What is the white stuff on newborn babies
UNRAVELING THE MYSTERY OF VERNIX CASEOSA
1. The oxford english dictionary. Oxford, England: Oxford University Press; 1989. [Google Scholar]
2. Hoath SB, Narendran V, Visscher M. Role and biology of vernix. Neonatal Infant Nurs Rev. 2001;1:53–8. [Google Scholar]
3. Pochi P. The sebaceous gland. In: Maibach H, Berardesca E, editors. Neonatal skin. New York: Marcel Dekker; 1982. pp. 67–80. [Google Scholar]
4. Dietel K. Morphological and functional development of the skin. In: Stave U, editor. Perinatal physiology. New York: Plenum Press; 1978. pp. 111–4. [Google Scholar]
5. Moore KL. Philadelphia, Penna: Saunders; 1988. The developing human: Clinically oriented embryology. [Google Scholar]
6. Nemes Z, Steinert PM. Bricks and mortar of the epidermal barrier. Exp Mol Med. 1999;31:5–19. [PubMed] [Google Scholar]
7. Snell RS. Clinical embryology for medical students. Boston: Little; 1983. [Google Scholar]
8. Pansky B. Medical embryology. New York: Macmillin; 1982. [Google Scholar]
9. Langman J. Medical embryology. Baltimore, MD: Williams and Wilkins; 1981. [Google Scholar]
10. Narendran V. Hoath SB. The Biology of Vernix Caseosa. J Neonatol. 2002;16:9–17. [Google Scholar]
11. Holbrook K, Odland G. Regional development of the human epidermis in the first trimester fetus (age related to the timing of amniocentesis and fetal biopsy) J Invest Dermatol. 1980;74:161–8. [PubMed] [Google Scholar]
12. Holbrook K. Structure and function of the developing human skin. In: Goldsmith L, editor. Physiology, biochemistry and molecular biology of the skin. Oxford: Oxford university Press; 1991. pp. 63–110. [Google Scholar]
13. Hardman MJ, Sisi P, Banbury DN, Byrne C. Patterned acquisition of skin barrier function during development. Development. 1998;125:1541–52. [PubMed] [Google Scholar]
14. Elias P. The stratum corneum revisited. J Dermatol. 1996;23:756–8. [PubMed] [Google Scholar]
15. Pochi PE. The sebaceous gland. In: Maibach HI, Boisits EK, editors. Neonatal skin. New York: Marcel Dekker; 1982. pp. 67–80. [Google Scholar]
The sebaceous gland. In: Maibach HI, Boisits EK, editors. Neonatal skin. New York: Marcel Dekker; 1982. pp. 67–80. [Google Scholar]
16. Holbrook KA. Structural and biochemical organogenesis of skin and cutaneous appendages in the fetus and newborn. In: Polin FW, Fox RA, editors. Fetal and neonatal physiology. Philadelphia: WB Saunders Company; 1998. pp. 729–52. [Google Scholar]
17. Froh DK, Ballard PL. Fetal lung maturation. In: Thorburn GD, Harding R, editors. Textbook of fetal physiology. New York: Oxford University Press; 1994. pp. 168–85. [Google Scholar]
18. Narendran V, Wickett RR, Pickens WL, Hoath SB. Interaction between pulmonary surfactant and vernix: A potential mechanism for induction of amniotic fluid turbidity. Pediatr Res. 2000;48:120–4. [PubMed] [Google Scholar]
19. Atherton DJ, Gennery AR, Cant AJ. The neonate. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Text Book of Dermatology. 7th ed [Google Scholar]
20. Rutter N. The immature skin. Eur J Pediatr. 1996;155:S18–20. [PubMed] [Google Scholar]
The immature skin. Eur J Pediatr. 1996;155:S18–20. [PubMed] [Google Scholar]
21. Akiba T. Studies on biological actions of vernix caseosa. Jpn Obstet Gynecol Soc. 1955;2:396–411. [PubMed] [Google Scholar]
22. Visscher MO, Narendran V, Pickens WL, LaRuffa AA, Meinzen-Derr J, Allen K, et al. Vernix caseosa in neonatal adaptation. J Perinatol. 2005;25:440–6. [PubMed] [Google Scholar]
23. Hoeger PH, Schreiner V, Klaassen IA, Enzmann CC, Friedrichs K, Bleck O. Epidermal Barrier lipids in human vernix caseosa: Corresponding ceramide pattern in vernix and fetal skin. Br J Dermatol. 2002;146:194–201. [PubMed] [Google Scholar]
24. Warner R, Lilly N. Correlation of water content with ultrastructure of stratum corneum. In: Elsner P, Berardesca E, Maibach HI, editors. Bioengineering of the skin: water and the stratum corneum. Boca Raton, Fla: CRC Press; 1994. pp. 3–12. [Google Scholar]
25. Sumida Y, Yakumaru M, Tokitsu Y, et al. Studies on the function of Vernix caseosa: The secrecy of Baby's skin. Cannes, France: International Federation of the Societies of Cosmetic Chemists 20th International Conference; 1998. pp. 1–7. [Google Scholar]
Cannes, France: International Federation of the Societies of Cosmetic Chemists 20th International Conference; 1998. pp. 1–7. [Google Scholar]
26. Rissmann R, Groenink HW, Weerheim AM, Hoath SB, Ponec M, Bouwstra JA. New insights into ultrastructure, lipid composition and organization of Vernix Caseosa. J Invest Dermatol. 2006;126:1823–33. [PubMed] [Google Scholar]
27. Pickens W, Warner R, Boissy R, Sb H. Characterization of human vernix: Water content, morphology and elemental analysis. J Invest Dermatol. 2000;115:875–81. [PubMed] [Google Scholar]
28. Agarastos T, Hollweg G, Grussendorf EI, Papaloucas A. Features of vernix caseosa cells. Am J Perinatol. 1988;5:253–9. [PubMed] [Google Scholar]
29. Tollin M, Jagerbrink T, Haraldsson A, Agerberth B, Jornvall H. Proteome analysis of vernix caseosa. Pediatr Res. 2006;20:430–4. [PubMed] [Google Scholar]
30. Baker SM, Balo NN, Abdul Aziz FT. Is Vernix a protective material to the newborn? A biochemical approach. Indian J Pediatr. 1995;62:237–9. [PubMed] [Google Scholar]
1995;62:237–9. [PubMed] [Google Scholar]
31. Buchman AL. Glutamine: Is it conditionally required nutrient for human gastrointestinal system? J Am Coll Nutr. 1996;15:199–205. [PubMed] [Google Scholar]
32. Haubrich RA. Role of vernix caseosa in the neonate. AACN Clin Issues. 2003;14:457–64. [PubMed] [Google Scholar]
33. Saunders C. The Vernix Caseosa and subnormal temperatures in premature infants. Br J Obstet Gynaecol. 1948;55:442–4. [PubMed] [Google Scholar]
34. Shaulak B. The antibacterial action of Vernix Caseosa. Harper Hosp Bull. 1963;21:111–7. [PubMed] [Google Scholar]
35. Riesenfeld B, Strombery B, Sedin G. The influence of Vernix Caseosa on water transport through semi permeable membranes and the skin of full- term infants. Neonatal Physiological Measurements. 1984:3–6. [Google Scholar]
36. Visscher MS, Munson KA, Bare DE, Hoath SB. Early Adaptation of human skin following birth: A biophysical assessment. Skin Res Technol. 1999;5:213–20. [Google Scholar]
37. Hoeger PH, Enzmann CC. Skin Physiology of the neonate and young infant: A prospective study of functional skin parameters during early infancy. Pediatr Dermatol. 2002;19:256–62. [PubMed] [Google Scholar]
Hoeger PH, Enzmann CC. Skin Physiology of the neonate and young infant: A prospective study of functional skin parameters during early infancy. Pediatr Dermatol. 2002;19:256–62. [PubMed] [Google Scholar]
38. Herrmann F, Behrendt H, Karp F. On the acidity of the surface of the scalp and other areas of the skin in children. J Invest Dermatol. 1946;7:215. [PubMed] [Google Scholar]
39. Puhvel SM, Reisner RM, Amirian DA. Quantification of bacteria in isolated pilosebaceous follicles in normal skin. J Invest Dermatol. 1975;65:525–31. [PubMed] [Google Scholar]
40. Aly R, Maibach HI, Rahman R, Shinefield HR, Mandel AD. Correlation of human in vivo and in vitro cutaneous antimicrobial factors. J Infect Dis. 1975;131:579–83. [PubMed] [Google Scholar]
41. Fluhr JW, Kao J, Jain M, Abn SK, Feingold KR, Elias PM. Generation of free fatty acids from phospholipids regulates stratum corneum acidification and integrity. J Invest Dermatol. 2001;117:44–51. [PubMed] [Google Scholar]
42. Parra JL, Paye M. EEMCO guidance for the in vivo assessment of skin surface PH. Skin Pharmacol Appl Skin Physiol. 2003;16:188–202. [PubMed] [Google Scholar]
Parra JL, Paye M. EEMCO guidance for the in vivo assessment of skin surface PH. Skin Pharmacol Appl Skin Physiol. 2003;16:188–202. [PubMed] [Google Scholar]
43. Lukacs A. Invitro control of the growth of important bacteria of the resident flora by changes in PH. In: Brain-Falco O, Korting H, editors. Skin cleansing with synthetic detergents. Berlin: Springer; 1992. pp. 97–105. [Google Scholar]
44. Thiele J, Weber S, Packer L. Sebaceous gland secretion is a major physiological route of Vitamin E delivery to skin. J Invest Dermatol. 1999;113:1006–10. [PubMed] [Google Scholar]
45. Thiele J, Packer L. Non-invasive measurement of alpha-tocopherol gradients in human stratum corneum by high performance liquid chromatography analysis of sequential tape strippings. Met Enzymol. 1999;300:413–9. [PubMed] [Google Scholar]
46. Pickens W, Zhou Y, Wickett R, Vischer M, Hoath S. Antioxidant defense mechanisms in Vernix Caseosa: Potential role of endogenous Vitamin E. Pediatr Res. 2000;47:425A. [Google Scholar]
2000;47:425A. [Google Scholar]
47. Youssef W, Hoath S. Surface free energy characterization of Vernix caseosa: Role in waterproofing the newborn infant. Skin Res Technol. 2001;7:1–17. [PubMed] [Google Scholar]
48. Thiele JJ, Traber MG, Polefka TG, Cross CE, Packer L. Ozone-exposure depletes Vitamin E and induces lipid perioxidation in murine stratum corneum. J Invest Dermatol. 1997;108:753–7. [PubMed] [Google Scholar]
49. Thiele JJ, Traber MG, Packer L. Depletion of human stratum corneum Vitamin E: An early and sensitive in vivo marker of UV induced photooxidation. J Invest Dermatol. 1998;110:756–61. [PubMed] [Google Scholar]
50. Joglekar VM. Barrier properties of Vernix Caseosa. Arch Dis Child. 1980;55:817–9. [PMC free article] [PubMed] [Google Scholar]
51. Tansirikongkol A, Wickett RR, Visscher MO, Hoath SB. Effect of Vernix Caseosa on the penetration of chymotryptic enzyme: Potential role in epidermal Barrier development. Pediatr Res. 2007;62:49–53. [PubMed] [Google Scholar]
52. Yoshio H, Tollin M, Gudmundsson GH, Lagercrantz H, Jornvall H, Marchini G, et al. Antimicrobial polypeptides of human Vernix Caseosa and amniotic fluid: Implications for newborn innate defense. Pediatr Res. 2003;53:211–6. [PubMed] [Google Scholar]
Yoshio H, Tollin M, Gudmundsson GH, Lagercrantz H, Jornvall H, Marchini G, et al. Antimicrobial polypeptides of human Vernix Caseosa and amniotic fluid: Implications for newborn innate defense. Pediatr Res. 2003;53:211–6. [PubMed] [Google Scholar]
53. Tollin M, Bergsson G, Kai-Larsen Y, Lengqvist J, Sjövall J, Griffiths W, et al. Vernix Caseosa as a multi component defense system based on polypeptides, lipids and their interactions. Cell Mol Life Sci. 2005;62:2390–9. [PMC free article] [PubMed] [Google Scholar]
54. Akinbi HT, Narendran V, Pass AK, Markart P, Hoath SB. Host defense proteins in Vernix Caseosa and amniotic fluid. Am J Obstet Gynecol. 2004;191:2090–6. [PubMed] [Google Scholar]
55. Narendran V, Hull W, Akinbi H. Vernix Caseosa contains surfactant proteins: Potential Role in innate immune function in the fetus. Pediatr Res. 2000;47:420A. [Google Scholar]
56. Kuroki Y, Sano H. Functional roles and structural analysis of lung collectins SP-A and SP-D. Biology Neonate.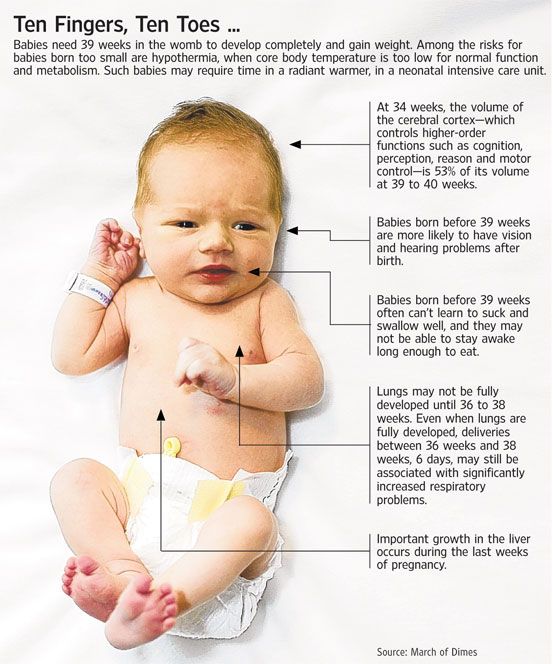 1999;76:19–21. [PubMed] [Google Scholar]
1999;76:19–21. [PubMed] [Google Scholar]
57. Bautista MI, Wickett RR, Vischer MO, Pickens WL, Hoath SB. Characterization of Vernix Caseosa as a natural biofilm: Comparison to standard oil based ointments. Pediatr Dermatol. 2000;17:253–60. [PubMed] [Google Scholar]
58. Rawlings AV, Scott IR, Harding CR, Bowser PA. Stratum corneum moisturization at the molecular level. J Invest Dermatol. 1994;103:734–41. [PubMed] [Google Scholar]
59. Nopper AJ, Horii KA, Sookdeo-Drost S, Wang TH, Mancini AJ, Lane AT. Topical ointment therapy benefits premature infants. J Pediatr. 1996;128:660–9. [PubMed] [Google Scholar]
60. Conner JM, Soll RF, Edward WH. Topical ointment for preventing infection in preterm infants. Cochrane Database Syst Rev. 2004. CD001150. [PubMed]
61. Barai N. College of Pharmacy. Cincinnati, OH: University of Cincinnati; 2005. Effect of Vernix Caseosa on epidermal barrier development-repair: Implications in wound healing. [Google Scholar]
62. Grubauer G, Elias P, Feingold K. Transepidermal water loss: The signal for recovery of barrier structure and function. J Lipid Res. 1989;30:323–33. [PubMed] [Google Scholar]
Transepidermal water loss: The signal for recovery of barrier structure and function. J Lipid Res. 1989;30:323–33. [PubMed] [Google Scholar]
63. Proksch E, Holleran WM, Menon GK, Elias PM, Feingold KR. Barrier function regulates epidermal lipid and DNA synthesis. Br J Dermatol. 1993;128:473–82. [PubMed] [Google Scholar]
64. Zhukov B, Neverova E, Nikitin K. A comparative evaluation of the use of Vernix Caseosa and Solcoseryl in treating patients with trophic ulcers of lower extremities. Vestnik Khirurgii Imeni I I Grekova. 1992;148:339–41. [PubMed] [Google Scholar]
65. Roos TC, Geuer S, Roos S, Brost H. Recent advances in treatment strategies for Atopic Dermatitis. Drugs. 2004;64:2639–66. [PubMed] [Google Scholar]
66. Morailli R, Pickens WL, Vischer MO, Hoath SB. A novel role for Vernix Caseosa as a skin cleanser. Biol Neonate. 2004;87:8–14. [PubMed] [Google Scholar]
67. Lund C, Kuller J, Lane A, Lott JW, Raines DA. Neonatal skin care: The scientific basis for practice. Neonatal Netw. 1999;18:15–27. [PubMed] [Google Scholar]
Neonatal Netw. 1999;18:15–27. [PubMed] [Google Scholar]
68. Lott J, Hoath S. Neonatal skin: The ideal nursing interface. J Pediatr Nurs. 1998;13:302–6. [PubMed] [Google Scholar]
69. Association of Women's Health Obstetrical and Neonatal Nurses (AWHONN) and National Association of Neonatal Nursing (NANN) Evidence-based nursing practice-skin care. Washington DC: 2001. [Google Scholar]
70. Hoath SB, Narendran V. 50 years ago in The Journal of Pediatrics. J Pediatr. 2004;144:396. [Google Scholar]
71. Dolyniuk M, Orfei E, Vania H, Karlman R, Tomich P. Rapid diagnosis of amniotic fluid embolism. Obstet Gynecol. 1983;61:28S. [PubMed] [Google Scholar]
72. McLaughlan JM, Chang AM. Lecithin: Sphingomyelin ratio and presence of vernix in amniotic fluid. South Brisbane, Queensland: Department of Obstetrics and Gynaecology, Mater Misericordiae Mothers' Hospital; 1977. pp. 1544–5. [PMC free article] [PubMed] [Google Scholar]
73. Varela J, Pettinelli E, Molina R, Naverrete J, Zambrano N, Vera R. Analysis of the vernix in the amniotic fluid as a prognostic index of the weight of the newborn. Rev Chil Obstet Ginecol. 1974;39:49–51. [PubMed] [Google Scholar]
Analysis of the vernix in the amniotic fluid as a prognostic index of the weight of the newborn. Rev Chil Obstet Ginecol. 1974;39:49–51. [PubMed] [Google Scholar]
74. Sepulveda WH, Araneda H, Avendano A. Ultrasonic detection of fetal vernix in amniotic fluid as an index to fetal maturity. Rev Chil Obstet Ginecol. 1991;56:43–7. [PubMed] [Google Scholar]
75. Moore C, Dempsey D, Deitermann D, Lewis D, Leikin J. Fetal cocaine exposure: Analysis of vernix caseosa. J Anal Toxicol. 1996;20:509–11. [PubMed] [Google Scholar]
76. O'Grady JP, Prefontaine M, Hoffman DE. Vernixuria: Another sign of uterine rupture. J Perinatol. 2003;23:351–2. [PubMed] [Google Scholar]
77. Boothby R, Lammert N, Benrubi GI, Weiss B. Vernix caseosa granuloma: A rare complication of cesarean section. Southern Med J. 1985;78:1395–6. [PubMed] [Google Scholar]
78. Krunerman MS, Pouliot GJ. Maternal vernix caseosa peritonitis: Rare complications of cesarean sections. N Y State J Med. 1976;76:1879–80. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
79. Mahmoud A, Silapaswas S, Lin K, Penney D. Vernix caseosa: An unusual cause of post-cesarean section peritonitis. Am Surg. 1997;63:382–5. [PubMed] [Google Scholar]
80. Levine RS, Dolin P. Pregnancy and breast cancer: A possible explanation for the negative association. Med Hypotheses. 1992;38:278–83. [PubMed] [Google Scholar]
81. Hoath SB, Pickens WL, Visscher MO. The biology of vernix caseosa. Int J Cosmet Sci. 2006;28:319–33. [PubMed] [Google Scholar]
82. Nishijima K, Shukunami K, Inoue S, Kotsuji F. Management for neonatal aspiration syndrome caused by vernix caseosa. Fetal Diagn Ther. 2005;20:194–6. [PubMed] [Google Scholar]
83. Ohlsson A, Cumming WA, Najjar H. Neonatal aspiration syndrome due to vernix caseosa. Pediatr Radiol. 1985;15:193–5. [PubMed] [Google Scholar]
84. Midha R, Becker LE. Vernix caseo granulomatous meningitis (vernicomyelia) Can J Neurol Sci. 1991;18:63–5. [PubMed] [Google Scholar]
What Is Vernix Caseosa and What Is Its Function
Babies are often born covered in a creamy-looking substance called vernix caseosa, a protective film that benefits sensitive newborn skin. Read on to learn more about what vernix is, what its function is, why some babies are born with the coating still on, and when you should first bathe your baby if your little one was born with lots of vernix still on.
Read on to learn more about what vernix is, what its function is, why some babies are born with the coating still on, and when you should first bathe your baby if your little one was born with lots of vernix still on.
What Is Vernix Caseosa?
Vernix caseosa, or vernix for short, is a white, cheesy-looking substance that coats the skin of your baby while in the uterus. Some babies are born with some of this protective coating still on the skin. The meaning of the name vernix caseosa is “varnish of a cheesy nature.”
During your pregnancy, vernix plays an essential role, acting as a waterproof barrier to protect your baby’s skin against the amniotic fluid that surrounds her until she is born.
A naturally occurring biofilm, vernix begins to cover your baby’s skin during the second trimester. The sebaceous glands — which are responsible for producing oil in the skin —begin to produce the vernix coating at around 17 weeks of pregnancy.
Vernix caseosa is simply a creamy, greasy substance mostly composed of water, lipids, and proteins. It contains enzymes and other innate immune proteins that have antibacterial properties.
What Are the Benefits of Vernix Caseosa?
You can think of vernix caseosa as a protective layer for your baby’s skin. It helps shield his delicate skin from abrasions, chapping, and hardening that could be caused by prolonged exposure to amniotic fluid, and it also has some benefits for your baby after birth.
The Benefits of Vernix Caseosa in the Womb
Before your baby is born, vernix caseosa’s function in utero is to:
Protect the fetus from damaging substances, like urea and electrolytes, in the amniotic fluid.
Help with thermoregulation.
During a vaginal delivery, vernix acts as a lubricant and a protective biofilm, and also acts as an antimicrobial cover against any bacteria in the genital tract.
The Benefits of Vernix Caseosa After Birth
Vernix also has a few benefits for your baby after she is born:
It acts as a natural moisturizer. Vernix could help prevent your newborn’s skin from becoming dry. Its high water content helps lock moisture into the skin and reduces moisture loss.
It may have antibacterial properties. Vernix could protect your newborn baby from getting a skin infection shortly after birth.
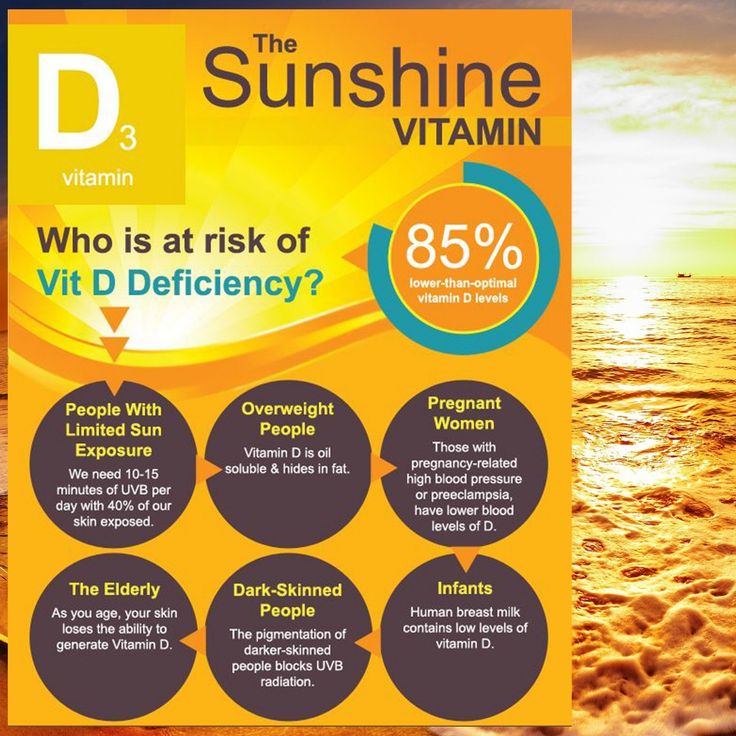
It has antioxidant properties. Vernix contains antioxidants like vitamin E and melanin, which help slow down cell damage due to free radicals.
When to Wash the Vernix Off
In the past, most hospitals and birthing centers would bathe babies within an hour or two of birth. Now, however, this practice is changing, as more is known about the benefits of vernix and the benefits of postponing the first bath.
When your baby is born, he’ll be covered in amniotic fluid, perhaps some blood, and potentially some vernix. It’s natural to want to bathe your baby, but you may also be wondering whether there are benefits in leaving the vernix on for longer, especially given all its benefits.
The World Health Organization (WHO) recommends waiting at least 6 hours before bathing the newborn baby and ideally waiting about 24 hours. The WHO also recommends not wiping off the vernix at birth.
It’s natural to want to bathe your baby, but you may also be wondering whether there are benefits in leaving the vernix on for longer, especially given all its benefits.
The World Health Organization (WHO) recommends waiting at least 6 hours before bathing the newborn baby and ideally waiting about 24 hours. The WHO also recommends not wiping off the vernix at birth.
The main reasons to wait with your baby’s first bath include:
Keeping your little one warm and stabilizing blood sugar levels. Babies who are bathed too soon after birth are more likely to become cold and could develop hypothermia. The stress of having a bath right after birth could also cause a drop in blood sugar levels.
Allowing time for breastfeeding and bonding. The “golden hour” period right after you give birth is great for skin-to-skin contact and parent-child bonding. This shared time can also help with early breastfeeding. In fact, one study found a 166 percent increase in hospital breastfeeding success when infants were bathed 12 hours or more after birth compared to those babies who were bathed within hours of birth.

Helping prevent dry skin. Leaving vernix on the skin for a few hours can help keep newborn skin supple and hydrated.
How Long Can You Leave Vernix Caseosa on Your Baby?
The WHO recommends leaving vernix on your baby’s skin for at least 6 hours but preferably 24 hours.
If you’re considering leaving it on for longer, ask your baby’s healthcare provider how long it remains beneficial to leave the vernix coating on your baby’s skin and how long to wait with your little one’s first bath.
What Is Lanugo?
Other than vernix, you might also notice a layer of downy hair on your baby’s skin at birth — this is called lanugo.
Lanugo covered your baby’s skin during the latter part of your pregnancy and is usually shed before birth. The presence of lanugo while your baby was in the womb helped the vernix stick to the skin. Lanugo is actually the first type of hair your baby has!
About 30 percent of babies are born with some lanugo still present. It's more likely to be present if your little one is born prematurely.
If your baby was born with some lanugo still on, it usually sheds within a week or two.
It's more likely to be present if your little one is born prematurely.
If your baby was born with some lanugo still on, it usually sheds within a week or two.
The Bottom Line
Vernix caseosa has lots of benefits for your baby both when he is still in the womb and in the hours after birth.
If you can, wait six hours or more before bathing your little one. This won’t just have benefits for your baby’s skin, but it also gives you more time to focus on bonding, skin-to-skin contact, and even on breastfeeding if this is something you would like to try.
Although you might think it’s a little icky and sticky to leave the vernix on, its beneficial properties are important for your baby, and it won’t be long before you’ll have your freshly washed baby skin to kiss and cuddle.
In the meantime, wrap your baby in a soft blanket and enjoy these unforgettable first few hours with your baby, safe in the knowledge that the coating of vernix is also working to protect your baby’s delicate skin. For more information on baby skin care, read up on caring for delicate newborn skin.
For more information on baby skin care, read up on caring for delicate newborn skin.
White coating on the child's tongue - causes and treatment
Article
It has long been believed that the tongue speaks about the state of the whole organism, because even before the onset of symptoms of some disease, the tongue already signals violations in the functioning of organs. There are many microorganisms on the mucous membrane of the tongue, and when bacteria or fungi appear, dead cells get stuck between the papillae - this is how plaque appears.
Normal coating on the tongue
Coating on the tongue does not always indicate a violation, because in some cases it is considered the norm. First of all, the healthy color of the tongue is pale pink. In newborn babies, a uniform white coating may appear after feeding. Older children may have a thin white coating, but if you can see the color of the tongue through it, this is also considered the norm. Usually such plaque can be cleaned with a toothbrush and does not require treatment.
Usually such plaque can be cleaned with a toothbrush and does not require treatment.
Normal tongue:
- not enlarged, medium size;
- pale pink;
- is odour-free;
- Moisture and papillae moderately pronounced;
- no cracks or wounds;
- has normal sensitivity.
Causes and treatment of white coating on the tongue
White coating that is not removed, tightly fits the tongue and has an unpleasant odor is not considered the norm, because such a coating is the result of the multiplication of bacteria and fungi.
Children often complain with him about:
- abdominal pain;
- bloating;
- change in appetite and stool.
These symptoms may signal problems in the digestive system. Accordingly, to solve the problem, it is necessary to consult a gastroenterologist, examine the digestive system and find the cause of the violation.
Often in newborns and children under one year of age, a white coating can cover not only the tongue, but also the lips and cheeks, which indicates thrush - an infection caused by Candida fungi. The reason for this raid is still fragile immunity. Soothers and bottles must be carefully sterilized to avoid disease. Sometimes thrush can also appear in older children - most often these are children with weakened immune systems and asthmatics.
The reason for this raid is still fragile immunity. Soothers and bottles must be carefully sterilized to avoid disease. Sometimes thrush can also appear in older children - most often these are children with weakened immune systems and asthmatics.
Treatment will be with antifungal medications to be prescribed by a pediatrician or neonatologist.
Other causes of plaque on the tongue include:
- dysbacteriosis;
- beriberi;
- infectious diseases;
- improper hygiene;
- effects of drugs;
- inflammatory processes and the like.
Tongue whitening prevention
White coating on the tongue can be prevented if:
- the room where the baby lives is clean, sterile, well ventilated and humidified;
- monitor your health and seek help if you have the slightest symptoms;
- do not self-medicate and do not give the child medicines that have not been prescribed by a doctor;
- limit the use of sweets that contain synthetic pigments and can affect the discoloration of the tongue.

If your child has a white coating on the tongue, it is necessary to consult a pediatrician or neonatologist who can determine the cause of its occurrence, refer to a related specialist or for the necessary tests and studies, and also choose the necessary treatment. Call (067) 127-03-03, (044) 490-25-03 or fill out the form on the website to make an appointment with a doctor.
Related directions:
- Pediatrics
- Neonatology
- Pediatric Otolaryngology
Available methods and prevention of treatment of white plaque on the tongue in infants in an article on the site Pandaland.kz
08.02.2021, 17:29
Modified: 02/08/2023, 13:14
Pandalad always tries to be helpful to moms, dads and grandmas. Today we will discuss the topic of white plaque in the tongue of infants. We will find out the causes of the “white milk path”, consider the methods and prevention of treatment for this disease, and also find out the opinion of an experienced and popular pediatric pediatrician - Evgeny Komarovsky.
White coating on the child's tongue
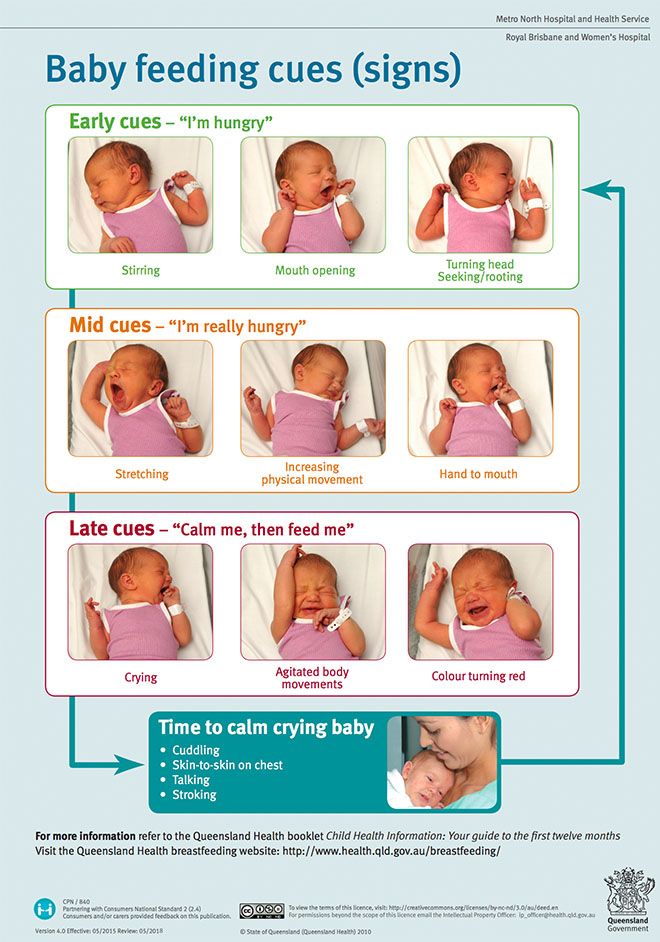
The first year for new parents is not easy, because they have to learn a lot. First of all, it is important to monitor the well-being of the baby, so that if necessary, notice ailments in time and take the necessary measures. One of the common problems is white coating on the tongue of a newborn baby . The reasons for its appearance can be very different. In most cases, plaque consists of normal food leftovers from breastfeeding or formula feeding. But also a white tongue in a newborn can be a manifestation of:
- thrush
- viral stomatitis
- and other diseases
The most common cause of a white tongue in a baby is quite harmless - plaque can appear after breastfeeding or formula. But also a white tongue can be associated with diseases such as thrush or viral stomatitis, which require medical intervention.
Many parents are wondering how to determine when to see a doctor and when there is no reason to worry?
Answer:
Soak a cotton swab in water and gently slide it over your tongue.
The usual plaque is easily removed, and in case of illness, it will remain on the tongue due to the thick curd consistency. In the second case, redness may also appear under the plaque.
There are other signs that indicate the disease:
- If the plaque is only on the tongue, then most likely it is a common trace after feeding.
- But if the inside of the cheeks, palate and gums are covered with white spots, then most likely it is thrush . Also, when sick, the baby may lose his appetite and act up.
The causes of thrush and stomatitis are associated with the ingress of bacteria into the baby's mouth.
Dr. Komarovsky's advice about white coating on the tongue in babies
According to Dr. Komarovsky, thrush can indeed appear in children. Fungal plaque occurs not only on the tongue, but, as a rule, on the mucous membranes (on the inner surface of the cheeks and tongue). The white track on the tongue is the so-called milk plaque. This phenomenon occurs because the child's mouth dries up.
The white track on the tongue is the so-called milk plaque. This phenomenon occurs because the child's mouth dries up.
Milky plaque and thrush occur for the same reasons, because thick saliva dries up in the mouth. It is believed that if the mouth does not dry out, then the entire plaque will disappear without any intervention.
The doctor does not recommend wiping the mouth because it injures the mucosa. Evgeny Komarovsky notes that this method is not effective and even harmful. Parents need to create conditions under which the child will not dry out in the mouth.
Ukrainian pediatrician identifies several main reasons for drying out:
- occasional festivities
- dry and warm air
- continuous screams
- obstructed nasal breathing
The reason for the occurrence of thrush in young children is enough. The doctor notes that you need to fuss when the spots appeared not only on the tongue, but also on the cheeks. For children who are breastfed or artificially fed, a white coating on the tongue is the norm.
For children who are breastfed or artificially fed, a white coating on the tongue is the norm.
The most effective way to treat and prevent thrush is to restore the bactericidal properties of saliva. To do this, parents need:
- a lot of walking
- humidify/ventilate the room
- after drinking milk, give a couple of sips of water so that there are no milk residues in the mouth. If the child is in comfortable conditions, if he does not have pathological fluid losses, then the child does not need to be supplemented. If the room is hot and the child's mouth dries up, while the baby experiences discomfort, then he needs additional liquid (plain water).
Stories from mothers who had white coating on the tongue of their children
Tatiana, 29 years old
According to Tatiana, she first encountered white coating on the tongue when she gave birth to her third child. The two older children did not have any white lines in the oral cavity, but the youngest son had a plaque in the first month of birth. The woman did not understand why the child had a white coating on the tongue. The kid was moody, restless and cried a lot. Tatyana went to the pediatrician and the doctor prescribed a treatment method, after which Tatyana and her family forgot about the thrush.
The two older children did not have any white lines in the oral cavity, but the youngest son had a plaque in the first month of birth. The woman did not understand why the child had a white coating on the tongue. The kid was moody, restless and cried a lot. Tatyana went to the pediatrician and the doctor prescribed a treatment method, after which Tatyana and her family forgot about the thrush.
Bibigul, 30 years old
Bibigul, when she became a mother for the first time, did not know that white coating on the tongue of babies is a fairly common case. The woman and her husband lived in another city away from their relatives, so there was no one to turn to for advice. The first three months after the birth, Bibigul's daughter had no signs of thrush, and after that the baby began to eat poorly and did not breastfeed. The woman made an appointment with the pediatrician, where they found thrush.
How to remove white coating on the tongue of an infant?
As we have already said, white deposits do not need to be purposefully removed. If parents want to make sure what kind of plaque it is, then you can gently swipe along the white path with a moistened cotton swab. If the plaque is easily removed, and there is no redness under it, then this indicates dried milk. Otherwise, we can talk about the disease that has arisen.
If parents want to make sure what kind of plaque it is, then you can gently swipe along the white path with a moistened cotton swab. If the plaque is easily removed, and there is no redness under it, then this indicates dried milk. Otherwise, we can talk about the disease that has arisen.
Once again, we emphasize that plaque formed by dried breast milk or formula is the norm. It will be helpful if you give your baby a sip of water after feeding - this way you will clear the mouth of milk residues and reduce the risk of bacteria breeding.
Treatment and prevention of white plaque on the tongue of a child
To prevent such diseases, sterility must be carefully monitored:
- children's toys
- nipple
- all tableware
When breastfeeding, it is important to take care of breast hygiene.
If you suspect that the plaque is related to the disease in the baby, then it is necessary to consult a doctor to treat the white coating on the child's tongue.