Normal nt at 12 weeks
Chromosomally and Anatomically Normal Fetuses With Increased First Trimester Nuchal Translucency Conceived by ICSI
Iran J Radiol. 2015 Apr; 12(2): e7157.
Published online 2015 Apr 21. doi: 10.5812/iranjradiol.7157
1,* and 1
Author information Article notes Copyright and License information Disclaimer
Nuchal translucency (NT) measurements in the first trimester screening between 11 and 14 weeks’ gestation are regarded as a clear marker for aneuploidies. The presence of a thickened NT, even if the karyotype is normal, can be associated with structural abnormalities. Having an abnormal screening of NT, parents and physicians could face dilemma over abortion particularly in a case of IVF/ICSI fetuses. Measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5%. Hereby we present six cases of chromosomally normal fetuses with an increased NT thickness in the first trimester, a normal karyotype and normal follow-up scans, who had a good prognosis for a normal early childhood. This report may help increase the confidence of couples who are reluctant to terminate the pregnancy.
Keywords: Congenital Abnormalities, Prenatal Diagnosis, Nuchal Translucency Measurement
Fetal nuchal translucency (NT) refers to the sonographic appearance of subcutaneous edema in the fetal neck measured according to the fetal medicine foundation (FMF) guidelines. NT is defined as the maximal thickness of the sonolucent zone (fluid accumulation) between the inner aspect of the fetal skin and the outer aspect of the soft tissue overlying the cervical spine or the occipital bone (). To avoid false negative or positive results, the fetus should be in a neutral position, with the head in line with the spine. During the scan, more than one measurement must be taken and the maximum one that meets the criteria should be considered.
Open in a separate window
According to the FMF guidelines, NT is measured as the maximal thickness of the sonolucent zone (fluid accumulation) between the inner aspect of the fetal skin and the outer aspect of the soft tissue overlying the cervical spine or the occipital bone.
For this report, the outcome of 703 pregnancies presenting at Royan Institute after intra cytoplasmic sperm injection (ICSI) between the years 2008 and 2009 were reviewed. First trimester measurements of NT were performed during the routine first trimester screening for 856 fetuses. A total of 12 fetuses with an increased NT (NT ≥ 3) were considered for further investigation. In the follow-up ultrasounds, six out of 12 fetuses showed no anomalies and the result of amniocentesis (karyotype), fetal echocardiography and triple test or double test (the biochemical markers of pregnancy-associated plasma protein-A and free β-human chorionic gonadotropin) were also normal. Six healthy neonates were followed during their first and second year by routine pediatrician visits and the mental, physical or motor developmental delay was not observed in any of the cases and their functions were normal.
All sonographic measurements were carried out by an expert radiologist with 10 years of experience and FMF certification in the measurement of NT. Images were saved and re-checked by another expert radiologist. Increased NT can be associated with a high incidence rate of chromosomal and non-chromosomal abnormalities. However, in nine studies that have addressed the issue of pediatric long-term follow-up of chromosomally and anatomically normal fetuses with increased NT, this measurement was suggested to be an indefinite indicator for the evaluation of fetal anomalies (1-9).
Images were saved and re-checked by another expert radiologist. Increased NT can be associated with a high incidence rate of chromosomal and non-chromosomal abnormalities. However, in nine studies that have addressed the issue of pediatric long-term follow-up of chromosomally and anatomically normal fetuses with increased NT, this measurement was suggested to be an indefinite indicator for the evaluation of fetal anomalies (1-9).
2.1. Case 1
A 28-year-old woman with a twin pregnancy, which was conceived by ICSI, was referred for routine screening test in the first trimester. The result of semen analysis showed a low motility (35%) with a high abnormal morphology (87%). In the routine first trimester screening at 12 weeks and 2 days of gestation, the NT measurements of the first fetus was 3.4 mm (normal range for this age is 1.2-3.1 mm). Although she refused to undergo the triple test and we had no result for amniocentesis (karyotype) and fetus echocardiography, follow-up ultrasounds revealed normal results. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 3400 grams. Neonates were followed during the first 2 years of their life and none of them had developmental delay.
Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 3400 grams. Neonates were followed during the first 2 years of their life and none of them had developmental delay.
2.2. Case2
A 35-year-old woman, who was conceived by ICSI, was referred for the routine screening test during her pregnancy. Her obstetric and medical history revealed primary infertility for a period of 7 years, mild endometriosis and polycystic ovaries. The result of semen analysis indicated low motility (35%) and high abnormal morphology (88%). During the routine first trimester screening at 13 weeks of gestation, NT was measured at 3 mm. The normal range of NT for this age is 1.6-2.4 mm. Nuchal skin fold (NF) measurements and prenatal follow-up ultrasound findings were normal. A Triple test was performed, and it showed a positive result and a high risk of trisomy 21. The patient was referred for amniocentesis or chorionic villus sampling.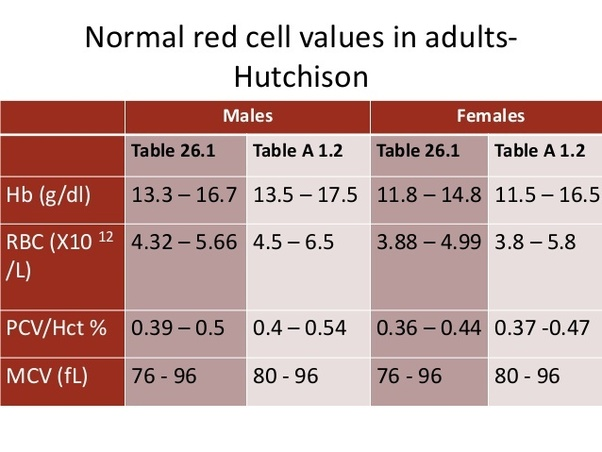 The amniocentesis findings were normal and a healthy baby girl (weight = 3600 grams) was born after a full-term pregnancy. She was followed during the first and second year of life and no developmental delay was detected.
The amniocentesis findings were normal and a healthy baby girl (weight = 3600 grams) was born after a full-term pregnancy. She was followed during the first and second year of life and no developmental delay was detected.
2.3. Case 3
A 33-year-old pregnant woman conceived by ICSI was referred for a routine screening test. Her obstetric and medical histories were unremarkable. The result of semen analysis indicated low motility (30%) and high abnormal morphology (81%). The result of the routine first trimester screening at 11 weeks and 5 days gestation showed a significant increased NT (NT = 5). The normal range of NT for this age is 1-2.8 mm. Later examination revealed that collection of fluid was not confined to the neck but was enveloped throughout the fetus. The result of follow-up such as prenatal ultrasound findings, result of an amniocentesis (karyotype) and echocardiography were reported normal. She gave birth to a healthy baby boy (weight = 3500 grams) at 37 weeks of pregnancy by elective cesarean section at term.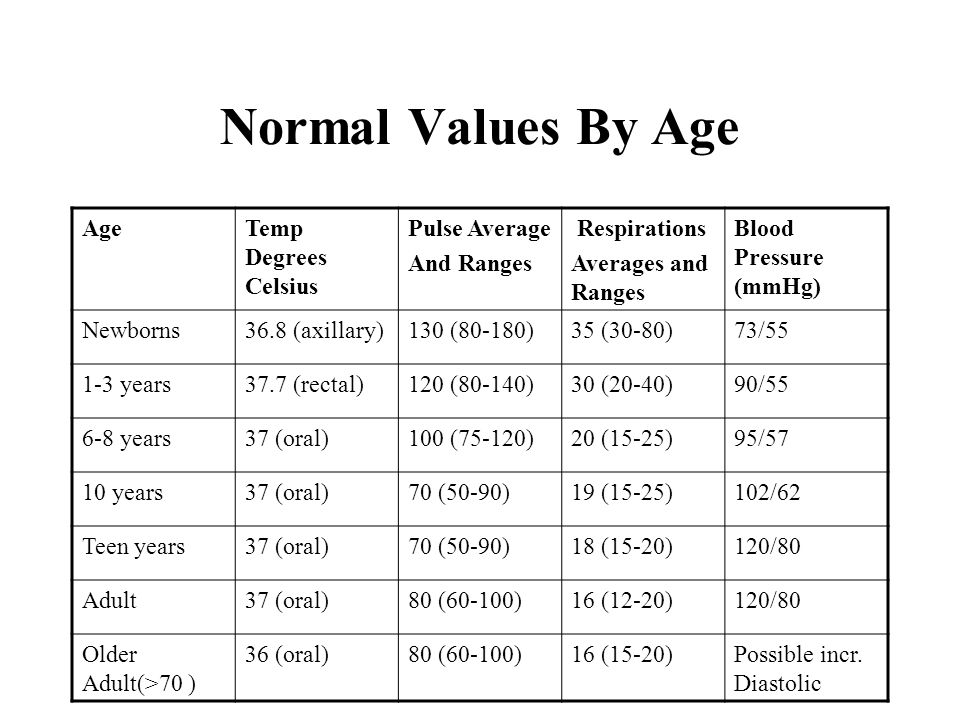 Follow-up after birth till 2 years has revealed no developmental delay.
Follow-up after birth till 2 years has revealed no developmental delay.
2.4. Case 4
A 26-year-old woman who was conceived by ICSI was referred for a routine screening test during her pregnancy. Her obstetric and medical history showed 8 years of primary infertility and polycystic ovaries. The result of semen analysis showed a low sperm concentration with a low total sperm count, low motility (30%) and high abnormal morphology (86%). First trimester measurement of NT at 12 weeks of gestation was 3.2 mm during the routine first trimester screening. The normal range of NT for this age is 1.1-3 mm. Although she refused to undergo amniocentesis (karyotype) and fetal echocardiography, triple test and follow-up prenatal ultrasound findings were normal. She gave birth at term to a healthy baby boy at 38 weeks (weight = 3500 grams). The 2-year follow-up after birth revealed no developmental delay.
2.5. Case 5
Following the routine screening test during pregnancy, a 31-year-old woman (conceived by ICSI) was referred to this institute. Her obstetric and medical history apart from 7 years primary infertility was unremarkable. The result of semen analysis revealed a low motility (35%) and a high abnormal morphology (92%). The result of routine first trimester screening at 12 weeks and 5 days of gestation showed an increased NT (3.3 mm) and generalized edema. The normal range of NT for this age is 1.5-3 mm. Although she refused to do the triple test and fetal echocardiography, follow-up prenatal ultrasound findings and amniocentesis (karyotype) were normal. She gave birth to a healthy term baby girl (weight = 3400 grams). Follow-up after birth revealed no developmental delay.
Her obstetric and medical history apart from 7 years primary infertility was unremarkable. The result of semen analysis revealed a low motility (35%) and a high abnormal morphology (92%). The result of routine first trimester screening at 12 weeks and 5 days of gestation showed an increased NT (3.3 mm) and generalized edema. The normal range of NT for this age is 1.5-3 mm. Although she refused to do the triple test and fetal echocardiography, follow-up prenatal ultrasound findings and amniocentesis (karyotype) were normal. She gave birth to a healthy term baby girl (weight = 3400 grams). Follow-up after birth revealed no developmental delay.
2.6. Case 6
A 30-year-old patient (conceived by ICSI) first presented to our institute at 12 weeks and 1 day of gestation and a twin pregnancy was detected. The second fetus was diagnosed with an increased NT (NT = 3.5 mm). The normal range of NT for this age is 1.2-3 mm. The couples’ history was significant for abnormal semen analysis. The result of semen analysis showed a sperm motility of 35% and an abnormal morphology of 80%. In this case, follow-up prenatal ultrasound findings and triple test were normal. Amniocentesis (karyotype) and echocardiography were cancelled because the patient refused to do so. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 2900 grams. The neonates were followed for the first and second year of their life and none of them had developmental delay.
The result of semen analysis showed a sperm motility of 35% and an abnormal morphology of 80%. In this case, follow-up prenatal ultrasound findings and triple test were normal. Amniocentesis (karyotype) and echocardiography were cancelled because the patient refused to do so. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 2900 grams. The neonates were followed for the first and second year of their life and none of them had developmental delay.
Although measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5% (10), it is regarded as a basic screening test with high sensitivity for identifying fetuses at risk for aneuploidy (1, 11, 12). However, NT is increased in 4.4% of euploid fetuses who are at risk for fetal anomalies and an adverse pregnancy outcome (12).
For this report first trimester ultrasound screening was performed for 703 women with a total number of 856 fetuses who were conceived by ICSI. First trimester measurement of NT was performed for 856 fetuses and 12 out of 856 fetuses with increased NT (NT ≥ 3) were taken for further investigation. In this report, six out of 12 cases who were chromosomally and anatomically normal fetuses with increased first trimester NT were described in detail. All these six fetuses had favorable prognosis despite the increased NT. We had no chromosomal report of the remained six fetuses because of reduction due to multiple pregnancies (4/12) and intrauterine fetal death (IUFD 2/12).
First trimester measurement of NT was performed for 856 fetuses and 12 out of 856 fetuses with increased NT (NT ≥ 3) were taken for further investigation. In this report, six out of 12 cases who were chromosomally and anatomically normal fetuses with increased first trimester NT were described in detail. All these six fetuses had favorable prognosis despite the increased NT. We had no chromosomal report of the remained six fetuses because of reduction due to multiple pregnancies (4/12) and intrauterine fetal death (IUFD 2/12).
The chance of delivering a healthy baby decreases with NT thickness from approximately 70% for an NT of 3.5-4.4 mm to about 15% for an NT of 6.5 mm or more (13). Based on previous studies, fetuses with increased NT (less than 4 mm), normal karyotype and normal findings in the 20-week scan, showed a markedly increased favorable outcome (14). After a normal detailed genetic sonography and fetal echocardiography, the incidence of adverse outcome and developmental delay were not significantly different from the normal population (9). According to studies performed by Souka et al. fetuses with increased NT thickness have a high risk of adverse or poor pregnancy outcome (1, 13). In this study, we only had one case of increased NT and intrauterine fetal death (IUFD) and one case of premature rupture of the membranes (PROM).
According to studies performed by Souka et al. fetuses with increased NT thickness have a high risk of adverse or poor pregnancy outcome (1, 13). In this study, we only had one case of increased NT and intrauterine fetal death (IUFD) and one case of premature rupture of the membranes (PROM).
This report is limited in number and should be further completed. In this series, semen analysis of all six cases were abnormal with a low motility of 30-35% and a high abnormal morphology of 80-92%. Although specific semen preparation technique in the case of impaired semen parameters in ART cycles is advisable, couples diagnosed with male-factor infertility should receive genetic counseling about the increased risk of congenital abnormalities before IVF-ICSI (15). This report provided six cases of increased NT with normal outcomes. It may help increase the confidence of couples who are reluctant to terminate the pregnancy. However, caution is necessary in cases of increased NT and parents should be offered a detailed fetal evaluation (genetic sonography) at the end of the first trimester and also at 18-22 weeks of gestation.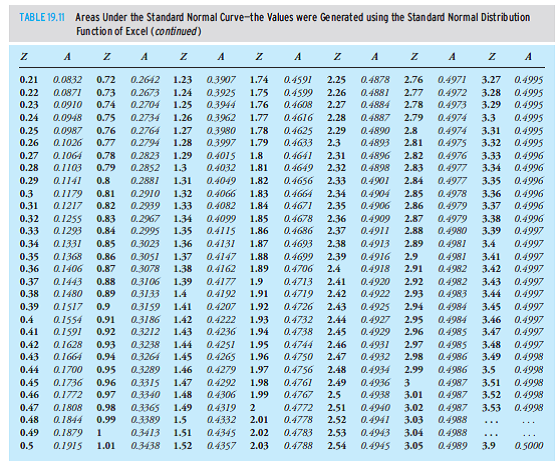 Triple test, amniocentesis, fetal echocardiography and follow-up after birth are necessary.
Triple test, amniocentesis, fetal echocardiography and follow-up after birth are necessary.
1. Souka AP, Krampl E, Bakalis S, Heath V, Nicolaides KH. Outcome of pregnancy in chromosomally normal fetuses with increased nuchal translucency in the first trimester. Ultrasound Obstet Gynecol. 2001;18(1):9–17. doi: 10.1046/j.1469-0705.2001.00454.x. [PubMed] [CrossRef] [Google Scholar]
2. Van Vugt JM, Tinnemans BW, Van Zalen-Sprock RM. Outcome and early childhood follow-up of chromosomally normal fetuses with increased nuchal translucency at 10-14 weeks' gestation. Ultrasound Obstet Gynecol. 1998;11(6):407–9. doi: 10.1046/j.1469-0705.1998.11060407.x. [PubMed] [CrossRef] [Google Scholar]
3. Brady AF, Pandya PP, Yuksel B, Greenough A, Patton MA, Nicolaides KH. Outcome of chromosomally normal livebirths with increased fetal nuchal translucency at 10-14 weeks' gestation. J Med Genet. 1998;35(3):222–4. [PMC free article] [PubMed] [Google Scholar]
4. Adekunle O, Gopee A, el-Sayed M, Thilaganathan B. Increased first trimester nuchal translucency: pregnancy and infant outcomes after routine screening for Down's syndrome in an unselected antenatal population. Br J Radiol. 1999;72(857):457–60. doi: 10.1259/bjr.72.857.10505009. [PubMed] [CrossRef] [Google Scholar]
Increased first trimester nuchal translucency: pregnancy and infant outcomes after routine screening for Down's syndrome in an unselected antenatal population. Br J Radiol. 1999;72(857):457–60. doi: 10.1259/bjr.72.857.10505009. [PubMed] [CrossRef] [Google Scholar]
5. Maymon R, Jauniaux E, Cohen O, Dreazen E, Weinraub Z, Herman A. Pregnancy outcome and infant follow-up of fetuses with abnormally increased first trimester nuchal translucency. Hum Reprod. 2000;15(9):2023–7. [PubMed] [Google Scholar]
6. Hiippala A, Eronen M, Taipale P, Salonen R, Hiilesmaa V. Fetal nuchal translucency and normal chromosomes: a long-term follow-up study. Ultrasound Obstet Gynecol. 2001;18(1):18–22. doi: 10.1046/j.1469-0705.2001.00481.x. [PubMed] [CrossRef] [Google Scholar]
7. Senat MV, De Keersmaecker B, Audibert F, Montcharmont G, Frydman R, Ville Y. Pregnancy outcome in fetuses with increased nuchal translucency and normal karyotype. Prenat Diagn. 2002;22(5):345–9. doi: 10.1002/pd.321. [PubMed] [CrossRef] [Google Scholar]
8. Cheng CC, Bahado-Singh RO, Chen SC, Tsai MS. Pregnancy outcomes with increased nuchal translucency after routine Down syndrome screening. Int J Gynaecol Obstet. 2004;84(1):5–9. [PubMed] [Google Scholar]
Cheng CC, Bahado-Singh RO, Chen SC, Tsai MS. Pregnancy outcomes with increased nuchal translucency after routine Down syndrome screening. Int J Gynaecol Obstet. 2004;84(1):5–9. [PubMed] [Google Scholar]
9. Senat MV, Bussieres L, Couderc S, Roume J, Rozenberg P, Bouyer J, et al. Long-term outcome of children born after a first-trimester measurement of nuchal translucency at the 99th percentile or greater with normal karyotype: a prospective study. Am J Obstet Gynecol. 2007;196(1):53 e1–6. doi: 10.1016/j.ajog.2006.08.026. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Nicolaides KH, Spencer K, Avgidou K, Faiola S, Falcon O. Multicenter study of first-trimester screening for trisomy 21 in 75 821 pregnancies: results and estimation of the potential impact of individual risk-orientated two-stage first-trimester screening. Ultrasound Obstet Gynecol. 2005;25(3):221–6. doi: 10.1002/uog.1860. [PubMed] [CrossRef] [Google Scholar]
11. Pandya PP, Kondylios A, Hilbert L, Snijders RJ, Nicolaides KH. Chromosomal defects and outcome in 1015 fetuses with increased nuchal translucency. Ultrasound Obstet Gynecol. 1995;5(1):15–9. doi: 10.1046/j.1469-0705.1995.05010015.x. [PubMed] [CrossRef] [Google Scholar]
Chromosomal defects and outcome in 1015 fetuses with increased nuchal translucency. Ultrasound Obstet Gynecol. 1995;5(1):15–9. doi: 10.1046/j.1469-0705.1995.05010015.x. [PubMed] [CrossRef] [Google Scholar]
12. Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352(9125):343–6. [PubMed] [Google Scholar]
13. Souka AP, Von Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH. Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol. 2005;192(4):1005–21. doi: 10.1016/j.ajog.2004.12.093. [PubMed] [CrossRef] [Google Scholar]
14. Bilardo CM, Muller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30(1):11–8. doi: 10.1002/uog. 4044. [PubMed] [CrossRef] [Google Scholar]
4044. [PubMed] [CrossRef] [Google Scholar]
15. Allen VM, Wilson RD, Cheung A, Genetics Committee of the Society of O, Gynaecologists of C, Reproductive Endocrinology Infertility Committee of the Society of O, et al. Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can. 2006;28(3):220–50. [PubMed] [Google Scholar]
Normal reference range of fetal nuchal translucency thickness in pregnant women in the first trimester, one center study
J Res Med Sci. 2015 Oct; 20(10): 969–973.
doi: 10.4103/1735-1995.172786
,,,1 and 2
Author information Article notes Copyright and License information Disclaimer
Background:
Considering that establishment of reference value of nuchal translucency (NT)-related to the crown rump length (CRL) during the first trimester will be helpful for determining an appropriate cutoff level for screening of increased NT thickness-related abnormalities, we determined the NT thickness and investigated its relation with different chromosomal and nonchromosomal abnormalities among a large sample size of pregnant Iranian women.
Materials and Methods:
In this analytic cross-sectional study, pregnant women who were in their first trimester were enrolled at their antenatal visit. Using an abdominal ultrasonography, the fetal NT thickness of the studied population was measured. Those with increased NT thickness were determined. The reference value of NT thickness (5th, 25th, 50th, 75th, and 95th percentiles) within each 5-mm range of CRL and during the 11th, 12th, and 13th gestational weeks were determined. The presences of the different chromosomal and nonchromosomal abnormalities were compared in women with different percentiles of NT thickness who underwent amniocentesis and those who did not.
Results:
1,614 pregnant women were evaluated. The mean NT thickness was 1.30 ± 0.54 mm. Increased NT thickness >2 mm and >95th percentile according to their gestational age (GA) was detected in 89 (5.5%) and 58 (3.6%) pregnant women. The reference 95th percentile value range for NT was 1. 8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
Conclusion:
The obtained reference range in our studied population was different from that reported for other ethnic groups and it is suggested that using this values are more favorable for screening of chromosomal abnormalities during the first trimester of pregnancy than the recommended single cutoff value.
Keywords: Crown rump length (CRL), nuchal translucency (NL), reference values
Nuchal translucency (NT) is the normal fluid-filled subcutaneous space between the back of the fetal skin and the overlying skin.[1] NT is visible and can be measured by ultrasonographic imaging between 11 weeks and 14 weeks gestation.[2] Increased NT is associated with different fetal chromosomal and nonchromosomal abnormalities. There is growing evidence that increased NT thickness during the first trimester of pregnancy in a chromosomally normal fetus is associated with numerous fetal structural abnormalities, genetic syndromes, heart defects, and poor perinatal outcomes such as miscarriage and intrauterine death. [3,4,5]
[3,4,5]
The first definition for increased NT was a measure >95th percentile for a given crown rump length (CRL) and a NT value of 2.5-3 mm, which was reported as a normal range for the marker. Recently, some studies indicated that NT >99th percentile or NT value that exceeds of 3.5 mm are associated with the most common adverse outcomes.[6,7]
The utility of NT as a sensitive and noninvasive ultrasonographic marker for screening and detection of aneuploidies and major structural anomalies in modern obstetrical practice has been demonstrated recently. Its use as a new screening method for the mentioned purposes has been developed in many developed countries.[8,9,10]
Since the introduction of NT thickness, several studies worldwide have determined the normal range of NT in different populations. The results were different regarding the normative value of NT. One of the explanations for the reported great variety of NT thickness range is ethnic variation. [11,12,13,14,15] However, there are still controversies regarding the role of ethnicity on the value of NT. Some reported a significant role of ethnicity in this regard, whereas others did not support the association.[16,17] However, recently the establishment of reference value for NT in different populations was performed. It is suggested that ethnic and region-specific reference value of NT could have a significant impact on its screening efficacy and using a single cutoff for fetal NT could not be an appropriate tool in this field.[18]
[11,12,13,14,15] However, there are still controversies regarding the role of ethnicity on the value of NT. Some reported a significant role of ethnicity in this regard, whereas others did not support the association.[16,17] However, recently the establishment of reference value for NT in different populations was performed. It is suggested that ethnic and region-specific reference value of NT could have a significant impact on its screening efficacy and using a single cutoff for fetal NT could not be an appropriate tool in this field.[18]
So considering that establishment of reference value of NT related to the CRL during the first trimester will be helpful for determining an appropriate cutoff level for screening of increased NT thickness-related abnormalities and the presence of few reports in this field among the Iranian population, in this study we determined the reference values of NT thickness among Isfahani pregnant women to evaluate the role of ethnicity on the normative value of NT as well as the association of increased NT thickness with chromosomal and nonchromosomal abnormalities during the first trimester.
In this analytic cross-sectional study, pregnant women referred to a private radiology center for ultrsonographic assessment during the antenatal visit in their first trimester were enrolled. The study was performed from January 2013 to December 2013 in Isfahan, Isfahan Province, Iran.
The protocol of the study was approved by the Regional Ethics Committee of Isfahan University of Medical Sciences.
Pregnant women with gestational age (GA) of 11-13 weeks and 6 days and/or CRL 45-84 mm were included.
The pregnant women were selected by the consecutive method. Those who did not agree to have the ultrasonography performed, with multiple pregnancies, fetal malformation, and those with inappropriate cooperation were excluded. Written informed consent was obtained from all the selected participants. The selected pregnant women underwent abdominal ultrasonography. The sonography was performed by an expert radiologist. The fetal NT thickness of the studied population was measured.
Those with NT thickness of 2 mm were considered as women with increased NT thickness.[19]
The mean of CRL and GA were compared in women with and without increased NT thickness.
The reference value of NT thickness (5th, 25th, 50th, 75th, and 95th percentiles) within each 5-mm range of CRL and during the 11th, 12th, and 13th gestational weeks were determined.
Women with NT thickness of >95th percentile were determined. The women were followed up and fetal outcomes were evaluated by the neonatologists at birth. The presence of different chromosomal abnormalities as well as nonchromosomal abnormalities including cardiac malformation, genitourinary or renal abnormalities, diaphragmatic hernia, spontaneous miscarriage, and intrauterine fetal death (IUFD) were compared in women with different percentiles of NT thickness who underwent amniocentesis and those who did not.
Ultrasonographic measurements
The ultrasonographic measurements were performed in pregnant women in a supine position.
Fetal CRL and NT thickness measurements were performed by transabdominal ultrsonography using a multi fz: 3.5 MHz tranduser (GE Volusun 730). The measurement was performed based on the criteria recommended by the Fetal Medicine Foundation (FMF).[20] According to the criteria, the fetus should be in a neutral position, with the head aligned with the spine in a way that fetus occupied at least 75% of the image. NT was defined as the black area between the inner skin outlines echo and the outer border of the soft tissue overlying the cervical spine.
The maximal thickness of the black area was measured with caliper placed on the inner borders of the NT space, perpendicular to the long axis of the fetus when a sagittal section with a neutral position of the fetus was obtained. The measurements were recorded to the nearest 0.1-mm interval. At least three NK measurements were taken and the largest was recorded.
CRL was measured at the same time and recorded.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 21 (SPSS Inc., Chicago, IL, USA). Using regression equation, the expected 5th, 25th, 50th, 75th, and 5th percentile values of NT thickness according to the CRL categories of CRL (5-mm interval) and GA (11th, 12th, and 13th weeks) were obtained. Quantitive and qualitative values were compared using the t-test and chi-square test, respectively. P value of <0.05 was considered to be statistically significant.
During this study, 1,614 pregnant women were evaluated. Among the studied pregnant women 382 (23.7%), 871 (54.0%), and 361 (22.4) were in the 11th, 12th, and 13th gestational week. The mean of GA, CRL, and NT thickness in the studied population were 12.46 ± 0.62 weeks, 59.35 ± 8.35 mm, and 1.30 ± 0.54 mm, respectively. Pearson correlation test indicated that there was a significant positive correlation between NT and CRL (r = 0.238, P < 0.001), NT and GA (r = 0.24, P < 0.001 and GA) and CRL (r = 0.8, P < 0.001).
Pearson correlation test indicated that there was a significant positive correlation between NT and CRL (r = 0.238, P < 0.001), NT and GA (r = 0.24, P < 0.001 and GA) and CRL (r = 0.8, P < 0.001).
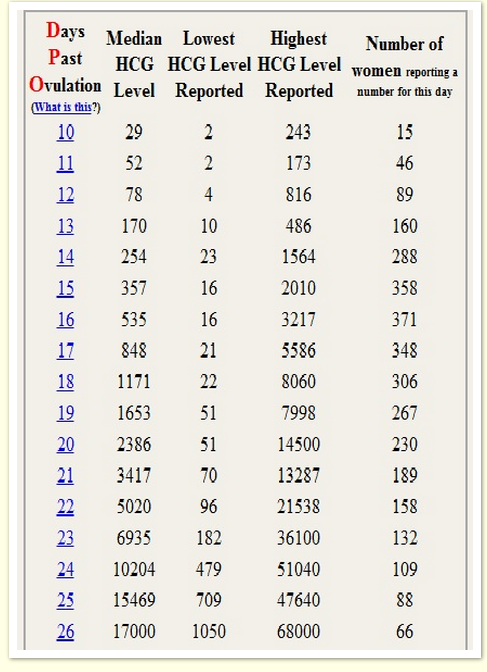
Increased NT thickness (NT >2 mm) was detected in 89 (5.5%) pregnant women. The mean of CRL and GA in pregnant women with normal and increased NT thickness are presented in .
Table 1
Mean ± SD of CRL and GA in pregnant women with normal and increased NT thickness
Open in a separate window
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness to CRL and GA are listed in Tables and . Using the obtained reference value of NT, 58 (3.6%) pregnant women were determined as those with NT thickness >95th percentile according to their GA. During follow-up, 31/58 (53.4%) underwent amniocentesis. Distribution of chromosomal and nonchromosomal abnormalities in pregnant women with NT thickness >95th percentile according to their GA in total and among those with and without amniocentesis are presented in . Frequency of chromosomal abnormalities were significantly higher in those pregnant women with increased NT thickness who underwent the amniocentesis procedure (P = 0.001). The frequency of different nonchromosomal abnormalities were not significantly different between the two studied groups (P > 0.05).
Frequency of chromosomal abnormalities were significantly higher in those pregnant women with increased NT thickness who underwent the amniocentesis procedure (P = 0.001). The frequency of different nonchromosomal abnormalities were not significantly different between the two studied groups (P > 0.05).
Table 2
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness (mm) to CRL
Open in a separate window
Table 3
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness (mm) to gestational age (GA)
Open in a separate window
Table 4
Distribution of chromosomal and nonchromosomal abnormalities in pregnant women with NT thickness >95th percentile according to their GA in total and among those with and without amniocentesis
Open in a separate window
In this study, we determined the reference values of NT thickness among pregnant Isfahani women to evaluate the role of ethnicity on the normative value of NT as well as the association of increased NT thickness with chromosomal and nonchromosomal abnormalities during the first trimester. The results indicated that the reference 95th percentile value range for NT was 1.8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
The results indicated that the reference 95th percentile value range for NT was 1.8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
Several reports from different parts of the worlds and Iran have demonstrated the utility of NK measurement for screening different chromosomal and nonchromosomal abnormalities.[20,21,22,23]
Most of the studies have used the recommended definition for NT thickness by the FMF (i.e., 2.5-3 mm),[6] whereas recent studies reported that using NT thickness as a continuous variable was more appropriate than using a single cutoff value for the fetal NT and consequently, the outcomes of its increased values and screening programs.[18] So, establishment of reference values of NT have been developed in different regions and ethnic groups worldwide.
Though there were studies in Iran, which investigated the association between increased NT value and Down syndrome[22] and adverse pregnancy outcome including miscarriage, fetal loss, and fetal abnormalities,[23] there was not any study, which reported the normative value of NT thickness for the Iranian population.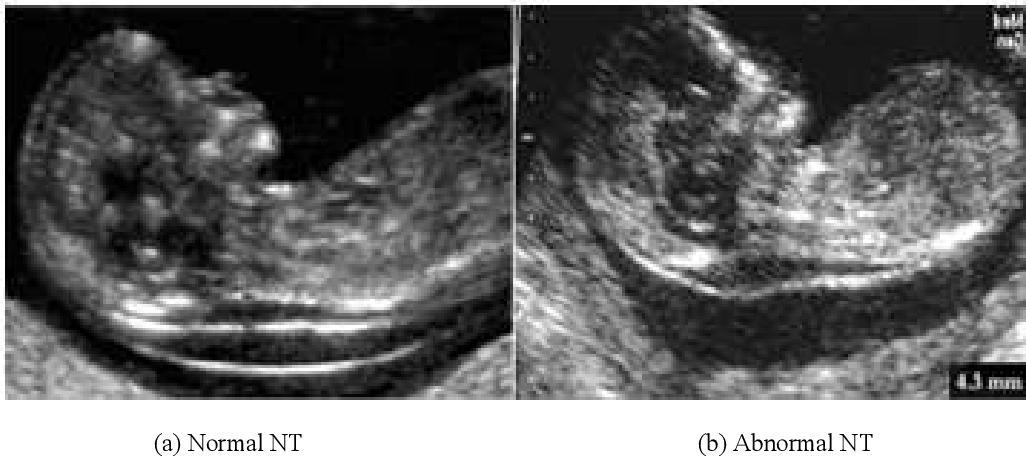 So, this study was designed to determine the ethnic specific reference value of NT thickness for pregnant Iranian women. Our results indicated that the median NT thicknesses for a CRL between 45 mm and 80 mm ranged from 1.00 to 1.65 mm, and the 95th percentiles ranged from 1.8 to 2.35 mm. The median NT thickness for GA were 1.0 mm, 1.2 mm, and 1.4 mm for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively, and the 95th percentiles of NT thickness were 1.8, 1.9, and 2.2 for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively.
So, this study was designed to determine the ethnic specific reference value of NT thickness for pregnant Iranian women. Our results indicated that the median NT thicknesses for a CRL between 45 mm and 80 mm ranged from 1.00 to 1.65 mm, and the 95th percentiles ranged from 1.8 to 2.35 mm. The median NT thickness for GA were 1.0 mm, 1.2 mm, and 1.4 mm for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively, and the 95th percentiles of NT thickness were 1.8, 1.9, and 2.2 for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively.
The distribution of the NT thickness for CRL has been reported in many studies. The median NT thicknesses has been reported to be 1.2-1.9 mm, 1.22-2.10 mm, and 1.19-1.73 mm for a CRL between 45 mm and 80 mm in Japan, Korea, and Brazil, respectively.[11,12,13] Our reported median value was lower than the other reports.
The 95th NT thickness percentiles have been reported to be 2.1-3.2 mm, 2.14-2.3 mm, 1.57-2. 10 mm, 1.00-2.90 mm, and 1.84-2.35 mm for a CRL between 45 mm and 80 mm in Japan, Korea, Brazil, Thailand, and China, respectively.[11,12,13,14,15] Our results were similar to the reported reference value range of Brazil.[13] Although there was no report from the Eastern Mediterranean region in this field, the values were not similar to the values reported from the Asian countries.
10 mm, 1.00-2.90 mm, and 1.84-2.35 mm for a CRL between 45 mm and 80 mm in Japan, Korea, Brazil, Thailand, and China, respectively.[11,12,13,14,15] Our results were similar to the reported reference value range of Brazil.[13] Although there was no report from the Eastern Mediterranean region in this field, the values were not similar to the values reported from the Asian countries.
Reported variations in the index measurements in the different studies might have been due to factors such as radiologist experience, quality of the ultrasound, method of measurement, and an inappropriate fetal and nuchal cord position. In addition, as mentioned by Kor-anantaku et al. in Thailand some investigators have considered the average of two or three measurements of NT thickness, whereas others considered the largest measurement.[14]
There are controversial reports regarding the impact of ethnicity on NT thickness values and its utility for screening. Thilaganathan et al.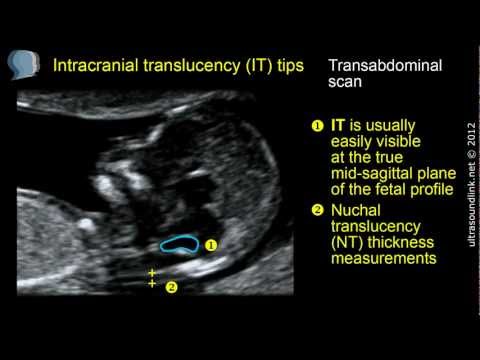 have investigated the possible role of ethnicity on NT screening and concluded that the reported differences could not have a significant impact in this regard.[24] Many other studies have also showed that ethnic differences in NT measurements are not clinically significant, especially when it used for screening of Down syndrome.[17,24,25] However, it seems that using ethnic-specific reference values of NT thickness could help us in the first trimester screening programs mainly for chromosomal abnormality, especially when they are integrated with other ultrasonographic and biochemical measurements.
have investigated the possible role of ethnicity on NT screening and concluded that the reported differences could not have a significant impact in this regard.[24] Many other studies have also showed that ethnic differences in NT measurements are not clinically significant, especially when it used for screening of Down syndrome.[17,24,25] However, it seems that using ethnic-specific reference values of NT thickness could help us in the first trimester screening programs mainly for chromosomal abnormality, especially when they are integrated with other ultrasonographic and biochemical measurements.
In this study using the single cutoff value of 2 mm, 5.5% of the studied pregnant women were considered to have high-risk pregnancy and after using our obtained reference value the rate decreased to 3.6%. Thus, it seems that using normative values of NT thickness is more useful for the first trimester screening and it could optimize the screening results by reducing false positive cases.
In addition, there was significant association between performing the amniocentesis procedure and detection of chromosomal abnormalities among women with increased NT thickness.
The advantage of the current study was a larger sample size of enrolled pregnant women.
The limitation of the current study was that we did not determine the sex-specific reference value of 95th percentiles of NT and its association with both chromosomal and nonchromosomal abnormalities. We followed up only pregnant women with increased NT thickness and did not determine the frequency of the mentioned abnormalities in pregnant women with normal NT. It was due to the reason that follow-up of that large a sample size was not assessable in the framework of the current study. In addition, we enrolled the patients who were referred to a single referral radiologic center, which could not be a representative sample of the whole population. It is suggested that the large sample size of the studied population could partially alleviate the abovementioned limitation.
Further, the planning of further studies that also determine the 99th percentile values of NT thickness is recommended because recent studies demonstrated that chromosomal and nonchromosomal abnormalities are mainly associated with the 99th percentile value of NT thickness.[7]
The results of our study indicated the reference value of NT thickness in a large sample size of Isfahani pregnant women. The obtained reference range in our studied population was different from that reported for other ethnic groups and it is suggested that using this values are more favorable for screening of chromosomal abnormalities during the first trimester of pregnancy than the recommended single cutoff value. The relation between increased NT thicknesses with chromosomal abnormalities also confirms its utility. The results of the current study could be used as baseline information for other follow-up studies and designing first trimester screening programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
All authors contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
The study was supported by Isfahan University of Medical Sciences (research project number; 393486).
1. Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K. Fetal nuchal translucency: Ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ. 1992;304:867–9. [PMC free article] [PubMed] [Google Scholar]
2. Szabó J, Gellén J. Nuchal fluid accumulation in trisomy-21 detected by vaginosonography in first trimester. Lancet. 1990;336:1133. [PubMed] [Google Scholar]
3. Vogel M, Sharland GK, McElhinney DB, Zidere V, Simpson JM, Miller OI, et al. Prevalence of increased nuchal translucency in fetuses with congenital cardiac disease and a normal karyotype. Cardiol Young. 2009;19:441–5. [PubMed] [Google Scholar]
4. Bilardo CM, Müller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: Time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30:11–8. [PubMed] [Google Scholar]
Bilardo CM, Müller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: Time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30:11–8. [PubMed] [Google Scholar]
5. Saldanha FA, Brizot Mde L, Moraes EA, Lopes LM, Zugaib M. Increased fetal nuchal translucency thickness and normal karyotype: Prenatal and postnatal follow-up. Rev Assoc Med Bras. 2009;55:575–80. [PubMed] [Google Scholar]
6. Salman Guraya S. The associations of nuchal translucency and fetal abnormalities; significance and implications. J Clin Diagn Res. 2013;7:936–41. [PMC free article] [PubMed] [Google Scholar]
7. Souka AP, Von Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH. Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol. 2005;192:1005–21. [PubMed] [Google Scholar]
8. Stefanovic V, Äyräs O, Eronen M, Paavonen1 J, Tikkanen M. Clinical utility of nuchal translucency screening. Res Rep Neonatol. 2014;4:169–76. [Google Scholar]
[Google Scholar]
9. Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK Multicentre Project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352:343–6. [PubMed] [Google Scholar]
10. Miron P, Côté YP, Lambert J. Nuchal translucency thresholds in prenatal screening for down syndrome and trisomy 18. J Obstet Gynaecol Can. 2009;31:227–35. [PubMed] [Google Scholar]
11. Hasegawa J, Nakamura M, Hamada S, Matsuoka R, Ichizuka K, Sekizawa A, et al. Distribution of nuchal translucency thickness in Japanese fetuses. J Obstet Gynaecol Res. 2013;39:766–9. [PubMed] [Google Scholar]
12. Chung JH, Yang JH, Song MJ, Cho JY, Lee YH, Park SY, et al. The distribution of fetal nuchal translucency thickness in normal Korean fetuses. J Korean Med Sci. 2004;19:32–6. [PMC free article] [PubMed] [Google Scholar]
13. Araujo Júnior E, Pires CR, Martins WP, Nardozza LM, Filho SM. Reference values of nuchal translucency thickness in a Brazilian population sample: Experience from a single center. J Perinat Med. 2014;42:255–9. [PubMed] [Google Scholar]
Reference values of nuchal translucency thickness in a Brazilian population sample: Experience from a single center. J Perinat Med. 2014;42:255–9. [PubMed] [Google Scholar]
14. Kor-Anantakul O, Suntharasaj T, Suwanrath C, Chanprapaph P, Sirichotiyakul S, Ratanasiri T, et al. Distribution of normal nuchal translucency thickness: A multicenter study in Thailand. Gynecol Obstet Invest. 2011;71:124–8. [PubMed] [Google Scholar]
15. Sun Q, Xu J, Hu SQ, Chen M, Ma RM, Lau TK, et al. Distribution and normal reference range of fetal nuchal translucency thickness in Kunming pregnant women in the first trimester. Zhonghua Fu Chan Ke Za Zhi. 2012;47:514–7. [PubMed] [Google Scholar]
16. Huang T, Wang F, Boucher K, O’Donnell A, Rashid S, Summers AM. Racial differences in first trimester nuchal translucency. Prenat Diagn. 2007;27:1174–6. [PubMed] [Google Scholar]
17. Chen M, Lam YH, Tang MH, Lee CP, Sin SY, Tang R, et al. The effect of ethnic origin on nuchal translucency at 10-14 weeks of gestation. Prenat Diagn. 2002;22:576–8. [PubMed] [Google Scholar]
Prenat Diagn. 2002;22:576–8. [PubMed] [Google Scholar]
18. Taipale P, Hiilesmaa V, Salonen R, Ylöstalo P. Increased nuchal translacency as a marker for fetal chromosomal defects. N Engl J Med. 1997;337:1654–8. [PubMed] [Google Scholar]
19. Kim SM, Jun JK. Simplified protocol of nuchal translucency measurement: Is it still effective? Obstet Gynecol Sci. 2013;56:307–11. [PMC free article] [PubMed] [Google Scholar]
20. Kagan KO, Avgidou K, Molina FS, Gajewska K, Nicolaides KH. Relation between increased fetal nuchal translucency thickness and chromosomal defects. Obstet Gynecol. 2006;107:6–10. [PubMed] [Google Scholar]
21. Barati M, Zargar M, Masihi S, Taherpour S. Evaluation of nuchal translucency measurement in first trimester pregnancy. Int J Fertil Steril. 2011;5:35–8. [PMC free article] [PubMed] [Google Scholar]
22. Elahifar MA, Hasanzadeh M, Dahmardeh H, Elahifar A. The relationship between thickness of nuchal translucency and Down syndrome in the first trimester of pregnancy. Zahedan J Res Med Sci. 2012;14:26–8. [Google Scholar]
Zahedan J Res Med Sci. 2012;14:26–8. [Google Scholar]
23. Tahmasebpour A, Rafiee NB, Ghaffari S, Jamal A. Increased nuchal translucency and pregnancy outcome. Iran J Public Health. 2012;41:92–7. [PMC free article] [PubMed] [Google Scholar]
24. Thilaganathan B, Khare M, Williams B, Wathen NC. Influence of ethnic origin on nuchal translucency screening for Down's syndrome. Ultrasound Obstet Gynecol. 1998;12:112–4. [PubMed] [Google Scholar]
25. Hsu JJ, Hsieh CC, Chiang CH, Lo LM, Hsieh TT. Preliminary normal reference values of nuchal translucency thickness in Taiwanese fetuses at 11-14 weeks of gestation. Chang Gung Med J. 2003;26:12–9. [PubMed] [Google Scholar]
Importance of ultrasound at 12 weeks of gestation
Ultrasound at 12 weeks of gestation
Nowadays, monitoring the course of pregnancy is difficult to imagine without ultrasound. This method is safe, painless and universal in terms of the fact that the doctor has the opportunity to evaluate various parameters of fetal development, and the functional features of the placenta, uterus, and umbilical cord.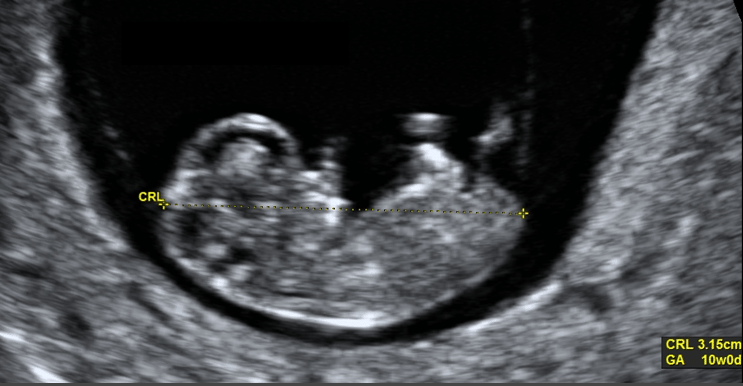
According to the norms established by the Ministry of Health of the Russian Federation, the first screening ultrasound is done to women at the 12th week of pregnancy.
Why is ultrasound done at 12 weeks pregnant?
At the end of the first trimester, namely at 12 weeks (perhaps a little earlier or a little later), every pregnant woman should undergo an ultrasound screening. This procedure is carried out in order to:
- Confirm pregnancy (after all, sometimes tests or blood tests for hCG can give ambiguous results).
- Confirm the correct position and attachment of the gestational sac with the embryo. Pregnancy must be uterine. The ectopic location of the fetal egg is a serious pathology that requires immediate medical intervention.
- Identification of pathologies of the female reproductive system, which may adversely affect the process of bearing a fetus. For example, at the first ultrasound, the length of the cervix is estimated.
 If it has an insufficient value (1-1.5 mm), this indicates the presence of isthmic-cervical insufficiency, which can lead to miscarriage.
If it has an insufficient value (1-1.5 mm), this indicates the presence of isthmic-cervical insufficiency, which can lead to miscarriage. - Specify the gestational age, that is, the gestational age.
- Assess the level of development of the fetus and the preliminary result of the process of laying its main internal organs.
- Assess how correctly and fully formed the fetal heart muscle.
- Detect primary markers of chromosomal or genetic disorders. Not all such pathologies can be detected at a period of 12 weeks, but, for example, it is possible to suspect Down syndrome in an unborn child after the first screening.
Ultrasound at the 12th week of pregnancy (screening of the research norms will be described below) is also the first opportunity for a future mother to see her baby, which, of course, causes a lot of positive, useful emotions.
How to prepare for screening?
Ultrasound during pregnancy is a procedure that does not require special preparation. Women are only recommended 2-3 days before the study to refrain from food that provokes excessive gas formation in the intestines. Otherwise, you just need to come to the doctor’s appointment calm and in a good mood.
Women are only recommended 2-3 days before the study to refrain from food that provokes excessive gas formation in the intestines. Otherwise, you just need to come to the doctor’s appointment calm and in a good mood.
How is the first ultrasound at 12 weeks?
There are two options for doing an ultrasound at 12 weeks of gestation:
- Transvaginally - using a special vaginal probe inserted into the pregnant woman's vagina.
- Transabdominal - examination is carried out through the skin of the abdomen of a pregnant woman using a special gel.
What does ultrasound show at 12 weeks pregnant?
An ultrasound at week 12 shows the size of the fetus, the location of the fetal egg, the place of attachment of the chorion (future placenta), the level of the fetal heartbeat, and the amount of amniotic fluid.
If an ultrasound scan at 12 weeks of gestation shows that the fetus is developing abnormally, the attending physician should assess how critical this deviation is and how it may affect the health of the unborn child. Perhaps a slight discrepancy in the size of the fetus is due to its anatomical or physiological features and it is impossible to speak of the presence of a gross pathology. To clarify the diagnosis, an additional ultrasound is usually prescribed a few weeks after the first one.
Perhaps a slight discrepancy in the size of the fetus is due to its anatomical or physiological features and it is impossible to speak of the presence of a gross pathology. To clarify the diagnosis, an additional ultrasound is usually prescribed a few weeks after the first one.
If ultrasound, as well as the results of other tests, indicate that the fetus has a certain chromosomal disorder, then the question of terminating the pregnancy may be raised. The decision in this case should be made by the woman, and the doctor is obliged to give her his recommendations.
Child gender
The gender of the child is a criterion that is not included in the mandatory protocol for ultrasound examination. Gender does not affect the normal development of the fetus, but almost every expectant mother wants to know as soon as possible who will be born to her, a daughter or a son.
At 12 weeks it is difficult to determine the sex of the unborn child. Some ultrasound specialists, by measuring the angle of the genital tubercle, may suggest whether it will be a boy or a girl. The error rate is 50%, so you need to be patient and wait at least until 16-20 weeks, when the sex can be seen more clearly.
Some ultrasound specialists, by measuring the angle of the genital tubercle, may suggest whether it will be a boy or a girl. The error rate is 50%, so you need to be patient and wait at least until 16-20 weeks, when the sex can be seen more clearly.
Heart rate limits
The study of the heart of the unborn child is one of the main aspects of ultrasound at 12 weeks of pregnancy, the norms for it are as follows:
- From 0 to 5 weeks, when the embryo is just born and its size is from 2 to 15 mm, the heart rate can be 80-130 bpm.
- From 5 to 8 weeks, the fetal heart may beat at a rate of 120-170 bpm.
- By week 12, heart rate may be 170-190 bpm.
KTR
KTR, that is, the size of the fetus from the coccyx to the crown, is an important criterion for assessing development in the first trimester of pregnancy. For a period of 12 weeks, it can be 42-59mm. This parameter is included in the mandatory ultrasound protocol of the first trimester.
Child head BPR norms
After ultrasound of 12 weeks of pregnancy , the decoding of its results and their comparison with the norm are carried out immediately. First of all, the doctor evaluates the biparietal size of the fetal head. At 12 weeks, it should be approximately 21 mm.
If BDP turns out to be more than normal, but at the same time all other fetal parameters (KTR, femur length, and so on) exceed it, we can say that this is just a large fetus.
If BDP exceeds the norm, and all other indicators fit into it, fetal hydrocephalus is most often suspected.
Nose length standards
When deciphering an ultrasound at 12 weeks of gestation, such an indicator as the length of the fetal nose (the length of the nasal bone) is necessarily taken into account. More precisely, first of all, the doctor evaluates whether the nasal bone is visualized in principle. Its size (length) for a period of 12 weeks should be approximately 3 mm.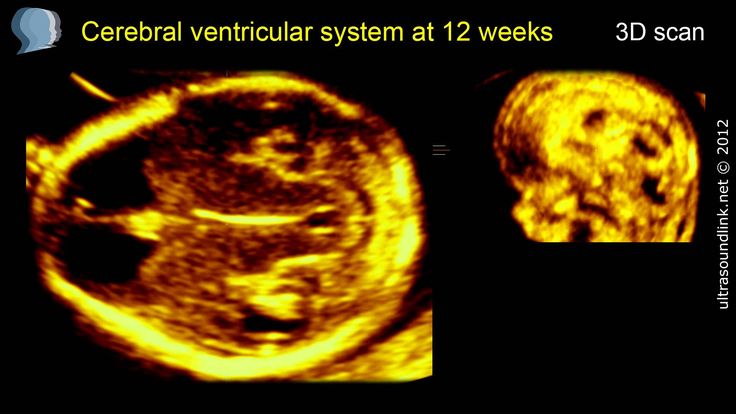
In cases where the nasal bone of the fetus is not visualized, there is a risk that the child will be born with Down syndrome. For a more accurate determination of this chromosomal pathology, another indicator is analyzed - the thickness of the collar space (NTP). This is a space of accumulation of fluid between the neck of the fetus and the upper shell of its skin. If TVP is greater than normal, and the nasal bone is not visualized, the likelihood of the fetus having chromosomal abnormalities is assessed as high.
Is it necessary to have an ultrasound at 12 weeks?
If a woman wants to endure and give birth to a healthy child, reduce the risk of miscarriage or pregnancy fading, then she definitely needs to undergo an ultrasound scan in the first trimester of pregnancy. No hard deadlines have been set. Ultrasound can be done both at 12 and, for example, at 11 or 13 weeks (but no later than 14 weeks). It all depends on the course of pregnancy, the woman's well-being, the results of a blood test. The best advice on when to have an ultrasound can only be given by your doctor.
The best advice on when to have an ultrasound can only be given by your doctor.
how the fetus develops, the size of the abdomen, what the baby looks like, how it feels
Published: 06/02/2017
Reading time: 6 min.
Number of reads: 18336
The 12th week of pregnancy according to the embryonic method of counting is equal to the 14th obstetric. This is a significant date for you and your baby - the end of the first trimester is approaching. It is at this time, from a medical point of view, the embryo (embryo) becomes a fetus. This means that the rudiments of all organs are formed, and their growth and development becomes the main task. The baby has grown significantly in the last three weeks. Its size has almost doubled.
What happens to the baby
The fetus at the 12th week of pregnancy weighs about 16 grams, and its length is 6-7.5 centimeters. The baby can already respond to mom's touch on the tummy. Mom does not feel it yet, but knowing this fact makes her touch her stomach more often at the 12th week and communicate with the baby. The baby's fingers and toes have separated at 12 weeks, and the nails continue to grow. The first hairs appear on the body. The digestive system is actively developing. The small intestine is already capable of contracting and pushing water. From it, the fetus receives nutrients at 12 weeks. The baby actively moves: unbends and bends the legs and arms, unclenches and compresses the fists. Due to the small size, the expectant mother does not yet feel this.
The baby's fingers and toes have separated at 12 weeks, and the nails continue to grow. The first hairs appear on the body. The digestive system is actively developing. The small intestine is already capable of contracting and pushing water. From it, the fetus receives nutrients at 12 weeks. The baby actively moves: unbends and bends the legs and arms, unclenches and compresses the fists. Due to the small size, the expectant mother does not yet feel this.
What happens to the expectant mother
Depending on the size of the woman in position, the belly at the 12th week of pregnancy may not be visible at all or is already slightly noticeable. Many women want to know where the fetus is, what is the size of the uterus during this period, and how much weight can be gained. The uterus at this time increases in size so much that it already becomes cramped in the small pelvis, and mommy can feel it above the pubic part. Symptoms characteristic of the first months (nausea, vomiting, aversion to specific odors), during the normal course of pregnancy, gradually disappear.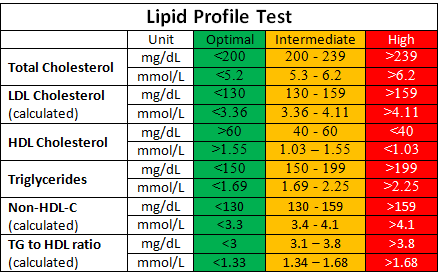 At 12 weeks, a woman's weight gain of 300-400 grams per week is considered the norm. The baby should receive all the necessary nutrients from the mother, so it is necessary to eat the right and moderately high-calorie food.
At 12 weeks, a woman's weight gain of 300-400 grams per week is considered the norm. The baby should receive all the necessary nutrients from the mother, so it is necessary to eat the right and moderately high-calorie food.
Mother's nutrition
Nutrition at 12 weeks does not differ from the characteristics of food intake throughout pregnancy. It is recommended to eat healthy, rich in vitamins and minerals food often, but in small portions. Taste preferences at 12 weeks can also continue to amaze both the pregnant woman herself and her family. But it is worth knowing that a large amount of consumed salty foods provoke puffiness and increase pressure. Sugar is also bad for the gums, teeth, and intestines.
Examinations and tests
At the beginning of the 12th week or at 12.5 weeks, the doctor sends the expectant mother for the first serious and informative examination - screening. This is a complex of studies, consisting of ultrasound and a blood test for biochemistry.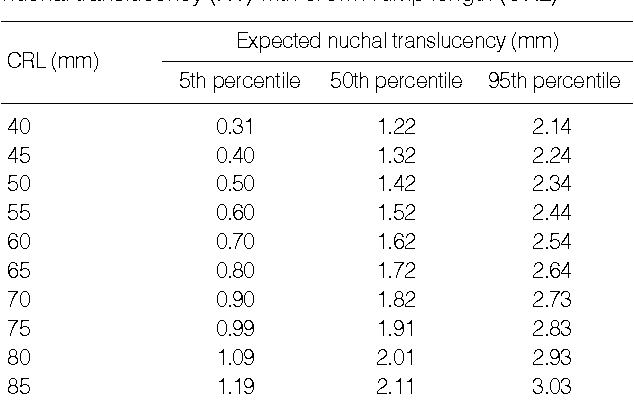 It will show if the baby has any pathologies, anomalies, whether its size corresponds to the gestational age. The study will make it possible to determine the degree of risk of developing Down syndrome, etc. Despite the highly accurate results, if there is a suspicion of a disease based on the results of screening, the doctor sends the pregnant woman for an additional examination to genetics. In these situations, the doctor will never make a diagnosis based on the screening results alone. In addition, for a period of exactly 12 weeks, the future mother is measured weight, pressure. They may give a referral to a urine test to determine the level of sugar and protein.
It will show if the baby has any pathologies, anomalies, whether its size corresponds to the gestational age. The study will make it possible to determine the degree of risk of developing Down syndrome, etc. Despite the highly accurate results, if there is a suspicion of a disease based on the results of screening, the doctor sends the pregnant woman for an additional examination to genetics. In these situations, the doctor will never make a diagnosis based on the screening results alone. In addition, for a period of exactly 12 weeks, the future mother is measured weight, pressure. They may give a referral to a urine test to determine the level of sugar and protein.
Physical activity
Many pregnant women want to keep their body in good shape. Physical education and other sports allowed for pregnant women will benefit the mother, baby and the future process of childbirth. Physical education increases the overall tone, strengthens ligaments, muscles, joints. It strengthens the parts of the body that will work during childbirth, and is also the prevention of stretch marks on the abdomen and thighs. It is important to understand that mommy can lead an active, sporty lifestyle only if there are no prohibitions from the doctor. Currently, in addition to physical education for pregnant women, many other special activities are offered. It can be specially prepared for women in the position of the program of shaping, yoga, water aerobics. It is important that the instructor be professional and ensure that all exercises are performed correctly.
It is important to understand that mommy can lead an active, sporty lifestyle only if there are no prohibitions from the doctor. Currently, in addition to physical education for pregnant women, many other special activities are offered. It can be specially prepared for women in the position of the program of shaping, yoga, water aerobics. It is important that the instructor be professional and ensure that all exercises are performed correctly.
Psychological state
In the normal course of pregnancy, by 12 weeks, the psychological state of the expectant mother becomes more stable. She is already getting used to her new role, toxicosis is gradually receding, her stomach is still quite small in order to somehow interfere with her physical condition with her size. Scientists have conducted an experiment. During it, with the help of special video recording, the relationship between the psychological state of the pregnant woman and the mood of the child in the womb was monitored. Experience has shown that when a woman was cheerful, then the baby in her stomach smiled. And when the mother was sad, the expression on the child's face became sad. Mom is the baby's universe. Especially when he lives in her stomach. It is important to understand this and take care of your psychological state during pregnancy.
Experience has shown that when a woman was cheerful, then the baby in her stomach smiled. And when the mother was sad, the expression on the child's face became sad. Mom is the baby's universe. Especially when he lives in her stomach. It is important to understand this and take care of your psychological state during pregnancy.
Possible ailments
A beautiful position brings many changes to a woman's body. This may affect her physical condition. In order to properly respond to changes, you need to be aware of possible ailments, sensations and how to behave correctly when they appear.
Stretch marks. Due to the growth of the uterus and weight gain, as early as the twelfth week, a woman may develop stretch marks on her stomach, chest, and hips. If before pregnancy, mommy ate right, led an active lifestyle, if the skin in problem areas is elastic enough, stretch marks may not occur. To prevent stretch marks, you can use a special cream against stretch marks, it will moisturize the skin, make it more elastic. Ask your husband to give you a gentle massage with a hypoallergenic massage oil. Light massaging movements will also make the skin more elastic. In addition, this procedure is also very pleasant. She will cheer up mommy, and your baby will feel daddy's touch.
Ask your husband to give you a gentle massage with a hypoallergenic massage oil. Light massaging movements will also make the skin more elastic. In addition, this procedure is also very pleasant. She will cheer up mommy, and your baby will feel daddy's touch.
Headache. This ailment often occurs in women during pregnancy, especially in the first and second trimester, when the expectant mother is forced to go to work. Emotional and physical stress cause fatigue, which in turn is often accompanied by a headache. If the mother has a hard or nervous job, it is necessary to take frequent breaks during working hours. If possible, take a walk at lunchtime, ventilate the room. It is also important to remember about frequent meals, not to starve. You should try to avoid loud music, noise, large crowds. The cause of the headache may be the wrong position of the body. If you have to sit at the computer a lot, try to change the position of the body, periodically do a light workout.
Insomnia. Emotional swings, fatigue, feeling unwell can provoke insomnia. To restore sleep, you need to spend more time in the fresh air during the day, try not to overload your stomach with heavy food and invigorating drinks a few hours before bedtime. The cause of nocturnal insomnia may be a long daytime sleep of a pregnant woman. Therefore, if you want to sleep during the day and you have such an opportunity, do not sleep for more than an hour - an hour and a half. Ventilate the bedroom before going to bed, take care of a comfortable pillow and mattress. You can purchase a special pillow for pregnant women, which will help the expectant mother to take comfortable positions during sleep.
Emotional swings, fatigue, feeling unwell can provoke insomnia. To restore sleep, you need to spend more time in the fresh air during the day, try not to overload your stomach with heavy food and invigorating drinks a few hours before bedtime. The cause of nocturnal insomnia may be a long daytime sleep of a pregnant woman. Therefore, if you want to sleep during the day and you have such an opportunity, do not sleep for more than an hour - an hour and a half. Ventilate the bedroom before going to bed, take care of a comfortable pillow and mattress. You can purchase a special pillow for pregnant women, which will help the expectant mother to take comfortable positions during sleep.
In general, at 12 weeks, the baby is already quite well fixed in the womb. After this period, the likelihood of miscarriage is minimized (with the exception of women with a burdened obstetric history). If the expectant mother is concerned about such signs as frequent pulling pains, spotting, etc., you should immediately consult a doctor.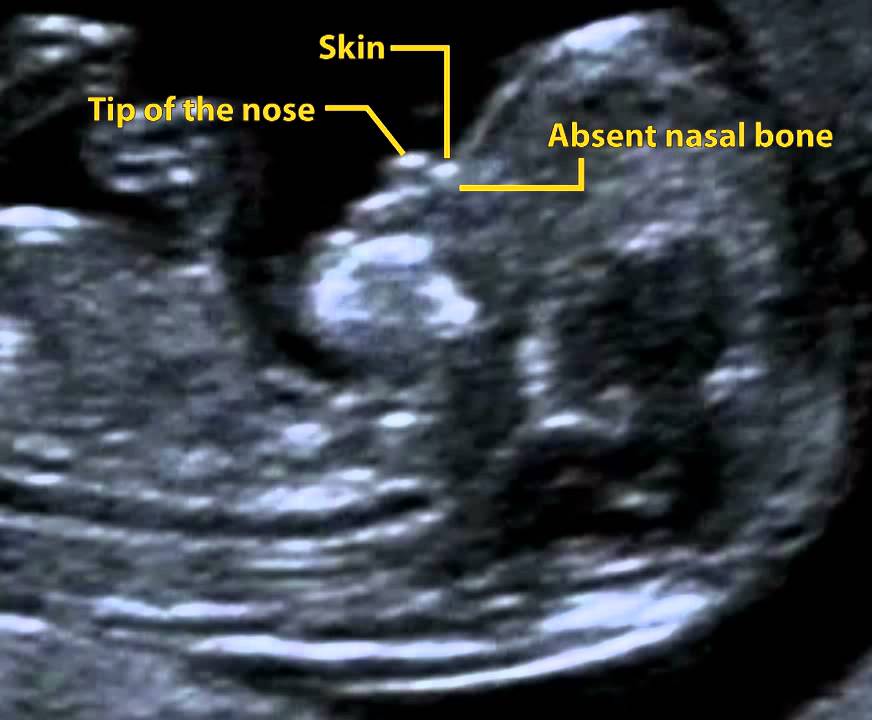 Don't wait for the house to improve. Timely medical measures taken will help save the health and, possibly, the life of the child.
Don't wait for the house to improve. Timely medical measures taken will help save the health and, possibly, the life of the child.
Weight control
Pregnant women should not eat high-calorie foods, as this can lead to excess weight gain. But you can’t deny yourself eating healthy food. This can lead to a lack of trace elements and vitamins, which can adversely affect the health of the expectant mother and baby. At each appointment, the doctor monitors weight gain and, if necessary, gives advice on adjusting mom's diet. In general, there are basic tips that suit most women.
If the increase is too high. If you follow all the rules, and the weight is still growing by leaps and bounds, your doctor should conduct additional diagnostics. Excessive weight gain can occur due to metabolic disorders, kidney function, etc. If all the tests are in order, then you should adjust your diet: reduce fat intake, exclude fried foods, mayonnaise from the diet. It is also necessary to remember about an active lifestyle, because eating even healthy foods can lead to weight gain if you move very little. For a woman expecting twins, there are slightly different weight criteria.
If the gains are too small. Here the situation is directly opposite to that described above. If you are not gaining enough weight, you need to increase your fat intake and thus get more calories. It is worth eating more healthy high-calorie foods. If you don't have an appetite, try eating wheat or other foods that stimulate your appetite. If you prefer an active and eventful lifestyle, try to slow down a bit. In any case, before correcting your diet and your habits, you should consult a doctor and find out the exact reasons for small weight gain.
Personal care tips
To stay healthy and attractive during pregnancy, you need to take care of yourself. But you need to do this taking into account your interesting position. As early as 12 weeks, you may need pants, a dress, and other maternity clothes. And skin care will require correction. Features of selection of clothes for pregnant women. Do not delay the moment of buying special things and hide loose trousers under long sweaters. When ordinary things become narrow and uncomfortable, it is worth visiting a specialty store. Currently, there are a lot of such boutiques. The expectant mother can find in them clothes of any style, style and size. Tights with a "pocket" that do not squeeze the abdomen, special panties and bras made from natural fabrics are especially popular. Trousers or jeans with an adjustable insert are the solution for every day.
Skin care features. Due to hormonal changes, the skin on the face and body can change its type. Those means that a woman used before pregnancy may not be suitable for her while carrying a baby. You need to pay attention to changes and respond to them by changing your care. It is important to choose care products that contain a minimum of harmful components.