What causes bad headaches during pregnancy
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Headaches in women can often be triggered by a change in hormones during pregnancy. Expectant mothers may experience an increase or decrease in the number of headaches. Unexplained, frequent headaches later in your pregnancy could be a sign of a more serious condition called pre-eclampsia, so tell your doctor if this is the case.
Causes of headache during pregnancy
Many women experience headaches during pregnancy, especially in the first and third trimesters. If you're pregnant, you may notice an increase in the number of headaches you have at around week 9 of your pregnancy.
As well as hormonal changes, headaches in the early stages of pregnancy can be caused by an increase in the volume of blood your body is producing.
Other causes of headaches during pregnancy can include:
- not getting enough sleep
- withdrawal from caffeine (e.g. in coffee, tea or cola drinks)
- low blood sugar
- dehydration
- feeling stressed
- poor posture, particularly as your baby gets bigger
- having depression or anxiety
Migraine
Migraine is a particular type of headache that mostly occurs on one side of the head – it can be either moderate or very painful. People who experience migraine can also feel sick or vomit, and be sensitive to light or sound.
In pregnancy, migraine may get worse for the first few months, but for many women it can improve in the later stages of their pregnancy when the level of the hormone oestrogen stabilises. Other women may experience no change or a decrease in the number of migraine headaches while pregnant.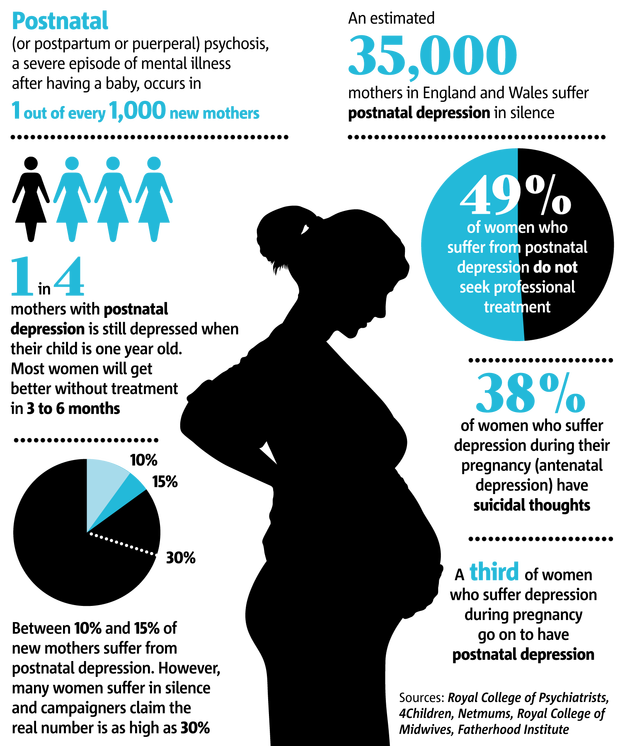 Some women may experience differences in migraine during different pregnancies.
Some women may experience differences in migraine during different pregnancies.
Treatment
It’s not advisable for pregnant women with migraine to use migraine medicine. For other headaches it's also recommended that you try to treat your headache without medicine.
You could try:
- getting more sleep or rest and relaxation
- pregnancy yoga classes or other exercise
- practising good posture, particularly later in your pregnancy
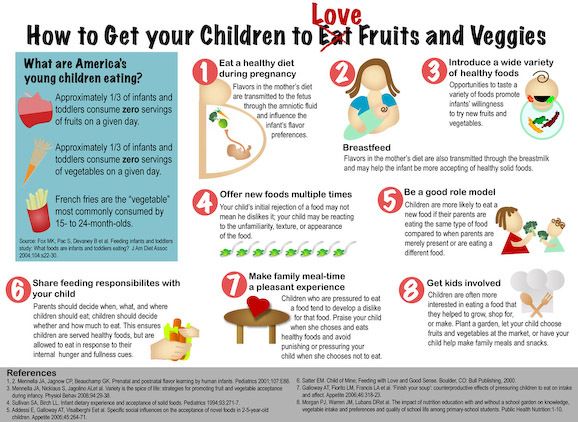
- eating regular, well-balanced meals
- putting a warm facecloth on your eye and nose area, if it is a sinus headache
- putting a cold pack on the back of your neck, taking a bath or using a heat pack, if it is a tension headache
- neck and shoulders massage
Pregnant women who experience migraine should avoid things that may trigger their migraine. This may include:
- chocolate
- yoghurt
- peanuts
- bread
- sour cream
- preserved meats
- aged cheese
- monosodium glutamate (MSG)
- caffeine (withdrawal from)
- bright or flickering lights
- strong smells
- loud sounds
- computer or movie screens
- sudden or excessive exercise
- emotional triggers such as arguments or stress
If you do take medicine for your headache or migraine you should check with your doctor, pharmacist or midwife first. Paracetamol, with or without codeine, is generally considered safe for pregnant women to use but you should avoid using other pain medicine such as aspirin or ibuprofen.
Paracetamol, with or without codeine, is generally considered safe for pregnant women to use but you should avoid using other pain medicine such as aspirin or ibuprofen.
When to contact your doctor
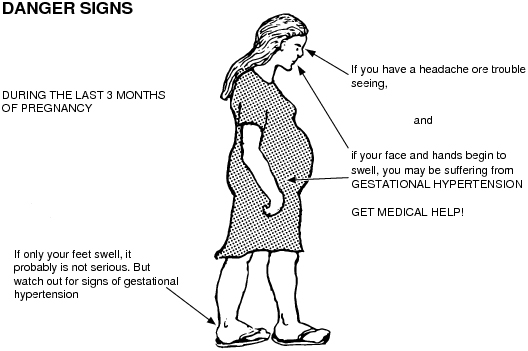
If you experience frequent headaches that don't go away with paracetamol, it could be a sign of a more serious medical condition called pre-eclampsia. This usually involves an increase in the pregnant woman's blood pressure and problems with her kidneys. There are also other serious risks for both you and your baby. Pre-eclampsia mostly occurs in the second half of pregnancy.
Contact your doctor, particularly if, along with your headaches, you have a pain below your ribs, feel like you have heartburn, you suddenly swell in your face, hands or feet, or you have problems with your eyesight.
Further information
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia
- Phone Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.

- For more information about headaches during pregnancy, visit Headache Australia.
- For more information about medication during pregnancy, see your doctor or pharmacist, or visit NPS MedicineWise.
Sources:
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Pre-eclampsia and high blood pressure during pregnancy), Headache Australia (Migraine), Women's and Children's Health Network (Medicines during pregnancy), Headache Australia (Adults and headache), Headache Australia (Migraine – A common and distressing disorder), Raising Children Network (9 weeks pregnant), Raising Children Network (34 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Perinatal Anxiety and Depression), American Pregnancy Association (Pregnancy and Headaches), NPS Medicinewise (Taking medicines in pregnancy), Australian and New Zealand College of Obstetricians and Gynaecologists (Is paracetamol safe to use in pregnancy?)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Common discomforts during pregnancy
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What Causes Them and What You Can Do
If you’re pregnant and having headaches, you’re not alone. A medical review reports that 39 percent of pregnant and postpartum women have headaches.
Though during pregnancy you may have a different kind of headache than you usually do, most headaches during pregnancy aren’t harmful.
Headache pain during the first trimester of pregnancy may happen for different reasons than headaches in the second or third trimester. In some cases, headache pain may be a sign of other health problems during pregnancy.
Tell your doctor about any headache you have during, before, and after pregnancy. Keep a journal to record how often you have headaches and how serious the pain is. Additionally, record any other symptoms you have.
Keep a journal to record how often you have headaches and how serious the pain is. Additionally, record any other symptoms you have.
Most headaches during pregnancy are primary headaches. This means that the headache pain happens by itself. It’s not a sign or symptom of another disorder or a complication in the pregnancy. Primary headaches include:
- tension headaches
- migraine attacks
- cluster headaches
About 26 percent of headaches during pregnancy are tension headaches. Tell your doctor if you have chronic headaches or migraine during pregnancy or if you have a history of migraine.
Some women with a history of migraine get fewer migraine attacks during pregnancy. Migraine has also been linked to complications that happen later in pregnancy or after the birth of your baby.
Secondary headaches are a caused by a complication in the pregnancy, such as high blood pressure.
Headache pain may vary from one person to the next. You may have:
- dull ache
- throbbing or pulsating pain
- severe pain on one or both sides
- sharp pain behind one or both eyes
Migraine pain may also include:
- nausea
- vomiting
- seeing lines or flashes of light
- blind spots
First trimester
Tension headaches are common in the first trimester of your pregnancy. This may happen because your body is undergoing several changes at this time. These changes may trigger headache pain:
This may happen because your body is undergoing several changes at this time. These changes may trigger headache pain:
- hormonal changes
- higher blood volume
- weight changes
Common causes of headache pain during the first trimester of pregnancy also include:
- dehydration
- nausea and vomiting
- stress
- lack of sleep
- caffeine withdrawal
- poor nutrition
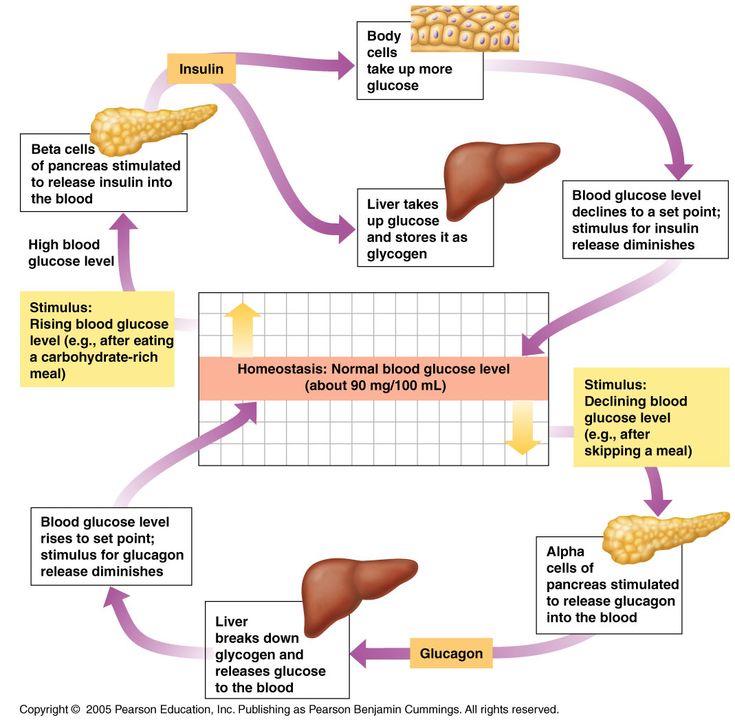
- low blood sugar levels
- too little physical activity
- sensitivity to light
- changes in vision
Some foods may also cause headaches. Your trigger foods may change during pregnancy. Common foods that may cause headaches in some people include:
- dairy
- chocolate
- cheese
- yeast
- tomatoes
Second and third trimester
Headaches during your second and third trimester may have different causes. These include:
- extra weight
- posture
- too little sleep
- diet
- muscle strain and tightness
- high blood pressure
- diabetes
High blood pressure
Headaches during your second or third trimester of pregnancy may be a sign that you have high blood pressure. About 6 to 8 percent of pregnant women ages 20 to 44 in the United States have high blood pressure.
About 6 to 8 percent of pregnant women ages 20 to 44 in the United States have high blood pressure.
The Centers for Disease Control and Prevention (CDC) warns that this treatable condition can cause serious complications for both mother and baby. This is most common after week 20 of pregnancy.
If you’re pregnant, high blood pressure can raise the risk of:
- stroke
- preeclampsia
- eclampsia
- low oxygen flow to the baby
- preterm delivery, before 37 weeks
- placental abruption
- low baby birth weight, which is less than 5 pounds, 8 ounces
Treatment for hypertension during pregnancy
Your doctor may prescribe medication to treat your high blood pressure. You’ll also need to cut down on salt and add more fiber to your daily diet. Regular exercise is also very important to help balance your blood pressure.
Other causes of headache during pregnancy include common infections and more serious illnesses:
- sinus infection
- low blood pressure
- blood clots
- bleeding
- sickle cell anemia
- brain tumor
- aneurysm
- stroke
- heart conditions
- meningitis or encephalitis
Talk to your doctor before taking your regular headache pain medication during pregnancy. Don’t take aspirin and ibuprofen (Advil, Motrin etc.).
Don’t take aspirin and ibuprofen (Advil, Motrin etc.).
The CDC warns that these pain relief drugs can be harmful to your growing baby, especially if taken during the first trimester. Many women may take acetaminophen (Tylenol) during pregnancy. However, some studies suggest there may be effects from taking acetaminophen as well.
Your doctor can recommend alternative medications to treat headache during pregnancy and natural headache remedies, such as:
- drinking plenty of water
- rest
- ice pack
- heating pad
- massage
- exercise and stretching
- essential oils, such as peppermint, rosemary, and chamomile
When to see your doctorSee your doctor if you have any headache pain at all during pregnancy. Get urgent medical attention if you have:
- fever
- nausea and vomiting
- blurred vision
- severe pain
- headache that lasts longer than a few hours
- frequent headache pain
- fainting
- seizure
Your doctor may recommend tests and scans to find out the cause of your headaches. These include:
These include:
- checking your blood pressure
- blood test
- blood sugar test
- vision test
- ultrasound of the head and neck
- heart or head scan
- checking eye health with a scope
- spine puncture
Headache pain during pregnancy is common. You may have tension headaches during your first trimester of pregnancy. This may happen because of the many changes that you’re going through in a short period.
Headache pain may happen in the second and third period of your pregnancy for other reasons. Some causes of headaches in your mid to late pregnancy may be serious.
High blood pressure is a serious cause of headache pain during pregnancy. You can have high blood pressure at any time in your pregnancy. You may not have any symptoms at all. Check your blood pressure at least once a day with a home monitor.
Tell your doctor if you have headaches at any time in your pregnancy. Let your doctor know right away if you have a personal or family history of migraine, high blood pressure, seizures or diabetes.
Take all medications and treatment exactly as prescribed by your doctor. Follow all diet and exercise advice carefully. See your doctor for all follow-up and regular check-ups. Most causes of headaches during pregnancy are treatable or preventable with the right care.
For more pregnancy guidance and weekly tips tailored to your due date, sign up for our I’m Expecting newsletter.
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.

Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations. This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make seizures less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods.
 Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted.
 However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Follow our Instagram to read the latest materials on the diagnosis and treatment of headaches!
cluster headache. Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Headache during pregnancy: where does it come from and how to get rid of it
Share
0When to call an ambulance
Call 103 or 112 urgently if you experience the following symptoms:
- sudden and severe headache;
- consciousness becomes confused or completely lost;
- pain worsens over 5 minutes;
- flies, spots flash in the eyes;
- throbbing and noisy in the ears;
- speech has become slurred, words are drawn out;
- arms and legs weaken, convulsions set in;
- the muscles of the neck are very stiff, it is impossible to reach the chest with the chin;
- temperature rises to 39 °C or more;
- increased heart rate at rest;
- severe shortness of breath;
- the child pushes without stopping or stops abruptly;
- leaking water or blood;
- pain in the lower abdomen, as if contractions had begun.

Why pregnant women can get headaches
Pregnancy headaches are not always life threatening. But the doctor needs to be told about it in any case. If the symptom appeared for the first time and does not hurt much, postpone the conversation until a scheduled visit. If your headache is recurring or gets worse, it's best to make an appointment as soon as possible. The gynecologist will decide what needs to be done or refer you to another doctor.
There are many causes of headaches. Scientists have found that in pregnant women in 57% of cases it is primary, that is, not associated with other diseases. The most common are migraines and tension headaches.
Everything else is a secondary headache caused by various pathologies. Usually it is high blood pressure and infections. But there are also more dangerous reasons.
1. Stress and fatigue
A pregnant woman's body experiences increased stress, because it has to work for two. If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she develops a tension headache.
Discomfort lasts from 30 minutes to several days. The head hurts in the forehead, occiput, both temples. But there is no feeling that they put on a tight hoop or helmet. The pain does not get worse when bending over, walking, or climbing stairs, bright lights, or sounds.
What to do
Tension headache can go away on its own: just get some fresh air or sleep. Sometimes pleasant emotions help, which distract from experiences.
If the pain persists for 2-3 consecutive days, see a doctor. He will select painkillers that are safe for the child.
2. Taking medications
Any medication that enters the stomach or blood can cause headaches even if the dosage is correct. In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
Long-term use of non-steroidal anti-inflammatory drugs for headaches may cause the opposite effect: the pills do not remove, but provoke symptoms.
What to do
If your head hurts a few hours after taking the medicine, you need to see a doctor to change the medicine. Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
3. Love or refusal to coffee
Coffee can cause headaches during pregnancy. Unpleasant symptoms occur if you drink more than 3-4 cups a day.
Abrupt refusal of coffee is also harmful. It is worth finding out about pregnancy and stopping brewing a fragrant drink, and after 1-2 days, aching pain will appear in the temples and the back of the head.
What to do
Coffee is best avoided during pregnancy. If a headache occurs a day after this, you can drink a small cup of the drink and wait a day again. Gradually, the dependence on coffee will pass.
Coffee drinkers can reduce their drink intake to 1-2 cups per day.
4. Infection with fever
Acute viral (usually SARS) or bacterial (eg, streptococcal tonsillitis) infections cause fever and headache. This is a normal reaction to foreign microorganisms.
But any infection is dangerous for pregnant women. It can cause fetal defects, growth retardation and even miscarriage. And with meningitis, especially listeriosis, there is a threat to the life of the mother.
What to do
If you have a headache with fever, call your doctor. He will prescribe safe medications or give you a referral to the hospital if a severe infection is suspected. In this case, you need strong antibiotics, droppers to maintain the body and sometimes hormones.
5. Preeclampsia and preeclampsia
After 20 weeks, preeclampsia may develop in pregnant women. This is a disease in which one of three symptoms or a combination of them may appear: high blood pressure, edema, and protein in the urine.
Without proper treatment, preeclampsia turns into preeclampsia. The pressure rises sharply, the head and lower abdomen hurt unbearably, the baby pushes unusually hard or, on the contrary, suddenly calms down. Preeclampsia can lead to placental abruption, damage to the liver and other organs, bleeding, and even seizures. Without urgent medical care, the fetus and mother die.
Without urgent medical care, the fetus and mother die.
What to do
When the first signs of preeclampsia appear, the pregnant woman is hospitalized to find treatment. After that, she is discharged home under the supervision of her gynecologist.
But if her health worsens, the doctor again sends the woman to the hospital, where she is prescribed medicines to reduce pressure, special droppers to keep her body functioning. If improvement does not occur within a day, a caesarean section is performed.
6. Migraine
One of the causes of migraine is a change in estrogen levels. But the disease very rarely appears due to pregnancy. On the contrary, in 70% of women, the symptoms subside dramatically after conception. Nevertheless, migraines torment many.
It may begin with an aura: flashes of light, spots before the eyes, tingling in the hands or numbness of half of the face, sometimes tinnitus. Each symptom can last from 20 minutes to an hour.
A migraine attack develops after the aura. In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
Seizures last from a few hours to a week or more. After a migraine, there is a feeling of severe fatigue, exhaustion, and an awkward turn of the head can return the pain.
What to do
Any medication for migraine during pregnancy must be prescribed by a doctor. In some cases, drugs from the group of beta-blockers are used.
Studies have shown that frequent migraine in pregnancy is associated with a lack of magnesium. The doctor will help you choose the appropriate type of vitamin and mineral complex and its dosage.
7. Cerebral vascular disease
Hormone problems in some pregnant women increase blood clotting, which increases the risk of thrombosis, stroke, or bleeding in the meninges. These conditions are very dangerous: a woman can die within a few minutes or remain disabled.
Vascular involvement is always accompanied by several symptoms:
- severe headache on one side;
- nausea and vomiting;
- blurred vision;
- loss of consciousness;
- convulsions.
What to do
Urgently call an ambulance. The pregnant woman must be laid or seated so that she does not hit when she falls. You can't give medicine! You can only open the window so that there is more air in the room.
Which treatment the doctor prescribes depends on the specific disease. These can be drugs that reduce blood clotting and dissolve blood clots. In some cases, urgent surgery is needed.
8. Brain tumors
Studies show that progesterone and estrogen during pregnancy can trigger or accelerate the growth of tumors in the brain. Symptoms of the disease appear slowly, over several months, and depend on the size and location of the tumor.
Headache may gradually increase, then vision, speech, hearing deteriorate, limbs go numb and convulsions appear. Sometimes it is difficult for a woman to keep her balance.
Sometimes it is difficult for a woman to keep her balance.
What to do
If a pregnant woman often has a headache or she forgets what she wanted to buy in the store and how to cook her favorite borscht, confuses her way home, you need to go to a neurologist. First, he will prescribe standard treatment, simple and safe medicines, rest, good sleep.
If this does not help, the symptoms persist or worsen, a deep examination is required. The pregnant woman will be sent for an MRI of the brain. This procedure is safe for the fetus. If the diagnosis is confirmed, surgery may be required.
What to do if the doctor cannot find the cause of the pain
If you have been examined and the doctor cannot tell you why your head hurts and diagnoses you with vascular dystonia, this is a reason to be wary. There is no such disease.
Look for another doctor. Perhaps he uses new diagnostic methods that will help to deal with the problem and choose a treatment.