Vaccine birth defects
COVID-19 vaccine not associated with birth defects detectable on ultrasound
Findings fill gap left vacant when pregnant people were excluded from the initial trials
April 4, 2022 | By Kristin Samuelson
Dr. Emily Miller (right) and fellow study author Dr. Rachel Ruderman.
- COVID-19
- Feinberg School of Medicine
- Medicine
- Women’s Health
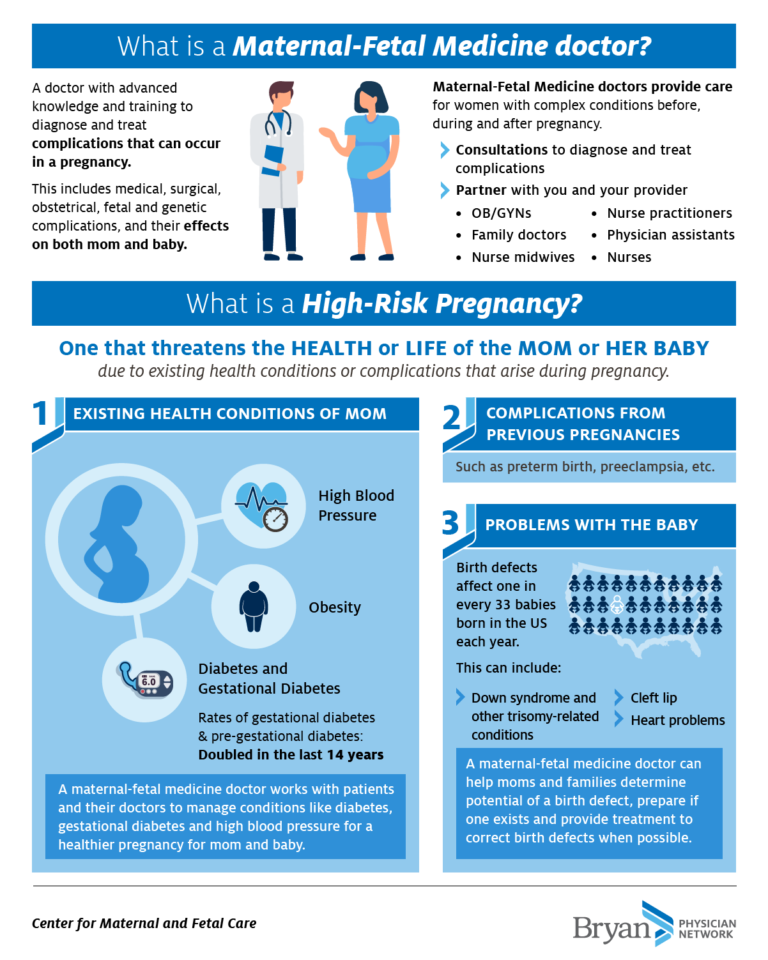
The exclusion of pregnant patients in initial COVID-19 vaccine clinical trials left many patients and doctors wondering how the vaccine might affect pregnant patients and their unborn babies. But a new Northwestern Medicine study finds the vaccine is not associated with birth defects that are detectable on ultrasound.
“This is yet another important piece of data that helps bridge the chasm that was left when pregnant individuals were excluded from those initial vaccine trials,” said corresponding author Dr. Emily Miller, chief of obstetrics at Northwestern Medicine and assistant professor of maternal fetal medicine at Northwestern University Feinberg School of Medicine.
The study was published April 4 in the journal JAMA Pediatrics.
“One of the reasons women struggle with the vaccine in pregnancy is they’re worried about their babies and don’t want to take any risks,” said first author Dr. Rachel Ruderman, a fourth-year resident in obstetrics and gynecology at Feinberg. “This study shows there really is no increased risk of birth defects, and it supports other evidence that shows the vaccine is safe and beneficial for mom and baby.”
Looking for a wide range of birth defects
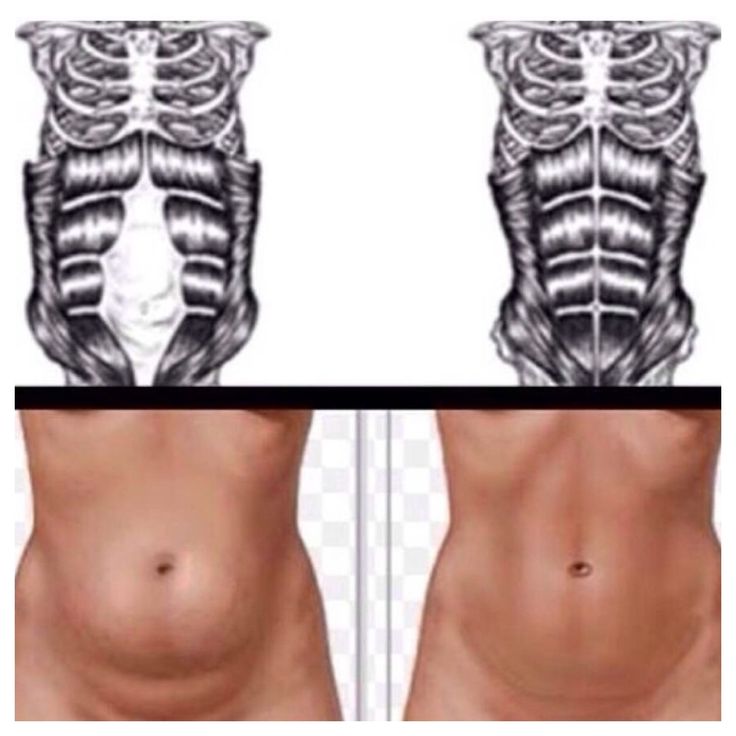
The types of birth defects the scientists were looking for on the study participants’ ultrasounds were ones they deemed “major fetal structural anomalies,” such as the baby’s heart not forming correctly or the spine not closing properly. In the United States, 3 to 5% of births are impacted by these types of defects, resulting in increases in infant morbidity, mortality and billions of dollars in cost.
“During the early part of pregnancy when the organs are forming, there can be abnormalities in how they form, and they can take the form of birth defects that can have implications for the life of the child,” Miller said.
“For example, if the baby’s heart isn’t forming correctly, that could lead to the baby needing major cardiac surgery or long-term medication,” Miller said. “However, if the ultrasound identified extra fluid in the fetus’ kidney, that might end up fixing itself down the road. We looked for those extremes and everything in between.”
Advancing CDC findings
The U.S. Centers for Disease Control and Prevention (CDC) in September 2021 released similar findings from its study in pregnant individuals. This study builds on and advances the CDC’s data, Miller said.
While the CDC compared its study data to historical data, the new Northwestern study used contemporary controls—current pregnant patients who chose not to get vaccinated or were not vaccinated within the window the scientists defined as of biologic risk for birth defects (having received vaccination from 30 days prior to conception until 14 weeks gestational age).1.jpg)
“I think the big strength of this study is that we compared against other women who were vaccinated, but at different point in their pregnancies,” Miller said. “People who choose vaccination are often different from people who choose not to be vaccinated. Our study design helps account for some of those differences.”
The study analyzed electronic medical records (including ultrasounds and COVID-19 vaccination records) from a cohort of 3,156 pregnant people who received a complete fetal anatomical survey (19-week ultrasound) at Northwestern Medicine Prentice Women’s Hospital between March and November 2021. Of those pregnant patients, 2,622 (83.1%) received at least one vaccine dose and 1,149 (43.8%) were vaccinated inside of the scientists’ defined vaccination window (30 days prior to conception until 14 weeks gestational age).
Boosting trust in vaccines?
Both Miller and Ruderman see patients at Prentice. As part of her residency, Ruderman also sees patients at the John H. Stroger, Jr. Hospital of Cook County. Despite new and emerging data that continue to support the safety of vaccination among pregnant individuals, hesitancy is still present, they said.
Stroger, Jr. Hospital of Cook County. Despite new and emerging data that continue to support the safety of vaccination among pregnant individuals, hesitancy is still present, they said.
“Patients say, ‘I don’t think the data is good, and everyone is getting COVID anyway, so why would I expose my baby?’” said Ruderman, who received her booster shot during week 12 of pregnancy. “Then I tell people, ‘Actually, the data is really good,’ and I feel like they’re receptive. So, these findings will only add to that.”
For Journalists: view the news release for media contacts and assets
Editor’s Picks
Investing in new water filtration membranes is worth it
September 12, 2022
Martins drive support for Law School faculty through matching gift challenge
September 22, 2022
CRISPR pioneer Jennifer Doudna receives inaugural Kimberly Prize
September 14, 2022
Never miss a story:
Get the latest stories from Northwestern Now sent directly to your inbox.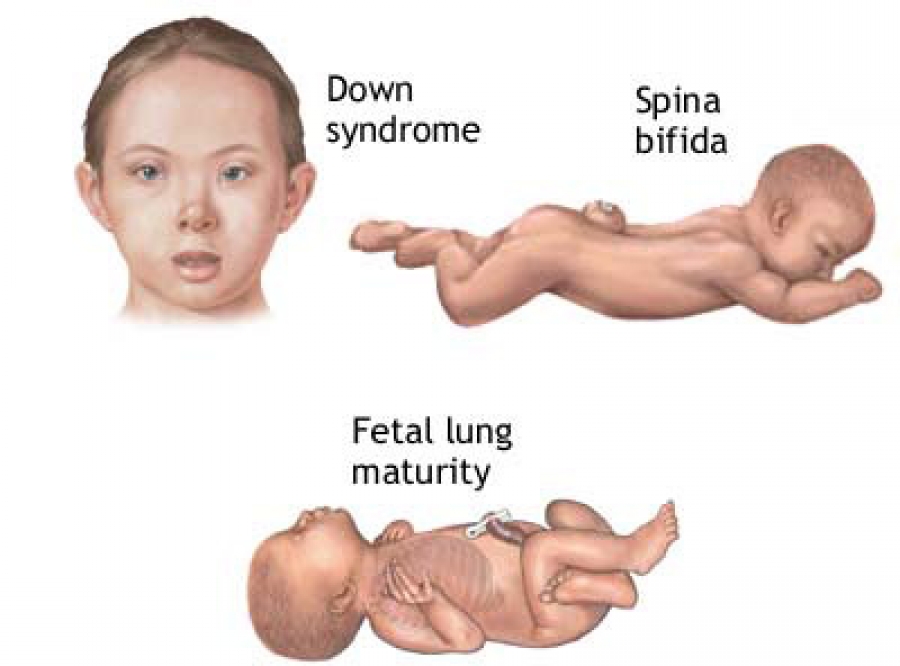
Subscribe
Association of COVID-19 Vaccination During Early Pregnancy With Risk of Congenital Fetal Anomalies | Congenital Defects | JAMA Pediatrics
Research Letter
April 4, 2022
Rachel S. Ruderman, MD, MPH1; Jessica Mormol, BS2; Emma Trawick, MD1; et al Madeline F. Perry, MD1; Emma C. Allen, BS3; Danielle Millan, BS2; Emily S. Miller, MD, MPH4
Author AffiliationsArticle Information
-
1Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, Chicago, Illinois
-
2Northwestern University Feinberg School of Medicine, Chicago, Illinois
-
3Penn State College of Medicine, Hershey
-
4Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, Chicago, Illinois
JAMA Pediatr. 2022;176(7):717-719. doi:10.1001/jamapediatrics.2022.0164
2022;176(7):717-719. doi:10.1001/jamapediatrics.2022.0164
Pregnant individuals with SARS-CoV-2 infection experience increased maternal and neonatal morbidity.1-3 Although effective COVID-19 vaccines became available in December 2020, pregnant people were excluded from initial trials. Whereas data suggest that COVID-19 vaccines are safe and effective during pregnancy, there is concern about whether the vaccines are associated with risks to the fetus.4 We evaluated the association between COVID-19 vaccination during early pregnancy and risk of major fetal structural anomalies identified on ultrasonography.
Methods
This cohort study included pregnant people receiving care at a quaternary medical center in Chicago, Illinois, who completed a fetal anatomic survey between March and November 2021 and had COVID-19 vaccination records. This study followed the STROBE reporting guideline. The Northwestern University institutional review board provided approval, with a waiver of informed consent because data were collected retrospectively and each participant could not be contacted. Most pregnant people who delivered neonates at the center received outpatient care in community practices. Patient characteristics were abstracted from electronic medical records (EMRs). Race and ethnicity were self-reported and were included to assess whether vaccination uptake varied among racial and ethnic groups. First vaccination date was obtained from EMRs and the Illinois Comprehensive Automated Immunization Registry Exchange and included both messenger RNA and adenovirus vector vaccines. Thirty days before conception until 14 weeks’ gestation was considered the teratogenic window. Participants were considered unvaccinated if there was EMR documentation of declination of vaccination. Fetal congenital anomalies were defined as structural anomalies identifiable in the second trimester (eg, 18-24 weeks’ gestation) that may affect a neonate’s life expectancy, health, or functioning and were categorized according to the Brighton Collaboration Congenital Anomalies Working Group recommendations.
Most pregnant people who delivered neonates at the center received outpatient care in community practices. Patient characteristics were abstracted from electronic medical records (EMRs). Race and ethnicity were self-reported and were included to assess whether vaccination uptake varied among racial and ethnic groups. First vaccination date was obtained from EMRs and the Illinois Comprehensive Automated Immunization Registry Exchange and included both messenger RNA and adenovirus vector vaccines. Thirty days before conception until 14 weeks’ gestation was considered the teratogenic window. Participants were considered unvaccinated if there was EMR documentation of declination of vaccination. Fetal congenital anomalies were defined as structural anomalies identifiable in the second trimester (eg, 18-24 weeks’ gestation) that may affect a neonate’s life expectancy, health, or functioning and were categorized according to the Brighton Collaboration Congenital Anomalies Working Group recommendations.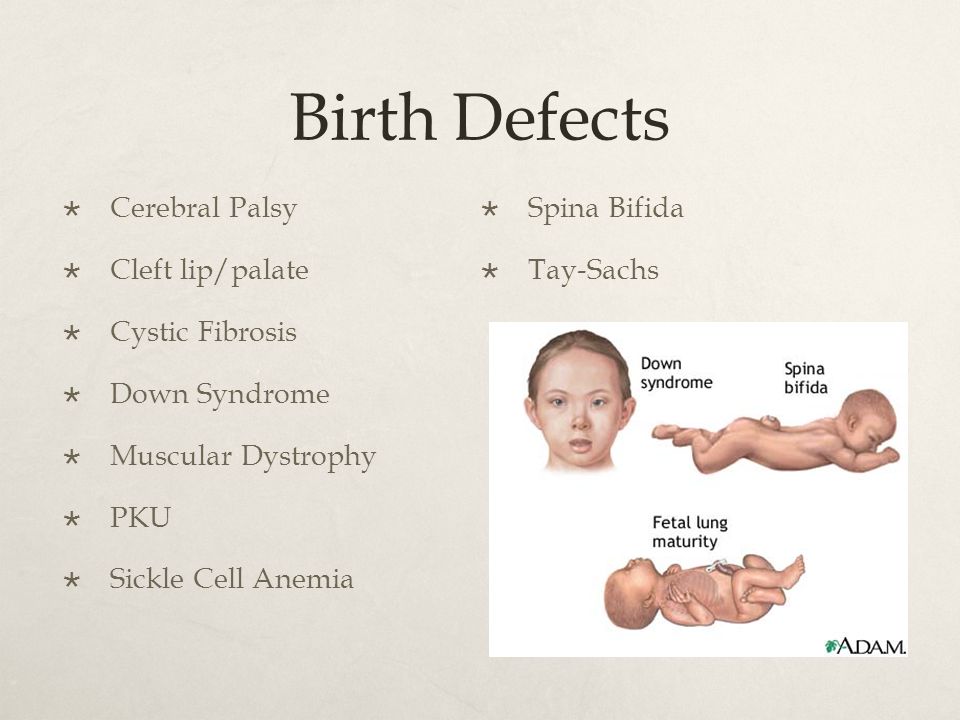 5 Functional defects (eg, galactosemia) cannot be assessed using ultrasonography and thus were excluded. Sonographic interpretation was performed by perinatologists or obstetrics and gynecology specialists with additional training in obstetric ultrasonography. Vaccination status was not routinely available to clinicians at the time of ultrasonography.
5 Functional defects (eg, galactosemia) cannot be assessed using ultrasonography and thus were excluded. Sonographic interpretation was performed by perinatologists or obstetrics and gynecology specialists with additional training in obstetric ultrasonography. Vaccination status was not routinely available to clinicians at the time of ultrasonography.
Primary analyses compared unvaccinated individuals and those vaccinated outside the teratogenic window (ie, individuals without a potential teratogenic exposure) with those vaccinated within the teratogenic window. Analyses were conducted using Stata, version 15.0. Sensitivity analyses used a narrower teratogenic window to categorize exposure (2-10 weeks’ gestation). Two-sided P < .05 was considered significant.
Results
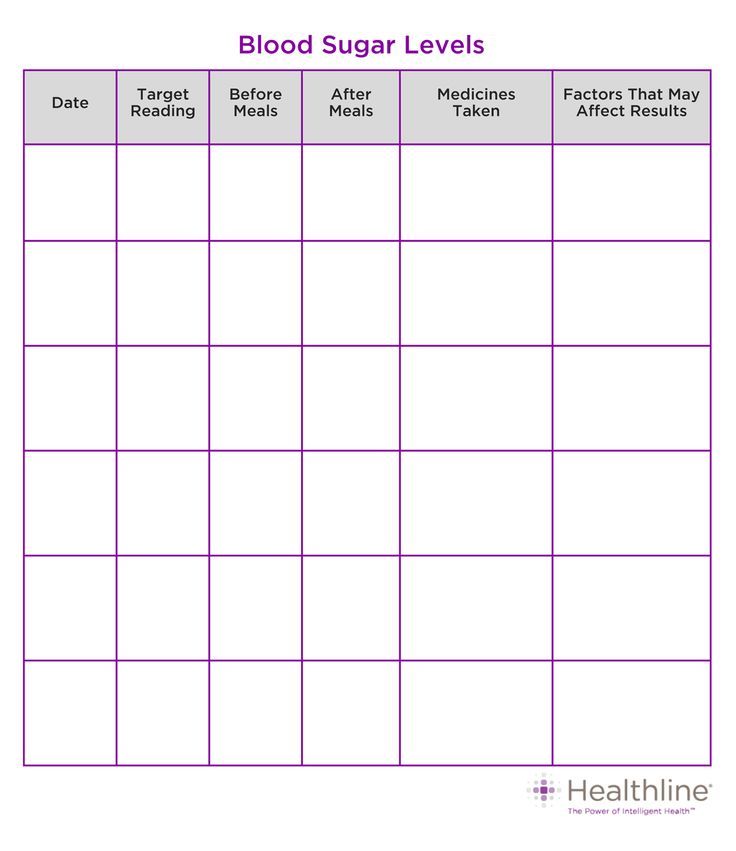
Of 3156 patients (100% female; mean [SD] age, 33.4 [4.6] years) who met the inclusion criteria, 2622 (83.1%) received at least 1 vaccine dose and 1149 (43.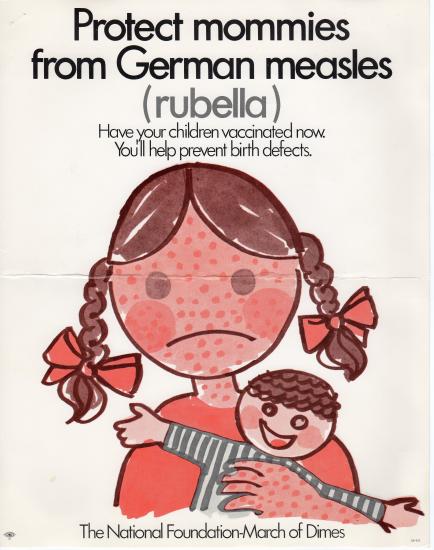 8%) were vaccinated within the teratogenic window (Table 1). An anomaly was identified in 27 of 534 unvaccinated people (5.1%) and 109 of 2622 people who received at least 1 dose of vaccine (4.2%) (P = .35). Similar findings were seen when the teratogenic window was narrowed (Table 2). After controlling for potential confounders (age at delivery, nulliparity, chronic hypertension, and hemoglobin A1c level during the first trimester), vaccination within the teratogenic window was not associated with presence of a congenital anomaly identified on ultrasonography (adjusted odds ratio, 1.05; 95% CI, 0.72-1.54).
8%) were vaccinated within the teratogenic window (Table 1). An anomaly was identified in 27 of 534 unvaccinated people (5.1%) and 109 of 2622 people who received at least 1 dose of vaccine (4.2%) (P = .35). Similar findings were seen when the teratogenic window was narrowed (Table 2). After controlling for potential confounders (age at delivery, nulliparity, chronic hypertension, and hemoglobin A1c level during the first trimester), vaccination within the teratogenic window was not associated with presence of a congenital anomaly identified on ultrasonography (adjusted odds ratio, 1.05; 95% CI, 0.72-1.54).
Discussion
In 3% to 5% of births in the US, neonates are born with structural defects, which are associated with increased infant morbidity, mortality, and billions of dollars in cost.5,6 Our findings suggest that COVID-19 vaccination during early pregnancy is not associated with an increased risk of fetal structural anomalies identified with ultrasonography.
The findings are limited by the retrospective, single-center origin of the data and by limitations of EMRs. Not all confounding variables could be reasonably ascertained (eg, folic acid intake). Furthermore, ultrasonography markers are surrogate outcomes, and many pregnancies in the data set are ongoing; thus, neonatal outcomes were not uniformly available. Given the urgent need for safety data on COVID-19 vaccines, these preliminary findings may be useful when considering vaccination during early pregnancy. The adjustment for preexisting risk factors (eg, hyperglycemia) allowed for a better understanding of associations between vaccination and anomalies. Clinicians may use this evidence in counseling their patients on the safety of vaccination.
Back to top
Article Information
Accepted for Publication: January 10, 2022.
Published Online: April 4, 2022. doi:10.1001/jamapediatrics.2022.0164
doi:10.1001/jamapediatrics.2022.0164
Corresponding Author: Rachel S. Ruderman, MD, MPH, Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, 250 E Superior St, 5th Floor, Chicago, IL 60611 ([email protected]).
Author Contributions: Drs Ruderman and Miller had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Ruderman, Perry, Miller.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Ruderman, Trawick, Perry, Millan, Miller.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Trawick, Perry, Millan, Miller.
Administrative, technical, or material support: Ruderman, Trawick, Perry, Allen, Miller.
Supervision: Ruderman, Miller.
Conflict of Interest Disclosures: Dr Miller reported serving as the site principal investigator for a Pfizer phase 2/3 randomized clinical trial of the COVID-19 vaccine during pregnancy outside the submitted work. No other disclosures were reported.
References
1.
Metz TD, Clifton RG, Hughes BL, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network. Disease severity and perinatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19). Obstet Gynecol. 2021;137(4):571-580. doi:10.1097/AOG.0000000000004339 PubMedGoogle ScholarCrossref
2.
Woodworth
KR, Olsen
EO, Neelam
V,
et al; CDC COVID-19 Response Pregnancy and Infant Linked Outcomes Team; COVID-19 Pregnancy and Infant Linked Outcomes Team (PILOT). Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy—SET-NET, 16 jurisdictions, March 29-October 14, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1635-1640. doi:10.15585/mmwr.mm6944e2 PubMedGoogle ScholarCrossref
Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy—SET-NET, 16 jurisdictions, March 29-October 14, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1635-1640. doi:10.15585/mmwr.mm6944e2 PubMedGoogle ScholarCrossref
3.
Sentilhes L, De Marcillac F, Jouffrieau C, et al Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol. 2020;223(6):914.e1-914.e15. doi:10.1016/j.ajog.2020.06.022Google Scholar
4.
Goncu Ayhan S, Oluklu D, Atalay A, et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynaecol Obstet. 2021;154(2):291-296. doi:10.1002/ijgo.13713 PubMedGoogle ScholarCrossref
5.
DeSilva M, Munoz FM, Mcmillan M, et al; Brighton Collaboration Congenital Anomalies Working Group. Congenital anomalies: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2016;34(49):6015-6026. doi:10.1016/j.vaccine.2016.03.047 PubMedGoogle ScholarCrossref
6.
Centers for Disease Control and Prevention (CDC). Update on overall prevalence of major birth defects—Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5. https://www.ncbi.nlm.nih.gov/pubmed/18185492.PubMedGoogle Scholar
Malformations
Malformations- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- D
- E
- 9000
- f
- x
- C
- h
- Sh
9000 WHO in countries »- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.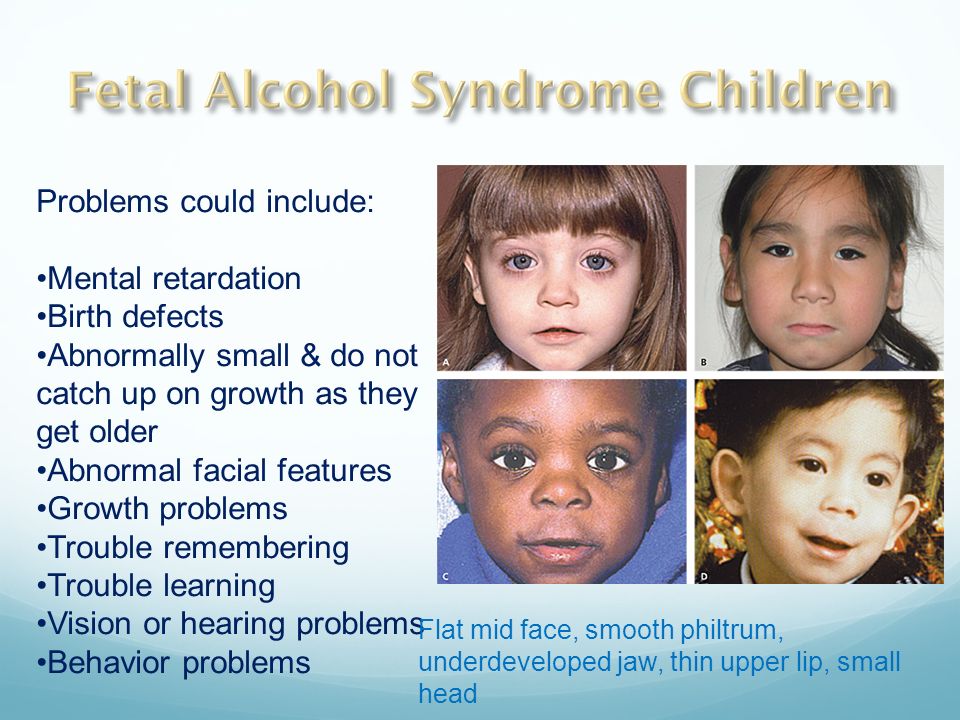 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
\n
Genetic factors
\n
\nIncest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
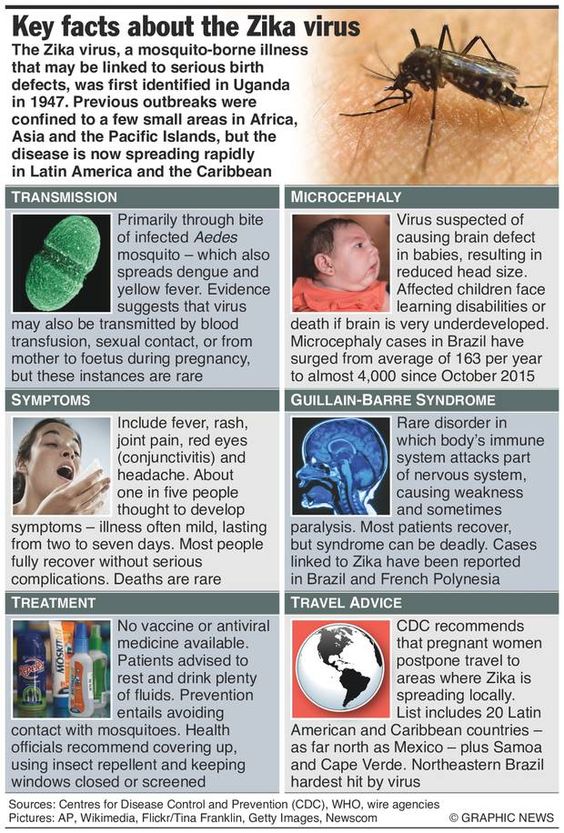
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiency in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
\n
Prevention
\n
\nPregnancy and conception preventive health care, as well as prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 \n
\n - Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol. \n
- Prevention of diabetes during pre-pregnancy and pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposures (such as x-rays) is justified and based on a careful analysis of the health risks and benefits. \n
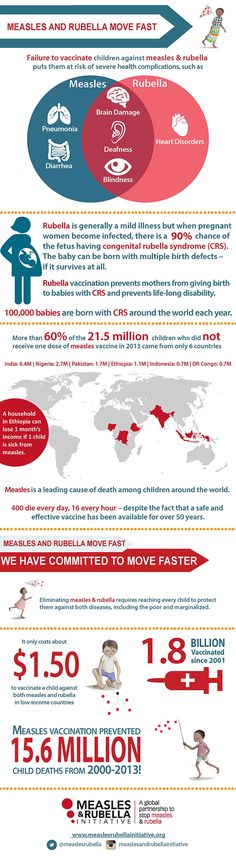
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. \n
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and intensifying training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (peri-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 \n
\n - Preconception screening: Maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. \n
- Newborn screening includes a clinical examination, as well as screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and ensure that children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
\n
\nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy to fortify foods with salt folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.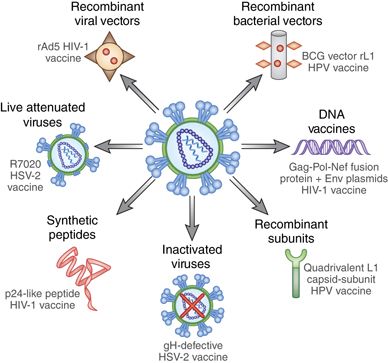 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.
\n
\nWHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"};
Key Facts
- An estimated 303,000 children die each year from malformations in the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, with significant impacts on individuals, their families, health systems and society.
- The most severe malformations include heart defects, neural tube defects and Down's syndrome.

- Although malformations may be genetic, infectious or environmental in origin, the exact cause is often difficult to establish.
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.

Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .
- Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous environmental substances (eg, heavy metals, pesticides, certain drugs).
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (eg x-rays) is justified and based on a careful analysis of the health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood.
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and intensifying training for health professionals and other staff involved in strengthening the prevention of malformations.
Identification
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: Maternal characteristics may increase risk and screening results should be used to provide appropriate care based on risk.
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. - Newborn screening includes a clinical examination, as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.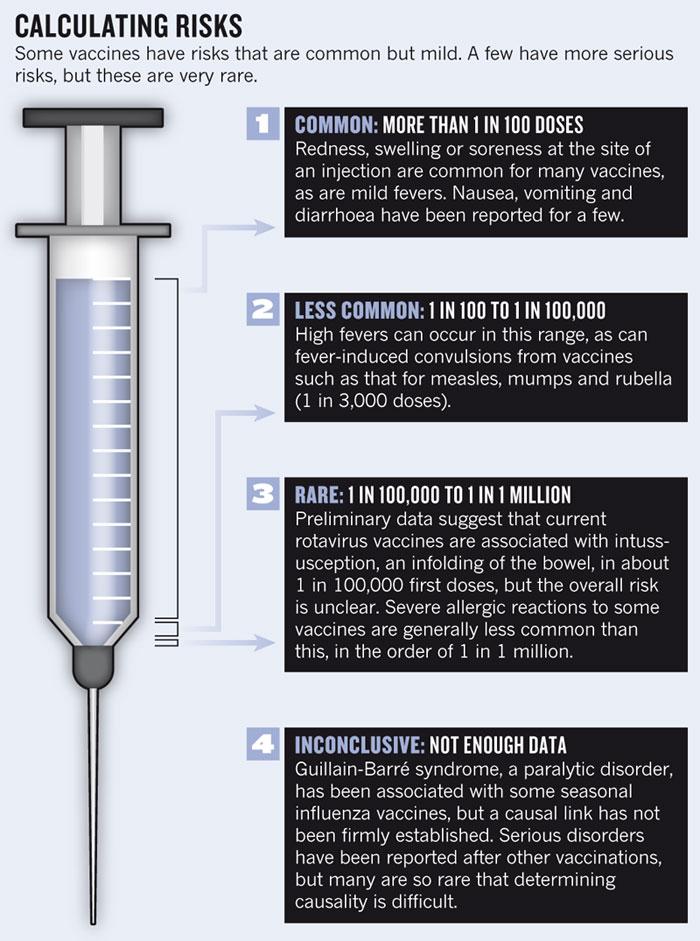
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).
Photos of children with anomalies born by vaccinated women in Turkey
Fake checking in partnership with Facebook
Information spread on the net that: children with anomalies: some of them have several arms or legs, others are blind, have tails and skin like animals, or one eye;
Screenshot of the publication
We explain what is wrong. Previously, such fakes were refuted by independent fact-checkers from Lead Stories, Teyit and fact-checkers from Uz.Daily.uz.
The photo of children with birth defects was taken before the start of the COVID-19 pandemic.
At a press conference, the head of the Turkish Welfare Party, Fatih Erbakan, showed photos of children with various congenital anomalies and claimed that this was a consequence of the influence of the mRNA vaccine. According to him, mRNA vaccines change the human genome.
According to him, mRNA vaccines change the human genome.
One of these photos shows a baby with a tail. However, the Alamy stock photo platform for August 3, 2009 states that this image has been edited.
Edited image: baby with tail
Another photo shows a baby with a thick coat of hair. This child was born in 2013 in India and has the genetic condition "werewolf syndrome" (or hypertrichosis). In 2019, 17 cases of hypertrichosis in babies were found in Spain. The reason for this is the use of drugs containing an ingredient used in hair loss products.
Hypertrichosis - excessive hair growth on any part of the body in men or women.
Photo of a child with hypertrichosis
The third photo shows Siamese twins born in 2016 in India. The newborn boy and girl shared several organs and only one pair of legs, making it impossible to separate them.
Photos of Siamese twins
October 15, 2021 Lorrie Harris-Sagaribay of MotherToBaby and specialist in information on factors that can deform embryos, in a conversation with Lead Stories emphasized that mRNA vaccines cannot be freely distributed in the body.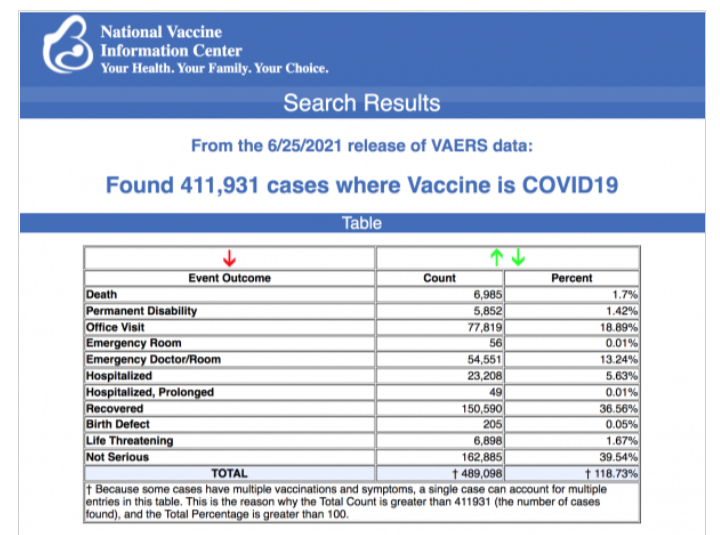 If the child's mother is vaccinated, the vaccine does not enter the child's body. However, antibodies produced in the mother's body in response to the vaccine may cross the placenta and benefit the baby.
If the child's mother is vaccinated, the vaccine does not enter the child's body. However, antibodies produced in the mother's body in response to the vaccine may cross the placenta and benefit the baby.
MotherToBaby is a non-profit organization that promotes evidence-based information about the safety and risks of various medications and their effects during pregnancy and breastfeeding.
According to Lorrie Harris-Sagaribay, COVID-19 vaccines only protect against infection with the SARS-CoV-2 virus and have no effect on the development or prevention of birth defects. Both vaccinated and unvaccinated people have a small chance of a child developing birth defects of one form or another. From 3 to 5% of children are born with birth defects.
A US Centers for Disease Control and Prevention (CDC) fact sheet states that COVID-19 vaccination is recommended for people 12 years of age and older, specifically those who are planning or are pregnant.
The American College of Obstetricians and Gynecologists Advisory Board has advised that COVID-19 vaccines do not enter fetuses and do not alter human DNA. So far, no concerns have been identified with the safety of COVID-19 vaccines for pregnant women.
So far, no concerns have been identified with the safety of COVID-19 vaccines for pregnant women.
Claiming to be from COVID-19 vaccinesmillions of people died, the authors of the video refer to a report called The vaccine death report. Report authors include David Sorensen and Vladimir Zelenko. David Sorensen is an entrepreneur and writer who spreads conspiracy theories that a group of multi-billionaires rule the world and argues that COVID-19 vaccines are Bill Gates' tool to reduce the population. Vladimir Zelenko is an American family doctor, the author of "experimental treatment". We have previously written about it here.
Sorensen and Zelenko cite the VAERS system as evidence that millions of people have died due to the COVID-19 vaccination. In fact, the information in the VAERS system is for reporting purposes only, and does not prove a causal relationship between vaccination and adverse health effects on patients after vaccination. We wrote about it here and here.