What is a congenital condition
What is a congenital disorder?
What is a congenital disorder? | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a congenital disorder?
A congenital disorder is a condition that is present from birth. Congenital disorders can be inherited or caused by environmental factors. Their impact on a child’s health and development isn’t always severe, and sometimes it can be quite mild. However, a child with a congenital disorder may experience a disability or health problems throughout life.
It’s natural to be concerned about congenital disorders if you’re pregnant or planning a pregnancy, especially if your family has a history of a particular disorder. It’s possible to test for some, but not all disorders during pregnancy, and there are also things you can do to reduce the chances of your baby being born with a congenital disorder.
What are the most common congenital disorders?
Some common congenital disorders are:
- cleft lip and cleft palate — usually diagnosed during routine scans in pregnancy
- congenital heart disease — including a hole in the heart, a valve problem or a problem with the blood vessels. These are usually diagnosed during routine scans in pregnancy or during newborn screening.
- cerebral palsy — usually diagnosed in the first few years of life
- Fragile X syndrome — may be diagnosed through genetic testing during pregnancy or in the first few years of life
- Down syndrome (Trisomy 21) — usually diagnosed through genetic during pregnancy
- spina bifida — usually diagnosed during routine scans in pregnancy
- cystic fibrosis — usually diagnosed during newborn screening
What tests for congenital disorders are available in pregnancy?
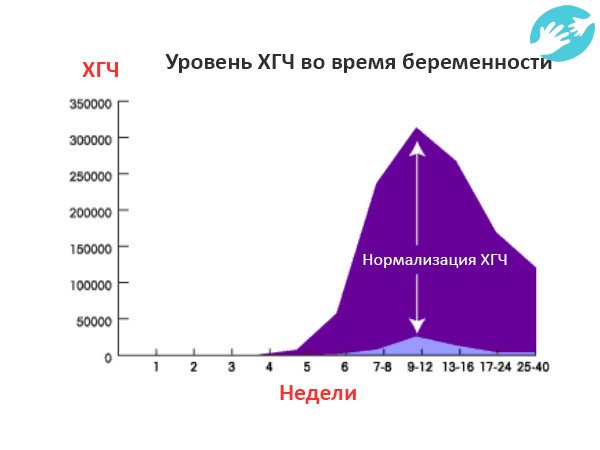
Testing for some congenital disorders, such as Down syndrome, can be performed using a blood test from 10 weeks of pregnancy onwards.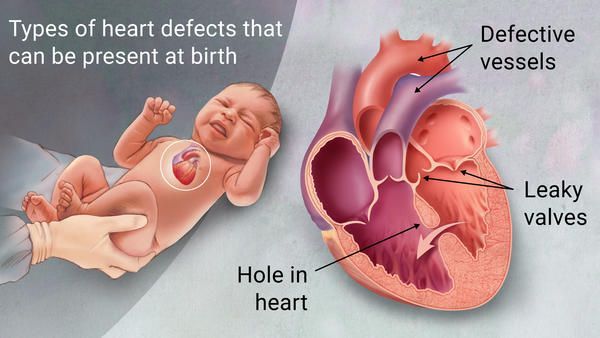 Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Screening tests are designed to identify babies who may be at increased risk of a congenital disorder. If a screening test does not rule out your baby having a congenital disorder, the next step is to have a diagnostic test.
Diagnostic tests, such as ultrasound scans, blood tests and sometimes urine tests, aim to identify babies who have a congenital disorder and to find out what that disorder is.
However, it is not possible to test for all congenital disorders during pregnancy, and testing is not perfect.
Chorionic villus sampling (CVS)
Chorionic villus sampling, or CVS, is usually performed between 10 and 13 weeks of pregnancy if screening tests show your baby may have a congenital disorder. CVS can be used to diagnose babies with Down syndrome or other genetic conditions. You would be given a local anaesthetic and a doctor would use a needle to collect a small sample of cells from your placenta, which is then sent for testing.
Amniocentesis
This test is done after 15 weeks of pregnancy and may be done instead of, or as well as CVS. It can provide a definite answer as to whether your baby has Down syndrome or another congenital disorder.
Amniocentesis involves taking a small amount of fluid from around your baby, using a needle and after a local anaesthetic, which is then sent for testing.
There is a very small risk of miscarriage with both CVS and amniocentesis.
Can congenital disorders be prevented?
If you have a personal or family history of certain congenital disorders, you can have genetic tests before you become pregnant. You may wish to meet with a genetic counsellor to discuss your family history, the likelihood your baby will have any congenital disorders, and possibly to arrange to have genetic testing.
If you are having in vitro fertilisation (IVF) treatment, your embryo can be tested at 2 to 4 days old, before it is implanted into your uterus.
Other things you can do to try to prevent congenital disorders include:
- eating a healthy diet with enough vitamins and minerals, in particular folic acid, during the reproductive years
- taking folic acid supplements before you become pregnant and for the first trimester of pregnancy
- avoiding alcohol, smoking and other drugs because these can harm the fetus
- controlling diabetes and gestational diabetes
- avoiding exposure to chemicals in your environment, such as pesticides or lead
- being vaccinated, especially against rubella
Newborn testing and assessment
A paediatrician and other health professionals examine your baby in the first few days of life to check for hearing problems, heart conditions, and blood, metabolism and hormone disorders. This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
Sources:
Raising Children Network (Tests in pregnancy), Raising Children Network (Newborn screening), Raising Children Network (Antenatal tests: chromosomal abnormalities and other conditions), Raising Children Network (Congenital heart disease), World Health Organization (Congenital anomalies), The Royal Children's Hospital Melbourne (Cleft lip and palate), Cerebral Palsy Alliance (Signs and symptoms of Cerebral Palsy), Fragile X Association of Australia (Testing and screening for Fragile X), NSW Health Centre for Genetics Education (Screening tests during pregnancy), Sydney Children's Hospitals Network (Spina bifida)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2021
Back To Top
Related pages
- What is a childhood disability?
- Your feelings about your child's disability
- Early childhood intervention
- Disability and parenting support
- Disability rights for children
Need more information?
Fragile X syndrome
People with Fragile X syndrome (or Fragile X) have intellectual disability, behavioural and learning challenges as well as certain physical characteristics
Read more on Pregnancy, Birth & Baby website
Fragile X syndrome in children | Raising Children Network
Fragile X syndrome causes intellectual disability and other challenges. Early intervention and support helps children with Fragile X explore their abilities.
Early intervention and support helps children with Fragile X explore their abilities.
Read more on raisingchildren.net.au website
Fragile X syndrome - Better Health Channel
The facts about fragile X syndrome are complicated, and parents and family members are invited to ask their doctor to refer them to a genetics clinic.
Read more on Better Health Channel website
Congenital heart disease: 0-18 years | Raising Children Network
Children with congenital heart disease are born with heart defects. Many heart defects don’t need treatment, and most children go on to live active, healthy lives.
Read more on raisingchildren.net.au website
Cyanotic Congenital Heart Disease (CCHD) | HeartKids
Cyanotic congenital heart disease (CCHD) refers to birth defects that result in a low blood oxygen level & causes a bluish skin colour.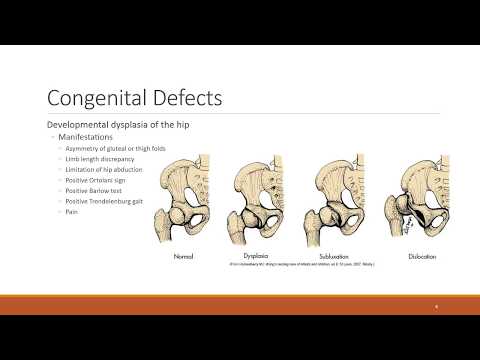 Learn more about it.
Learn more about it.
Read more on HeartKids website
Heart abnormality birth defects - Better Health Channel
Some congenital heart defects are mild and cause no significant disturbance to the way the heart functions.
Read more on Better Health Channel website
What is Down syndrome?
Down syndrome is a genetic disorder characterised by mental and developmental impairments.
Read more on Pregnancy, Birth & Baby website
Caring for a child with Down syndrome
When caring for a child with Down syndrome, you might face some challenges different to other parents.
Read more on Pregnancy, Birth & Baby website
Screening for Down syndrome
Down syndrome is a chromosomal disorder that affects 1 in 1,00 babies.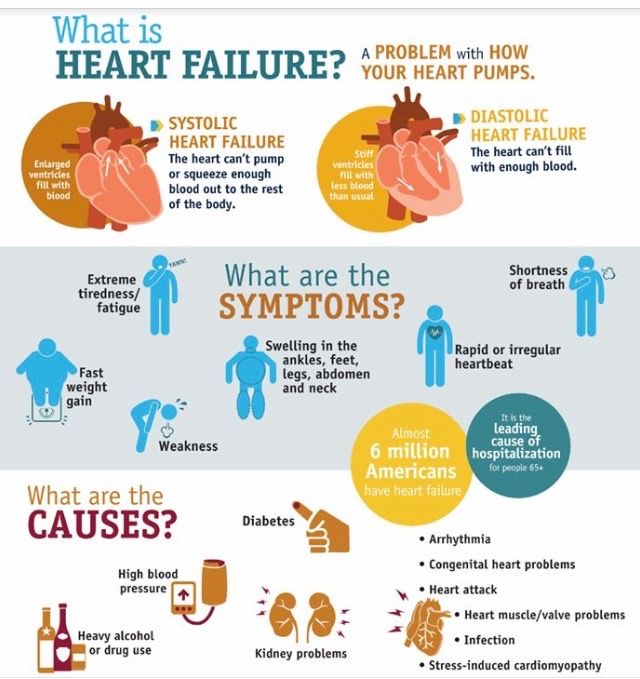 Find out about the screening and diagnostic tests that can detect the condition.
Find out about the screening and diagnostic tests that can detect the condition.
Read more on Pregnancy, Birth & Baby website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Congenital anomalies
Congenital anomalies- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- WHO's Health Emergency Appeal 2023
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Programme Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Member States Portal
- Home/
- Health topics/
- Congenital anomalies
UNICEF/Noorani
Newborn baby in Timor-Leste
© Credits
Fact sheets
Questions and answers
Guidelines
Databases and tools
Resolutions and decisions
Technical work
- Newborn Health Unit
- Maternal, Newborn, Child and Adolescent Health and Ageing
- Nutrition and Food Safety
- Sensory Functions, Disability and Rehabilitation
- Sexual and Reproductive Health
Our work
News
All →Publications
All →A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,.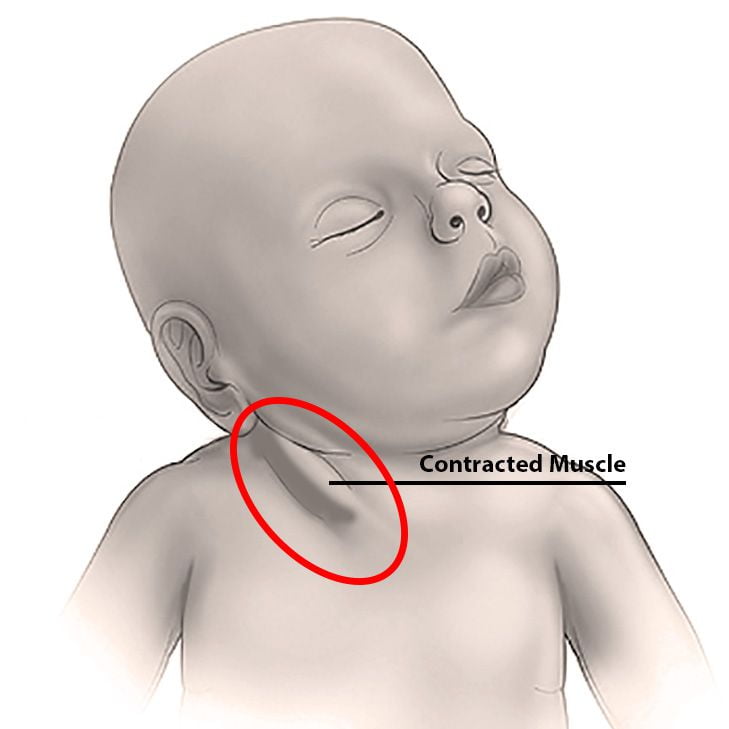 ..
..
Congenital anomalies, also known as birth defects, are structural or functional abnormalities, including metabolic disorders, that are present from birth....
Survive and thrive: transforming care for every small and sick newborn maps out a pathway towards 2030. It is built upon epidemiology, historical trends,...
Feature stories
Related health topics
Congenital metabolic diseases | Hospital Sant Joan de Déu
We provide individualized treatments for metabolic pathologies that manifest as neurological diseases.
Description
Department of Congenital Metabolic Diseases Hospital Hospital Sant Joan de Deu Barcelona is the leader in the treatment of metabolic pathologies in the country and Europe. Patient care is based on extensive experience, research results and collaboration with research societies to provide individually tailored treatment to each person who seeks our help.
What are hereditary metabolic diseases?
What are hereditary metabolic diseases?
Pathologies, also known as congenital metabolic disorders, are diseases that are caused by a genetic change in a protein or enzyme, as a result of which a certain metabolic process is blocked. This blockage affects the normal functioning of certain cells and organs and manifests itself in a number of symptoms, which are different for each patient . Among these symptoms, various types of neurological syndromes can occur.
This blockage affects the normal functioning of certain cells and organs and manifests itself in a number of symptoms, which are different for each patient . Among these symptoms, various types of neurological syndromes can occur.
This group of pathologies is very extensive, but it can be systematized using the current classification , which is currently undergoing significant changes due to the fact that today we have much greater knowledge about the basic mechanisms for the development of such pathologies. Below are main groups of pathologies, compiled on the basis of the type of damage to the body in each of them .
Main groups:
- Congenital disorder of small molecule metabolism: Affect intermediate metabolism. These include aminoacidopathy (phenylketonuria and propionic aciduria). It also includes disorders of the metabolism of carbohydrates or neurotransmitters and neuromodulators.
- Congenital disorder of energy metabolism: Characterized by insufficient production and use of energy. This includes mitochondrial diseases, insufficient production of pyruvate or glucose (muscle or liver), etc.
- Congenital disorder of complex molecule metabolism: A group of diseases that interfere with the synthesis of large molecules. They manifest as persistent symptoms that are not related to nutrition. This includes lysosomal (mucopolysaccharidosis, oligosaccharidosis, sphingolipidosis, etc.), peroxisomal (Zelweger syndrome, X-linked adrenoleukodystrophy) diseases and congenital glycosylation disorders, as well as other congenital metabolic disorders.
Why Sant Joan de Deu?
Why Sant Joan de Deu?
Why Sant Joan de Deu?
On average, we diagnose such diseases in 80 patients per year.
We have extensive experience in the treatment of complex pathologies.
We have more than 40 years of experience in the field of congenital metabolic disorders. During these years, our employees have mastered the methods of diagnosis, treatment and interaction with families to perfection. We diagnose 80 new cases of every year.
During these years, our employees have mastered the methods of diagnosis, treatment and interaction with families to perfection. We diagnose 80 new cases of every year.
These disorders, also known as congenital metabolic disorders, are considered rare or extremely rare. Despite the fact that such diseases are rare, congenital metabolic disorders (ECM) are included in a large group, which already includes about 800 different diseases . 90% of cases are accompanied in one way or another with damage to the nervous system . At the moment in Catalonia it is possible to detect twenty varieties of ECM at an early stage by screening of newborn patients based on standard protocols.
In the Department of Congenital Metabolic Disorders, we diagnose 80 patients per year, one third of which are infants. In recent years, this figure has increased due to early diagnosis, which allows us to tailor therapies as accurately as possible according to the characteristics of each patient and avoid future complications. Our department also analyzes samples from other medical institutions that need a second opinion for the most accurate diagnosis.
Why Sant Joan de Deu?
Genetic tests allow us to make accurate diagnoses.
Hospital Sant Joan de Deu Barcelona is one of three European centers that research amino acids and neurotransmitters in its own biochemical laboratory
these diseases.
Congenital metabolic diseases involve the presence of biochemical markers or symptoms that are common to various diseases. Therefore, much effort must be made to identify the genetic origin of each pathology. Thanks to the technologies that are at the disposal of our laboratory, we can guarantee a high accuracy of diagnosis.
Why Sant Joan de Deu?
ECM is staffed by a wide range of specialists in various fields.
Our professionals closely coordinate with each other and join in at various stages of diagnosis, treatment and follow-up of patients, especially in difficult cases.
This is about 15 neuropediatrics, gastroenterology, nutrition, psychology, pharmaceuticals and biochemistry specialists working with patients and their families.
Our professionals clearly coordinate with each other and join in at various stages of diagnosis , treatment and follow-up of patients, especially in difficult cases.
Proper therapeutic diet or training rules are indispensable in individual cases and therefore we not only treat children and adolescents, but also consult with their families.
Why Sant Joan de Deu?
We are involved in various research projects and European networks
We exchange knowledge with various international centers and hospitals.
We are part of the European Registry and Network for Metabolic Intoxication Diseases (EIMD), in which we have been the leader among Spanish members since 2011. We are also members of the Homocystinuria Treatment Network (E-HOD) and co-lead the International Neurotransmitter Disorders (INTD) Working Group.
We have recently joined the European Congenital Metabolic Diseases Reference Network (metab-ERN), where we lead a subgroup focused on small molecules that affect brain metabolism (neurotransmitters, metals and deficiency of glucose transporters in the brain etc.).
This allows us to provide clinical guidance on the management of these complex diseases , as well as to discover new areas of work based on clinical evidence and experience from other hospitals.
Medical Specialists
Medical Specialists
Àngels García Cazorla
Pediatric Neurologist
Specialist Profile
Judith Armstrong Morón
Specialist Profile
0003
Children's gastroenterologist, hepatologist and nutrition specialist
Cristina Sierra March
Pharmacology
Specialist profile
Délia Yubero Siles
Biologist
RESTURITISS
RESTROUSE 9000 In addition to treating patients, the staff of the Department of Congenital Metabolic Diseases (ECM) at Hospital Sant Joan de Déu Barcelona also conducts various studies aimed at improving the diagnosis and treatment of congenital metabolic disorders and other rare genetic diseases.
This activity has enabled our department to join CIBERER, a center for research on rare diseases that studies genetic and metabolic disorders among rare diseases. The main subjects of research are:
- FKU and other disorders of intermediate metabolism.
- Energy metabolism in mitochondria and ataxia.
- Applied research neuromuscular diseases.
- Synaptic dysfunction and neural connections in neurometabolic diseases (laboratory for the study of metabolism in synapses).
- Movement disorders, related to vitamins.
- Collaborative study of Low's syndrome.
- Development of clinical and radiological scores to assess birth defects in protein glycosylation .
- Diagnosis in patients with ECM in the Atlas Mountains of Morocco thanks to the NGO Nousol.
ECM also collaborates with various European research networks, including the following.
- MetabERN (European Reference Network for Metabolic Disorders).
- E-IMD (European Intoxication Metabolic Disease Registry).
- E-HOD (European Homocystinuria Registry).
- InNerMed (Hereditary neurometabolic diseases).
- I-NTD (International Working Group on Neurotransmitter Disorders).
- INPDA (International Niemann-Pick Disease Alliance).
- Connecting The Growing Brain
- RRD Foundation (Recordati Foundation for Rare Diseases), participation in the scientific committee and development of special programs.
Hereditary and hereditarily predisposed diseases
The main goal of medical genetics is to study the role of genetic components in the etiology and pathogenesis of various human diseases. These diseases are divided into two classes: actually hereditary diseases, which include chromosomal and gene diseases, and diseases with a hereditary predisposition, which are called multifactorial diseases.
Chromosomal diseases are caused by a violation of the number or structure of chromosomes. Genetic diseases are caused by the presence of mutations in genes. Monogenic diseases are diseases caused by the presence of mutations in one gene. In the etiology of multifactorial diseases, along with the action of unfavorable external factors, the states of not one, but many genes have a significant influence. The number of these genes that form a hereditary predisposition to the disease is sometimes in the tens or even hundreds. The total frequency of hereditary diseases reaches 1.5%, of which chromosomal diseases account for 0.5% and monogenic diseases up to 1%. Most of the most common human diseases are multifactorial.
Chromosomal diseases: Currently, about 1000 nosological forms of chromosomal diseases have been described. All of them are characterized by a number of common features, such as: small weight and body length at birth, prenatal hypoplasia; lag in mental and physical development from the moment of birth, especially pronounced in autosomal anomalies; delay and anomalies of sexual development: hypogonadism, cryptorchidism, amenorrhea, infertility, etc. , more pronounced with abnormalities of the sex chromosomes; multiple congenital malformations to a greater extent with autosomal anomalies; a complex of dysmorphogenetic and dysplastic signs of various manifestations and severity, simultaneously affecting many systems and organs of the patient. Chromosomal disorders are rarely inherited, and more than 9In 5% of cases, the risk of re-birth in the family of a sick child with a chromosomal pathology does not exceed the general population level. The exception is those cases when the parents of a sick child carry balanced chromosomal rearrangements, most often translocations, in which there is no loss of genetic material. Carriers of balanced translocations are practically healthy people, but the likelihood of miscarriages, missed pregnancies or the birth of children with unbalanced chromosomal rearrangements, and therefore with chromosomal diseases, is very high. Therefore, in case of infertility, stillbirth, habitual miscarriage, as well as in the presence of a child with a chromosomal pathology in the family, it is necessary to analyze the karyotype of each of the parents in order to diagnose balanced chromosomal rearrangements.
, more pronounced with abnormalities of the sex chromosomes; multiple congenital malformations to a greater extent with autosomal anomalies; a complex of dysmorphogenetic and dysplastic signs of various manifestations and severity, simultaneously affecting many systems and organs of the patient. Chromosomal disorders are rarely inherited, and more than 9In 5% of cases, the risk of re-birth in the family of a sick child with a chromosomal pathology does not exceed the general population level. The exception is those cases when the parents of a sick child carry balanced chromosomal rearrangements, most often translocations, in which there is no loss of genetic material. Carriers of balanced translocations are practically healthy people, but the likelihood of miscarriages, missed pregnancies or the birth of children with unbalanced chromosomal rearrangements, and therefore with chromosomal diseases, is very high. Therefore, in case of infertility, stillbirth, habitual miscarriage, as well as in the presence of a child with a chromosomal pathology in the family, it is necessary to analyze the karyotype of each of the parents in order to diagnose balanced chromosomal rearrangements.
Monogenic diseases The diversity of monogenic diseases is quite large and their number, according to some estimates, reaches 5000. Among monogenic diseases, a significant percentage of fermentopathy, various forms of mental retardation, defects in the organs of hearing, vision, skeletal dysplasia, congenital malformations, diseases of the nervous, endocrine , connective tissue, immune and other systems. Monogenic variants of the course of the disease in rare cases are found among any nosological forms that are generally not hereditary. For example, monogenic forms of hypertension, Alzheimer's and Parkinson's diseases, epilepsy and other major psychoses, immunodeficiencies, various oncological diseases, and many other pathological conditions are described. Monogenic variants of the disease, as a rule, differ from sporadic forms in a more severe course and early onset. Most of the mutations associated with monogenic diseases strongly determine the development of the disease, and environmental factors have little or no effect on the development of the disease. That is why they are so difficult to correct. However, there are many examples of monogenic diseases with incomplete penetrance and variable expressivity, the causes of which most often remain unknown. Fortunately, monogenic diseases are rare. The best-known monogenic diseases include phenylketonuria, cystic fibrosis, galactosemia, adrenogenital syndrome, hemophilia A and B, Duchenne/Becker muscular dystrophy, proximal spinal muscular atrophy, hepatolenticular degeneration, and many other diseases. Prevention of severe incurable monogenic diseases is carried out on the basis of prenatal diagnosis.
That is why they are so difficult to correct. However, there are many examples of monogenic diseases with incomplete penetrance and variable expressivity, the causes of which most often remain unknown. Fortunately, monogenic diseases are rare. The best-known monogenic diseases include phenylketonuria, cystic fibrosis, galactosemia, adrenogenital syndrome, hemophilia A and B, Duchenne/Becker muscular dystrophy, proximal spinal muscular atrophy, hepatolenticular degeneration, and many other diseases. Prevention of severe incurable monogenic diseases is carried out on the basis of prenatal diagnosis.
Multifactorial diseases are caused by the combined action of unfavorable external and genetic risk factors that form a hereditary predisposition to the disease. Multifactorial diseases include the vast majority of chronic human diseases, including cardiovascular, endocrine, immune, neuropsychiatric, oncological, etc. Genetic components can be present in the etiology of even those diseases whose development is entirely induced by external influences and is impossible without their presence, such such as infectious diseases. However, even in these cases, individual sensitivity to such external adverse influences can be genetically determined. For example, today it is known that protein products of such genes of the detoxification system as GSTM1, GSTT1, CYP1A1, GSTP1, NAT2, etc. are involved in the pathology of bronchial asthma, leukemia and their relapses. The complete decoding of the human genome has opened up great opportunities for studying the association of various genes. a person with monogenic and multifactorial diseases. These studies are the basis for the systematic development, together with specialists of various medical profiles, of new pathogenetic and etiological methods of treating hereditary diseases, as well as preventing the development of those diseases to which a person has a genetic tendency.
However, even in these cases, individual sensitivity to such external adverse influences can be genetically determined. For example, today it is known that protein products of such genes of the detoxification system as GSTM1, GSTT1, CYP1A1, GSTP1, NAT2, etc. are involved in the pathology of bronchial asthma, leukemia and their relapses. The complete decoding of the human genome has opened up great opportunities for studying the association of various genes. a person with monogenic and multifactorial diseases. These studies are the basis for the systematic development, together with specialists of various medical profiles, of new pathogenetic and etiological methods of treating hereditary diseases, as well as preventing the development of those diseases to which a person has a genetic tendency.
Currently, there is no single classification of hereditary diseases, and they are often confused with congenital and family diseases. The cause of the development of hereditary diseases are mutations in certain genes present in the germ cells of the parents. These mutations can be passed on to offspring over a number of generations. Congenital diseases appear immediately after birth, and they can be either hereditary or acquired, for example, under the influence of teratogenic factors or complications in childbirth. Acquired congenital malformations are not inherited. Familial diseases are diseases that are present in several members of the same family. They can also be hereditary or environmental, such as poor diet, bad habits, or the presence of toxic compounds in the environment. In turn, hereditary diseases are not necessarily congenital or familial.
These mutations can be passed on to offspring over a number of generations. Congenital diseases appear immediately after birth, and they can be either hereditary or acquired, for example, under the influence of teratogenic factors or complications in childbirth. Acquired congenital malformations are not inherited. Familial diseases are diseases that are present in several members of the same family. They can also be hereditary or environmental, such as poor diet, bad habits, or the presence of toxic compounds in the environment. In turn, hereditary diseases are not necessarily congenital or familial.
In the etiology of childhood disability and disability, a significant proportion belongs to hereditary factors. So, in the Republic of Sakha (Yakutia), among the causes of childhood disability, congenital malformations are in first place (28.5%), diseases of the nervous system are in second (23.9%), and mental disorders are in third (11.9%) . According to Rosstat, among the causes of infant mortality, congenital malformations occupy the second or third place in the Republic of Sakha (Yakutia) and in the Russian Federation as a whole.