Pregnancy and birthing
What happens to your body during childbirth
Childbirth is challenging and complications occur, but women's bodies are designed to give birth. The shape of the pelvis, hormones, powerful muscles and more all work together to help you bring your baby into the world - before, during and after childbirth.
How your body prepares for labour
Here are some of the ways your body will prepare both you and your baby for the birth ahead.
Braxton Hicks contractions
In the weeks or days before you start having proper contractions, you may experience Braxton Hicks contractions. This is your uterus tightening then relaxing. These contractions don't usually hurt and are thought to help your uterus and cervix get ready for labour.
Braxton Hicks contractions may become more regular as you get closer to the time of birth, but unlike labour contractions, they don't change the shape of the cervix and are sometimes referred to as 'false labour'. Your midwife can tell you if you're experiencing Braxton Hicks contractions or if you are in labour by doing a vaginal examination to look at your cervix.
Changes to the cervix
As labour gets closer, your cervix softens and becomes thinner, getting ready for the dilation (widening) that will allow the baby to enter the vagina. You may also see a 'show', which is a pinkish plug of mucus, stained with blood.
Engagement
Your baby may move further down your pelvis as the head engages, or sits in place over your cervix, ready for the birth. Some women feel they have more room to breathe after the baby has moved down. This is called 'lightening'.
Rupture of the membranes, or 'waters breaking'
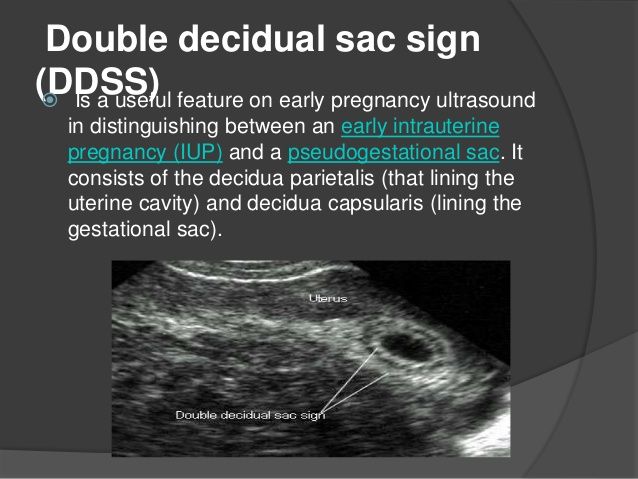
Some women find the sac of amniotic fluid containing the baby breaks before labour, contractions start and the fluid runs (or gushes) out of the vagina. This is referred to as rupture of the membranes, or 'waters breaking'.
Let your maternity team know when your waters have broken and take notice of the colour of the fluid. It is usually light yellow. If it is green or red, tell your maternity team since this could mean the baby is having problems.
If your waters have broken but you have not started having regular contractions within 24 hours, you may need your labour to be induced because there is a risk of infection. Your midwife or doctor will talk to you about this.
How will you know when labour has started?
Movies often show women suddenly being struck by painful contractions and rushing to hospital. In real life, many women are not sure if they have actually started their labour.
You may feel restless, have back pain or period-like pain, or stomach disturbances such as diarrhoea.
Labour officially begins with contractions, which start working to open up the cervix. You should phone your midwife when your contractions start, although you probably won't be encouraged to come to the hospital or birthing centre until your contractions are closer together.
In preparation for labour, your baby may move further down your pelvis as the head engages, or sits in place over your cervix.How the pelvis is designed for childbirth
Your pelvis is located between your hip bones. Women typically have wider, flatter pelvises than men, as well as a wider pelvic cavity (hole) to allow a baby to pass through.
Women typically have wider, flatter pelvises than men, as well as a wider pelvic cavity (hole) to allow a baby to pass through.
The organs sitting in a woman's pelvis include the uterus, cervix and vagina, which are held together by a group of muscles. During childbirth, the muscles at the top of your uterus press down on the baby's bottom. Your baby's head then presses on your cervix which, along with the release of the hormone oxytocin (see 'How hormones help you give birth', below), brings on contractions. Your cervix should dilate so your baby can pass through it.
Your pelvis has bones and ligaments that move or stretch as the baby travels into the vagina. Your baby also has spaces between the skull bones called 'sutures', and the gaps where the sutures meet on the skull are called fontanelles. This allows for the baby's head to mould as the skull bones meet or overlap, allowing it to fit more easily as it travels through your pelvis.
How hormones help you give birth
Your body produces hormones that trigger changes in your body before, during and after childbirth. Here's how they work to help you deliver your baby.
Here's how they work to help you deliver your baby.
- Prostaglandin Before childbirth, a higher level of prostaglandin will help open the cervix and make your body more receptive to another important hormone, oxytocin.
- Oxytocin This hormone causes contractions during labour, as well as the contractions that deliver the placenta after the baby is born. These post-birth contractions, including more that can occur during breastfeeding, help your uterus shrink back to its normal size. Oxytocin and prolactin are the two main hormones that produce and let down breast milk for your baby. Skin-to-skin contact between a mother and baby helps to release more of these hormones.
- Relaxin The hormone relaxin helps soften and stretch the cervix for birth, while helping your waters break and stretching the ligaments in your pelvis to allow the baby to come through.
- Beta-endorphins During childbirth, this type of endorphin helps with pain relief and can cause you to feel joyful or euphoric.

- 'Baby blues' After birth, your hormone balance can change again, and this is believed to cause the ‘baby blues’ in some women. You may feel teary, anxious and irritable and your mood can go up and down.
When childbirth doesn’t go to plan
Sometimes, complications can occur before or during childbirth that mean things don’t go as expected.
Sometimes, labour needs to be induced or started. There are a few ways to induce labour, including the mother being offered synthetic prostaglandin. This is inserted into the vagina to soften the cervix and start contractions.
If contractions slow down or stop during labour, the mother may be offered synthetic oxytocin from a drip to increase the contractions. In both these cases contractions can come on strongly and more pain relief may be needed. Your maternity team should explain the benefits and risks of this with you before you agree to it.
The baby could be in a posterior or breech position, not ideally placed above the cervix before the birth. Your maternity team may need to use forceps or a vacuum to help turn the baby or help the baby travel out of the vagina. Sometimes a caesarean is needed.
Your maternity team may need to use forceps or a vacuum to help turn the baby or help the baby travel out of the vagina. Sometimes a caesarean is needed.
In rare cases, a mother may experience cephalopelvic disproportion (CPD), which is when the baby’s head is too big to fit through the pelvis. A diagnosis of CPD is usually made when labour hasn’t progressed and synthetic oxytocin has not helped. A caesarean is usually the next step.
More information
If you have any questions about childbirth or pregnancy, you can call Pregnancy, Birth and Baby on 1800 882 436, 7 days a week, to speak to a maternal health nurse.
Learn more here about the development and quality assurance of healthdirect content.
Giving birth - stages of labour
Giving birth - stages of labour | Pregnancy Birth and Baby beginning of content5-minute read
Listen
Why is labour defined in stages?
While every labour is different, there are 3 distinct stages that can help describe the process of labour and childbirth. Some people consider the recovery period to be a fourth stage.
Some people consider the recovery period to be a fourth stage.
Defining labour in stages can help your health team know how far along you are, communicate with each other and prepare for what you and your baby need before during and after birth.
These stages all have defining features, such as the length of your contractions and the time between them. However, because every labour is different, it can be difficult for you to know exactly what stage of labour you are in. Your midwife can help you to understand what stage you are going through at any point.
The first stage
The first stage of labour is broken down into three phases.
The first phase of the first stage of labour is called the latent phase. This is the longest phase and can last for many hours or even days. Your cervix becomes thinner and begins to open (dilate) to around 4–6 centimetres in preparation for birth. During this phase, you may have regular or irregular contractions, although they are normally not painful. Some women may not notice their contractions during this phase, since they can be very mild. You can usually stay at home during this phase of labour. Try to rest and relax by doing gentle stretches or by practising mindfulness, meditation or other calming techniques.
Some women may not notice their contractions during this phase, since they can be very mild. You can usually stay at home during this phase of labour. Try to rest and relax by doing gentle stretches or by practising mindfulness, meditation or other calming techniques.
The second phase of the first stage of labour is called the active phase. This is when your cervix dilates up to around 8 centimetres. During this phase, your contractions will become stronger and more regular. During this phase, your contractions may be around 3 or 4 minutes apart, with each contraction lasting between 30 to 60 seconds. Most women choose to come to a hospital or birthing centre during this phase.
The third phase of first stage of labour is called the transition phase. During this phase, your cervix becomes fully dilated, meaning that there is an opening of 10 centimetres for your baby to pass through. Towards the end of the first stage of labour, your contractions will become stronger, and you may feel pressure in your bottom or a sensation like you need to go to the toilet. This is caused by your baby pressing on your rectum.
This is caused by your baby pressing on your rectum.
The second stage
Once your cervix is fully dilated, the second stage of labour begins. During the second stage of labour, your uterus contracts powerfully, although your contractions may become more spaced out, to give your body a chance to rest in between. You will need to work with your body to push your baby, and out into the world.
You may feel an urge to push to help your baby be born. This is because the baby’s head is pressing down on your pelvic area. The second stage of labour can last for up to 2 hours, but it can be much quicker than this if this is not your first baby.
The second stage of labour can be painful as well as emotional for you and your partner or support person. There are several different ways to manage pain during this stage, including with medicines and non-medical treatment. It can be helpful to think ahead and discuss your ideas about pain relief with your doctor or midwife during a prenatal visit to make sure that they will be suitable for your circumstances.
The third stage
After your baby is born, the third stage of labour begins. During this stage, the placenta and the membranes that surrounded your baby in your uterus are delivered. Your midwife may ask you to push gently to help with this. You may feel contractions during this stage, but they will not be as strong as the contractions you experienced while birthing your baby.
During this stage of labour, the umbilical cord, which connected your baby to your placenta, is clamped and cut. If you would like the umbilical cord to be left intact, or to be clamped later, you should let your midwife know ahead of time so that they can arrange this. If your birth partner would like to cut the cord, talk to your midwife and add it to your birth plan.
Recovery stage
After labour is complete, you will be able to rest, meet your baby and begin to recover your strength. The midwives in the postnatal ward or birthing centre will monitor you during your recovery, including by checking your pulse rate, blood pressure and temperature. They will feel your abdomen to check the top of your uterus and check that it has started to contract back. They will also look at your perineum to check for bruising and to make sure that you are not bleeding excessively.
They will feel your abdomen to check the top of your uterus and check that it has started to contract back. They will also look at your perineum to check for bruising and to make sure that you are not bleeding excessively.
Some hospitals or birthing units have a counselling or debriefing service for new mothers and their partners to check on emotional wellbeing after the birth. This is especially important if your labour did not go as expected, or if your baby needs any special care. You can also call Pregnancy, Birth and Baby, 7 days a week on 1800 882 436 to speak with a maternal child health nurse if you have any questions or concerns, or would like to talk with someone about your birth experience.
Listen to our podcast on understanding your choices when having a baby.
Sources:
Royal Women's (Stages of labour), Queensland government (Stages of Labour- The First Stage of Labour), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Queensland government (Stages of Labour - The Third Stage of Labour)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2022
Back To Top
Related pages
- Giving birth - third stage of labour
- Giving birth - second stage of labour
- Giving birth - first stage of labour
- Giving birth - waters breaking
- Giving birth - contractions
Need more information?
Giving birth - first stage of labour
Find out what happens during the first stage of labour.
Read more on Pregnancy, Birth & Baby website
Giving birth - third stage of labour
The third stage of labour is immediately after the birth of your child.
Read more on Pregnancy, Birth & Baby website
Giving birth - second stage of labour
The second stage of labour is when you give birth to your baby.
Read more on Pregnancy, Birth & Baby website
Slow progress in labour
Slow progress in labour (also known as failure to progress in labour or prolonged labour) occurs when labour doesn’t go as quickly as expected. Your doctor may need to intervene to help you have your baby.
Read more on Pregnancy, Birth & Baby website
Induced labour
Induced labour is a medical treatment to start labour. It may be recommended if your baby needs to be born before labour is due to start naturally.
Read more on Pregnancy, Birth & Baby website
Labour and birth using water
Information to help you make an informed choice for you and your baby about using water during the first stage of your labour or having a waterbirth.
Read more on WA Health website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after the baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Shoulder dystocia
Shoulder dystocia happens when a baby's shoulder gets stuck behind the mother’s pubic bone during birth. It is a medical emergency that requires immediate intervention. Find out why here.
Read more on Pregnancy, Birth & Baby website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Positions for labour and birth
Choosing your own positions for labour and giving birth can help you feel in control, reduce pain and open your pelvis to help the baby come out. Find out more.
Find out more.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
1st, 2nd and 3rd trimester
During the period of carrying a baby, the expectant mother carefully monitors her well-being, worrying, first of all, about the health of the fetus.
Important!
To avoid groundless worries, a woman should know which symptoms are quite normal for pregnancy or, on the contrary, pose a danger to both her and the child. Acquaintance with relevant literature or conversations with specialists will be especially useful for girls who are preparing to become a mother for the first time.
Acquaintance with relevant literature or conversations with specialists will be especially useful for girls who are preparing to become a mother for the first time.
A woman already has her own experience with a second pregnancy. She can compare her feelings, catch possible deviations from the norm.
Well-being during pregnancy depends on the age of the expectant mother, on the initial state of her health and even on the sex of the child (although the latter statement has not been scientifically proven and is in the nature of a sign). A young girl without malformations and chronic ailments will more easily endure pregnancy. And qualified specialists will help a woman with certain diseases to give birth to a healthy baby.
Despite the fact that bearing a child is a unique and highly individual process, there are a number of characteristic features in the state of health at different stages of pregnancy:
- The first trimester is often accompanied by some emotional instability of the expectant mother.
 At the same time, her general well-being is characterized by weakness and drowsiness. A rare woman in the first trimester bypasses toxicosis: its mild degree in the form of morning sickness is a completely expected phenomenon.
At the same time, her general well-being is characterized by weakness and drowsiness. A rare woman in the first trimester bypasses toxicosis: its mild degree in the form of morning sickness is a completely expected phenomenon. - The second trimester of pregnancy is considered the most comfortable and carefree. The expectant mother will soon feel the timid movements of her baby. Her appetite is noticeably improving.
- Pregnancy in the third trimester, approaching its end, brings a number of physical difficulties due to a significant increase in the size of the uterus. The psychological well-being of the expectant mother is characterized by a balance of two processes - the fear of childbirth and the anticipation of the joy of the upcoming meeting with the baby.
Feeling well in the first trimester of pregnancy
Shortly after conception, a kind of revolutionary transformation of the hormonal background takes place in the body of a woman. The endocrine system of the mother tries to create the most favorable conditions for the intrauterine development of the fetus. A woman's well-being during pregnancy, especially in the first trimester, changes primarily under the influence of progesterone - the ovaries begin to actively synthesize this hormone after fertilization. Thanks to progesterone, the vessels that feed the pelvic organs expand. Thus, the flow of oxygen and nutrients to the embryo improves, and other organs of the expectant mother find themselves in a somewhat deprived position.
A woman's well-being during pregnancy, especially in the first trimester, changes primarily under the influence of progesterone - the ovaries begin to actively synthesize this hormone after fertilization. Thanks to progesterone, the vessels that feed the pelvic organs expand. Thus, the flow of oxygen and nutrients to the embryo improves, and other organs of the expectant mother find themselves in a somewhat deprived position.
Important!
The redistribution of blood in a woman's body in the first trimester of pregnancy leads to a slight drop in blood pressure, which may cause increased drowsiness, absent-mindedness, fatigue and general weakness.
In the early stages of bearing a child, a woman's well-being can be overshadowed by toxicosis of varying severity - from mild nausea to persistent vomiting in response to food intake or certain odors. Experts will help to cope with malaise by recommending fractional meals and a special medical and protective regimen of the day in the first trimester. Prolonged toxicosis can cause hospitalization: it interferes with the normal absorption of food, as a result, the full supply of the baby with the necessary substances.
During pregnancy, taste preferences may change, some quirks may appear. A woman begins to feel an aversion to meat, gravitates towards salty foods and is ready to absorb chalk, tooth powder or dry pasta with pleasure. Such a perversion of taste is often explained by the development of iron deficiency anemia during pregnancy.
In the first trimester, the expectant mother notes discomfort in the mammary glands, pigmentation of the nipples, increased vaginal discharge, increased urination. These processes are physiological. But the appearance of pulling pains in the lower abdomen and blood from the genital tract are pathological symptoms. To maintain pregnancy, you should immediately seek medical help.
The well-being of the expectant mother: the second trimester
The first three dangerous (due to the relatively high risk of miscarriage) months of pregnancy have passed. The second trimester of childbearing has begun. The baby and mother are used to coexistence. Toxicosis receded, general well-being improved. The woman's tummy is noticeably rounded and clearly pleasing to the eye.
The second trimester of childbearing has begun. The baby and mother are used to coexistence. Toxicosis receded, general well-being improved. The woman's tummy is noticeably rounded and clearly pleasing to the eye.
Closer to the 20th week of pregnancy, the expectant mother listens especially carefully to her well-being, waiting for the first time to feel the baby moving.
An increase in the level of estrogen and, as a result, the retention of excess fluid in the body of a pregnant woman can adversely affect her well-being in the second trimester. It is not so much the obvious swelling of the lower extremities that is dangerous, but the swelling of the placenta that is not visible to the eye, the development of which can disrupt the blood supply to the fetus. Refusal of liquid food is not the best solution to the problem. After all, water, along with foods rich in vegetable fiber, helps to avoid the development of constipation in the second trimester.
The expectant mother's appetite has noticeably improved. When catching up, do not overdo it, remember the list of prohibited foods: fast food, fatty, spicy, smoked dishes, raw eggs, sushi, moldy cheeses, carbonated drinks, coffee, alcohol. Give preference to healthy food: meat, lean fish, cereals.
When catching up, do not overdo it, remember the list of prohibited foods: fast food, fatty, spicy, smoked dishes, raw eggs, sushi, moldy cheeses, carbonated drinks, coffee, alcohol. Give preference to healthy food: meat, lean fish, cereals.
The second trimester is a time of strict control over body weight. An increase of no more than 300 g is allowed weekly. In the third trimester of pregnancy, this increase should not exceed 400 g. In case of excess weight, the doctor will review the diet of a pregnant woman and prescribe fasting days.
Pregnant woman's well-being: third trimester
From the 27th obstetric week, the third trimester of childbearing begins. Pregnancy, approaching completion, introduces a number of physical inconveniences into the well-being of the expectant mother. By the end of the third trimester, the maximally enlarged uterus causes some displacement of the internal organs. The woman is worried about shortness of breath, lower back pain, frequent urination, possible constipation, varicose veins in the legs.
Psychological well-being in the third trimester is often disturbing, fear of childbirth may appear.
Important!
In the third trimester, you need to carefully monitor your well-being in order to timely detect possible pathological phenomena (preeclampsia, placental abruption) and seek help.
In the last months of pregnancy, the growing baby becomes cramped in the uterine cavity, and the expectant mother no longer feels timid movements, but active pushes with her hand or heel.
In the third trimester, the harbingers of childbirth (sagging abdomen, training contractions, mucus plug discharge) will tell the woman that the meeting with the baby will take place very soon.
Good health during pregnancy is an indicator of its favorable course. The deterioration of the condition of the expectant mother is the reason for a visit to a specialist.
what happens in 1, 2, 3 months
Wise nature endowed a woman with everything she needs to carry and give birth to a child. But this does not prevent expectant mothers from being interested in what is connected with conception, pregnancy and childbirth - asking important questions and looking for answers to them. They want to know what happens in the first trimester of pregnancy, how the baby develops, what processes take place in the body, what can and cannot be done. Let's talk about this in more detail.
But this does not prevent expectant mothers from being interested in what is connected with conception, pregnancy and childbirth - asking important questions and looking for answers to them. They want to know what happens in the first trimester of pregnancy, how the baby develops, what processes take place in the body, what can and cannot be done. Let's talk about this in more detail.
Excursion to obstetrics
First, let's define the terminology.
The entire pregnancy (gestation) of a woman lasts 40 weeks (280 days). These data are conditional, because normally, childbirth can begin at almost any time for a period of 37-42 weeks. This entire period is divided into three trimesters. The first trimester of pregnancy lasts from the first day of the last menstrual period until the end of the 13th week.
The division of pregnancy into weeks and trimesters is accepted in obstetrics. But women more often measure this period by months. This is not entirely correct, because one month includes 4 or 5 weeks. Therefore, in the article we will focus specifically on the obstetric weeks of gestation, but we will also correlate them with the months familiar to many women.
Therefore, in the article we will focus specifically on the obstetric weeks of gestation, but we will also correlate them with the months familiar to many women.
What happens in the first trimester of pregnancy
Obstetricians calculate the gestational age from the first day of the last menstruation. This is convenient - after all, most women keep a calendar and know this date. However, there is still no fetus during this period. Conception happens later - during ovulation, after about two weeks. It would be possible to count the gestational age from the moment of conception, but this date is difficult to calculate. In addition, ovulation may not occur in the middle of the cycle, but much earlier or later - and then it will be even more difficult to calculate it.
So, there are two stages of pregnancy:
- Obstetric - from the first day of the last menstruation.
- Embryonic - from the moment of conception.
We will focus on the obstetric period
In the article we will divide this period into weeks, not stages. Conventionally, the first trimester of pregnancy can also be divided into three months.
Conventionally, the first trimester of pregnancy can also be divided into three months.
First month of pregnancy
The first month of pregnancy is the period from the 1st to the 4-5th week.
No baby in the first two weeks. During this period, the woman's body is preparing for a possible pregnancy. Follicles mature in the ovaries, one (rarely two or more) dominant follicles stand out among them. If ovulation occurs, the egg is released from the follicle. When it meets sperm, fertilization occurs and new life is born.
In the third week of gestation, the fertilized egg moves through the fallopian tubes. Its task is to get into the uterine cavity and attach to its wall. This happens on the 7-8th day after conception - by the beginning of the 4th week. After implantation, the development of the fetal egg, the new life in it, continues. By the way, a child in early pregnancy is called an embryo, and after a full 8 weeks it will be called a fetus.
At the 3rd week, the embryo is a multitude of cells that are constantly dividing and developing. By the end of the first month of pregnancy, it already begins to influence the hormonal background of a woman due to the production of its own hormone - hCG (human chorionic gonadotropin). It is by the concentration of the hormone that it is possible to determine whether conception occurred in this menstrual cycle.
By the end of the first month of pregnancy, it already begins to influence the hormonal background of a woman due to the production of its own hormone - hCG (human chorionic gonadotropin). It is by the concentration of the hormone that it is possible to determine whether conception occurred in this menstrual cycle.
In the 1st month of gestation, the woman's well-being practically does not change. And only at the end of the 4th week toxicosis can develop. It is manifested by nausea, vomiting, increased salivation and weakness. Many women do not have toxicosis - and this is also a variant of the norm. The belly in the first month of pregnancy is not yet visible.
The second month of pregnancy
The 2nd month of gestation is the period from the 4-5th to the 8-9th week.
In the early stages of pregnancy, the active development of the embryo continues. It still has a C-shape. By the end of the 4th week, limb rudiments are formed, a circulatory system and a two-chamber heart rudiment appear. At the 6th week, the heart begins to beat - and it can be heard during an ultrasound.
At the 6th week, the heart begins to beat - and it can be heard during an ultrasound.
At the beginning of the 5th week, further development of the nervous system of the embryo takes place. The rudiment of the brain is isolated, conditions are created for its further differentiation.
On the 6th week of the 1st trimester, the organs of vision develop, the rudiments of the genital organs appear. The heart becomes three-chambered. At the 8th week, the sex of the embryo is determined - but it cannot yet be seen on ultrasound. As a result of all these transformations, in the second month of pregnancy, the fetus acquires a clear human appearance.
A woman's feelings change in the middle of the 1st trimester. Symptoms appear, which are usually called characteristic signs of pregnancy:
- Nausea, vomiting, increased salivation - this is how toxicosis manifests itself.
- General weakness, fatigue.
- Sudden mood swings.
- Frequent urination.

- Breast augmentation and enhancement of its sensitivity.
- Increased sensitivity to odors.
- Predilection or aversion to certain foods.
The belly is not yet visible in early pregnancy. The uterus is already growing, but so far it is completely in the pelvic cavity and does not go beyond the womb. But the breasts in the 2nd month of pregnancy already noticeably increase, become sensitive or even slightly painful.
The third month of pregnancy
The 3rd month is the period from the 8th-9th to the 12th-13th week.
In the third month of pregnancy, the further development of the child continues. Now it is called fruit. Its head, rudiments of limbs, torso, rudiments of eyes, nose and mouth are clearly visible. The fruit reaches the size of a goose egg.
On the 9-10th week, the cerebral cortex differentiates in the fetus, and the development of the nervous system continues. By the 12th week, foci of hematopoiesis appear in the bone marrow, and the first cells appear in the blood. At the 13th week, the formation of all organs of the fetus is completed, and the placenta is formed.
At the 13th week, the formation of all organs of the fetus is completed, and the placenta is formed.
The placenta in early pregnancy is usually low, near the cervix. It provides the baby with everything necessary - oxygen and nutrients, and removes metabolic products. It connects to the fetus through the umbilical cord, in which two arteries and one vein pass. Gradually, the placenta migrates and by the end of the second trimester, as a rule, takes the correct position.
The feelings of a woman in the 3rd month of pregnancy remain the same. As before, she feels weakness, mood swings, changes in taste preferences. There may be signs of toxicity. But some women do not notice significant changes in their well-being - and this is also the norm.
The belly is not visible at the 3rd month. Only on the 12-13th week the uterus goes beyond the womb. A slight rounding of the abdomen will be visible only at the 14-16th week.
What problems can be in the first trimester of pregnancy
The expectant mother should be alerted by the appearance of such symptoms: There are no periods during pregnancy. Seek medical attention if bleeding occurs.
Seek medical attention if bleeding occurs.
If you experience any unusual sensations and symptoms, you should contact your doctor as soon as possible!
What examinations are needed in the early stages of pregnancy
To confirm the fact of pregnancy, you can donate blood for hCG as early as the 1st month. This hormone rises 8-10 days after conception - after the implantation of the embryo. It is recommended to donate blood for hCG immediately after a missed period.
It is recommended to donate blood for hCG immediately after a missed period.
If hCG is positive, you need to contact a gynecologist and get registered. To clarify the diagnosis, the doctor may refer you to an ultrasound scan. With ultrasound in the 1st trimester, from the 3rd-4th week, you can see the fetal egg, from the 6th week, you can hear the fetal heartbeat. The next ultrasound, if there are no other indications, is carried out for a period of 11-14 weeks. This will be the first screening where you can assess the condition of the fetus and placenta, make sure that there are no malformations and other complications.
In the first trimester of pregnancy, all women are recommended to be screened:
- Pass blood and urine tests (the list will be issued by the attending physician).
- Get checked out by a dentist and an ophthalmologist.
- If necessary, visit other specialists (for example, an endocrinologist - if there is a thyroid disease).

- Make an ECG and consult a therapist.
All this is necessary to make sure that the expectant mother is healthy, can bear and give birth to a child.
Many women wonder how to behave if the pregnancy is less than a month old. Here are some recommendations:
In the first trimester of pregnancy, all women are advised to be screened:
- Give up alcohol and quit smoking if you did not do so before conception.
- Do not take medicines without a doctor's prescription.
- Avoid overheating and hypothermia.
- Do not take x-rays, MRIs, or similar procedures unless you have a strong indication and a referral from a doctor.
- Do not overexert, reduce physical activity, including in sports.
- Avoid stressful situations.
In the following weeks of the first trimester, the recommendations remain the same, and nutritional advice is added:
- Eat often, in small portions, 5-6 times a day.

- Eat only fresh produce.
- Avoid foods that increase the symptoms of toxicosis and provoke constipation.
- Avoid feeling hungry, but don't overeat either.
It is worth noting that the nutrition of the expectant mother affects not only her, but also the baby, and it is worth taking a responsible approach to this. Yes, a special universal diet has not been developed, but the doctor may recommend that the expectant mother adhere to a certain diet after the examination (add certain foods to the diet if any elements are missing, etc.).
It is recommended to follow the general principles of a healthy diet:
- Eat more fresh vegetables, fruits and greens - up to 5 servings per day.
- Limit salt and added sugar intake.
- Reduce the proportion of animal fats in the diet.
- Refuse fried, spicy, salty foods, sausages and smoked meats.
- Prefer whole grains.
If you need to follow a special diet for health reasons, you should discuss this with your doctor.