Runny nose and watery eyes on one side of face
Hay Fever (Rhinitis) | Symptoms & Treatment
Symptoms
People with allergic rhinitis generally experience symptoms after breathing in an allergy-causing substance such as pollen or dust. In the spring, the most common triggers are tree and grass pollen. In the fall, a common allergen is ragweed or other weed pollens or outdoor mold.
When a sensitive person inhales an allergen, the body’s immune system may react with the following symptoms (listed in order of frequency):
- Stuffy nose due to blockage or congestion
- Runny nose or post nasal drainage
- Itching, usually in the nose, mouth, eyes, or throat
- Red and watery eyes
- Puffy, swollen eyelids
- Sneezing
- Cough
Symptoms also may be triggered by common irritants such as:
- Cigarette smoke
- Strong odors, such as perfume, or hair spray and fumes
- Cleaning solutions, pool chlorine, car exhaust and other air pollutants (i.e., ozone)
- Air fresheners
There are two types of allergic rhinitis:
- Seasonal: Symptoms can occur in spring, summer, and early fall.
They are usually caused by sensitivity to airborne mold spores or to pollens from trees, grasses, or weeds.
- Perennial: Symptoms occur year-round and are generally caused by sensitivity to dust mites, pet hair or dander, cockroaches or mold.
Allergic rhinitis can be associated with:
- Decreased concentration and focus
- Limited activities
- Decreased decision-making capacity
- Impaired hand-eye coordination
- Problems remembering things
- Irritability
- Sleep disorders
- Fatigue
- Missed days of work or school
- More motor vehicle accidents
- More school or work injuries
Many parents of children with allergic rhinitis have said that their children are more moody and irritable during allergy season. Since children cannot always express their symptoms verbally, they may express their discomfort by acting up at school and at home. In addition, some children feel that having an allergy is a stigma that separates them from others.
It is important that the irritability or other symptoms caused by allergy symptoms are not mistaken for attention deficit disorder. With proper treatment, symptoms can be kept under control and disruptions in learning and behavior can be avoided.
Symptoms of allergic rhinitis have other causes as well, the most customary being the common cold – an example of infectious rhinitis. Most infections are relatively short-lived, with symptoms improving in three to seven days.
Many people have recurrent or chronic nasal congestion, excess mucus production, itching and other nasal symptoms similar to those of allergic rhinitis. In those cases, an allergy may not be the cause.
Diagnosing
Occasional allergies aren’t just something you have to live with. Consulting an allergist is the most effective way to diagnose and treat allergic rhinitis symptoms and help you find relief.
Your allergist may start by taking a detailed history, looking for clues in your lifestyle that will help pinpoint the cause of your symptoms. You’ll be asked, among other things, about your work and home environments (including whether you have a pet) your family’s medical history and the frequency and severity of your symptoms.
You’ll be asked, among other things, about your work and home environments (including whether you have a pet) your family’s medical history and the frequency and severity of your symptoms.
Sometimes allergic rhinitis can be complicated by several medical conditions, such as a deviated septum (curvature of the bone and cartilage that separate the nostrils) or nasal polyps (abnormal growths inside the nose and sinuses). Any of these conditions will be made worse by catching a cold. Nasal symptoms caused by more than one problem can be difficult to treat, often requiring the cooperation of an allergist and another specialist, such as an otolaryngologist (ear, nose, and throat specialist surgeon).
Your allergist may recommend a skin test, in which small amounts of suspected allergens are introduced into your skin. Skin testing is the easiest, most sensitive, and generally least expensive way of identifying allergens.
Types of skin tests
- Prick or scratch test: In this test, a tiny drop of a possible allergen is pricked or scratched into the skin.
 Also known as a percutaneous test, this is the most common type of skin test. The results are known within 10 to 20 minutes.
Also known as a percutaneous test, this is the most common type of skin test. The results are known within 10 to 20 minutes. - Intradermal test: A small amount of a possible allergen is injected under the skin using a thin needle. The site is checked for a reaction after about 20 minutes. This test is typically more sensitive than the prick or scratch test.
Management and Treatment
Avoidance
The first approach in managing seasonal or perennial forms of allergic rhinitis or hay fever should be to avoid the allergens that trigger symptoms, if possible.
Outdoor exposure
- Stay indoors as much as possible when pollen counts are at their peak, usually during the midmorning and early evening (this may vary according to plant pollen), and when wind is blowing pollens around.
- Avoid using window fans that can draw pollens and molds into the house.
- Wear glasses or sunglasses when outdoors to minimize the amount of pollen getting into your eyes.

- Don’t hang clothing outdoors to dry; pollen may cling to towels and sheets.
- Try not to rub your eyes; doing so will irritate them and could make your symptoms worse.
Indoor exposure
- Keep windows closed and use air conditioning in your car and home. Make sure to keep your air conditioning unit clean.
- Reduce exposure to dust mites, especially in the bedroom. Use “mite-proof” covers for pillows, comforters and duvets, and mattresses and box springs. Wash your bedding frequently, using hot water (at least 130 degrees Fahrenheit).
- To limit exposure to mold, keep the humidity in your home low (between 30 and 50 percent) and clean your bathrooms, kitchen, and basement regularly. Use a dehumidifier, especially in the basement and in other damp, humid places, and empty and clean it often. If mold is visible, clean it with mild detergent and a 5 percent bleach solution as directed by an allergist.
- Clean floors with a damp rag or mop, rather than dry-dusting or sweeping.
Exposure to pets
- Wash your hands immediately after petting any animals; wash your clothes after visiting friends with pets.
- If you are allergic to a household pet, keep your pet out of your home as much as possible. If the pet must be inside, keep it out of your bedroom so you are not exposed to pet allergens while you sleep.
- Close the air ducts to your bedroom if you have forced-air or central heating or cooling. Replace carpeting with hardwood, tile, or linoleum, all of which are easier to keep dander-free.
Medications
Many allergens that trigger allergic rhinitis are airborne, so you can’t always avoid them. If your symptoms can’t be well-controlled by simply avoiding triggers, your allergist may recommend medications that reduce nasal congestion, sneezing, and an itchy and runny nose. They are available in many forms – oral tablets, liquid medication, nasal sprays and eyedrops. Some medications may have side effects, so discuss these treatments with your allergist so they can help you live the life you want.
Intranasal corticosteroids
Intranasal corticosteroids are the single most effective drug class for treating allergic rhinitis. They can significantly reduce nasal congestion as well as sneezing, itching and a runny nose.
Ask your allergist about whether these medications are appropriate and safe for you. These sprays are designed to avoid the side effects that may occur from steroids that are taken by mouth or injection. Take care not to spray the medication against the center portion of the nose (the nasal septum). The most common side effects are local irritation and nasal bleeding. Some older preparations have been shown to have some effect on children’s growth; data about some newer steroids don’t indicate an effect on growth.
Antihistamines
Antihistamines are commonly used to treat allergic rhinitis. These medications counter the effects of histamine, the irritating chemical released within your body when an allergic reaction takes place. Although other chemicals are involved, histamine is primarily responsible for causing the symptoms. Antihistamines are found in eyedrops, nasal sprays and, most commonly, oral tablets and syrup.
Antihistamines are found in eyedrops, nasal sprays and, most commonly, oral tablets and syrup.
Antihistamines help to relieve nasal allergy symptoms such as:
- Sneezing and an itchy, runny nose
- Eye itching, burning, tearing and redness
- Itchy skin, hives and eczema
There are dozens of antihistamines; some are available over the counter, while others require a prescription. Patients respond to them in a wide variety of ways.
Patients respond to them in a wide variety of ways.
Generally, the newer (second-generation) products work well and produce only minor side effects. Some people find that an antihistamine becomes less effective as the allergy season worsens or as their allergies change over time. If you find that an antihistamine is becoming less effective, tell your allergist, who may recommend a different type or strength of antihistamine. If you have excessive nasal dryness or thick nasal mucus, consult an allergist before taking antihistamines. Contact your allergist for advice if an antihistamine causes drowsiness or other side effects.
Proper use: Short-acting antihistamines can be taken every four to six hours, while timed-release antihistamines are taken every 12 to 24 hours. The short-acting antihistamines are often most helpful if taken 30 minutes before an anticipated exposure to an allergen (such as at a picnic during ragweed season). Timed-release antihistamines are better suited to long-term use for those who need daily medications. Proper use of these drugs is just as important as their selection. The most effective way to use them is before symptoms develop. A dose taken early can eliminate the need for many later doses to reduce established symptoms. Many times, a patient will say that he or she “took one, and it didn’t work.” If the patient had taken the antihistamine regularly for three to four days to build up blood levels of the medication, it might have been effective.
Proper use of these drugs is just as important as their selection. The most effective way to use them is before symptoms develop. A dose taken early can eliminate the need for many later doses to reduce established symptoms. Many times, a patient will say that he or she “took one, and it didn’t work.” If the patient had taken the antihistamine regularly for three to four days to build up blood levels of the medication, it might have been effective.
Side effects: Older (first-generation) antihistamines may cause drowsiness or performance impairment, which can lead to accidents and personal injury. Even when these medications are taken only at bedtime, they can still cause considerable impairment the following day, even in people who do not feel drowsy. For this reason, it is important that you do not drive a car or work with dangerous machinery when you take a potentially sedating antihistamine. Some of the newer antihistamines do not cause drowsiness.
A frequent side effect is excessive dryness of the mouth, nose, and eyes. Less common side effects include restlessness, nervousness, overexcitability, insomnia, dizziness, headaches, euphoria, fainting, visual disturbances, decreased appetite, nausea, vomiting, abdominal distress, constipation, diarrhea, increased or decreased urination, urinary retention, high or low blood pressure, nightmares (especially in children), sore throat, unusual bleeding or bruising, chest tightness or palpitations. Men with prostate enlargement may encounter urinary problems while on antihistamines. Consult your allergist if these reactions occur.
Less common side effects include restlessness, nervousness, overexcitability, insomnia, dizziness, headaches, euphoria, fainting, visual disturbances, decreased appetite, nausea, vomiting, abdominal distress, constipation, diarrhea, increased or decreased urination, urinary retention, high or low blood pressure, nightmares (especially in children), sore throat, unusual bleeding or bruising, chest tightness or palpitations. Men with prostate enlargement may encounter urinary problems while on antihistamines. Consult your allergist if these reactions occur.
Important precautions:
- Follow your allergist’s instructions.
- Alcohol and tranquilizers increase the sedation side effects of antihistamines.
- Do not use more than one antihistamine at a time, unless prescribed.
- Keep these medications out of the reach of children.
- Know how the medication affects you before working with heavy machinery, driving, or doing other performance-intensive tasks; some products can slow your reaction time.

- Some antihistamines appear to be safe to take during pregnancy, but there have not been enough studies to determine the absolute safety of antihistamines in pregnancy. Again, consult your allergist or your obstetrician if you are pregnant or considering getting pregnant.
- While antihistamines have been taken safely by millions of people in the last 50 years, don’t take antihistamines before telling your allergist if you are allergic to, or intolerant of, any medicine; are pregnant or intend to become pregnant while using this medication; are breast-feeding; have glaucoma or an enlarged prostate; or are ill.
- Never take anyone else’s medication.
Decongestants
Decongestants help relieve the stuffiness and pressure caused by swollen nasal tissue. They do not contain antihistamines, so they do not cause antihistaminic side effects. They do not relieve other symptoms of allergic rhinitis. Oral decongestants are available as prescription and nonprescription medications and are often found in combination with antihistamines or other medications. It is not uncommon for patients using decongestants to experience insomnia if they take the medication in the afternoon or evening. If this occurs, a dose reduction may be needed. At times, men with prostate enlargement may encounter urinary problems while on decongestants. Patients using medications to manage emotional or behavioral problems should discuss this with their allergist before using decongestants. Patients with high blood pressure or heart disease should check with their allergist before using. Pregnant patients should also check with their allergist before starting decongestants.
It is not uncommon for patients using decongestants to experience insomnia if they take the medication in the afternoon or evening. If this occurs, a dose reduction may be needed. At times, men with prostate enlargement may encounter urinary problems while on decongestants. Patients using medications to manage emotional or behavioral problems should discuss this with their allergist before using decongestants. Patients with high blood pressure or heart disease should check with their allergist before using. Pregnant patients should also check with their allergist before starting decongestants.
Nonprescription decongestant nasal sprays work within minutes and last for hours, but you should not use them for more than a few days at a time unless instructed by your allergist. Prolonged use can cause rhinitis medicamentosa or rebound swelling of the nasal tissue, leading to more frequent congestion and need to re-dose medication more frequently than recommended. Stopping the use of the decongestant nasal spray will cure the swelling if there is no underlying disorder.
Other nasal sprays
Nonprescription saline nasal sprays will help counteract symptoms such as dry nasal passages or thick nasal mucus. Unlike decongestant nasal sprays, a saline nasal spray can be used as often as it is needed. Sometimes an allergist may recommend washing (douching) the nasal passage. There are many OTC delivery systems for saline rinses, including neti pots and saline rinse bottles.
Nasal cromolyn (Nasalcrom) blocks the body’s release of allergy-causing substances. It does not work in all patients. The full dose is four times daily, and improvement of symptoms may take several weeks. Nasal cromolyn can help prevent allergic nasal reactions if taken prior to an allergen exposure.
Nasal ipratropium bromide spray (Atrovent) can help reduce nasal drainage from allergic rhinitis or some forms of nonallergic rhinitis.
Another prescription nasal spray option is an intranasal antihistamine. These medications, such as azelastine (Astelin) or olopatadine (Patanase), are older antihistamines with some allergy cell stabilizing properties that can be used alone or with other medications including oral antihistamines and intranasal steroids. One nice feature of these medications is that they work quickly enough that they can be used as needed rather than every day. They can also help relieve nasal congestion and post nasal drainage but can cause sedation in some patients. Azelastine in particular may have an unpleasant taste.
One nice feature of these medications is that they work quickly enough that they can be used as needed rather than every day. They can also help relieve nasal congestion and post nasal drainage but can cause sedation in some patients. Azelastine in particular may have an unpleasant taste.
Leukatriene pathway inhibitors
Leukotriene pathway inhibitors (montelukast, zafirlukast and zileuton) block the action of leukotriene, a substance in the body that can cause symptoms of allergic rhinitis. These drugs are also used to treat asthma and are only available by prescription. Montelukast was recently given a warning from the FDA regarding potential behavioral changes.
ImmunotherapyImmunotherapy may be recommended for people who don’t respond well to treatment with medications or who experience side effects from medications, who have allergen exposure that is unavoidable or who desire a more permanent solution to their allergies. Immunotherapy can be very effective in controlling allergic symptoms, but it doesn’t help the symptoms produced by nonallergic rhinitis.
Two types of immunotherapy are available: allergy shots and sublingual (under-the-tongue) tablets.
- Allergy shots: A treatment program, which typically continues for three to five years, consists of injections of a diluted allergy extract, administered frequently in increasing doses until a maintenance dose is reached. Then the injection schedule is changed so that the same dose is given with longer intervals between injections. Immunotherapy helps the body build tolerance to the effects of the allergen, reduces the intensity of symptoms caused by allergen exposure and sometimes can make skin test reactions disappear.
 As tolerance develops over several months, symptoms should improve.
As tolerance develops over several months, symptoms should improve. - Sublingual tablets: This type of immunotherapy was approved by the Food and Drug Administration in 2014. Starting several months before allergy season begins, patients dissolve a tablet under the tongue daily. Some patients benefit from year-round treatment. Treatment can continue for as long as three years. Only a few allergens (certain grass and ragweed pollens and house dust mite) can be treated now with this method, but it is a promising therapy for the future.
Eye allergy preparations and eyedrops
Eye allergy preparations may be helpful when the eyes are affected by the same allergens that trigger rhinitis, causing redness, swelling, watery eyes and itching. OTC eyedrops and oral medications are commonly used for short-term relief of some eye allergy symptoms. They may not relieve all symptoms, though, and prolonged use of some of these drops may cause your condition to worsen.
Prescription eyedrops and oral medications also are used to treat eye allergies. Prescription eyedrops provide both short- and long-term targeted relief of eye allergy symptoms.
Check with your allergist or pharmacist if you are unsure about a specific drug or formula.
Treatments that are not recommended for allergic rhinitis
- Antibiotics: Effective for the treatment of bacterial infections, antibiotics do not affect the course of uncomplicated common colds (a viral infection) and are of no benefit for noninfectious rhinitis, including allergic rhinitis.
- Nasal surgery: Surgery is not a treatment for allergic rhinitis, but it may help if patients have nasal polyps or chronic sinusitis that is not responsive to antibiotics or nasal steroid sprays.
Occupational Rhinitis
If you develop symptoms that resemble those of hay fever and that appear or become more serious at work, you may be suffering from occupational rhinitis.
Occupational rhinitis, or work-related rhinitis, is a condition in which symptoms are triggered or further aggravated by allergens in the workplace. These symptoms can include sneezing, a runny nose and watering eyes. Common triggers include cleaning products, chemical fumes, certain types of dust, and corrosive gases.
If your allergy symptoms appear at work, or seem to get worse there, ask your allergist to help you identify potential triggers and develop a treatment plan.
Rhinitis | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is rhinitis?
Rhinitis is when a reaction occurs that causes a stuffy nose, runny nose, sneezing, and itching. Most types of rhinitis are caused by an inflammation and lead to symptoms in the eyes, ears, or throat. There are several types of rhinitis. The most common types of rhinitis are:
Most types of rhinitis are caused by an inflammation and lead to symptoms in the eyes, ears, or throat. There are several types of rhinitis. The most common types of rhinitis are:
- Acute rhinitis, which is often caused by a viral illness
- Allergic rhinitis (can be seasonal or year round)
- Nonallergic rhinitis
Allergic rhinitis is caused when allergens in the air trigger the release of histamine in the nose and sinuses. Histamine causes itching, swelling, and fluid to build up in the fragile linings of the nasal passages, sinuses, and eyelids.
What causes rhinitis?
The most common causes of rhinitis are:
- Pollen given off by trees, grass, and weeds
- Dust mites
- Mold
- Cockroach waste
- Animal dander
- Fumes and odors
- Extreme temperature or changes in temperature
- Hormonal changes
- Certain medicines and overuse of topical nose sprays
- Changes in the environment
- Irritants such as strong odors and tobacco smoke
- Certain foods or spices
Who is at risk for rhinitis?
People with asthma are at a higher risk for rhinitis. Allergic rhinitis is a common problem that may be linked to asthma. But this link is not fully understood. Experts think that since rhinitis makes it hard to breathe through the nose, it's harder for the nose to work normally. Breathing through the mouth does not warm, filter, or humidify the air before it enters the lungs. This can make asthma symptoms worse.
Allergic rhinitis is a common problem that may be linked to asthma. But this link is not fully understood. Experts think that since rhinitis makes it hard to breathe through the nose, it's harder for the nose to work normally. Breathing through the mouth does not warm, filter, or humidify the air before it enters the lungs. This can make asthma symptoms worse.
Asthma and allergies are also caused by many of the same chemical triggers in the body.
Controlling allergic rhinitis may help control asthma in some people.
What are the symptoms of rhinitis?
Symptoms of rhinitis include:
- Sneezing
- Stuffy nose
- Runny nose
- Itchy nose, throat, eyes, and ears
- Nosebleeds
- Clear drainage from the nose
- Ear infections that keep coming back
- Snoring
- Breathing through the mouth
How is rhinitis diagnosed?
Most often, the diagnosis is made by your healthcare provider based on a full health history and physical exam.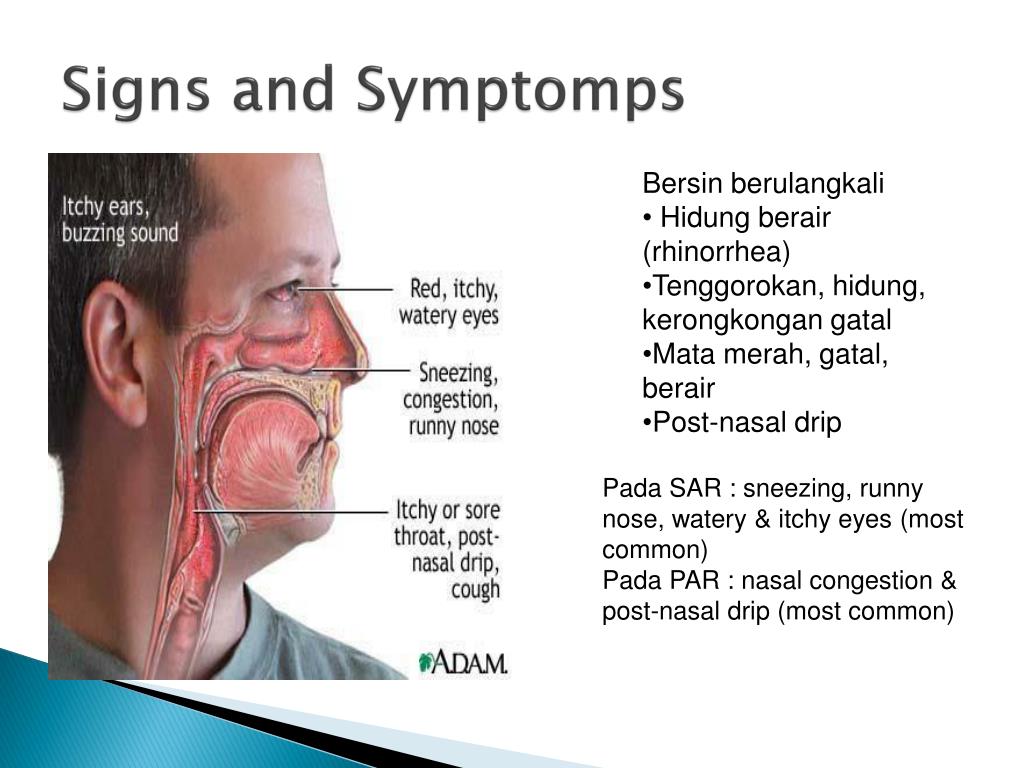 In addition to the above signs, the healthcare provider may find:
In addition to the above signs, the healthcare provider may find:
- Dark circles under the eyes (more common in children)
- Creases under the eyes
- Swollen tissues inside the nose
- Mouth breathing
How is rhinitis treated?
Staying away from the allergens that are causing the problem is the best treatment. Sometimes it can be hard to stay away from triggers (including allergens), such as pollens. The symptoms of rhinitis sometimes look like other conditions or health problems. Always see your healthcare provider for a diagnosis.
Treatments for rhinitis may include:
- Antihistamines
- Nose sprays
- Decongestants
- Medicines for asthma symptoms
- Allergy shots
- Surgery for some health problems
Can I prevent rhinitis?
Preventive measures depend on what triggers your rhinitis.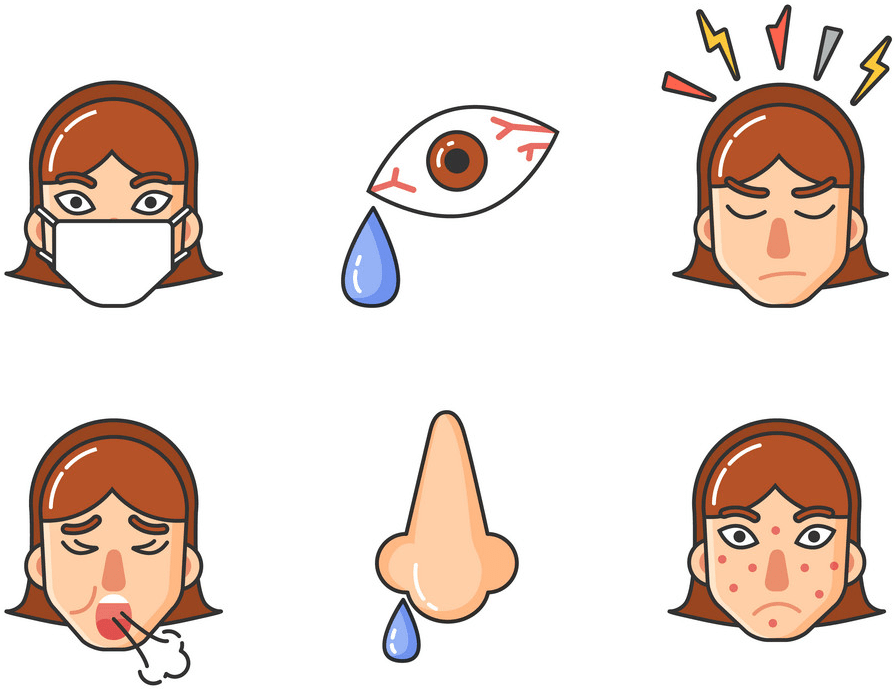 These can include:
These can include:
- Staying away from areas where there is heavy dust, mites, or molds
- Not being around pets
- Staying away from what you know you are allergic to, or what triggers your rhinitis
- Controls in your environment, such as air conditioning during pollen season
- Staying away from people who are smoking
- Staying away from strong odors and irritants when possible
- Using nose sprays only for the prescribed length of time
Key points about rhinitis
- Allergic rhinitis is a reaction that happens in the eyes, nose, and throat when allergens in the air trigger histamine to be released in the body.
- Some of the most common causes of allergic rhinitis are pollen, dust mites, mold, cockroach waste, animal dander
- Nonallergic rhinitis is inflammation in the nose, eyes, and throat from nonallergic sources such as fumes and odors, hormonal changes, and smoke.

- Symptoms of rhinitis include sneezing, stuffy and runny nose, nosebleeds, and itchy throat, eyes, and ears.
- Treatment may include medicines, allergy shots, and surgery for some health problems.
- Preventive measures for rhinitis include staying away from what you are allergic to and avoiding your triggers.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.

- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.

Medical Reviewer: Deborah Pedersen MD
Medical Reviewer: Marianne Fraser MSN RN
Medical Reviewer: Daphne Pierce-Smith RN MSN
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Edema of the mucous membrane of the sinuses of the nose
Co-author, editor and medical expert - Maksimov Alexander Alekseevich.
Date last updated: 10/26/2022
Number of views: 267,666.
Average reading time: 5 minutes.
Contents:
Causes
Symptoms
Consequences
Diagnosis
Treatment
The bones of the facial skull are covered with a mucous membrane of the airways 4 . In anatomical terminology, they are called paranasal (paranasal) sinuses 4 , which are capable of self-cleaning 1 . Normally, about 40-60% of microbes and dust particles that enter the nasal cavity with inhaled air are neutralized and removed along with nasal mucus 1 . With a properly functioning airway self-cleaning mechanism, all foreign agents are removed through natural openings (ostia) 1 , connecting the airways with the nasal cavity 4.6 . However, in case of inflammation of the paranasal sinuses, the mucous membrane swells due to increased blood and lymph flow, partially or completely blocking the communication routes 5.6 . This pathological condition is called edema of the mucous membrane of the paranasal sinuses 6 .
Normally, about 40-60% of microbes and dust particles that enter the nasal cavity with inhaled air are neutralized and removed along with nasal mucus 1 . With a properly functioning airway self-cleaning mechanism, all foreign agents are removed through natural openings (ostia) 1 , connecting the airways with the nasal cavity 4.6 . However, in case of inflammation of the paranasal sinuses, the mucous membrane swells due to increased blood and lymph flow, partially or completely blocking the communication routes 5.6 . This pathological condition is called edema of the mucous membrane of the paranasal sinuses 6 .
Up to content
Causes
Swelling of the sinuses is a fairly common phenomenon in otolaryngology 2 that occurs due to various reasons 7 . It can be caused by:
- hypothermia 7 ;
- infections of the upper respiratory tract 5.7 ;
- exposure to adverse environmental factors 5.
 7 ;
7 ; - mechanical trauma to the nose 5 ;
- substances of an allergic nature 5.7 ;
- polyps 8 or adenoids 6 ;
- deviated septum and other developmental anomalies 5,6,8 .
Up to contents
Symptoms
Clinical manifestations of paranasal sinus edema are divided into inflammatory and functional.
| Inflammatory symptoms | These include hyperemia, swelling of the affected area, burning, drying of the nasal mucosa, heaviness in the head, nasal congestion, sneezing, lacrimation, headaches of varying intensity and localization, weakness, fever body 6,8,9 . |
| Functional disorders | Manifested by a change in the nature of mucus 8 , impaired nasal breathing and sense of smell 9 , dysphonia (change in voice, strength and timbre 90 190 2). |
Up to the content0025 11 . A breakthrough of pus into the surrounding soft tissues can provoke the development of the following complications:
- osteomyelitis of the jawbone 15 ;
- trigeminal neuritis 16 ;
- atrophy of the nasal mucosa 8 ;
- inflammation of the meninges (meningitis) 11 ;
- brain abscess 11 ;
- inflammation of the optic nerve 11.16 .
Top of page
Diagnosis
Diagnosis of paranasal edema includes the following activities: physical examination, instrumental and laboratory examinations.
| Physical examination 17 | Manual examination (palpation 12 ) of the area of the affected sinus determines the severity of edematous-infiltrative changes. |
| Instrumental examinations | Instrumental methods for detecting edema of the nasal mucosa include anterior and posterior rhinoscopy 6 , microrhinoscopy 13 and fibroendoscopy 13. |
| Laboratory examinations | Laboratory diagnostics includes examination of the pathological secretion of the nasal cavity, involving the use of bacteriological 5.12 , biochemical 17 , cytological 17 and immunological methods 14.17 . |
Additionally, according to medical indications, the patient may be prescribed fluoroscopy or diaphonoscopy 14 .
Up the content
Treatment
| The use of local vasoconstrictor drugs | includes nasal drops and sprays 8 , eliminating mucous membranes and quickly eliminating the inextricable symptoms0025 9 . Topical decongestants are symptomatic treatments and should be used strictly as directed in 9 . |
| Antibacterial therapy | It is prescribed only after confirmation of the bacterial nature of the disease 3. |
| Antiallergic treatment | The indication for the use of antihistamines is the high susceptibility of the human body to foreign proteins (allergens) 6 . |
Tizin ® - a tool that facilitates nasal breathing 18
Tizin ® is a vasomic drug for a symptomatic use, containing an active active substance that helps relieve swelling of nasal pussies and murder breathing 18 . This is an over-the-counter drug approved for use in children and adults (in the appropriate concentration - 0.05% or 0.1%) 18 . It is recommended to use in situations where you need to quickly eliminate nasal congestion.
The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
Read also:
Why the nose is blocked
Nasal congestion without runny nose
Neuritis of the facial nerve / Diseases / Clinic EXPERT
Neuritis of the facial nerve or Bell's palsy is a lesion of the facial nerve, manifested by unilateral paresis or paralysis of the mimic muscles of the face. As a result, weakness develops in these muscles, leading to a decrease (paresis) or complete absence (paralysis) of facial movements and the appearance of facial asymmetry.
As a result, weakness develops in these muscles, leading to a decrease (paresis) or complete absence (paralysis) of facial movements and the appearance of facial asymmetry.
Neuritis of the facial nerve affects one of 3-5 thousand people. Neuritis of the facial nerve is possible in any age group, the average age of the diseased is 40 years. Men and women in general are equally affected.
Causes
Depending on whether the facial nerve is caused by an infection or not, a distinction is made between primary neuritis of the facial nerve (non-infectious) and secondary, or symptomatic, neuritis of the facial nerve (infectious).
The most common causes of primary neuritis of the facial nerve are:
- local hypothermia of the neck and ear, especially under the influence of cold, wind, draft or air conditioning
- insufficient blood supply (ischemia) to the nerve due to vascular problems circulatory disorders in the vertebral artery.).
It is generally accepted that secondary neuritis of the facial nerve is associated with an infectious factor, primarily with the herpes simplex virus type I. In addition to herpes, it can be caused by an ear disease - otitis media, eustachitis, mastoiditis (the so-called otogenic neuritis).
In addition to herpes, it can be caused by an ear disease - otitis media, eustachitis, mastoiditis (the so-called otogenic neuritis).
It should be noted that neuritis of the facial nerve can occur without an inflammatory process. In such cases, experts talk about neuropathy of the facial nerve.
Symptoms
Usually, facial neuritis develops gradually. At the beginning there is pain behind the ear, after 1-2 days the asymmetry of the face becomes noticeable, a characteristic facial asymmetry is created on the side of the affected nerve:
- smoothing of the nasolabial fold
- absence of folds on the corresponding half of the forehead
- lagophthalmos ("hare's eye") - a white strip of sclera between the iris and the lower eyelid
- may cause dry eyes or watery eyes. In some cases, a symptom of "crocodile tears" develops - against the background of constant dryness of the eye, the patient lacrimation occurs during meals.

Healthy side:
- sharp lowering of the corner of the mouth to the healthy side, as a result, the face is distorted to the healthy side
- less sharp pulling of the nose to the healthy side.
All these disorders are especially noticeable when trying to make active mimic movements.
Patient unable to close eyelids. When he tries to do this, his eye turns upward (Bell's symptom).
Weakness of facial muscles is manifested by the inability to move them:
- when the teeth are bared, the mouth and nose are pulled even more sharply to the healthy side
- inflation of the cheeks fails
- when frowning, vertical wrinkles do not appear on the diseased side
- when the eyebrows are raised upward, there are no horizontal wrinkles on the forehead due to insufficient salivation functions of the muscles of the mouth.
Additional symptoms may join the main picture:0056

Diagnosis
The main method of examination for neuritis of the facial nerve is an examination by a neurologist, however, in some cases, additional laboratory and instrumental studies are required, which depend on the symptoms identified by the neurologist:
- measurement of blood pressure
- dopplerography and duplex examination of the vessels of the head and neck
In some cases, the doctor may prescribe:
It is especially important that in the conditions of the EXPERT Clinic, a collegiate discussion of the patient's problem with doctors of other specialties (consilium of a general practitioner, endocrinologist, otorhinolaryngologist, immunologist, dentist, etc.) is possible. This allows you to reduce the number of "unnecessary" examinations and speed up the correct diagnosis, and hence the appointment of adequate treatment.
Treatment
The effectiveness of the treatment of neuritis of the facial nerve depends on the correct identification of the cause and the timely initiation of therapy. As a rule, if a patient goes to a neurologist as soon as possible, then the likelihood of recovery is much greater.
As a rule, if a patient goes to a neurologist as soon as possible, then the likelihood of recovery is much greater.
Do not self-medicate!
When neuritis of the facial nerve is diagnosed, treatment should be started as early as possible - preferably within the first hours after the onset of symptoms. In this case, the success of the treatment of neuritis of the facial nerve will be maximum and in 75-80% of cases it will completely eliminate the symptoms of the disease. Treatment is carried out individually, depending on the cause of the symptoms.
During the 1st week of illness, the affected muscles need rest. During this period, the following are prescribed:
- dehydrating drugs
- vasodilators
- B vitamins
- in the presence of an inflammatory process and pain syndrome, painkillers and anti-inflammatory drugs are indicated
- short courses of treatment with hormonal drugs
- from non-contact heat therapy - physiotherapy procedures.

On the 2nd week, massage is started, exercise therapy with a gradually increasing load, adhesive plaster fixation of the affected muscles is carried out, paraffin applications are used. From the end of the 2nd week, the use of anticholinesterase drugs and dibazol is advisable; more intensive physical therapy. In some cases, conduct electrical stimulation.
After 2-3 months, with incomplete recovery, it is advisable to prescribe biostimulants. Reflexology should also be used. With neuritis of the facial nerve, therapeutic facial massage is also useful.
Eye care for neuritis of the facial nerve includes:
- instillation of artificial lacrimal fluid or saline solution (every 1-2 hours)
- wearing glasses
- wearing a wet patch on the eye medical paper
- never use medical products made of cotton for contact with the eye, as cotton scratches the eyeball
- in case of any discomfort in the eye, redness - it is necessary to consult an ophthalmologist.

In the conditions of the EXPERT Clinic, the attending physician can help the patient by prescribing treatment in the comfortable conditions of a day hospital.
Prognosis
Prognosis of neuritis of the facial nerve depends on its location and the presence of concomitant pathology (otitis media, mumps, herpes). In 75% of cases, a complete recovery occurs, but with a disease duration of more than 3 months, complete recovery of the nerve is much less common. Recurrent neuritis has a favorable prognosis, but each subsequent relapse is more severe and prolonged.
Severe forms can cause the following complications:
- irreversible damage to the facial nerve
- improper regrowth of nerve fibers, which leads to involuntary movement of some muscles when a person tries to use others - synkinesis (for example, when a person smiles, they may involuntarily close eyes)
- partial or complete loss of vision caused by the inability to lower the eyelids and, as a result, excessive dryness of the eyes.

In case of persistent residual effects in the long-term period (after 2 years), the issue of surgical treatment is resolved
Recommendations
complex treatment, we recommend that you consult a qualified neurologist.
Frequently Asked Questions
Is it possible to massage the face with neuritis of the facial nerve?
Conventional classical massage for neuritis is not indicated, because this can lead to contractures of the facial muscles on the affected side. A special "point" massage and physiotherapy exercises are shown.
I had neuritis of the facial nerve 3 times. Is there a preventive treatment to avoid it again?
It all depends on the causes of recurrent neuritis of the facial nerve. If it is provoked by a vasoneural conflict (of the facial nerve and blood vessels), then it is possible to quickly eliminate this conflict. In other cases, provoking factors should be avoided (general and local hypothermia - parotid region, etc.

 14 .
14 .  5 .
5 .