What about teenage pregnancy
Adolescent pregnancy
Adolescent pregnancy- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- WHO's Health Emergency Appeal 2023
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Programme Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Member States Portal
- Home/
- Newsroom/
- Fact sheets/
- Detail/
- Adolescent pregnancy
UNICEF/Versiani
© Credits
","datePublished":"2022-09-15T09:05:00. 0000000+00:00","image":"https://cdn.who.int/media/images/default-source/imported/adolescent-pregnancy.jpg?sfvrsn=792a9e8_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-09-15T09:05:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy","@context":"http://schema.org","@type":"Article"};
Key facts
- As of 2019, adolescents aged 15–19 years in low- and middle-income countries (LMICs) had an estimated 21 million pregnancies each year, of which approximately 50% were unintended and which resulted in an estimated 12 million births (1)(2).
- Data on childbirths among girls aged 10–14 are not widely available; limited available data from Angola, Bangladesh, Mozambique and Nigeria point to birth rates in this age group exceeding 10 births per 1000 girls as of 2020 (3).

- Based on 2019 data, 55% of unintended pregnancies among adolescent girls aged 15–19 years end in abortions, which are often unsafe in LMICs (1).
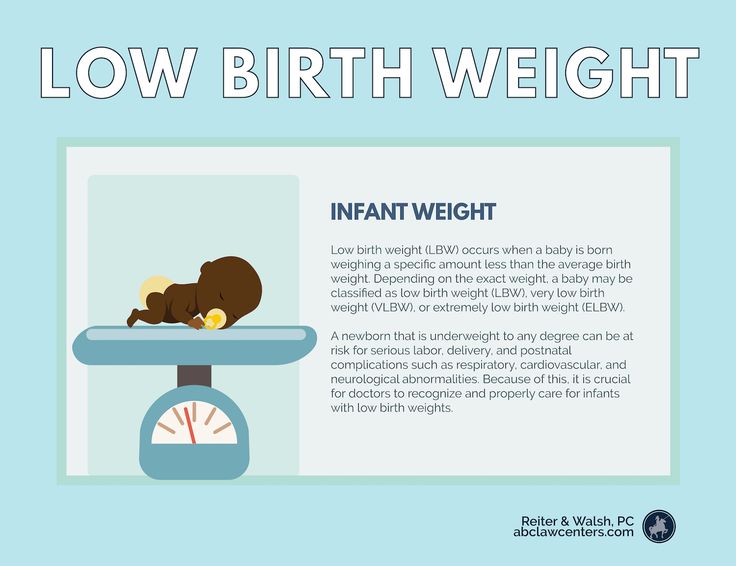
- Adolescent mothers (aged 10–19 years) face higher risks of eclampsia, puerperal endometritis and systemic infections than women aged 20–24 years, and babies of adolescent mothers face higher risks of low birth weight, preterm birth and severe neonatal condition.
- Preventing pregnancy among adolescents and pregnancy-related mortality and morbidity are foundational to achieving positive health outcomes across the life course and imperative for achieving the Sustainable Development Goals (SDGs) related to maternal and newborn health.
Overview
Adolescent pregnancy is a global phenomenon with clearly known causes and serious health, social and economic consequences. Globally, the adolescent birth rate (ABR) has decreased, but rates of change have been uneven across regions. There are also enormous variations in levels between and within countries. Adolescent pregnancy tends to be higher among those with less education or of low economic status. Further, there is slower progress in reducing adolescent first births amongst these and other vulnerable groups, leading to increasing inequity. Child marriage and child sexual abuse place girls at increased risk of pregnancy, often unintended. In many places, barriers to obtaining and using contraceptives prevent adolescents from avoiding unintended pregnancies. There is growing attention being paid to improving access to quality maternal care for pregnant and parenting adolescents. WHO works with partners to advocate for attention to adolescent pregnancy, to build an evidence base for action, to develop policy and programme support tools, to build capacity and to support countries to address adolescent pregnancy effectively.
Adolescent pregnancy tends to be higher among those with less education or of low economic status. Further, there is slower progress in reducing adolescent first births amongst these and other vulnerable groups, leading to increasing inequity. Child marriage and child sexual abuse place girls at increased risk of pregnancy, often unintended. In many places, barriers to obtaining and using contraceptives prevent adolescents from avoiding unintended pregnancies. There is growing attention being paid to improving access to quality maternal care for pregnant and parenting adolescents. WHO works with partners to advocate for attention to adolescent pregnancy, to build an evidence base for action, to develop policy and programme support tools, to build capacity and to support countries to address adolescent pregnancy effectively.
Scope of the problem
Every year, an estimated 21 million girls aged 15–19 years in developing regions become pregnant and approximately 12 million of them give birth (1).
Globally, ABR has decreased from 64.5 births per 1000 women in 2000 to 42.5 births per 1000 women in 2021. However, rates of change have been uneven in different regions of the world with the sharpest decline in Southern Asia (SA), and slower declines in the Latin American and Caribbean (LAC) and sub-Saharan Africa (SSA) regions. Although declines have occurred in all regions, SSA and LAC continue to have the highest rates globally at 101 and 53.2 births per 1000 women, respectively, in 2021 (4).
There are enormous differences within regions in ABR as well. In LAC, for example, Nicaragua recorded the highest estimated ABR at 85.6 per 1000 adolescent girls in 2021, compared to 24.1 per 1000 adolescent girls in Chile (4). Even within countries, there are enormous variations, for example in Zambia the percentage of adolescent girls aged 15–19 who have begun childbearing (women who either have had a birth or are pregnant at the time of interview) ranged from 14. 9% in Lusaka to 42.5% in the Southern Province in 2018 (5). In the Philippines, this ranged from 3.5% in the Cordillera Administrative Region to 17.9% in the Davao Peninsula Region in 2017 (6).
9% in Lusaka to 42.5% in the Southern Province in 2018 (5). In the Philippines, this ranged from 3.5% in the Cordillera Administrative Region to 17.9% in the Davao Peninsula Region in 2017 (6).
While the estimated global ABR has declined, the actual number of childbirths to adolescents continues to be high. The largest number of estimated births to 15–19-year-olds in 2021 occurred in SSA (6 114 000), whereas far fewer births occurred in Central Asia (68 000). The corresponding number was 332 000 among adolescents aged 10–14 years in SSA, compared to 22 000 in South-East Asia (SEA) in the same year (4).
Context in which adolescent pregnancies occur
Studies of risk and protective factors related to adolescent pregnancy in LMICs indicate that levels tend to be higher among those with less education or of low economic status (7). Progress in reducing adolescent first births has been particularly slow amongst these vulnerable groups, leading to increasing inequity.
Several factors contribute to adolescent pregnancies and births. First, in many societies, girls are under pressure to marry and bear children. As of 2021, the estimated global number of child brides was 650 million: child marriage places girls at increased risk of pregnancy because girls who are married very early typically have limited autonomy to influence decision-making about delaying child-bearing and contraceptive use Second, in many places, girls choose to become pregnant because they have limited educational and employment prospects. Often in such societies, motherhood – within or outside marriage/union – is valued, and marriage or union and childbearing may be the best of the limited options available to adolescent girls.
Contraceptives are not easily accessible to adolescents in many places. Even when adolescents can obtain contraceptives, they may lack the agency or the resources to pay for them, knowledge on where to obtain them and how to correctly use them. They may face stigma when trying to obtain contraceptives. Further, they are often at higher risk of discontinuing use due to side effects, and due to changing life circumstances and reproductive intentions
They may face stigma when trying to obtain contraceptives. Further, they are often at higher risk of discontinuing use due to side effects, and due to changing life circumstances and reproductive intentions. Restrictive laws and policies regarding the provision of contraceptives based on age or marital status pose an important barrier to the provision and uptake of contraceptives among adolescents. This is often combined with health worker bias and/or lack of willingness to acknowledge adolescents’ sexual health needs.
Child sexual abuse increases the risk of unintended pregnancies. A WHO report dated 2020 estimates that 120 million girls aged under 20 years have experienced some form of forced sexual contact. This abuse is deeply rooted in gender inequality; it affects more girls than boys, although many boys are also affected. Estimates suggest that in 2020, at least 1 in 8 of the world’s children had been sexually abused before reaching the age of 18, and 1 in 20 girls aged 15–19 years had experienced forced sex during their lifetime.
The WHO report titled Violence against women prevalence estimates 2018 notes that “adolescents aged 15–19 years (24%) are estimated to have already been subjected to physical and/or sexual violence from an intimate partner at least once in their lifetime, and 16% of adolescent girls and young women aged 15–24 have been subjected to this violence within the past 12 months.”
Preventing adolescent pregnancy and childbearing as well as child marriage is part of the SDG agenda with dedicated indicators, including indicator 3.7.2, “Adolescent birth rate (aged 10–14 years; aged 15–19 years) per 1000 women in that age group,” and 5.3.1, “Proportion of women aged 20–24 years married before the age of 18 years.”
Strategies and interventions related to adolescent pregnancy have focused on pregnancy prevention. However, there is growing attention being paid to improving access to and quality of maternal care for pregnant and parenting adolescents. Available data on access paints a mixed picture. Access to quality care depends on the geographic context and the social status of adolescents. Even where access is not limited, adolescents appear to receive a lower quality of both clinical care and interpersonal support than adult women do.
Access to quality care depends on the geographic context and the social status of adolescents. Even where access is not limited, adolescents appear to receive a lower quality of both clinical care and interpersonal support than adult women do.
WHO response
WHO works with partners to advocate for attention to adolescents, build the evidence and epidemiologic base for action, develop and test programme support tools, build capacity, and pilot initiatives in the small but growing number of countries that began to recognize the need to address adolescents’ sexual and reproductive health. As a result of these collective efforts, adolescent health has moved to the centre of the global health and development agenda. In this changed context, WHO continues its work on advocacy, evidence generation, tool development and capacity building, while working with partners within and outside the United Nations system to support countries to address adolescent pregnancy effectively in the context of their national programmes.
Adolescent pregnancy is a global phenomenon with clearly known causes and serious health, social and economic consequences to individuals, families and communities. There is consensus on the evidence-based actions needed to prevent it. There is growing global, regional and national commitment to preventing child marriage and adolescent pregnancy and childbearing. Nongovernmental organizations have led the effort in several countries. In a growing number of countries, governments are taking the lead to put in place large-scale programmes. They challenge and inspire other countries to do what is doable and urgently needs to be done – now.
References
- Sully EA, Biddlecom A, Daroch J, Riley T, Ashford L, Lince-Deroche N et al., Adding It Up: Investing in Sexual and Reproductive Health 2019. New York: Guttmacher Institute; 2020.
- Darroch J, Woog V, Bankole A, Ashford LS. Adding it up: Costs and benefits of meeting the contraceptive needs of adolescents.
 New York: Guttmacher Institute; 2016.
New York: Guttmacher Institute; 2016. - United Nations, Department of Economic and Social Affairs, Population Division. Fertility among young adolescents aged 10 to 14 years. New York: UNDESA, PD, 2020.
- United Nations Department of Economic and Social Affairs. World Population Prospects, 2019 Revision: Age-specific fertility rates by region, subregion and country, 1950-2100 (births per 1,000 women) Estimates. Online Edition [cited 2021 Dec 10]. Available from: https://population.un.org/wpp/Download/Standard/Fertility/
- Zambia Statistics Agency, Ministry of Health (MOH) Zambia, and ICF. Zambia Demographic and Health Survey 2018. Lusaka, Zambia, and Rockville, Maryland, USA: Zambia Statistics Agency, Ministry; 2018.
- Philippine Statistics Authority (PSA) and ICF. Philippines National Demographic and Health Survey 2017. Quezon City, Philippines, and Rockville, Maryland, USA: PSA and CF; 2018.
- Chung, W.
 H, Kim, ME., Lee, J. Comprehensive understanding of risk and protective factors related to adolescent pregnancy in low- and middle-income countries: A systematic review. Journal of Adolescence. 2018; 69: 180-188.
H, Kim, ME., Lee, J. Comprehensive understanding of risk and protective factors related to adolescent pregnancy in low- and middle-income countries: A systematic review. Journal of Adolescence. 2018; 69: 180-188.
About Teen Pregnancy | CDC
The US teen birth rate (births per 1,000 females aged 15 to 19 years) has been declining since 1991. Teen birth rates continued to decline from 17.4 per 1,000 females in 2018 to 16.7 per 1,000 females in 2019. This is another record low for US teens and a decrease of 4% from 2018.1,2 Birth rates fell 7% for females aged 15 to 17 years and 4% for females aged 18 to 19 years.2
Although reasons for the declines are not totally clear, evidence suggests these declines are due to more teens abstaining from sexual activity, and more teens who are sexually active using birth control than in previous years.3, 4
Still, the US teen birth rate is substantially higher than in other western industrialized nations,5 and racial/ethnic and geographic disparities in teen birth rates persist. 1,2
1,2
Disparities in Teen Birth Rates
Teen birth rates declined from 2018 to 2019 for several racial groups and for Hispanics.1,2 Among 15- to 19-year-olds, teen birth rates decreased:
- 5.2% for Hispanic females.
- 5.8% for non-Hispanic White females.
- 1.9% for non-Hispanic Black females.
Rates for non-Hispanic American Indian/Alaska Natives (AI/AN), non-Hispanic Asians, and non-Hispanic Native Hawaiian, and other Pacific Islander teenagers were unchanged.
In 2019, the birth rates for Hispanic teens (25.3) and non-Hispanic Black teens (25.8) were more than two times higher than the rate for non-Hispanic White teens (11.4). The birth rate of American Indian/Alaska Native teens (29.2) was highest among all race/ethnicities.1
Birth Rates for Females Aged 15 to 19 Years, by Race and Hispanic Origin of Mother: United States, 2018 and 2019
Data source: Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021;70(2):1–50.
Births: final data for 2019. Natl Vital Stat Rep. 2021;70(2):1–50.
Geographic differences in teen birth rates persist, both within and across states. Although among states with low overall teen birth rates, some counties have high teen birth rates.6
Social determinants of health, such as low education and low income levels of a teen’s family, may contribute to high teen birth rates.7 Teens in certain settings are at higher risk of teen pregnancy and birth than other groups. For example, young women living in foster care are more than twice as likely to become pregnant than young women not in foster care.8
To improve the life opportunities of adolescents facing significant health disparities and to have the greatest effect on overall US teen birth rates, CDC uses data to inform and direct interventions and resources to areas with the greatest need.
Top of Page
Evidence-based teen pregnancy prevention programs have been identified by the US Department of Health and Human Services (HHS) Teen Pregnancy Prevention Evidence Reviewexternal icon, which used a systematic process for reviewing evaluation studies against a rigorous standard. The Evidence Review covers a variety of diverse programs, including sexuality education programs, youth development programs, abstinence education programs, clinic-based programs, and programs specifically designed for diverse populations and settings. In addition to evidence-based prevention programs, teens need access to youth-friendly reproductive health services and support from parents and other trusted adults, who can play an important role in helping teens make healthy choices about relationships, sex, and birth control. Efforts at the community level that address social and economic factors associated with teen pregnancy also play a critical role in addressing racial/ethnic and geographical disparities observed in teen births in the United States.
The Evidence Review covers a variety of diverse programs, including sexuality education programs, youth development programs, abstinence education programs, clinic-based programs, and programs specifically designed for diverse populations and settings. In addition to evidence-based prevention programs, teens need access to youth-friendly reproductive health services and support from parents and other trusted adults, who can play an important role in helping teens make healthy choices about relationships, sex, and birth control. Efforts at the community level that address social and economic factors associated with teen pregnancy also play a critical role in addressing racial/ethnic and geographical disparities observed in teen births in the United States.
Top of Page
Teenage pregnancy. What is Teen Pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
Teenage pregnancy is the state of carrying a developing embryo and fetus by an underage teenage girl. Clinically manifested by the same signs as gestation in adults: the absence of regular menstruation, causeless nausea and vomiting, changes in taste habits, engorgement of the mammary glands, hyperpigmentation of the areola and nipples, weight gain, and an increase in abdominal circumference. When making a diagnosis, they use the data of a gynecological examination, the results of a pregnancy test and ultrasound of the uterus. When the patient decides to keep the child, management tactics are aimed at the timely detection and correction of complications, the choice of an appropriate method of delivery.
- Causes of teenage pregnancy
- Pathogenesis
- Classification
- Symptoms of teenage pregnancy
- Complications
- Diagnostics
- Management of teenage pregnancy
- Prognosis and prevention
- Prices for treatment
General
Teenage pregnancy is not only a medical problem, but also a social one. In developed countries, its prevalence reaches 12 cases per 1,000 adolescents, in Russia this figure is 8-9times higher. According to WHO, about 16 million girls aged 15-19 years old give birth to children every year, which is up to 11% of all births in the world. 95% of such cases are detected in countries with low and middle incomes. The level of teenage pregnancy is largely influenced by national and religious traditions - in Islamic states it is much less common. According to statistics, up to 30% of pregnancies in girls end in artificial interruption, 14% in miscarriage, and 56% in childbirth. Two thirds of minors give birth out of wedlock. According to the social status, 72% of patients study at school, vocational schools or are housewives.
In developed countries, its prevalence reaches 12 cases per 1,000 adolescents, in Russia this figure is 8-9times higher. According to WHO, about 16 million girls aged 15-19 years old give birth to children every year, which is up to 11% of all births in the world. 95% of such cases are detected in countries with low and middle incomes. The level of teenage pregnancy is largely influenced by national and religious traditions - in Islamic states it is much less common. According to statistics, up to 30% of pregnancies in girls end in artificial interruption, 14% in miscarriage, and 56% in childbirth. Two thirds of minors give birth out of wedlock. According to the social status, 72% of patients study at school, vocational schools or are housewives.
Teenage pregnancy
Causes of teenage pregnancy
Physiological opportunities for fertilization of the egg arise in the girl after the onset of the first menstruation (menarche). However, the real causes of early pregnancy are not related to the biological, but to the social aspect. The provocative factors differ in different countries and are largely determined by the level of economic development, the organization of education and medical care, local norms and traditions. According to experts in the field of obstetrics and gynecology, the onset of pregnancy in adolescence is facilitated by:
However, the real causes of early pregnancy are not related to the biological, but to the social aspect. The provocative factors differ in different countries and are largely determined by the level of economic development, the organization of education and medical care, local norms and traditions. According to experts in the field of obstetrics and gynecology, the onset of pregnancy in adolescence is facilitated by:
- Insufficient sexual education and education. Adolescents are not always fully aware of the consequences of unprotected sex, the need and rules for contraception. This is due to the lack of targeted programs for the sexual education of schoolchildren, the sanctimonious attitude of adults, and examples of the asocial lifestyle that parents lead.
- Sexual emancipation. 9 out of 10 girls have their first sexual experience before the age of 20. This is facilitated by the availability of low-alcohol drinks, narcotic substances, and pornographic materials.
 Studies have shown that teens who watch TV shows and movies with sex scenes are at twice the risk of early pregnancy.
Studies have shown that teens who watch TV shows and movies with sex scenes are at twice the risk of early pregnancy. - Contraceptive prejudice. There is still a persistent stereotype in society that the use of male barrier contraceptives reduces the severity of pleasure and affects the romanticism of relationships. As a result, some girls and young women, in fear of losing their partners, are embarrassed to ask them for condom protection.
- Sexual abuse. About 10% of pregnant adolescents under the age of 15 report the forced nature of their first sexual relationship. Often, coercion to have sex is caused by the girl's being in an unfavorable social environment, much less often it is an element of blackmail by a partner who threatens to end the romantic relationship.
- Poor socio-economic situation. This reason is one of the most significant for low-income countries. For some adolescents, the financial allowance at the birth of a child and social assistance provided until they reach a certain age become a significant argument in favor of early motherhood, and sometimes the only source of income.
Some of these reasons are relevant for poor countries with high unemployment, inaccessibility of educational and medical services, and low incomes. However, the increase in the frequency of early pregnancy in developed countries indicates the shortcomings of the implemented state policy and the lack of targeted efforts aimed at solving this problem.
Pathogenesis
Although, in general, the development of teenage pregnancy is based on the same mechanisms as normal, it has a number of features that affect the course of the gestational period and childbirth. First of all, these features are associated with the functional immaturity of the genital organs and endocrine regulation systems. In adolescence, complications of pregnancy are more often noted, and the likelihood of traumatism in childbirth increases. The onset of gestation in a teenager leads to an acceleration of the processes of puberty and somatic maturation - the size of the bone pelvis increases to typical for 16-18-year-old girls, which, combined with sufficient hydrophilicity and elasticity of the ligamentous apparatus, makes the bone ring more pliable.
Classification
In order to predict the development and choose the optimal tactics for supporting teenage pregnancy, it is advisable to systematize, taking into account a number of medical, physiological and social factors. Such a classification allows you to identify the risks of the gestational period in advance, prevent possible complications and determine the optimal delivery option. The main criteria for systematizing teenage pregnancy are:
- Menstrual age (MW). Taking into account the time of onset of menarche, groups of pregnant adolescents with a menstrual age of up to 1 year, 2 years, 3 years and more are distinguished. The lower the MV, the more likely the pathological course of pregnancy, childbirth and the postpartum period.
- Age of the pregnant woman. Girls under 9 years of age with accelerated sexual development are called "super-young primiparas", at the age of 9-15 years with incomplete puberty - "young primiparas", at 15-18 years old - adolescents ready for the implementation of childbearing function.
- State of health. Depending on the presence of concomitant pathology, there are categories of completely healthy pregnant adolescents, young pregnant women suffering from extragenital diseases, and adolescent girls with complications of the gestational period.
- Circumstances of pregnancy. There are primiparous girls with a desired pregnancy from prosperous and complete families, young pregnant women with an unwanted pregnancy from dysfunctional and single-parent families, adolescents who become pregnant due to rape.
Symptoms of teenage pregnancy
The key sign of onset gestation is the absence of another menstruation, although girls with an irregular monthly cycle may underestimate the significance of this symptom. A possible pregnancy is evidenced by the appearance of unreasonable nausea and vomiting, a change in taste and food preferences, breast engorgement, soreness in the nipple-areolar zone. As the uterus grows, the urge to urinate becomes more frequent, weight gain and an increase in the circumference of the abdomen are observed. Adolescent pregnancies are characterized by sudden mood swings with emotional lability, tearfulness, and tantrums. Often girls complain of unusual drowsiness, general weakness and fatigue.
Complications
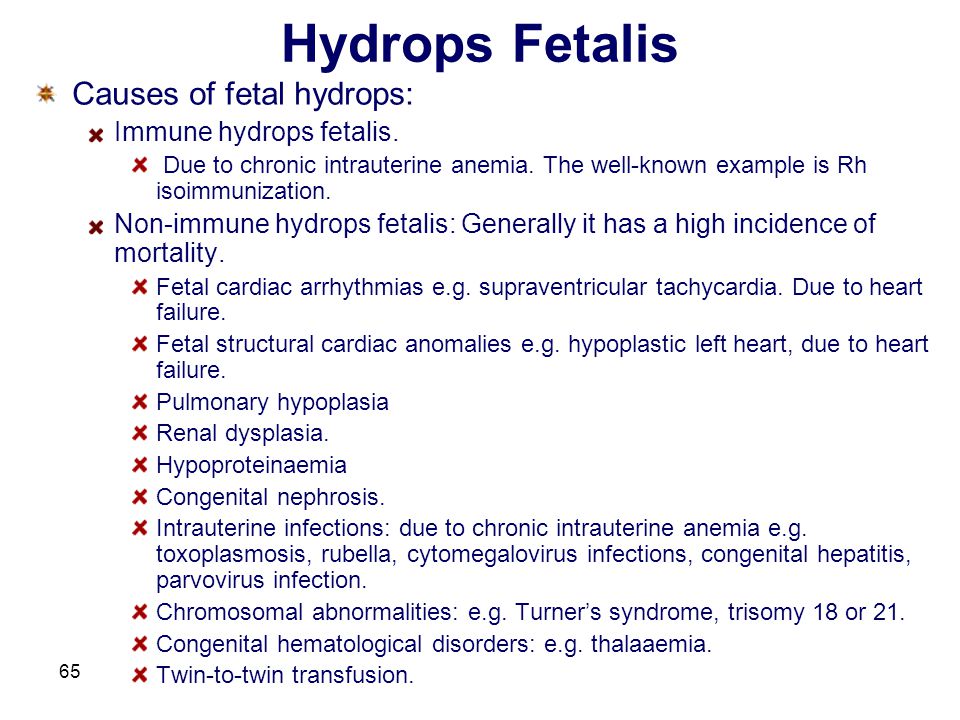
Pregnancy and childbirth put an increased burden on the immature teenage body. In addition, in recent years there has been a significant deterioration in the somatic and reproductive health of girls - up to 75-86% of adolescents suffer from chronic somatic diseases, from 10 to 15% have genital pathology that affects fertility. As a result, teenage pregnancy often has a complicated course. Underage pregnant women are three times more likely to suffer from treatment-resistant anemia. Every second girl has preeclampsia, which manifests on average 12-14 days earlier, mostly has a moderate or severe course. Due to the presence of concomitant genital infections in the adolescent age group, the likelihood of developing an ectopic pregnancy increases.
Fetoplacental insufficiency with hypoxia, antenatal distress and fetal growth retardation is more often formed in pregnant girls of menstrual age 1-2 years. Insufficient secretion of steroids by the fetoplacental system leads to anomalies in the birth forces. With a teenage pregnancy, the risk of spontaneous abortions and premature births increases. Hypoglobulinemia and insufficient reserve potential of phagocytes provoke immune failure, which is manifested by an increase in infectious and inflammatory processes at the gestational and postpartum stages.
The course of childbirth directly depends on the menstrual age of the minor. With CF up to 1-2 years, anatomical or functional narrowing of the pelvis is observed in 50-66% of primiparas, breech presentation occurs more often, childbirth is complicated by spastic irregular contractions in the preliminary period, violent labor, primary weakness of the labor force, traumatization of soft tissues, hypotonic postpartum hemorrhage arising from pathological attachment of the placenta. Girls with 3-year-old CF often give birth quickly or rapidly, they have signs of primary weakness or incoordination of labor, there are ruptures of the birth canal, especially the perineum and cervix. After childbirth, postpartum endometritis, subinvolution of the uterus, hypogalactia and agalactia are detected twice as often in juvenile women in labor.
Diagnostics
A feature of teenage pregnancy is its late diagnosis, due to the fact that up to 35-55% of girls do not suspect that they are carrying a child, or hide it. Often, adolescents turn to an obstetrician-gynecologist only at a later date, and 8-11% of underage pregnant women are not registered at all. The "gold" standard for diagnosing the condition is based on identifying the same presumptive, probable and reliable signs as in the adult reproductive group. To finally confirm pregnancy in a girl with a delay in menstruation, they carry out:
- Chair examination. With bimanual palpation, an increase in the uterus to the probable gestational age, softening of its isthmus, and increased mobility of the cervix are determined. Examination in the mirrors allows you to identify possible signs of a genital infection (inflammation of the vaginal mucosa, discharge from the cervical canal).
- Pregnancy test. Laboratory diagnostics is based on the determination of chorionic gonadotropin in the urine, a specific hormone that begins to be secreted from the time of implantation of a fertilized egg in the uterus. Modern inkjet tests are highly sensitive, and their reliability reaches 99%.
- Ultrasound of the uterus. Sonographic examination is the most popular and affordable method that reliably confirms the fact of pregnancy in a teenager. With the help of ultrasound in the uterine cavity, the fetus, placenta, membranes are detected. Regular screening allows you to dynamically monitor gestation, and fetometry - to assess the development of the fetus.
To exclude a possible infectious and inflammatory pathology of the genital organs, microscopy of a smear from the vagina, bacteriological seeding on nutrient media, TORCH-complex, RIF, ELISA, PCR diagnostics are performed. Subsequently, CTG is recommended for early detection of signs of fetoplacental insufficiency. Differential diagnosis is carried out with neoplasms of the abdominal cavity and small pelvis, malformations of the uterus, hypothalamic-pituitary disorders, primary ovarian insufficiency, metabolic and endocrine disorders in diabetes mellitus, hypofunction and hyperfunction of the thyroid gland, and other diseases accompanied by amenorrhea. According to the indications, the patient is consulted by an adolescent pediatrician, an endocrinologist, an infectious disease specialist, a dermatologist, a neuropathologist, a neurosurgeon, a psychologist, and a psychiatrist.
Management of teenage pregnancy
After detecting gestation, a teenage girl, her relatives and employees of a medical institution need to decide on the advisability of bearing a child, patient management tactics and the optimal method of delivery. Possible options for solving the problem, taking into account all possible factors and the opinion of the pregnant woman, can be:
- Induced abortion.
The girl and her relatives need to be explained that medical or surgical abortion performed at adolescence is more often complicated by traumatic injuries of the uterus, inflammation of the reproductive organs, and a violation of the ovarian cycle. In the future, such patients increase the likelihood of miscarriage and infertility. If a girl insists on terminating a pregnancy, it is important to intervene at an earlier date.
- Pregnancy with natural delivery. The management of young primiparas does not differ significantly from standard protocols and involves the timely correction of emerging complications. In more than 90% of cases, a teenage girl is able to give birth to a child on her own. Even with an anatomically narrow pelvis, a clinical discrepancy between the size of the fetal head and the mother's pelvis is observed in only 10% of patients, which is associated with the frequent onset of preterm birth.
- Pregnancy and caesarean section. The decision to operate in each case is made individually, and the young age of the patient should not be taken as an obstacle to timely surgical intervention.
Indications for operative delivery in adolescent women in labor are the same as in adult women. A caesarean section is performed when anomalies of labor activity that are resistant to conservative therapy, a clinically narrow pelvis, and signs of intranatal fetal hypoxia are detected.
When managing a girl carrying a child, an obstetrician-gynecologist pays attention to both the medical aspects of pregnancy and the correction of the patient's lifestyle. Since the adolescent age group often eat irregular and unbalanced meals, the importance of rational diet and food intake is being educated. Particular attention is paid to the discussion of smoking, alcohol and drug use, prevention of sexually transmitted infections, psychoprophylactic preparation for the upcoming birth. Given the increased risk of complications in childbirth, pregnant adolescents are shown hospitalization in highly qualified obstetric hospitals for 37-39week of gestational age.
Prognosis and prevention
The prognosis with proper management of teenage pregnancy and the choice of the optimal method of delivery is favorable. The average duration of gestation in the adolescent group is shorter than in adults, averaging 37.9 weeks. Ensuring adequate medical support can significantly reduce the risks of possible complications. Preventive measures should be aimed at preventing the early onset of sexual activity, the use of contraceptives, targeted educational work with schoolchildren and especially girls from risk groups (living in asocial families who use alcohol and drugs).
You can share your medical history, what helped you in the treatment of teenage pregnancy.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Ozyorskaya Central District Hospital: teenage pregnancy is a problem that is relevant to society | Ozyory
According to statistics, every tenth pregnancy in Russia is “underage”. Teenage pregnancy is pregnancy between the ages of 12 and 17.
According to the Ozersk Central District Hospital, last year our obstetricians gave birth to five underage pregnant women, one girl was registered for pregnancy this year.
“Despite the significant difference in the statistics of early pregnancy in Russia and in our district, the problem is relevant for society, but the girls who face it are not prepared,” says the head of the department, obstetrician-gynecologist, candidate of medical Sciences Evgeny Peskov. “Neither they, nor future dads, nor their parents know how to behave in this non-standard situation. If pregnancy symptoms are present and the test shows a positive result, the first step is to do an ultrasound to find out the age and condition of the fetus. After that, it is very important not to rush and think before making a decision.
Sometimes young girls feel that they are not ready to become a mother, in which case there are two options: give birth to a child and give it up for adoption, or terminate the pregnancy.
Each method has its pros and cons.
Give the child to another family
This is a good decision for a teenage girl who is ready to bear a child until the end of her term, but does not want to raise it. Today, in about every third couple, a woman over 35 experiences fertility problems, so a child from a young healthy mother quickly finds a new family.
Have an abortion
In accordance with article 54 of the law “On the Fundamentals of Protecting the Health of Citizens of the Russian Federation”, a girl at the age of 15 can independently decide on an abortion, this does not require additional permission. At the same time, medical workers do not have the right, without the consent of the patient, to report the news to parents or at the place of study.
If the teenager is under the age of 15, written permission from a parent or guardian will be required.
Before having an abortion, ask yourself the following questions:
- How much will all procedures cost?
- Should parents and partner be informed?
- How to terminate a teenage girl's pregnancy and what are the risks?
- What will be the physical and psychological state after the procedure?
- How will this action affect the future?
- Is abortion really the only way to continue education?
- Do moral or religious beliefs prevent you from taking this step?
To give birth and raise by yourself
For those who decide to give birth and raise a child on their own, it is very important to make a plan in order to be ready for the arrival of the baby.
The following questions need to be addressed:
- Is it worth raising a child alone or with a father?
- How to support yourself and your baby financially?
- Will the parents help take care of the child, and if so, for how long?
- Is it possible to continue education during pregnancy and after childbirth?
How to have a healthy teenage pregnancy
Because the body is still developing and growing at a young age, it is not fully prepared for pregnancy and childbearing. IMPORTANT THINGS TO DO:
- Find a good OB/GYN
- Eat a balanced diet and drink enough water
- Take prenatal vitamins
- Exercise and get 8-9 hours of sleep
- Quit smoking, alcohol and drugs
- Practice safe sex or abstinence to avoid infections
- Stay in a good mood and avoid stress
- Sign up for pregnancy classes
- Avoid traumatic situations
It's important to remember that a growing baby only needs about 300 calories per day! The saying that you are now "eating for two" is misleading: you don't need to double your meal.
Continuing education
Early teen pregnancy becomes a significant barrier to education, with many teenage mothers dropping out of school to care for their children. However, studying is very important, it will allow young mothers to find work in the future and be able to provide for a new family. In this situation, it is worth talking to teachers about the possibility of homeschooling and flexible visiting schedules.
Rights of underage mothers
According to the law, an underage mother is a child herself and does not have full legal capacity. However, she has parental rights.
According to article 62 of the Family Code of the Russian Federation, teenage parents have the right:
- to live together with the child and participate in his upbringing;
- for independent exercise of parental rights when they reach 16 years of age.
If the parents are under 16, the child will be assigned a guardian who will take part in the upbringing of the child.
Most often, a teenage mother is left to live on the maintenance of her parents and does not receive special benefits from the state. If the girl does not marry in the future, she will receive monthly payments for single mothers.
How to behave and what to do if you are the mother of a teenage girl who is pregnant
If your teenage daughter is showing signs of pregnancy, you may need time to recover. Chances are you're feeling irritated, frustrated, scared, angry, denied, confused, or even a whole range of emotions all at the same time, and that's completely normal.
Remember, your daughter probably didn't want this to happen either. Think about how scared and bad she is. Yes, she had made the adult decision to have sex and was now faced with equally adult consequences in the form of pregnancy. The best and most correct thing you can do in this situation is to subdue your emotions and support your daughter, to persuade her to take responsibility for her actions and their consequences.
Take a deep breath. Try not to let your emotions take over. You may need to sit in silence for a few minutes before collecting your thoughts and saying something. Never lash out at the child in anger, say things that you will definitely regret later, and do not kick her out of the house. Remember, she is still your daughter, no matter what happened.
Yes, she disappointed you and broke a few of your rules. And yes, she probably doesn't even regret it. The last thing you wanted was to be a mother who is forced to ask the question: “What if the daughter is pregnant at 16?” (give or take a few years). But now she is responsible for the tiny life that is born inside her. And while the girl lives under the same roof with you, and you are responsible for her. If you put her out the door, you will endanger your own daughter and your growing grandson.
- Accept the situation as it is. What happened can't be brought back. You will be very angry - there is no escape from this.
But try not to take out the aggression on your daughter. So she will have 9 difficult months of pregnancy, and if she wants to keep the child for herself, then 18 years of responsibility. Try to be calm.
- Listen to her. Her excuses and plans for the future may sound childishly naive, but it will help you better understand her, which is very important in a stressful situation.
- Explain that she needs to take responsibility for her actions - this will help her solve problems in the future. Help your daughter make a decision about pregnancy. If she wants to leave the baby, let her decide the future herself: visit doctors, take vitamins and look for ways to earn money. Let her decide how to balance caring for the newborn, work, and attend school. Let her make mistakes: it can be tough, but it will teach her how to deal with problems in the future.
- Talk to the father of the child - get to know him better: ask about work, about the desire to have children, about whether he is going to marry your daughter.
This will help you decide whether he will take part in the upbringing of the child.
Ask if your daughter wants to have an abortion, raise a baby, or give him up for adoption? Express your point of view, so you will help her realize things that she did not think about. But the teenager must make the final decision himself.
Suggest that she go to the doctor and have a complete check-up. Whichever option she chooses, an ultrasound is necessary to confirm the viability of the fetus and the gestational age. You can offer to go to the office together or let her ask the doctor questions herself.
Who will babysit?
Some grandmothers agree to babysit their grandchildren, others prefer to hire a nanny. Discuss in advance when you will be ready to babysit (during your daughter's working hours, during school / college / university hours, etc.).
What will people say?
This is a really important question, especially if you live in a small town or if you have a wide social circle.
It will seem to you that everyone around is discussing you and your daughter - and so it will be. Pregnancy at a minor age is a scandalous and controversial topic. People tend to gossip, and the news about you will be the most discussed for some time, but gradually the intensity of passions will subside.
If others say to your face that you raised your child poorly, let them know that you did your best, but in the end the daughter made her own decision. If unsolicited advisers insult your girl, do not make excuses for her, but emphasize that she is still your child and you will support her.
Let your daughter know that people gossip, but you are still on her side. Help her figure out how to respond to insults. For example, "Yes, I made a stupid mistake, but now I am responsible for a living being and will protect him."
How can you help your daughter but raise her on her own?
It would be a huge mistake to plan everything for her: doctor's appointments, buying vitamins, enrolling in parenting courses, washing children's clothes.