Complications of delivery
Labor complications: 10 common problems
The labor and birth process is usually straightforward, but sometimes complications arise that may need immediate attention.
Complications can occur during any part of the labor process.
According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development, specialized help is more likely to be needed if a pregnancy lasts more than 42 weeks, if there has been a previous cesarean delivery, or when the mother is of an older age.
This article will look at ten of the problems that can occur, why they happen, the treatment available, and some measures that can help prevent them.
Share on PinterestIf delivery takes longer than expected, this may be described as “failure to progress.” This can happen for a number of reasons.Prolonged labor, labor that does not progress, or failure to progress is when labor lasts longer than expected. Studies suggest that this affects around 8 percent of those giving birth. It can happen for a number of reasons.
The American Pregnancy Association define prolonged labor as lasting over 20 hours if it is a first delivery. For those who have previously given birth, failure to progress is when labor lasts more than 14 hours.
If prolonged labor happens during the early, or latent, phase it can be tiring but does not usually lead to complications.
However, if it happens during the active phase, medical assessment and intervention may be needed.
Causes of prolonged labor include:
- slow cervical dilations
- slow effacement
- a large baby
- a small birth canal or pelvis
- delivery of multiple babies
- emotional factors, such as worry, stress, and fear
Pain medications can also contribute by slowing or weakening uterine contractions.
If labor fails to progress, the first advice is to relax and wait. The American Pregnancy Association advise taking a walk, having a sleep, or running a warm bath.
In the later stages, health professionals may give labor-inducing medications or recommend a cesarean delivery.
“Non-reassuring fetal status,” previously known as fetal distress, is used to describe when a fetus does not appear to be doing well.
The new term is recommended by the American College of Obstetricians and Gynecologists (ACOG), because “fetal distress” is not specific, and it may result in inaccurate treatment.
Non-reassuring fetal status may be linked to:
- an irregular heartbeat in the baby
- problems with muscle tone and movement
- low levels of amniotic fluid
Underlying causes and conditions can include:
- insufficient oxygen levels
- maternal anemia
- pregnancy-induced hypertension in the mother
- intrauterine growth retardation (IUGR)
- meconium-stained amniotic fluid
It is more likely to occur in pregnancies that last 42 weeks or longer.
Strategies that may help with during episodes of non-reassuring fetal status include:
- changing the mother’s position
- increasing maternal hydration
- maintaining oxygenation for the mother
- amnioinfusion, where fluid is inserted into the amniotic cavity to relieve pressure on the umbilical cord
- tocolysis, a temporary stoppage of contractions that can delay preterm labor
- intravenous hypertonic dextrose
In some cases, a cesarian delivery may be necessary.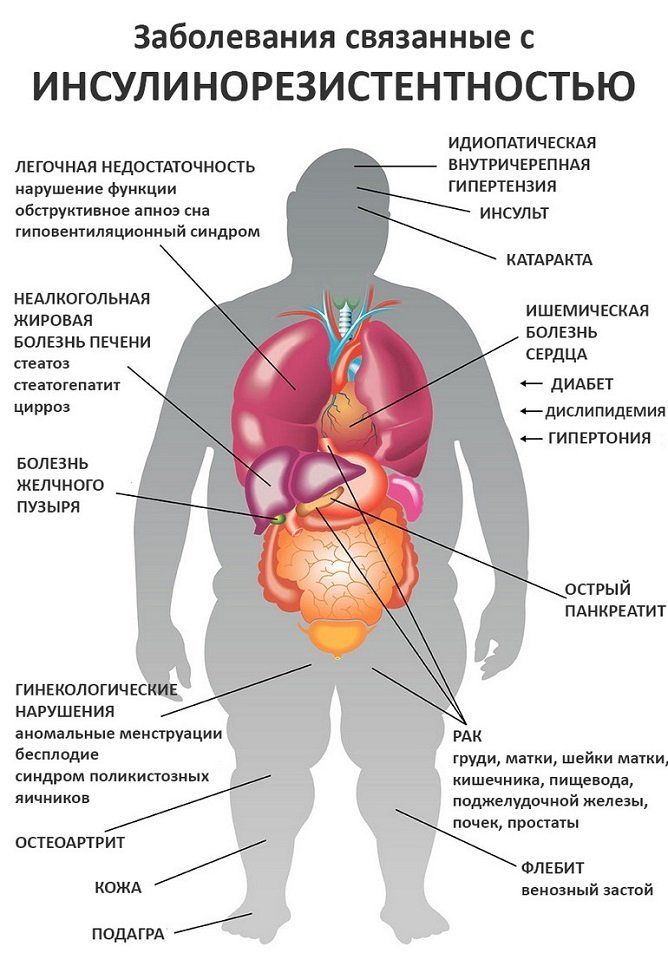
Perinatal asphyxia has been defined as “failing to initiate and sustain breathing at birth.”
It can happen before, during or immediately after delivery, due to an inadequate supply of oxygen.
It is a non-specific term that involves a complex range of problems.
It can lead to:
- hypoxemia, or low oxygen levels
- high levels of carbon dioxide
- acidosis, or too much acid in the blood
Cardiovascular problems and organ malfunction can result.
Before delivery, symptoms may include a low heart rate and low pH levels, indicating high acidity.
At birth, there may be a low APGAR score of 0 to 3 for more than 5 minutes.
Other indications may include:
- poor skin color
- low heart rate
- weak muscle tone
- gasping
- weak breathing
- meconium-stained amniotic fluid
Treatment of perinatal asphyxia can include providing oxygen to the mother, or carrying out a cesarean delivery.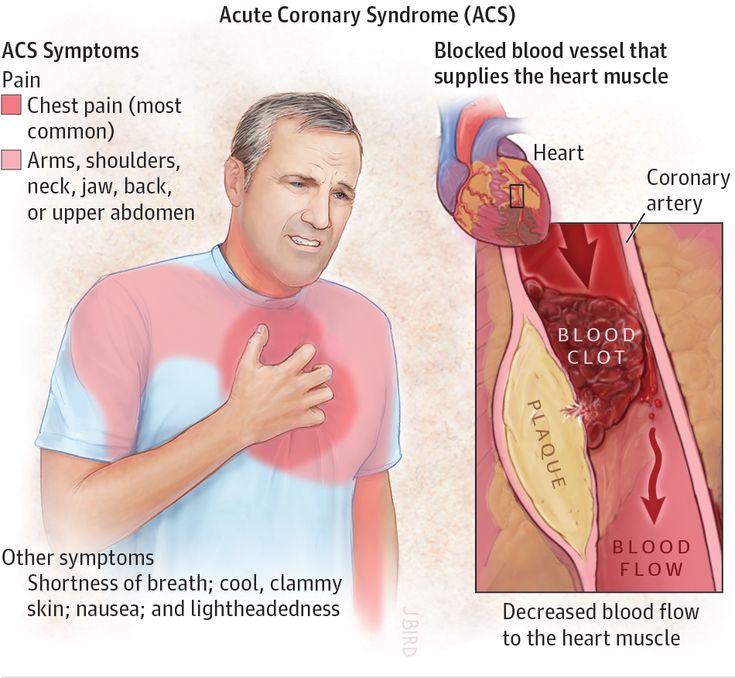
After delivery, mechanical breathing or medication may be necessary.
Share on PinterestChanging position may help resolve shoulder dystocia.
Shoulder dystocia is when the head is delivered vaginally but the shoulders remain inside the mother.
It is not common, but it is more likely to affect women who have not given birth before, and is responsible for half of all cesarean deliveries in this group.
Health providers may apply specific maneuvers to release the shoulders:
These include:
- changing the mother’s position
- manually turning the baby’s shoulders
An episiotomy, or surgical widening of the vagina, may be needed to make room for the shoulders.
Complications are usually treatable and temporary. However, if a non-reassuring fetal heart rate is also present, this may indicate other problems.
Possible problems include:
- fetal brachial plexus injury, a nerve injury that may affect the shoulder, arms, and hand but usually heals in time
- fetal fracture, in which the humerus or collar-bone break, which usually heal without problems
- hypoxic-ischemic brain injury, or a low oxygen supply to the brain, which can, in rare cases, be life-threatening or lead to brain damage
Maternal complications include uterine, vaginal, cervical or rectal tearing and heavy bleeding after delivery.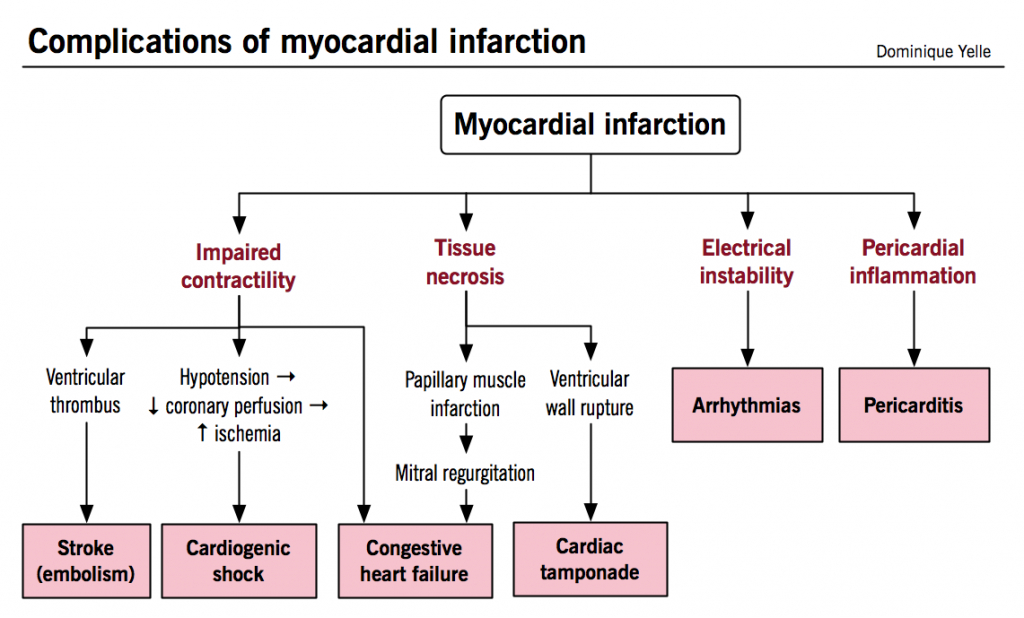
On average, women lose 500 milliliters (ml) of blood during the vaginal delivery of a single baby. During a cesarian delivery for a single baby, the average amount of blood lost is 1,000 ml.
It can occur within 24 hours after delivery or up to 12 weeks later, in the case of secondary bleeding.
Around 80 percent of cases of postpartum hemorrhage result from a lack of uterine tone.
Bleeding happens after the placenta is expelled, because the uterine contractions are too weak and cannot provide enough compression to the blood vessels at the site of where the placenta was attached to the uterus.
Low blood pressure, organ failure, shock, and death can result.
Certain medical conditions and treatments can increase the risk of developing postpartum hemorrhage:
- placental abruption or placenta previa
- uterine overdistention
- multiple gestation pregnancy
- pregnancy-induced hypertension
- several prior births
- prolonged labor
- the use of forceps or a vacuum-assisted delivery
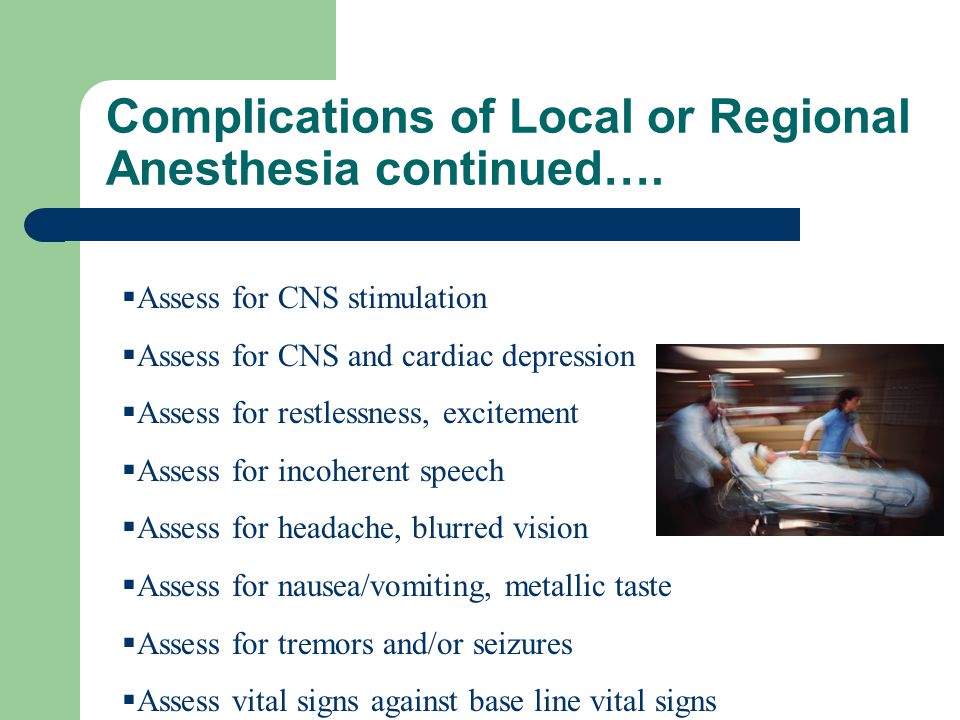
- use of general anesthesia or medications to induce or stop labor
- infection
- obesity
Other medical conditions that can lead to a higher risk include:
- cervical, vaginal or uterine blood vessel tears
- hematoma of the vulva, vagina or pelvis
- blood clotting disorders
- placenta accreta, increta, or percreta
- uterine rupture
Treatment aims to stop the bleeding as soon as possible.
Options include:
- the use of medication
- uterine massage
- removal of retained placenta
- uterine packing
- tying off bleeding blood vessels
- surgery, possible a laparotomy, to find the cause of the bleeding, or hysterectomy, to remove the uterus
Excessive bleeding can be life-threatening, but with rapid and appropriate medical help, the outlook is normally good.
Share on PinterestA cesarian delivery, episiotomy, or forceps delivery may be necessary if the baby’s position is preventing the birth.
Not all babies will be in the best position for vaginal delivery. Facing downward is the most common fetal birth position, but babies can be in other positions.
They include:
- facing upward
- breech, either buttocks first (frank breech) or feet first (complete breech)
- lying sideways, horizontally across the uterus instead of vertically
Depending on the position of the baby and the situation, it may be necessary to:
- manually change the fetal position
- use forceps
- carry out an episiotomy, to surgically enlarge the opening
- perform a cesarian delivery
Umbilical cord
Problems with the umbilical cord include:
- become wrapped around the baby
- getting compressed
- emerging before the baby
If it is wrapped around the neck, if it is compressed, or emerges before the baby does, medical help will probably be needed.
When the placenta covers the opening of the cervix, this is referred to as placenta previa. A cesarian delivery is usually necessary.
It affects around 1 in 200 pregnancies in the third trimester.
It is most likely to occur in those who:
- have had previous deliveries, and especially four or more pregnancies
- previous placenta previa, cesarean delivery, or uterine surgery
- have a multiple gestation pregnancy
- are aged over 35 years
- have fibroids
- smoke
The main symptom is bleeding without pain during the third trimester. This can range from light to heavy.
Other possible indications include:
- early contractions
- the baby being in breech position
- a large uterus size for the stage of pregnancy
Treatment is usually:
- bed rest or supervised rest in the hospital, in severe cases
- blood transfusion
- immediate cesarean delivery, if the bleeding does not stop or if the fetal heart reading is non-reassuring
It can increase the risk of a condition known as placenta accreta, a potentially life-threatening condition in which the placenta becomes inseparable from the wall of the uterus.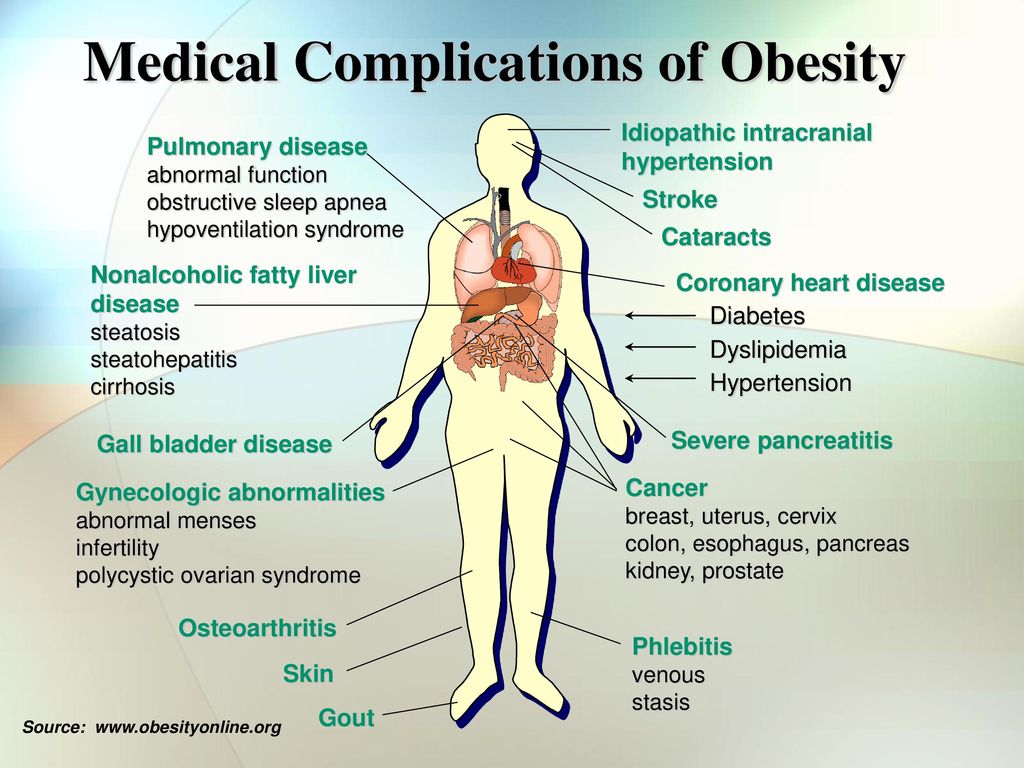
The doctor may recommend avoiding intercourse, limiting travel, and avoiding pelvic examinations.
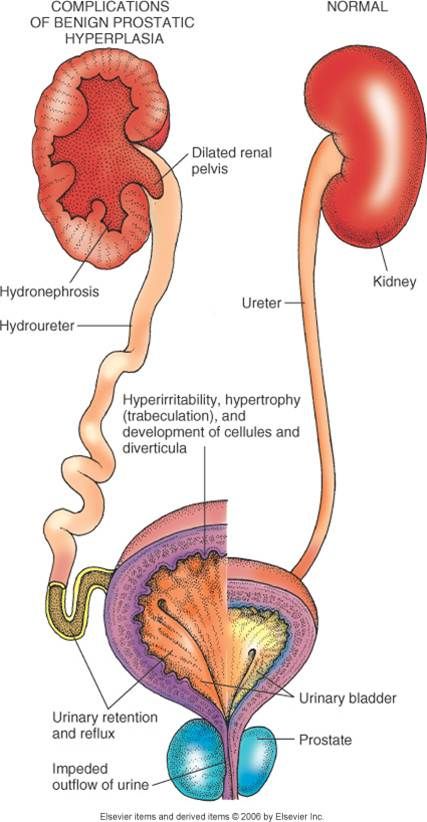
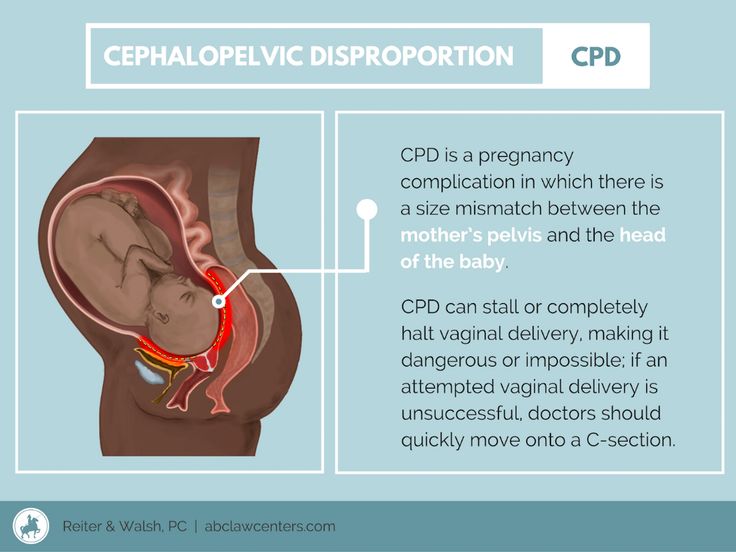
Cephalopelvic disproportion (CPD) is when a baby’s head is unable to fit through the mother’s pelvis.
According to the American College of Nurse Midwives, cephalopelvic disproportion occurs in 1 in 250 pregnancies.
This can happen if:
- the baby is large or has a large head size
- the baby is in an unsual position
- the mother’s pelvis is small or has an unusual shape
A cesarian delivery will normally be necessary.
If someone has previously had a cesarian delivery, there is a small chance that the scar could open during future labor.
If this happens, the baby may be at risk of oxygen deprivation and a cesarian delivery may be necessary. The mother may be at risk of excessive bleeding.
Apart from a previous cesarean delivery, other possible risk factors include:
- the induction of labor
- the size of the baby
- maternal age of 35 years or more
- the use of instruments in vaginal delivery
Women who plan for a vaginal birth after previously having a cesarian delivery should aim to deliver at a health care facility.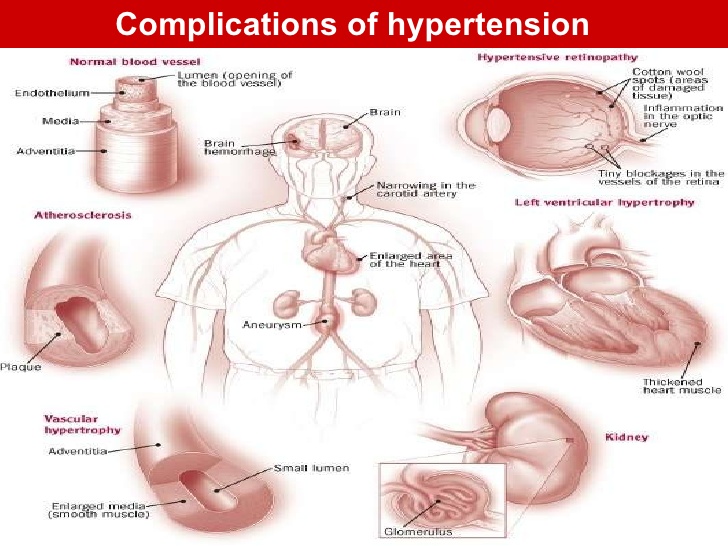 This will provide access to facilities for a cesarean delivery and blood transfusion, should they be needed.
This will provide access to facilities for a cesarean delivery and blood transfusion, should they be needed.
Signs of a uterine rupture include:
- an abnormal heart rate in the baby
- abdominal pain and scar tenderness in the mother
- slow progress in labor
- vaginal bleeding
- rapid heart rate and low blood pressure in the mother
Appropriate care and monitoring can reduce the risk of serious consequences.
Together, the three stages of labor typically last for 6 to18 hours, but sometimes it lasts only 3 to 5 hours.
This is known as rapid labor or precipitous labor.
The chances of rapid labor are increased when:
- the baby is smaller than average
- the uterus contracts efficiently and strongly
- the birth canal is compliant
- there is a history of rapid labor
Rapid labor can start with a sudden series of quick, intense contractions. This can leave little time in between for rest. They may resemble one continuous contraction.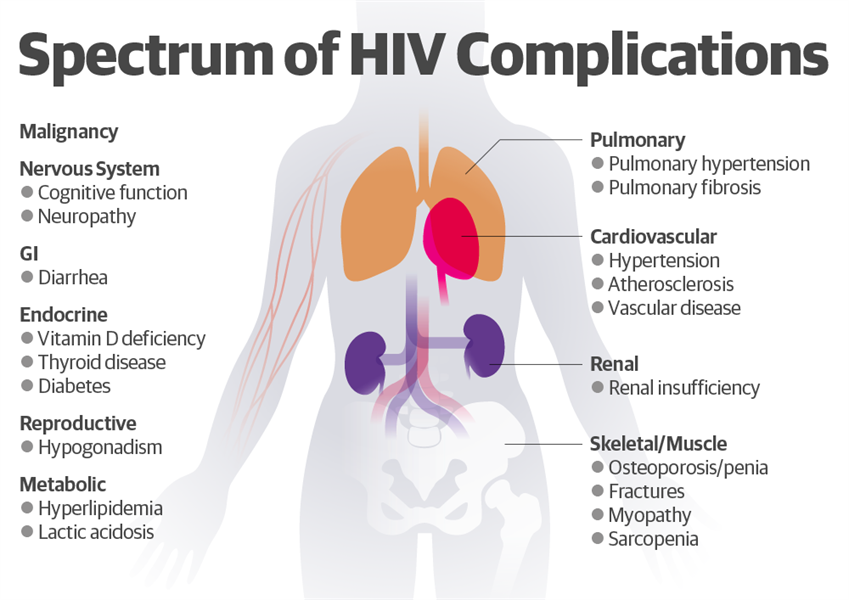
Disadvantages of rapid labor are that:
- it can leave the mother feeling out of control
- there may not be enough time to get to a health care facility
- it can increase the risk of tearing and laceration to the cervix and vagina, hemorrhage, and postpartum shock
Risks for the baby include:
- aspiration of amniotic fluid
- a higher chance of infection if delivery takes place in an unsterile location
If there are signs of rapid labor starting, it is important to:
- contact a doctor or midwife.
- use breathing techniques and calming thoughts to feel more in control
- remaining in a sterile place
Lying down on the back or side may help.
Complications during can be life-threatening in parts of the world where there is a lack of proper health care.
Worldwide, 303,000 fatalities were expected to occur in 2015, according to the World Health Organization (WHO).
In the U.S., the figure is around 700 each year.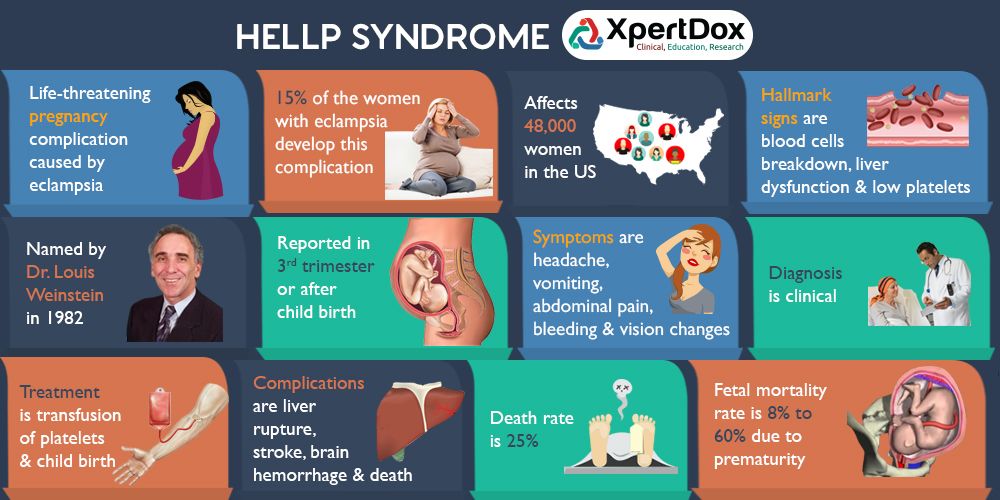
The main causes are:
- bleeding
- infection
- unsafe termination
- eclampsia, leading to high blood pressure and seizures
- pregnancy complications that worsen at the time of delivery
Appropriate health care can prevent or resolve most of these problems.
It is vital to attend all prenatal visits during pregnancy, and to follow the doctor’s advice and instructions regarding pregnancy and delivery.
Labor complications: 10 common problems
The labor and birth process is usually straightforward, but sometimes complications arise that may need immediate attention.
Complications can occur during any part of the labor process.
According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development, specialized help is more likely to be needed if a pregnancy lasts more than 42 weeks, if there has been a previous cesarean delivery, or when the mother is of an older age.
This article will look at ten of the problems that can occur, why they happen, the treatment available, and some measures that can help prevent them.
Prolonged labor, labor that does not progress, or failure to progress is when labor lasts longer than expected. Studies suggest that this affects around 8 percent of those giving birth. It can happen for a number of reasons.
The American Pregnancy Association define prolonged labor as lasting over 20 hours if it is a first delivery. For those who have previously given birth, failure to progress is when labor lasts more than 14 hours.
If prolonged labor happens during the early, or latent, phase it can be tiring but does not usually lead to complications.
However, if it happens during the active phase, medical assessment and intervention may be needed.
Causes of prolonged labor include:
- slow cervical dilations
- slow effacement
- a large baby
- a small birth canal or pelvis
- delivery of multiple babies
- emotional factors, such as worry, stress, and fear
Pain medications can also contribute by slowing or weakening uterine contractions.
If labor fails to progress, the first advice is to relax and wait. The American Pregnancy Association advise taking a walk, having a sleep, or running a warm bath.
In the later stages, health professionals may give labor-inducing medications or recommend a cesarean delivery.
“Non-reassuring fetal status,” previously known as fetal distress, is used to describe when a fetus does not appear to be doing well.
The new term is recommended by the American College of Obstetricians and Gynecologists (ACOG), because “fetal distress” is not specific, and it may result in inaccurate treatment.
Non-reassuring fetal status may be linked to:
- an irregular heartbeat in the baby
- problems with muscle tone and movement
- low levels of amniotic fluid
Underlying causes and conditions can include:
- insufficient oxygen levels
- maternal anemia
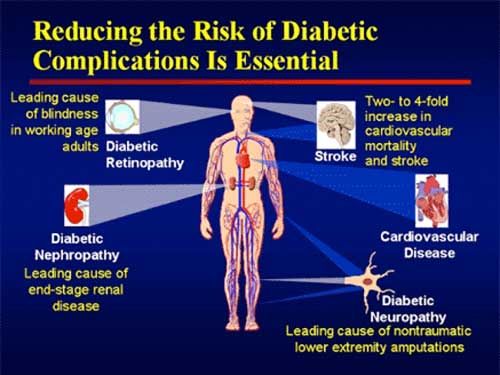
- pregnancy-induced hypertension in the mother
- intrauterine growth retardation (IUGR)
- meconium-stained amniotic fluid
It is more likely to occur in pregnancies that last 42 weeks or longer.
Strategies that may help with during episodes of non-reassuring fetal status include:
- changing the mother’s position
- increasing maternal hydration
- maintaining oxygenation for the mother
- amnioinfusion, where fluid is inserted into the amniotic cavity to relieve pressure on the umbilical cord
- tocolysis, a temporary stoppage of contractions that can delay preterm labor
- intravenous hypertonic dextrose
In some cases, a cesarian delivery may be necessary.
Perinatal asphyxia has been defined as “failing to initiate and sustain breathing at birth.”
It can happen before, during or immediately after delivery, due to an inadequate supply of oxygen.
It is a non-specific term that involves a complex range of problems.
It can lead to:
- hypoxemia, or low oxygen levels
- high levels of carbon dioxide
- acidosis, or too much acid in the blood
Cardiovascular problems and organ malfunction can result.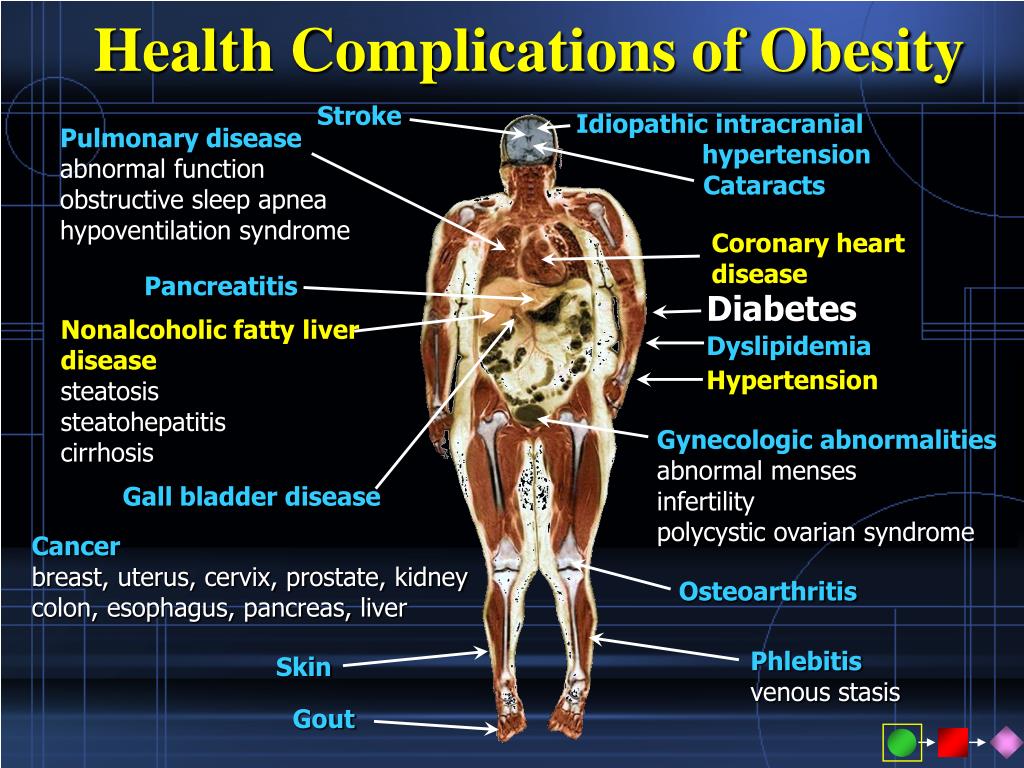
Before delivery, symptoms may include a low heart rate and low pH levels, indicating high acidity.
At birth, there may be a low APGAR score of 0 to 3 for more than 5 minutes.
Other indications may include:
- poor skin color
- low heart rate
- weak muscle tone
- gasping
- weak breathing
- meconium-stained amniotic fluid
Treatment of perinatal asphyxia can include providing oxygen to the mother, or carrying out a cesarean delivery.
After delivery, mechanical breathing or medication may be necessary.
Share on PinterestChanging position may help resolve shoulder dystocia.
Shoulder dystocia is when the head is delivered vaginally but the shoulders remain inside the mother.
It is not common, but it is more likely to affect women who have not given birth before, and is responsible for half of all cesarean deliveries in this group.
Health providers may apply specific maneuvers to release the shoulders:
These include:
- changing the mother’s position
- manually turning the baby’s shoulders
An episiotomy, or surgical widening of the vagina, may be needed to make room for the shoulders.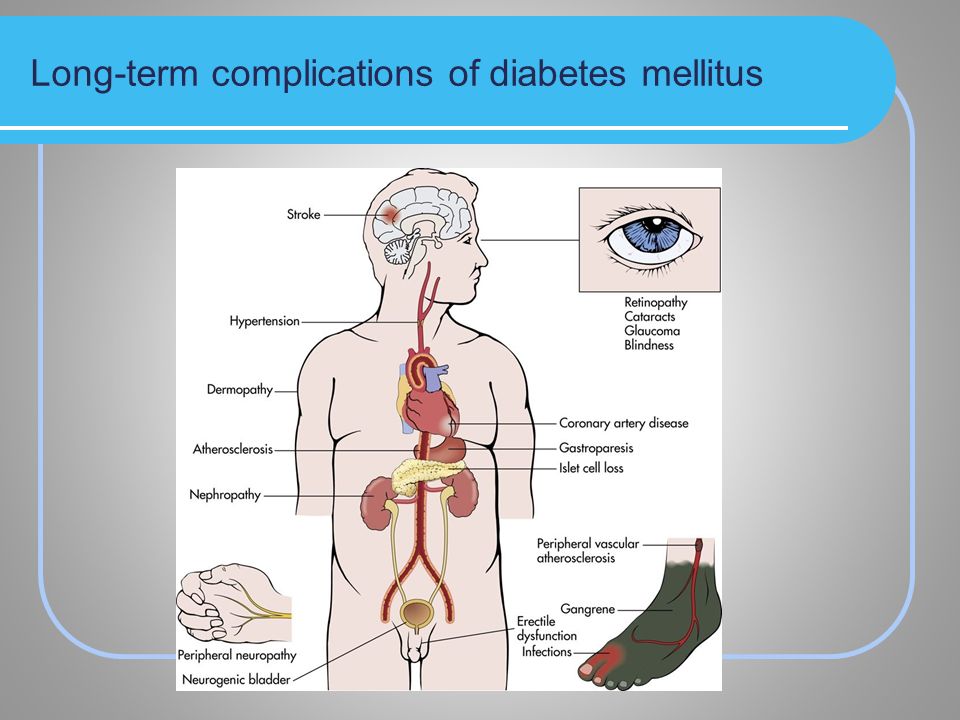
Complications are usually treatable and temporary. However, if a non-reassuring fetal heart rate is also present, this may indicate other problems.
Possible problems include:
- fetal brachial plexus injury, a nerve injury that may affect the shoulder, arms, and hand but usually heals in time
- fetal fracture, in which the humerus or collar-bone break, which usually heal without problems
- hypoxic-ischemic brain injury, or a low oxygen supply to the brain, which can, in rare cases, be life-threatening or lead to brain damage
Maternal complications include uterine, vaginal, cervical or rectal tearing and heavy bleeding after delivery.
On average, women lose 500 milliliters (ml) of blood during the vaginal delivery of a single baby. During a cesarian delivery for a single baby, the average amount of blood lost is 1,000 ml.
It can occur within 24 hours after delivery or up to 12 weeks later, in the case of secondary bleeding.
Around 80 percent of cases of postpartum hemorrhage result from a lack of uterine tone.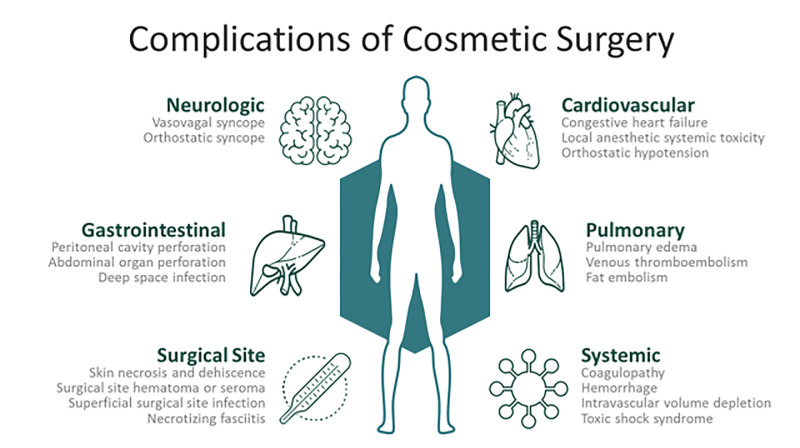
Bleeding happens after the placenta is expelled, because the uterine contractions are too weak and cannot provide enough compression to the blood vessels at the site of where the placenta was attached to the uterus.
Low blood pressure, organ failure, shock, and death can result.
Certain medical conditions and treatments can increase the risk of developing postpartum hemorrhage:
- placental abruption or placenta previa
- uterine overdistention
- multiple gestation pregnancy
- pregnancy-induced hypertension
- several prior births
- prolonged labor
- the use of forceps or a vacuum-assisted delivery
- use of general anesthesia or medications to induce or stop labor
- infection
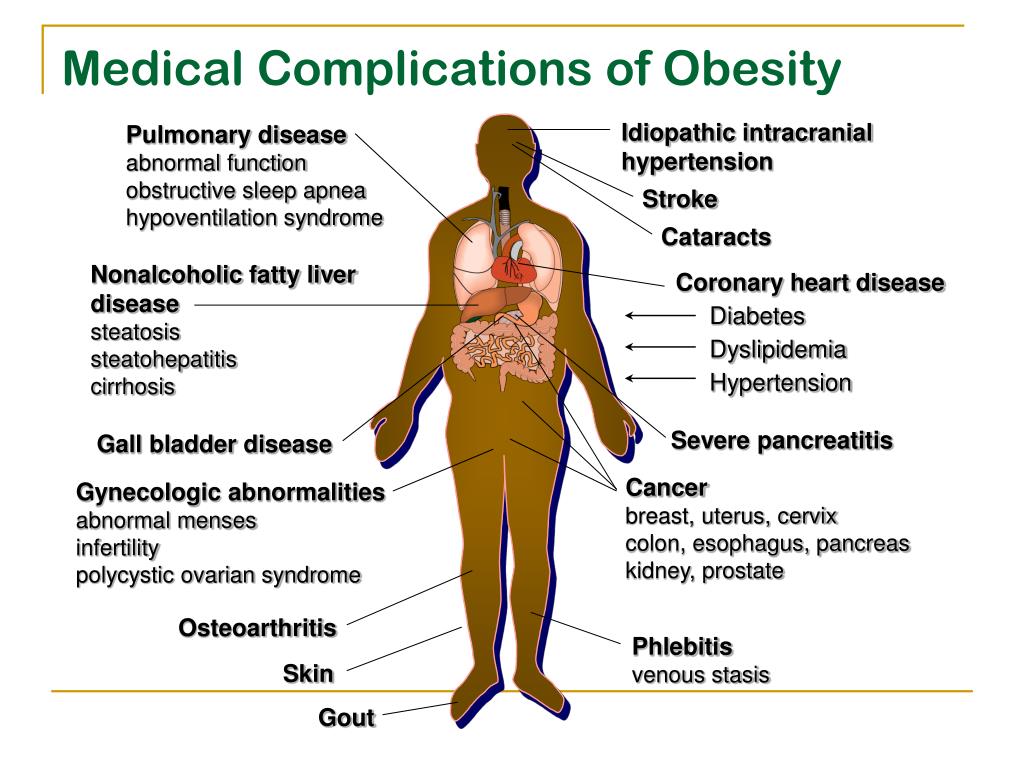
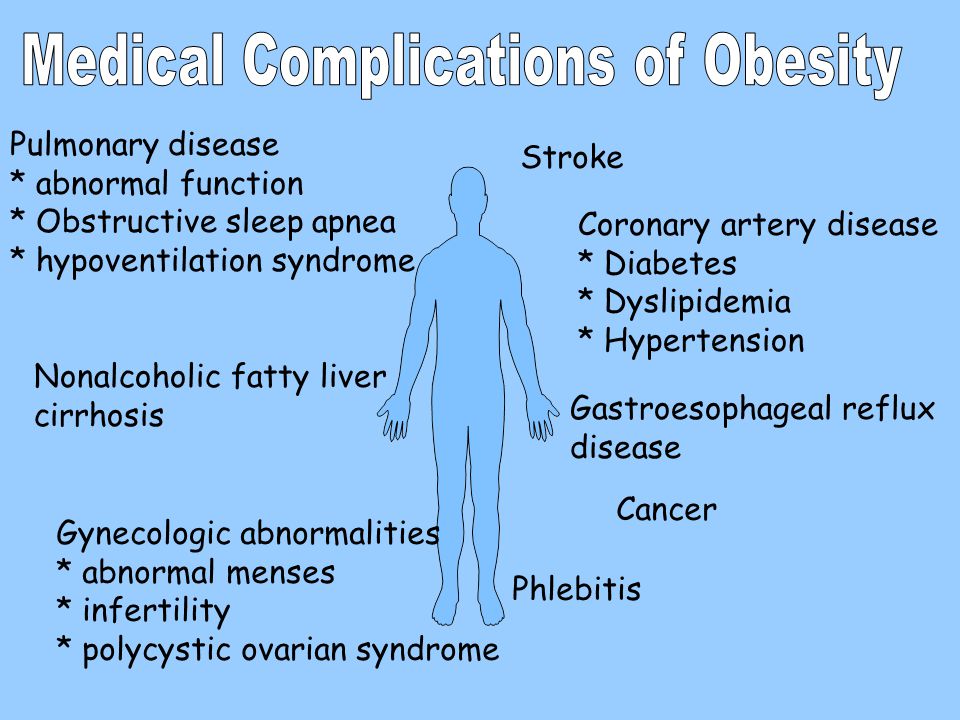
- obesity
Other medical conditions that can lead to a higher risk include:
- cervical, vaginal or uterine blood vessel tears
- hematoma of the vulva, vagina or pelvis
- blood clotting disorders
- placenta accreta, increta, or percreta
- uterine rupture
Treatment aims to stop the bleeding as soon as possible.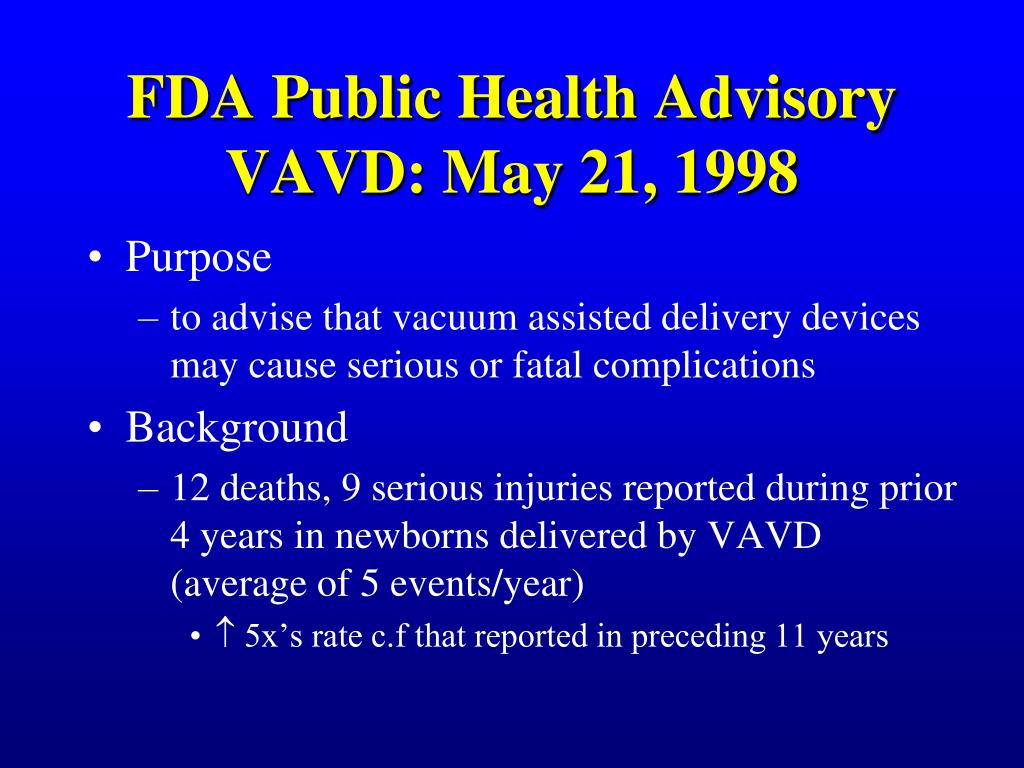
Options include:
- the use of medication
- uterine massage
- removal of retained placenta
- uterine packing
- tying off bleeding blood vessels
- surgery, possible a laparotomy, to find the cause of the bleeding, or hysterectomy, to remove the uterus
Excessive bleeding can be life-threatening, but with rapid and appropriate medical help, the outlook is normally good.
Share on PinterestA cesarian delivery, episiotomy, or forceps delivery may be necessary if the baby’s position is preventing the birth.
Not all babies will be in the best position for vaginal delivery. Facing downward is the most common fetal birth position, but babies can be in other positions.
They include:
- facing upward
- breech, either buttocks first (frank breech) or feet first (complete breech)
- lying sideways, horizontally across the uterus instead of vertically
Depending on the position of the baby and the situation, it may be necessary to:
- manually change the fetal position
- use forceps
- carry out an episiotomy, to surgically enlarge the opening
- perform a cesarian delivery
Umbilical cord
Problems with the umbilical cord include:
- become wrapped around the baby
- getting compressed
- emerging before the baby
If it is wrapped around the neck, if it is compressed, or emerges before the baby does, medical help will probably be needed.
When the placenta covers the opening of the cervix, this is referred to as placenta previa. A cesarian delivery is usually necessary.
It affects around 1 in 200 pregnancies in the third trimester.
It is most likely to occur in those who:
- have had previous deliveries, and especially four or more pregnancies
- previous placenta previa, cesarean delivery, or uterine surgery
- have a multiple gestation pregnancy
- are aged over 35 years
- have fibroids
- smoke
The main symptom is bleeding without pain during the third trimester. This can range from light to heavy.
Other possible indications include:
- early contractions
- the baby being in breech position
- a large uterus size for the stage of pregnancy
Treatment is usually:
- bed rest or supervised rest in the hospital, in severe cases
- blood transfusion
- immediate cesarean delivery, if the bleeding does not stop or if the fetal heart reading is non-reassuring
It can increase the risk of a condition known as placenta accreta, a potentially life-threatening condition in which the placenta becomes inseparable from the wall of the uterus.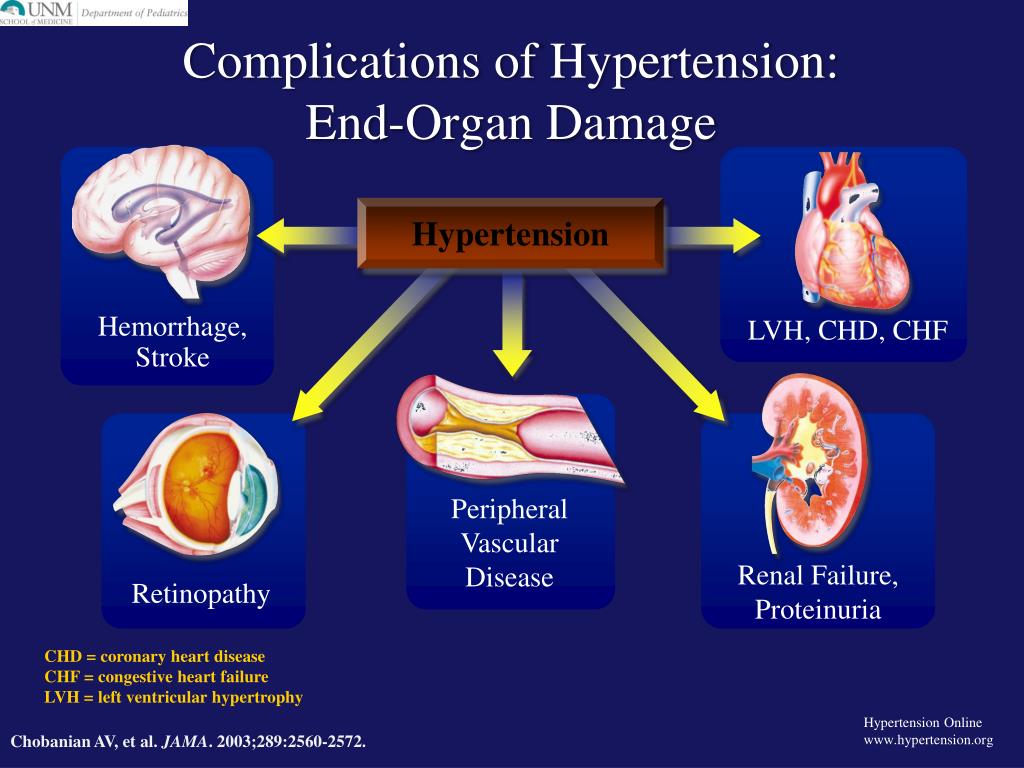
The doctor may recommend avoiding intercourse, limiting travel, and avoiding pelvic examinations.
Cephalopelvic disproportion (CPD) is when a baby’s head is unable to fit through the mother’s pelvis.
According to the American College of Nurse Midwives, cephalopelvic disproportion occurs in 1 in 250 pregnancies.
This can happen if:
- the baby is large or has a large head size
- the baby is in an unsual position
- the mother’s pelvis is small or has an unusual shape
A cesarian delivery will normally be necessary.
If someone has previously had a cesarian delivery, there is a small chance that the scar could open during future labor.
If this happens, the baby may be at risk of oxygen deprivation and a cesarian delivery may be necessary. The mother may be at risk of excessive bleeding.
Apart from a previous cesarean delivery, other possible risk factors include:
- the induction of labor
- the size of the baby
- maternal age of 35 years or more
- the use of instruments in vaginal delivery
Women who plan for a vaginal birth after previously having a cesarian delivery should aim to deliver at a health care facility.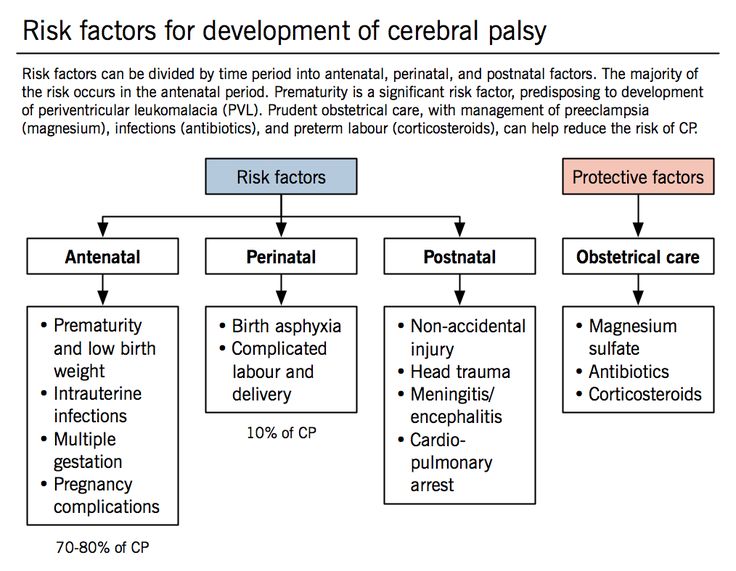 This will provide access to facilities for a cesarean delivery and blood transfusion, should they be needed.
This will provide access to facilities for a cesarean delivery and blood transfusion, should they be needed.
Signs of a uterine rupture include:
- an abnormal heart rate in the baby
- abdominal pain and scar tenderness in the mother
- slow progress in labor
- vaginal bleeding
- rapid heart rate and low blood pressure in the mother
Appropriate care and monitoring can reduce the risk of serious consequences.
Together, the three stages of labor typically last for 6 to18 hours, but sometimes it lasts only 3 to 5 hours.
This is known as rapid labor or precipitous labor.
The chances of rapid labor are increased when:
- the baby is smaller than average
- the uterus contracts efficiently and strongly
- the birth canal is compliant
- there is a history of rapid labor
Rapid labor can start with a sudden series of quick, intense contractions. This can leave little time in between for rest. They may resemble one continuous contraction.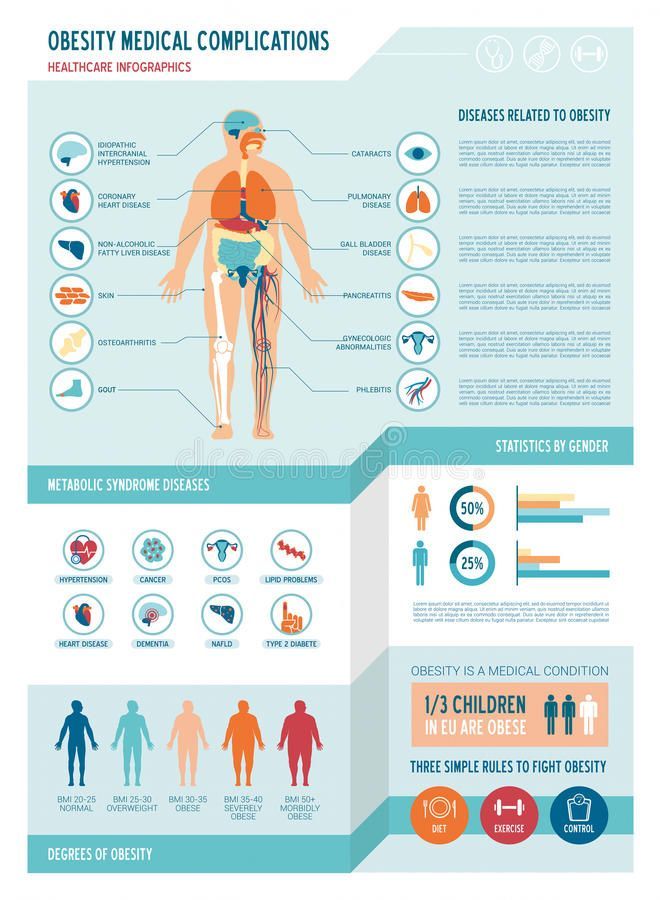
Disadvantages of rapid labor are that:
- it can leave the mother feeling out of control
- there may not be enough time to get to a health care facility
- it can increase the risk of tearing and laceration to the cervix and vagina, hemorrhage, and postpartum shock
Risks for the baby include:
- aspiration of amniotic fluid
- a higher chance of infection if delivery takes place in an unsterile location
If there are signs of rapid labor starting, it is important to:
- contact a doctor or midwife.
- use breathing techniques and calming thoughts to feel more in control
- remaining in a sterile place
Lying down on the back or side may help.
Complications during can be life-threatening in parts of the world where there is a lack of proper health care.
Worldwide, 303,000 fatalities were expected to occur in 2015, according to the World Health Organization (WHO).
In the U.S., the figure is around 700 each year.
The main causes are:
- bleeding
- infection
- unsafe termination
- eclampsia, leading to high blood pressure and seizures
- pregnancy complications that worsen at the time of delivery
Appropriate health care can prevent or resolve most of these problems.
It is vital to attend all prenatal visits during pregnancy, and to follow the doctor’s advice and instructions regarding pregnancy and delivery.
Complications of childbirth. What are Birth Complications?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Complications of childbirth are pathological conditions that occur during labor, are associated with it, affect the course and outcome of childbirth. They are manifested by a violation of the contractile activity of the myometrium, pain syndrome, bleeding, deterioration in the general condition of the woman in labor (dizziness, weakness, loss of consciousness, coma). For diagnosis, methods of external obstetric examination, vaginal examination, cardiotocography, less often ultrasound, and in the afterbirth period, revision of the birth canal and uterus are used. The tactics of conducting labor in case of complications is determined by the nature of the identified pathology, it may involve both natural and operative delivery.
- Causes of birth complications
- Classification
- Symptoms of labor complications
- Diagnostics
- Treatment of complications of childbirth
- Prognosis and prevention
- Prices for treatment
General
To date, only 37% of births proceed physiologically. In other cases, various types of complications are determined, and 23-25% of births are completed surgically. According to the results of studies in the field of obstetrics and gynecology, the most common complications are ruptures of the cervix (up to 27% of cases of childbirth) and perineum (7-15%), premature rupture of amniotic fluid (12-15%), anomalies of labor forces (about 10% ), infectious processes (2-8%), bleeding (2-5%) and premature detachment of the placenta (0.45-1.2%). If not managed properly, complicated births pose a threat to the health and life of both the mother and the fetus. Despite the constant decline in maternal mortality rates, up to 200 women die each year during childbirth in Russia.
According to the results of studies in the field of obstetrics and gynecology, the most common complications are ruptures of the cervix (up to 27% of cases of childbirth) and perineum (7-15%), premature rupture of amniotic fluid (12-15%), anomalies of labor forces (about 10% ), infectious processes (2-8%), bleeding (2-5%) and premature detachment of the placenta (0.45-1.2%). If not managed properly, complicated births pose a threat to the health and life of both the mother and the fetus. Despite the constant decline in maternal mortality rates, up to 200 women die each year during childbirth in Russia.
Complications of childbirth
Causes of birth complications
The pathological course of childbirth may be due to provoking factors from the mother, the fetus and its membranes. The main causes of violations that occur during childbirth are:
- Abnormal pregnancy. With a complicated gestational period, the risk of violations in childbirth increases - premature detachment of the placenta, weakness of the birth forces, decompensation of chronic diseases of the mother, bleeding.
- Anatomical features of the birth canal. A narrow pelvis, volumetric formations of the cervix, vagina, pelvic organs, high perineum become physical obstacles for the passage of the fetus. With infantilism, a saddle uterus and other developmental anomalies, the contractile activity of the myometrium often decreases. Age-related decrease in tissue elasticity increases the likelihood of tissue rupture.
- Inflammatory diseases. In the presence of endometritis, cervicitis, colpitis, chorioamnionitis, the risk of bleeding, birth trauma of the mother, infection of the child during passage through the birth canal increases.
- Previous invasive interventions. Scar-changed tissues of the genital organs are worse stretched, less resistant to the loads that occur during childbirth. Therefore, in women after gynecological operations and diagnostic manipulations (abortions, curettage, etc.), complications such as soft tissue injuries are more often observed.
- Injuries in past births.
 Scars formed after past ruptures of the perineum, cervix and body of the uterus are more susceptible to damage.
Scars formed after past ruptures of the perineum, cervix and body of the uterus are more susceptible to damage. - Extragenital pathology. Hypertension, diabetes mellitus, renal failure, myopia and other chronic diseases can decompensate during childbirth. Some of them increase the likelihood of bleeding, prolonged course, DIC, and other complications.
- Incorrect position and presentation. Childbirth in an oblique position, breech, frontal or occipital presentation is accompanied by birth trauma, premature rupture of amniotic fluid, prolapse of the umbilical cord and small parts of the fetus. Natural delivery in the transverse position of the fetus is impossible.
- Anatomical features of the child. With large sizes, hydrocephalus or gross birth defects, it is more difficult for the fetus to pass through the birth canal. In such cases, the likelihood of female and prenatal injuries increases.
- Multiple pregnancy. Childbirth with more than one child, especially if it is the first, is more often characterized by a complicated course with an increased risk of bleeding and injury.
- Pathology of membranes. Bleeding, fetal hypoxia, and other complications of childbirth can be caused by early rupture of the amniotic bladder, entanglement or prolapse of the umbilical cord, low or polyhydramnios, tight attachment, accretion, ingrowth, germination, or premature detachment of a normally or low-lying placenta.
- Medical errors. Incorrect tactics of pregnancy and childbirth, the choice of an inappropriate method of delivery or type of surgical intervention, unreasonable stimulation of labor activity are fraught with the risk of injury, other complications, and even death of a woman or child.
Classification
The clinical classification of complications is based on the level of emerging disorders (pathology of childbirth, damage to the mother or fetus), their nature and time of occurrence. Varieties of pathological childbirth are:
- Premature birth. At the onset of labor before 37 weeks, the likelihood of complications in the fetus is higher.
 Therefore, even with a normal course, they are considered complicated.
Therefore, even with a normal course, they are considered complicated. - Prolonged labor. An increase in the duration of labor due to weak or discoordinated labor activity, a clinically or anatomically narrow pelvis, and other reasons increases the risk of trauma, hypoxia, and postpartum hemorrhage.
- Rapid delivery. With violent uterine contractions, ruptures of the soft tissues of the birth canal, fetal injury, placental abruption, placental blood flow disorders, and hypotonic bleeding often occur.
- Operative delivery. Since a caesarean section, the application of a vacuum extractor or forceps, obstetric rotation and other interventions increase the risk of complications in a woman and a child, such births are obviously considered complicated.
In a woman in connection with childbirth, the following types of complications are possible:
- Birth injury. Under the influence of significant tensile loads during childbirth, ruptures of the perineum, vagina, cervix and its body occur.
 In the most severe cases, injuries of the sphincter and rectal wall, divergence of the pelvic bones are observed.
In the most severe cases, injuries of the sphincter and rectal wall, divergence of the pelvic bones are observed. - Decompensation of extragenital diseases. Significant physical activity associated with childbirth can provoke a hypertensive crisis, acute cardiac, cerebral, renal or hepatic failure, diabetic coma, retinal detachment and other disorders.
- Bleeding. With tissue ruptures, disorders in the blood coagulation system, partial or complete accreta of the placenta, hypotension of the myometrium, prolonged bleeding often occurs, leading to significant blood loss, hypovolemic shock and DIC.
- Amniotic fluid embolism. A terrible complication caused by the ingress of amniotic fluid into the mother's bloodstream. In 70-80% of cases, it ends with the death of a woman, in 60-80% - with the death of the fetus.
- Retention of parts of the placenta in the uterus. Even in the absence of bleeding, fragments of the placenta, adherent or ingrown into the wall of the uterus, pose a threat to the woman's health.
 They can become a nutrient substrate for the development of inflammation or be reborn.
They can become a nutrient substrate for the development of inflammation or be reborn. - Postpartum inflammatory processes. In severe and protracted labor, various invasive interventions, the risk of developing endometritis, adnexitis, cervicitis, peritonitis and sepsis increases.
The main complications of childbirth on the part of the fetus are:
- Prenatal injury. During childbirth, a child can get a spinal injury, a fracture of the collarbone and humerus. Intraorganic hemorrhages in the tissues of the brain, kidneys, liver, adrenal glands, cerebrovascular accidents, the formation of cephalohematoma are possible.
- Acute hypoxia. Reduction or complete cessation of blood flow from mother to child due to placental abruption or clamping of the umbilical cord is accompanied by oxygen starvation. With prolonged hypoxia, irreversible changes in the tissues of the fetus may occur.
- Infection during childbirth. With a clinical course or asymptomatic carriage in the mother of infections of the birth canal, the child may be infected with opportunistic flora, pathogens of herpes, gonorrhea, chlamydia and other diseases.
Taking into account the time of occurrence of the consequences associated with childbirth, there are complications of the period of contractions (premature onset, prolonged course, etc.), the straining period (fetal hypoxia, birth trauma, decompensation of concomitant pathology), the afterbirth period (bleeding), the postpartum period (inflammatory diseases ). In addition, there are long-term consequences of childbirth associated with their complicated course - ectropion and cicatricial deformity of the cervix, prolapse and prolapse of the vagina, uterus, chorionepithelioma in a woman, cerebral palsy, other disabling symptom complexes and diseases in a child.
Symptoms of labor complications
A complicated course of childbirth may be indicated by changes in the strength and nature of contractions, pain, vaginal discharge, disturbances in the general well-being of a woman, and fetal movement. With weak labor activity, the woman in labor notes rare short contractions, which are usually less painful.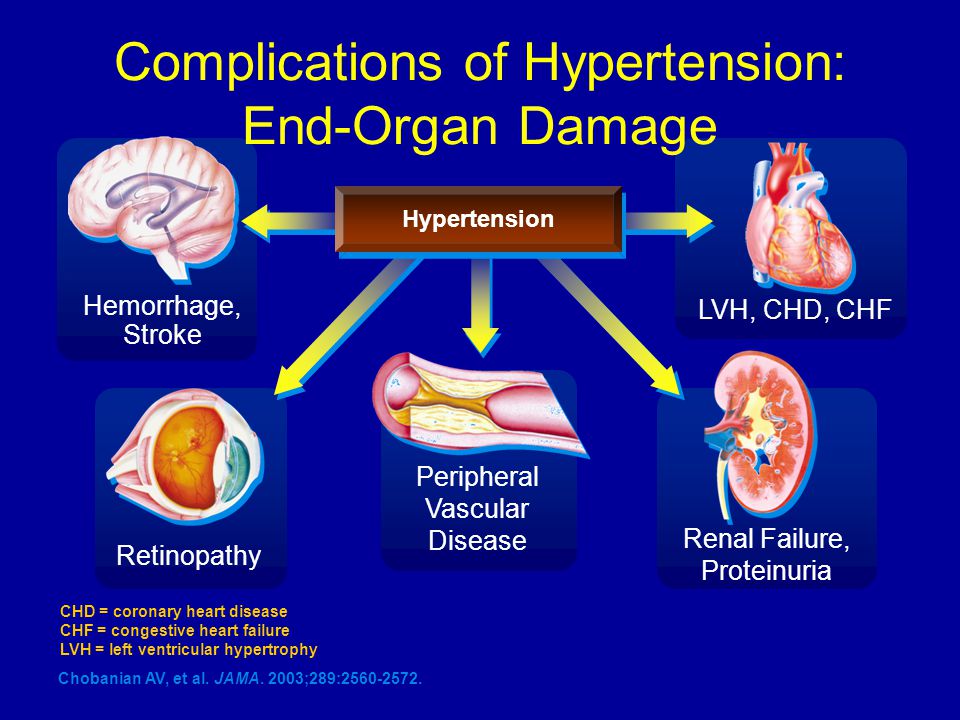 Discoordinated contractions are accompanied by a noticeable increase in the tone of the myometrium, an irregular rhythm of its contraction and relaxation, uneven strength of contractions and pain in labor. Usually at the same time the woman feels the expressed anxiety.
Discoordinated contractions are accompanied by a noticeable increase in the tone of the myometrium, an irregular rhythm of its contraction and relaxation, uneven strength of contractions and pain in labor. Usually at the same time the woman feels the expressed anxiety.
Although pain is always present in childbirth in the absence of anesthesia, a change in its intensity may indicate the development of complications. More often, a pronounced pain syndrome occurs with a threatening and incipient uterine rupture. Immediately at the moment of rupture, the pain decreases, and the contractions of the myometrium stop. If during childbirth or immediately after them, a woman complains of a sharp (“shooting”) pain in the area of the pubic joint, a discrepancy or rupture of the pelvic ring can be suspected.
The appearance of abundant watery discharge from the vagina indicates the outflow of amniotic fluid. In contrast to the timely opening of the fetal bladder in normal childbirth, its premature rupture is considered a complication, often provokes a weakening of labor activity, prolapse of parts of the fetus or umbilical cord into the vagina. Bloody discharge in the first stage of labor is usually the result of premature exfoliation of the placenta. In the second period, they most often accompany ruptures of the birth canal, and in the third they occur as a result of myometrial hypotension or retention of parts of the placenta in the uterine cavity.
Bloody discharge in the first stage of labor is usually the result of premature exfoliation of the placenta. In the second period, they most often accompany ruptures of the birth canal, and in the third they occur as a result of myometrial hypotension or retention of parts of the placenta in the uterine cavity.
With the development of extragenital complications of childbirth, general changes in the woman's well-being are observed. She may feel sudden weakness, dizziness, loss of vision, flies or blurred vision, palpitations, sweating, feeling cold, trembling. In the period between contractions and, especially, during contractions, fetal movements are usually not felt, but when hypoxia occurs, the discomfort experienced by the child makes him move actively. Therefore, the increased activity of the fetus in the period between contractions should be a reason for the alertness of the obstetrician-gynecologist.
Diagnostics
Diagnostic measures during childbirth are aimed at assessing the condition of the woman in labor and the child, timely detection of complications and determining their severity.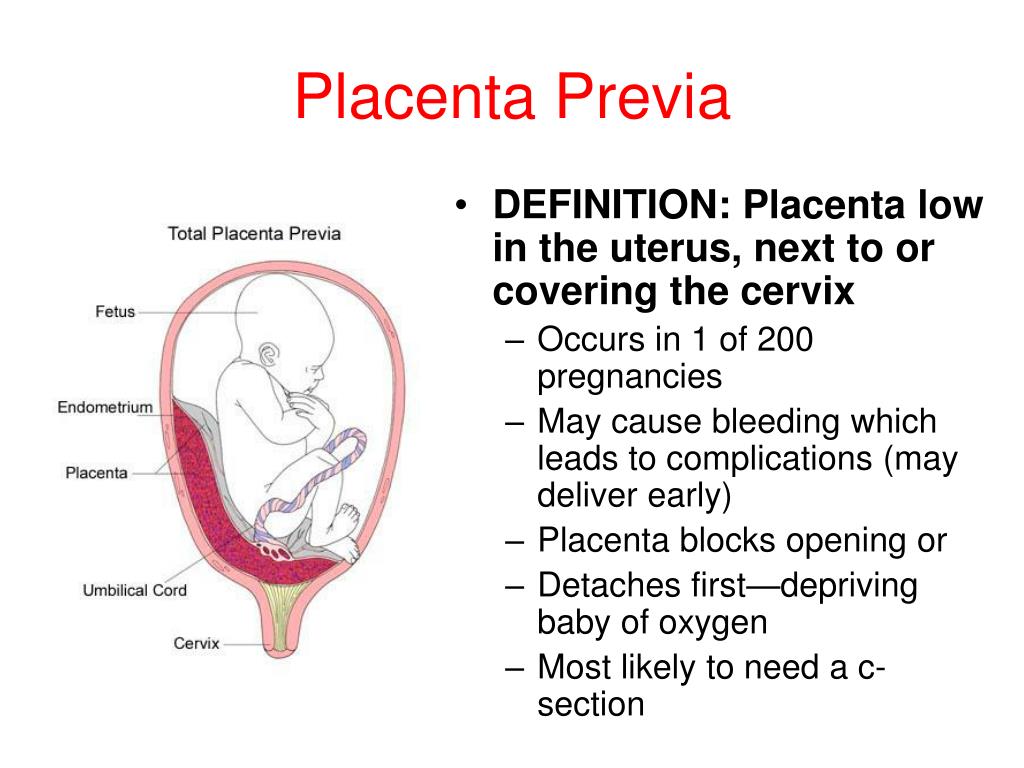 If you suspect a complicated course of childbirth, the following are recommended:
If you suspect a complicated course of childbirth, the following are recommended:
- External obstetric examination. Allows you to determine the shape and size of the uterus, the height of its bottom, the degree of cervical opening (approximately), the correspondence between the size of the pelvis and the head of the child, assess the frequency, strength and rhythm of contractions, identify areas of local pain.
- Vaginal examination. It is used to determine the state of the cervix, the degree of its disclosure, the integrity of the amniotic bladder, the presenting part of the fetus and the features of its progress through the birth canal. During the examination, blood, umbilical cord, parts of the fetus can be detected in the vagina.
- Cardiotocography. Allows you to monitor the contractile activity of the uterus and the fetal heartbeat, to detect signs of hypoxia and other threats to the child in time, accompanied by an increase or slowdown in cardiac activity.
- Gynecological ultrasound. Due to the rapid dynamics of childbirth during their management, ultrasound examinations are prescribed much less frequently than during pregnancy. In some cases, with their help, the position of the fetus, the umbilical cord, the condition of the placenta and the scar on the uterus are clarified.
- Inspection of the birth canal after childbirth. Revision of the cervix with the help of special spoon-shaped mirrors makes it possible to identify and suture its tears in time. The vagina and perineum are then examined for tears.
- Manual examination of the uterus. It is a medical and diagnostic procedure. It is carried out in case of suspicion of a delay in the uterine cavity of fragments of the placenta.
If necessary, a woman is prescribed a complete blood count, ECG, monitoring of pulse and blood pressure. Since pathological conditions are directly related to the process of childbirth, differential diagnosis is carried out between various types of complications. According to the indications, an anesthesiologist-resuscitator, therapist, neuropathologist, neonatologist are involved in the management of childbirth.
According to the indications, an anesthesiologist-resuscitator, therapist, neuropathologist, neonatologist are involved in the management of childbirth.
Treatment of birth complications
Obstetric tactics is aimed at choosing the optimal method of delivery with minimizing the consequences for the woman in labor and the fetus. The choice of specific drugs and techniques is determined by the type of complications. In natural complicated childbirth are assigned:
- Uterine contraction stimulants. Strengthen contractions and accelerate the process of childbirth in patients with complications in the form of primary or secondary weakness of labor.
- Tocolytics. They allow you to relax the uterine muscles during violent or discoordinated contractions, hypertonicity, the threat of scar rupture.
- Painkillers. Depending on the intensity of pain and its subjective perception by the woman in labor, a wide range of drugs and methods are used, from the appointment of analgesics to epidural or paravertebral anesthesia and general anesthesia.
- Sedative preparations. They reduce emotional stress, potentiate the effect of analgesic therapy, allow a woman to better control the birth process in response to instructions from midwives and doctors.
Complication of childbirth by bleeding serves as an indication for the appointment of infusion therapy using hemostatics, blood-substituting solutions and blood products, oxygen inhalation through a mask. With persistent bleeding after the birth of a child, a revision of the birth canal for ruptures is shown, followed by suturing and manual examination of the uterine cavity to detect and remove the remains of the placenta. In rapid labor, at the birth of a large fetus, a child with hydrocephalus or in a non-physiological position / presentation, when using obstetric aids or operations, the threat of damage to the birth canal increases. Therefore, the woman in labor routinely produce an episiotomy.
Incorrect presentation and position of the fetus is an indication for the use of one of the obstetric aids - turning the fetus on the head (according to Arkhangelsk) or leg, classical manual or Tsovyanov's aid in breech presentation.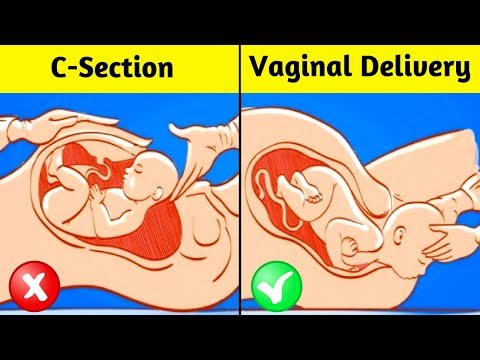 If the position of the fetus prevents natural childbirth, a caesarean section is recommended. If the mother and child are threatened, obstetric operations can be used to complete labor more quickly - vacuum extirpation of the fetus, its extraction by the pelvic end, or the application of obstetric forceps. In the event of the death of the child and the impossibility of completing the birth naturally or by caesarean section, fruit-destroying operations are performed.
If the position of the fetus prevents natural childbirth, a caesarean section is recommended. If the mother and child are threatened, obstetric operations can be used to complete labor more quickly - vacuum extirpation of the fetus, its extraction by the pelvic end, or the application of obstetric forceps. In the event of the death of the child and the impossibility of completing the birth naturally or by caesarean section, fruit-destroying operations are performed.
Urgent delivery by caesarean section is indicated in case of an acute threat to the life of the woman in labor and the child (uterine rupture, placental abruption, prolapse of the umbilical cord). In some cases, abdominal surgery ends with extirpation of the uterus. Hysterectomy is performed with massive ruptures with the formation of intraligamentary hematomas, ongoing bleeding, placenta ingrowth, a long anhydrous period with a complication of its infectious process.
Prognosis and prevention
The prognosis of complicated births depends on the type of pathology, the timeliness of its diagnosis and the adequacy of obstetric tactics. In the vast majority of cases, the outcome is favorable for the child and for the mother. In Russia, the maternal mortality rate has been declining year by year and in 2016 reached a historic low of 8.3 per 100,000 births. Infant, including intrapartum, mortality is also constantly declining. For the prevention of complications of childbirth, timely registration and dynamic monitoring in the antenatal clinic, treatment of identified concomitant diseases and complications of pregnancy, planned hospitalization in the maternity hospital, if indicated, are important. A key role in preventing intranatal threats is played by the correct choice of the method of delivery and the professionalism of medical personnel in the conduct of childbirth.
In the vast majority of cases, the outcome is favorable for the child and for the mother. In Russia, the maternal mortality rate has been declining year by year and in 2016 reached a historic low of 8.3 per 100,000 births. Infant, including intrapartum, mortality is also constantly declining. For the prevention of complications of childbirth, timely registration and dynamic monitoring in the antenatal clinic, treatment of identified concomitant diseases and complications of pregnancy, planned hospitalization in the maternity hospital, if indicated, are important. A key role in preventing intranatal threats is played by the correct choice of the method of delivery and the professionalism of medical personnel in the conduct of childbirth.
You can share your medical history, what helped you in the treatment of complications of childbirth.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.
 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor. complications of childbirth - Articles about pregnancy and childbirth
sections
- Pregnancy on the background of diseases
- Pregnancy Conducting
- Ectopic pregnancy
- where and how to give birth to
- Decree leave
- 9001 fertilization
- Pregnancy calendar
- Caesarean section
- Breastfeeding
- Beauty and pregnancy
- Courses for pregnant women
- Medicines and pregnancy
- Miscarriage
- Non-traditional childbirth
- Labor pain relief
- Lifestyle
- Ovulation. Conception
- Pregnancy complications
- Corn complications
- Pregnancy planning
- purchases for mom and baby
- after birth
- Borning of birth
- Signs of pregnancy
- Child Born
- Typical complaints0012
- Physiology of pregnancy
- Physiology of childbirth
Difficult labor
Pregnancy is one of the most exciting periods in a woman's life. And this is connected not only with the expectation of joy from the appearance of the baby, but also with many fears: how the birth will go, whether everything will be fine, whether the child will be healthy, how long it will take to recover. Some women are so afraid of the process of having a baby that they may refuse to have children at all because of it. But many troubles can be prevented by arming with the necessary knowledge.
And this is connected not only with the expectation of joy from the appearance of the baby, but also with many fears: how the birth will go, whether everything will be fine, whether the child will be healthy, how long it will take to recover. Some women are so afraid of the process of having a baby that they may refuse to have children at all because of it. But many troubles can be prevented by arming with the necessary knowledge.
Narrow pelvis
Anomalies of the bony pelvis are among the most common causes of disrupted labor.
Weakness of labor: causes, diagnosis, treatment
Weakness of labor is said to be when contractions do not intensify over time, but weaken.
Cervical ruptures
Cervical ruptures occur in 6% of women in labor, and are 4 times more common in first births than in second births.
Perineal tears
Perineal tears are one of the most frequent complications of childbirth, they occur in about 35% of women in labor, and in primiparas 2-3 times more often than in multiparous.
Premature birth
Premature birth is defined as 22-36 weeks of gestation, or to be more precise, on the 154th-259th day from the first day of the last menstruation³. You can find out that preterm labor (hereinafter referred to as PR) has begun by obvious symptoms. We will tell you what to look for so as not to miss their onset, how to act in this case, and what modern methods of treatment are used in medicine to maintain pregnancy.
Premature rupture of amniotic fluid
Normally, rupture of the amniotic sac should occur when the cervix is fully or almost fully dilated (at the end of the first stage of labor).
Postpartum haemorrhage
Unfortunately, only 14% of births are uneventful. The most common symptom of the pathological postpartum period is bleeding.
Firm attachment or accreta of the placenta If it doesn't, doctors may suspect a placental accreta or placenta accreta.
Delayed or strangulated placenta
Birth does not end with the baby.