Pregnant stomach burning sensation
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms. However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
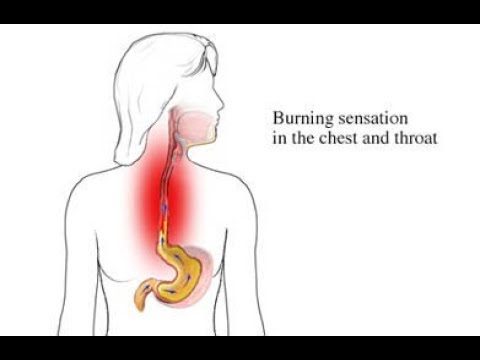
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Feeling the burn? Tips to manage heartburn, GERD in pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
July 30, 2019
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
Alan Kramer, M.P.H. Assistant Vice President for Health System Emerging Strategies
The pregnancy hormone progesterone can increase heartburn, starting in the first trimester.Heartburn is common in adults – especially during pregnancy. While some research suggests women who have moderate heartburn during pregnancy give birth to babies with fuller heads of hair, having symptoms more than twice a week might be a sign of gastroesophageal reflux disease (GERD), or recurrent heartburn.
According to a study of 510 pregnant women, approximately 26% have GERD symptoms during the first trimester. The rate jumps to 36% in the second trimester and 51% during the third trimester. That’s substantial compared with the 20% of adults in the U.S. who experience heartburn.
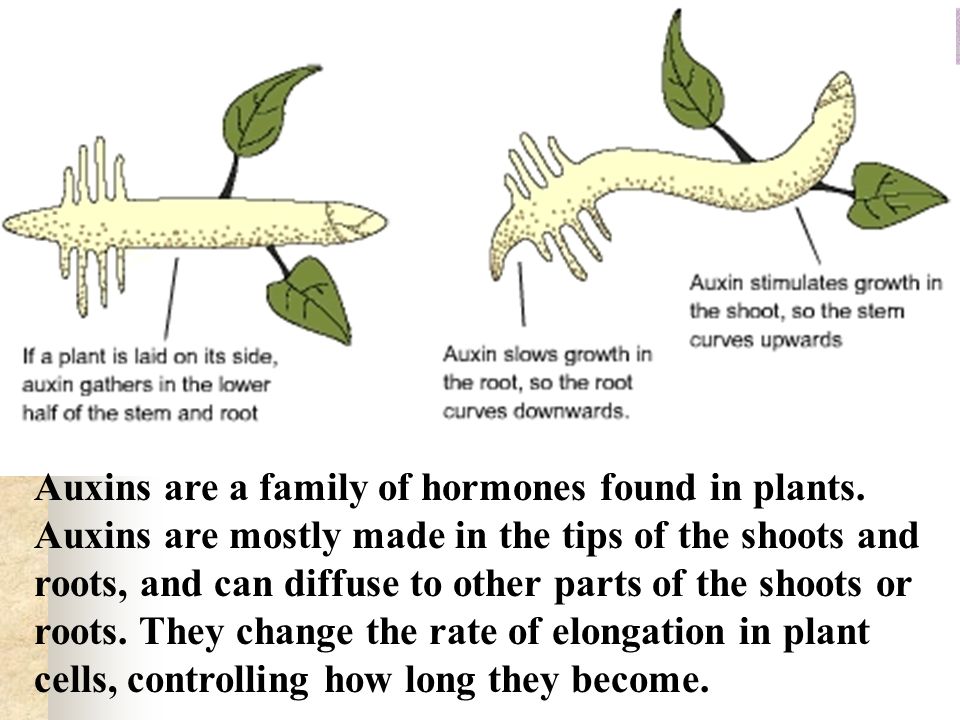
Why the increase in symptoms during pregnancy? Progesterone, a hormone that increases early in pregnancy, relaxes smooth muscle in the body. It helps your uterus stretch to accommodate the growing fetus, but also reduces the reliability of the esophageal sphincter – a ring-like structure that seals off stomach contents from the throat.
Increased pressure placed on the stomach externally from the growing uterus, especially in the third trimester, can also worsen heartburn symptoms such as:
- Burning pain in the center of the chest, especially after eating
- Sour or bitter taste in the mouth
- Sore throat or cough
Thankfully, there are several pregnancy-safe ways to deal with acute heartburn and ongoing cases of GERD.
"Progesterone, a hormone that increases early in pregnancy, also reduces the reliability of the esophageal sphincter, which means that certain foods such as spicy dishes may trigger heartburn symptoms."
Robyn Horsager-Boehrer, M.D.
Heartburn treatment options during pregnancy
Lifestyle changes
Consider these diet and sleep modifications to relieve or prevent heartburn:
- Avoid tobacco and alcohol. These substances worsen the symptoms, and it’s already recommended for all women during pregnancy to avoid smoking, vaping, and drinking alcohol. Need to quit? We offer a free tobacco cessation program.
- Shift your eating schedule. Smaller, more frequent meals fill the stomach less and may reduce symptoms. Also, avoid bending over or lying flat after meals to reduce acid reflux.

- Prop yourself up in bed. Try sleeping with an extra pillow under your head or a small wedge under your pillow. The incline can help prevent stomach acid from splashing into your lower esophagus.
- Skip the sauce or spice. If you notice that certain foods such as tomato sauces or spicy dishes trigger symptoms, avoid them until after the baby comes.
Medications
Heartburn and GERD symptoms are less severe when there is less acid in the stomach. That said, you need a certain amount of acid to properly digest food. Three types of medication can help create that balance.
Oral antacids like aluminum and magnesium hydroxide (think Maalox or Mylanta) and calcium carbonate (like TUMS) neutralize acid already present in the stomach. Calcium carbonate has the added benefit of supplementing calcium intake during pregnancy. It’s safe to follow the directions on the package – there’s no need to change the dosage or schedule due to pregnancy.
It’s safe to follow the directions on the package – there’s no need to change the dosage or schedule due to pregnancy.
On the flip side, two types of medications actually reduce acid production before it can enter the stomach.
h3-receptor antagonists (h3-blockers) reduce h3 histamine, which stimulates cells in the stomach to produce acid. Thus, less stomach acid is produced. Examples include ranitidine (Zantac), cimetidine (Tagamet HB), and famotidine (Pepcid). All of these are available over the counter and in generic forms.
Proton pump inhibitors (PPIs) block an enzyme in stomach cells that’s needed to produce acid. These drugs are available over the counter but can take several days to provide maximum relief, so you might consider trying an antacid or h3 blocker first. Examples of PPIs include lansoprazole (Prevacid) and omeprazole (Prilosec), as well as generic versions. Both brand name and generic are considered safe during pregnancy.
Please note, because stomach acid is necessary for iron absorption, h3 blockers and PPIs can decrease the effectiveness of iron supplements. Talk to your doctor if this might be an issue for you.
Talk to your doctor if this might be an issue for you.
Related reading: 4 common pregnancy-related GI issues
When to call the doctor
If heartburn symptoms are associated with headaches or swelling of the hands and face, talk with your provider before trying these remedies, especially if the symptoms are new and present in the last trimester of pregnancy.
Heartburn-like pain can be a symptom of preeclampsia, or dangerously high blood pressure during pregnancy. Preeclampsia puts mothers and babies at risk, and further evaluation may be necessary.
As mentioned, heartburn is very common in pregnancy. If your symptoms don’t resolve with diet changes or medication, let your provider know so you can find an effective treatment.
Tired of feeling the burn? Call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.D.
August 23, 2022
More Articles
© 2022 The University of Texas Southwestern Medical Center
Member of Southwestern Health Resources
Toxemia, Intestinal Problems, and Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.

During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 1–13 weeks | 900 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid reflux | Constipation Acid Office 9000 9000 9000 9000 Flatulence Constipation Heartburn Violation of the outflow of bile Hemorrhoids |
The Atlas Genetic Test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.

Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a vacation in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Blood or mucus stools;
- Sudden weight loss;
- Pain in the abdomen;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially in the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve bowel movements and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for future pregnancy and reduce the risk of digestive problems.
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems in the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.
 S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy
S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy - Robyn Horsager-Boehrer, M.D., UT Southwestern Medical Center, Should pregnant moms be concerned about gastroenteritis?, 2018
- International Foundation for Gastrointestinal Disorders, Pregnancy and Irritable Bowel Syndrome, 2016
- NHS Vomiting and morning sickness in pregnancy
- NHS, Severe vomiting in pregnancy
- Lindsey J Wegrzyniak et al., Treatment of Hyperemesis Gravidarum, 2012
- Karen Miles, Diarrhea during pregnancy, 2020
- Cleveland Clinic, Diarrhea
- You and your hormones, Progesterone
- Traci C. Johnson, MD, Pregnancy, Bloating, 2020
Article "Pregnancy and heartburn"
Hormonal changes that the body undergoes during pregnancy is the root cause of heartburn. In early pregnancy, the ovaries, and then the placenta, produce the hormone progesterone, one of the main functions of which is to relax the smooth muscles of the body, including the muscles of the uterus. Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn.
Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn.
Another cause of heartburn in pregnant women is a weakening of motility - the wave-like movement of the gastrointestinal tract, slowing down the processes of digestion. Food passes through the digestive tract more slowly, lingering in the stomach. Heartburn in pregnant women is also provoked by the large size of the uterus, which increases intra-abdominal pressure and increases pressure on all the internal organs of the pregnant woman - the stomach and intestines as well. The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn.
The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn.
Heartburn can start at any stage of pregnancy, but is most common in the second and third trimesters. As a rule, discomfort occurs after 24 weeks, when the uterus rises above the navel, and becomes especially severe after 30 weeks. Especially intense heartburn can be in a woman if she had an increased acidity of gastric juice before pregnancy.
To avoid heartburn during pregnancy, first of all, you need to review your menu and exclude fatty, fried, spicy, salty foods from it, you must give up coffee and carbonated drinks. Include cereals, dairy products, lean meats and mashed vegetables in the diet. It is advisable to eat often and in small portions every 1.5-2 hours. Spend more time eating, remember to chew food thoroughly so that it is digested properly. Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it.
Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it.
At the first signs of heartburn, you can drink a small amount of alkaline mineral water without gas or take a few sips of low-fat milk. Drink should be in small sips. Kissels work well. They envelop the esophagus and thus reduce burning sensation. The safest in the treatment of heartburn in pregnant women are antacids containing sodium bicarbonate, calcium carbonate, preparations containing magnesium and other substances. Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus.