Little raised bumps on hands
Pictures, Types, Causes, and Treatment
Raised skin bumps are very common, and in most cases, they’re harmless. They can result from a number of conditions, including:
- infections
- allergic reactions
- skin disorders
- skin cancer
Skin bumps can vary in appearance and number depending on the cause. They may be the same color as your skin or a different color. They may be itchy, large, or small. Some can be hard, while others can feel soft and movable.
Most skin bumps do not need treatment. However, you should speak with a doctor if your bumps are causing discomfort. You should also call a doctor if you’re concerned about any changes in your bumps or in the overall condition of your skin.
Many conditions can cause raised bumps to appear on the skin. Here’s a list of 25 possible causes.
Warning: Graphic images ahead.
Acne
- commonly located on the face, neck, shoulders, chest, and upper back
- breakouts on the skin composed of blackheads, whiteheads, pimples, or deep, painful cysts and nodules
- may leave scars or darken the skin if untreated
Read the full article on acne.
Cold sore
- red, painful, fluid-filled blister that appears near the mouth and lips
- affected area will often tingle or burn before the sore is visible
- may be accompanied by mild, flu-like symptoms, such as low fever, body aches, and swollen lymph nodes
Read the full article on cold sores.
Corns and calluses
- small, round circles of thickened skin with a painful, horn-like central area of hardened tissue
- commonly found on the tops and sides of the toes and on the soles of the feet
- caused by friction and pressure
Read the full article on corns and calluses.
Skin tags
- skin growths that can become up to half an inch long
- same color as your skin or slightly darker
- most likely caused by friction
- commonly found near the neck, armpits, breasts, groin, stomach, or eyelids
Read the full article on skin tags.
Nodule
- small to medium growth that may be filled with tissue, fluid, or both
- usually wider than a pimple and may look like a firm, smooth elevation under the skin
- usually harmless, but may cause discomfort if it presses on other structures
- nodules may also be located deep inside the body where you cannot see or feel them
Read the full article on nodules.
Impetigo
- common in babies and children
- irritating rash and fluid-filled blisters that pop easily and form a honey-colored crust
- rash is often located in the area around the mouth, chin, and nose
Read the full article on impetigo.
Molluscum contagiosum
- bumps that may appear in a patch of up to 20
- small, shiny, and smooth
- flesh-colored, white, or pink
- firm and dome-shaped with a dent or dimple in the middle
Read the full article on molluscum contagiosum.
Lipoma
- soft to the touch and moves easily if prodded with your finger
- small, just under the skin, and pale or colorless
- commonly located in the neck, back, or shoulders
- only painful if it presses on a nerve
Read the full article on lipoma.
Cyst
- slow-growing bump under the skin that has a smooth surface
- can be large or small and is usually painless
- typically not a problem unless it’s infected, very large, or growing in a sensitive area
- some grow deep inside your body where you can’t see or feel them
Read the full article on cysts.
Wart
- caused by many different types of a virus called human papillomavirus (HPV)
- may be found on the skin or mucous membranes
- may occur as one wart or in groups
- contagious and may be passed to others
Read the full article on warts.
Actinic keratosis
- typically less than 2 centimeters (cm), or about the size of a pencil eraser
- thick, scaly, or crusty skin patch
- appears on parts of the body that receive a lot of sun exposure (hands, arms, face, scalp, and neck)
- usually pink in color but can have a brown, tan, or gray base
Read the full article on actinic keratosis.
Basal cell carcinoma
- raised, firm, and pale areas that may resemble a scar
- dome-like, pink or red, shiny, and pearly areas that may have a sunk-in center, like a crater
- visible blood vessels on the growth
- easy bleeding or oozing wound that doesn’t seem to heal, or heals and then reappears
Read the full article on basal cell carcinoma.
Squamous cell carcinoma
- often occurs in areas exposed to ultraviolet (UV) radiation, such as the face, ears, and back of the hands
- scaly, reddish patch of skin that progresses to a raised bump and continues to grow
- growth that bleeds easily and doesn’t heal, or heals and then reappears
Read the full article on squamous cell carcinoma.
Melanoma
- the most serious form of skin cancer, more common in people with lighter skin tones
- mole anywhere on the body that has irregularly shaped edges, asymmetrical shape, and multiple colors
- mole that has changed color or gotten bigger over time
- usually larger than a pencil eraser
Read the full article on melanoma.
Boils
- bacterial or fungal infection of a hair follicle or oil gland
- can appear anywhere on the body but are most common on the face, neck, armpit, and buttock
- red, painful, raised bump with a yellow or white center
- may rupture and weep fluid
Read the full article on boils.
Bullae
- clear, watery, fluid-filled blister that is greater than 1 cm in size
- can be caused by friction, contact dermatitis, and other skin disorders
- if clear liquid turns milky, there might be an infection
Read the full article on bullae.
Contact dermatitis
- appears hours to days after contact with an allergen
- rash has visible borders and appears where your skin touched the irritating substance
- skin is itchy, red, scaly, or raw
- blisters that weep, ooze, or become crusty
Read the full article on contact dermatitis.
Cherry angioma
- common skin growth that can be found anywhere on the body but is most likely to be seen on the torso, arms, legs, and shoulders
- more common in people over age 30
- small, bright red circular or oval spots that may be raised or smooth and bleed if rubbed or scratched
- generally harmless but may require removal if they’re in problem areas
Read the full article on cherry angioma.
Keloids
- symptoms occur at the site of a previous injury
- lumpy or rigid area of skin that may be painful or itchy
- area is flesh-colored, pink, or red
Read the full article on keloids.
Keratosis pilaris
- common skin condition that’s most often seen on the arms and legs but might also occur on the face, buttocks, and torso
- often clears up on its own by age 30
- patches of skin that appear bumpy, slightly red, and feel rough
- may get worse in dry weather
Read the full article on keratosis pilaris.
Seborrheic keratoses
- common, harmless skin growth that is usually seen in older adults
- can be located anywhere on the body except for the palms of the hands and soles of the feet
- round, oval, dark-colored growth with a “stuck-on” appearance
- raised and bumpy with a waxy feel
Read the full article on seborrheic keratoses.
Chickenpox
- clusters of itchy, red, fluid-filled blisters in various stages of healing all over the body
- accompanied by fever, body aches, sore throat, and loss of appetite
- remains contagious until all blisters have crusted over
Read the full article on chickenpox.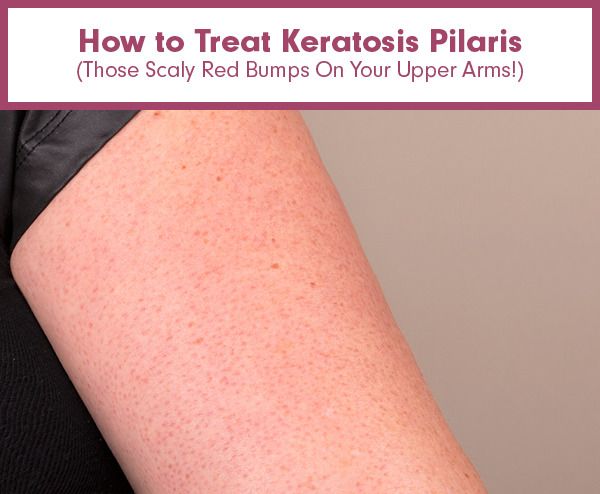
MRSA (staph) infection
This condition is considered a medical emergency. Urgent care may be required.
- an infection caused by a type of Staphylococcus, or staph, bacteria that is resistant to many different antibiotics
- causes an infection when it enters through a cut or scrape on the skin
- skin infection that often looks like a spider bite, with a painful, raised, red pimple that may drain pus
- needs to be treated with powerful antibiotics and can lead to more dangerous conditions like cellulitis or blood infection
Read the full article on MRSA (staph) infection.
Scabies
- symptoms may take 4 to 6 weeks to appear
- extremely itchy rash that may be pimply, made up of tiny blisters, or scaly
- raised white or flesh-colored lines
Read the full article on scabies.
Strawberry nevus
- red or purplish raised mark, commonly located on the face, scalp, back, or chest
- appears at birth or in very young children
- gradually gets smaller or disappears as the child ages
Read the full article on strawberry nevus.
The most common causes of raised skin bumps are harmless and do not require medical treatment unless you have discomfort. Here are some of the possible reasons for raised skin bumps:
- Acne is the most common skin condition in the United States, according to the American Academy of Dermatology. It causes skin bumps that can range from very small and painless to large and painful. The bumps are usually accompanied by redness and swelling.
- Boils are infected hair follicles that look like red, raised bumps on the skin. They can be painful, but they eventually go away once they burst and release fluid.
- Bullae are raised, fluid-filled bumps that can result from friction, or conditions like contact dermatitis and chickenpox.
- Cherry angiomas are common skin growths that can form on most areas of the body. They develop when blood vessels clump together and create a raised, bright-red bump under or on the skin.

- Cold sores are red, fluid-filled bumps that form around the mouth or other areas of the face and can burst. They’re caused by a common virus called herpes simplex.
- Contact dermatitis is an allergic skin reaction that produces an itchy, red skin rash. The rash may consist of raised, red bumps that ooze, drain, or crust.
- Corns or calluses are rough, thickened areas of skin. They’re most often found on the feet and hands.
- Cysts are growths that contain fluid, air, or other substances. They develop under the skin in any part of the body. They feel like a small ball and can usually be moved around slightly.
- Keloids are smooth, raised growths that form around scars. They’re most commonly found on the chest, shoulders, and cheeks.
- Keratosis pilaris is a skin condition marked by an overgrowth of a protein called keratin. It causes small bumps around hair follicles on the body.

- Lipomas are collections of fatty tissue under the skin and are often painless. They usually form on the neck, back, or shoulders.
- Molluscum contagiosum are small, flesh-colored bumps with a dimple in the center that often form in all parts of the body. They can arise from skin-to-skin contact with someone affected with them.
- Nodules result from growth of abnormal tissue, and can appear on the skin in common areas like the armpits, groin, and head and neck region.
- Seborrheic keratoses are round, rough spots on the surface of the skin. They can affect many areas of the body, including the chest, shoulders, and back. They may be skin-colored, brown, or black.
- Skin tags are small, fleshy flaps of skin. They usually grow on the neck or in the armpits. They may be the same color as the skin or slightly darker.
- Strawberry nevus is a red birthmark also known as a hemangioma.
 They are most common in young children and usually disappear by age 10.
They are most common in young children and usually disappear by age 10. - Warts are raised, rough bumps caused by the human papillomavirus (HPV). They typically develop on the hands and feet. They may be skin-colored, pink, or slightly brown.
Less commonly, raised skin bumps are caused by more serious conditions that require treatment. Certain bacterial and viral infections cause bumps and will only get worse if they go undiagnosed and untreated. These serious conditions include:
- chickenpox, a common childhood virus characterized by red, itchy bumps that form all over the body
- impetigo, a bacterial skin infection common in young children that is highly contagious and results in reddish blisters that ooze and develop a honey-colored crust
- MRSA (staph) infection, an illness triggered by a staph bacteria that commonly lives on the skin, causing a swollen, painful bump with a white center
- scabies, a skin infestation caused by a tiny mite called Sarcoptes scabiei, producing an itchy, pimple-like rash
Other types of raised skin bumps can be caused by skin cancer. There are several types of skin cancer, all requiring medical management and treatment:
There are several types of skin cancer, all requiring medical management and treatment:
- Actinic keratosis is a precancerous skin condition characterized by scaly, crusty spots on areas of sun-exposed skin, such as hands, arms, or face. These spots are typically brown, gray, or pink. The affected area may itch or burn.
- Basal cell carcinoma is a form of cancer that affects the top layer of skin. It produces painful bumps that bleed in the early stages. The associated bumps appear on sun-exposed skin and may be discolored, shiny, or scar-like.
- Squamous cell carcinoma is a type of skin cancer that begins in the squamous cells. These cells make up the outermost layer of skin. The condition causes scaly, red patches and raised sores to develop on the skin. These abnormal growths often form in areas exposed to ultraviolet radiation.
- Melanoma is the least common but most serious form of skin cancer.
 It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
Most skin bumps are harmless and aren’t cause for concern. However, you should see your doctor if:
- skin bumps change or worsen in appearance, or last for a long time
- you are in pain or they cause discomfort
- you don’t know the cause of the bumps
- you suspect you have an infection or skin cancer
Your doctor will perform a physical examination and inspect the skin bumps. Expect to answer questions about your bumps, medical history, and lifestyle habits.
Your doctor may also perform a skin biopsy to test if the skin bump is cancerous. This procedure involves taking a small sample of skin tissue from the affected area for analysis. Depending on the results, your doctor may refer you to a dermatologist or other specialist for further evaluation.
The Healthline FindCare tool can provide options in your area if you don’t already have a doctor.
Removal
Treatment for raised skin bumps depends on the underlying cause. Most of the common causes of skin bumps are harmless, so you probably won’t need treatment. However, if your skin bumps are bothering you, you might be able to have them removed for cosmetic reasons.
For example, a dermatologist can remove skin tags or warts by freezing them off. A dermatologist can also surgically remove certain skin bumps, including cysts and lipomas. Other bumps that are itchy or irritated may be treated with topical ointments and creams.
If your doctor finds that your skin bumps are cancerous or precancerous, they will most likely remove the bumps completely. You will also need to attend regular follow-up appointments so your doctor can check the area and make sure the cancer doesn’t come back.
Medication
In cases where additional medical treatment is required, your doctor will prescribe medications that can help eliminate your skin bumps and the underlying cause.
For a bacterial infection, such as MRSA, you may need antibiotics. For a viral infection, such as chickenpox, your doctor may recommend over-the-counter medications and home treatments. Some viral infections, such as herpes, can’t be cured. However, your doctor can give you medications to ease symptoms.
For most skin bumps, the long-term outlook is excellent. The majority of bumps are caused by harmless, temporary conditions that don’t require treatment. If skin bumps are caused by an infection or long-term condition, timely medical treatment should either clear it up or effectively ease the symptoms. The outlook is also good when skin cancer is caught early. However, frequent follow-ups will be necessary to ensure the cancer doesn’t return or grow. The outlook for more advanced forms of skin cancer varies with each situation.
What’s Causing Your Itchy Skin? (with Pictures)
Itchiness can be generalized (all over the body) or localized to one small region or spot.
The possible causes are numerous and varied. Itching may be a result of something very serious, such as:
- kidney failure
- liver disease
- thyroid disease
- lymphoma
- diabetes (uncommon)
Itchiness can also come from something less severe, such as:
- dry skin
- allergies
- insect bites (more likely)
Skin conditions
Many common skin conditions can cause itchy skin. The following can affect any area of skin on the body:
- Dermatitis. Dermatitis is an inflammation of the skin.
- Eczema. This is a chronic skin disorder that includes itchy, scaly rashes.
- Psoriasis. This autoimmune disease causes skin discoloration and irritation, usually in the form of plaques.
- Dermatographia. With dermatographia, pressure on the skin leads to elevated levels of histamine that cause a raised, red, itchy rash.
- Hives.
 These are itchy, raised, discolored welts on the skin that are usually caused by an allergic reaction.
These are itchy, raised, discolored welts on the skin that are usually caused by an allergic reaction. - Ringworm. Ringworm is a fungal infection of the skin.
- Shingles. This infection is caused by the same virus that causes chickenpox.
- Allergies. Skin can become itchy due to an allergic reaction to something you ate or touched.
A few causes of itchy skin that are less common include:
- Bullous pemphigoid. This is a blister-like skin issue caused by friction, viruses, and more.
- Dermatitis herpetiformis. This itchy rash is often caused by gluten intolerance or celiac disease.
- Lichen planus. A skin rash triggered by the immune system, lichen planus may be caused by infections, genetics, stress, allergens, and more.
- Cutaneous lymphoma. This is a cancer that occurs in the lymph system.
- Scleroderma.
 This autoimmune disorder affects the skin.
This autoimmune disorder affects the skin.
Infections that cause itching include:
- chickenpox
- measles
- fungal rashes
- mites, including bed bugs
- lice
- pinworms
- scabies
- parasites such as filariasis and trichinosis
- HIV
- parvovirus (hand foot and mouth)
Irritants and allergens
There are many substances that irritate the skin and make it itchy.
Some plants and insects produce substances that cause itching, including:
- poison ivy
- poison oak
- mosquitoes
Some people get itchy when in contact with:
- wool
- perfumes
- certain soaps or dyes
- chemicals
Allergies can irritate the skin as well, including allergies to:
- certain foods
- latex
- antifungals
- heat and cold exposure
- aspirin and other medications
Internal disorders
Some internal diseases that may be very serious cause itching. The following diseases may cause generalized itching, but the skin usually appears typical:
The following diseases may cause generalized itching, but the skin usually appears typical:
- bile duct obstruction
- liver failure
- cholestasis
- delusional parasitosis
- peripheral neuropathy
- HIV
- cirrhosis
- anemia
- leukemia
- thyroid disease
- lymphoma
- kidney failure
Nervous system conditions
Other diseases can cause itching as well, especially those that affect the nerves. These include:
- diabetes
- multiple sclerosis
- shingles
- neuropathy
- brachioradial pruritus
- notalgia paresthetica
- meralgia
- inflammatory demyelinating polyneuropathy
- trigeminal trophic syndrome
Medications
The following medications often cause rashes and widespread itching:
- antifungals
- antibiotics, especially sulfa-based antibiotics
- pain relievers that are categorized as narcotics
- anticonvulsant medications
- aspirin
- B vitamins
- quinidine
- nitrates
- rifampin
- vancomycin
Pregnancy
Some pregnant people experience itching when pregnant. The National Health Service (NHS) says that it usually occurs on the abdomen. Sometimes this is due to a preexisting condition, such as eczema, that is made worse by the pregnancy.
The National Health Service (NHS) says that it usually occurs on the abdomen. Sometimes this is due to a preexisting condition, such as eczema, that is made worse by the pregnancy.
Some causes of itching in pregnancy include:
- pruritic urticarial papules
- prurigo of pregnancy (common in second half of pregnancy)
- pemphigoid gestationis (uncommon)
- intrahepatic cholestasis of pregnancy (uncommon)
There are many reasons your skin could itch. Here is a list of possible causes.
Dry skin
- Some symptoms include scaling, itching, and cracking.
- According to the American Academy of Dermatology (AAD), it can be caused by outdoor temperature, certain medications, smoking, vitamin deficiencies, and more.
- It can often be solved with lifestyle changes.
Read full article on dry skin.
Food allergy
This condition is considered a medical emergency. Urgent care may be required.
- This can occur when your immune system reacts inappropriately to common substances found in foods or drinks.

- The symptoms range from mild to severe, according to the NHS, and include sneezing, itchy eyes, swelling, rash, hives, stomach cramps, nausea, vomiting, and difficulty breathing.
- Depending on your immune system’s response, symptoms may occur minutes to hours after consuming a food that causes an allergic reaction.
- Common allergy trigger foods include cow’s milk, eggs, peanuts, fish, shellfish, tree nuts, wheat, and soy.
Read full article on food allergies.
Candida
Share on PinterestCandida rash in the skin fold of the buttocks. Nau Nau/Shutterstock
- The Centers for Disease Control and Prevention (CDC) says that this usually occurs in skin folds, such as the armpits, buttocks, under breasts, and between fingers and toes.
- It often begins with an itching, stinging, and burning discolored rash with wet appearance and dry crusting at the edges.
- It often progresses to cracked and sore skin with blisters and pustules that may become infected with bacteria.

Read full article on candida.
Biliary (bile duct) obstruction
This condition is considered a medical emergency. Urgent care may be required.
- It’s most commonly caused by gallstones, but it may also be caused by injury to the liver or gallbladder, inflammation, tumors, infections, cysts, or liver damage.
- Symptoms may include yellowing of the skin or eyes, extremely itchy skin without rash, light-colored stools, and very dark urine.
- It may cause pain in the upper right side of the abdomen, nausea, vomiting, and fever.
- An obstruction can cause serious infection that requires urgent medical attention.
Read full article on biliary (bile duct) obstruction.
Cirrhosis
Share on PinterestBy James Heilman, MD via Wikimedia Commons
- The National Institute of Diabetes and Digestive and Kidney Diseases says that symptoms can include diarrhea, decreased appetite and weight loss, and swelling belly.

- A person with cirrhosis may experience easy bruising and bleeding.
- Small, spider-shaped blood vessels may be visible underneath the skin.
- Other symptoms may include yellowing of the skin or eyes and itchy skin.
Read full article on cirrhosis.
Ragweed allergy
- Itchy, watery eyes are primary symptoms.
- Other symptoms may include a scratchy or sore throat.
- Runny nose, sinus pressure, congestion, and sneezing are also common.
Read full article on ragweed allergies.
Diaper rash
Share on PinterestDiaper dermatitis in an infant. lavizzara/Shutterstock
- The AAD says this rash is located on areas that have contact with a diaper.
- The skin often looks red, wet, and irritated.
- The skin is often warm to the touch.
Read full article on diaper rash.
Allergic reaction
Share on PinterestRed, raised bumpy rash on the forearms from a contact irritant causing contact dermatitis. vvoe/Shutterstock
vvoe/Shutterstock
This condition is considered a medical emergency. Urgent care may be required.
- These rashes occur when your immune system reacts to allergens on the skin, according to the NHS.
- Itchy, raised welts can appear minutes to hours after skin contact with an allergen.
- Symptoms may include a red, itchy, scaly rash that can appear hours to days after skin contact with an allergen.
- Severe and sudden allergic reactions may cause swelling and difficulty breathing that require emergency attention.
Read full article on allergic reactions.
Athlete’s foot
Share on PinterestDry flaky skin between the toes caused by tinea pedis (athlete’s foot). Yopan90/Shuttertsock
Share on PinterestRed rash with scaly skin and skin maceration between the toes caused by tinea pedis (athlete’s foot) Zay Nyi Nyi/Shutterstock
- The NHS says that symptoms include itching, stinging, and burning between the toes or on the soles of feet.

- There may be blisters on the feet that itch.
- A person may have discolored, thick, and crumbly toenails.
- There may be raw skin on the feet.
Read full article on athlete’s foot.
Contact dermatitis
Share on PinterestRedness and inflammation on the lower abdomen from metal belt buckle causing contact dermatitis. RiverNile/Shuttertsock
- According to the NHS, it appears hours to days after contact with an allergen.
- The rash has visible borders and appears where your skin touched the irritating substance.
- The skin is often itchy, discolored, scaly, or raw.
- A person may experience blisters that weep, ooze, or become crusty.
Read full article on contact dermatitis.
Flea bites
Share on PinterestFlea bites of the lower leg causing red bumps and scabbing. Angela Hampton Picture Library / Alamy Stock Photo
- They are usually located in clusters on the lower legs and feet.

- The bites can be itchy, and look like a red bump surrounded by a red/discolored halo.
- The symptoms begin immediately after being bitten.
Read full article on flea bites.
Hives
Share on Pinterest Created by Samuel Freire da Silva, M.D. in homage to The Master And Professor Delso Bringel Calheiros. Image obtained from Dermatology Atlas
Share on Pinterest Dermatology11/Shutterstock
- According to the American College of Allergy, Asthma, and Immunology, hives are itchy, raised welts that occur after exposure to an allergen.
- They can be red, warm, and mildly painful to the touch.
- They can be small, round, and ring shaped, or large and randomly shaped.
Read full article on hives.
Allergic eczema
Share on PinterestGabdrakipova Dilyara/Shutterstock
- The National Eczema Association says that this skin issue may resemble a burn.
- It is often found on hands and forearms.
- The skin is often itchy, discolored, scaly, or raw.

- A person may experience blisters that weep, ooze, or become crusty.
Read full article on allergic eczema.
Rashes
Share on PinterestArkom Suvarnasiri/Shutterstock
This condition may be considered a medical emergency. Urgent care may be required.
- A rash is defined as a noticeable change in the color or texture of the skin.
- According to a 2015 study, rashes may be caused by many things, including insect bites, allergic reactions, medication side effects, fungal skin infection, bacterial skin infection, infectious disease, or autoimmune disease.
- You can manage many rash symptoms at home. But severe rashes, especially those seen in combination with other symptoms such as fever, pain, dizziness, vomiting, or difficulty breathing, may require urgent medical treatment.
Read full article on rashes.
Body lice
Share on PinterestPhoto DermNet New Zealand
- Different from head or pubic lice, body lice and their tiny eggs can sometimes be seen on the body or clothing, according to the CDC.
- This rash is caused by an allergic reaction to body lice bites.
- Symptoms may include red, itchy bumps on the skin.
- Thickened or darkened areas of skin are common in irritated areas.
Read full article on body lice.
Impetigo
Share on Pinterest Zay Nyi Nyi/Shutterstock
- The CDC says that this issue is common in babies and children.
- The rash is often located in the area around the mouth, chin, and nose.
- A person may experience an irritating rash and fluid-filled blisters that pop easily and form a honey-colored crust.
Read full article on impetigo.
Head lice
Share on Pinterestkozorog/Getty Images
- A louse is about the size of a sesame seed, according to the CDC. Both lice and their eggs (nits) may be visible in the hair.
- A person may experience extreme scalp itchiness caused by allergic reaction to louse bites.
- A person may develop sores on their scalp from scratching.

- It may feel like something is crawling on your scalp.
Read full article on head lice.
Bites and stings
Share on PinterestGalih Surya Alam/Shutterstock
This condition is considered a medical emergency. Urgent care may be required.
- The NHS says that people may experience redness or swelling at the site of a bite or sting.
- There may be itching and soreness at the site of the bite.
- There may be pain in the affected area or in the muscles.
- A person may feel heat around the bite or sting.
Read full article on bites and stings.
Jock itch
Share on PinterestBy Robertgascoign, via Wikimedia Commons
- There is usually redness, persistent itching, and burning in the groin area.
- Other symptoms include flaking, peeling, or cracking skin in the groin area.
- The rash in the groin area may worsen with activity.
Read full article on jock itch.![]()
Ringworm
Share on Pinterestrodrigobellizzi/Getty Images
Share on PinterestRingworm on the front of the knee. Aiman Khair/Shutterstock
- According to a 2020 review, ringworm looks like circular scaly rashes with raised borders.
- The skin in the middle of the ring appears clear and healthy, and the edges of the ring may spread outward.
- Ringworm is typically itchy.
Read full article on ringworm.
Eczema
Share on PinterestCare_SMC | Flickr
- Eczema will often appear yellow or white with scaly patches that flake off.
- The affected areas may be discolored, itchy, greasy, or oily.
- Hair loss may occur in the area with the rash.
Read full article on eczema.
Latex allergy
Share on PinterestPhoto DermNet New Zealand
This condition may be considered a medical emergency in the event of a serious reaction. Urgent care may be required.
- A rash may occur within minutes to hours after exposure to a latex product.

- Symptoms may include warm, itchy, red wheals at the site of contact that may take on a dry, crusted appearance with repeated exposure to latex.
- Airborne latex particles may cause cough, runny nose, sneezing, and itchy, watery eyes.
- A severe allergy to latex can cause swelling and difficulty breathing.
Read full article on latex allergies.
Scabies
Share on Pinterest Zay Nyi Nyi/Shutterstock
Share on Pinterest Muhammad Hasan Faiz/Shutterstock
- Symptoms may include an extremely itchy rash that may be pimply, made up of tiny blisters, or scaly.
- There are typically raised, white, or flesh-toned lines around the rash.
- Creams can typically clear up the scabies.
Read full article on scabies.
Measles
Share on PinterestBilanol/Getty Images
- Symptoms include fever, sore throat, red watery eyes, loss of appetite, cough, and runny nose.
- Discolored rash spreads from the face down the body 3 to 5 days after first symptoms appear.

- Tiny red spots with blue-white centers appear inside the mouth.
Read full article on measles.
Psoriasis
Share on PinterestIrina Gulyayeva/Getty Images
- A psoriasis rash is often a scaly, silvery, and sharply defined patch of skin.
- It’s commonly located on the scalp, elbows, knees, and lower back.
- Psoriasis may be itchy or asymptomatic.
Read full article on psoriasis.
Dermatographia
Share on PinterestPhoto DermNet New Zealand
- Dermatographia is a rash that appears soon after rubbing or lightly scratching the skin.
- Rubbed or scratched areas of skin turn red, become raised, develop wheals, and may be slightly itchy.
- The rash usually disappears within up to 30 minutes.
Read full article on dermatographia.
Chickenpox
Share on PinterestMixmike/Istock
Share on PinterestGrook da oger, CC BY-SA 4.0, via Wikimedia Commons
- Chickenpox looks like clusters of itchy, discolored, fluid-filled blisters in various stages of healing all over the body.

- The rash is often accompanied by fever, body aches, sore throat, and loss of appetite.
- It remains contagious until all blisters have crusted over.
Read full article on chickenpox.
Pinworms
- It is highly contagious, according to a 2019 review.
- Symptoms include intense itching and irritation in the anal area, restless sleep, and discomfort due to anal itching.
- They may be diagnosed using the “tape test” to collect eggs for your doctor to examine under a microscope.
Read full article on pinworms.
Poison oak, poison sumac, and poison ivy
Share on PinterestDermNet New Zealand
Share on Pinterest Photography courtesy of CDC
- It is caused by skin contact with urushiol, which is an oil found on the leaves, roots, and stems of these plants.
- Rash appears within hours after contact with the plant and may last up to 1 month after exposure.
- There may be intense itching, redness, and swelling as well as fluid-filled blisters.

Read full article on poison oak.
Contact your doctor if:
- You don’t know what’s causing your itching.
- It’s severe.
- You experience other symptoms along with the itching.
It’s important to contact your doctor for a diagnosis when the cause isn’t obvious, because some of the causes of itching are serious, yet treatable, conditions.
Your doctor will give you a physical examination and ask you several questions about your symptoms, such as:
- How long have you had the irritation?
- Where on the body is the itching occurring?
- Does it come and go?
- Have you been in contact with any irritating substances or new scented products?
- Do you have allergies?
- Where is the itching most severe?
- What medications are you taking, or have recently taken?
- Do you have any other symptoms such as fatigue, unusual sweating, chronic cough?
- Have you traveled recently?
You may need more testing if your doctor can’t determine the cause of your itching from your answers and a physical exam.
Tests include:
- Blood test. This may indicate an underlying condition.
- Test of your thyroid function. Thyroid testing can rule out thyroid issues.
- Skin test. This test can determine if you’re having an allergic reaction to something.
- Scraping or biopsy of your skin. Your doctor may use these tests to determine if you have an infection.
When or if your doctor has pinpointed the cause of your itchiness, they can treat the cause of your itching. They may also recommend a topical medication to decrease your itching. If the cause is a disease or infection, your doctor will suggest the best course of treatment for the underlying problem.
When the cause is more superficial, you may receive a prescription for a cream that will help relieve the itching.
Treatment options for itchy skin can vary depending on the cause. Oral medications, topical medications, lifestyle changes, and other natural remedies may be beneficial.
Oral medication
Oral medications could provide relief from itchy skin caused by several conditions, including:
- allergies
- fungal infections
- autoimmune disorders
- cirrhosis
- insect bites or stings
- impetigo
- eczema
- dermatographia
- hives and rashes
According to a 2016 review, medications that may be beneficial include:
- Antihistamines. Oral antihistamines are used to treat allergic reactions and itchy skin or rashes caused by insect bites or stings, hives, eczema, dermatographia, and contact dermatitis.
- Oral steroids. Also known as corticosteroids, these drugs help alleviate inflammation and may be used to treat conditions like systemic lupus erythematosus (SLE), chronic hives, eczema, psoriasis, and severe allergic reactions.
- Immunosuppressants. This type of medication lowers immune activity. Immunosuppressant drugs may be useful to treat flare-ups caused by inflammatory conditions like SLE, chronic hives, and eczema.

- Antifungal medications. These medications treat fungal infections and could reduce itching caused by athlete’s foot, jock itch, ringworm, or diaper rash. Some examples of antifungal medications include griseofulvin (Gris-PEG), fluconazole (Diflucan), and itraconazole (Sporanox).
- Antibiotics. These drugs stop infections caused by bacteria. According to a 2019 study, some specific types of antibiotics, like rifampicin (Rifadin), are also used to control itching caused by liver disease. Oral antibiotics like amoxicillin/clavulanate (Augmentin) or clindamycin (Cleocin) can also treat severe cases of impetigo.
- Beta-blockers. These medications are used to treat cirrhosis and portal hypertension, which is high blood pressure in the vein that carries blood to the liver.
- Bile acid sequestrants. Medications like cholestyramine (Prevalite) help remove bile salts from the body, which can treat cirrhosis.

- Antidepressants. Selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft) and fluoxetine (Prozac) are often used to decrease itchy skin caused by liver disease.
- Antiparasitic drugs. Medications like mebendazole (Vermox) and albendazole (Albenza) are sometimes prescribed for pinworm infection.
- Diuretics. This type of drug can help lower fluid buildup to alleviate symptoms of cirrhosis.
Topical medication
Several types of topical creams can also help reduce itching caused by conditions such as:
- allergies
- fungal infections
- hives and rashes
- autoimmune disorders
- eczema
- lice infestation
- insect bites or stings
- scabies
Some of the most common topical medications that are used to treat itchy skin include:
- Topical steroids. Steroid creams are applied to the skin to lower swelling and inflammation.
 They may be purchased over the counter or prescribed for conditions like eczema, scabies, psoriasis, neuropathic itching, SLE, contact dermatitis, insect bites, allergic reactions, and rashes.
They may be purchased over the counter or prescribed for conditions like eczema, scabies, psoriasis, neuropathic itching, SLE, contact dermatitis, insect bites, allergic reactions, and rashes. - Antifungal creams. These creams are often recommended to reduce itchy skin caused by fungal infections like ringworm, athlete’s foot, diaper rash, and jock itch.
- Topical antidepressants. Doxepin (Zonalon) is a tricyclic antidepressant that is applied topically. According to a 2014 review, it is sometimes used to treat issues like eczema.
- Topical anesthetics. These include pramoxine lotion, hydrocortisone-pramoxine cream, and other topical anesthetics. They’re used to provide temporary relief from pain and itching caused by conditions like scabies, insect bites or stings, hives, and rashes.
- Scabicide. Permethrin cream is a type of topical scabicide prescribed for the treatment of scabies.
- Zinc oxide.
 Available as either a cream or a paste, zinc oxide can decrease skin irritation caused by diaper rash or other types of rashes. It’s also found in products like calamine lotion.
Available as either a cream or a paste, zinc oxide can decrease skin irritation caused by diaper rash or other types of rashes. It’s also found in products like calamine lotion. - Pediculicide. This type of topical medication is sometimes used to treat lice infestation.
Lifestyle changes
In addition to using oral or topical medications, some lifestyle changes may also help soothe itchy skin caused by:
- allergies
- dry skin
- eczema
- fungal infections
- autoimmune disorders
- cirrhosis
- dermatographia
- pinworm infection
- lice infestation
- impetigo
Here are a few lifestyle changes that could help prevent itchy skin:
- Keep skin moisturized. Applying moisturizer daily, limiting your time in the bath or shower, staying hydrated, and using a humidifier can soothe itching caused by dry skin or eczema.
- Wear comfortable, loose-fitting clothing.
 This can alleviate skin irritation and allow your skin to breathe, which may prevent fungal infections.
This can alleviate skin irritation and allow your skin to breathe, which may prevent fungal infections. - Eat a healthy, balanced diet. A 2020 review suggests that making changes to your diet could help control symptoms of psoriasis, lupus, cirrhosis, and eczema.
- Reduce stress. According to a 2018 review, stress reduction techniques like yoga, meditation, and deep breathing exercises could prevent flare-ups of conditions like eczema, psoriasis, dermatographia, and SLE.
- Avoid hot water. Hot water can irritate the skin and may worsen hives or dry skin.
- Practice proper hygiene. Showering regularly, laundering clothes and bedding, and changing your clothing every day could protect against pinworm infection and lice infestation. It may also help stop the spread of other conditions, like impetigo and ringworm.
- Use mild, hypoallergenic, and fragrance-free soaps and wipes.
 This can prevent irritation caused by dry skin, eczema, and diaper rash.
This can prevent irritation caused by dry skin, eczema, and diaper rash. - Avoid allergens. Identifying and avoiding foods, products, and environmental allergens that trigger symptoms for you can be beneficial.
Home care for itching
At home, you can do several things to help prevent and relieve itchy skin. Try:
- using a good moisturizer, that is unscented, to keep your skin hydrated
- avoiding scratching, which can worsen the itch
- staying away from soaps, detergents, and other substances that contain perfumes and color dyes
- taking a cool bath with oatmeal or baking soda
- using over-the-counter anti-itch creams
- taking an oral antihistamine
Most itching is treatable and doesn’t indicate a serious problem. However, it’s best to check with your doctor to confirm a diagnosis and treatment.
A bump has appeared on the finger and hurts
Symptomatic means problematic
The growths are visible to the naked eye. The reason for their occurrence can be judged by their appearance.
The reason for their occurrence can be judged by their appearance.
Hard and dense bumps on the joints, covered with smooth skin, usually form in men over 40 years of age and indicate gout. They are called gouty tophi. They grow during periods of exacerbation of the disease. The patient becomes weak, complains of malaise. The temperature in the tophi region rises, the pain sometimes becomes unbearable.
If the skin on the bump is rough and red, and the growth itself is round and elastic, this is a hygroma. It usually forms in women 20-30 years old and can be single-chamber or multi-chamber. Hygromas differ from other types of growths in that their size gradually increases, and pain is felt when pressed.
The formations on the interphalangeal joints, appearing after 60 years, are called Heberden's nodes. They are equally likely to be found on any phalanx and are signs of osteoarthritis. This disease leads to stiffness of the hands and deformation of the joints.
Nodules up to 2 cm in diameter, which form in 20% of patients with rheumatoid arthritis, are rheumatoid nodules. They do not cause pain, but the course of the disease is accompanied by other unpleasant symptoms: lethargy, fatigue, fever, and sometimes weight loss.
They do not cause pain, but the course of the disease is accompanied by other unpleasant symptoms: lethargy, fatigue, fever, and sometimes weight loss.
Diagnosis of everything head
In order to identify the root cause of the disease and choose an effective course of treatment, the doctor gives the patient an appointment for ultrasound, X-ray, MRI, urinalysis. The study of uric acid salts will determine the presence of gout. X-rays will reliably demonstrate the presence of osteoarthritis or rheumatoid arthritis. However, the results of a visual examination and verbal complaints from the patient alone are often sufficient to make a diagnosis.
How to treat if a bump on the thumb hurts
Alas, this problem is usually caused by chronic diseases and cannot be completely cured. Only the hygroma can be removed once and for all. All other types of growths will remain for life - but exacerbations can be avoided if a stable remission is achieved.
Rheumatoid arthritis is treated with corticosteroids or non-steroidal anti-inflammatory drugs. The same non-steroidal anti-inflammatory drugs, as well as colchicine, are effective against gout.
In case of osteoarthritis, chondroprotectors, finger therapeutic exercises and physiotherapy sessions are prescribed: multichannel electrical stimulation and laser therapy. With multichannel electrical stimulation, muscles are stimulated with short pulses of electricity to relieve tension and improve blood supply. In the laser therapy procedure, the joint growth is exposed to a laser beam to relieve inflammation and activate blood flow inside the tissues.
Osteoarthritis is also treated with physiotherapy: ultrasound (reduces tissue volume), shock wave therapy (activates blood flow, eliminates swelling and pain with acoustic impulses), laser therapy.
Surgery may be required if cartilage and joint surfaces are severely damaged in the advanced stages of arthritis or arthrosis, with fingers swollen, stiff, and painful. In especially severe cases, arthroplasty is prescribed, when a worn joint is replaced with an artificial one. The operation can be performed in the presence of a malignant tumor. The oncologist prepares an individual therapy program for each patient.
In especially severe cases, arthroplasty is prescribed, when a worn joint is replaced with an artificial one. The operation can be performed in the presence of a malignant tumor. The oncologist prepares an individual therapy program for each patient.
Traditional medicine is powerless when there is a lump on the joint of the finger and it hurts. None of the homeopathic remedies contain components from which the bump would resolve. Therefore, relying on chance in the case of such a disease is highly undesirable: all hopes for a miracle can ultimately come down to serious consequences.
A few words about prevention
The best prevention for growths is a healthy lifestyle: a balanced diet, regular consumption of fresh vegetables and fruits, giving up bad habits, sweets and fried foods. Wear protective gloves before handling chemicals. Avoid stress and lack of sleep.
If you are a schoolboy or student, you have a bump on your finger and it hurts - you probably write too much and hold the pen incorrectly. In this case, the growth is a common callus that will come down over time. Do not put a patch on it or try to get rid of it by other methods. Better buy a soft-bodied pen, try holding it a little differently and don't squeeze too hard with your fingers.
In this case, the growth is a common callus that will come down over time. Do not put a patch on it or try to get rid of it by other methods. Better buy a soft-bodied pen, try holding it a little differently and don't squeeze too hard with your fingers.
12 reasons why you have small bumps on your face - Kavun City
Rest assured that you are not alone if you notice a few small bumps on your face. The good news is that most of these buds, which come in many shapes, colors, and textures, are completely harmless. You can easily identify some of them as pimples, while others will require detective work and a doctor to figure out what they really are. In some cases, this may be a sign of a more serious concern.
In general, as long as the bump on your face isn't bleeding, darkening, or changing, it probably doesn't need any medical attention, says Joel Schlessinger, MD, dermatologist and RealSelf consultant. Some bumps, like acne, can often be treated at home or by a dermatologist with a skincare regimen, he says.
But "if a bump changes color or shape, bleeds, or grows in size rapidly, it's time to schedule an appointment with a board-certified dermatologist to get it checked out," says Dr. Schlessinger. These are signs that the bump may be related to an underlying health problem (more on that in a moment), so it's important to pay attention to it.
Of course, it may be inconvenient for you to make an appointment in person right now because of the pandemic. Many doctors, including dermatologists, can help with virtual sessions, depending on your specific concerns. (Here are some helpful tips on how to make an appointment with your doctor during a pandemic.) If you're worried about any abnormalities, call your dermatologist or your GP if possible to discuss the problem.
But again, many small bumps are harmless. The following information can help you determine what type of bumps you have and whether they should be reported to your doctor.
1. Comedones
These common bumps can appear on the face and other parts of the body and are divided into two groups: closed comedones (better known as white dots) and open comedones (black dots).
"They are similar in that they are pores clogged with excess oil and dead skin cells," says Dr. Schlessinger. The difference is that "blackheads have an open comedone, so fatty and dead cells are oxidized, turning brown or black," he explains. Whiteheads, on the other hand, are closed, causing the cocktail inside to appear white, pinkish, or flesh-colored.
How to treat and prevent comedones
While not harmful, these bumps can be annoying. To manage them (and prevent full blown breakouts), Dr. Schlessinger recommends always washing your face before bed with a cleanser containing at least 2% salicylic acid (available over the counter). It dissolves dead skin cells, clears clogged pores, and helps prevent future breakouts. Neutrogena Oil-Free Acne Wash is affordable and recommended by experts. Retinoids, benzoyl peroxide, azelaic acid, and oral antibiotics (which are required by prescription) may also be helpful. A dermatologist can help put together a skin care regimen that makes sense for you if over-the-counter products aren't working. Be patient and give the medication time to work - for example, using salicylic acid to reduce acne can take several weeks.
Be patient and give the medication time to work - for example, using salicylic acid to reduce acne can take several weeks.
It is also important not to use blackhead removal strips. "The glue used to stick them to the skin can damage the complexion," says Dr. Schlessinger. “In addition, they cleanse the skin of natural oils and usually only successfully remove the tops of blackheads, keeping pores clogged and leaving the problem unresolved.”
2. Inflamed pimples
You know you have one of these when you notice a painful bump on your face, sometimes with a large white head and possibly a red circle around it. This happens when the bacteria in our pores start to mix with the excess buildup of dead skin cells and oil that causes acne. Inflamed pimples are often red, painful, swollen, and sometimes filled with pus.
If you have inflammatory pimples, whatever you do, do not pop them, as this can lead to more redness and inflammation. It can also increase the risk of scarring, says Jerome Garden, MD, a dermatologist and director of the Institute for Laser and Dermatology Medicine in Chicago.
How to Treat and Prevent Inflamed Pimples
To try and reduce these pimples, Dr. Garden recommends using a gentle cleanser containing benzoyl peroxide and oil-free skin care products. You can also add some anti-inflammatories: “Once a pimple has formed, a safe way to quickly reduce inflammation is to mix a 1% hydrocortisone cream and benzoyl peroxide cream and apply to the pimple twice a day until the inflammation has resolved,” he says. Cerave Hydrocortisone Cream 1% and La-Roche Posay Effaclar Duo Acne Treatment with Benzoyl Peroxide are two good options.
3. Milia
If you've ever noticed a few tiny white dot-like bumps on your face that didn't budge no matter how many times you tried to wash them off with an acne cleanser, they probably were harmless cysts known as milia.
These keratin-filled cysts “commonly appear around the eyes, cheeks, and nose, can occur in any skin type or color, and tend to be very common in newborns,” explains Dr. Schlessinger. “Milia often appear without any specific cause, although they are more common in people with skin conditions such as rosacea, as well as those with excessive sun damage, skin injuries such as burns, or those whose pores are chronically clogged with oil, cosmetics, and skin care products.”
Schlessinger. “Milia often appear without any specific cause, although they are more common in people with skin conditions such as rosacea, as well as those with excessive sun damage, skin injuries such as burns, or those whose pores are chronically clogged with oil, cosmetics, and skin care products.”
How to Treat and Prevent Milia
Milia are basically dead skin cells stuck under the skin and are not harmful. But if you want to try and get rid of them, Dr. Schlessinger recommends choosing products with alpha hydroxy acids (AHAs) like glycolic or lactic acid to exfoliate your skin. A good option is L'Oréal Revitalift Derm Intensives 10% Pure Glycolic Acid Serum. In addition, a dermatologist can remove milia with a small incision.
4. Keratosis pilaris
These tiny, goosebump-like marks usually appear on the thighs and upper arms, says Dr. Schlessinger, but they can also appear on your face. Sometimes they can also be hereditary, and although they can appear at any age, they are usually more common in children.
"Keratosis pilaris bumps can be confused with goosebumps or even pimples, but are actually caused by small plugs of dead cells that block the hair follicle," explains Dr. Schlessinger. "They don't pose a health risk and don't require treatment, but regular skin exfoliation can help reduce keratosis bumps."
How to treat and prevent keratosis pilaris
Doctors don't know why some people, such as people with eczema, are more likely to get keratosis pilaris, so according to the Cleveland Clinic, there is no real method of prevention. Many people find that this condition improves with age. In the meantime, Dr. Schlessinger recommends a face wash containing glycolic acid, which exfoliates the skin to visibly reduce blemishes. Dry skin can aggravate bumps, which is why the Cleveland Clinic recommends moisturizing your skin with a lotion that contains AHAs.
5. Moles
Whether you've had them forever or just notice that some moles appear on your skin as you age, they're perfectly normal and in most cases harmless. They often appear as brown, red, or flesh-colored spots or bumps on the face, as well as other parts of the body, and are quite common. In fact, according to the American Academy of Dermatological Association, almost everyone has at least one mole.
They often appear as brown, red, or flesh-colored spots or bumps on the face, as well as other parts of the body, and are quite common. In fact, according to the American Academy of Dermatological Association, almost everyone has at least one mole.
These types of bumps or spots form when melanocytes, the skin cells that produce melanin, stick together or grow in clusters rather than spreading. Experts aren't entirely sure what causes moles to form, but sun exposure is thought to increase the number of moles on your skin, AAD explains.
"Moles can be flat or raised and, if harmless, are usually round," says Dr. Schlessinger. AAD explains that it is normal for them to lighten or darken with age. A mole that does not pose a risk for cancer does not require treatment or removal.
How to treat and prevent moles
Ordinary moles do not usually require treatment. According to the AAD, dermatologists remove moles for cosmetic reasons if the mole rubs against your clothes and it bothers you, or if they suspect the mole may be skin cancer. Dr. Schlessinger warns that if a mole starts to change or grow in size, it could be a sign of something more serious, especially skin cancer. The Mayo Clinic also reports that the mole is asymmetrical, irregularly bordered, variable or uneven in color, and is over a quarter of an inch in diameter. (This is a good time to talk about the importance of using sunscreen. If you don't have one you like, this story will help you figure out what works best for your needs. Minimum SPF 30 every day.)
Dr. Schlessinger warns that if a mole starts to change or grow in size, it could be a sign of something more serious, especially skin cancer. The Mayo Clinic also reports that the mole is asymmetrical, irregularly bordered, variable or uneven in color, and is over a quarter of an inch in diameter. (This is a good time to talk about the importance of using sunscreen. If you don't have one you like, this story will help you figure out what works best for your needs. Minimum SPF 30 every day.)
6. Papular dermatosis black (PCHD)
These are not moles, but a different type of skin bump: papular dermatosis black (PKD), which are completely benign and harmless skin patches characteristic of darker skin tones that usually found in families. According to Dr. Garden, these spots are technically not moles and cannot become cancer. "Moles are deeper in the skin, but PSCs are a very superficial collection of epidermal cells and usually start to appear around the age of 20," he says. “These brown bumps can be very small and not grow more than a few millimeters; however, one person can have dozens of spots on their face.”
“These brown bumps can be very small and not grow more than a few millimeters; however, one person can have dozens of spots on their face.”
How to treat and prevent
If you think you may have PCD, you can call your dermatologist to confirm your suspicion. There is little you can do to prevent it from forming or becoming more visible other than using sunscreen and practicing sun protection. Sunscreen is an important part of any skin care routine to help prevent skin cancer, so it's important to choose the one you like.
If you already have bumps, you can try an over-the-counter face wash that contains salicylic acid or glycolic acid, which are "mild chemical exfoliators that can reduce or completely erase these bumps," adds Dr. Garden. "In addition, prescription retinoids also have the potential to reduce the appearance of PSHD, although they are unlikely to be removed."
You can also gently remove these spots by a certified dermatologist with a laser or moxibustion. However, people with dark skin can develop hyperpigmentation due to laser use, so you should talk to your doctor about the best treatment for you.
However, people with dark skin can develop hyperpigmentation due to laser use, so you should talk to your doctor about the best treatment for you.
7. Skin tags
These are usually benign oval-shaped lesions that are connected to the skin of the body or face through a stalk. They are soft to the touch and typically appear on the neck, upper chest, eyelids, groin, and underarms, according to Dr. Schlessinger. Skin tags tend to develop in older adults, according to Mount Sinai Health, which experts say can form when skin rubs against each other.
How to Treat and Prevent
Skin tags are completely harmless as long as they don't grow quickly, change color, become infected, or cause pain. "It's very common for me to have patients who think they have some sort of 'skin marks' but it's actually skin cancer or some other, more dangerous condition," says Dr. Schlessinger. Therefore, if any dangerous changes are found on your skin tag (for example, moles), if possible, contact a dermatologist to have it checked.
However, if your skin tags don't bother you, there's no reason to remove them. "But for aesthetic purposes, a dermatologist can remove them by cutting them off or cauterizing them with heat," says Dr. Schlessinger.
8. Allergic reaction
Sometimes bumps on the face or other parts of the body can be the result of an allergic reaction to something you have eaten or worn, or to a product you have applied.
In some cases, the marks on your body may be hives, which are red, itchy, or scarring that suddenly appear when exposed to an allergen. If the hives are mild, Dr. Schlessinger recommends simply treating it at home with a cool bath, over-the-counter allergy medication, or applying cool compresses to the site. If the hives are more severe, or you are also experiencing shortness of breath, swelling, or difficulty breathing, call your doctor or the emergency room if you do not have one.
Another type of common allergic reaction or skin sensitivity that occurs on the skin is known as irritant contact dermatitis. It is markedly different from urticaria in that it is more of a general redness than individual welts. It is also the result of direct skin contact with things like poison ivy, jewelry, or ingredients in skincare or cosmetics.
It is markedly different from urticaria in that it is more of a general redness than individual welts. It is also the result of direct skin contact with things like poison ivy, jewelry, or ingredients in skincare or cosmetics.
How to treat and prevent allergic reactions
This is probably obvious, but you should definitely stop using or coming into contact with whatever is causing your reaction if you can pinpoint the source. To determine the cause of an allergy, it's helpful to think about any recent changes you've made, such as a new cleanser, shower gel, or deodorant. Then try not to scratch the area so that the damaged skin can begin to heal. You can take an oral antihistamine and use an over-the-counter hydrocortisone balm, according to Dr. Schlessinger.
If this tactic doesn't work, talk to your dermatologist, who may prescribe a stronger anti-itch or a corticosteroid shot to calm the inflammation.
9. Bumps due to eczema
This common skin condition, also called atopic dermatitis, usually appears before the age of five, but technically can occur at any age. "Eczema often appears as oozing or crusted bumps, patches, or plaques, and when chronic, even as thick scales, and results from the interaction of both genes and the environment," said Jeremy A. Brower, MD, a dermatologist at New York.
"Eczema often appears as oozing or crusted bumps, patches, or plaques, and when chronic, even as thick scales, and results from the interaction of both genes and the environment," said Jeremy A. Brower, MD, a dermatologist at New York.
There are several types of eczema, but it usually occurs when the top layer of skin cannot retain moisture and protect you from irritants, allergens, and environmental elements. And, as we just explained, this condition goes beyond dry skin and can cause severe discomfort to people suffering from this condition.
How to treat and prevent eczema
You can't prevent this condition, but you can manage the flare-ups. You can talk to your doctor to confirm that you have eczema so that you can find the right treatment together. Several factors, including a patient's age and their symptoms, can affect treatment, which usually includes oral, topical, or injectable medications. "In many cases, changing environmental factors - avoiding known triggers, changing bathing habits - can relieve symptoms," says Dr. Brouwer.
Brouwer.
He recommends that patients choose shorter warm showers using gentle, unscented products followed by moisturizing. He also suggests washing your clothes with a cleanser for sensitive skin, as well as washing your hands less frequently or making sure to use a moisturizer afterwards. The Cleveland Clinic also recommends using a humidifier at night, applying a moisturizer (more effective than lotion) several times a day, and using a cortisone cream to help relieve symptoms.
10. Rosacea bumps
Dr. Garden says that another chronic inflammatory condition, rosacea, usually appears on the face. "It tends to cause background redness of the cheeks, nose, chin and lower forehead, as well as pimples in some patients."
How to Treat and Prevent Rosacea
Unfortunately, no one knows what causes rosacea and there is no complete cure yet. However, there are ways to reduce the inflammation that causes redness and bumps. “People with rosacea tend to have more sensitive skin on the affected areas of the face, so it’s helpful to replace harsh soaps with gentle cleansers and light moisturizers,” says Dr. Garden. "Sun protection is also paramount for rosacea, as UV exposure exacerbates inflammation."
“People with rosacea tend to have more sensitive skin on the affected areas of the face, so it’s helpful to replace harsh soaps with gentle cleansers and light moisturizers,” says Dr. Garden. "Sun protection is also paramount for rosacea, as UV exposure exacerbates inflammation."
But everyone has their own set of triggers, which can include things like alcohol, exercise, and certain skin care or makeup ingredients. Therefore, it is important to control the impact of these triggers as much as possible.
There are some other treatment options such as topical azelaic acid, topical prescriptions, and oral antibiotics that your dermatologist can refer you to. Because there are many skin conditions that can mimic rosacea, such as acne, eczema, and lupus, it's important to consult with a board-certified dermatologist who can identify your bumps before embarking on self-treatment at home.
11. Bumps due to ingrown hairs
Most of us have had ingrown hairs on our body or face at some point as a result of hair removal. Usually, when the hair grows back, it grows up and over the skin. But if it starts to curl up instead, it can get stuck and form a small, raised, reddened bump that may or may not be filled with pus. People with thick curly hair have more ingrown hairs than people with thin hair, but no one is completely immune.
Usually, when the hair grows back, it grows up and over the skin. But if it starts to curl up instead, it can get stuck and form a small, raised, reddened bump that may or may not be filled with pus. People with thick curly hair have more ingrown hairs than people with thin hair, but no one is completely immune.
How to treat and prevent the bumps associated with ingrown hairs
The best way to prevent ingrown hairs is to avoid waxing, shaving and tweezing, but this is not always a practical option for some people committed to hair removal, explains Dr. Garden. Another way to reduce ingrown hairs is to always wash your skin with mild soap and rub in a lubricating cream gel before shaving.
"If your razor has been used a few times, replace it with a new one, as dull blades don't make clean, precise cuts and can increase the risk of ingrown hairs," says Dr. Garden.
Another long-term solution is laser hair removal, which completely removes hair at a deeper level, damaging the hair follicle. “Laser hair removal requires multiple treatments over several weeks and months, but the results are usually semi-permanent, although it is less effective on light or very light hair,” says Dr. Garden. "Because there are powerful lasers involved and risks including skin discoloration, burns, and even scarring, it's important to find a board-certified dermatologist experienced with lasers." African Americans, Native Americans, and/or people with dark skin tones should make sure their doctor is experienced in treating dark skin, as some lasers can only be used on fair skin, according to the Cleveland Clinic. But again, this option is not an easy decision and you may not be able to schedule electives during a pandemic.
“Laser hair removal requires multiple treatments over several weeks and months, but the results are usually semi-permanent, although it is less effective on light or very light hair,” says Dr. Garden. "Because there are powerful lasers involved and risks including skin discoloration, burns, and even scarring, it's important to find a board-certified dermatologist experienced with lasers." African Americans, Native Americans, and/or people with dark skin tones should make sure their doctor is experienced in treating dark skin, as some lasers can only be used on fair skin, according to the Cleveland Clinic. But again, this option is not an easy decision and you may not be able to schedule electives during a pandemic.
- Lipoma
A lipoma is a growth of fatty tissue that can occur almost anywhere on the body (including the face), but is most common on the chest, back, shoulders, neck and armpits. “While they tend to grow slowly, often over months or years, you will notice them as a rubbery bulge under the skin that is usually less than 2 inches across and seems to move,” explains Dr. Garden. "Sometimes larger lipomas occur, some reaching almost 8 inches in diameter, although this is rare."
Garden. "Sometimes larger lipomas occur, some reaching almost 8 inches in diameter, although this is rare."
The good news is that lipomas are almost always benign. However, there is a very rare form of cancer known as liposarcoma, which occurs in fatty tissue and can look like a deep lipoma, explains Dr. Garden. Therefore, if you notice something like a lipoma that is painful or growing rapidly, it should be checked out by a dermatologist who will determine if a biopsy is needed.
How to Treat and Prevent Lipomas
According to Dr. Garden, although the cause of lipomas is unknown, some people have genetic conditions that predispose them to developing dozens of lipomas. In most cases, lipomas do not need treatment, however, the patient may choose to have the lipoma removed surgically if this causes any discomfort.
Many types of bumps on the face are not a cause for concern or can be easily managed at home. However, don't pick at the bumps or try to remove them yourself, as this can lead to infections or scarring.