Small fetus at 20 weeks
When is a baby too small? Managing third-trimester fetal growth restriction | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
July 6, 2021
Your Pregnancy Matters
Patricia Santiago-Munoz, M. D. Obstetrics and Gynecology
The third trimester is generally considered the home stretch of pregnancy. For most patients, it’s a less stressful time regarding fetal health, since the risk of miscarriage drops significantly after the first trimester and most patients have had the opportunity to learn about the health of their baby through second trimester ultrasounds and screening tests.
However, it’s not uncommon for mild to moderate growth disruptions to occur in the third trimester. Often, these healthy babies are simply small because their parents are small in stature or they were small babies themselves. But in approximately one-third of small babies, we find a potentially serious health problem called fetal growth restriction (FGR), which is associated with low birthweight, developmental problems, and stillbirth.
FGR refers to babies who are below the 10th percentile for estimated fetal weight, which means they’re smaller than approximately 90 percent of babies at the same gestational age. There are many potential causes of FGR, which generally fall under maternal, fetal, or placental complications.
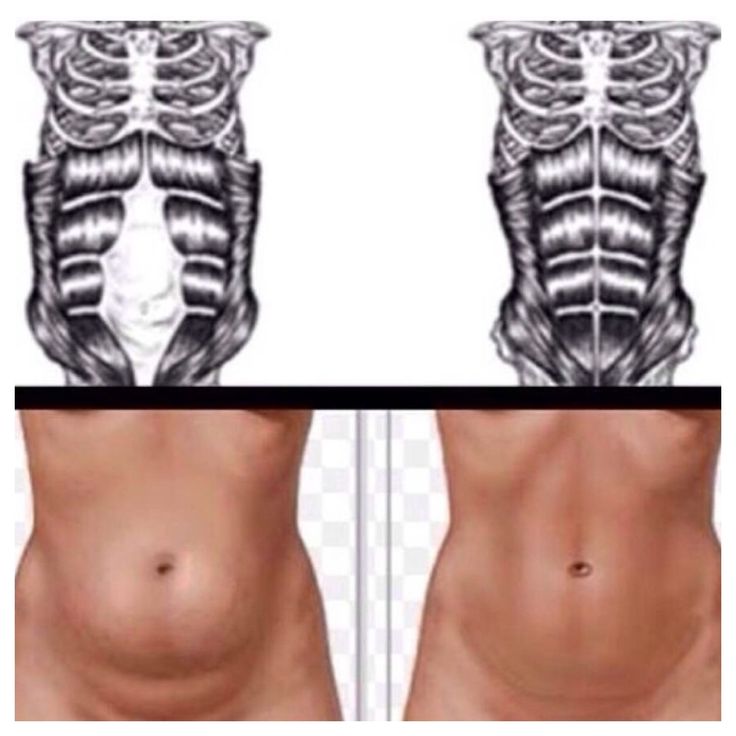
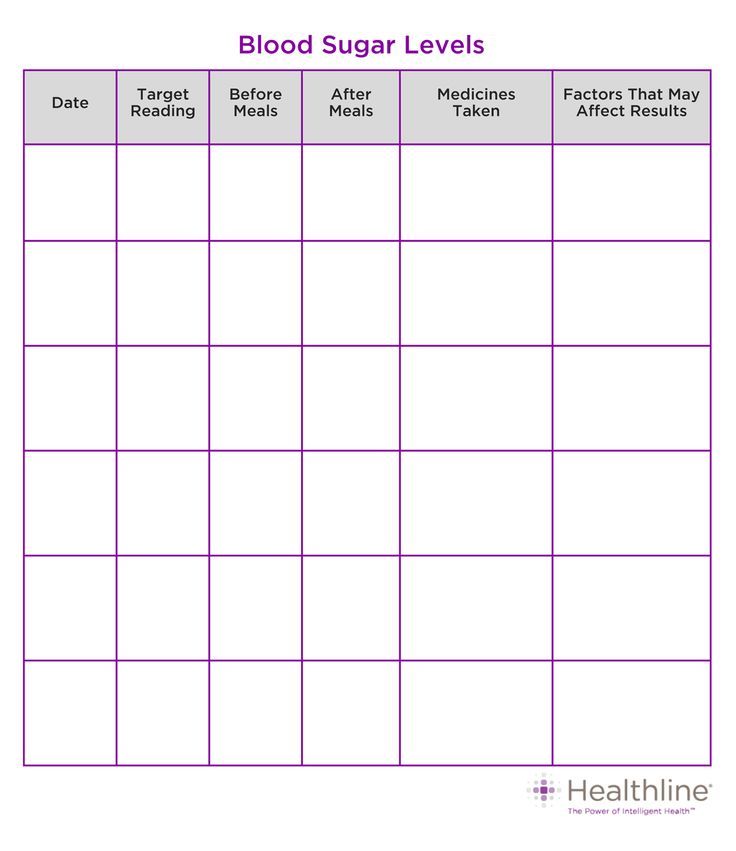
Every patient who gets prenatal care is screened for FGR at every visit by taking regular belly measurements. We’re checking your fundal height – from the top of your uterus to your pubic bone. This number helps estimate the baby’s size and whether it is growing as expected.
After 20 weeks, the fundal height should correlate approximately with how long you’ve been pregnant. For example, it should measure approximately 20cm at 20 weeks’ gestation, 30cm at 30 weeks, etc. If your baby measures smaller than expected, we’ll confirm its size with an ultrasound.
“Generally, growth restriction is associated with either maternal risk factors, fetal anomalies, or a problem with the placenta – and sometimes a combination of these situations.
Dr. Santiago-MunozSome risk factors can be controlled, and some cannot.”
Is my baby small-but-healthy? Or could it be FGR?
By definition, babies diagnosed with FGR fall below the 10th percentile for estimated fetal weight and fundal height. Even if the baby is growing steadily, they may be diagnosed with FGR if they are below that benchmark.
But following these definitions FGR is sometimes over-diagnosed. Longstanding best practices data show that babies in the 3rd percentile or lower are more likely to have an FGR-related complication, and those above the 3rd percentile are more likely to be constitutionally small (based on non-health-related family history of smaller stature).
The UT Southwestern MFM team follows standard of care protocols for babies below the 10th percentile. We investigate every scenario to avoid taxing patients with undue stress related to overdiagnosis and over-management of FGR.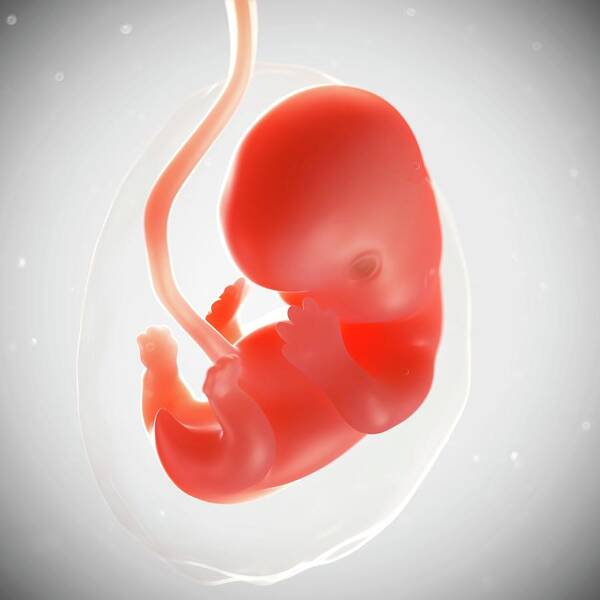 Our goal is to understand:
Our goal is to understand:
- Why your baby is small,
- Whether your pregnancy is at risk of serious complications, and
- Whether early delivery or continued monitoring is the safest choice for you and your baby.
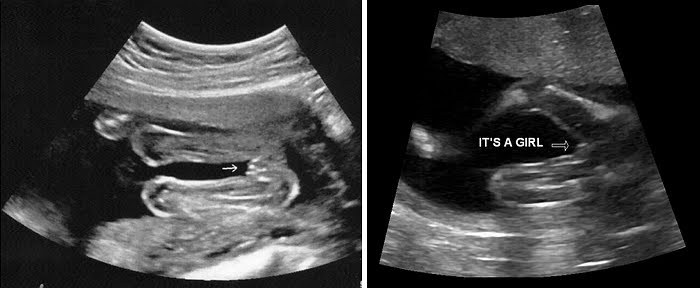
To answer these questions, we rely on two diagnostic tools: amniotic fluid measurement and Doppler ultrasound examination of the umbilical cord. These evaluations may help determine the origin of the FGR and guide further management.
What can cause FGR?
Generally, growth restriction is associated with maternal risk factors, fetal anomalies, or a problem with the placenta – and sometimes a combination of these situations. Some risk factors can be controlled, and some cannot.
Maternal risk factors
Some of the most common maternal risk factors for FGR include:
- Certain autoimmune conditions, such as lupus
- Certain viral infections, such as rubella or malaria
- Pregestational diabetes
- Having twins or more
- Hypertension (high blood pressure)
- Smoking, drinking alcohol, and substance use
While it is tough to quit smoking, it’s best to quit before becoming pregnant. However, quitting smoking during pregnancy is proven safe and beneficial for you and the baby. Your prenatal care provider can connect you with effective, judgment-free smoking cessation or substance use treatment designed specifically for pregnant patients.
However, quitting smoking during pregnancy is proven safe and beneficial for you and the baby. Your prenatal care provider can connect you with effective, judgment-free smoking cessation or substance use treatment designed specifically for pregnant patients.
Fetal anomalies
Heart conditions are among the most common fetal problems that cause FGR. Genetic abnormalities such as trisomy 21 (Down syndrome) also tend to result in babies that are smaller compared with the general population. Fetal anomalies are also more frequently associated with stillbirth.
Problems with the placenta
The placenta, like any organ, can develop improperly. Sometimes the umbilical cord is inserted in the wrong place on the placenta or only one umbilical artery forms develops in the cord instead of two, situations associated with reduced placental blood flow to an otherwise healthy baby.
In rare cases, we see a placental tumor called a chorioangioma, disrupting normal function. Placental issues are often the cause of late-onset growth complications.
Placental issues are often the cause of late-onset growth complications.
How is FGR diagnosed?
The diagnosis is based on ultrasound, and most centers use the 10th percentile cutoff to raise the alarm of possible fetal growth restriction. The next step is to have a discussion with the patient about her health history and her prior obstetrical history.
If a patient’s previous baby was less than 6 pounds at birth but was full-term and healthy, her current baby simply may be constitutionally small. If this is her first, or if previous babies were bigger, we will be more concerned about FGR. In either case, we will check the amniotic fluid and umbilical blood flow to help in the evaluation of placental function.
What happens next?
If the amniotic fluid and Doppler ultrasound are normal, we’ll watch the baby over the next few weeks and, if steady growth continues with no new concerns, that’s a good sign. The actual delivery timing will depend on how well the baby continues to grow and whether the amniotic fluid and the Doppler testing remain normal.
We generally recommend delivering the baby as close to the due date as possible to reduce the risk of needing long-term, specialized care after delivery. If the baby is:
- Between the 3rd and 10th percentiles for size, we try to get them to 38 weeks gestation.
- Smaller than the 3rd percentile, we try to get them to 37 weeks.
Often, our specialized team can safely get babies to 38 or 39 weeks before delivery, provided they have no other risk factors. Centers with less FGR management expertise tend to deliver earlier to avoid the risk of stillbirth. However, the earlier a baby arrives, the longer they typically stay in the neonatal intensive care unit (NICU).
Since the causes and severity of IUG can be so varied, your care plan will be customized based on your needs. Some patients are hospitalized for daily fetal heart rate monitoring. If you are hospitalized, we may recommend a complete course of steroids to help support fetal lung development before delivery.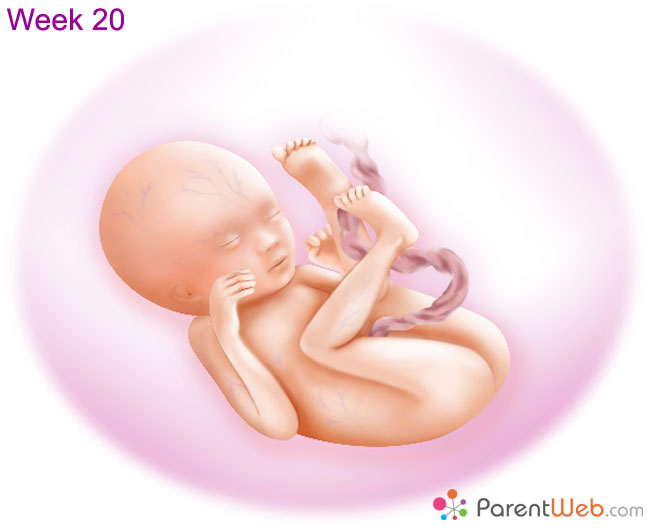
If you end up needing early delivery, it does not mean an automatic cesarean section (C-section). Many babies are otherwise healthy except for being small, so it is likely safe to try vaginal delivery. Babies that are severely growth restricted or that have abnormal Doppler patterns may not do well with labor, so C-section may be indicated. A discussion with your doctor is always recommended.
What care will the baby need after birth?
Depending on how premature the baby is and the severity of its health problems, the newborn may need to stay in the NICU. Sometimes, these babies have trouble breastfeeding at first because they burn so many calories trying to latch and nurse.
Babies who are growth restricted often need many extra calories – more than breast milk or regular formula can provide. Our NICU specialists will work with nutritionists to supplement your baby’s diet with specialized, calorie-rich formula.
Many babies who start out being bottle-fed after growth restriction can learn to latch and breastfeed once they grow stronger. Patients who want to breastfeed are welcome to begin pumping to start building their milk supply.
Patients who want to breastfeed are welcome to begin pumping to start building their milk supply.
It can be scary to learn that your baby is smaller than expected. Sometimes, babies simply grow on their own developmental curve. With specialized care during pregnancy and after delivery, most babies diagnosed with FGR in the third trimester have good outcomes.
To visit with a pregnancy care provider, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.
 D.
D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.D.
August 2, 2022
Your Pregnancy Matters
- Abey Eapen, M.
 D., Ph.D.
D., Ph.D.
July 26, 2022
More Articles
© 2022 The University of Texas Southwestern Medical Center
Member of Southwestern Health Resources
Small fetal size before 20 weeks' gestation: associations with maternal tobacco use, early preterm birth, and low birthweight
Comparative Study
. 2008 Jun;198(6):673.e1-7; discussion 673.e7-8.
doi: 10.1016/j.ajog.2008.01.036. Epub 2008 Mar 20.
Brian M Mercer 1 , Amy A Merlino, Cynthia J Milluzzi, John J Moore
Affiliations
Affiliation
- 1 Department of Obstetrics and Gynecology, Case Western Reserve University School of Medicine, MetroHealth Medical Center, Cleveland, OH, USA.
- PMID: 18355777
- DOI: 10.1016/j.ajog.2008.01.036
Comparative Study
Brian M Mercer et al. Am J Obstet Gynecol. 2008 Jun.
. 2008 Jun;198(6):673.e1-7; discussion 673.e7-8.
doi: 10.1016/j.ajog.2008.01.036. Epub 2008 Mar 20.
Authors
Brian M Mercer 1 , Amy A Merlino, Cynthia J Milluzzi, John J Moore
Affiliation
- 1 Department of Obstetrics and Gynecology, Case Western Reserve University School of Medicine, MetroHealth Medical Center, Cleveland, OH, USA.

- PMID: 18355777
- DOI: 10.1016/j.ajog.2008.01.036
Abstract
Objective: The objective of the study was to determine whether small fetal size before 20 weeks' gestation is associated with preterm birth (PTB), low birthweight (LBW), and poor fetal growth.
Study design: A total of 4405 singleton pregnancies at 10-19 weeks' gestation (GA) based on a known last menstrual period (LMP) were evaluated. Ultrasound-estimated GA (US-GA) was calculated based on crown-rump length at 10-13 weeks and by femur, head, and abdominal measurements from 14 to 19 weeks. The outcomes were compared between small (1-10 days smaller than LMP-GA) and large (0-10 days larger than LMP-GA) fetuses.
Results: At 10-19 weeks, small fetuses measured 2.7 days younger and were more likely to have mothers who smoked (P = .004). Small fetuses had no more PTB (11.4 vs 12.1%, P = .47) but did have more early PTB before 34 (5.4 vs 4.3%, P = .07) and before 32 weeks (4.1 vs 2.7%, P = .009). Small fetuses had lower birthweights (BWT), more frequent BWT below 2500 g (13.0 vs 8.6%), below 1500 g (4.0 vs 2.4%), and below 1000 g (2.9 vs 1.4%) as well as BWT below 2500 g at term (4.9 vs 2.3%) and BWT less than the 10th percentile (8.8 vs 3.7%), P < or = .003 for each. Small fetuses at 10-19 weeks also had less frequent macrosomia and were less frequently large for gestational age at birth (P < .0001 for each). These findings largely persisted in multivariable analyses.
Conclusion: Small fetal size at 10-19 weeks is associated with tobacco use in pregnancy, early PTB, LBW, and poor fetal growth.
Similar articles
-
Foetal size and body proportion at 17-19 weeks of gestation and neonatal size, proportion, and outcome.
Rasmussen S, Kiserud T, Albrechtsen S. Rasmussen S, et al. Early Hum Dev. 2006 Oct;82(10):683-90. doi: 10.1016/j.earlhumdev.2006.01.010. Epub 2006 Mar 23. Early Hum Dev. 2006. PMID: 16556490
-
Risk factors and outcomes associated with first-trimester fetal growth restriction.
Mook-Kanamori DO, Steegers EA, Eilers PH, Raat H, Hofman A, Jaddoe VW. Mook-Kanamori DO, et al. JAMA. 2010 Feb 10;303(6):527-34. doi: 10.1001/jama.2010.78. JAMA. 2010. PMID: 20145229
-
Preterm birth and fetal growth restriction in HIV-infected Brazilian pregnant women.

Dos Reis HL, Araujo Kda S, Ribeiro LP, Da Rocha DR, Rosato DP, Passos MR, Merçon De Vargas PR. Dos Reis HL, et al. Rev Inst Med Trop Sao Paulo. 2015 Mar-Apr;57(2):111-20. doi: 10.1590/S0036-46652015000200003. Rev Inst Med Trop Sao Paulo. 2015. PMID: 25923889 Free PMC article.
-
The small fetus: growth-retarded and preterm.
Tambyraja RL, Ratnam SS. Tambyraja RL, et al. Clin Obstet Gynaecol. 1982 Dec;9(3):517-37. Clin Obstet Gynaecol. 1982. PMID: 6756748 Review.
-
Small fetal thymus and adverse obstetrical outcome: a systematic review and a meta-analysis.
Caissutti C, Familiari A, Khalil A, Flacco ME, Manzoli L, Scambia G, Cagnacci A, D'antonio F. Caissutti C, et al. Acta Obstet Gynecol Scand.
 2018 Feb;97(2):111-121. doi: 10.1111/aogs.13249. Epub 2017 Dec 6. Acta Obstet Gynecol Scand. 2018. PMID: 29057456 Review.
2018 Feb;97(2):111-121. doi: 10.1111/aogs.13249. Epub 2017 Dec 6. Acta Obstet Gynecol Scand. 2018. PMID: 29057456 Review.
See all similar articles
Cited by
-
Preliminary analysis of in utero low-level arsenic exposure and fetal growth using biometric measurements extracted from fetal ultrasound reports.
Davis MA, Higgins J, Li Z, Gilbert-Diamond D, Baker ER, Das A, Karagas MR. Davis MA, et al. Environ Health. 2015 Mar 30;14:12. doi: 10.1186/1476-069X-14-12. Environ Health. 2015. PMID: 25971349 Free PMC article.
-
Fetal volume measurements with three dimensional ultrasound in the first trimester of pregnancy, related to pregnancy outcome, a prospective cohort study.
Smeets NA, Prudon M, Winkens B, Oei SG.
Smeets NA, et al. BMC Pregnancy Childbirth. 2012 May 28;12:38. doi: 10.1186/1471-2393-12-38. BMC Pregnancy Childbirth. 2012. PMID: 22640017 Free PMC article. Clinical Trial.
-
Complement activation fragment Bb in early pregnancy and spontaneous preterm birth.
Lynch AM, Gibbs RS, Murphy JR, Byers T, Neville MC, Giclas PC, Salmon JE, Van Hecke TM, Holers VM. Lynch AM, et al. Am J Obstet Gynecol. 2008 Oct;199(4):354.e1-8. doi: 10.1016/j.ajog.2008.07.044. Am J Obstet Gynecol. 2008. PMID: 18928972 Free PMC article.
Publication types
MeSH terms
Child development by week | Regional Perinatal Center
Expectant mothers are always curious about how the fetus develops at a time when it is awaited with such impatience. Let's talk and look at the photos and pictures of how the fetus grows and develops week by week.
Let's talk and look at the photos and pictures of how the fetus grows and develops week by week.
What does the puffer do for 9 whole months in mom's tummy? What does he feel, see and hear?
Let's start the story about the development of the fetus by weeks from the very beginning - from the moment of fertilization. A fetus up to 8 weeks old is called embryo , this occurs before the formation of all organ systems.
Embryo development: 1st week
The egg is fertilized and begins to actively split. The ovum travels to the uterus, getting rid of the membrane along the way.
On the 6th-8th days, implantation of eggs is carried out - implantation into the uterus. The egg settles on the surface of the uterine mucosa and, using the chorionic villi, attaches to the uterine mucosa.
Embryo development: 2-3 weeks
Picture of embryo development at 3 weeks.
The embryo is actively developing, starting to separate from the membranes. At this stage, the beginnings of the muscular, skeletal and nervous systems are formed. Therefore, this period of pregnancy is considered important.
At this stage, the beginnings of the muscular, skeletal and nervous systems are formed. Therefore, this period of pregnancy is considered important.
Embryo development: 4–7 weeks
Fetal development by week in pictures: week 4
Fetal development by week photo: week 4
Photo of an embryo before the 6th week of pregnancy.
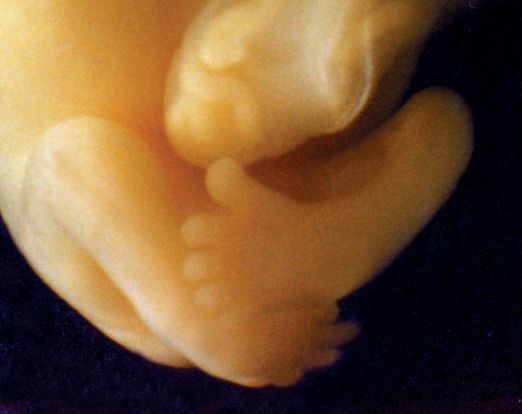
The heart, head, arms, legs and tail are formed in the embryo :) . Gill slit is defined. The length of the embryo at the fifth week reaches 6 mm.
Fetal development by week photo: week 5
At the 7th week, the rudiments of the eyes, stomach and chest are determined, and fingers appear on the handles. The baby already has a sense organ - the vestibular apparatus. The length of the embryo is up to 12 mm.
Fetal development: 8th week
Fetal development by weeks photo: weeks 7-8
The face of the fetus can be identified, the mouth, nose, and auricles can be distinguished. The head of the embryo is large and its length corresponds to the length of the body; the fetal body is formed. All significant, but not yet fully formed, elements of the baby's body already exist. The nervous system, muscles, skeleton continue to improve.
The head of the embryo is large and its length corresponds to the length of the body; the fetal body is formed. All significant, but not yet fully formed, elements of the baby's body already exist. The nervous system, muscles, skeleton continue to improve.
Fetal development in the photo already sensitive arms and legs: week 8
The fetus developed skin sensitivity in the mouth (preparation for the sucking reflex), and later in the face and palms.
At this stage of pregnancy, the genitals are already visible. Gill slits die. The fruit reaches 20 mm in length.
Fetal development: 9–10 weeks
Fetal development by week photo: week 9
Fingers and toes already with nails. The fetus begins to move in the pregnant woman's stomach, but the mother does not feel it yet. With a special stethoscope, you can hear the baby's heartbeat. Muscles continue to develop.
Weekly development of the fetus photo: week 10
The entire surface of the fetal body is sensitive and the baby develops tactile sensations with pleasure, touching his own body, the walls of the fetal bladder and the umbilical cord. It is very curious to observe this on ultrasound. By the way, the baby first moves away from the ultrasound sensor (of course, because it is cold and unusual!), And then puts his hands and heels trying to touch the sensor.
It's amazing when a mother puts her hand to her stomach, the baby tries to master the world and tries to touch with his pen "from the back".
The development of the fetus: 11–14 weeks
Development of the fetus in the photo of the legs: weeks 11
The baby, legs and eyelids are formed, and the genitals become distinguishable (you can find out the gender (you can find out the gender child). The fetus begins to swallow, and if something is not to its taste, for example, if something bitter got into the amniotic fluid (mother ate something), then the baby will begin to frown and stick out his tongue, making less swallowing movements.
The fetus begins to swallow, and if something is not to its taste, for example, if something bitter got into the amniotic fluid (mother ate something), then the baby will begin to frown and stick out his tongue, making less swallowing movements.
Fruit skin appears translucent.
Fruit development: Week 12
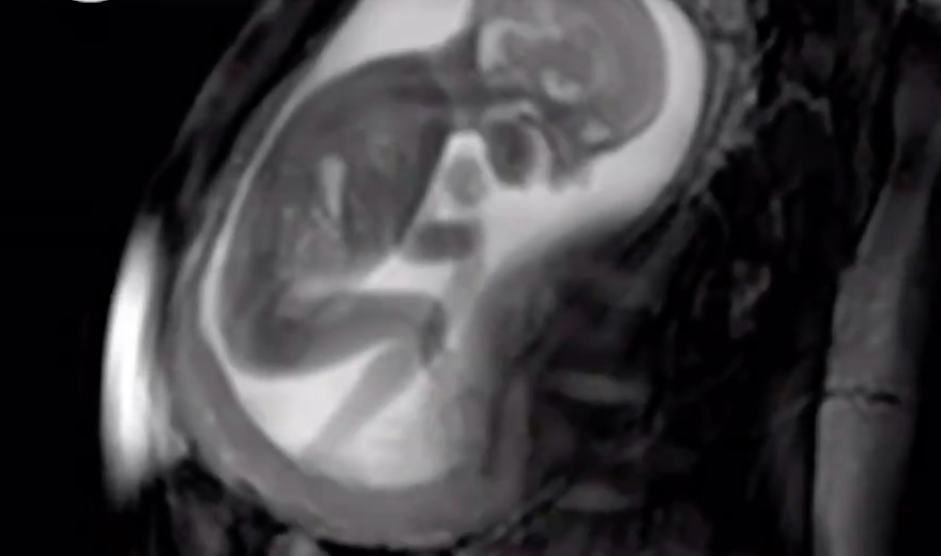
Photo of the fetus 12 weeks per 3D Uzi
buds are responsible for production for production urine. Blood forms inside the bones. And hairs begin to grow on the head. Moves more coordinated. The skin turns pink, the ears and other parts of the body, including the face, are already visible. Imagine, a child can already open his mouth and blink, as well as make grasping movements. Baby sucks his thumb, becomes more energetic. Pseudo-feces are formed in the intestines of the fetus - meconium , kidneys begin to work. During this period, the brain develops very actively. The auditory ossicles become stiff and now they are able to conduct sounds, the baby hears his mother - heartbeat, breathing, voice. The fetus intensively gains weight, fat deposits are formed. The weight of the fetus reaches 650 g, and the length is 300 mm. The lungs at this stage of fetal development are so developed that the baby can survive in the artificial conditions of the intensive care unit. Lungs continue to develop. Lips and mouth become more sensitive. The eyes develop, open slightly and can perceive light and squint from direct sunlight. In girls, the labia majora do not yet cover the small ones, and in boys, the testicles have not yet descended into the scrotum. Fetal weight reaches 900–1200 g, and the length is 350 mm. 9 out of 10 children born at this term survive. The lungs are now adapted to breathe normal air. Breathing is rhythmic and body temperature is controlled by the CNS. The baby can cry and responds to external sounds. Child opens eyes while awake and closes during sleep. The skin becomes thicker, smoother and pinkish. Starting from this period, the fetus will actively gain weight and grow rapidly. The fetus reacts to a light source. Muscle tone increases and the baby can turn and raise his head. On which, the hairs become silky. The child develops a grasping reflex. The lungs are fully developed. The fetus is quite developed, prepared for birth and considered mature. The baby has mastered over 70 different reflex movements. Due to the subcutaneous fatty tissue, the baby's skin is pale pink. The head is covered with hairs up to 3 cm. The baby perfectly mastered the movements of his mother , knows when she is calm, excited, upset and reacts to this with her movements. During the intrauterine period, the fetus gets used to moving in space, which is why babies love it so much when they are carried in their arms or rolled in a stroller. The nails protrude beyond the tips of the fingers, the cartilages of the ears and nose are elastic. In boys, the testicles have descended into the scrotum, and in girls, the large labia cover the small ones. The weight of the fetus reaches 3200-3600 g, and the length is 480-520 mm. After the birth, the baby longs for touching his body, because at first he cannot feel himself - the arms and legs do not obey the child as confidently as it was in the amniotic fluid. Therefore, so that your baby does not feel lonely, it is advisable to carry him in your arms, press him to you while stroking his body. And one more thing, the baby remembers the rhythm and sound of your heart very well . Therefore, you can comfort the baby in this way - take him in your arms, put him on the left side and your miracle will calm down, stop crying and fall asleep. Gynecology It happens that expectant mothers hear a frighteningly incomprehensible abbreviation - ZRP at the appointment with the attending physician or in the ultrasound room. Its decoding is even more frightening: "delayed fetal development." A pregnant woman faced with a similar diagnosis is tormented by many questions. How dangerous is this condition? How will it affect the health of the baby? Will he be able to catch up? Adult people are not alike, and among the many external differences, they differ in height and weight. Even the same person at different periods of his life can lose weight or gain weight, and this does not cause alarm in anyone. Very young children are another matter: clear criteria are calculated for them, a deviation from which indicates that something is wrong with the baby. And the smaller the child, the more important is the correspondence of his physical development to certain norms. The weight of a child at birth is very important for his development, especially in the first year of life, and affects his health in the future. Children born with low body weight (up to 2500 grams) are more prone to obstetric complications: they tolerate childbirth worse, they develop hypoxia and even asphyxia more often than children with normal weight, and neurological disorders also occur. As a result, these babies do not adapt well to a new life. In infancy, they suffer from hyperexcitability, increased or, conversely, decreased muscle tone, sluggishly suck and often spit up food, gain weight poorly, and may lag behind their peers in psychomotor development. Even at the age of 7-8 years, such children are hyperactive, clumsy and do not know how to concentrate on the necessary subject for a long time. The difference between healthy babies and small babies only blurs by 9-10 years, although in height and weight they catch up with their peers by the age of two. FGR can be symmetrical, when all organs are evenly reduced, and asymmetric, when the brain and skeleton correspond to the gestational age, and the internal organs lag behind in development. The reasons for this are smoking, alcohol consumption, chromosomal abnormalities, infections, but most often - fetoplacental insufficiency and other conditions that lead to circulatory disorders: high or low blood pressure, toxicosis of the second half of pregnancy, diabetes mellitus with vascular damage, kidney disease, etc. Maternal age affects the development of fetal malnutrition . The fact is that the body of very young mothers (16-18 years old) is simply not yet ready for the upcoming stresses, while older mothers (32-40 years old) most often already have a “baggage” of chronic diseases. Smoking, addiction to alcohol and any drugs clearly contribute to the development of malnutrition, as they cause pronounced vasoconstriction and reduce uteroplacental blood flow. Alas, quite often hypotrophy is observed during multiple pregnancies, since two or even three twins have to share, literally brotherly, the nutrients received from the mother. One of the simplest methods of monitoring fetal development is to measure the size of the uterus. As soon as it can be easily felt above the womb - approximately at the fourth month of pregnancy, at each visit, the doctor will measure the height of the fundus of the uterus, and in the second half of pregnancy, the circumference of the abdomen at the level of the navel. The most accurate diagnostic method is the ultrasound biometry used in our Clinic , which measures and evaluates several fetal parameters. The most traditional is the measurement of the head, tummy and femur, but if the doctor has doubts, he will also take additional measurements. The accuracy of the diagnosis is ensured by the high qualification of the doctor conducting the study, the excellent resolution of our Sonix OP ultrasound scanner and the possibility of conducting a Doppler study. Ultrasound also controls the amount of amniotic fluid, reveals signs of placental dysfunction, as well as changes in blood flow in it, which helps the doctor to accurately make a preliminary diagnosis and begin treatment. The first signs of IGR can be detected in such a study as early as 24-26 weeks, and its symmetrical form is more often noted. The occurrence of malnutrition after 32 weeks is more typical for the asymmetric form, and fetal hypoxia usually also joins it. Identified fetal growth retardation should be treated. Depending on the severity of the condition of the fetus, the treatment is carried out on an outpatient basis, for example, in our day hospital, or in the maternity hospital. The method and timing of delivery largely depend on the condition of the fetus. If the treatment of FGR is successful and the baby is growing, then it makes no sense to rush things, because by the end of pregnancy it can reach quite a decent size. If, despite all efforts, the child does not gain weight or has any other problems, then they resort to early delivery.
Development of the fetus for weeks: Week 14 9000 9000 Fetal development: 15-18 weeks
Fetal development by weeks photo: week 15  The fetus begins to actively push in the mother's tummy. The sex of the fetus can be determined by ultrasound.
The fetus begins to actively push in the mother's tummy. The sex of the fetus can be determined by ultrasound. Fetal development: 19-23 weeks
Fetal development by week photo: week 19
Fetal development by weeks photo: week 20 Fetal development: 24-27 weeks
 Now the baby is already falling asleep and waking up. Downy hairs appear on the skin, the skin becomes wrinkled and covered with grease. The cartilage of the ears and nose is still soft.
Now the baby is already falling asleep and waking up. Downy hairs appear on the skin, the skin becomes wrinkled and covered with grease. The cartilage of the ears and nose is still soft.
Fetal development by week photo: week 27 Fetal development: 28-32 weeks
 Almost all babies born prematurely at this time are viable. The weight of the fetus reaches 2500 g, and the length is 450 mm.
Almost all babies born prematurely at this time are viable. The weight of the fetus reaches 2500 g, and the length is 450 mm. Fetal development: 33-37 weeks
Fetal development by week photo: week 36 Fetal development: 38-42 weeks
Fetal development by weeks photo: week 40  For a baby, this is a completely natural state, so he will calm down and fall asleep when he is shaken.
For a baby, this is a completely natural state, so he will calm down and fall asleep when he is shaken.  And for you, finally, the time of bliss will come :) .
And for you, finally, the time of bliss will come :) . Fetal growth restriction (FGR)
 And to assess the state of intrauterine development of the fetus, its size is the most objective criterion.
And to assess the state of intrauterine development of the fetus, its size is the most objective criterion.  However, the consequences of the transferred condition can “come around” already in adulthood. Recent studies have shown an association between low birth weight and an increased risk of developing cardiovascular disease, obesity, diabetes mellitus and elevated blood lipids, all of which are associated with congenital endocrine disorders seen in low birth weight infants. Therefore, such a pathology as - Fetal growth restriction - (FGR or fetal malnutrition) deserves special attention.
However, the consequences of the transferred condition can “come around” already in adulthood. Recent studies have shown an association between low birth weight and an increased risk of developing cardiovascular disease, obesity, diabetes mellitus and elevated blood lipids, all of which are associated with congenital endocrine disorders seen in low birth weight infants. Therefore, such a pathology as - Fetal growth restriction - (FGR or fetal malnutrition) deserves special attention. 
 This will allow the doctor to roughly judge the size of the fetus. Obviously, these indicators are not objective enough, because their value is influenced by the thickness of the anterior abdominal wall, the amount of amniotic fluid, and the physique of the woman.
This will allow the doctor to roughly judge the size of the fetus. Obviously, these indicators are not objective enough, because their value is influenced by the thickness of the anterior abdominal wall, the amount of amniotic fluid, and the physique of the woman.  To clarify the diagnosis, we carry out Doppler study of the vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), , which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heartbeats in response to movements or uterine contractions. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus. In this case, we simply observe the woman without any therapy.
To clarify the diagnosis, we carry out Doppler study of the vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), , which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heartbeats in response to movements or uterine contractions. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus. In this case, we simply observe the woman without any therapy.  The goal of treatment in this case is not to “fatten the baby”, but to normalize metabolic processes and support the vital functions of the fetus. Of course, the success of treatment largely depends on how timely it is started. A large arsenal of medicines is used to treat malnutrition. It should be individual, taking into account the cause that caused IGR in this particular case and aimed at treating both the woman's diseases and pregnancy complications. For expectant mothers who are carrying a small child, it is very important to have a good diet rich in vitamins and animal proteins, as well as a regimen with limited physical activity. Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.
The goal of treatment in this case is not to “fatten the baby”, but to normalize metabolic processes and support the vital functions of the fetus. Of course, the success of treatment largely depends on how timely it is started. A large arsenal of medicines is used to treat malnutrition. It should be individual, taking into account the cause that caused IGR in this particular case and aimed at treating both the woman's diseases and pregnancy complications. For expectant mothers who are carrying a small child, it is very important to have a good diet rich in vitamins and animal proteins, as well as a regimen with limited physical activity. Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.  Although, as you know, houses and walls help, but in severe cases it is better not to refuse hospitalization. In the hospital, it is easier to monitor the condition of the mother and baby, and therefore provide more effective assistance. The effect of therapeutic measures must be constantly monitored using ultrasound and CTG, which are usually prescribed at intervals of 2 weeks, and if necessary, more often. FGR treatment almost always produces good results. In most cases, it is possible to observe adequate fetal growth: for example, in 7-10 days, the size of the fetus increases accordingly, and does not lag even further, which is considered a completely satisfactory result.
Although, as you know, houses and walls help, but in severe cases it is better not to refuse hospitalization. In the hospital, it is easier to monitor the condition of the mother and baby, and therefore provide more effective assistance. The effect of therapeutic measures must be constantly monitored using ultrasound and CTG, which are usually prescribed at intervals of 2 weeks, and if necessary, more often. FGR treatment almost always produces good results. In most cases, it is possible to observe adequate fetal growth: for example, in 7-10 days, the size of the fetus increases accordingly, and does not lag even further, which is considered a completely satisfactory result.