Vomiting and cramps during pregnancy
Abdominal Pain in Early Pregnancy
Case Objectives
- Recognize when nausea and vomiting in pregnancy is abnormal.
- Identify the most common causes of non-obstetric abdominal pain and acute abdomen in early pregnancy.
- Review the diagnosis of appendicitis in pregnancy.
- Discuss a diagnostic imaging algorithm for pregnant women with suspected appendicitis.
Case & Commentary—Part 1
A 34-year-old woman who was 14 weeks pregnant presented to the emergency department (ED) with 5 days of nonspecific abdominal pain, nausea, and vomiting. On examination, she appeared well with normal vital signs and had some mild diffuse abdominal tenderness. Her white blood cell count was 19,000 cells/μL, and a urinalysis was positive for nitrates and leukocyte esterase (indicating possible infection). She was diagnosed with a urinary tract infection and was discharged on antibiotic therapy. No imaging was performed at this initial visit.
The patient returned the following day with unchanged abdominal pain and more nausea and vomiting. A fetal ultrasound was performed and found normal fetal heart activity. No further testing was done, and she was discharged home with instructions to continue the antibiotics.
Abdominal pain remains the most common reason for emergency department (ED) visits, comprising more than 11% of all visits in 2008.(1) In 2011, 54% of patients that presented to the ED were female, more than 25% were of childbearing age, and the pregnancy rate in the United States is approximately 10% at any given time.(2,3) For these reasons, clinicians that evaluate patients with abdominal pain in the ED should be familiar with common causes of abdominal pain in pregnant women and appreciate when nausea and vomiting in pregnancy is abnormal.
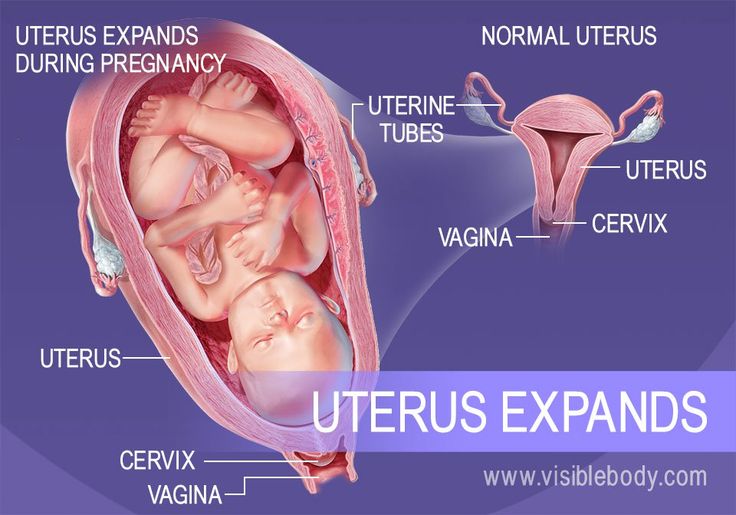
Nausea, vomiting, and abdominal pain are very common in pregnancy. Up to 80% of pregnant women experience nausea and vomiting, most commonly in the first trimester. Symptoms and signs that may indicate another cause include nausea and vomiting persisting past mid-pregnancy (approximately 20 weeks) and associated abdominal pain, fever, or diarrhea. In these instances, a more thorough evaluation is indicated.(4) Due to the enlarging uterus and fetal position/movement, abdominal pain is also common in pregnancy. Warning signs include pain that is localized, abrupt, constant, or severe, or pain that is associated with nausea and vomiting, vaginal bleeding, or fever. With any of these, further investigation into nonpregnancy-related causes is warranted. If any of the warning signs above is present, consultation with an obstetric specialist is recommended.
In these instances, a more thorough evaluation is indicated.(4) Due to the enlarging uterus and fetal position/movement, abdominal pain is also common in pregnancy. Warning signs include pain that is localized, abrupt, constant, or severe, or pain that is associated with nausea and vomiting, vaginal bleeding, or fever. With any of these, further investigation into nonpregnancy-related causes is warranted. If any of the warning signs above is present, consultation with an obstetric specialist is recommended.
Women of childbearing age who present to the ED with abdominal pain at minimum should receive a urine pregnancy test, and the location and gestational age of the pregnancy should be determined with ultrasound. Miscarriage and ectopic pregnancy are the most frequent causes of abdominal pain in early pregnancy and are often accompanied by vaginal bleeding.(5,6) Once an early gestational age and intrauterine location is confirmed and miscarriage is ruled out, nonobstetric causes of abdominal pain should be explored, especially if any of the warning signs above are present.
With the exception of ovarian torsion, which is more common in the first trimester, the cause and incidence of non-obstetric abdominal pain in pregnancy varies little by gestational age of the fetus. The following are approximate incidences of some causes of acute abdomen in pregnancy: appendicitis (1/1500 pregnancies), cholecystitis, nephrolithiasis, pancreatitis, and small bowel obstruction (each occur in approximately 1/3000), with ovarian pathology (torsion or symptomatic masses) and uterine leiomyomas less common.(7)
After a history, physical examination, and the pregnancy test and ultrasound, laboratory tests that can assist in narrowing the differential diagnosis—including a complete blood count, liver and pancreatic enzymes, and urinalysis—should be reviewed. The white blood cell count increases to 10,000–14,000 cells/μL in normal pregnancy (and as high as 30,000 cells/μL in labor). However, a left shift in the differential and the presence of bands are abnormal and require further investigation. (8) If clinical signs and symptoms accompanied by laboratory data are not conclusive, prompt imaging may be necessary.
(8) If clinical signs and symptoms accompanied by laboratory data are not conclusive, prompt imaging may be necessary.
Imaging in pregnancy should begin with ultrasound or magnetic resonance imaging (MRI) as they have no ionizing radiation and have not been linked with fetal harm. Compression ultrasound may be useful in the evaluation of suspected appendicitis, cholecystitis, nephrolithiasis, and ovarian pathology in this setting. However, compression ultrasound becomes less sensitive and specific in pregnancy and relies heavily on the skill of the technician or radiologist. If the ultrasound is nondiagnostic, MRI can be considered as its lack of ionizing radiation also makes it safe for the fetus. MRI can aid in diagnosing acute appendicitis, cholecystitis, bowel obstruction, and ovarian pathology. If MRI is unavailable and there is serious concern for a nonpregnancy-related cause for the abdominal pain, computed tomography (CT) scanning can be performed.
If diagnostic tests that contain ionizing radiation (e. g., CT scanning) are deemed to be clinically necessary, they should not be withheld in the pregnant patient even with the concerns for an increased risk of fetal harm. Although a fetus can be harmed by radiation (including miscarriage, fetal anomalies, fetal growth restriction, intellectual disability, and future childhood cancer), the risk is low, especially at lower radiation doses. During the first 2 weeks of pregnancy, ionizing radiation is associated with an all-or-none type effect (miscarriage or intact survival) based on the radiation dose. After this time period, a dose less than 5 rads is recommended in order to decrease the chances of fetal harm.(9) A normal CT scan of the abdomen and pelvis delivers approximately 1 rad of radiation. As a rule, the least amount of ionizing radiation in necessary diagnostic tests should be utilized in the pregnant patient, and consultation with a radiologist and obstetrician is often helpful to achieve this goal.(9) A full discussion of the fetal risks associated with CT scanning is beyond the scope of this commentary, but a CT scan in this setting should only be obtained after obstetrical consultation.
g., CT scanning) are deemed to be clinically necessary, they should not be withheld in the pregnant patient even with the concerns for an increased risk of fetal harm. Although a fetus can be harmed by radiation (including miscarriage, fetal anomalies, fetal growth restriction, intellectual disability, and future childhood cancer), the risk is low, especially at lower radiation doses. During the first 2 weeks of pregnancy, ionizing radiation is associated with an all-or-none type effect (miscarriage or intact survival) based on the radiation dose. After this time period, a dose less than 5 rads is recommended in order to decrease the chances of fetal harm.(9) A normal CT scan of the abdomen and pelvis delivers approximately 1 rad of radiation. As a rule, the least amount of ionizing radiation in necessary diagnostic tests should be utilized in the pregnant patient, and consultation with a radiologist and obstetrician is often helpful to achieve this goal.(9) A full discussion of the fetal risks associated with CT scanning is beyond the scope of this commentary, but a CT scan in this setting should only be obtained after obstetrical consultation.
In this case, at the first visit to the ED, the combination of abdominal pain, nausea, and vomiting appropriately raised concern for a nonpregnancy-related cause and triggered further investigations. The patient was found to have a leukocytosis and a positive urinalysis and was treated for urinary tract infection (UTI). At that first visit, she also should have had a urine pregnancy test and an ultrasound to establish the location and gestational age of the pregnancy. In addition, it would have been reasonable for the providers to have considered imaging, since the symptom constellation—5 days of constant abdominal pain, nausea, vomiting, abdominal tenderness on exam, and an elevated white blood cell count—were incompletely explained by a simple UTI. An ultrasound was performed when the patient returned to the ED and indicated a normal viable pregnancy. However, no further imaging was pursued. Given the severity and persistence of her symptoms despite treatment, a complete abdominal ultrasound (looking for nonpregnancy-related intra-abdominal pathology) would have been appropriate.
Case & Commentary—Part 2
The patient again returned to the ED within 24 hours with persistent complaints. She now appeared more ill, with increased abdominal pain on examination. Magnetic resonance imaging of the abdomen was performed and revealed a ruptured appendix with signs of peritoneal inflammation. The patient was taken immediately to the operating room and was found to have diffuse peritonitis secondary to the ruptured appendix. An emergent laparoscopic appendectomy was performed, which the patient tolerated well. Unfortunately, 3 hours after the operation, she had a spontaneous abortion and subsequent severe bleeding requiring multiple transfusions. She was discharged home days later.
In retrospect, it may not have been appropriate to discharge this patient from the ED after her initial presentation without further evaluation, and she experienced a tragic adverse event.
In early pregnancy, the symptoms of appendicitis are identical to those seen in the nonpregnant state: periumbilical pain that migrates to the right lower quadrant, accompanied by anorexia, fever, nausea, and vomiting. With advancing gestational age and in parous women, the diagnosis may become more challenging, largely due to the laxity of the anterior abdominal wall.(10) As the uterus enlarges and fills the peritoneal cavity, a possible cephalad movement of the appendix into the upper quadrant (Figure) can confuse the clinical presentation. Patients may actually present with right upper quadrant pain. Moreover, as the distance between the peritoneum and the appendix increases, peritoneal signs may be masked. Lastly, accurate imaging of the appendix becomes more challenging. Uterine contractions, more common in later gestation, also decrease the ability to accurately elicit peritoneal signs and abdominal tenderness on physical examination. Notwithstanding these variations, clinicians should be aware that right lower quadrant pain remains the most common symptom of appendicitis in pregnant women.(10) Given that appendicitis is the most common cause of acute abdomen in pregnancy, a high index of suspicion is warranted to decrease maternal and fetal morbidity and mortality.
With advancing gestational age and in parous women, the diagnosis may become more challenging, largely due to the laxity of the anterior abdominal wall.(10) As the uterus enlarges and fills the peritoneal cavity, a possible cephalad movement of the appendix into the upper quadrant (Figure) can confuse the clinical presentation. Patients may actually present with right upper quadrant pain. Moreover, as the distance between the peritoneum and the appendix increases, peritoneal signs may be masked. Lastly, accurate imaging of the appendix becomes more challenging. Uterine contractions, more common in later gestation, also decrease the ability to accurately elicit peritoneal signs and abdominal tenderness on physical examination. Notwithstanding these variations, clinicians should be aware that right lower quadrant pain remains the most common symptom of appendicitis in pregnant women.(10) Given that appendicitis is the most common cause of acute abdomen in pregnancy, a high index of suspicion is warranted to decrease maternal and fetal morbidity and mortality. In this case, the patient had a somewhat uncommon presentation, with no localization of the abdominal pain. However, the nausea and vomiting and persistent symptoms should have led the clinicians to consider the diagnosis of appendicitis early in the evaluation.
In this case, the patient had a somewhat uncommon presentation, with no localization of the abdominal pain. However, the nausea and vomiting and persistent symptoms should have led the clinicians to consider the diagnosis of appendicitis early in the evaluation.
If appendicitis is suspected, diagnostic imaging can help rule in or rule out the diagnosis. Ultrasound is the test of choice in this setting—the diagnosis of appendicitis is made when a noncompressible, blind-ended tubular structure greater than 6 mm is visualized in the right lower quadrant. Unfortunately, the appendix cannot always be visualized with ultrasound, and ultrasound may be less accurate in the setting of a ruptured appendix or with advancing gestational age.(11) The American College of Radiology suggests MRI as the second modality when evaluating for appendicitis in the pregnant patient. The diagnosis is made with visualization of a fluid filled appendix greater than 7 mm in diameter. MRI has high sensitivity and specificity for diagnosing appendicitis. (12) However, MRI technology and expertise are not always available, especially in smaller hospitals or off hours. When this is the case, CT with or without contrast should be used. CT is readily available in most centers, and it has high sensitivity and specificity for the diagnosis of appendicitis. The diagnosis is made by visualization of a fecalith, an enlarged nonfilling tubular structure, or right lower quadrant inflammation. The use of contrast typically enhances diagnostic accuracy with the potential increase in fetal harm (see above). The decision to use contrast should balance the potential fetal harm with the possible delay in diagnosis from nonvisualization of the appendix if contrast is not used. A delay can lead to rupture of the appendix and increase fetal mortality. The fetal loss rate increases from 3%–5% in nonruptured appendicitis to as high as 25% if the appendix ruptures.(13) Maternal morbidity is also higher in the setting of a ruptured appendix.
(12) However, MRI technology and expertise are not always available, especially in smaller hospitals or off hours. When this is the case, CT with or without contrast should be used. CT is readily available in most centers, and it has high sensitivity and specificity for the diagnosis of appendicitis. The diagnosis is made by visualization of a fecalith, an enlarged nonfilling tubular structure, or right lower quadrant inflammation. The use of contrast typically enhances diagnostic accuracy with the potential increase in fetal harm (see above). The decision to use contrast should balance the potential fetal harm with the possible delay in diagnosis from nonvisualization of the appendix if contrast is not used. A delay can lead to rupture of the appendix and increase fetal mortality. The fetal loss rate increases from 3%–5% in nonruptured appendicitis to as high as 25% if the appendix ruptures.(13) Maternal morbidity is also higher in the setting of a ruptured appendix.
Institutions should develop an algorithm for optimal imaging of pregnant patients with an acute abdominal process, and this algorithm should be communicated to all the clinicians that care for pregnant patients. The algorithm should take into account best practices as well as the expertise and capability of the radiology team. The goal should be to minimize ionizing radiation and fetal harm while maintaining diagnostic accuracy. The use of the algorithm as well as the clinical outcomes of pregnant patients with abdominal pain should be audited and reviewed. The results of these reviews should be provided to clinicians and could easily be incorporated into institutional meetings that focus on hospital improvement.
The algorithm should take into account best practices as well as the expertise and capability of the radiology team. The goal should be to minimize ionizing radiation and fetal harm while maintaining diagnostic accuracy. The use of the algorithm as well as the clinical outcomes of pregnant patients with abdominal pain should be audited and reviewed. The results of these reviews should be provided to clinicians and could easily be incorporated into institutional meetings that focus on hospital improvement.
The implementation of a checklist may also help to decrease morbidity in the pregnant patient who presents with abdominal pain without introducing any negative effect on safety. Checklists in medicine have been associated with reduced morbidity and mortality, enhanced communication, decreased adverse events, and improved adherence to hospital operating procedures.(14) A computerized checklist could review atypical signs and symptoms in the pregnant patient and prompt clinicians to consider other diagnoses. In this case for example, 5 days of abdominal pain, nausea, and vomiting, with abdominal tenderness on physical examination should have prompted an exploration of diagnoses other than a UTI and may have led to abdominal imaging.
In this case for example, 5 days of abdominal pain, nausea, and vomiting, with abdominal tenderness on physical examination should have prompted an exploration of diagnoses other than a UTI and may have led to abdominal imaging.
In the above case, in the initial visit, pregnancy location and gestational age should have been documented, and a further investigation into the patient's signs and symptoms should have prompted imaging of the abdomen and pelvis and consultation with an obstetric specialist. When the patient returned with worsening symptoms, appropriate imaging was pursued and revealed acute appendicitis. The error (delay in diagnosis) led to a catastrophic adverse event—the loss of the fetus. A checklist highlighting the warning signs above or an algorithm for early and safe imaging may have led to an earlier diagnosis and a better outcome.
Take-Home Points
- Nausea and vomiting are common in early pregnancy, but symptoms that persist after 16–20 weeks or are accompanied by abdominal pain should be considered abnormal and evaluated.

- Initial imaging in the evaluation of abdominal pain in the pregnant patient should begin with ultrasound or MRI, but ionizing imaging that is clearly indicated by the clinical situation should not be delayed or withheld in the pregnant patient due to concerns of fetal harm.
- Emergency department physicians, in conjunction with obstetric specialists, should develop a diagnostic imaging algorithm for pregnant patients with abdominal pain based on the availability and expertise of their radiologic staff.
- Consultation with an obstetric specialist should be strongly considered in patients with abdominal pain associated with nausea and vomiting in pregnancy.
- Appendicitis remains the most common cause of acute abdomen in pregnancy, and a delay in diagnosis increases fetal mortality.
Charlie C. Kilpatrick, MD Associate Professor of Obstetrics and Gynecology Residency Program Director Baylor College of Medicine, Houston, Texas
Faculty Disclosure: Dr. Kilpatrick has declared that neither he, nor any immediate member of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
Kilpatrick has declared that neither he, nor any immediate member of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Emergency Department Visits for Chest Pain and Abdominal Pain: United States, 1999–2008. Atlanta, GA: National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; September 2010. NCHS Data Brief No. 43. [Available at]
2. The National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; November 2014. [Available at]
[Available at]
3. Pregnancy Rates for U.S. Women Continue to Drop. Atlanta, GA: National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; December 2013. NCHS Data Brief No. 136. [Available at]
4. McCarthy FP, Lutomski JE, Greene RA. Hyperemesis gravidarum: current perspectives. Int J Womens Health. 2014;6:719-725. [go to PubMed]
5. Doubilet PM, Benson CB, Bourne T, Blaivas M; Society of Radiologists in Ultrasound Multispecialty Panel on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369:1443-1451. [go to PubMed]
6. Lipscomb GH. Ectopic pregnancy: still cause for concern. Obstet Gynecol. 2010;115:487-488. [go to PubMed]
7. Kilpatrick CC, Monga M. Approach to the acute abdomen in pregnancy. Obstet Gynecol Clin North Am. 2007;34:389-402. [go to PubMed]
8. Kuvin SF, Brecher G. Differential neutrophil counts in pregnancy. N Engl J Med. 1962;266:877-878. [go to PubMed]
9. ACOG Committee on Obstetric Practice. ACOG Committee Opinion #299 (replaces #158, September 1995): guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104:647-651. [go to PubMed]
10. Mourad J, Elliot JP, Erikson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182:1027-1029. [go to PubMed]
11. Lim HK, Bae SH, Seo GS. Diagnosis of acute appendicitis in pregnant women: value of sonography. AJR Am J Roentgenol. 1992;159:539-542. [go to PubMed]
12. Andreotti RF, Lee SI, Dejesus ASO, et al. ACR Appropriateness Criteria acute pelvic pain in the reproductive age group. Ultrasound Q. 2011;27:205-210. [go to PubMed]
13. Doberneck RC. Appendectomy during pregnancy. Am Surg. 1985;51:265-268. [go to PubMed]
14. Thomassen Ø, Storesund A, Søfteland E, Brattebø G. The effects of safety checklists in medicine: a systematic review. Acta Anaesthesiol Scand. 2014;58:5-18. [go to PubMed]
Figure
Figure. Illustration Showing How Position of Appendix Changes in Pregnancy. (Illustration © 2015 Chris Gralapp.)
4 common pregnancy-related GI issues, and when to call the doctor | Your Pregnancy Matters
Mild gastrointestinal issues are common during pregnancy, but if you’re concerned, call your doctor.Gastrointestinal (GI) issues are common during pregnancy. As your baby grows, you’ll have less available real estate in your abdomen for your intestines, stomach, and esophagus to function. Additionally, hormonal changes can affect digestion and other GI functions.
Most GI symptoms pass relatively quickly during pregnancy and can be treated with over-the-counter remedies at home. However, to avoid potential complications, women should be aware of what’s normal and when to call the doctor when it comes to GI health during pregnancy.
1. Nausea and vomiting
During the first 16 weeks of pregnancy, we expect some mild to moderate nausea and vomiting – the infamous period of morning sickness. In fact, for many women, nausea is one of the earliest symptoms of pregnancy.
If you have severe symptoms, a doctor can recommend medication to reduce dehydration and discomfort. For mild symptoms, or if you prefer not to take medication, you can usually manage symptoms with dietary changes or vitamin therapy under the care of your doctor.
After 16 weeks of pregnancy, vomiting typically is not pregnancy-related and might be due to a bug or infection. In rare cases, vomiting can be caused by more serious medical concerns, such as hepatitis, pancreatitis, or ulcers. If you experience nausea or vomiting past the first trimester of pregnancy, don’t assume it’s pregnancy-related, and don’t let your doctor assume so, either, without checking for underlying causes.
2. Heartburn
Heartburn, or gastroesophageal reflux, affects three of five people in the general population. By the time women reach the third trimester, as many as half will experience heartburn at one point or another. During pregnancy, the muscle between the esophagus and stomach relaxes due to hormonal changes related to pregnancy. At the same time, the growing uterus puts increased pressure on the stomach. The combination is a perfect storm for heartburn.
Eating smaller, more frequent meals can help stave off heartburn. Standard treatments – antacids, proton pump inhibitors (Prevacid), or h3 blockers (Tagamet or Pepcid) – are generally safe during pregnancy.
However, if you experience pain below the ribs in your upper abdomen, call your doctor. Although rare, epigastric pain can be a sign of fatty liver disease or preeclampsia, a serious blood pressure disease that can arise suddenly during pregnancy.
3. Diarrhea
Let’s face it – diarrhea is the worst. When it lasts just a few days, diarrhea typically is related to an infection (usually gastroenteritis) or eating something that upsets your stomach. Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Diarrhea that develops without an identifiable trigger or in combination with low back pain and increased vaginal discharge or mucus can be symptoms of preterm labor. Call your doctor immediately if you experience this combination of symptoms.
4. Constipation
Pregnancy hormones affect the lower GI tract, effectively slowing down the transit of stool through the bowels. This slow-motion process allows more water to be absorbed in the stools, which makes them hard to pass. Certain prenatal vitamins and iron therapy also can contribute to constipation. Later in pregnancy, pressure from the growing uterus can also make it harder to pass stools, which increases the risk of hemorrhoids.
Drinking more fluids and eating more fiber is effective in reducing and preventing constipation. Stool softeners are safe to use as well, and some iron supplements actually contain them. More severe constipation might require a mild laxative. Talk to your doctor about additional treatments if you experience abdominal pain, bloody stools, or painful hemorrhoids.
More severe constipation might require a mild laxative. Talk to your doctor about additional treatments if you experience abdominal pain, bloody stools, or painful hemorrhoids.
Most women will experience GI concerns at some point during pregnancy. If your symptoms are serious or if you are concerned, talk to your doctor. It’s better to be safe, and we’re here to help your pregnancy – and GI tract – flow smoothly.
Stay on top of health care news. Subscribe to our blog today.
Convulsions during pregnancy: treatment and prevention
Every woman at least once in her life has come across the concept of convulsions. This is especially unpleasant, and, unfortunately, not uncommon, the phenomenon manifests itself during pregnancy. Should I be scared or worried?
Pregnant women often experience convulsions at night when falling asleep or before waking up. The sensations are so painful, strong and unbearable that they do not allow her to fully rest.
In the first trimester, the expectant mother suffers from convulsions against the background of early toxicosis due to a lack of healthy substances. But usually this phenomenon manifests itself in the second or third trimester due to the increased load on the woman's body and the likely nervous displacements.
Causes of sudden seizures during pregnancy
What are the sources of seizures in a pregnant woman and how to deal with them?
As already mentioned above, involuntary muscle contractions can lie in wait for a woman during any period of expectation of a baby. Accordingly, the causes of occurrence are different, they are united by one thing: there are failures and disorders in the body, ranging from a lack of vitamins and trace elements to complications.
According to experts, the main sources of unpleasant painful impulsive muscle contractions can be:
- Deficiency of trace elements such as calcium, potassium, magnesium and vitamin B6.
 What caused this deficit?
What caused this deficit? -
- Toxicosis, accompanied by profuse vomiting. Consequently, the female body is deprived of a large number of trace elements (most often in the first trimester of expecting a child).
- Uncontrolled use of diuretics.
- The fetus requires more needs for development (which is more in the middle of pregnancy).
- Improper and unbalanced diet, which leads to insufficient intake of nutrients into the body.
- The amount of hemoglobin decreases - that is, the protein that is responsible for delivering oxygen to all organs. During pregnancy, the health of the mother and child depends on the level of hemoglobin.
- If the expectant mother violates the diet, eats a lot of carbohydrates, is fond of sweets, eats rarely, but in large portions - all this can lead to a violation of blood sugar levels.
- Varicose veins, especially if the pregnant woman puts a lot of pressure on her legs.
- Uncountable consumption of caffeinated drinks by a woman.
 Such abuse is fraught with dehydration of the muscles, their tension. This may result in the development of seizures.
Such abuse is fraught with dehydration of the muscles, their tension. This may result in the development of seizures. - “Inferior vena cava syndrome” is a condition in which an enlarged uterus presses on the inferior vena cava. A significant additional load is provoked on the work of the heart, blood vessels, blood supply to the fetus, and a violation of the venous outflow from the legs. One result is the development of seizures. This condition occurs in the last term, especially when resting on the back or right side.
- All kinds of diseases and complications of pregnancy.
Leg cramps
Many expectant mothers, when talking to their gynecologist and talking about painful sensations, complain about spasms in the muscles of the legs, more precisely, cramps in the calf muscles. The time of occurrence of these unpleasant symptoms is either in the evening or in a dream, at night.
At night, the body rests, is at rest and relaxed. It is at such moments that women often wake up from the pain of cramps in the muscles of the legs. Therefore, some pregnant women put a pin near them to prick a cramped muscle.
Therefore, some pregnant women put a pin near them to prick a cramped muscle.
Causes:
- Leg cramps can be triggered by many factors: deficiency of trace elements, primarily magnesium and calcium, vitamins D and B6, and many others. But the main thing is that an additional burden falls on the woman's body.
- Spasms at night are the result of increased stress on the legs during the day. It is worth paying special attention to women in the "position" on the shoes they wear throughout the day. High heels are absolutely not recommended for pregnant women if they have a predisposition to cramps. Therefore, all doctors advise wearing low-speed shoes: the legs will not be overloaded, and, accordingly, there will be less muscle contractions at night.
- If you have a habit of crossing your legs while sitting on a chair or in an armchair, you should stop it.
- Proper healthy nutrition is a must. Starting from 4 months, it is recommended to rest on the left side so that the condition of the “inferior vena cava syndrome” does not appear.

Help:
- If at any time of the day the leg is "crumpled" - use a pin or needle, lightly prick the muscle.
- A good method is to strain and pull the toe of the leg in which the spasm has developed towards you, sometimes helping with your hands. Repeat several times and try to relax while doing it. And then massage in the place where unpleasant painful sensations arose to restore blood circulation. After that, you can slowly walk around or sit, raising your legs to a dais.
Leg cramps
Leg muscle contractions are not the only ones that can disturb a pregnant woman: during this period of life, the expectant mother also experiences discomfort in her arms.
Causes:
- The main sources of pain are the same as described above: improper and irregular nutrition, lack of useful trace elements, overheating, excessive abuse of diuretic drugs, various diseases and complications of pregnancy, prolonged muscle tension.

- Women who have the same type of hand movements for a long time are susceptible to such spasms. For example: office workers, musicians, assembly line workers and others. But housewives should also think about how to take care during pregnancy. After all, a long time to cut vegetables or do other homework can lead to painful sensations.
Help:
- If a pregnant woman works all day, it is imperative to plan the work so that her hands can rest. The best option is to alternate work and rest every 15 minutes. Rest is recommended to be combined with light exercises: waving your arms, clenching and unclenching your fists, rotating your hand, shaking your hands.
- Hand massage is an excellent method. It is quite enough to massage problem areas and the result will please you very soon.
If all the above recommendations do not help, be sure to consult your doctors. The possibility of internal diseases should be excluded. For example, symptoms of neuropathy are frequent cramps in the same place, problems with the cardiovascular system - frequent painful cramps in the left arm.
For example, symptoms of neuropathy are frequent cramps in the same place, problems with the cardiovascular system - frequent painful cramps in the left arm.
Abdominal cramps
Abdominal cramps are usually very frightening for a woman, she becomes very nervous and imagines the worst options for herself. But often all the sensations that a pregnant woman takes for cramps are uterine contractions that are inevitable during pregnancy.
- During any period of pregnancy, you should not worry about the above sensations, provided that there are no concomitant signs: bloody or brown discharge, the general condition of the pregnant woman has not worsened, no sudden weaknesses appear throughout the day.
- If seizures occur shortly after conception, the likely cause is the attachment and implantation of a fertilized egg to the uterus. Further, when the fetus is fixed and begins to grow, this may become a factor in abdominal cramps, although not felt by most women.

Attention!
Starting from the 20th week of pregnancy, expectant mothers may experience mild, non-painful cramps: the uterus is preparing for the upcoming birth and is training contractions in advance.
False contractions (the concept was introduced by an English doctor, after his name they are called “Braxton-Hicks contractions”) - completely safe, they do not cause the opening of the cervix, therefore, do not lead to labor. The main signs of Braxton-Hicks contractions are irregularity, unpredictability, short duration and relative painlessness.
Pre-delivery training contractions also occur at earlier dates, but usually the woman does not identify them.
If a pregnant woman notices that the contraction is regular, repeating at regular intervals, accompanied by pain in the back or abdomen, there is a brown spotting discharge, seek medical help immediately. All of the above signs may indicate an increased tone of the uterus and the risk of miscarriage.
Treatment of seizures during pregnancy
The most important thing that a woman expecting a child must do when seizures appear is to contact her gynecologist. The doctor, after consulting with specialists and excluding serious diseases, will give recommendations to reduce or completely stop muscle spasms.
The main recommendation, which will sound from the lips of doctors, is to review the diet of a pregnant woman. It is necessary to add to the menu more foods that are rich in essential nutrients - potassium, magnesium, calcium.
- Potassium
Every cell in the body contains potassium, which is extremely important. Toxicosis, improper use of drugs, excessive consumption of caffeine lead to a lack of this element.
Potassium deficiency is manifested by:
- Convulsions
- Constipation
- Thirst
- Depression and nervousness
- Tachycardia.
Foods rich in potassium: melon, dried apricots, beans, beef liver, bananas, broccoli, potatoes.
- Calcium
Calcium is one of the most essential minerals for humans.
Calcium deficiency is manifested by:
- Tooth decay
- Cramps
- Insomnia
- Numbness and convulsions
- Nervousness
- Brittle nails.
Sources of calcium - dairy products, asparagus, broccoli, legumes, nuts, cabbage, figs.
- Magnesium
Comprehensive stabilizer of body processes. The need for magnesium during pregnancy increases by 2-3 times.
Magnesium deficiency is manifested by:
- Convulsions
- Decrease in body temperature
- Arrhythmia.
Contained in sunflower seeds, carrots, nuts, legumes, green vegetables.
Painful spasms can be eliminated by massage, a specially selected course of exercises, various ointments and gels. Any medications can be taken only after prescription by specialists.
Prevention of seizures
In order to prevent seizures, doctors advise:
- wear comfortable shoes with low, stable heels;
- with a predisposition to the expansion of the superficial veins of the legs, you should wear special designed stockings;
- rest more often with legs elevated;
- if you have to be on your feet for a long time without moving, it is recommended to do simple exercises: rise in turn on your toes, then lower yourself to the foot;
- late pregnancy, try to lie on the left side;
- take contrast showers;
- Relaxing foot baths with warm water and sea salt are recommended before going to bed.
Interventions for leg cramps during pregnancy
What is the problem?
Leg cramps manifest themselves as sudden, intense involuntary contractions of the leg muscles. This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching.
They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching.
Why is this important?
The purpose of this review was to find out which treatment for leg cramps during pregnancy is effective and safe.
What evidence did we find?
In September 2019, we searched for evidence and identified eight randomized controlled trials in 576 women 14 to 36 weeks gestation comparing magnesium, calcium, calcium with vitamin D, or B vitamins versus placebo or no treatment, and compared vitamin C with calcium. All drugs were given as tablets to chew or swallow.
Magnesium supplements may reduce the incidence of leg cramps in women compared with placebo or no treatment, although studies have not been consistent. Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Calcium did not always reduce the incidence of leg cramps in women after treatment compared to those who did not receive any treatment. It also found that the evidence was of very low quality, so we cannot be sure of the results.
More women who received B-vitamin supplements made a full recovery compared to those who received no treatment; however, these results were based on a small sample size and the study had design limitations.
The frequency of leg cramps did not differ between women receiving calcium and women receiving vitamin C. with placebo.
with placebo.
What does this mean?
The quality of the evidence was low to very low. This was mainly due to small study sample sizes and study design weaknesses. Four studies were well-conducted and presented their reports. The remaining four had flaws in their design: in several studies, women were not best assigned to different treatment groups, and in two studies, women knew whether they were receiving treatment or not. Adverse effects, such as the effect of treatment on complications of pregnancy, childbirth and child, were not reported. Several studies have focused primarily on serum calcium and magnesium levels. The frequency and intensity of seizures and duration of pain were not uniformly reported, and there was often no information on whether they were assessed during treatment, at the end of treatment, or after treatment was discontinued.
It is not clear from the evidence reviewed whether any oral interventions (magnesium, calcium, calcium with vitamin D, B vitamins, vitamin D, or vitamin C) are an effective and safe treatment for leg cramps during pregnancy.