Vomiting during third trimester
When Morning Sickness Doesn't Go Away: Third Trimester Nausea
When Morning Sickness Doesn't Go Away: Third Trimester NauseaMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Sarah Bradley on July 30, 2020
We’re just gonna come right out and say it: morning sickness sucks. Like, it might actually be the single worst part of pregnancy other than the part where you have to push a human being out of you.
Plus, it has the most inaccurate name of anything ever because it does not just happen in the morning (seriously… who was in charge of this?).
The only saving grace here is that it’s a first trimester problem. Once you get through the first 12 or 13 weeks, you’re good to go, right?
Yeah, no. Sometimes morning sickness lasts well into the second trimester and, for some especially unfortunate pregnant souls, it can drag all the way into the third trimester, too.
Here’s what’s probably going on and what you can do to feel better (other than induce labor and get this nausea-provoking baby out of you, already).
If you’re nearing your due date and wondering why you’re still barfing up your breakfast, know that while most cases of morning sickness get better after the first trimester, some just don’t — and it doesn’t mean anything is wrong.
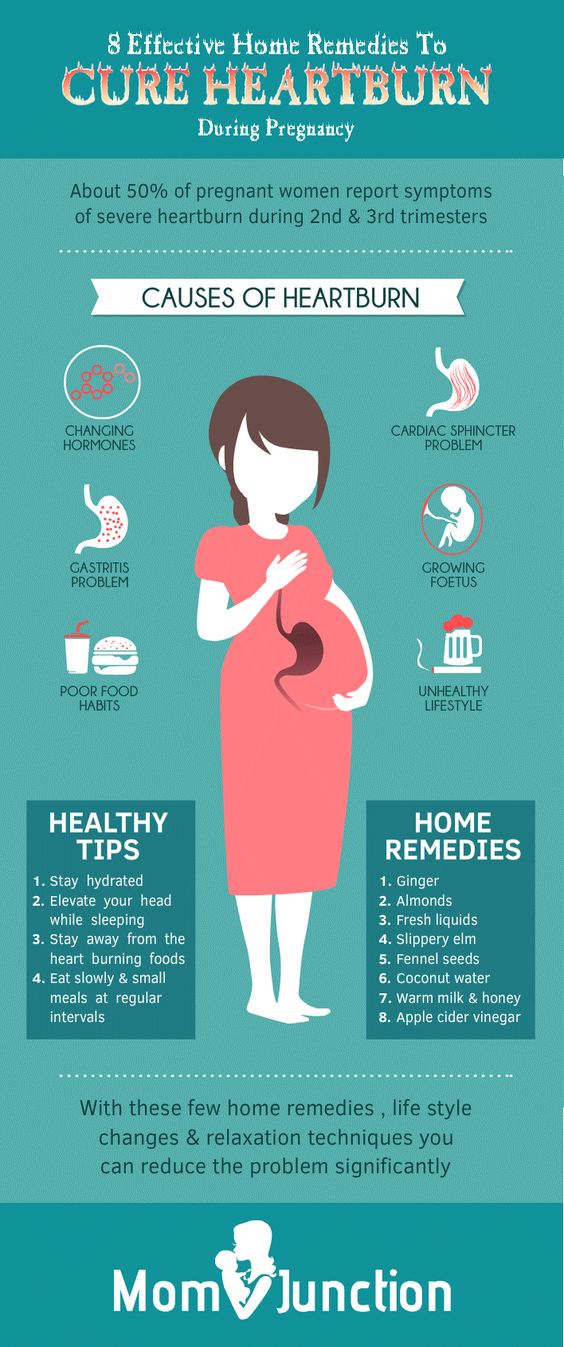
While your initial nausea might have been caused by the sudden change in hormones as your body adjusted to being pregnant, third trimester nausea may be caused by a variety of things:
- Your growing baby. You’re running out of room in your stomach as baby grows, which puts pressure on your digestive system. This can cause everything from constipation to heartburn to nausea.
- Your prenatal vitamin. Some people have trouble digesting the high amounts of iron in prenatal vitamins without GI distress. If your nausea never really went away or if you changed brands mid-pregnancy, it could be causing nausea.
- Your diet. Is baby craving chili peppers? Well, good for baby, but you’re the one suffering the ill effects of spicy, oily, and acid-based foods.
 Especially with less room in your stomach these days, foods that tend to be irritating to the GI tract can really do a number on you.
Especially with less room in your stomach these days, foods that tend to be irritating to the GI tract can really do a number on you. - Hormones, again. These do typically level out after the first trimester, but let’s face it: Pregnancy is a hormonal roller coaster because they’re constantly in flux. If your nausea comes and goes by the day, it might be due to the up-and-down nature of your hormones.
If you’ve felt sick during most of your pregnancy, continuing to have symptoms in the third trimester isn’t unusual and can probably be blamed on one of these things.
If feeling excessively nauseated during the third trimester is a new thing for you this pregnancy, you should check in with your doctor.
Your stomach upset could still be caused by your changing body or an external factor like diet. But nausea is also a symptom of a few serious pregnancy conditions. Both preeclampsia (a severe form of high blood pressure) and gestational liver problems, like HELLP syndrome, can cause nausea.
If you’re feeling nauseated during the third trimester, it’s probably a GI issue — everything is getting squished in there, causing your digestion to slow down.
You may also be constipated or have abdominal bloating or gas, or you might have symptoms of reflux, like heartburn and indigestion.
If your changing hormones are to blame, you may also be feeling super tired, just like you did in the first trimester. Pregnancy really is the gift that just keeps on giving, isn’t it?
Your third trimester nausea could also be paired up with loss of appetite, persistent vomiting, and difficulty losing weight. In that case, you might actually have hyperemeis gravidarium, an extreme form of morning sickness that often requires medical treatment.
For the most part, you can treat third trimester nausea the same way you did way back at week 8 of your pregnancy.
Focus on eating smaller, more frequent meals (to avoid becoming overly full) and cutting back on foods that are agitating your digestive system (like those buffalo-style potato chips you can’t stop craving).
You can also:
- sip ginger tea or nibble on ginger gummies
- avoid any triggering foods or odors
- suck on peppermint or lemon hard candies
- snack on carb-heavy foods, like pretzels and crackers
- get extra sleep
- take a B6 supplement (if approved by your doctor)
- make changes to your prenatal vitamin, like splitting doses, changing the timing of doses, or switching to a gummy instead of a capsule
If you’re nauseated all the time and none of these remedies help, contact your doctor. Also give them a call if you’re having persistent vomiting or trouble keeping food or fluids down, even if you think you’ve caught a run-of-the-mill stomach bug.
Pregnant people need to be careful not to get dehydrated, so your doctor may want to monitor your symptoms.
Sometimes you can feel nauseated when labor is getting closer, but you’re much more likely to have nausea during active labor or the transition phase of labor.
Instead of wondering if your queasy stomach is a sign that you’re approaching the Big Day, pay attention to more reliable signs of labor, like:
- loss of your mucus plug
- rupture of the amniotic sac
- back pain
- lightening
- diarrhea
- an increase in the severity and frequency of Braxton-Hicks contractions
Some of us are just unlucky enough to feel sick for 9 months, either intermittently or nonstop through all 3 trimesters.
But feeling nauseated 24/7 during the third trimester — especially if nothing helps alleviate it — is enough of a red flag to see your doctor for an exam. It could just be an unpleasant symptom you have to deal with until the end of pregnancy, but it’s always a good idea to rule out any issues.
Last medically reviewed on July 30, 2020
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chik Jwa S, et al. (2016). Validation of a food-frequency questionnaire for assessing vitamin intake of Japanese women in early and late pregnancy with and without nausea and vomiting. DOI:
10. 1017/jns.2016.14
1017/jns.2016.14 - HELLP syndrome. (2018).
rarediseases.info.nih.gov/diseases/8528/hellp-syndrome - Mukhtar F, et al. (2018). Nausea and vomiting during pregnancy and sikanjbeen lemooni — A review.
ijrar.org/papers/IJRAR1944281.pdf
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Sarah Bradley on July 30, 2020
related stories
When Will This Ever End? How Long Morning Sickness Lasts
The Peak of Your Morning Sickness
The 14 Best Foods to Eat When You’re Nauseous
Real Moms Share Unexpected Pregnancy Symptoms (That Your Best Friend Failed to Mention)
Treating Morning Sickness with Unisom and Vitamin B6
Read this next
When Will This Ever End? How Long Morning Sickness Lasts
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
If you're newly pregnant, you may be experiencing what seems like endless nausea and vomiting.
 Exactly how long does morning sickness last? Usually…
Exactly how long does morning sickness last? Usually…READ MORE
The Peak of Your Morning Sickness
Medically reviewed by Fernando Mariz, MD
Morning sickness is very common during pregnancy, but when does it peak? Learn about what to expect, and get tips on minimizing this type of nausea.
READ MORE
The 14 Best Foods to Eat When You’re Nauseous
By Elise Mandl, BSc, Msc, APD
Those with nausea seem to tolerate certain foods and drinks better than others. Here are the best foods and drinks for when you’re feeling nauseous.
READ MORE
Real Moms Share Unexpected Pregnancy Symptoms (That Your Best Friend Failed to Mention)
You think you’ve heard it all, from swollen feet to shiny hair, but there are certain pregnancy symptoms that don’t typically make the cut in…
READ MORE
Treating Morning Sickness with Unisom and Vitamin B6
Medically reviewed by Amy Richter, RD
Here’s the deal on morning sickness and whether it’s worth taking Unisom and vitamin B6 to try to make it go away.

READ MORE
Hyperemesis Gravidarum
Hyperemesis gravidarum (HG) is an extreme form of morning sickness that causes severe nausea and vomiting during pregnancy. Learn treatment options…
READ MORE
Ginger Tea in Pregnancy: Benefits, Safety, and Directions
By Lizzie Streit, MS, RDN, LD
Ginger has been linked to various health benefits, including nausea relief. This article reviews the effectiveness of ginger tea for relieving…
READ MORE
No Morning Sickness? You Don’t Need to Worry
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Morning sickness is so often discussed as a pregnancy symptom you may worry if you don't feel sick. Learn more about why you may not have morning…
READ MORE
Your Poop May Change During Pregnancy — Here’s How
Medically reviewed by Carolyn Kay, M.
 D.
D.Pregnancy poop may not be something you want to talk about — but it’s something you need to think about. Here are all the ways your bowel movements…
READ MORE
Welcome to Pregnancy Fatigue: The Most Tired You Have Ever Felt
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
You're not showing yet. You may have just seen the positive result on a pregnancy test. So it may surprise you that you feel so amazingly tired. Is…
READ MORE
When Morning Sickness Doesn't Go Away: Third Trimester Nausea
When Morning Sickness Doesn't Go Away: Third Trimester NauseaMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Sarah Bradley on July 30, 2020
We’re just gonna come right out and say it: morning sickness sucks. Like, it might actually be the single worst part of pregnancy other than the part where you have to push a human being out of you.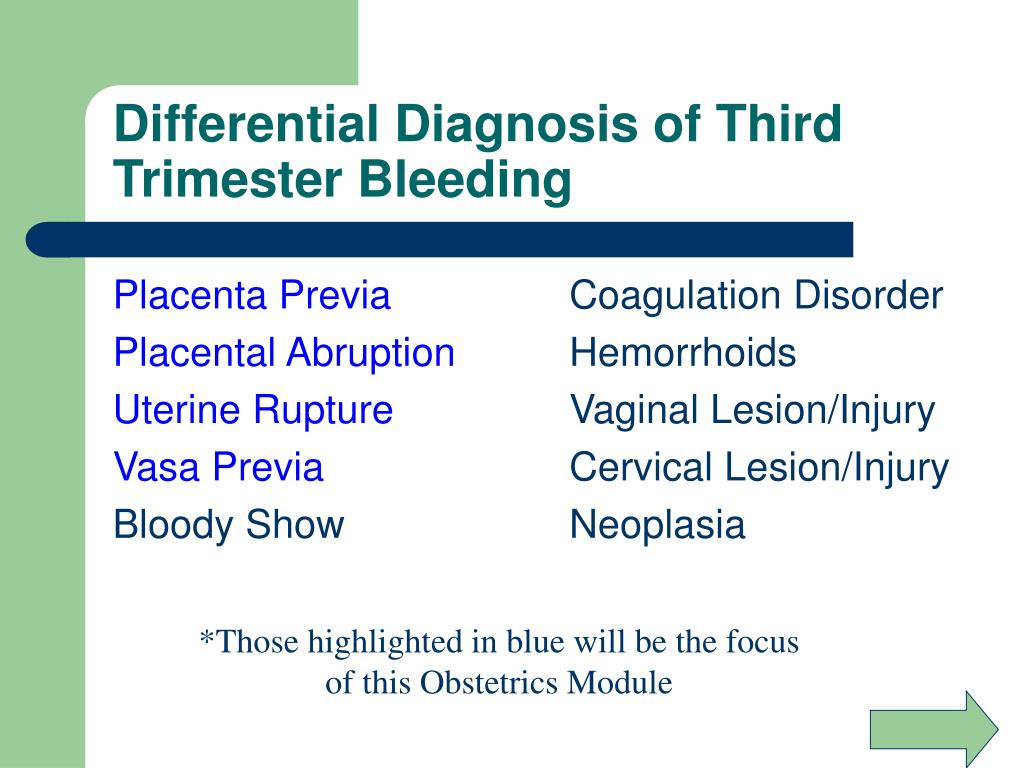
Plus, it has the most inaccurate name of anything ever because it does not just happen in the morning (seriously… who was in charge of this?).
The only saving grace here is that it’s a first trimester problem. Once you get through the first 12 or 13 weeks, you’re good to go, right?
Yeah, no. Sometimes morning sickness lasts well into the second trimester and, for some especially unfortunate pregnant souls, it can drag all the way into the third trimester, too.
Here’s what’s probably going on and what you can do to feel better (other than induce labor and get this nausea-provoking baby out of you, already).
If you’re nearing your due date and wondering why you’re still barfing up your breakfast, know that while most cases of morning sickness get better after the first trimester, some just don’t — and it doesn’t mean anything is wrong.
While your initial nausea might have been caused by the sudden change in hormones as your body adjusted to being pregnant, third trimester nausea may be caused by a variety of things:
- Your growing baby.
 You’re running out of room in your stomach as baby grows, which puts pressure on your digestive system. This can cause everything from constipation to heartburn to nausea.
You’re running out of room in your stomach as baby grows, which puts pressure on your digestive system. This can cause everything from constipation to heartburn to nausea. - Your prenatal vitamin. Some people have trouble digesting the high amounts of iron in prenatal vitamins without GI distress. If your nausea never really went away or if you changed brands mid-pregnancy, it could be causing nausea.
- Your diet. Is baby craving chili peppers? Well, good for baby, but you’re the one suffering the ill effects of spicy, oily, and acid-based foods. Especially with less room in your stomach these days, foods that tend to be irritating to the GI tract can really do a number on you.
- Hormones, again. These do typically level out after the first trimester, but let’s face it: Pregnancy is a hormonal roller coaster because they’re constantly in flux. If your nausea comes and goes by the day, it might be due to the up-and-down nature of your hormones.

If you’ve felt sick during most of your pregnancy, continuing to have symptoms in the third trimester isn’t unusual and can probably be blamed on one of these things.
If feeling excessively nauseated during the third trimester is a new thing for you this pregnancy, you should check in with your doctor.
Your stomach upset could still be caused by your changing body or an external factor like diet. But nausea is also a symptom of a few serious pregnancy conditions. Both preeclampsia (a severe form of high blood pressure) and gestational liver problems, like HELLP syndrome, can cause nausea.
If you’re feeling nauseated during the third trimester, it’s probably a GI issue — everything is getting squished in there, causing your digestion to slow down.
You may also be constipated or have abdominal bloating or gas, or you might have symptoms of reflux, like heartburn and indigestion.
If your changing hormones are to blame, you may also be feeling super tired, just like you did in the first trimester. Pregnancy really is the gift that just keeps on giving, isn’t it?
Pregnancy really is the gift that just keeps on giving, isn’t it?
Your third trimester nausea could also be paired up with loss of appetite, persistent vomiting, and difficulty losing weight. In that case, you might actually have hyperemeis gravidarium, an extreme form of morning sickness that often requires medical treatment.
For the most part, you can treat third trimester nausea the same way you did way back at week 8 of your pregnancy.
Focus on eating smaller, more frequent meals (to avoid becoming overly full) and cutting back on foods that are agitating your digestive system (like those buffalo-style potato chips you can’t stop craving).
You can also:
- sip ginger tea or nibble on ginger gummies
- avoid any triggering foods or odors
- suck on peppermint or lemon hard candies
- snack on carb-heavy foods, like pretzels and crackers
- get extra sleep
- take a B6 supplement (if approved by your doctor)
- make changes to your prenatal vitamin, like splitting doses, changing the timing of doses, or switching to a gummy instead of a capsule
If you’re nauseated all the time and none of these remedies help, contact your doctor. Also give them a call if you’re having persistent vomiting or trouble keeping food or fluids down, even if you think you’ve caught a run-of-the-mill stomach bug.
Also give them a call if you’re having persistent vomiting or trouble keeping food or fluids down, even if you think you’ve caught a run-of-the-mill stomach bug.
Pregnant people need to be careful not to get dehydrated, so your doctor may want to monitor your symptoms.
Sometimes you can feel nauseated when labor is getting closer, but you’re much more likely to have nausea during active labor or the transition phase of labor.
Instead of wondering if your queasy stomach is a sign that you’re approaching the Big Day, pay attention to more reliable signs of labor, like:
- loss of your mucus plug
- rupture of the amniotic sac
- back pain
- lightening
- diarrhea
- an increase in the severity and frequency of Braxton-Hicks contractions
Some of us are just unlucky enough to feel sick for 9 months, either intermittently or nonstop through all 3 trimesters.
But feeling nauseated 24/7 during the third trimester — especially if nothing helps alleviate it — is enough of a red flag to see your doctor for an exam. It could just be an unpleasant symptom you have to deal with until the end of pregnancy, but it’s always a good idea to rule out any issues.
It could just be an unpleasant symptom you have to deal with until the end of pregnancy, but it’s always a good idea to rule out any issues.
Last medically reviewed on July 30, 2020
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chik Jwa S, et al. (2016). Validation of a food-frequency questionnaire for assessing vitamin intake of Japanese women in early and late pregnancy with and without nausea and vomiting. DOI:
10.1017/jns.2016.14 - HELLP syndrome. (2018).
rarediseases.info.nih.gov/diseases/8528/hellp-syndrome - Mukhtar F, et al.
 (2018). Nausea and vomiting during pregnancy and sikanjbeen lemooni — A review.
(2018). Nausea and vomiting during pregnancy and sikanjbeen lemooni — A review.
ijrar.org/papers/IJRAR1944281.pdf
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Sarah Bradley on July 30, 2020
related stories
When Will This Ever End? How Long Morning Sickness Lasts
The Peak of Your Morning Sickness
The 14 Best Foods to Eat When You’re Nauseous
Real Moms Share Unexpected Pregnancy Symptoms (That Your Best Friend Failed to Mention)
Treating Morning Sickness with Unisom and Vitamin B6
Read this next
When Will This Ever End? How Long Morning Sickness Lasts
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
If you're newly pregnant, you may be experiencing what seems like endless nausea and vomiting.
 Exactly how long does morning sickness last? Usually…
Exactly how long does morning sickness last? Usually…READ MORE
The Peak of Your Morning Sickness
Medically reviewed by Fernando Mariz, MD
Morning sickness is very common during pregnancy, but when does it peak? Learn about what to expect, and get tips on minimizing this type of nausea.
READ MORE
The 14 Best Foods to Eat When You’re Nauseous
By Elise Mandl, BSc, Msc, APD
Those with nausea seem to tolerate certain foods and drinks better than others. Here are the best foods and drinks for when you’re feeling nauseous.
READ MORE
Real Moms Share Unexpected Pregnancy Symptoms (That Your Best Friend Failed to Mention)
You think you’ve heard it all, from swollen feet to shiny hair, but there are certain pregnancy symptoms that don’t typically make the cut in…
READ MORE
Treating Morning Sickness with Unisom and Vitamin B6
Medically reviewed by Amy Richter, RD
Here’s the deal on morning sickness and whether it’s worth taking Unisom and vitamin B6 to try to make it go away.

READ MORE
Hyperemesis Gravidarum
Hyperemesis gravidarum (HG) is an extreme form of morning sickness that causes severe nausea and vomiting during pregnancy. Learn treatment options…
READ MORE
Ginger Tea in Pregnancy: Benefits, Safety, and Directions
By Lizzie Streit, MS, RDN, LD
Ginger has been linked to various health benefits, including nausea relief. This article reviews the effectiveness of ginger tea for relieving…
READ MORE
No Morning Sickness? You Don’t Need to Worry
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Morning sickness is so often discussed as a pregnancy symptom you may worry if you don't feel sick. Learn more about why you may not have morning…
READ MORE
Your Poop May Change During Pregnancy — Here’s How
Medically reviewed by Carolyn Kay, M.
 D.
D.Pregnancy poop may not be something you want to talk about — but it’s something you need to think about. Here are all the ways your bowel movements…
READ MORE
Welcome to Pregnancy Fatigue: The Most Tired You Have Ever Felt
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
You're not showing yet. You may have just seen the positive result on a pregnancy test. So it may surprise you that you feel so amazingly tired. Is…
READ MORE
Toxemia, Intestinal Problems, and Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 1–13 weeks | 900 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid reflux | Constipation Acid Office 9000 9000 9000 9000 Flatulence Constipation Heartburn Violation of the outflow of bile Hemorrhoids |
The Atlas Genetic Test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.

Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a vacation in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Blood or mucus stools;
- Sudden weight loss;
- Pain in the abdomen;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially in the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve bowel movements and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for future pregnancy and reduce the risk of digestive problems.
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems in the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.
 S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy
S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy - Robyn Horsager-Boehrer, M.D., UT Southwestern Medical Center, Should pregnant moms be concerned about gastroenteritis?, 2018
- International Foundation for Gastrointestinal Disorders, Pregnancy and Irritable Bowel Syndrome, 2016
- NHS Vomiting and morning sickness in pregnancy
- NHS, Severe vomiting in pregnancy
- Lindsey J Wegrzyniak et al., Treatment of Hyperemesis Gravidarum, 2012
- Karen Miles, Diarrhea during pregnancy, 2020
- Cleveland Clinic, Diarrhea
- You and your hormones, Progesterone
- Traci C. Johnson, MD, Pregnancy, Bloating, 2020
What is preeclampsia? - ADONIS Medical Center in Kyiv
Preeclampsia, or late toxicosis, is a complication of pregnancy that develops in the 2nd and 3rd trimesters. It is possible to suspect its development in the early stages by the formation of edema and increased pressure. At the same time, the diagnosis can be confirmed or refuted only by the results of blood and urine tests.
At the same time, the diagnosis can be confirmed or refuted only by the results of blood and urine tests.
Late toxicosis, compared with early, develops infrequently. According to the World Health Organization, its symptoms occur in an average of 8% of pregnant women. At the same time, in the territory of the CIS countries, this figure reaches 10-17%.
Severe preeclampsia is rare, but the risk of such complications cannot be ignored. Unlike early toxicosis, late toxicosis poses a serious threat to the life of the mother and child. It is one of the main causes of perinatal morbidity and maternal mortality.
Although the consequences of preeclampsia seem frightening, do not worry ahead of time. First, edema and hypertension can occur for other reasons. Secondly, with the timely diagnosis of late toxicosis and the selection of the correct therapy, a woman can fully bear the pregnancy and give birth to a healthy baby.
At what time does late toxicosis begin? It is believed that the early onset of preeclampsia is associated with a severe course and often leads to premature birth, including by caesarean section.
Causes of late toxicosis in pregnant women
What exactly provokes the development of preeclampsia in pregnant women has not been established. There are several theories that have a different number of supporters, but none of them allows you to accurately determine which woman will develop late toxicosis and which will not.
At risk are pregnant women with:
- Hypertension;
- Diseases of the kidneys, liver, biliary tract, thyroid gland, adrenal glands, lungs and/or heart;
- Violation of fat metabolism and obesity;
- Anemia;
- Fetal growth retardation;
- Rh incompatibility;
- Multiple pregnancy;
- Birth or abortion within the last two years;
- Under the age of 19 or over 36.
The likelihood of developing late toxicosis increases against the background of chronic diseases. However, even if there are several risk factors, it cannot be said with certainty that there will be a complication.
How preeclampsia manifests itself
When preeclampsia develops in a woman, first there is a spasm of all vessels and a violation of blood circulation, as well as its clotting and fluidity. Because of this, hypoxia can develop, affecting the functioning of the heart, kidneys, liver, brain and placenta. As a result, dystrophic changes may occur in these organs.
There are 4 stages of preeclampsia:
- Edema;
- Nephropathy;
- Preeclampsia;
- Eclampsia.
At the first stage, late toxicosis is manifested by edema on the legs, arms, abdomen and in the face and neck. Most often, they do not provoke a significant deterioration in the well-being of a pregnant woman or the development of severe complications in her. In addition, with timely therapy, the following forms of preeclampsia develop in no more than 20% of cases.
With nephropathy, in addition to edema, hypertension and impaired renal function appear, which is determined by the release of protein in the urine.
Preeclampsia is the third stage of preeclampsia, which develops in only 5% of pregnant women. It is characterized by changes in the central nervous system that cause nausea, vomiting, headache, and other symptoms.
The most difficult stage of late toxicosis is eclampsia. With its development, pathological disorders are aggravated, and, in addition to the listed symptoms, the woman also has convulsions, a sharp increase in pressure and the risk of stroke.
Late toxicosis may result in:
- Severe edema;
- Hypertension;
- Disorders of the functions of the kidneys, liver and other organs;
- Detachment of the placenta, leading to fetal hypoxia, slowing down its development, premature birth and perinatal pathologies.
In severe preeclampsia, the condition of a pregnant woman may become critical.
Features of preeclampsia treatment
For the diagnosis of preeclampsia, a number of laboratory blood and urine tests are prescribed, ultrasound is performed, an examination of the fundus and, if necessary, other examinations.