Can early pregnancy cause cold sores
Cold sores in pregnancy | Pregnancy Birth and Baby
Cold sores in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is HSV?
If you or your partner has the virus that causes cold sores or genital herpes, you might be worried about what could happen when you're pregnant or have a new baby. Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
The herpes simplex virus is a very common virus carried by most people. Sometimes it causes cold sores or genital herpes.
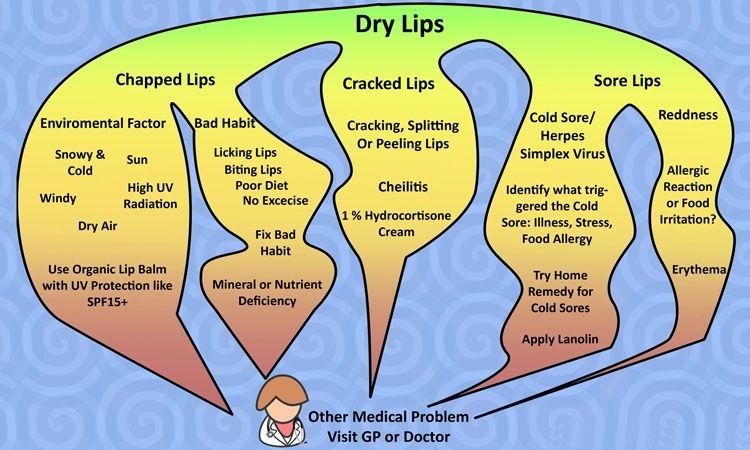
Cold sores are blisters that form on the lips, around the mouth and nose. Genital herpes is blisters or sores around the genitals or anus. The blisters may form a crust after about 3 days. The sores go away by themselves within 2 weeks.
There are two main types of HSV:
- HSV-1 causes mostly cold sores on the face and lips, and sometimes on the genitals
- HSV-2 causes mostly genital herpes
Both viruses are transferred though contact of the skin, saliva or genitals, and the viruses stay in the body for life. The viruses do not always cause symptoms, so you can carry the virus without knowing it.
HSV-1 is very common, with about 8 in 10 Australians carrying it in their bloodstream. But only 1 in 3 people with the virus has ever had a cold sore. HSV-2 is less common.
It is common for women who have had cold sores in the past to experience an outbreak while pregnant.
What happens if I get cold sores or genital herpes during pregnancy?
Having the HSV virus does not affect your chance of becoming pregnant.
It is quite common for women to have a cold sore during their pregnancy, even if they haven’t had one for a long time. Cold sores should not affect your unborn baby. But they are infectious, so it’s a good idea to treat them.
But they are infectious, so it’s a good idea to treat them.
Genital herpes should not affect the baby if you have your first outbreak or it comes back in the first 34 weeks. But it can be transferred to your baby during the birth, especially if it’s your first outbreak.
If you've ever had a cold sore or genital herpes and you become pregnant, or you develop these conditions during pregnancy, it's important to tell your doctor or midwife about it. Together you can make a plan for managing herpes during pregnancy and birth.
How is HSV treated during pregnancy or breastfeeding?
You can treat cold sores and genital herpes with:
- aciclovir cream, available from a pharmacist without prescription
- aciclovir or valaciclovir tablets, for which you need a prescription
These 'antiviral' drugs are known to be safe for pregnant and breastfeeding women and are effective most of the time.
Famciclovir tablets are not recommended to take during pregnancy. Speak to your doctor if the cold sore is severe.
Speak to your doctor if the cold sore is severe.
How is genital herpes treated during pregnancy?
You should take acyclovir or valaciclovir tablets, as above.
If it's your first outbreak of genital herpes, your baby may be more at risk because you haven't had time to develop immune protection against the virus, which also helps protect the baby.
Some women experiencing an outbreak of genital herpes might be advised to have a caesarean. This would prevent the herpes virus passing from mother to baby during a vaginal birth. But most women in Australia with genital herpes do give birth safely to healthy babies vaginally.
It's often recommended that women who have ever had genital herpes take antiviral tablets prior to the birth, even if the herpes isn't active at the time.
Talk to your doctor or midwife about the best course of action for your situation.
How do I protect my baby from herpes?
Herpes can cause serious problems in a baby, such as infections to the eyes and throat, brain damage and even death.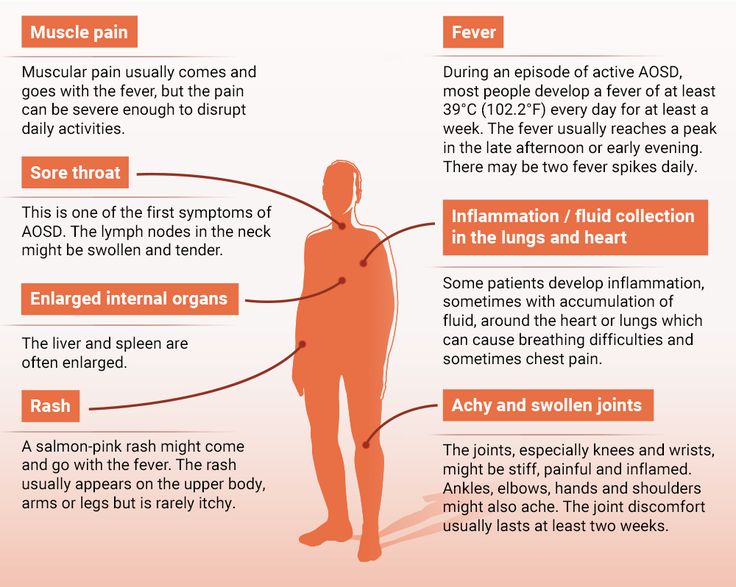
A newborn baby can catch HSV-1 and HSV-2 from being kissed or touched by someone with cold sores, or during childbirth.
Fortunately, most babies born to women who carry the virus are not affected. But if you or your partner has a cold sore or genital herpes, talk to your doctor about keeping it under control during the pregnancy and after the birth. It is also important to treat these conditions aggressively while you are breastfeeding.
It's important to maintain strict hygiene habits when caring for a new baby if you, or anyone in close contact with the baby, have cold sores.
If you have cold sores, you should:
- cover cold sores when you're around the baby
- avoid kissing your baby until the sores are completely healed
- avoid touching the cold sores then touching your baby
- wash your hands thoroughly before touching your baby
What if I have a cold sore while breastfeeding?
If you have cold sores, it is safe to breastfeed your baby as long as the cold sores are not on the breast or nipple.
If they are, it may be wise to breastfeed from the unaffected nipple only until the lesions have cleared up. You would express and dispose of breastmilk from the affected nipple. Breastmilk itself doesn't contain the herpes virus but it can be contaminated through the skin lesions.
Talk to your doctor or midwife as soon as you notice any cold sores on your breast or nipple.
What happens if my baby gets herpes?
It is very important that herpes in a newborn is recognised and treated by a doctor in hospital immediately. Signs of herpes in a newborn include:
- blisters on the skin
- fever
- irritability
- tiredness
- lack of appetite
If you think your baby might have the herpes virus, don't wait to see if they get better — seek medical help. Tell medical staff if you or your partner carry the herpes virus.
Resource and Support
If you are worried about your baby, see a doctor or midwife, or take them to the hospital.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
If you're not sure what to do or want more information, you call Pregnancy Birth Baby on 1800 882 436 to speak with a maternal child nurse.
Sources:
Family Planning NSW (Genital herpes), The Royal Woman’s Hospital (Genital herpes), Mothersafe (Cold sores in pregnancy and breastfeeding), Queensland Government Health (Genital Herpes and Pregnancy), SA Health (Cold sores (herpes simplex type 1) - including symptoms, treatment and prevention), Safer Care Victoria (Herpes simplex virus in neonates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Need more information?
Cold sores overview - MyDr.
 com.au
com.au A cold sore is a skin infection that is caused by the herpes simplex virus (HSV). Cold sores usually occur on or around the lips or nose and are very common. They have nothing to do with colds.
Read more on myDr website
Cold sores: self-care - MyDr.com.au
Cold sores are caused by the herpes simplex type 1 virus. Most people carry this virus in their bodies. Find out what products are available for cold sores.
Read more on myDr website
Cold sores | SA Health
Herpes simplex virus type 1 (HSV1) causes cold sores on the face or lips - it is spread by skin or mucous membrane contact with infected saliva
Read more on SA Health website
Cold sore infections - MyDr.
 com.au
com.au Find the answers to common questions about cold sores, irritating blisters which are caused by the herpes simplex type 1 virus and can be triggered by stress, fatigue or exposure to sunlight.
Read more on myDr website
Cold sores - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Cold sores: children & teens | Raising Children Network
Cold sores are quite common in older children and teenagers. Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Read more on raisingchildren.net.au website
Genital Herpes | Family Planning NSW
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV).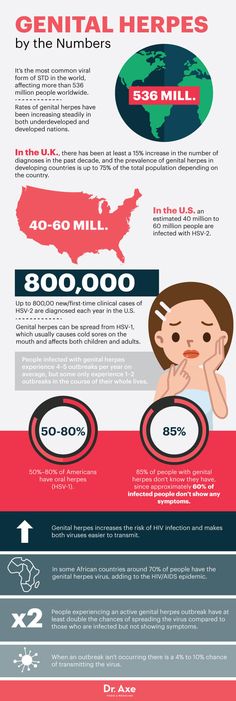 There are two types of herpes simplex virus.
There are two types of herpes simplex virus.
Read more on Family Planning NSW website
Genital Herpes and Pregnancy
If you are pregnant and you get genital herpes, it is important to tell your midwife or obstetrician.
Read more on Queensland Health website
Genital herpes
Genital herpes is a sexually transmitted infection (STI) which shows as blisters or sores on the genitals. This is caused by the herpes simplex virus (HSV).
Read more on WA Health website
Genital herpes: what is it? - MyDr.com.au
Genital herpes is a viral infection characterised by outbreaks of blisters and sores around your genital area.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How Common Are Cold Sores (Fever Blisters) During Pregnancy?
You may contract the virus again while pregnant if it was contracted before.
Research-backed
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies.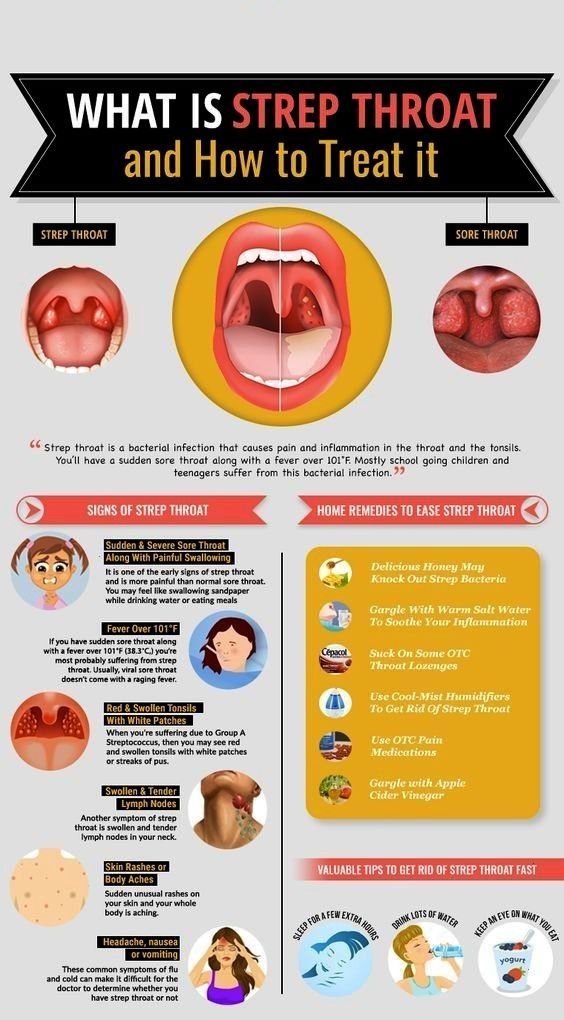 However, if you find any incongruencies, feel free to write to us.
However, if you find any incongruencies, feel free to write to us.
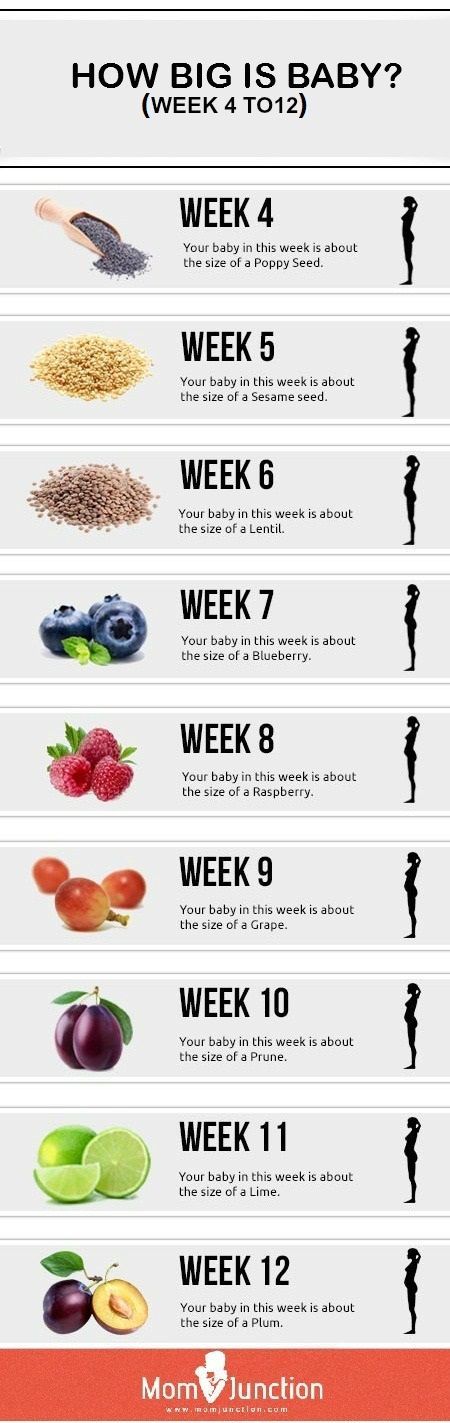
Image: Shutterstock
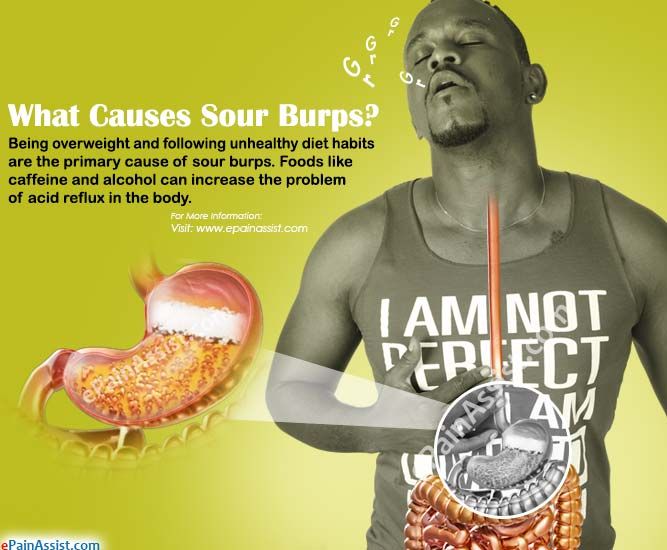
Cold sores or fever blisters erupt inside the lips or cheeks, around the mouth, or near the nose and chin. These itchy and tingly sores might sometimes be painful too. Usually, cold sores are likely to disappear in a couple of weeks. But what happens when they occur during pregnancy? What should you do about them?
We tell you about it in this MomJunction post. Keep reading to know more about cold sores during pregnancy.
Are Cold Sores Common In Pregnancy?
Cold sores are usually caused by herpes simplex virus (HSV), especially type 1 of the virus (1). Therefore, they are likely to be common in women who have experienced them in the past (2).
What Are The Causes Of Cold Sores During Pregnancy?
Cold sores are caused by the herpes simplex viruses named HSV1 and HSV2. The virus transmits from one person to another through skin to skin contact during touching, sexual intimacy, kissing, or sharing contaminated items (3).
Once a woman has contracted the virus, the following risk factors could trigger the cold sore virus.
- Hormonal changes that frequently rise and fall could make the body susceptible to viral infection, including a cold sore outbreak (4).
- Psychological concerns, such as stress and fear could trigger the virus (5).
- Certain foods (acidic, spicy, or salty), citrus fruits, exposure to the sun, and hot water could trigger the virus and cause cold sores (6).
Signs And Symptoms Of Cold Sores In Pregnancy
The common signs and symptoms that could indicate cold sores during pregnancy include:
- Swelling of the lips
- Small, painful blisters
- Redness
- Tiny bumps over your lips
- Fever
- Pains and aches
- Sore throat
Cold sores develop gradually, in five different stages, when you might experience the above symptoms. Understanding the changes in each of these stages might help you take the right steps to prevent them from spreading to other parts of the body.
Stages Of Cold Sores
The cold sores last for seven to 12 days, and during this time, they might progress in different stages (7).
Stage 1: The tingling stage
You may experience a tingling sensation for about a couple of days. The skin (inside your lips, on your lips, or inside the cheeks) might turn sore and red and might even swell and become itchy.
Stage 2: The blister stage
This stage lasts for about two days. During this stage, new blisters may form and spread to other parts in the absence of proper care.
Stage 3: The weeping stage
At this stage, the blisters may burst, and you might experience pain. The cold sores might scab over at this point.
Stage 4: The scabbing stage
The scabs may crack and even bleed. They could be itchy, but make sure you are not poking them.
Stage 5: The healing stage
In this stage, all the scabs flake off and disappear soon after. Even the scars slowly vanish.
Observe the progress of cold sores and treat them in time to prevent the infection from spreading.
Are Cold Sores Contagious?
According to the World Health Organization (WHO), herpes infections are highly contagious when symptoms such as ‘cold sores’ are present (8). The virus may be passed from one person to another. If the bump ruptures, the active virus could spread via lipstick, cups, utensils, kissing, or through oral sex (9).
According to the UT Southwestern Medical Center, HSV 1 or the cold sore infection could pass from the infected person to the baby. This usually happens when the person kisses the baby or when the baby is touched after the cold sore is touched (10).
Therefore, it is important to treat the cold sore in pregnancy to prevent the virus from spreading to the baby after it is born. Herpes infection is mild for the mother but can be life-threatening for the baby.
How To Treat Cold Sores In Pregnancy?
Home care measures for the sores might alleviate pain and discomfort. In some cases, medication may be necessary.
In some cases, medication may be necessary.
1. Home treatment
- You may try some home remedies to ease the cold sore-related pain and discomfort
- Placing a cold compress (wet, cool cloth, or towel) on the sores may help reduce the redness and pain.
- A mouthwash containing baking soda may also reduce the soreness.
- Apply sunscreen before going outside.
You may apply aloe vera gel or lip balm containing soothing ingredients on the sores.
2. Clinical medicine
Before you take any medication for cold sores in pregnancy, talk to your doctor. Ideally, antiviral medications are prescribed to treat cold sores. According to the American Academy of Family Physicians, the common options include valacyclovir, famciclovir, and acyclovir (11). These fall under pregnancy category B medications of the US Food and Drug Administration.
If the cold sores get severe, the doctor may change the dose or prescribe other treatment.
Are Cold Sores An Early Sign Of Pregnancy?
Cold sores are common, and most pregnant women may experience them. But they may not be an early sign of pregnancy. A woman may get cold sores at any point during the gestation period.
Are Cold Sores During Pregnancy Harmful To The Baby?
According to the Royal Hospital for Women, Australia, cold sores may not affect newborn babies. But they are infectious and should be treated in time, so they don’t spread to the infant (1). However, if you have genital herpes, then there are chances of the virus transmitting to the baby during the process of childbirth (known as acquired herpes). This can be very dangerous for the baby. Hence, a cesarean section is indicated to avoid contact of the baby with the cold sores.
1. Can pregnancy flare-up cold sores?
Pregnancy modulates the immune system, and women who have herpes may have an increased risk of outbreaks of cold sores during pregnancy (12) (13).
2. Can pregnancy hormones cause cold sores?
Cold sores may be triggered due to hormonal changes during pregnancy or menstruation in women already exposed to the herpes simplex virus type 1 (HSV-1) (14).
3. Can I use Abreva for cold sores while pregnant?
The manufacturer’s instruction states that Abreva is not recommended for treating cold sores in pregnant or lactating women unless advised by a doctor (15).
4. Can I use cold sores cream when pregnant?
A doctor may prescribe cold sores creams containing aciclovir, an antiviral medication, for treating cold sores during pregnancy (2).
HSV1 and HSV2 can produce cold sores during pregnancy that can emerge inside the lips or cheeks, near the nose and chin, or around the mouth. The advancement and healing may occur in stages over seven to twelve days. It is advised to avoid touching the sores when they erupt, follow a well-balanced diet, and get plenty of rest to avoid cold sores during pregnancy. Also, stay away from spicy meals and wash your hands frequently. Though cold sores are not a cause for concern during pregnancy, you should visit your doctor and have them treated as soon as possible.
Key Pointers
- Cold sores are blisters inside the mouth or near the nose, caused by the herpes simplex virus and commonly seen in women with past exposure.

- The virus is contagious, and factors such as hormonal or psychological changes can trigger its occurrence in pregnant women.
- It is not an alarming concern. You may try some effective home remedies or consult your ob/gyn for pregnancy-safe medications.
References:
MomJunction's articles are written after analyzing the research works of expert authors and institutions. Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
1. Cold sores (herpes simplex type 1) – including symptoms, treatment and prevention; Government Of South Australia (2019)
2. Cold sores in Pregnancy and Breastfeeding; The Royal Hospital For Women (2016)
3. Cold sores in pregnancy; Pregnancy, Birth and Baby; Healthdirect Australia (2019
4. Cold sores; University of Wisconsin-Madison
5. D. B. Donahue; Diagnosis and Treatment of Herpes Simplex Infection During Pregnancy; Journal of Obstetric, Gynecologic & Neonatal Nursing (2002)
D. B. Donahue; Diagnosis and Treatment of Herpes Simplex Infection During Pregnancy; Journal of Obstetric, Gynecologic & Neonatal Nursing (2002)
6. Herpes simplex; Mount Sinai
7. Cold Sores; San Diego State University
8. Herpes simplex virus; World Health Organization (2017)
9. D. Shipp; How contagious are cold sores?; The Ohio State University (2019)
10. R. Horsager-Boehrer and J. Kahn; How to protect your baby from herpes infection; UT Southwestern Medical Center (2017)
11. ACOG Releases Guidelines on Managing Herpes in Pregnancy; American Academy of Family Physician (2008)
12. Gil Mor and Ingrid Cardenas; The Immune System in Pregnancy: A Unique Complexity; American Journal of Reproductive Immunology (2010)
13. Cold sores in pregnancy; Pregnancy Birth & Baby
14. Cold Sores; Cleveland Clinic
15. Understanding cold sores; Abreva Canada
The following two tabs change content below.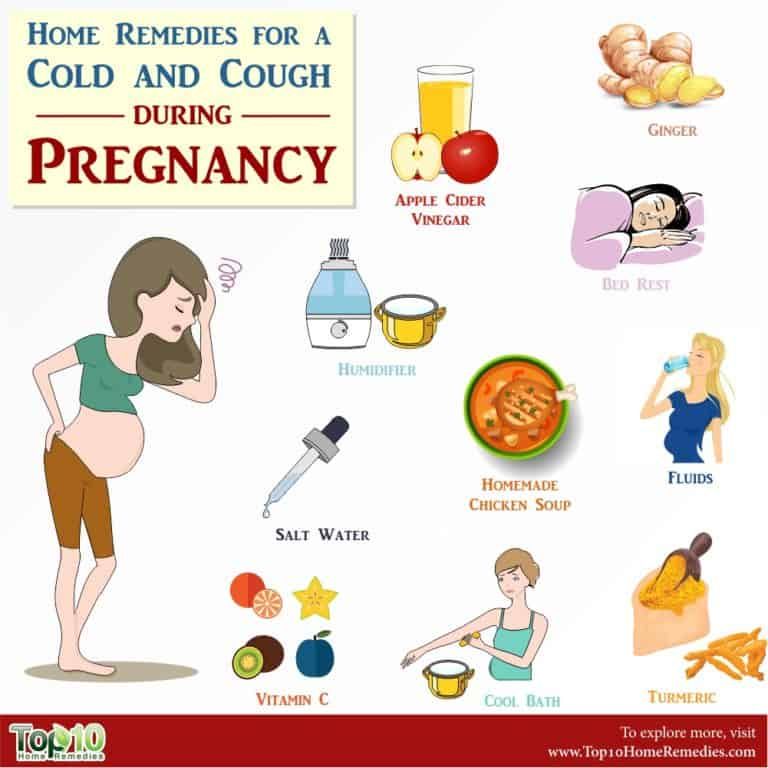
- Reviewer
- Author
Rebecca is a pregnancy writer and editor with a passion for delivering research-based and engaging content in areas of fertility, pregnancy, birth, and post-pregnancy. She did her graduation in Biotechnology and Genetics from Loyola Academy, Osmania University and obtained a certification in ‘Nutrition and Lifestyle in Pregnancy’ from Ludwig Maximilian University of Munich (LMU). She has been into health and... more
Dr. Ben Abbes Taarji Hicham is a practicing obstetrician and gynecologist with over 20 years of experience. Having worked in various Moroccan hospitals, he currently runs a private practice. Dr. Hicham specializes in rejuvenation and cosmetic gynecology, medically assisted reproduction, breast and gynecological cancers, HPV diseases, hysteroscopy and laparoscopy, and hormonal disorders.
Baby Dry Scalp: Causes, Home Remedies..
Baby Dry Scalp: Causes, Home Remedies..
Baby Heat Rash: Types, Symptoms And.
 .
.Baby Heat Rash: Types, Symptoms And..
Strong Urine Smell In Babies: Causes,..
Strong Urine Smell In Babies: Causes,..
20 Reasons Why Baby Fusses Or Cries..
20 Reasons Why Baby Fusses Or Cries..
Why Do Babies Roll Their Eyes While..
Why Do Babies Roll Their Eyes While..
Fever During Pregnancy: Symptoms,..
Fever During Pregnancy: Symptoms,..
Beckwith-Wiedemann Syndrome In Babies:..
Beckwith-Wiedemann Syndrome In Babies:..
11 Reasons Why Baby Refuses To Eat And..
11 Reasons Why Baby Refuses To Eat And..
Stomach Pain During Pregnancy: Causes..
Stomach Pain During Pregnancy: Causes..
Herpes, cytomegalovirus, Epstein-Barr virus in pregnancy
Expecting a baby is always stressful for the female body, which has to work hard for nine months. And during pregnancy, the expectant mother has a lot of reasons for unrest.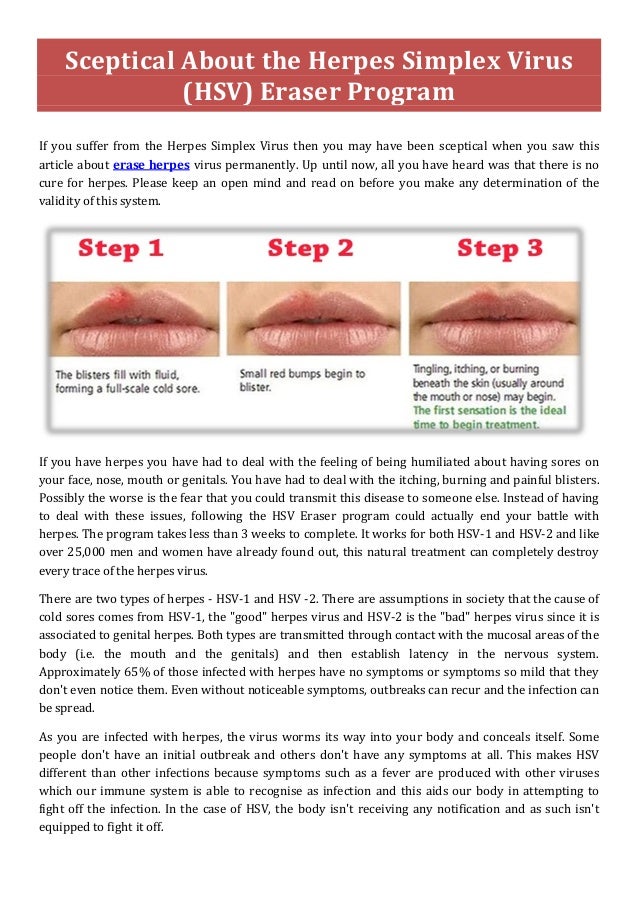 Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
Herpes
The concept of "herpes during pregnancy" is too broad and often becomes a cause for unreasonable panic among pregnant women who do not know what and in what cases a threat to their unborn child may appear. It is important for a pregnant woman to have information about all the features of this disease at different stages of pregnancy in order to contact a gynecologist in time and understand when there is really a danger to the fetus when a cold appears on the lips.
If a woman in an interesting position has a recurrent form of the virus, that is, she has already encountered it before pregnancy, almost any manifestation of herpes is not dangerous for the mother and child. A simple herpes virus can only be a threat during pregnancy if it is a primary infection, especially in the early stages, when all the internal organs of the baby are laid and, most dangerously, the neural tube. Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Cytomegalovirus
For a pregnant woman, the virus is dangerous during the primary infection during the expectation of a child. Infection from a sick person with an acute cytomegalovirus infection is the worst option for a pregnant woman, because due to the lack of antibodies in the blood, the virus easily crosses the placenta and has a negative effect on the fetus. According to statistics, infection of the fetus occurs in 40-50% of cases. The degree of adverse effect of the virus on the fetus depends on the duration of pregnancy. If the fetus is infected in early pregnancy, there is a high probability of spontaneous miscarriage or anomalies in the development of the child.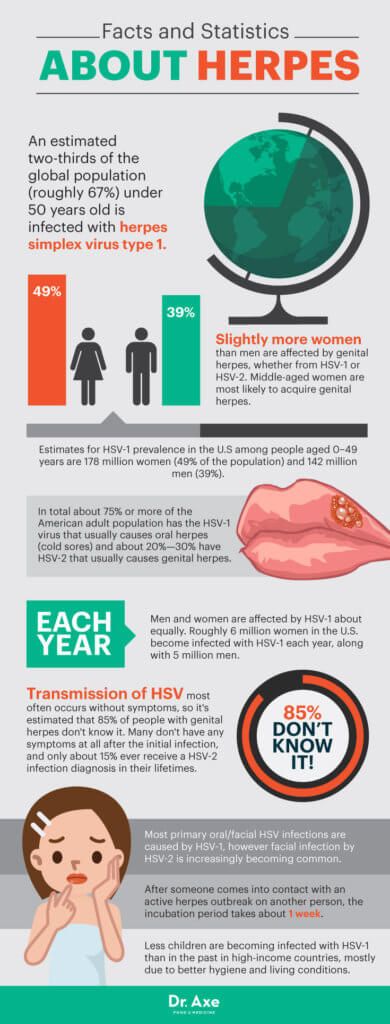 If the infection happened at a later date, no fetal malformations are observed, but quite often polyhydramnios occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
If the infection happened at a later date, no fetal malformations are observed, but quite often polyhydramnios occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
Eppstein-Barr virus
The Epstein-Barr virus predisposes to premature termination of pregnancy, fetal malnutrition, in newborn children causes damage to the nervous system, organs of vision, recurrent chroniosepsis, hepatopathy and respiratory distress syndrome. However, this virus provokes the listed pathologies only under certain conditions, in the presence of which during pregnancy it becomes dangerous. It is very bad if a pregnant woman has not previously encountered the Eppstein-Barr virus, which is why she does not have antibodies to this virus in her body. If there was still contact, and antibodies were found after treatment, then this is a good sign, because in this case there is nothing to be afraid of. This serves as evidence that if a woman's body is re-infected, it will cope with this dangerous disease on its own. This means that a pregnant woman will not have to take heavy and rather dangerous drugs for the development of the fetus.
This serves as evidence that if a woman's body is re-infected, it will cope with this dangerous disease on its own. This means that a pregnant woman will not have to take heavy and rather dangerous drugs for the development of the fetus.
THERE ARE CONTRAINDICATIONS. YOU NEED TO CONSULT WITH A SPECIALIST
The materials posted on this page are for informational purposes and are intended for educational purposes. Site visitors should not use them as medical advice. Determining the diagnosis and choosing a treatment method remains the exclusive prerogative of your doctor!
Reproductive Health Training CenterReproductive Health Training Center
Having genital herpes does not mean you cannot have children. According to the American Public Health Association (ASHA), only 0.1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
Breast-feeding during herpes recurrence is possible. Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
The initial episode of genital herpes is usually a tragedy during pregnancy. It is characterized by pronounced manifestations, tk. there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. As a rule, fetal death and miscarriage occur in the first trimester. Damage to the developing organs of the fetus, the occurrence of congenital deformities are possible. Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen. Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
HOW TO DETECT THAT I HAVE A PRIMARY EPISODE OF GENITAL HERPES?
What does primary episode mean? It means that in your life there has never been a recurrence of genital herpes and the body has not yet developed protective antibodies to HSV.
In some cases it is difficult to determine: what is it? Whether the first episode of genital herpes in life or the first recurrence with visible symptoms of genital herpes that was previously asymptomatic or with atypical symptoms. The fact is that in most people infected with HSV, the disease is almost asymptomatic. It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo.
It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo.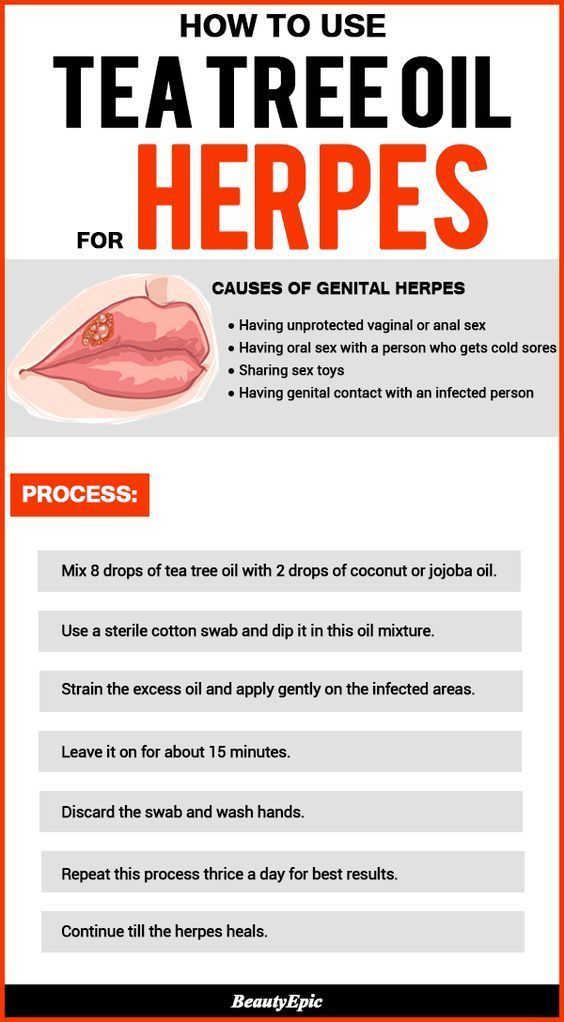 If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
There are no specific methods for preventing the transmission of genital herpes during pregnancy. From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
Should refrain from oral sex. Because if you have never had herpes of the lips in your life, and the husband or father of the child had it, then during cunniling he can bring the herpes simplex virus type I to your genitals. And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
Treatment with acyclovir and valtrex. However, these drugs do not always allow to achieve good success in treatment.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Against the background of a primary episode of genital herpes, the loss of a desired pregnancy is a severe psychological trauma for both potential parents. But in any case, there is hope. The next pregnancy will proceed already against the background of recurrent genital herpes. After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
Recurrent genital herpes during pregnancy
As blasphemous as it may sound, but recurrent genital herpes is the most favorable option during pregnancy. If a woman before the onset of this pregnancy already had relapses of genital herpes, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
STATISTICS:
During pregnancy, infection of a newborn with the herpes simplex virus from a mother with recurrent genital herpes occurs quite rarely: in approximately 0.02% of cases.
The risk of infection of a child in childbirth from a mother suffering from recurrent genital herpes is less than 1% (According to the study: Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L.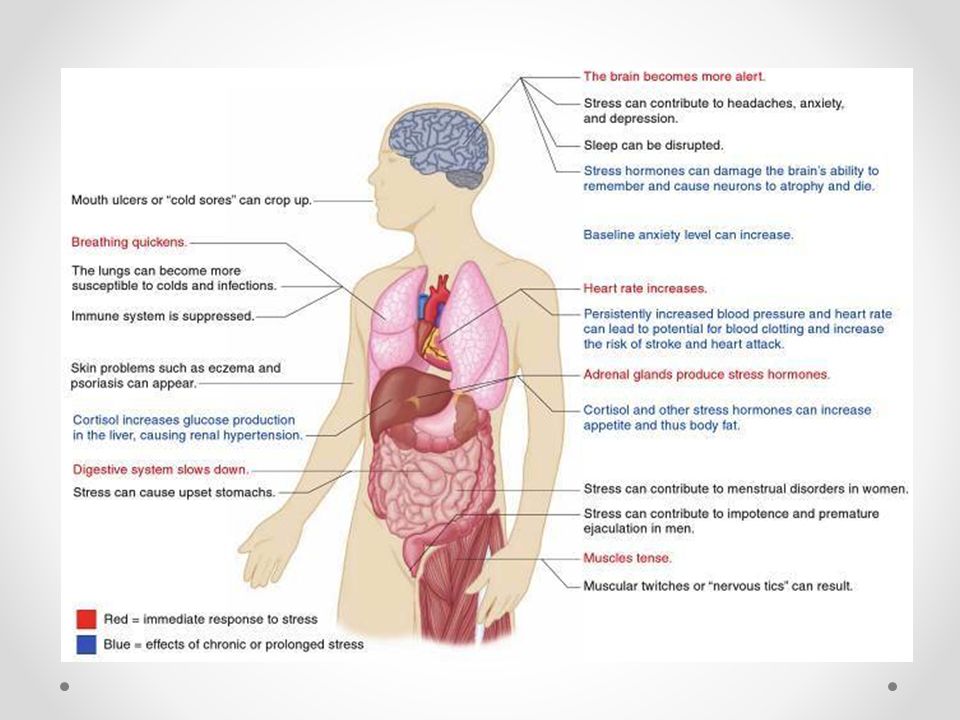 Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
BEFORE PREGNANCY: Plan the onset of pregnancy , eliminate bad habits from your life, heal chronic diseases, take a course of restorative treatment, cure foci of chronic infection before pregnancy (sore teeth, sinusitis, gastritis).
In some cases, a woman cannot know whether she had recurrences of genital herpes before or not. This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers).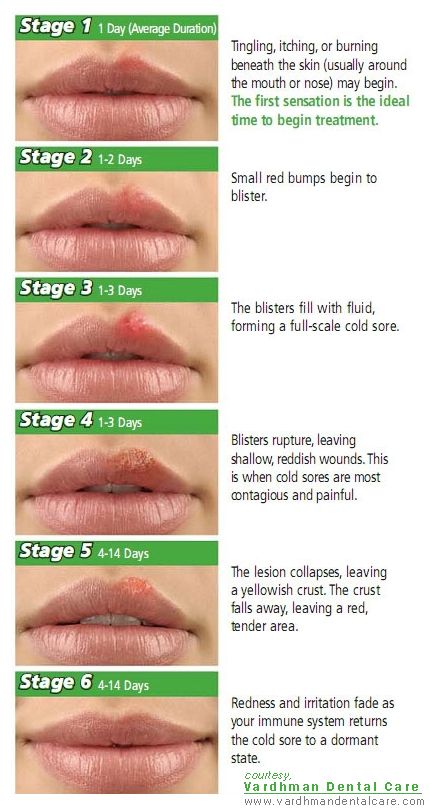 Regardless of the titer (the amount of Ig G & M), you can become pregnant.
Regardless of the titer (the amount of Ig G & M), you can become pregnant.
DURING PREGNANCY:
- When having sex always use a condom ;
- Avoid oral sex
If you get cold sores during pregnancy, you can transfer it to the penis of the father of your unborn child during oral sex. And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
PROPHYLAXIS DURING PREGNANCY:
To prevent recurrence during pregnancy after 36 weeks, your doctor may prescribe a course of preventive treatment with acyclovir or valaciclovir. During pregnancy, it is better to use acyclovir, manufactured by GlaxoSmithKline under the name Zovirax or Valtrex. Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Dynamic monitoring : Examination of pregnant women includes a mandatory three-time ultrasound examination: at 10-14 weeks of gestation, when the thickness of the nuchal space of the fetus is mainly assessed; at 20-24 weeks, ultrasound is performed to detect malformations and echographic markers of chromosomal diseases; an ultrasound examination at 32–34 weeks is performed in order to detect malformations with their late manifestation, as well as for the purpose of a functional assessment of the fetal condition. In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
Treatment: Only under medical supervision and prescription! Outwardly, you can use an ointment based on acyclovir. Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
PROPHYLAXIS DURING DELIVERY:
Treatment of the soft birth canal with polyvidone iodine (betadine, vocadine) or other antiseptics during childbirth can reduce the risk of neonatal herpes infection to the child to Genital herpes - abortion or childbirth?
Many women with recurrent genital herpes wonder how their illness might affect their unborn child.
The editor of the server received a letter describing a typical example of the illiterate approach of Soviet doctors to the management of pregnant women with genital herpes:
Professor D ***, from the Chelyabinsk Medical Academy, believes that it is highly undesirable to keep the pregnancy during an exacerbation of genital herpes in the early stages of pregnancy. He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
In developed countries, the optimal tactics for managing pregnant women with genital herpes has long been developed, based not on the private opinion of some “Professor D *** from the Chelyabinsk Medical Academy”, but on the data of long-term clinical studies and observations.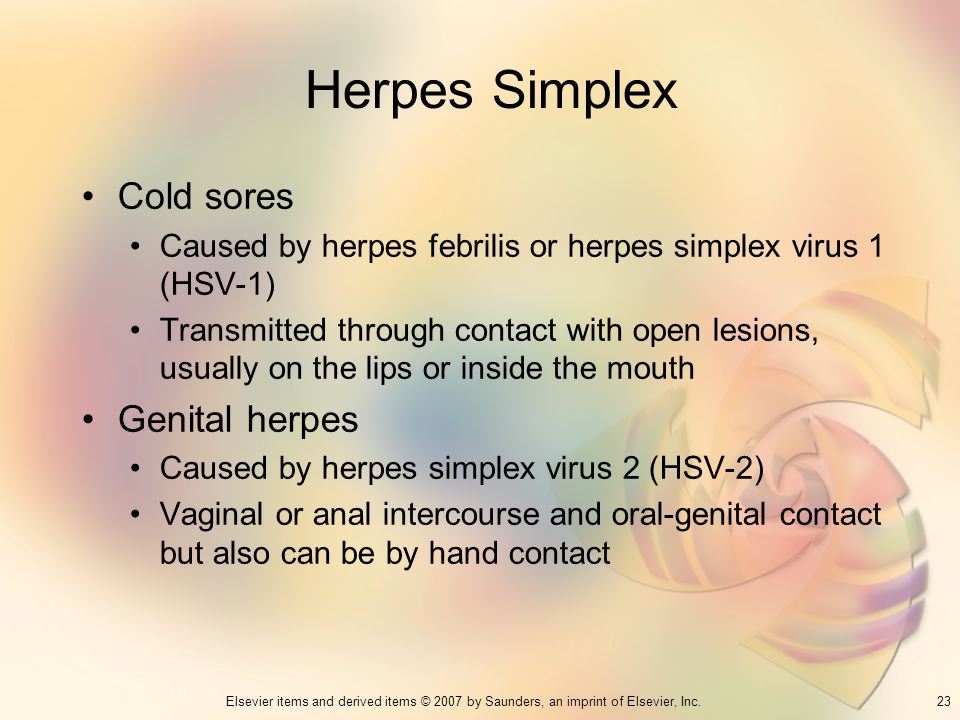
So that someone's subjective opinion does not lead you to an unnecessary abortion, we will tell you once again about what to do if you have herpes and pregnancy.
If a woman has the first time in her life during pregnancy there is a recurrence of genital herpes (primary genital herpes) or if the mother-to-be becomes infected with genital herpes during pregnancy, the fetus may be affected. The fact is that in this case, the mother's blood does not contain antibodies to the Herpes Simplex Virus - immunoglobulins G and Em (Ig G and Ig M), which block the pathological effect of the herpes simplex virus on fetal cells.
In the case of the first recurrence of genital herpes in a woman's life, the virus can penetrate the placenta and multiply in the tissues of the embryo or fetus, which leads to fetal death, miscarriage, congenital deformities, damage to the brain, liver, and other organs of the fetus, non-developing pregnancy. The risk of fetal damage in primary genital herpes is 75%.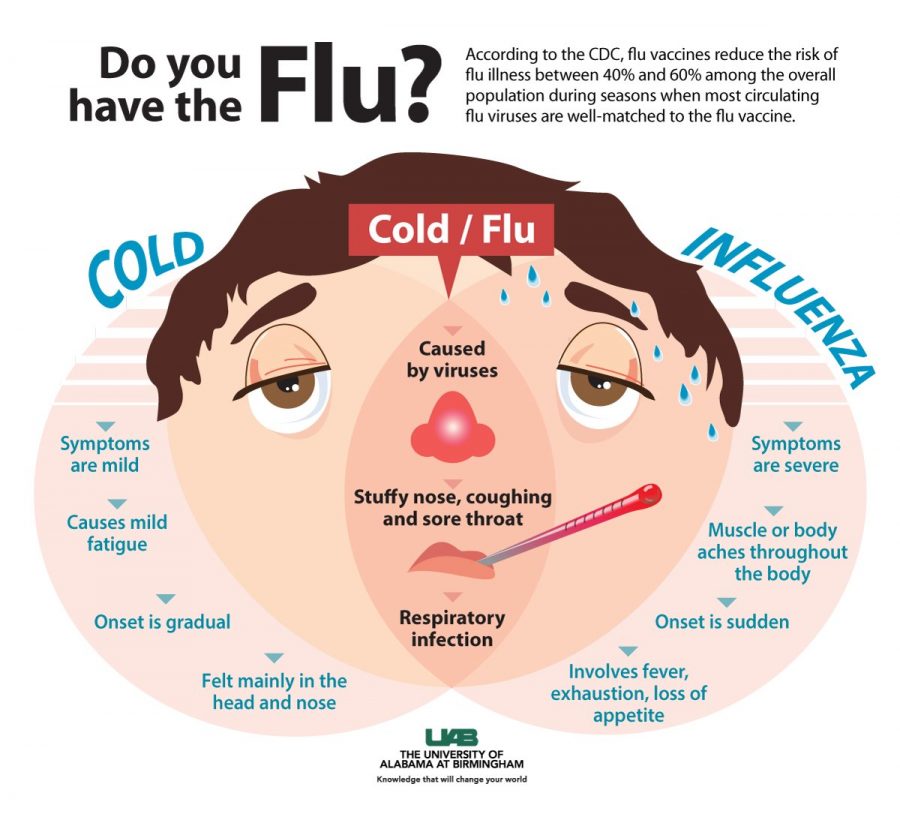
If the first recurrence of genital herpes occurs 30 days before delivery, delivery by caesarean section is recommended.
From 36 weeks of pregnancy, a doctor may prescribe Zovirax tablets to prevent the recurrence of herpes.
To prevent infection with genital herpes during pregnancy, it is imperative to use a condom and avoid oral sex, i. a man should not caress the sexual organs of a pregnant woman with his mouth. The reverse situation is allowed.
If a woman had recurrences of genital herpes before pregnancy, then antiherpetic antibodies float in the pregnant woman's blood, which limit the infection and neutralize the virus. These antibodies pass through the placenta to the fetus, protecting it. Therefore, recurrent genital herpes is not so dangerous during pregnancy. In this case, due to herpes, there are no deformities and lesions of internal organs.
In recurrent genital herpes , the baby can become infected during childbirth, passing through the birth canal, where the herpes virus is present.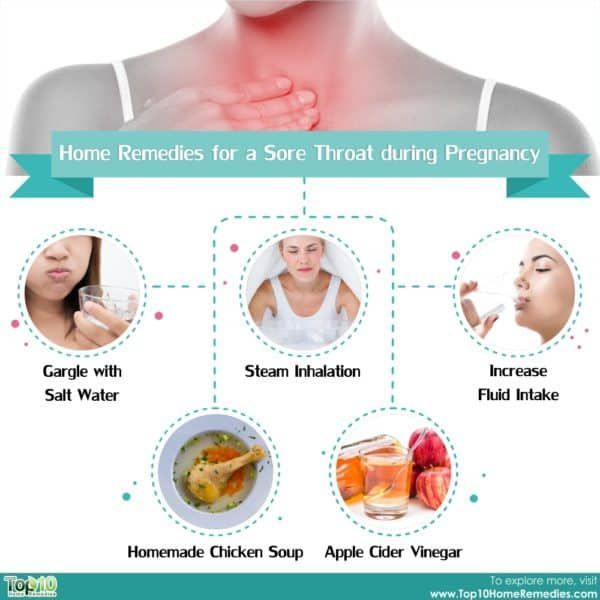 The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
Recurrent genital herpes is not an indication for abortion.
And despite all our clarifications about the relative safety of recurrent genital herpes during pregnancy, sometimes you have to receive such letters: A woman with recurrent genital herpes writes: “And most importantly, herpes is just natural selection. Nature removes lepers, because their offspring are doomed to death, so I don’t even dream of children ... ”It is ignorant to consider yourself a leper and refuse the happiness of motherhood just because you have recurrent genital herpes (the most favorable form for bearing and childbirth). Although, it cannot be ruled out that this is our medical defect.
There is also such a diagnosis as non-primary genital herpes . What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
Use of immunomodulators during pregnancy
The server editor received a letter describing a typical clinical situation:
« I have a problem that requires urgent consultation.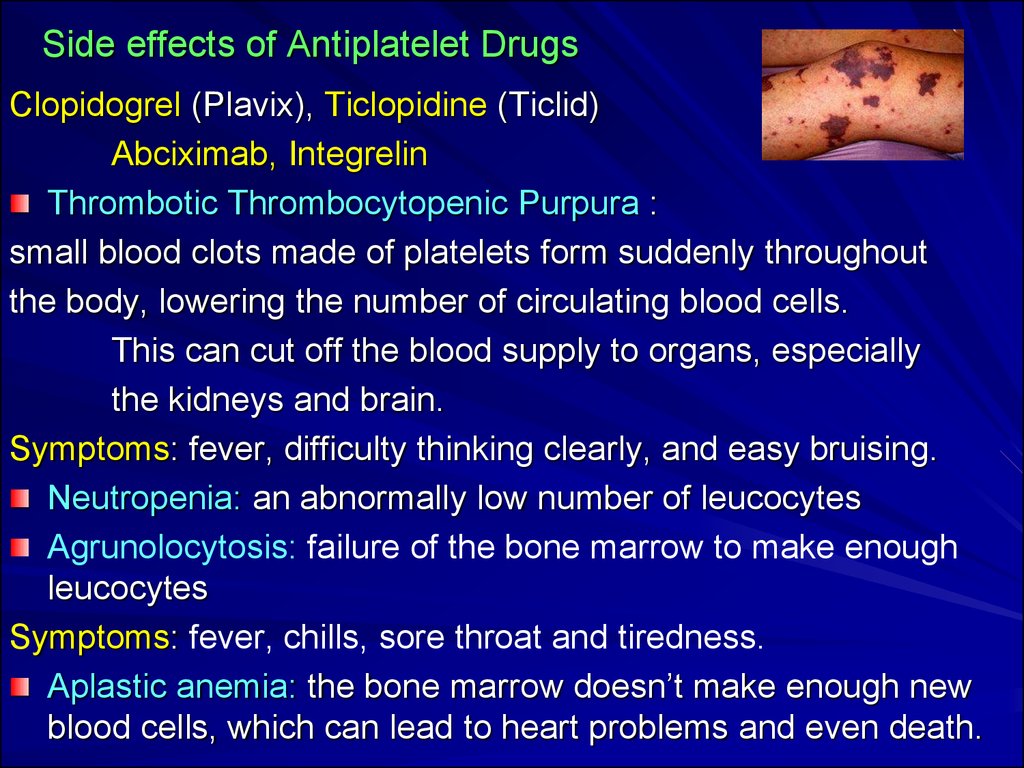 My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
In my opinion, the use of immunomodulators during pregnancy is IMPOSSIBLE:
* In this case, herpes on the lips of a woman cannot bring any harm to either the woman or the child.
*Long-term effect of immunomodulatory drugs on the fetus is unknown. As you know, some of these drugs, easily penetrating the placenta into the body of the fetus, can cause congenital deformities in the latter, disorders of the immune system, and increase the risk of developing cancer.