When can a baby be born and live
the long-term impacts of being born extremely early
Scientists are watching out for the health of adults born extremely premature, such as these people who took part in a photography project.Credit: Red Méthot
They told Marcelle Girard her baby was dead.
Back in 1992, Girard, a dentist in Gatineau, Canada, was 26 weeks pregnant and on her honeymoon in the Dominican Republic.
When she started bleeding, physicians at the local clinic assumed the baby had died. But Girard and her husband felt a kick. Only then did the doctors check for a fetal heartbeat and realize the baby was alive.
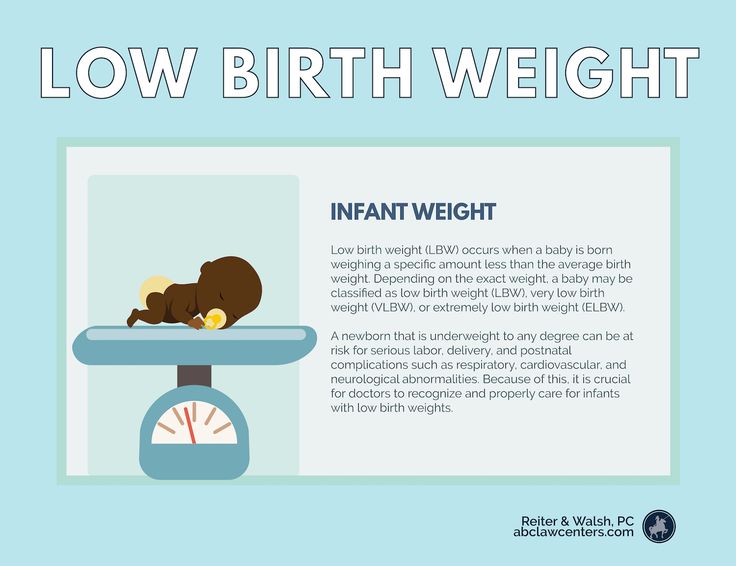
The couple was medically evacuated by air to Montreal, Canada, then taken to the Sainte-Justine University Hospital Center. Five hours later, Camille Girard-Bock was born, weighing just 920 grams (2 pounds).
Babies born so early are fragile and underdeveloped. Their lungs are particularly delicate: the organs lack the slippery substance, called surfactant, that prevents the airways from collapsing upon exhalation. Fortunately for Girard and her family, Sainte-Justine had recently started giving surfactant, a new treatment at the time, to premature babies.
After three months of intensive care, Girard took her baby home.
Today, Camille Girard-Bock is 27 years old and studying for a PhD in biomedical sciences at the University of Montreal. Working with researchers at Sainte-Justine, she’s addressing the long-term consequences of being born extremely premature — defined, variously, as less than 25–28 weeks in gestational age.
Families often assume they will have grasped the major issues arising from a premature birth once the child reaches school age, by which time any neurodevelopmental problems will have appeared, Girard-Bock says. But that’s not necessarily the case. Her PhD advisers have found that young adults of this population exhibit risk factors for cardiovascular disease — and it may be that more chronic health conditions will show up with time.
Camille Girard-Bock, born at 26 weeks of gestation, is now studying the effects of prematurity for a PhD. Credit: Red Méthot
Credit: Red Méthot
Girard-Bock doesn’t let these risks preoccupy her. “As a survivor of preterm birth, you beat so many odds,” she says. “I guess I have some kind of sense that I’m going to beat those odds also.”
She and other against-the-odds babies are part of a population which is larger now than at any time in history: young adults who are survivors of extreme prematurity. For the first time, researchers can start to understand the long-term consequences of being born so early. Results are pouring out of cohort studies that have been tracking kids since birth, providing data on possible long-term outcomes; other studies are trialling ways to minimize the consequences for health.
These data can help parents make difficult decisions about whether to keep fighting for a baby’s survival. Although many extremely premature infants grow up to lead healthy lives, disability is still a major concern, particularly cognitive deficits and cerebral palsy.
Researchers are working on novel interventions to boost survival and reduce disability in extremely premature newborns. Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Researchers are also investigating ways to help adults who were born extremely prematurely to cope with some of the long-term health impacts they might face: trialling exercise regimes to minimize the newly identified risk of cardiovascular disease, for example.
“We are really at the stage of seeing this cohort becoming older,” says neonatologist Jeanie Cheong at the Royal Women’s Hospital in Melbourne, Australia. Cheong is the director of the Victorian Infant Collaborative Study (VICS), which has been following survivors for four decades. “This is an exciting time for us to really make a difference to their health.”
The late twentieth century brought huge changes to neonatal medicine. Lex Doyle, a paediatrician and previous director of VICS, recalls that when he started caring for preterm infants in 1975, very few survived if they were born at under 1,000 grams — a birthweight that corresponds to about 28 weeks’ gestation. The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
“I remember when it arrived,” says Anne Monique Nuyt, a neonatologist at Sainte-Justine and one of Girard-Bock’s advisers. “It was a miracle.” Risk of death for premature infants dropped to 60–73% of what it was before1,2.
Marcelle Girard looks in at baby Camille, born weighing just 920 grams (2 pounds).Credit: Camille Girard-Bock
Today, many hospitals regularly treat, and often save, babies born as early as 22–24 weeks. Survival rates vary depending on location and the kinds of interventions a hospital is able to provide. In the United Kingdom, for example, among babies who are alive at birth and receiving care, 35% born at 22 weeks survive, 38% at 23 weeks, and 60% at 24 weeks3.
For babies who survive, the earlier they are born, the higher the risk of complications or ongoing disability (see ‘The effects of being early’). There is a long list of potential problems — including asthma, anxiety, autism spectrum disorder, cerebral palsy, epilepsy and cognitive impairment — and about one-third of children born extremely prematurely have one condition on the list, says Mike O’Shea, a neonatologist at the University of North Carolina School of Medicine in Chapel Hill, who co-runs a study tracking children born between 2002 and 2004. In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
“Preterm birth should be thought of as a chronic condition that requires long-term follow-up,” says Casey Crump, a family physician and epidemiologist at the Icahn School of Medicine at Mount Sinai in New York, who notes that when these babies become older children or adults, they don’t usually get special medical attention. “Doctors are not used to seeing them, but they increasingly will. ”
”
What should doctors expect? For a report in the Journal of the American Medical Association last year4, Crump and his colleagues scraped data from the Swedish birth registry. They looked at more than 2.5 million people born from 1973 to 1997, and checked their records for health issues up until the end of 2015.
Source: Ref. 4
Of the 5,391 people born extremely preterm, 78% had at least one condition that manifested in adolescence or early adulthood, such as a psychiatric disorder, compared with 37% of those born full-term. When the researchers looked at predictors of early mortality, such as heart disease, 68% of people born extremely prematurely had at least one such predictor, compared with 18% for full-term births — although these data include people born before surfactant and corticosteroid use were widespread, so it’s unclear if these data reflect outcomes for babies born today. Researchers have found similar trends in a UK cohort study of extremely premature births. In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
Such disabilities can impact education as well as quality of life. Craig Garfield, a paediatrician at the Northwestern University Feinberg School of Medicine and the Lurie Children’s Hospital of Chicago, Illinois, addressed a basic question about the first formal year of schooling in the United States: “Is your kid ready for kindergarten, or not?”
To answer it, Garfield and his colleagues analysed standardized test scores and teacher assessments on children born in Florida between 1992 and 2002. Of those born at 23 or 24 weeks, 65% were considered ready to start kindergarten at the standard age, 5–6 years old, with the age adjusted to take into account their earlier birth. In comparison, 85.3% of children born full term were kindergarten-ready6.
Despite their tricky start, by the time they reach adolescence, many people born prematurely have a positive outlook. In a 2006 paper7, researchers studying individuals born weighing 1,000 grams or less compared these young adults’ perceptions of their own quality of life with those of peers of normal birthweight — and, to their surprise, found that the scores were comparable. Conversely, a 2018 study8 found that children born at less than 28 weeks did report having a significantly lower quality of life. The children, who did not have major disabilities, scored themselves 6 points lower, out of 100, than a reference population.
As Marlow spent time with his participants and their families, his worries about severe neurological issues diminished. Even when such issues are present, they don’t greatly limit most children and young adults. “They want to know that they are going to live a long life, a happy life,” he says. Most are on track to do so. “The truth is, if you survive at 22 weeks, the majority of survivors do not have a severe, life-limiting disability. ”
”
A nurse uses electroencephalography (EEG) to carry out a check of brain development on a baby born at 25 weeks.Credit: BSIP/Universal Images Group via Getty
BreathlessBut scientists have only just begun to follow people born extremely prematurely into adulthood and then middle age and beyond, where health issues may yet lurk. “I’d like scientists to focus on improving the long-term outcomes as much as the short-term outcomes,” says Tala Alsadik, a 16-year-old high-school student in Jeddah, Saudi Arabia.
When Alsadik’s mother was 25 weeks pregnant and her waters broke, doctors went so far as to hand funeral paperwork to the family before consenting to perform a caesarean section. As a newborn, Alsadik spent three months in the neonatal-intensive-care unit (NICU) with kidney failure, sepsis and respiratory distress.
The complications didn’t end when she went home. The consequences of her prematurity are on display every time she speaks, her voice high and breathy because the ventilator she was put on damaged her vocal cords. When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
The brain, interrupted
That certainly wasn’t something her physicians knew to check for. In fact, doctors don’t often ask if an adolescent or adult patient was born prematurely — but doing so can be revealing.
Charlotte Bolton is a respiratory physician at the University of Nottingham, UK, where she specializes in patients with chronic obstructive pulmonary disease (COPD). People coming into her practice tend to be in their 40s or older, often current or former smokers. But in around 2008, she began to notice a new type of patient being referred to her owing to breathlessness and COPD-like symptoms: 20-something non-smokers.
Quizzing them, Bolton discovered that many had been born before 32 weeks. For more insight, she got in touch with Marlow, who had also become concerned about lung function as the EPICure participants aged. Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Treatments for premature babies have improved in recent decades, but survival rates vary by age and country.Credit: Mohammed Hamoud/Getty
VICS research backs up the cardiovascular concerns: researchers have observed diminished airflow in 8-year-olds, worsening as they aged10, as well as high blood pressure in young adults11. “We really haven’t found the reason yet,” says Cheong. “That opens up a whole new research area.”
At Sainte-Justine, researchers have also noticed that young adults who were born at 28 weeks or less are at nearly three times the usual risk of having high blood pressure12. The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The scientists were pessimistic as they began a pilot study of a 14-week exercise programme. They thought that the cardiovascular risk factors would be unchangeable. Preliminary results indicate that they were wrong; the young adults are improving with exercise.
Girard-Bock says the data motivate her to eat healthily and stay active. “I’ve been given the chance to stay alive,” she says. “I need to be careful.”
From the startFor babies born prematurely, the first weeks and months of life are still the most treacherous. Dozens of clinical trials are in progress for prematurity and associated complications, some testing different nutritional formulas or improving parental support, and others targeting specific issues that lead to disability later on: underdeveloped lungs, brain bleeds and altered eye development.
For instance, researchers hoping to protect babies’ lungs gave a growth factor called IGF-1 — which the fetus usually gets from its mother during the first two trimesters of pregnancy — to premature babies in a phase II clinical trial reported13 in 2016. Rates of a chronic lung condition that often affects premature babies halved, and babies were somewhat less likely to have a severe brain haemorrhage in their earliest months.
Could baby’s first bacteria take root before birth?
Another concern is visual impairment. Retina development halts prematurely when babies born early begin breathing oxygen. Later it restarts, but preterm babies might then make too much of a growth factor called VEGF, causing over-proliferation of blood vessels in the eye, a disorder known as retinopathy. In a phase III trial announced in 2018, researchers successfully treated 80% of these retinopathy cases with a VEGF-blocking drug called ranibizumab14, and in 2019 the drug was approved in the European Union for use in premature babies.
Some common drugs might also be of use: paracetamol (acetaminophen), for example, lowers levels of biomolecules called prostaglandins, and this seems to encourage a key fetal vein in the lungs to close, preventing fluid from entering the lungs15.
But among the most promising treatment programmes, some neonatologists say, are social interventions to help families after they leave the hospital. For parents, it can be nerve-racking to go it alone after depending on a team of specialists for months, and lack of parental confidence has been linked to parental depression and difficulties with behaviour and social development in their growing children.
At Women & Infants Hospital of Rhode Island in Providence, Betty Vohr is director of the Neonatal Follow-Up Program. There, families are placed in private rooms, instead of sharing a large bay as happens in many NICUs. Once they are ready to leave, a programme called Transition Home Plus helps them to prepare and provides assistance such as regular check-ins by phone and in person in the first few days at home, and a 24/7 helpline. For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
The results have been significant, says Vohr. The single-family rooms resulted in higher milk production by mothers: 30% more at four weeks than for families in more open spaces. At 2 years old, children from the single-family rooms scored higher on cognitive and language tests16. After Transition Home Plus began, babies discharged from the NICU had lower health-care costs and fewer hospital visits — issues that are of great concern for premature infants17. Other NICUs are developing similar programmes, Vohr says.
With these types of novel intervention, and the long-term data that continue to pour out of studies, doctors can make better predictions than ever before about how extremely premature infants will fare. Although these individuals face complications, many will thrive.
Alsadik, for one, intends to be a success story. Despite her difficult start in life, she does well academically, and plans to become a neonatologist. “I, also, want to improve the long-term outcomes of premature birth for other people.”
“I, also, want to improve the long-term outcomes of premature birth for other people.”
Premature birth statistics | Tommy's
Tommy's PregnancyHub
A preterm birth is one that happens before 37 weeks of pregnancy. Globally, more than 1 in 10 pregnancies will end in preterm birth.
A preterm birth is one that happens before 37 completed weeks of pregnancy.
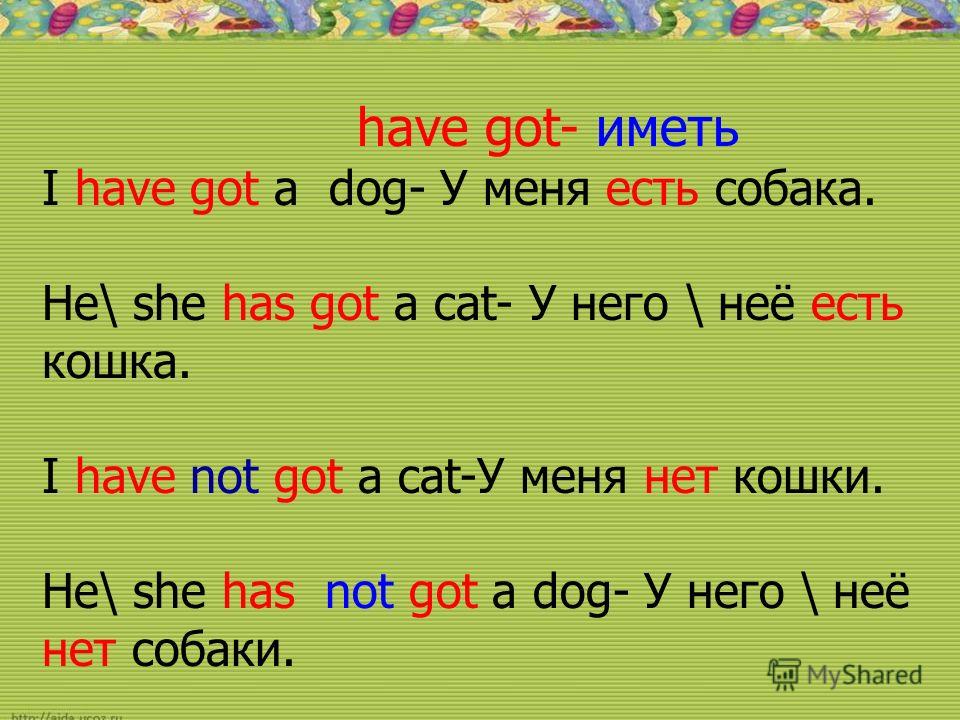
The World Health Organisation gives the following definitions for the different stages of preterm birth:
- Extremely preterm: before 28 weeks
- Very preterm: from 28 to 31 weeks
- Moderate to late preterm: from 32 to 37 weeks.
General UK premature birth statistics
- Around 8% of births in the UK are preterm. That is around 60,000 babies each year.
- This is higher than many countries in Europe and higher than Cuba and Iran
Of the births that were preterm in the UK:
- 5% were extremely preterm (before 28 weeks)
- 11% were very preterm (between 28 and 32 weeks)
- 85% were moderately preterm (between 32 and 37 weeks).

In 2019, live births where gestational age was under 24 weeks increased to 0.15% compared with 0.13% in 2018 and 0.11% in 2010.
Chances of survival following preterm birth
Medical advances mean that we are getting better at treating preterm babies but the chances of survival still depend on gestational age (week of pregnancy) at time of birth.
- Less than 22 weeks is close to zero chance of survival
- 22 weeks is around 10%
- 24 weeks is around 60%
- 27 weeks is around 89%
- 31 weeks is around 95%
- 34 weeks is equivalent to a baby born at full term.
Preterm birth and neonatal death
Complications arising from premature birth is the leading cause of neonatal death (death in the first few weeks after birth) in the UK.
Preterm birth and multiple pregnancies
Having more than one baby is a risk factor for preterm birth. On average, most singleton pregnancies last 39 weeks, twin pregnancies 37 weeks and triplets 33 weeks.
- Risk of prematurity with singleton pregnancy: 7%
- Risk of prematurity with multiple pregnancy: 57%
Risk of disability in preterm children
Generally, the earlier the birth, the higher the risk of problems. However these are only statistics and cannot predict how an individual child will do; some extremely premature babies do very well and develop into healthy children.
- 1 in 10 of all premature babies will have a permanent disability such as lung disease, cerebral palsy, blindness or deafness.
- 1 in 2 of premature babies born before 26 weeks of gestation will have some sort of disability (this includes mild disability such as requiring glasses).
In one study of 241 children born before 26 weeks' gestation the following was found:
- 22% severe disability (eg cerebral palsy + not walking, low cognitive scores, blindness, profound deafness)
- 24% moderate disability (eg cerebral palsy + walking, IQ/cognitive scores in the special needs range, lesser degree of visual or hearing impairment)
- 34% mild disability (defined as low IQ/cognitive score, squint, requiring glasses)
- 20% no problems.
Preterm birth by ethnicity
The risk of preterm birth is highest for Black Caribbean women and lowest for White British and White Other.
- Bangladeshi: 8%
- Indian: 7%
- Pakistani:7%
- Black African: 8%
- Black Caribbean: 10%
- White British: 7%
- White Other: 6%
Causes of preterm birth
In some cases a cause of preterm birth can be shown but more often it is unknown or unclear.
In 1 in 4 preterm births, the birth is planned (induced labour or c-section) to save the life of mother or baby from pregnancy complications such as pre-eclampsia, fetal growth restriction, waters breaking early (PPROM) or infection
Preventing premature birth
Too often health professionals are not able to tell women why they have had a premature birth. This area of research is underfunded, with many taking an unhelpful (and unique to pregnancy) approach of ‘It was not meant to be’.
Research into why premature birth happens is the only way we can save lives and prevent future loss.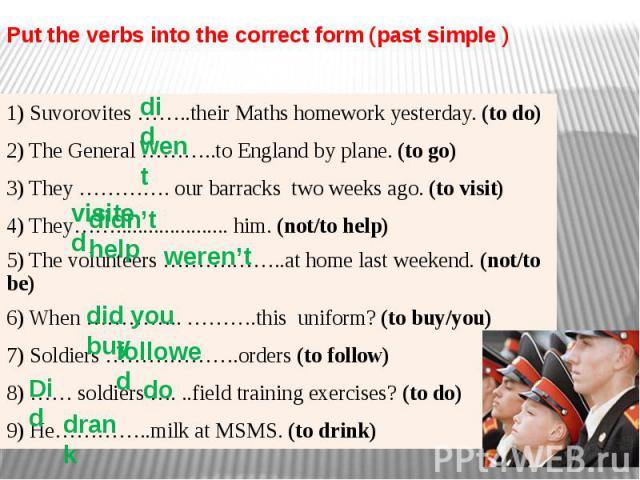 Tommy's funds more than £400k of research into premature birth every year. We are focused on predicting early which women will have a premature birth and treating them to prevent it happening.
Tommy's funds more than £400k of research into premature birth every year. We are focused on predicting early which women will have a premature birth and treating them to prevent it happening.
Read about our research into prematurity here.
Back to top
“His organs and systems are not ready” Why are they trying to save children in Russia who have almost no chance of surviving and being healthy: Society: Russia: Lenta.ru
period (less than 22 weeks) and extremely low weight (less than 500 grams). This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu.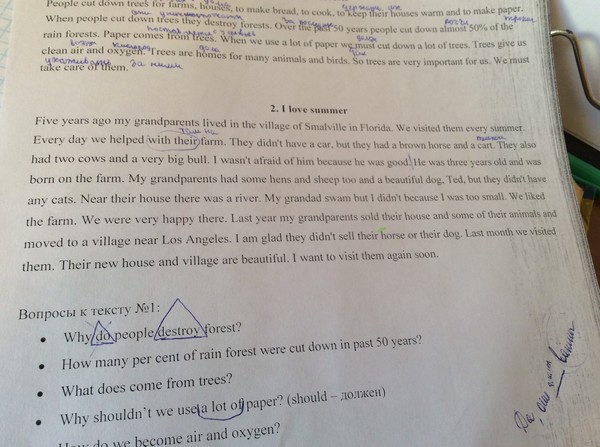 E. Veltishchev Elena Keshishyan.
E. Veltishchev Elena Keshishyan.
***
Lenta.ru: Now the minimum criteria for saving premature babies are 22-23 weeks and 500 grams of weight. Why?
Elena Keshishyan : In order to understand what is the limit of possibilities both in technical terms (creation of an environment close to intrauterine), and in terms of the maturity of the child's brain, which is able to develop out of utero, attempts were made in the world to give birth to premature babies of different ages. The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals.
Therefore, guided by research data and on the basis of a humanistic idea, the World Health Organization has established this limit for human live birth - 23 weeks, which corresponds to approximately 500 grams of weight. This is the minimum age at which the brain can differentiate into gray and white matter. And, accordingly, there is hope that it will already be a human person with mental abilities.
Countries with technological capabilities, including Russia, have agreed that those born at this gestational age can legally be considered human. That is, they have all human rights, including medical care.
Since 2012, Russia has moved to the WHO criteria for nursing premature babies. How many of these children have been saved during this time?
As a percentage of all those born, this is a minuscule amount. I don't have exact numbers. But I want to say that the body of children born almost half prematurely is very immature. And their survival rate, conditionally, is one in a hundred. Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors.
Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors.
One of the smallest surviving premature babies in the world. Amilya Taylor was born in 2006 in Miami, USA. She spent only 22 weeks in the womb and was born with a weight of 284 grams and a height of 24 centimeters.
Photo: Baptist Health South Florida / Reuters
And dear?
Of course. A day in a well-equipped neonatal intensive care unit costs several thousand dollars. And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply.
And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply.
If these children are not viable, cost too much, then why were these criteria established?
The medical task here is not at all to save without exception all children born at a term of five months. It is clear that there is not a single person who does not understand that this child is at risk of being blind, deaf and immobilized. The task of medicine in this situation is to acquire knowledge and experience.
Obstetricians learn how to prolong pregnancy as much as possible. There is a whole range of activities: prenatal diagnosis of genetic chromosomal diseases, various fetal malformations, identification of risk groups among pregnant women, their special monitoring, prenatal logistics and routing. They also hone the ability to properly take birth at this time. This must be done as carefully as possible and do not forget about the "golden hour". It is necessary to have time to give the child, without waiting until his condition worsens, what he could not get from his mother. That is, even if the child screamed, you need to understand that soon he will stop doing this and will not be able to breathe. The "golden hour" essentially determines whether or not there will be damage to brain cells. This means whether or not a child will have a full life.
And the qualifications of resuscitators working with such children are growing today. All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
And before?
About 30 years ago, about six or seven out of ten children would have become severely disabled. And today I had three 26-week-old babies at my appointment. And everyone is developing quite well, there is a slight backlog, but they will catch up. These children no longer have those possible malformations that, unfortunately, would have necessarily arisen in past years.
And this became possible thanks to the experience, the accumulation of knowledge about how such babies develop. There are no small things. This applies to everything - how to evaluate the heartbeat, how to interpret blood tests, and so on. Caring for a premature baby, both in the neonatal period and later, in the first or second year of life, is not the same as managing a normal, full-term baby. But knowledge allows timely adjustment of development, without even waiting for problems.
Photo: Science Photo Library / East News
It is important to understand that a premature baby is not a small copy of a normal one. This is a child who is forced to adapt to extrauterine life, when physiologically he should not do this. Its organs and systems are not prepared to function in the new conditions.
"This is painful love at the level of deep depression"
What do such children most often suffer from?
One of the typical pathologies is retinopathy of prematurity. In children, the mechanism that protects the eye from light has not yet matured. And they experience a real shock, suddenly falling into our bright world. Photons of light and the flow of oxygen begin to act on the retina, its vessels begin to grow rapidly, penetrate all the media of the eye, and, ultimately, exfoliate the retina, leading to total blindness. Earlier, even when I was just starting to work, although we knew about such a disease as retinopathy of prematurity, there were few children born and surviving at gestational ages of less than 30 weeks. Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness.
But we started learning very quickly. Now in perinatal centers in all intensive care units for premature babies - twilight. The cuveuses are completely covered with dark blankets. The staff does not need to watch the baby all the time - all readings are automatically recorded by special devices. In good ICUs, nurses who approach babies have headlights. This is to avoid disturbing other children. In many intensive care units, a large “ear” hangs. If the decibel level in the room begins to exceed the allowable limit, the device lights up red.
After the birth of the child, every week they begin to look at the eyes with a special method. If there is proliferation of blood vessels, laser coagulation of the retina is performed. There are specialists in such operations in almost every major city.
Approximately 400-600 babies pass through me every year, born at 26-28 weeks. Over the past few years, not a single blind person has been among them. Although earlier in hospitals for such newborns it was necessary to open entire departments.
Is there any data on how many premature babies later became healthy?
Now among premature babies born at five or six months (25-26 weeks of pregnancy), 25-30 percent become disabled. The same is true in developed countries. And even 20-30 years ago there were 75-80 percent of them.
The risks for these children are still very high. They require long-term observation and treatment. But still today they have incommensurably or better chances than before.
Photo: East News
Do unfortunate parents regret insisting on resuscitation at all costs?
As a doctor, no one has ever told me this. Naturally, the families had very different hopes for childbirth. In the doctor's office they cry, but they don't moan. These children are madly loved. But this is painful love at the level of deep depression. Probably, some of these mothers may think at night what would happen if they knew in advance how everything would turn out. Perhaps they voice this to their mothers, husbands, girlfriends . .. But not to doctors. This is where people prefer to stay.
.. But not to doctors. This is where people prefer to stay.
When a child is one or two years old, from a moral point of view, the situation is more difficult than in three days. Newborns are all wonderful bags, it is only then that children begin to differ from each other. These families have a very specific and difficult life. When a child lies at home, does not move, does not swallow, never looks at you, does not speak - this is very difficult. And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts.
What family support can I expect now?
When Russia switched to WHO standards, doctors began to say that if we started caring for such children, there would be a high incidence of cerebral palsy, mental retardation and other pathologies leading to severe disability. Without the development of a specialized service that will help such children, we will inflict enormous damage on a society that will not accept such an increase in the number of people with disabilities. Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly.
Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly.
The worst situation is with the social service. Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family.
Is there a support system in other countries?
I know that in Europe and in the USA it is built very well. The emphasis is not on medical rehabilitation, but on social rehabilitation. They have social workers who come and relieve these families of a significant part of their worries. Somewhere there are social centers where a child can be taken to a kindergarten. Moreover, they are zoned - parents do not need to go to the other end of the city.
Photo: Alexander Kondratyuk / RIA Novosti
“Even if it is clear that a child has pathologies that are incompatible with life, they must be saved to the last”
You say that some time ago, 1kg premature babies were also considered “non-residents”, but now they are quite promising. Is it possible that in 30-40 years the same can be said about 500-gram ones?
Indeed, even 30-40 years ago, when it was not possible to maintain breathing, children born before seven months of age survived very rarely.
Then, when some first mechanisms appeared, the bar was raised until the 28th week of pregnancy, which is about six months. But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants. They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants. They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
Technologically, the frontier could move indefinitely. If desired, you can simulate a situation where a woman is not needed at all to bear a child. But I have already said that scientists have established that the age of 22-23 weeks is the minimum period at which the cells of the cerebral cortex can develop postnatally. Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Is it true that they try to save all 500-gram children only in Russia and Turkey, and in other countries - only if the child has high chances for a normal life?
This is not true. In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
There is a special service in perinatal centers. When it becomes clear that preterm labor has begun, representatives approach relatives - the father and, if possible, the mother. “We assume that a baby will be born with such and such parameters. In this case, there are such and such development risks ... You have the right to choose either full resuscitation or palliative care. And depending on what the parents decide, the doctors act.
And depending on what the parents decide, the doctors act.
Photo: Sergey Pyatakov / RIA Novosti
In Russia, you can also choose a palliative today, right?
This is not prescribed by law. Today, even if it is clear that a child has pathologies incompatible with life, they must be saved to the last. It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”.
The medical community is very concerned about this ambiguous position of doctors. And we have a number of proposals to solve the problem of their protection.
What exactly is offered?
Legislative initiative to allow parents to independently decide whether resuscitation care is appropriate for a child born between the 23rd and 25th weeks. Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations.
Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations.
The Ministry of Health has now prepared new criteria for newborns born too early. In particular, it is proposed not to register such a child until he has lived seven days. Maybe this will fix the situation, protect doctors from murder charges?
There are a lot of pitfalls here. In Russia, there was a similar law on kilogram children. They were assisted from birth, but until the age of seven days the child was considered a fetus. If he died, then his mortality already went into other criteria, it was not considered the death of a newborn.
There are not many children born with extremely low rates, they simply cannot influence the demographic structure in any way. But if there is such a situation that you can not register for up to seven days, it seems to me that even more claims may arise against doctors regarding the failure to provide assistance.
These are very difficult questions. On the one hand, parents can say: you did not save the child. And others, on the contrary, will say: why are you torturing him in vain? And imagine a resuscitator who may be faced with an ethical choice: he has only one ventilator in the hospital, and a 23-week-old baby has been on it for the 40th day. And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do?
Are you speaking theoretically now or do such situations occur?
We cannot have this in federal centers. We have enough equipment. I just illustrated with an example that the issue of nursing such children is the most difficult, all aspects are in common in it - from medical to ethical and religious.
Photo: Sergei Krasnoukhov / RIA Novosti
“The issue of infant mortality has always been political”
The issue of infant mortality has recently become political. Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply?
Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply?
The issue of infant mortality has always been political. This is a socially significant parameter that determines the position of the country in terms of development. In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
The primary decrease in mortality occurred due to the high-quality saturation of hospitals with equipment, due to the construction of perinatal centers. This gave immediate results. And now these figures have reached a plateau. Another thing is that a plateau, for example, in Kaliningrad, St. Petersburg, is one thing. There mortality rates are at the European level. That is very low. And there are regions where mortality is high - the Altai Territory, the Jewish Autonomous Region, Magadan. There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it.
There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it.
We are not compact Switzerland. We have a huge country with difficult geographical conditions. There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
There are no good hospitals there?
Everything is there, but in one city - in Anadyr. And if a woman gave birth in another place, then often she can be cut off from the world. There are periods when even planes do not fly: a snowstorm, something else. And with routing too you will not guess. Because when you are expecting your first child, you are not going to give birth at 24 weeks. This is if the situation with childbirth repeats, then you can plan something, come closer to specialized care at the “dangerous” time . ..
..
Is it true that there have been more premature births lately?
No, their number is stable. This is approximately 7-10 percent of all newborns. Significantly increased their survival rate.
One of the most "inciting" topics on parenting Internet forums is that children who are "culled out" by nature have a bad effect on the quality of the gene pool. Is there any reason to think so?
In order for "survivors" to be able to influence the population, there must be a lot of them in percentage terms. For example, there are very few 26-week-olds - no more than two percent of all births. It can't affect anything in any way.
I know that at one time they discussed: what will happen if my child marries in the future someone who was once premature, will the gene pool suffer? Firstly, I can say that, as for children born after the 30th week, they are completely healthy, adapted and no different from others. They themselves give birth to beautiful healthy children, we have already seen many generations. The risk of preterm birth is not inherited. And usually premature babies are shaken, they are a lot of work. So in terms of development, these children can give odds to others.
The risk of preterm birth is not inherited. And usually premature babies are shaken, they are a lot of work. So in terms of development, these children can give odds to others.
As for children born at 5-6 months old, when they catch up with their peers, it is important that parents continue their active life with them, and not engage in a protective regime. We need songs, dances, sports. These children have behavioral patterns. But now there are centers that supervise such families. If you take care of children, everything will be fine. I look at these kids regularly. And I have a much more optimistic outlook. For example, the frequency of chronic diseases among them is approaching the norm. That is, it is not higher than in the population. Everyone has a chance for a full life, even the most hopeless, at first glance, child.
Can a premature baby grow up healthy? Who is to blame for preterm birth? And what do you need to know about vaccinating such children? Answering important questions about preterm babies
Fetus at 8 weeks
BSIP / UIG / Getty Images
Premature babies weighing over 500 grams are being nursed in Russia. Their parents are often very worried: whether the child will be healthy, what is happening in general, what to look for after discharge, and what are the restrictions. At the same time, people around may not support their parents at all and even condemn the mother for the fact that she is supposedly to blame for what happened. We decided to help such parents and their loved ones by answering important questions about premature babies.
Their parents are often very worried: whether the child will be healthy, what is happening in general, what to look for after discharge, and what are the restrictions. At the same time, people around may not support their parents at all and even condemn the mother for the fact that she is supposedly to blame for what happened. We decided to help such parents and their loved ones by answering important questions about premature babies.
When should a baby be born to be called premature?
Up to 37 weeks (usually a normal pregnancy lasts 40 weeks). More precisely, up to 36 weeks and 6 days, counting from the first day of the last menstruation.
The lower bound is much more complicated. In Russia, a child can be registered when at the same time:
- the pregnancy is 22 weeks or more;
- Birth weight of the baby is 500 grams or more (when weighed within the first hour after birth; this does not apply to multiple births) or if the baby's birth weight is unknown, the body length is 25 centimeters or more.
If one of these criteria is not met, but the child lives 168 hours, then they can also be registered. In other cases, a birth certificate is not issued.
But a child can be born and still not be alive. Therefore, official signs of live birth have also been approved: in addition to the birth itself, the presence of four signs of live birth (heartbeat, spontaneous breathing, umbilical cord pulsation or voluntary movement of the limbs) is important, while the most important sign is the presence of a heartbeat, notes the chief freelance neonatologist of the Ministry of Health in the North Caucasus Federal District Alexey Mostovoy, Head of the Department of Resuscitation and Intensive Care of Newborns of the Kaluga Regional Clinical Hospital. If none of these signs are present, the child can be considered stillborn.
Even if a child does not meet the registration criteria, doctors can still resuscitate and move to an incubator, providing warmth, nutrition, pain relief, mechanical ventilation and other supportive care. Then the child can survive and live those same 168 hours to get a birth certificate. But in reality, such children rarely survive. “If a child who does not meet the criteria for a live birth survives, this is a case that is described in specialized medical publications, and the regular press often writes about this,” says the Deputy Chief Physician for Obstetric and Gynecological Care of the City Clinical Hospital. F. I. Inozemtseva Sergey Apresyan. “That is, it happens, but as an extraordinary event.”
Then the child can survive and live those same 168 hours to get a birth certificate. But in reality, such children rarely survive. “If a child who does not meet the criteria for a live birth survives, this is a case that is described in specialized medical publications, and the regular press often writes about this,” says the Deputy Chief Physician for Obstetric and Gynecological Care of the City Clinical Hospital. F. I. Inozemtseva Sergey Apresyan. “That is, it happens, but as an extraordinary event.”
Strict criteria cause problems
Such strict registration criteria and signs of live birth are often criticized. At least because in practice this leads to rather strange situations: “The legal status of such children [who do not meet the signs of live birth] is still not defined - in the first seven days of life, they, according to the letter of the law, are neither live-born nor stillborn, - says the legal adviser on medical law, the founder of the company "Faculty of Medical Law" Polina Gabay. - <...> I read the decision of one court of appeal, which recognized a child who lived for several days in intensive care as unborn, because he, I quote: "Did not meet certain anthropometric parameters." I don’t even know who then, according to the court, was lying in the couveuse? It is known from the circumstances of the case that his weight was 20 grams less than that established by the birth criteria.”
- <...> I read the decision of one court of appeal, which recognized a child who lived for several days in intensive care as unborn, because he, I quote: "Did not meet certain anthropometric parameters." I don’t even know who then, according to the court, was lying in the couveuse? It is known from the circumstances of the case that his weight was 20 grams less than that established by the birth criteria.”
The World Health Organization (WHO) generally does not offer any strict criteria for determining a live birth. Her position is as follows: a child is recognized as live born regardless of the gestational age - the main thing is that he breathes or shows other signs of life, for example, a heartbeat. “The WHO recommendations on keeping statistics, which serve the sole purpose of standardizing data collection around the world, have been turned by officials into legal criteria that determine the status of a newborn child,” writes Diana Mustafina-Bredikhina, Senior Lecturer at Peoples’ Friendship University of Russia. “<...> The presence in the law of the lower limit of the live birth count has a strange effect on the investigative authorities, which have recently begun to initiate criminal cases more often, prosecuting doctors for the “deliberate murder” of premature babies with extremely low body weight.”
“<...> The presence in the law of the lower limit of the live birth count has a strange effect on the investigative authorities, which have recently begun to initiate criminal cases more often, prosecuting doctors for the “deliberate murder” of premature babies with extremely low body weight.”
In the UK and the US, when talking about how doctors should behave, doctors recommend focusing on prognosis. For children born before 22 weeks, it is very bad, so in such cases it is usually not even advised to start resuscitation, believing that it is more humane not to conduct active resuscitation. At a later date, it is advised to discuss this issue with parents. In such cases, the risk of death is also high, as is the risk of serious disorders in the development of the nervous system, so it is important to take their opinion into account. If they refuse resuscitation, then the child is provided with palliative care. In Russia, this is almost impossible: if a live birth is recorded, resuscitation must be carried out, refusing it is contrary to federal law.
Nine weeks
BSIP / Alamy / Vida Press
What happens to premature babies and their parents immediately after birth?
You need to prepare for the fact that immediately after the birth, and for a long time after, there will be a lot of uncertainty. It can even shock how a child looks.
“People who have not seen our children sometimes think that these are three-kilogram pink baby dolls, only small ones,” explains Elina Sushkevich, an anesthesiologist-resuscitator of the neonatal intensive care unit of the Regional Perinatal Center of the Kaliningrad Region. In fact, such children have very thin delicate skin through which blood vessels are visible and which poorly performs its barrier functions, that is, it only protects against dangerous bacteria and viruses. These children have little subcutaneous fat, so they look very fragile and emaciated. They lack some reflexes at birth, and it is difficult for a baby born before the 35th week to coordinate sucking and swallowing. “Anatomically formed organ systems do not have the proper functionality and do not fully cope with the conditions of extrauterine life,” writes Olga Evseichik, a pediatrician at the Rassvet Clinic, in response to a question from Meduza.
“Anatomically formed organ systems do not have the proper functionality and do not fully cope with the conditions of extrauterine life,” writes Olga Evseichik, a pediatrician at the Rassvet Clinic, in response to a question from Meduza.
“I would not recommend looking for any information on the survival rate, disability of a child,” writes Natalya Vasilyeva, a pediatrician and chief physician of the Rassvet children’s clinic, in response to a question from Meduza. “It can turn out to be false both positively and negatively.” “For such children, everything can change at any moment, both for the better and for the worse,” writes Olga Evseichik. “It’s impossible to predict this, and it’s not even always possible to explain changes after the fact.”
“In the first place [among the causes of death of premature babies] are severe congenital infections and related complications: necrotizing enterocolitis, intracranial hemorrhages,” writes Alexey Mostovoy.
Other causes include respiratory distress syndrome and congenital abnormalities. According to American data, out of 1000 children born before the 28th week of pregnancy, 625 will survive, from the 28th to the 31st week - 964, from the 32nd to the 33rd week - 984, from the 34th to the 36th th week - 993. According to Alexey Mostovoy, such all-Russian statistics are not kept. However, on average, as far as is known, the figures are comparable to those in other developed countries. On the other hand, a lot depends on the level of the clinic, and this indicator can vary greatly from region to region.
According to American data, out of 1000 children born before the 28th week of pregnancy, 625 will survive, from the 28th to the 31st week - 964, from the 32nd to the 33rd week - 984, from the 34th to the 36th th week - 993. According to Alexey Mostovoy, such all-Russian statistics are not kept. However, on average, as far as is known, the figures are comparable to those in other developed countries. On the other hand, a lot depends on the level of the clinic, and this indicator can vary greatly from region to region.
However, in order to make a prediction for a particular child, it is not enough to know only the date on which he was born.
If you do not have enough information about what is happening, Natalya Vasilyeva recommends asking questions to doctors. “It often turns out that the words “they don’t tell us anything” mean “yes, we didn’t ask anything,” the expert explains.
Perhaps in this difficult time you should seek support from a psychologist. This can be done online or by phone - for example, by contacting the hotline of the Right to a Miracle charity fund for helping premature babies (8 800 555 2924). On other important issues, for example, regarding financial assistance or legal support, they can also advise there. There are also foreign non-profit organizations whose websites have a lot of supportive and useful materials (for example, Tommyʼs and Bliss).
On other important issues, for example, regarding financial assistance or legal support, they can also advise there. There are also foreign non-profit organizations whose websites have a lot of supportive and useful materials (for example, Tommyʼs and Bliss).
Can a premature baby grow up healthy?
It is possible, but a lot depends on how old he was born, how much he weighed at birth, what diseases he had initially, and also what resources the medical organization he was in had.
The main negative consequences that premature babies have are cerebral palsy, cognitive impairment, visual and hearing impairments. The lower the weight and term of delivery, the more likely such consequences are. Therefore, if there is a threat of preterm birth, they try to push them back by various methods for at least a few days: this in itself improves the prognosis for the child, and makes it possible to use drugs that help the child quickly adapt to life outside the uterus. But even in extremely premature babies (born before the 28th week) there is a chance for the absence of all these disorders.
At school age, those who were born prematurely have a higher risk of becoming overweight and obese. In adulthood, the development of insulin resistance, high blood pressure, coronary heart disease and some other diseases. But, in fact, one can talk about some predictions only with the proviso that now the long-term consequences are visible in children who were born prematurely many years ago, when medical specialists had fewer tools. What the exact prognosis for children born now is is unclear.
Is it true that babies are born prematurely because the mother smoked or drank during pregnancy? What generally influences it?
Many circumstances can lead to preterm birth, including uncontrollable, unpredictable and unknown. Unidentified causes are responsible for most preterm births. And far from always, even known risk factors have a significant impact on their own - their combination can lead to preterm birth.
It is now believed that the risk of preterm birth is negatively increased by, for example, the following factors:
- smoking;
- pregnancy as a result of in vitro fertilization.
 This is largely due to the fact that in such cases, pregnancy is more often multiple, and twins and triplets tend to be born prematurely. That is why modern recommendations are changing, and now in most cases it is advised to transfer only one embryo into the uterine cavity at a time;
This is largely due to the fact that in such cases, pregnancy is more often multiple, and twins and triplets tend to be born prematurely. That is why modern recommendations are changing, and now in most cases it is advised to transfer only one embryo into the uterine cavity at a time; - pregnancy within 18 months of childbirth;
- age of mother - risks are higher if the woman is younger than 17 and older than 35;
- diabetes mellitus and certain other chronic diseases;
- preeclampsia. In this condition, a woman's blood pressure rises, which does not cause symptoms, but can be detected at the reception (while, of course, not every increase in pressure is a sign of preeclampsia). The danger is that the condition can be complicated by swelling, severe headache, vision problems, and then, in some women, seizures, stroke, and other severe and life-threatening conditions. In this case, doctors may perform a caesarean section or induce labor even if the pregnancy is less than 37 weeks because it is safer for both mother and baby.

As for stress, it may slightly increase the risk of preterm birth. However, this cannot be said with certainty: conducting research is complicated by the fact that almost everyone experiences stressful events. And at what stage of pregnancy they can at least theoretically have a negative effect, it is not clear.
11 weeks
BSIP / Alamy / Vida Press
How to prevent preterm labor?
In addition to dealing with the controllable risk factors already listed (smoking, number of embryos transferred), doctors can offer several more tools to delay labor. First of all, it is important that a woman plans a pregnancy, prepares for it and is subsequently observed by a doctor. According to Alexey Mostovoy, this approach has been common for a long time, for example, in Sweden, and as a result, more women are doing just that, as a result of which infant mortality in this country has decreased.
Here's what else you can do besides this.
- Sometimes you can "catch" a dangerous state in time.
 Women with a history of preterm labor and a singleton pregnancy between weeks 16 (some say week 18) to week 24 are advised to have their cervical length scanned by ultrasound (some experts suggest everyone should do this). If it is shorter than expected, then this means that the risk of preterm birth is increased. Then, to reduce the risks, you can prescribe progesterone in the form of a vaginal gel or put stitches on the cervix, or possibly a pessary, although it is getting worse with evidence of effectiveness.
Women with a history of preterm labor and a singleton pregnancy between weeks 16 (some say week 18) to week 24 are advised to have their cervical length scanned by ultrasound (some experts suggest everyone should do this). If it is shorter than expected, then this means that the risk of preterm birth is increased. Then, to reduce the risks, you can prescribe progesterone in the form of a vaginal gel or put stitches on the cervix, or possibly a pessary, although it is getting worse with evidence of effectiveness. - As a prophylaxis for women who have already given birth prematurely, you can immediately prescribe progesterone starting from the 16-20th week of pregnancy (if she is singleton). Also, if the doctor understands that the risk of preterm birth is high, he may prescribe corticosteroids - drugs that accelerate the development of the baby's organs (usually this occurs after the 24th week).

- If the woman is already in labor and her cervix is dilating, you can use tocolytic therapy (for example, indomethacin or nifedipine), which can stop the process for at least a few days. This requires hospitalization. However, tocolytic therapy cannot be used for prophylaxis: its safety and effectiveness are best balanced precisely in cases where a woman has started labor. During the time doctors gain in this way, corticosteroids can be administered. And magnesium sulfate, which helps protect the brain from damage and therefore reduces the risk of developing cerebral palsy. Even if tocolytics delay labor by a few hours, that's a good thing: magnesium sulfate and corticosteroids will have more time to work. Also, a woman has the opportunity to go to a more equipped clinic, where premature babies are regularly nursed. “The birth of a premature baby is always a high-risk birth,” explains pediatrician Natalya Vasilyeva. “By all standards, high-risk births in an ideal world should take place in specialized institutions that have all the technical capabilities to save the child.
 ”
”
It must also be remembered that in a third of cases, contractions stop on their own, and a woman gives birth on time.
Does bed rest or lying down help?
There is no good evidence that bed rest (or lying "on hold") reduces the risk of preterm birth, including in women with a short cervix. Moreover, this practice could theoretically be dangerous due to the increased risk of blood clots. Not to mention that it does not improve the quality of life.
However, there are exceptions. “In some situations, hospitalization makes sense at a very high risk of preterm birth to quickly save a premature baby (not to prevent preterm birth)," explains obstetrician-gynecologist, medical director of the Fomin Clinic Tatyana Rumyantseva. “[This happens] is relevant if a woman lives far from a large perinatal center and, theoretically, may not have time to get to it.”
What does it take to have a premature baby?
When a baby is born prematurely, he may need various types of help to survive: from mechanical ventilation to warming devices and a warm hat (often knitted by volunteers). In addition, doctors and nurses are trying to reduce the risks of negative consequences - both in the short term and in the long term. For example, they give oxygen and, with the help of drugs, correct various indicators of the body's functioning so that everything is normal, and this, among other things, reduces the risk of intracranial hemorrhage.
In addition, doctors and nurses are trying to reduce the risks of negative consequences - both in the short term and in the long term. For example, they give oxygen and, with the help of drugs, correct various indicators of the body's functioning so that everything is normal, and this, among other things, reduces the risk of intracranial hemorrhage.
In specialized medical organizations (perinatal centers) there are more opportunities to provide a premature baby with all the necessary care and improve his chances of survival and a healthy life than in ordinary maternity hospitals. Not only experienced specialists are concentrated in perinatal centers, but also modern equipment and drugs, without which it is impossible to provide adequate medical care: “Neonatal resuscitation is expensive, and working with very premature babies is even more expensive,” explains Natalya Vasilyeva. “There is no point in spreading resources around rural maternity hospitals, it makes sense to organize large perinatal centers and establish professional transportation of newborns if high-risk births took place outside their walls.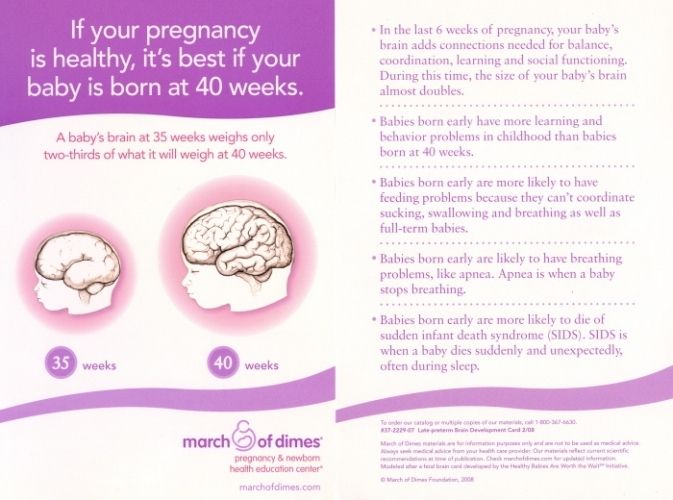 ”
”
Olga Yevseychik explains that such institutions have mobile resuscitation and advisory teams of intensive care units and neonatal intensive care units: “[They] make it possible to bring neonatal resuscitation care as close as possible to babies and ensure their most gentle transportation to the center,” Yevseychik writes.
Both experts provide a long list of what is needed to help premature babies. For example:
- heating systems (incubators). “[It should be] a normal ‘smart’ system that takes into account temperature fluctuations, sound insulation and the possibility of weighing a child without removing him from the incubator,” explains Natalya Vasilyeva. — <…> A premature baby cannot retain heat on its own. The incubator replaces the function of thermoregulation, maintaining the optimal temperature and humidity for the baby. And it also performs one of its most important functions - it protects the baby from loud sounds and bright lights.
 If you look at real photos from neonatal intensive care units, you will notice blankets and covers thrown over the incubators - this is additional protection from sound and light. As soon as the child can retain heat on his own, he can be transferred first to a heating source in a crib, and then to a regular crib without additional heat.
If you look at real photos from neonatal intensive care units, you will notice blankets and covers thrown over the incubators - this is additional protection from sound and light. As soon as the child can retain heat on his own, he can be transferred first to a heating source in a crib, and then to a regular crib without additional heat. - devices for various types of oxygen support: “From a “simple” neonatal ventilator to a high-frequency ventilator,” explains Natalya Vasilyeva;
- a plurality of microfluidizers;
- various types of parenteral nutrition, i.e. nutritional mixtures for intravenous administration;
- modern antibiotics, surfactants, that is, drugs that help the lungs open up, and other expensive medicines.
Various medical organizations, including the World Health Organization, recommend not to separate parents and a premature baby: if possible, establish breastfeeding and practice prolonged skin-to-skin contact - one of the parents sits in a chair, a child is placed under his clothes on his chest without clothes (except perhaps in a diaper), and they can sit like that for many hours. In English, this is called kangaroo care, that is, literally "kangaroo care", because the child is in contact with one of the parents, like a kangaroo in a mother's pouch. “If the baby’s condition allows it to be carried from place to place, then the number of wires and hoses connected to it does not matter — it can be placed on the hands/chest of the parents,” writes Natalya Vasilyeva. - It's just worth remembering that for babies in critical condition, moving can be deadly. There is a so-called "transfer test" - if the baby can tolerate it, then it can be moved.
In English, this is called kangaroo care, that is, literally "kangaroo care", because the child is in contact with one of the parents, like a kangaroo in a mother's pouch. “If the baby’s condition allows it to be carried from place to place, then the number of wires and hoses connected to it does not matter — it can be placed on the hands/chest of the parents,” writes Natalya Vasilyeva. - It's just worth remembering that for babies in critical condition, moving can be deadly. There is a so-called "transfer test" - if the baby can tolerate it, then it can be moved.
According to Olga Evseichik, this practice is not widespread in Russia, although there is evidence of its effectiveness.
When the child can breathe and eat normally on his own, maintain a normal body temperature, and gain stable weight, he or she will be discharged home.
22 weeks
BSIP / Alamy / Vida Press
What do you need to know about raising a premature baby?
Before being discharged, parents should be explained what is normal and what is not normal, and in what cases it is necessary to see a doctor (or even an ambulance). This often depends on the characteristics of the child himself. But in fact, there are fewer features in caring for such children than it might seem.
This often depends on the characteristics of the child himself. But in fact, there are fewer features in caring for such children than it might seem.
A premature baby may need frequent visits to the pediatrician (especially at first) to adjust the treatment of existing diseases, monitor changes and advise on other issues such as sleep and nutrition. All premature babies need to undergo additional screening tests. How often and which ones - depends on the specific situation. But the focus is usually on hearing loss, retinopathy of prematurity and other eye diseases, motor, intellectual and neuropsychiatric development (including autism spectrum disorders, the risk of which is increased in such children). Screening planning takes into account the adjusted age of the child.
“The task of a pediatrician is to summarize knowledge about the baby in one hand, combine observation plans in different directions into one, control them, change them as the child grows and improves / worsens,” writes Olga Evseichik. - The earlier the child was born, the more such checkpoints are in the list. How much is individual in each case. The expert also points out that such children require consultations of narrow specialists, but the list also depends on the specific situation.
- The earlier the child was born, the more such checkpoints are in the list. How much is individual in each case. The expert also points out that such children require consultations of narrow specialists, but the list also depends on the specific situation.
“The very word “premature” for parents is something like an internal stigma, some kind of seal of guilt that they feel latently at first,” explains Olga Evseichik. - They most often read a lot of different literature, they know how it "should be" and perceive all deviations from the "norm" as a threat. <...> [Parents] are worried about the weight of the child, the increase in his skills, [they] often ask, "when he will catch up." Unnecessary anxieties are similar to those in full-term children, there are just more of them: the chair is not the color, yesterday I added 30 grams in a day, and today only 25, I slept longer than usual, I could not fall asleep longer than usual, etc. ".
This is an understandable relationship, but sometimes it does not lead to very good results. Doctors even singled out such a phenomenon as the “vulnerable child syndrome”, which is caused by excessive protection of the child, in particular, if he was born prematurely. As a result, such children find it difficult to build relationships with peers, they have to miss school more often than they really need to, they develop anxiety and other physical and psychological problems arise.
Doctors even singled out such a phenomenon as the “vulnerable child syndrome”, which is caused by excessive protection of the child, in particular, if he was born prematurely. As a result, such children find it difficult to build relationships with peers, they have to miss school more often than they really need to, they develop anxiety and other physical and psychological problems arise.
Can premature babies be vaccinated?
Premature babies must be vaccinated, and not only according to the general calendar, but also additionally. “It should be taken into account that such children, in case of childhood infections, endure them much harder, it can be fatal for them, because vaccination is even more necessary for them,” Olga Evseichik explains. In addition, babies born before the 28th week do not have protection against certain diseases that should have been transmitted in utero from the mother. And those premature babies who were born after the 28th week will have less of this protection than if they were born at term. Some vaccines may protect these babies a little less because they produce fewer antibodies than full-term babies. But doctors agree that vaccination is still necessary. Sometimes you just need another shot later on over the calendar to get better protection.
Some vaccines may protect these babies a little less because they produce fewer antibodies than full-term babies. But doctors agree that vaccination is still necessary. Sometimes you just need another shot later on over the calendar to get better protection.
The UK recommends that these children be vaccinated eight weeks after birth. In the United States, it is not recommended to wait and is advised to be vaccinated according to chronological (not adjusted) age. In Russia, prematurity itself is not officially a contraindication. However, it is recommended to vaccinate from a month - “according to passport age, with all vaccines in usual doses after stabilization of the condition with adequate weight gain”, as indicated in the methodological recommendations of the Ministry of Health.
There are only a few differences in when certain vaccinations are given.
Hepatitis B virus
Children weighing from one and a half to two kilograms at birth and who have no visible diseases can be immediately vaccinated against hepatitis B in Russia. Or postpone vaccination for a month. In the US, the recommendations are similar.
Or postpone vaccination for a month. In the US, the recommendations are similar.
In other cases, if the child weighs less than two kilograms, you need to stabilize his condition or wait until he gains weight - then you can vaccinate against hepatitis B.
If the mother has a positive HBsAg test, regardless of the weight of the child, vaccination is needed on the first day (in the US, it is recommended to meet the first 12 hours).
Rotavirus
A vaccine against rotavirus infection is certainly needed for premature babies (although it is not on the main list of the Russian National calendar approved by the Ministry of Health). However, this is a live vaccine, and there is a theoretical risk that other children who are contraindicated for it and who are in the same intensive care unit may encounter the virus from the vaccine. This could end badly. Therefore, the child should receive the first dose at discharge (but not later than the 15th week of life).
BCG
This vaccination is contraindicated if the child weighs less than two kilograms. This is due to the fact that it is administered intradermally, while in children with low weight the skin is very thin, and it is technically impossible to vaccinate correctly. “Such children should be vaccinated upon discharge from the second stage, however, in practice, we encounter medical challenges in the vast majority of cases,” Olga Evseichik explains.
This is due to the fact that it is administered intradermally, while in children with low weight the skin is very thin, and it is technically impossible to vaccinate correctly. “Such children should be vaccinated upon discharge from the second stage, however, in practice, we encounter medical challenges in the vast majority of cases,” Olga Evseichik explains.
Respiratory syncytial virus
In this case, we are not talking about a vaccine, but about a drug that protects against respiratory syncytial virus in a different way. The drug palivizumab (in Russia it is sold under the sole commercial name Synagis) is a monoclonal antibody, that is, an antibody created using gene technology. When a conventional vaccine is administered, the body must develop antibodies to the virus or bacteria so that the next time it encounters a pathogen, the immune system responds quickly. Here, antibodies are introduced from the outside.
The Russian Union of Pediatricians recommends using this drug in premature babies in the first year of life and in some cases up to two years, and at the beginning of the seasonal spread of the respiratory syncytial virus (usually this is the cold season - in Russia they say that palivizumab should be administered every month from November to March).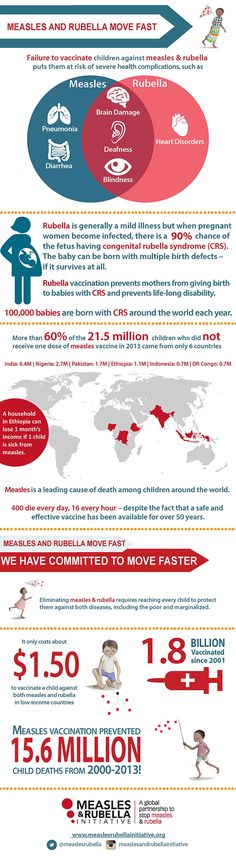 In some regions, the drug is administered free of charge.
In some regions, the drug is administered free of charge.
In the United States and Canada, recommendations for the use of palivizumab are narrower. This is probably due to its high cost.
Other dangerous viruses and bacteria
In many countries, all children, including premature babies, are recommended to be vaccinated against more diseases than indicated in the official Russian vaccination calendar. There are several reasons for this, and financial is one of them: what is included in the calendar should be provided "for free". However, the Union of Pediatricians of Russia has compiled an expanded “ideal vaccination schedule”, which includes everything an average child needs. In general, you can rely on these recommendations, however, the pediatrician is likely to make some adjustments depending on the individual characteristics of the child and the local epidemiological situation. Most likely, additional vaccines will be paid, however, in different regions, the calendar may be wider than the national one.