joints, which ultimately corresponds to the true incidence of dysplasia of 0.5%. It was these children who needed further treatment. In other words, 90% of newborns with clinical or ultrasound evidence of hip dysplasia improved spontaneously between two and six weeks of age to the point where they did not require medical intervention.
The incidence of hip dysplasia depends to some extent on ethnic factors. It is maximum among the Saami and American Indians (from 25 to 50 cases per 1000 births), minimum - in populations of African and Asian origin.
Both joints are affected in 37% of patients. Among unilateral cases, the left hip is more commonly affected than the right. The predominance of left-sided cases may be due to the typical location of the fetus in the uterus, in which the left thigh is pressed against the mother's sacrum.
Development of the hip joint depends on normal contact between the acetabulum and the femoral head to promote mutual induction. Abnormal development can result from disruption of this contact as a result of a variety of genetic and environmental factors, both prenatal and postnatal.
By the 11th week of pregnancy, the hip joint is usually fully formed. The head of the femur is spherical and is set deep in the acetabulum. However, it grows faster than the socket, so that by the end of pregnancy, the head of the femur is covered by the roof of the acetabulum by less than 50%. During the last four weeks of pregnancy, the femur is vulnerable to mechanical influences, such as adduction, which guide the femoral head away from the central part of the acetabulum. Conditions that limit fetal mobility, including breech presentation, exacerbate these mechanical factors. All this leads to eccentric contact between the femoral head and the acetabulum.
During the neonatal period, ligament weakness makes the developing hip susceptible to other external mechanical influences. A fixed position with extended hips, such as tight swaddling, can result in eccentric hip contact as the femoral head slides in or out of the acetabulum. If these factors persist, abnormal contact of the hip joint leads to structural anatomical changes. If the head of the femur has not entered deep into the acetabulum, the upper lip may turn out and flatten, and the round ligament may elongate. Abnormal ossification of the acetabulum occurs and a shallow variant develops.
Over time, hypertrophy of intra-articular structures occurs, including the upper lip with thickened ridge (neolimbus), round ligament, and fibro-adipose tissue (pulvinar). Contractures develop in the iliopsoas and hip adductors, and the inferior capsule retracts into the empty acetabulum, further reducing the likelihood of transition of the femoral head into the acetabulum. A false acetabulum can form where the head of the femur meets the lateral wall of the pelvis above the true acetabulum. Lack of contact between the femoral head and the acetabulum inhibits further normal development of the hip joint.
Lack of contact between the femoral head and the acetabulum inhibits further normal development of the hip joint.
With or without complete hip dislocation, dysplastic changes may develop. The most common result is a shallow acetabulum with reduced anterior and lateral coverage of the femoral head. There may also be asphericity of the femoral head, valgus angle of the neck and shaft, and persistence of excessive anteversion of the femur.
Dysplasia is more common among infants with certain risk factors (eg, female sex, breech presentation in the third trimester, family history, tight lower extremity swaddling). However, with the exception of females, most infants with a confirmed diagnosis of hip dysplasia do not have any specific risk factors that could be realized.
Female. The risk of dysplasia in girls is estimated at 1.9%. Hip dysplasia occurs in them two to three times more often than in boys. In a 2011 meta-analysis published in the European Journal of Radiology, which evaluated 24 studies and more than 556,000 patients, the relative risk of dysplasia for girls was 2. 5 compared with boys.
5 compared with boys.
Increasing incidence in girls is associated with a temporary increase in ligament laxity associated with increased susceptibility of female infants to the maternal hormone relaxin. However, some studies refute this hypothesis.
The increased incidence of dysplasia in girls is difficult to separate from the increased risk of this condition in breech presentation, which is also significantly more common in girls.
Presentation. Breech and breech presentation during the third trimester is the most significant single risk factor for hip dysplasia in children. The absolute risk of dysplasia is estimated at 12% in breech presentation girls and 2.6% in breech presentation boys. In the already mentioned meta-analysis of risk factors, 15 studies (more than 359300 patients) in presentation, and the relative risk of breech presentation was 3.8. It is not clear in the literature whether the amount of time spent in breech presentation, or the point on the pregnancy timeline at which the fetus was in breech presentation, affects the risk of dysplasia.
An increased risk of dysplasia is present regardless of mode of delivery. However, reducing the time spent in breech presentation by elective caesarean section may reduce the risk of clinically significant hip dysplasia. This was illustrated in a 2019 retrospective review.year, published in the journal Pediatrics & Child Health, which found a reduction in the incidence of dysplasia among children with breech presentation who were born by elective caesarean section (3.7% compared with 6.6% among children born by caesarean section during childbirth, and 8.1% among children born naturally).
Family history. Genetic factors seem to play a role in the development of hip dysplasia in children. The absolute risk in infants with a positive family history is approximately 1 to 4%. In the already mentioned 2011 meta-analysis in the European Journal of Radiology, the authors examined four studies (more than 14,000 patients) on the topic and determined that the relative risk of a positive family history was 1.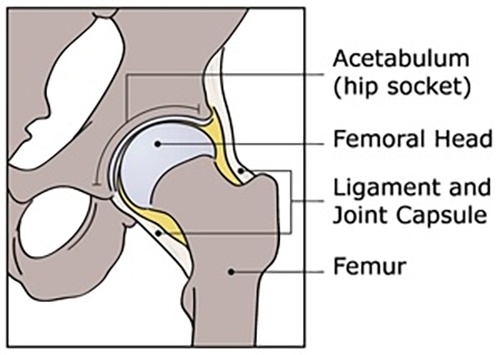 39. If one of the twins has dysplasia, the risk of a similar pathology in the other twin is higher if they are monozygotic than dizygotic (40% versus 3%).
39. If one of the twins has dysplasia, the risk of a similar pathology in the other twin is higher if they are monozygotic than dizygotic (40% versus 3%).
Family members of children with dysplasia are also at increased risk of occult acetabular dysplasia, which often develops before age 30.
Swaddling. The incidence of hip dysplasia is increasing in populations that use diapers and lullaby boards. These practices limit the mobility of the hip joint and fix the hip in adduction and extension, which may play a role in the development of hip dysplasia. In an experimental study in rats, traditional swaddling during hip adduction and extension resulted in a higher incidence of dislocations and dysplasia than no swaddling.
The American Academy of Pediatrics (AAP), the Pediatric Orthopedic Society of North America (POSNA), and the International Hip Dysplasia Institute (IHDI) recommend a “healthy hip swaddle,” also known as “loose swaddling,” that provides enough room for hip and knee flexion and free leg movement.
Other factors. Several other factors associated with decreased mobility or abnormal posture have been found to be associated with pediatric hip dysplasia, but no causal relationship has been proven. These include torticollis, plagiocephaly, adducted metatarsus, clubfoot, first birth, oligohydramnios, birth weight >4 kg, and multiple pregnancies.
Dysplasia in children, depending on the severity of the process, can be divided into the following stages:
Dysplasia. Violation of the shape of the hip joint, usually a shallow acetabulum, in which the upper and anterior edges are affected by the pathological process.
Reductive stage. The femur is dislocated at rest, but the femoral head can be placed into the acetabulum by manipulation, usually flexion and abduction.
Subluxation. The femoral head is in place at rest but may be partially dislocated or subluxated on examination. Joint with slight instability.
Joint with slight instability.
Sliding version. The head of the femur is within the cavity at rest, but easily goes beyond it not only during examination, but also simply when changing position. Joint with instability.
Subluxation. The femoral head partially extends beyond the acetabulum and at rest, but always remains in contact with it.
Dislocation. Complete loss of contact between the femoral head and the acetabulum.
The ICD codes for hip dysplasia in children should be looked up in class Q65, congenital hip deformities. These include the following options:
Q65.0. Congenital hip dislocation unilateral
Q65.1. Congenital hip dislocation bilateral
Q65.2. Congenital dislocation of hip, unspecified
Q65.3. Congenital hip subluxation unilateral
Q65.4. Congenital subluxation of the hip, bilateral
Q65.5. Congenital subluxation of hip, unspecified
Q65. 6. Unstable hip
6. Unstable hip
- Hip dislocation predisposition
- Hip subluxation predisposition
Q65.8. Other congenital deformities of the hip
- Anterior displacement of the femoral neck
- Congenital acetabular dysplasia
- Congenital:
√ valgus position [coxa valga]
√ varus position [coxa vara]
Q65.9. Congenital deformity of the hip, unspecified
General inspection. Neurological examination and examination of the spine and lower legs is important for diagnosis, during which it is looked for associated with hip dysplasia and other causes of its instability.
- The neurologic examination should include assessment of spontaneous movements of all four limbs and an assessment of spasticity.
- Examination of the spine should include range of motion (look for torticollis) and skin manifestations of spinal dysraphism.

- Examination of the limbs should include examination of the foot for the presence of the metatarsal muscle.
Mobility assessment. Results vary by age:
- In infants less than three months old, it is important to assess hip joint stability using the Ortolani maneuver. The Barlow maneuver, the Galeazzi test, and the Klisich test may also be helpful. There are usually no restrictions on joint abduction at this age
- In children older than three months, there may be an obvious discrepancy in the length of the legs (for unilateral cases). The Galeazzi tests for unilateral cases and the Klisich test may be considered better indicators of hip dysplasia than instability.
- In a walking child, weakness of the hip joints on the affected side can be recognized by a positive Tradelenburg test (inability to maintain the pelvis in a horizontal position when standing on the ipsilateral leg), as well as the presence of a Tradelenburg roll when walking.

Ultrasound. Ultrasound is the primary imaging modality for evaluating hip morphology and stability in suspected hip dysplasia. This is an important addition in the clinical evaluation of children under 4–6 months of age. The main drawback of the method is that an experienced and trained diagnostician is needed to accurately interpret the results. Ultrasound criteria for hip dysplasia have been established for both static and dynamic visualization of the flexed hip with and without the modified Barlow tension maneuver.
Radiography. May be useful in diagnosing hip dysplasia in children aged 4-6 months. In younger infants, it is not very informative, since the head of the femur and the acetabulum have not yet ossified and therefore do not contrast in the pictures.
Other imaging modalities. Computed tomography (CT) and magnetic resonance imaging (MRI) are not suitable for diagnosing hip dysplasia in children, but can be used to assess the quality of reposition after surgery. At the same time, special pediatric protocols should be used for CT, providing for a reduction in radiation exposure during the study.
At the same time, special pediatric protocols should be used for CT, providing for a reduction in radiation exposure during the study.
Differential diagnosis. The main pathology from which hip dysplasia in children should be distinguished is also accompanied by shortening of the limb:
- Proximal focal femoral deficiency, a rare congenital disease, the spectrum of which varies from hypoplasia of the femoral head to the absence of everything except the distal epiphysis of the femur .
- Coxa vara, defined by an angle of less than 120° between the femoral neck and the diaphysis, resulting in an elevation of the greater trochanter.
- Hemihypertrophy or hemihyperplasia (eg, Beckwith-Wiedemann syndrome).
- Agenesia of the sacrum with limb deformity.
In the vast majority of cases, hip dysplasia in children stabilizes on its own shortly after birth and does not require any special and separate interventions. In rare cases, with age, there may be a gradual progression of the disease, the appearance of chronic pain and accelerated development of osteoarthritis. The risk of such complications has not been determined, but it may be associated with the formation of a false acetabulum.
In rare cases, with age, there may be a gradual progression of the disease, the appearance of chronic pain and accelerated development of osteoarthritis. The risk of such complications has not been determined, but it may be associated with the formation of a false acetabulum.
The aim of the treatment of hip dysplasia in children is to obtain and maintain concentric contraction of the joint, that is, the alignment of the geometric centers of the femoral head and acetabulum. In young children, concentric reduction provides an optimal environment for the development of the components of the joint, in older children it helps to prevent or delay the development of osteoarthritis of the femoral joint.
The optimal environment for the development of the femoral head and acetabulum is one in which the cartilaginous surface of the femoral head is in contact with the cartilaginous floor of the acetabulum. Both the femoral head and the acetabulum have the ability to grow and reshape, which can lead to gradual resolution of the dysplasia over time (months to years) if concentric contraction is maintained. The upper age limit for acetabular remodeling has been estimated to be 18 months to 11 years, with maximum acetabular remodeling 4–6 years after hip dislocation reposition.
The upper age limit for acetabular remodeling has been estimated to be 18 months to 11 years, with maximum acetabular remodeling 4–6 years after hip dislocation reposition.
0-4 weeks. Dislocation of the hip is rare in children less than four weeks old, but joint weakness (mild instability) and/or a shallow acetabulum (dysplasia) is common. The management of infants less than four weeks of age depends on clinical findings and risk factors. At the same time, retrospective studies have not shown the advantage of starting the use of fixation devices as early as possible, therefore, these children are managed observationally, if necessary, performing follow-up ultrasounds.
4 weeks - 6 months. Various restraint devices are recommended: Pavlik stirrup, Aberdeen splint, Von Rosen splint for infants under six months of age with hip dislocation or permanently dislocated or subluxated joints. In this case, it is better to give preference to Pavlik's stirrups, which are essentially a dynamic splint that prevents hip extension and limits adduction, which can lead to dislocation, but allows flexion and abduction.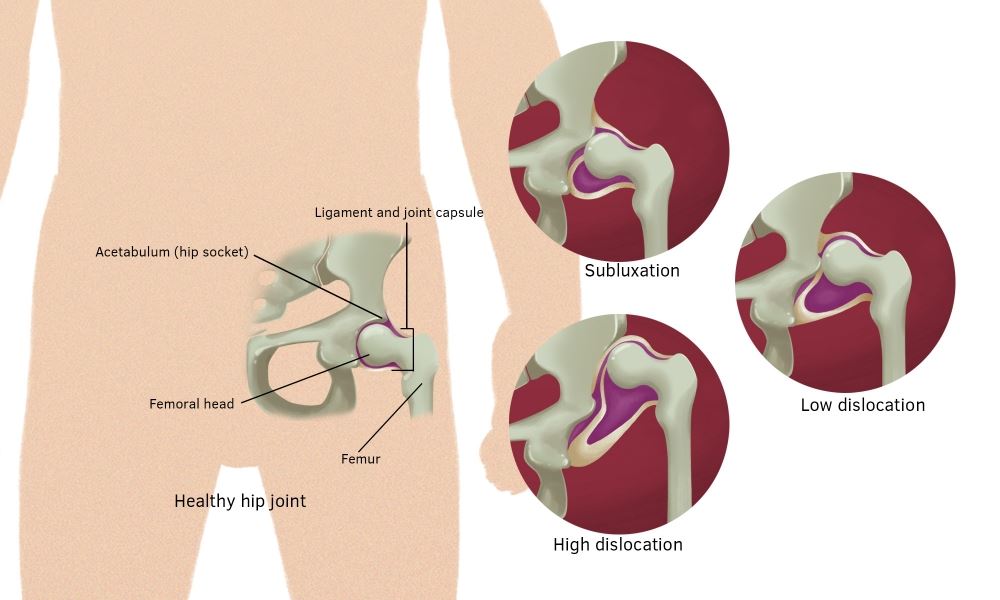 This position contributes to the normal development of the dysplastic joint, stabilization of its subluxation, and usually leads to a gradual reduction in the degree of dislocation, even if the joint does not return to normal on physical examination. It is not recommended to wear double or triple diapers on a child, although this approach was previously practiced. It has proven to be not only ineffective, but also potentially harmful, as it can promote hip extension, which is unfavorable for the normal development of the joint.
This position contributes to the normal development of the dysplastic joint, stabilization of its subluxation, and usually leads to a gradual reduction in the degree of dislocation, even if the joint does not return to normal on physical examination. It is not recommended to wear double or triple diapers on a child, although this approach was previously practiced. It has proven to be not only ineffective, but also potentially harmful, as it can promote hip extension, which is unfavorable for the normal development of the joint.
6-18 months. If the use of fixation devices is unsuccessful, surgical intervention may be undertaken, such as open or closed reduction under anesthesia. Children over six months of age have a less than 50% chance of successful recovery with Pavlik stirrups, and there is a higher risk of osteonecrosis (avascular necrosis) of the femoral head.
Orthopedists at most centers recommend treatment for a dislocated hip soon after diagnosis. The result is influenced by the age of the child and the development of the hip joint at the time of treatment. In observational studies, the earlier an intervention is undertaken, the higher the chance of success for a closed reduction; the older the patient, the greater the likelihood of needing open reduction and possible osteotomy of the femur and pelvis.
In observational studies, the earlier an intervention is undertaken, the higher the chance of success for a closed reduction; the older the patient, the greater the likelihood of needing open reduction and possible osteotomy of the femur and pelvis.
The long-term outcome of treatment depends on the severity of dysplasia, the age of diagnosis and treatment, and the presence of a concentrically reduced hip joint. It is generally accepted that the sooner a patient is treated, the higher the likelihood of a good outcome, which emphasizes the importance of early diagnosis. Approximately 90% of neonatal hips with instability or mild dysplasia resolve spontaneously with normal functional and radiographic findings.
If hip dysplasia is diagnosed before the age of six months, Pavlik stirrup treatment achieves and maintains hip contraction in approximately 95% of patients. Long-term follow-up is important to monitor residual dysplasia, which may occur in up to 20% of patients after successful treatment. Once the hip has stabilized and the patient has recovered from any surgical procedures, annual or biennial follow-up is recommended until skeletal maturity is reached.
Once the hip has stabilized and the patient has recovered from any surgical procedures, annual or biennial follow-up is recommended until skeletal maturity is reached.
Residual dysplasia after treatment or undiagnosed dysplasia may progress to osteoarthritis. Most young people who have undergone hip replacement due to dysplasia have not had
Hip dysplasia in children is a common pathology, but in the vast majority it resolves on its own and does not require special medical intervention. In more complex cases, for several weeks - before the completion of normal formation of the joint - it may be necessary to wear various fixation devices, while neither a cast nor "strict" swaddling is required. In isolated cases, surgery may be required, and the sooner it is performed, the higher the chances of success.
References
- Wedge JH, Wasylenko MJ. The natural history of congenital dislocation of the hip: a critical review // Clin Orthop Relat Res 1978; :154.
- Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip // J Bone Joint Surg Br 1979; 61-B:334.
- Crawford AH, Mehlman CT, Slovek RW. The fate of untreated developmental dislocation of the hip: long-term follow-up of eleven patients // J Pediatr Orthop 1999; 19:641.
- Bialik V, Bialik GM, Blazer S, et al. Developmental dysplasia of the hip: a new approach to incidence // Pediatrics 1999; 103:93.
- Castelein RM, Sauter AJ. Ultrasound screening for congenital dysplasia of the hip in newborns: its value // J Pediatr Orthop 1988; 8:666.
- Terjesen T, Holen KJ, Tegnander A. Hip abnormalities detected by ultrasound in clinically normal newborn infants // J Bone Joint Surg Br 1996; 78:636.
- Marks DS, Clegg J, al-Chalabi AN. Routine ultrasound screening for neonatal hip instability. Can it abolish late-presenting congenital dislocation of the hip? // J Bone Joint Surg Br 1994; 76:534.
- Dezateux C, Rosendahl K.
 Developmental dysplasia of the hip // Lancet 2007; 369:1541.
Developmental dysplasia of the hip // Lancet 2007; 369:1541. - Harris NH, Lloyd-Roberts GC, Gallien R. Acetabular development in congenital dislocation of the hip. With special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy // J Bone Joint Surg Br 1975; 57:46.
- Schwend RM, Pratt WB, Fultz J. Untreated acetabular dysplasia of the hip in the Navajo. A 34 year case series followup // Clin Orthop Relat Res 1999; :108.
- Wood MK, Conboy V, Benson MK. Does early treatment by abduction splintage improve the development of dysplastic but stable neonatal hips? // J Pediatr Orthop 2000; 20:302.
- Shaw BA, Segal LS, SECTION ON ORTHOPAEDICS. Evaluation and Referral for Developmental Dysplasia of the Hip in Infants // Pediatrics 2016; 138.
- Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome // J Bone Joint Surg Am 1995; 77:985.

- Terjesen T. Residual hip dysplasia as a risk factor for osteoarthritis in 45 years follow-up of late-detected hip dislocation // J Child Orthop 2011; 5:425.
- Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip // J Bone Joint Surg Am 1979; 61:112.
- Cherney DL, Westin GW. Acetabular development in the infant's dislocated hips // Clin Orthop Relat Res 1989; :98.
- Brougham DI, Broughton NS, Cole WG, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip // J Bone Joint Surg Br 1988; 70:733.
- Albinana J, Dolan LA, Spratt KF, et al. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures // J Bone Joint Surg Br 2004; 86:876.
- Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: Part II // Instr Course Lect 2004; 53:531.

- US Preventive Services Task Force. Screening for developmental dysplasia of the hip: recommendation statement // Pediatrics 2006; 117:898.
- Lorente Moltó FJ, Gregori AM, Casas LM, Perales VM. Three-year prospective study of developmental dysplasia of the hip at birth: should all dislocated or dislocatable hips be treated? // J Pediatr Orthop 2002; 22:613.
- Larson JE, Patel AR, Weatherford B, Janicki JA. Timing of Pavlik harness initiation: Can we wait? // J Pediatr Orthop 2017.
- Flores E, Kim HK, Beckwith T, et al. Pavlik harness treatment may not be necessary for all newborns with ultrasonic hip dysplasia // J Pediatr Health Care 2016; 30:304.
- Rosendahl K, Dezateux C, Fosse KR, et al. Immediate treatment versus sonographic surveillance for mild hip dysplasia in newborns // Pediatrics 2010; 125:e9.
- Burger BJ, Burger JD, Bos CF, et al. Frejka pillow and Becker device for congenital dislocation of the hip. Prospective 6-year study of 104 late-diagnosed cases // Acta Orthop Scand 1993; 64:305.

- Atar D, Lehman WB, Tenenbaum Y, Grant AD. Pavlik harness versus Frejka splint in treatment of developmental dysplasia of the hip: bicenter study // J Pediatr Orthop 1993; 13:311.
- Danielsson L, Hansson G, Landin L. Good results after treatment with the Frejka pillow for hip dysplasia in newborn infants: a 3-year to 6-year follow-up study // J Pediatr Orthop B 2005; 14:228.
- Czubak J, Piontek T, Niciejewski K, et al. Retrospective analysis of the non-surgical treatment of developmental dysplasia of the hip using Pavlik harness and Frejka pillow: comparison of both methods // Ortop Traumatol Rehabil 2004; 6:9.
- Carmichael KD, Longo A, Yngve D, et al. The use of ultrasound to determine timing of Pavlik harness discontinuation in treatment of developmental dysplasia of the hip // Orthopedics 2008; 31.
- Tiruveedhula M, Reading IC, Clarke NM. Failed Pavlik harness treatment for DDH as a risk factor for avascular necrosis // J Pediatr Orthop 2015; 35:140.
- Hedequist D, Kasser J, Emans J. Use of an abduction brace for developmental dysplasia of the hip after failure of Pavlik harness use // J Pediatr Orthop 2003; 23:175.
- Cashman JP, Round J, Taylor G, Clarke NM. The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up // J Bone Joint Surg Br 2002; 84:418.
- Nakamura J, Kamegaya M, Saisu T, et al. Treatment for developmental dysplasia of the hip using the Pavlik harness: long-term results // J Bone Joint Surg Br 2007; 89:230.
- Walton MJ, Isaacson Z, McMillan D, et al. The success of management with the Pavlik harness for developmental dysplasia of the hip using a United Kingdom screening program and ultrasound-guided supervision // J Bone Joint Surg Br 2010; 92:1013.
- Lerman JA, Emans JB, Millis MB, et al. Early failure of Pavlik harness treatment for developmental hip dysplasia: clinical and ultrasound predictors // J Pediatr Orthop 2001; 21:348.

- Kitoh H, Kawasumi M, Ishiguro N. Predictive factors for unsuccessful treatment of developmental dysplasia of the hip by the Pavlik harness // J Pediatr Orthop 2009; 29:552.
- Ömeroğlu H, Köse N, Akceylan A. Success of Pavlik Harness Treatment Decreases in Patients ≥ 4 Months and in Ultrasonographically Dislocated Hips in Developmental Dysplasia of the Hip // Clin Orthop Relat Res 2016; 474:1146.
- Eidelman M, Katzman A, Freiman S, et al. Treatment of true developmental dysplasia of the hip using Pavlik's method // J Pediatr Orthop B 2003; 12:253.
- Bialik GM, Eidelman M, Katzman A, Peled E. Treatment duration of developmental dysplasia of the hip: age and sonography // J Pediatr Orthop B 2009; 18:308.
- Murnaghan ML, Browne RH, Sucato DJ, Birch J. Femoral nerve palsy in Pavlik harness treatment for developmental dysplasia of the hip // J Bone Joint Surg Am 2011; 93:493.
- Hart ES, Albright MB, Rebello GN, Grottkau BE. Developmental dysplasia of the hip: nursing implications and anticipatory guidance for parents // Orthop Nurs 2006; 25:100.

- Hassan F.A. Compliance of parents with regard to Pavlik harness treatment in developmental dysplasia of the hip // J Pediatr Orthop B 2009; 18:111.
- Kosar P, Ergun E, Gökharman FD, et al. Follow-up sonographic results for Graf type 2A hips: association with risk factors for developmental dysplasia of the hip and instability // J Ultrasound Med 2011; 30:677.
- Luhmann SJ, Bassett GS, Gordon JE, et al. Reduction of a dislocation of the hip due to developmental dysplasia. Implications for the need for future surgery // J Bone Joint Surg Am 2003; 85-A:239.
- Holman J, Carroll KL, Murray KA, et al. Long-term follow-up of open reduction surgery for developmental dislocation of the hip // J Pediatr Orthop 2012; 32:121.
- Rampal V, Sabourin M, Erdeneshoo E, et al. Closed reduction with traction for developmental dysplasia of the hip in children aged between one and five years // J Bone Joint Surg Br 2008; 90:858.
- Carney BT, Clark D, Minter CL.
 Is the absence of the ossific nucleus prognostic for avascular necrosis after closed reduction of developmental dysplasia of the hip? // J Surg Orthop Adv 2004; 13:24.
Is the absence of the ossific nucleus prognostic for avascular necrosis after closed reduction of developmental dysplasia of the hip? // J Surg Orthop Adv 2004; 13:24. - Segal LS, Boal DK, Borthwick L, et al. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus // J Pediatr Orthop 1999; 19:177.
- Chen C, Doyle S, Green D, et al. Presence of the Ossific Nucleus and Risk of Osteonecrosis in the Treatment of Developmental Dysplasia of the Hip: A Meta-Analysis of Cohort and Case-Control Studies // J Bone Joint Surg Am 2017; 99:760.
- Gould SW, Grissom LE, Niedzielski A, et al. Protocol for MRI of the hips after spica cast placement // J Pediatr Orthop 2012; 32:504.
- Desai AA, Martus JE, Schoenecker J, Kan JH. Spica MRI after closed reduction for developmental dysplasia of the hip // Pediatr Radiol 2011; 41:525.
- Tiderius C, Jaramillo D, Connolly S, et al. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report // J Pediatr Orthop 2009; 29:14.
- Aksoy MC, Ozkoç G, Alanay A, et al. Treatment of developmental dysplasia of the hip before walking: results of closed reduction and immobilization in hip spica cast // Turk J Pediatr 2002; 44:122.
- Murray T, Cooperman DR, Thompson GH, Ballock T. Closed reduction for treatment of development dysplasia of the hip in children // Am J Orthop (Belle Mead NJ) 2007; 36:82.
- Senaran H, Bowen JR, Harcke HT. Avascular necrosis rate in early reduction after failed Pavlik harness treatment of developmental dysplasia of the hip // J Pediatr Orthop 2007; 27:192.
- Moseley CF. Developmental hip dysplasia and dislocation: management of the older child // Instr Course Lect 2001; 50:547.
- Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH // J Pediatr Orthop 2013; 33:714.
- Sewell MD, Rosendahl K, Eastwood DM. Developmental dysplasia of the hip // BMJ 2009; 339:b4454.
- Kamath SU, Bennet GC.
 Re-dislocation following open reduction for developmental dysplasia of the hip // Int Orthop 2005; 29:191.
Re-dislocation following open reduction for developmental dysplasia of the hip // Int Orthop 2005; 29:191. - Wada A, Fujii T, Takamura K, et al. Pemberton osteotomy for developmental dysplasia of the hip in older children // J Pediatr Orthop 2003; 23:508.
- Ertürk C, Altay MA, Yarimpapuç R, et al. One-stage treatment of developmental dysplasia of the hip in untreated children from two to five years old. A comparative study // Acta Orthop Belg 2011; 77:464.
- Subasi M, Arslan H, Cebesoy O, et al. Outcome in unilateral or bilateral DDH treated with one-stage combined procedure // Clin Orthop Relat Res 2008; 466:830.
- Sarkissian EJ, Sankar WN, Zhu X, et al. Radiographic Follow-up of DDH in Infants: Are X-rays Necessary After a Normalized Ultrasound? // J Pediatr Orthop 2015; 35:551.
- Engesaeter IØ, Lie SA, Lehmann TG, et al. Neonatal hip instability and risk of total hip replacement in young adulthood: follow-up of 2,218.596 newborns from the Medical Birth Registry of Norway in the Norwegian Arthroplasty Register // Acta Orthop 2008; 79:321.
- Carroll KL, Schiffern AN, Murray KA, et al. The Occurrence of Occult Acetabular Dysplasia in Relatives of Individuals With Developmental Dysplasia of the Hip // J Pediatr Orthop 2016; 36:96.
Latest Articles
10/11/2022
Diagnosis of disorders in the coagulation system, assessment of the risk of hemorrhagic complications in severe cirrhosis/liver diseases according to global screening tests of the hemostasis system and principles for their correction: guidelines
10.10.2022
Features of eating behavior in women: risk assessment of complications
09/29/2022
How to treat sinusitis in adults?
09/28/2022
Symptoms of perforation of the tympanic membrane
27. 09.2022
09.2022
Choan atresia
09/26/2022
How to treat SARS?
Hip dysplasia in children G. I. Turner develop and apply modern methods for the treatment of pathologies of the hip joints in children. Specialists deal with the most non-standard and serious cases, treat children not only from all regions of the country, but also from foreign countries.
Surgical treatment is carried out according to federal quotas as part of the provision of specialized and high-tech medical care, which is free of charge for patients under 18 years of age from any regions of Russia.
Employees of the only specialized department of hip joint pathology NMRC DTO named after. G.I. Turner successfully apply modern methods of conservative and surgical treatment of children with hip dysplasia of varying severity.
- According to international studies and statistics from our Center, 5-10 children per 1000 newborns suffer from this congenital pathology.
- The disease affects girls about 7 times more often than boys. Unilateral lesion occurs 1.5-2 times more often than bilateral.
- This pathology is the cause of every third case of coxarthrosis in adults.
What is hip dysplasia?
Hip dysplasia is a severe pathology characterized by underdevelopment of all elements of the hip joint (bones, ligaments, joint capsule, muscles, blood vessels, nerves).
The modern name for this pathology is Developmental dysplasia of the hip. developmental dysplasia of the hip joint, which occurs in the process of pre- and postnatal ontogenesis and may include neonatal instability, isolated underdevelopment of the acetabulum, subluxation and dislocation of the hip - the most severe degree of hip dysplasia, which is characterized by complete disconnection of the contact of the articular surfaces of the femoral head and acetabulum.
Classification and assessment of the condition of the hip joint
The condition of the hip joints is assessed on the basis of ultrasound and X-ray data. Ultrasound screening is carried out according to the method of R.Graf (1984)
The main advantages of ultrasound screening:
- The earliest possible diagnosis of hip joint pathology (the “gold standard” of conducting is in the maternity hospital)
- Reduction of terms of conservative treatment!!!
- A significant reduction in the likelihood of surgical interventions!
- No exposure
There are several types of hip joint structure, according to R.Graf evaluation criteria:
type 1a – mature hip joint
type 1b – transient – usually requires orthopedic treatment and does not require 905
2a type - immature hip joint. In children under 3 months of age, this type is regarded as functional immaturity and does not require orthopedic treatment; in children older than 3 months, such changes are considered pathological immaturity and require treatment, and the type itself is 2b
2c - hip subluxation
3 - hip subluxation
4 - hip dislocation
X-rays are performed in children older than 3 months in addition to ultrasound. Before this age, radiological research methods are not informative, since there is no proper ossification of the bone structures of the hip joint and their adequate assessment is extremely difficult.
Before this age, radiological research methods are not informative, since there is no proper ossification of the bone structures of the hip joint and their adequate assessment is extremely difficult.
Today, in the world practice, the degree of hip dysplasia is determined according to the data of X-ray examination according to the classification developed by the International Institute of Hip Dysplasia (International Hip Dysplasia Institute), which is based on the relationship between the femoral head and the acetabulum.
- First degree - hip joint without pathology
- Second degree (femoral subluxation) - the head of the femur is displaced cranially, but is below the upper-lateral edge of the true acetabulum
- Third degree (marginal dislocation of the hip) - the head of the femur is displaced cranially and is located at the level of the upper-lateral edge of the true acetabulum
- Fourth degree (supraacetabular dislocation of the hip) - the head of the femur is located above the upper-lateral edge of the true acetabulum
Main risk factors for occurrence:
- Heredity for congenital pathology of the hip joint
- Breech presentation
- Female
- First birth
- Large fruit (more than 4 kg)
- Viral or bacterial infection between 10 and 15 weeks of gestation
- Chronic diseases of the pelvic organs
Signs and symptoms of hip dysplasia
Symptoms of severe degrees of dysplasia (subluxation and dislocation) are pronounced in babies. To exclude the diagnosis, the child should be examined by a pediatric orthopedist for the purpose of prevention. The “golden” standard for diagnosis is the maternity hospital! In the first year of life, an orthopedic examination is performed at 1, 3, 6 and 12 months.
To exclude the diagnosis, the child should be examined by a pediatric orthopedist for the purpose of prevention. The “golden” standard for diagnosis is the maternity hospital! In the first year of life, an orthopedic examination is performed at 1, 3, 6 and 12 months.
Main specific clinical signs in a child 1-2 months old
- Barlow test and Ortolani test
Additional (low specific) clinical signs
- Asymmetric skin folds on the thighs
- Asymmetric gluteal folds
- Excessive hip rotation
- Foot External Rotation
- Oblique location of the genital slit in girls.
- Shortening of the lower limb
- Palpation of the femoral head behind the posterior edge of the socket
- Restriction of abduction of legs bent at right angles at the hip and knee joints
Diagnostics
Vissarionov Sergey ValentinovichVissarionov Sergey Valentinovich (Director of the National Research Center for Pediatric Traumatology and Orthopedics named after G.
I. Turner, Doctor of Medical Sciences, Professor, Corresponding Member of the Russian Academy of Sciences, laureate of the Prize of the Government of the Russian Federation)
We are currently focusing on the development of an innovative system for early diagnosis of hip dysplasia in infants and early functional conservative treatment. Our institution has developed a functional splint for the treatment of children with this pathological condition, which is being manufactured and is already used in the complex treatment of children with hip dysplasia.
The Hip Pathology Clinic of our center deals with the treatment of pathologies and dysplasia of the hip joints in newborns, children and adolescents.
A preliminary diagnosis is often made during the stay in the hospital. In such a situation, it is important to visit a pediatric orthopedist in the next three weeks. Necessary diagnostic procedures are radiography and ultrasonography.