Relief from pelvic pain
Chronic pelvic pain in women - Diagnosis and treatment
Diagnosis
Figuring out what's causing your chronic pelvic pain often involves a process of elimination because many different disorders can cause pelvic pain.
In addition to a detailed interview about your pain, your personal health history and your family history, your doctor may ask you to keep a journal of your pain and other symptoms.
Tests or exams your doctor might suggest include:
- Pelvic exam. This can reveal signs of infection, abnormal growths or tense pelvic floor muscles. Your doctor checks for areas of tenderness. Let your doctor know if you feel any discomfort during this exam, especially if the pain is similar to the pain you've been experiencing.
- Lab tests. During the pelvic exam, your doctor may order labs to check for infections, such as chlamydia or gonorrhea. Your doctor may also order bloodwork to check your blood cell counts and urinalysis to check for a urinary tract infection.
- Ultrasound. This test uses high-frequency sound waves to produce precise images of structures within your body. This procedure is especially useful for detecting masses or cysts in the ovaries, uterus or fallopian tubes.
- Other imaging tests. Your doctor may recommend abdominal X-rays, computerized tomography (CT) scans or magnetic resonance imaging (MRI) to help detect abnormal structures or growths.
- Laparoscopy. During this surgical procedure, your doctor makes a small incision in your abdomen and inserts a thin tube attached to a small camera (laparoscope). The laparoscope allows your doctor to view your pelvic organs and check for abnormal tissues or signs of infection. This procedure is especially useful in detecting endometriosis and chronic pelvic inflammatory disease.
Finding the underlying cause of chronic pelvic pain can be a long process, and in some cases, a clear explanation may never be found.
With patience and open communication, however, you and your doctor can develop a treatment plan that helps you live a full life with minimal discomfort.
More Information
- CT scan
- MRI
- Pelvic exam
- Ultrasound
- X-ray
Treatment
The goal of treatment is to reduce symptoms and improve quality of life.
If your doctor can pinpoint a specific cause, treatment will focus on that cause. However, if a cause can't be identified, treatment will focus on managing your pain and other symptoms. For many women, the optimal approach involves a combination of treatments.
Medications
Depending on the cause, your doctor may recommend a number of medications to treat your condition, such as:
- Pain relievers. Over-the-counter pain remedies, such as aspirin, ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others), may provide partial relief from your pelvic pain. Sometimes a prescription pain reliever may be necessary.
 Pain medication alone, however, rarely solves the problem of chronic pain.
Pain medication alone, however, rarely solves the problem of chronic pain. - Hormone treatments. Some women find that the days when they have pelvic pain may coincide with a particular phase of their menstrual cycle and the hormonal changes that control ovulation and menstruation. When this is the case, birth control pills or other hormonal medications may help relieve pelvic pain.
- Antibiotics. If an infection is the source of your pain, your doctor may prescribe antibiotics.
- Antidepressants. Some types of antidepressants can be helpful for chronic pain. Tricyclic antidepressants, such as amitriptyline, nortriptyline (Pamelor) and others, seem to have pain-relieving as well as antidepressant effects. They may help improve chronic pelvic pain even in women who don't have depression.
Other therapies
Your doctor may recommend specific therapies or procedures as a part of your treatment for chronic pelvic pain.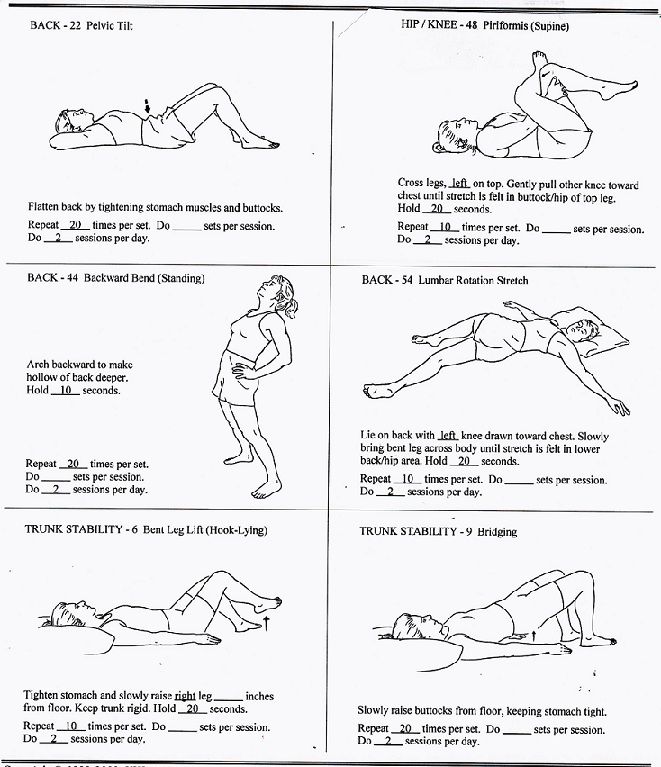 These may include:
These may include:
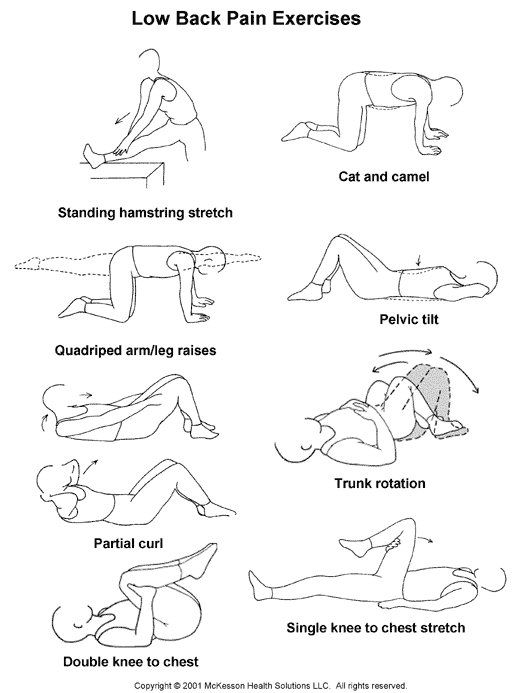
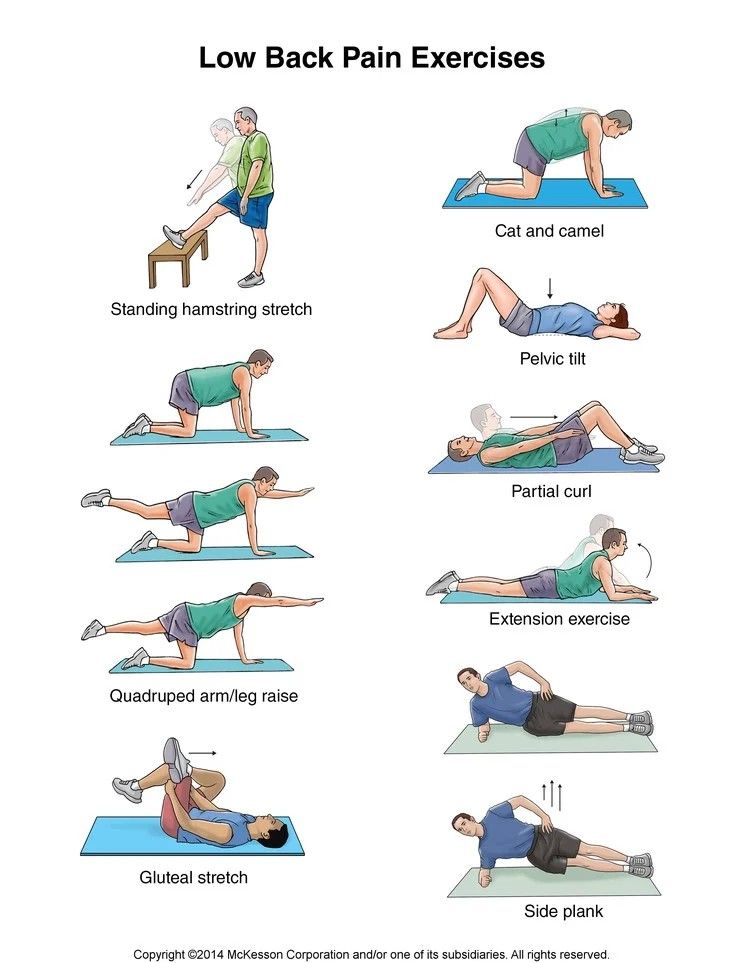
- Physical therapy. Stretching exercises, massage and other relaxation techniques may improve your chronic pelvic pain. A physical therapist can assist you with these therapies and help you develop coping strategies for the pain. Sometimes physical therapists target specific points of pain using a medical instrument called transcutaneous electrical nerve stimulation (TENS). TENS delivers electrical impulses to nearby nerve pathways. Physical therapists may also use a psychology technique called biofeedback, which helps you identify areas of tight muscles so that you can learn to relax those areas.
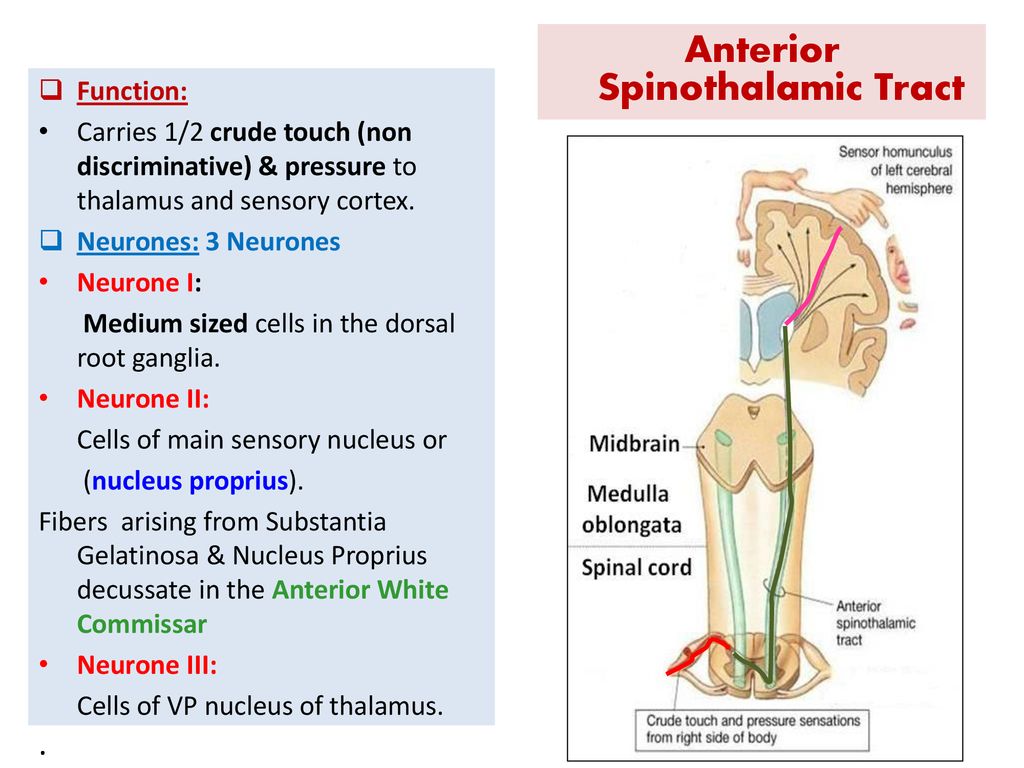
- Neurostimulation (spinal cord stimulation). This treatment involves implanting a device that blocks nerve pathways so that the pain signal can't reach the brain. It may be helpful, depending on the cause of your pelvic pain.
- Trigger point injections. If your doctor finds specific points where you feel pain, you may benefit from having a numbing medicine injected into those painful spots (trigger points).
 The medicine, usually a long-acting local anesthetic, can block pain and ease discomfort.
The medicine, usually a long-acting local anesthetic, can block pain and ease discomfort. - Psychotherapy. If your pain could be intertwined with depression, sexual abuse, a personality disorder, a troubled marriage or a family crisis, you may find it helpful to talk with a psychologist or psychiatrist. There are different types of psychotherapy, such as cognitive behavioral therapy and biofeedback. Regardless of the underlying cause of your pain, psychotherapy can help you develop strategies for coping with the pain.
Surgery
To correct an underlying problem that causes chronic pelvic pain, your doctor may recommend a surgical procedure, such as:
- Laparoscopic surgery. If you have endometriosis, doctors can remove the adhesions or endometrial tissue using laparoscopic surgery. During laparoscopic surgery, your surgeon inserts a slender viewing instrument (laparoscope) through a small incision near your navel and inserts instruments to remove endometrial tissue through one or more additional small incisions.
- Hysterectomy. In rare complicated cases, your doctors may recommend removal of your uterus (hysterectomy), fallopian tubes (salpingectomy) or ovaries (oophorectomy). There are important health consequences to having this procedure. Your doctor will discuss the benefits and risks in detail before recommending this option.
Pain rehabilitation programs
You may need to try a combination of treatment approaches before you find what works best for you. If appropriate, you might consider entering a pain rehabilitation program.
These types of programs, such as the Pain Rehabilitation Center at Mayo Clinic, typically provide a team approach to treatment, including medical and psychiatric aspects.
More Information
- Acupuncture
- Biofeedback
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Chronic pain can have a major impact on your daily life. When you're in pain, you may have trouble sleeping, exercising or performing physical tasks.
Chronic pain can also cause anxiety and stress, which in turn may worsen your pain.
Relaxation techniques can help release tension, reduce pain, calm emotions and induce sleep. Many techniques can be learned on your own, such as meditation and deep breathing.
Alternative medicine
Acupuncture
Limited evidence suggests that acupuncture may be helpful for some causes of pelvic pain.
During acupuncture treatment, a practitioner inserts tiny needles into your skin at precise points. Pain relief may come from the release of endorphins, your body's natural painkillers, but that's only one of many theories about how acupuncture works. Acupuncture is generally considered a safe treatment.
Talk with your doctor if you're considering trying a complementary or alternative therapy.
Preparing for your appointment
You're likely to start by seeing your family doctor or a doctor who specializes in conditions affecting the female reproductive tract (gynecologist).
Depending on the suspected cause of your pain, he or she may refer you to a digestive system specialist (gastroenterologist), a urinary and gynecologic specialist (urogynecologist) or a specialist in musculoskeletal pain (physiatrist or physical therapist).
What you can do
To prepare for your appointment:
- Make a list of any signs and symptoms you're experiencing. Include any that may seem unrelated to the reason for your appointment.
- Make a note of key medical information. Include any major stresses or recent life changes.
- Make a list of all medications and the doses. Include any prescription and nonprescription drugs, vitamins or other supplements you're taking.
- Consider taking a family member or friend along.
 Sometimes it can be difficult to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
Sometimes it can be difficult to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot. - Prepare questions. Your time with your doctor is limited, so preparing a list of questions can help you make the most of your time together.
Some basic questions to ask your doctor include:
- What are the possible causes of my symptoms or condition?
- What tests do you recommend?
- If these tests don't pinpoint the cause of my symptoms, what additional tests might be necessary?
- What approach will you recommend if we can't locate an underlying cause?
- What types of treatments are most likely to improve my symptoms?
- How long will I need to be treated?
- How long might it take for me to feel better?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
In addition to the questions you've prepared in advance, don't hesitate to ask questions during your appointment at any time that you don't understand something.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Being ready to answer them may leave extra time to go over any points you'd like to have clarified. Your doctor may ask:
- When did you first begin experiencing pelvic pain?
- Has your pain changed or spread over time?
- How often do you have pelvic pain?
- How severe is your pain, and how long does it last?
- Where is your pain located? Does it always occur in one place?
- How would you describe your pain?
- Does your pain come in waves or is it constant?
- Do you feel pain during urination or a bowel movement?
- Does your menstrual cycle affect your pain?
- Does anything make your pain better or worse?
- Does your pain limit your ability to function?
- Have you recently felt down, depressed or hopeless?
- Have you ever had pelvic surgery?
- Have you ever been pregnant?
- Have you ever been treated for a urinary tract or vaginal infection?
- Have you ever been touched against your will?
- What treatments have you tried so far for this condition? How have they worked?
- Are you currently being treated or have you recently been treated for any other medical conditions?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Pelvic Pain: Causes, Symptoms, Diagnosis, Treatment
Written by WebMD Editorial Contributors
In this Article
- What Causes Pelvic Pain?
- What Symptoms Suggest a Problem?
- How Is the Cause of Pelvic Pain Determined?
- How Is Pelvic Pain Treated?
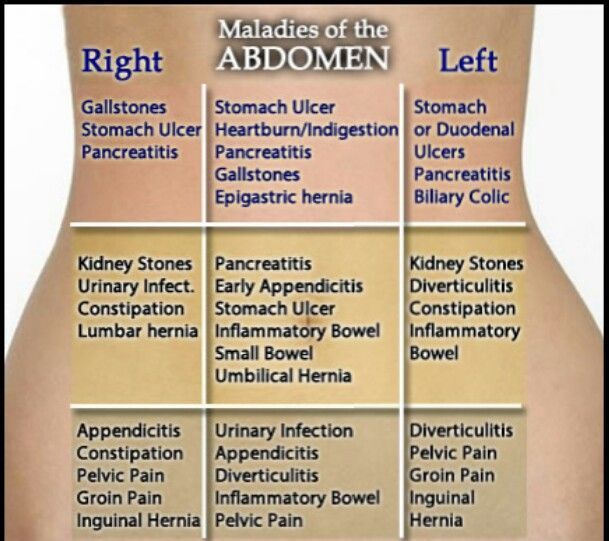
Although pelvic pain often refers to pain in the region of women's internal reproductive organs, pelvic pain can be present in men, too, and can stem from multiple causes. Pelvic pain may be a symptom of infection or may arise from pain in the pelvic bone or in non-reproductive internal organs, such as the bladder or colon. In women, however, pelvic pain can very well be an indication that there may be a problem with one of the reproductive organs in the pelvic area (uterus, ovaries, fallopian tubes, cervix, or vagina).
Pelvic pain may be a symptom of infection or may arise from pain in the pelvic bone or in non-reproductive internal organs, such as the bladder or colon. In women, however, pelvic pain can very well be an indication that there may be a problem with one of the reproductive organs in the pelvic area (uterus, ovaries, fallopian tubes, cervix, or vagina).
What Causes Pelvic Pain?
Possible causes of pelvic pain in both men and women may include:
- Appendicitis
- Bladder disorders (including urinary tract infections)
- Sexually transmitted diseases
- Kidney infection or kidney stones
- Intestinal disorders
- Nerve conditions
- Hernia
- Pelvis disorder
- Prostatitis
- Testicular disorders
- Broken pelvis
- Psychogenic pain
Possible causes of pelvic pain in women only may include:
- Ectopic pregnancy
- Miscarriage
- Pelvic inflammatory disease
- Ovulation
- Menstrual cramps
- Ovarian cysts or other ovarian disorders
- Fibroids
- Endometriosis
- Uterine cancer
- Cervical cancer
What Symptoms Suggest a Problem?
- Worsening of menstrual cramps
- Menstrual pain
- Vaginal bleeding, spotting or discharge
- Painful or difficult urination
- Constipation or diarrhea
- Bloating or gas
- Blood seen with a bowel movement
- Blood in urine
- Pain during intercourse
- Fever or chills
- Pain in the hip area
- Pain in the groin area
How Is the Cause of Pelvic Pain Determined?
To determine what is causing pelvic pain, your doctor will first ask you several questions about your symptoms and past medical problems.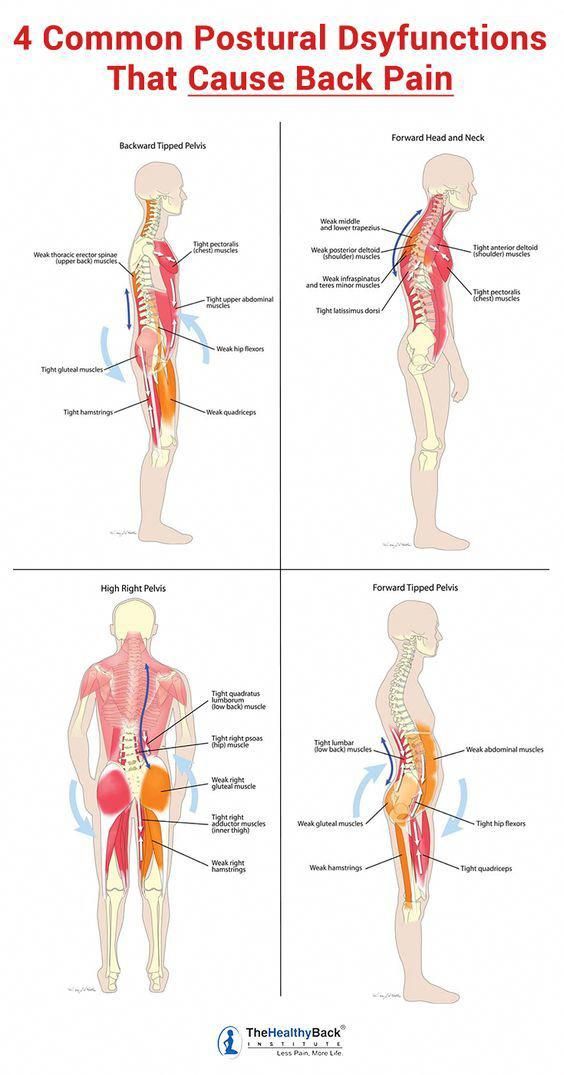 They will also perform a physical exam and may offer you tests to determine what is causing your pain. Other tests that may be given include:
They will also perform a physical exam and may offer you tests to determine what is causing your pain. Other tests that may be given include:
- Blood and urine tests
- Pregnancy tests in females of reproductive age
- Vaginal or penile cultures to check for sexually transmitted diseases such as gonorrhea and/or chlamydia
- Abdominal and pelvic X-rays
- MRI
- Bone density screening (special type of X-ray to determine the strength of bone)
- Diagnostic laparoscopy (procedure allowing a direct look at the structures in the pelvis and abdomen)
- Hysteroscopy (procedure to examine the uterus)
- Stool test (checking a stool sample for microscopic blood)
- Lower endoscopy (insertion of a lighted tube to examine the inside of the rectum and part or all of the colon)
- Ultrasound (test that uses sound waves to provide images of internal organs)
- CT scan of the abdomen and pelvis (scan that uses X-rays and computers to produce an image of a cross-section of the body)
How Is Pelvic Pain Treated?
The treatment of pelvic pain varies depending on the cause, how intense the pain is, and how often the pain occurs.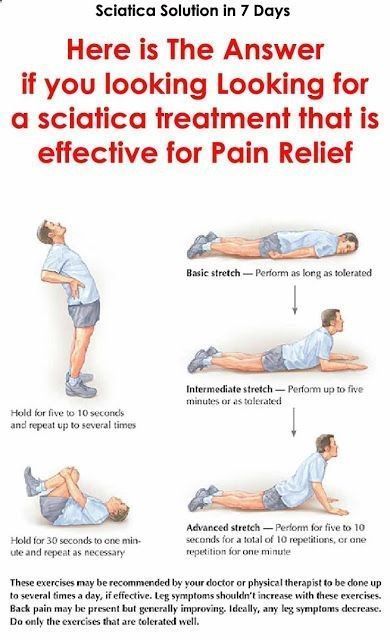 Sometimes, pelvic pain is treated with medications, including antibiotics if necessary. If the pain results from a problem with one of the pelvic organs, the treatment may involve surgery or other procedures. A doctor can provide more information about various treatments for pelvic pain.
Sometimes, pelvic pain is treated with medications, including antibiotics if necessary. If the pain results from a problem with one of the pelvic organs, the treatment may involve surgery or other procedures. A doctor can provide more information about various treatments for pelvic pain.
Pain Management Guide
- Types of Pain
- Symptoms & Causes
- Diagnosis & Tests
- Treatment & Care
- Living & Managing
- Support & Resources
Treatment of chronic pelvic pain | SMT Clinic Yekaterinburg. Multidisciplinary Medical Center
Home / Urology / Treatment of chronic pelvic pain
CHRONIC PELVIC PAIN is a constant or intermittent, recurring pain that is present in the pelvic area in men or women, lasting more than 6 months.
Pain is often associated with emotional deterioration, and may be accompanied by complaints of reproductive and/or sexual functions, as well as urinary function.
Chronic pelvic pain in urology has several forms and manifestations: painful bladder syndrome / interstitial cystitis, chronic prostatitis / chronic pelvic pain syndrome, scrotal, testicular, adnexal, penile, urethral and post-vasectomy (after surgery for ligation of the vas deferens in men ) pain syndromes.
Expand
Doctors
Reception 1 700 ₽
Seskutov Pavel Pavlovich
urologist-andrologist, neurourologist
Reception at the address:
Serova, 45
Leave a request - we will call you back.
reviews
about doctors
Pavel Pavlovich is a very good specialist
Doctor: Seskutov Pavel Pavlovich
Doctor Seskutov examined me and gave me the necessary recommendations, and, in my opinion, everything was at the highest level . I would say that the specialist did everything that was needed.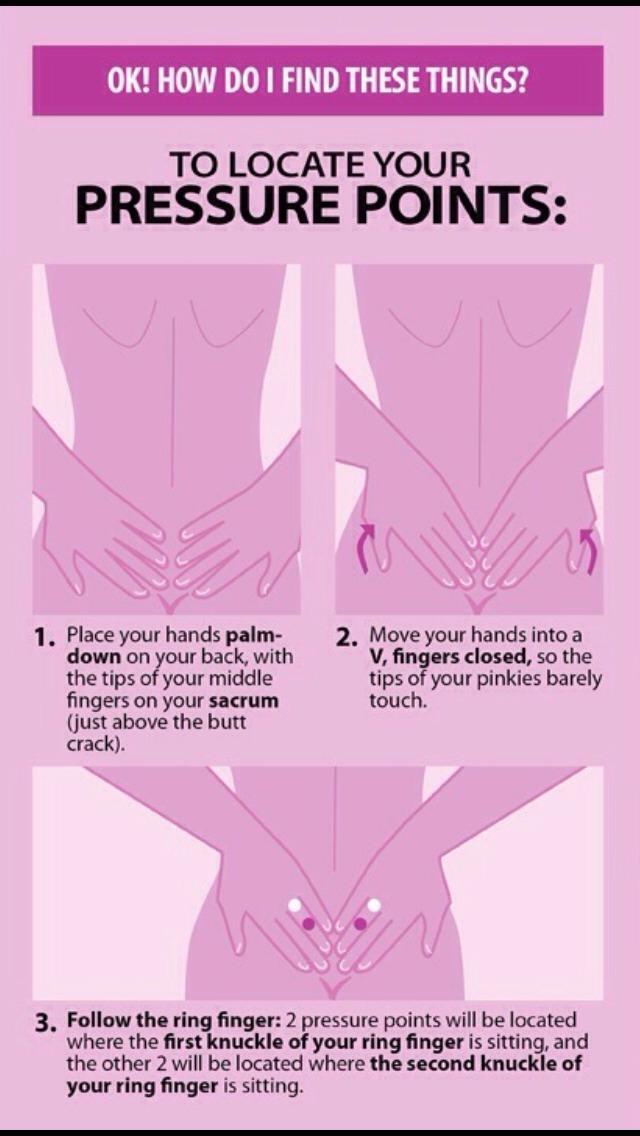 I told the doctor about my problems and their solution was very good.
I told the doctor about my problems and their solution was very good.
Dr. Seskutov examined me and gave me the necessary recommendations, and, in my opinion, everything was at the highest level. I would say that the specialist did everything that was needed. I told the doctor about my problems and their solution was very good.
As a result of the visit, he wrote me a treatment, and after completing his course, I want to go to the specialist again, besides, he recommended that I come again. I can’t say exactly how long the reception lasted, but it seemed to me that it was quite long and of high quality - we touched on all the questions that interested me. The doctor saw me at the appointed time. In my opinion, he has a very good manner of communication. I would say that Pavel Pavlovich talked to me like a doctor with a patient, and everything was civilized and understandable. I will definitely recommend him to my friends if needed.
Qualitative diagnostics, clarification
Doctor: Pavel Pavlovich Seskutov
I applied with a delicate problem. For men, she is always delicate. I received a full examination, the operation was at the highest level, I liked everything, I advise everyone. The rooms are clean, the staff is polite and humorous.
For men, she is always delicate. I received a full examination, the operation was at the highest level, I liked everything, I advise everyone. The rooms are clean, the staff is polite and humorous.
Applied with a delicate problem. For men, she is always delicate. I received a full examination, the operation was at the highest level, I liked everything, I advise everyone. The rooms are clean, the staff is polite and humorous.
Everything is fine. I recommend
Doctor: Seskutov Pavel Pavlovich
Hello. They turned to Pavel Pavlovich, my son (12 years old) fell ill. The doctor listened carefully, performed an examination, ultrasound, prescribed treatment. He explained everything in a very understandable way, leaving only positive impressions. The treatment helped, the recovery happened exactly as the doctor described.
Hello. They turned to Pavel Pavlovich, my son (12 years old) fell ill.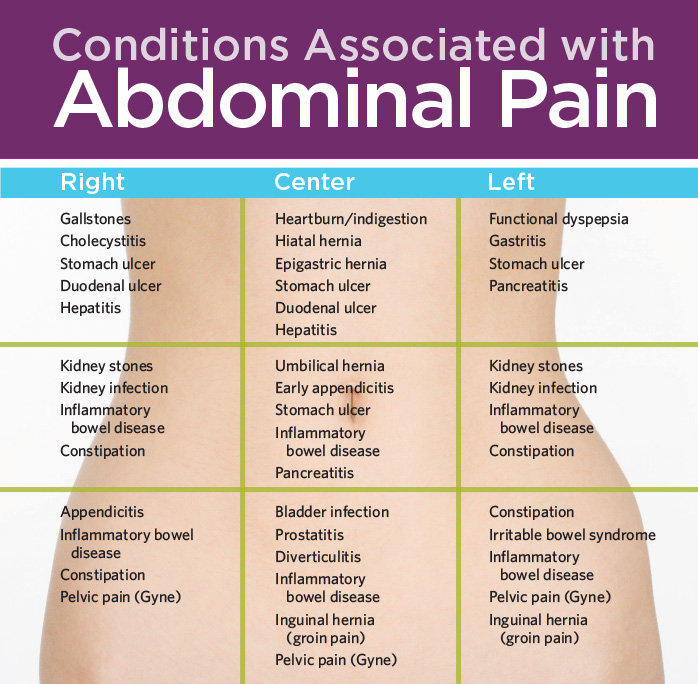 The doctor listened carefully, performed an examination, ultrasound, prescribed treatment. He explained everything in a very understandable way, leaving only positive impressions. The treatment helped, the recovery happened exactly as the doctor described.
The doctor listened carefully, performed an examination, ultrasound, prescribed treatment. He explained everything in a very understandable way, leaving only positive impressions. The treatment helped, the recovery happened exactly as the doctor described.
Everything is fine. I recommend.
I liked everything
Doctor: Pavel Pavlovich Seskutov
He came to me with pain during urination. The doctor diagnosed acute prostatitis. He explained everything clearly, gave directions for tests, prescribed medications. Within 10 days the disease was gone. Following the results of the last appointment, he prescribed two drugs - longidase and prostamol, to consolidate the results of treatment.
Applied with pain when urinating. The doctor diagnosed acute prostatitis. He explained everything clearly, gave directions for tests, prescribed medications. Within 10 days the disease was gone. Following the results of the last appointment, he prescribed two drugs - longidase and prostamol, to consolidate the results of treatment.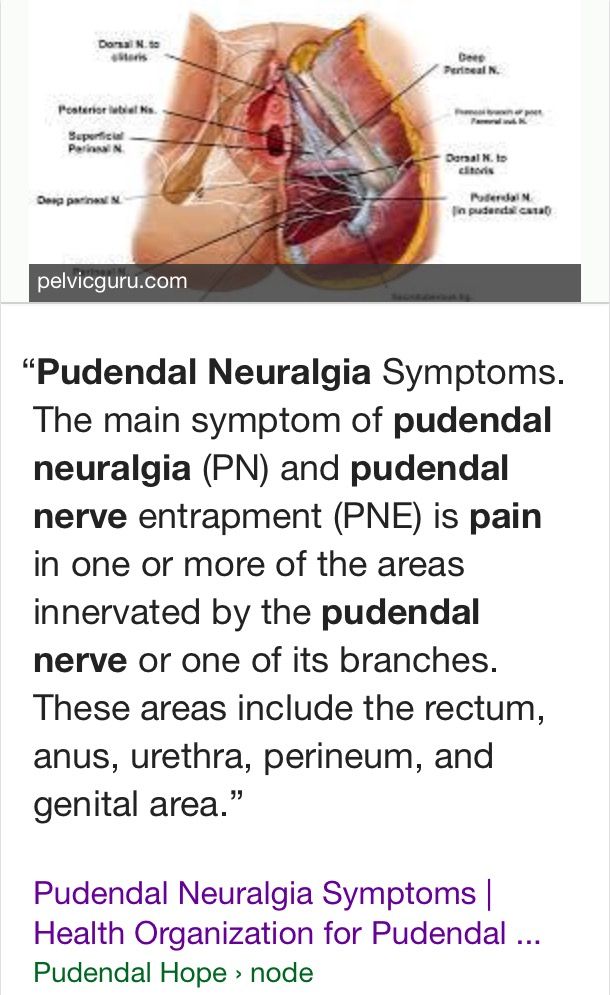
Desire to understand and help the patient
Doctor: Seskutov Pavel Pavlovich
I live in a small town where ultrasound occupies the main place in diagnosis, but with this disease, given my complaints, I needed CT and better with contrast. Pavel Pavlovich prescribed an examination, drugs for pain and urination disorders. In the future, surgical treatment is planned.
I live in a small town where ultrasound is the main diagnostic tool, but with this disease, considering my complaints, I needed CT and better with contrast. Pavel Pavlovich prescribed an examination, drugs for pain and urination disorders. In the future, surgical treatment is planned.
about the medical center
Convenient location in Yekaterinburg
Near the metro and not far from the center. It is convenient to get to the SMT Clinic from any area and by any means of transport. There are parking pockets on Surikov and Serov, the street is not overloaded with vehicles, it has entrances from any side of the city.
There are parking pockets on Surikov and Serov, the street is not overloaded with vehicles, it has entrances from any side of the city.
OWN LABORATORY. RESULTS IN 1-2 DAYS!
CMT saves time for patients and provides laboratory tests within 1-2 days within its own laboratory. The results of some types of analyzes are received by patients of the CMT Clinic almost immediately after admission.
WE ARE THE EXPERTS
We are not only equipped with expert medical equipment, but we are also proud of our doctors. CMT doctors constantly undergo additional training, speak at events, or teach at medical schools in our country.
CLINIC FOR THE WHOLE FAMILY
CMT is a multidisciplinary medical center. The clinic has 32 adult departments, 20 children's departments (on a separate floor of the building), as well as automobile and other types of commissions with a separate entrance to the building.
Treatment of patients with chronic pelvic pain syndrome in a single center | Kruglov
Introduction
Patients with complaints of pain in the pelvis and perineum are well known to practicing urologists.
These patients are clearly accentuated by the existing symptoms, are characterized by a negative psycho-emotional background, as a rule, they are treated for a long time and without a significant effect by various specialists [1].
Management of such patients is still an unsolved problem.
The stereotype that was previously formed in urological practice to interpret such symptoms as manifestations of chronic prostatitis has long and obviously outlived itself. Chronic pelvic pain syndrome (CPPS) is currently widely discussed.
An examination of the literature on this issue reveals at least two interpretations of this term. On the one hand, CPPS is, according to the accepted classification, one of the variants of chronic prostatitis (categories 3a and 3b), on the other hand, more modern position, CPPS is considered as a major syndrome, one of the many causes of which may be chronic prostatitis [2][3 ].
The term "pelvic pain" came to domestic medicine from foreign medical publications. According to the recommendations of the guidelines of the European Association of Urology (2009), chronic pelvic pain syndrome is persistent or recurring pain in the pelvic region, noted for at least 6 months.
According to the recommendations of the guidelines of the European Association of Urology (2009), chronic pelvic pain syndrome is persistent or recurring pain in the pelvic region, noted for at least 6 months.
"Pelvic" refers to pain localized in the lower abdomen below the navel, in the lower back and sacrum, as well as in the perineum, in the vulva, vagina, rectum. Often there is irradiation along the anterointernal surface of the thighs and the lower edge of the buttocks. Usually, patients cannot indicate the exact localization of pain and separate the epicenter of pain from the irradiation zone.
Chronic pelvic pain depresses the patient's psycho-emotional state, sharply reduces the quality of life. It is known that the effect of CPPS on the mental sphere of a patient is comparable to the effect of myocardial infarction, unstable angina pectoris, ulcerative colitis, and more than the effect of toothache and ear pain [4][5]. In the specialized literature, there are indications that 27% of patients with CPPS suffer from severe depression and drug dependence, 18% have significant emotional disorders during the period of exacerbation of the pain syndrome, and almost 35% of patients have a history of indications of suicidal attempts or intentions, which once again confirms medical and social significance of this pathology [3][6].
In addition to pain, the concept of CPPS also includes other manifestations related to disorders of the pelvic organs - increased urination, stool disorders, changes in the tone of the pelvic muscles, sexual dysfunction, psycho-emotional disorders. These symptoms are almost always present to varying degrees in patients with this problem, complicating and confusing the causal relationship between them. That is why recently, in foreign literature, instead of the term "chronic pelvic pain syndrome", the term "chronic pelvic pain syndrome and dysfunction" is used as a broader one.
It is now recognized that chronic pelvic pain syndrome is a collective name for a variety of pathological conditions, united by the presence of pain in the pelvic area, including those when the prostate gland is only indirectly involved in the pathological process or is not involved at all [7] [8][9].
Pain syndromes in the pelvic region have been described in the literature for a long time, however, the interpretation of their nature still causes great difficulties.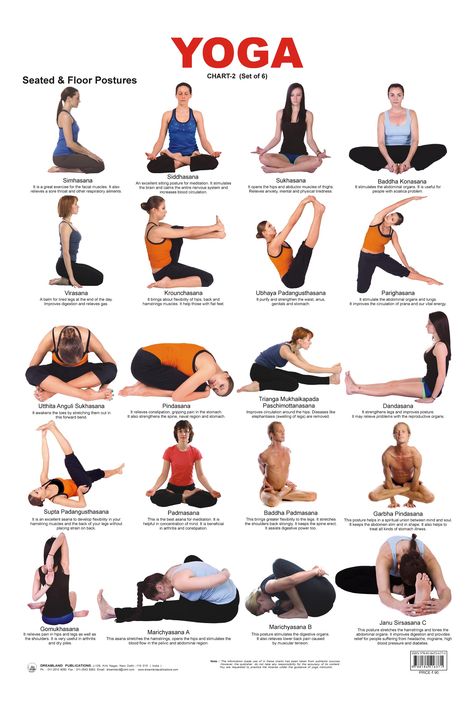 This syndrome, according to the figurative expression of D.H. Zermannetal from the University of Colorado (USA) is still a "diagnostic and therapeutic puzzle" [10][11]. L. Hahn (2001) believes that in differential diagnostic terms, one has to keep in mind more than 70 diseases that can cause pelvic pain. And, on the contrary, even with the most thorough examination, any pathology may not be found [12][13].
This syndrome, according to the figurative expression of D.H. Zermannetal from the University of Colorado (USA) is still a "diagnostic and therapeutic puzzle" [10][11]. L. Hahn (2001) believes that in differential diagnostic terms, one has to keep in mind more than 70 diseases that can cause pelvic pain. And, on the contrary, even with the most thorough examination, any pathology may not be found [12][13].
Chronic pain in the perineal region may be due to pathology of the internal organs of the pelvis and genital organs, damage to the muscles of the pelvic floor and the osseo-ligamentous apparatus, involvement of peripheral nerves, and may also be caused by psychological and other factors. The organs of the small pelvis are closely interconnected, often have a common innervation, blood circulation, musculoskeletal apparatus. In fact, the entire pelvic area is a vast reflexogenic zone, and the defeat of one organ often involves others in the pathological process.
The complexity and multifactorial nature of the etiopathogenesis of pain syndromes in the pelvic area is reflected in the attempts of foreign authors to systematize these patients.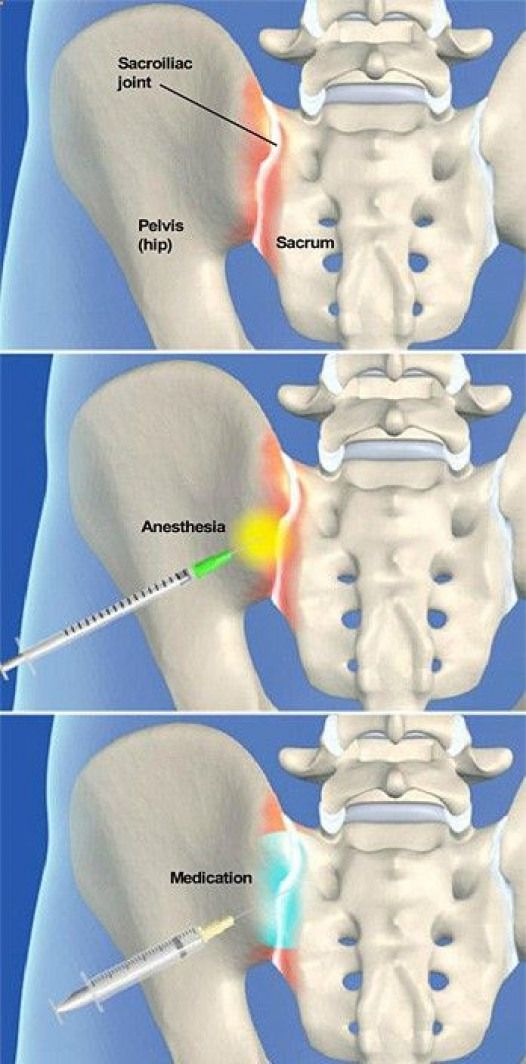 The most well-known and widely used is the so-called UPOINT clinical phenotyping system, which involves the assessment and summation of symptoms in 6 different diagnostic areas, referred to in the original technique as diagnostic domains. In particular, urinary, organ-specific (prostatic), infectious, neurological, psychosocial and muscle pain domains are distinguished. The system has proven to be effective in classifying patients with urological pelvic pain syndromes in a clinically relevant manner for appropriate therapy [14].
The most well-known and widely used is the so-called UPOINT clinical phenotyping system, which involves the assessment and summation of symptoms in 6 different diagnostic areas, referred to in the original technique as diagnostic domains. In particular, urinary, organ-specific (prostatic), infectious, neurological, psychosocial and muscle pain domains are distinguished. The system has proven to be effective in classifying patients with urological pelvic pain syndromes in a clinically relevant manner for appropriate therapy [14].
According to the literature, the point of view that the role of inflammatory diseases in the pathogenesis of chronic pelvic pain syndrome is becoming more and more dominant. Currently, the main role is given to myofascial (spastic) syndromes of the pelvic floor muscles and neuropathies of the pudendal nerve.
Myofascial pain syndromes (MFPS) are caused by chronic spasm of the musculo-ligamentous apparatus of the small pelvis. These syndromes are quite widespread, but rarely diagnosed in urological practice. Although, for example, Skootsky S. reports 30% of patients with chronic pelvic pain who were diagnosed with myofascial syndromes in specialized clinics for the treatment of pain syndromes, according to Bartoletti R. myofascial syndromes were detected in 13.8% of cases [11][ 15].
Although, for example, Skootsky S. reports 30% of patients with chronic pelvic pain who were diagnosed with myofascial syndromes in specialized clinics for the treatment of pain syndromes, according to Bartoletti R. myofascial syndromes were detected in 13.8% of cases [11][ 15].
Involvement of the pelvic floor muscles and peripheral nerves in the pathological process can occur at various stages of diseases of the pelvic organs and is an integral part of the chronicization of pelvic pain - that is, myofascial syndromes are usually secondary. But the complexity of the situation is that in some cases, the primary disease of the pelvic organs regresses against the background of specific therapy or spontaneously or passes into a latent, difficult-to-diagnose form, and pain in the pelvic region, caused by secondary changes in the muscles and peripheral nerves of the pelvic region, persists and even aggravated, "breaking away" from the root cause.
A long-term muscular-tonic syndrome can lead to muscle dysfunction with the development of myofascial syndrome, the appearance of trigger points characteristic of the latter and the corresponding reflected pain patterns. An increase in the tone of the muscles of the pelvic floor and perineum, together with pain, can initiate dysuric disorders of both mechanical and reflex origin [2][7][16].
An increase in the tone of the muscles of the pelvic floor and perineum, together with pain, can initiate dysuric disorders of both mechanical and reflex origin [2][7][16].
On the one hand, the diagnosis of MFPS must be a diagnosis of exclusion. On the other hand, the presence of, for example, “classic” bacterial chronic prostatitis in a patient does not exclude, but on the contrary, also suggests the presence of myofascial complications.
The pathophysiological mechanisms of the formation of chronic spasm of the musculo-ligamentous apparatus are presented as follows.
Any condition that causes pain more or less for a long time leads to a decrease in the threshold of pain sensitivity - this is the so-called central sensitization, which develops when the neurons of the posterior horns of the spinal cord receive a powerful "volley" of signals from pain receptors. At the same time, a progressive increase in neuronal activity occurs in the neurons of the posterior horns, known as the wind-up phenomenon, in which neurons become more sensitive to subsequent impulses.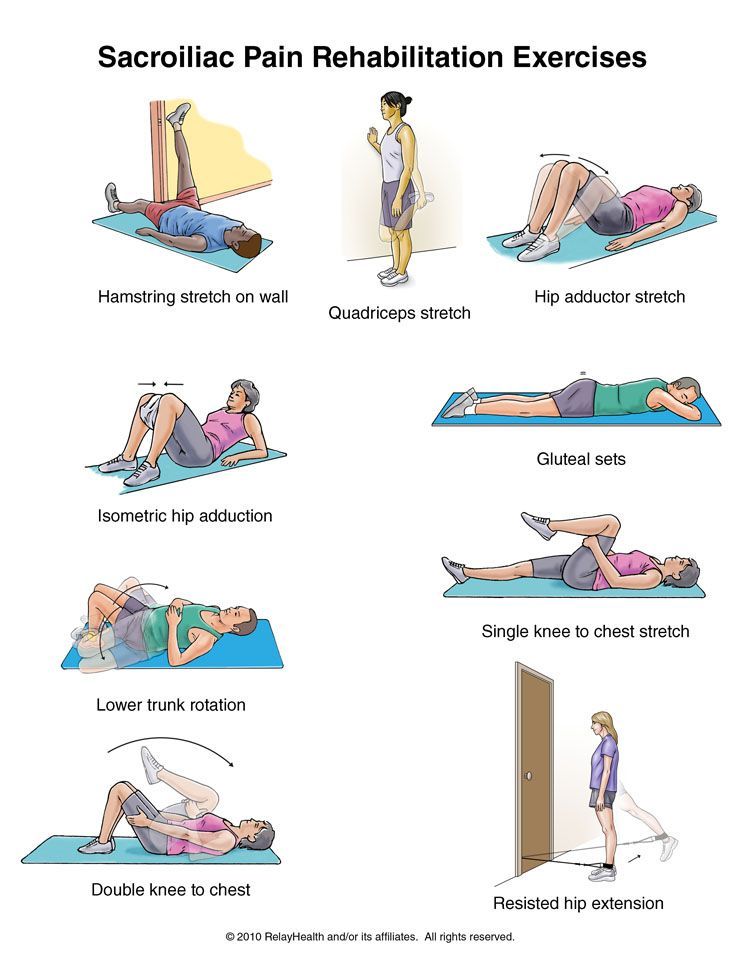 The next step is peripheral sensitization. In the affected organ, the production of nerve growth factor (NGF, NGF) increases. This leads to an increase in the number of receptors affiliated with demyelinated C-fibers, the main role of which is the transmission of chronic pain impulses. Accordingly, an increase in their number leads to an increase in pain in the affected organ.
The next step is peripheral sensitization. In the affected organ, the production of nerve growth factor (NGF, NGF) increases. This leads to an increase in the number of receptors affiliated with demyelinated C-fibers, the main role of which is the transmission of chronic pain impulses. Accordingly, an increase in their number leads to an increase in pain in the affected organ.
Given that the pelvic organs have cross-innervation, the number of receptors for C-fibers increases not only in the "original organ", but in those with which it is associated with cross-innervation - this is cross-sensitization. Such a cross-reaction is typical, for example, for the endo- and myometrium, and the bladder urothelium [9]. However, most muscles are not adapted to function under conditions of prolonged tonic tension, which is a physiological response to pain stimulation. This leads to the appearance of a large number of underoxidized metabolic products in the muscle tissue - secondary disorders appear in the muscle: vascular, metabolic, inflammatory and, as a result, local spasmodic zones are formed, which are called "trigger points" (the term was proposed by Janet Travell, 1942d). These are seals that are felt on palpation and are formed by tense muscle fibers. Thus, the pathogenesis of MFPS is very complicated, but pain that almost always arises and exists for some time triggers a vicious circle of processes that make it self-sustaining even in the absence of the root cause.
These are seals that are felt on palpation and are formed by tense muscle fibers. Thus, the pathogenesis of MFPS is very complicated, but pain that almost always arises and exists for some time triggers a vicious circle of processes that make it self-sustaining even in the absence of the root cause.
The most common pelvic myofascial syndromes include levator syndrome, internal obturator muscle syndrome, and piriformis syndrome.
Levator syndrome is associated with spasm of the levator ani muscle. According to J. Rigaud, this syndrome occurs in 100% of cases in patients with CPPS and is characterized by pain in the anus and rectum, aggravated in the sitting position, pain on palpation of the sphincter. The syndrome of the internal obturator muscle is caused by a spasm of m. obturatorius internus and is manifested by the feeling of a foreign body in the rectum, pain in the urethra and perineum [4][9].
Currently, there is no consensus regarding the treatment of CPPS, just as there is no way to accurately determine the pathophysiological causes of this disease in each specific case [7][16].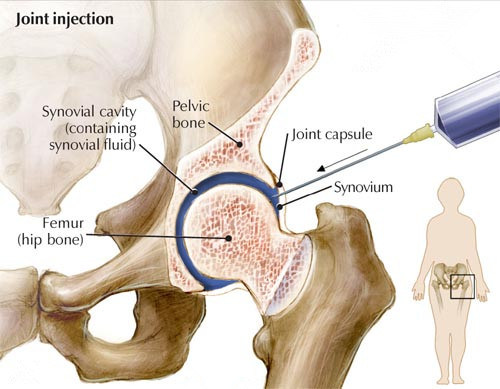
Long courses of antibiotic therapy have until recently been considered the mainstay of treatment for CPPS. However, studies conducted with long-term use of a number of antibiotics have not shown a significant positive result. The results of studies on the use of alpha-blockers are also very controversial. So Cheah P.Y. et al. in their works note the positive effect of the use of drugs of this group in CPPS [15][17]. Alexander R.B. et al. in their publication, on the contrary, they note a slight effect of the use of tamsulosin in patients with CPPS [15].
Anti-inflammatory drugs and immunomodulators as monotherapy are not recommended by many authors due to insignificant leveling of symptoms [2][6][12]. The use of a combination of corticosteroids with antibiotics was proposed as a hypothesis by Tomaskovic I. et al. [15][18]. Yang M.G. and et al. conducted a randomized double-blind study in which they noted a positive effect in the short term.
Foreign authors also note that such treatments as low-intensity shock wave therapy, acupuncture, biofeedback, invasive neuromodulation, the use of botulinum toxin injections require more thorough research to confirm the effectiveness of their use both as monotherapy and in combinations with other treatments [2].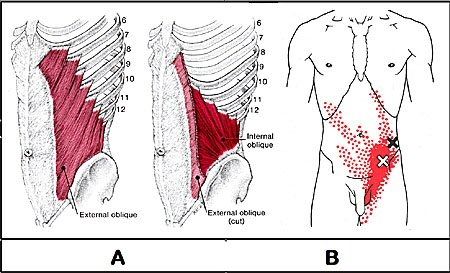
Also in the literature, muscle relaxants and analgesics of central action, antidepressants, local anesthetics and anticonvulsants used for the treatment of neuropathic pain appear in the literature as means of complex therapy for CPPS [15].
The given literature data demonstrates the absence of a generally accepted approach to the diagnosis and treatment of the syndrome, as well as to the etiopathogenetic nature of pain in the pelvic area. Obviously, the final resolution of the complex of contradictions is a matter for the future. However, quite a practical question about the treatment of patients with this symptomatology remains relevant. In our work, we aimed to improve the results of treatment of patients suffering from CPPS.
Materials and methods
The study included 46 patients who underwent course treatment at the urological clinic of the Astrakhan State Medical University on the basis of the Aleksandro-Mariinsky Regional Clinical Hospital from 2016 to August 2018.
These were men aged 26 to 57 years, the average age was 32.0 ± 5.1 years.
The main criterion for inclusion of patients in the study is the presence of a leading complaint of long-term pain in the pelvis and/or perineum. The average duration of the disease was 3.8±2.1 years.
Based on the concept of multifactoriality of chronic pelvic pain syndrome, all patients underwent an in-depth examination in order to exclude "dangerous" causes of CPPS, the so-called "red flags" [5][7][19].
The diagnostic complex included the determination of the state of the prostate gland and the severity of inflammatory changes in it and in the urinary system: complete blood and urine analysis, digital rectal examination of the prostate (PG), transrectal ultrasound examination of the pancreas (TRUS), determination of the volume of residual urine, CT of the retroperitoneal space, MRI of the pelvis, microscopic examination and bacterial culture of the secretion of the pancreas, microscopic examination of the urethral smear and PCR diagnostics to exclude sexually transmitted diseases (STIs).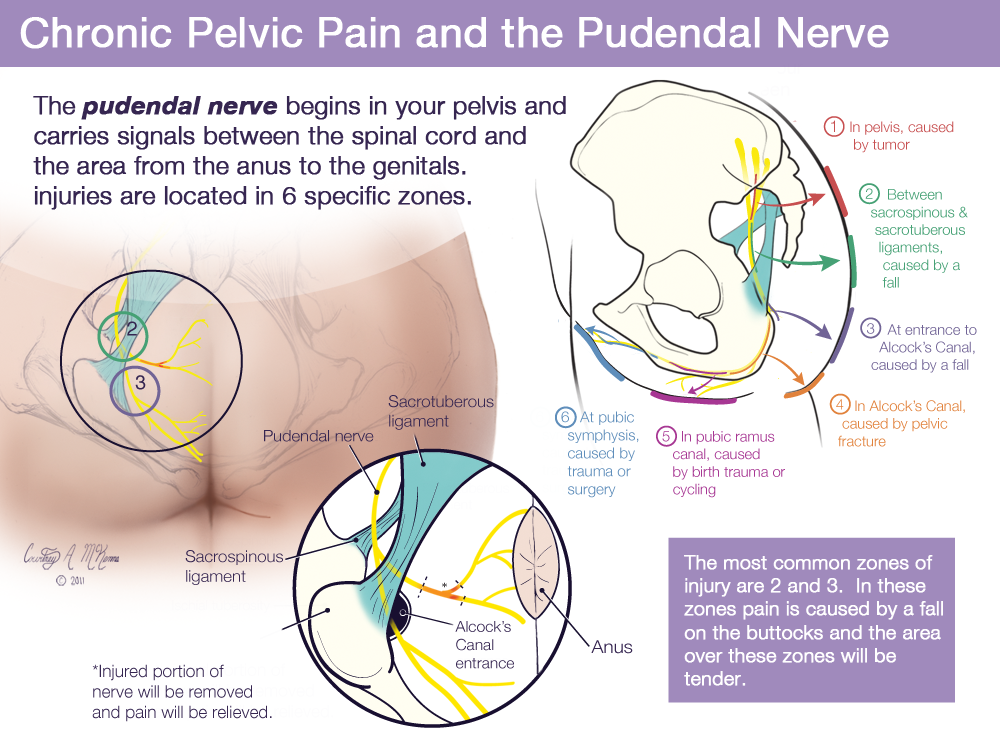 All patients over 40 years of age underwent a study of the level of prostate-specific blood antigen (PSA).
All patients over 40 years of age underwent a study of the level of prostate-specific blood antigen (PSA).
In some cases, when a pathology of the seminiferous tubercle was suspected, the examination was expanded by performing diagnostic urethrocystoscopy, which in some cases made it possible to identify hypertrophy and inflammatory changes in the seminal tubercle - such patients were not included in the study.
An additional diagnostic element specific for urological practice was an active search for myofascial pelvic syndromes in these patients to clarify the presence and severity of the neuropathic pain component. For this purpose, patients were examined to identify hypertonicity of the pelvic and perineal muscles, trigger points, and filled out the neuropathic pain questionnaire (DN4), intended for widespread use by practitioners. DN4 was developed as a tool for the diagnosis and differential diagnosis of neuropathic pain.
The exclusion criteria were acute urogenital inflammatory processes, sexually transmitted infections, other diseases of the pelvic organs, accompanied by pain, including vascular and oncological pathology, diseases of the lower thoracic and lumbosacral spine, decompensated conditions of other organs and systems.
Symptom severity was assessed by testing using the International Prostatic Symptom Score (IPSS) questionnaire. Pain severity was additionally assessed using a 10-point Numeric rating Scale for pain (NRS). Symptoms were assessed 3 times: at the beginning of treatment, in the middle of the course and at its completion.
According to the results of the examination, 20 patients (43.5%) showed signs of an inflammatory process in the prostate gland, 26 (56.5%) did not. As a criterion for the inflammatory process, the detection of more than 10 leukocytes in the field of view during microscopy of the secret of the prostate gland, a positive result of bacterial seeding of the secret of the prostate gland was taken.
Case management was organized as follows. Patients with proven inflammatory changes in the prostate gland were divided into two equal and comparable groups: the first group received "standard" therapy for chronic prostatitis (antibiotics, prostatotropic drugs, microcirculation and immunocorrection agents, physiotherapy), in the second group, patients received "standard" treatment in combination with myofascial blockades and neuropathic pain therapy. Patients without inflammatory changes in the prostate were combined into the third group and received only myofascial blockades and neuropathic pain therapy, since we consider it unjustified to prescribe antibiotic therapy in this case.
Patients without inflammatory changes in the prostate were combined into the third group and received only myofascial blockades and neuropathic pain therapy, since we consider it unjustified to prescribe antibiotic therapy in this case.
In accordance with the results of the examination, patients underwent blockades of m.levator ani, m. obturatorius internus under electromyostimulation control. The latter seems to be a very essential component of the methodology. Access to the muscles located in the pelvic cavity is limited, so the use of electrical stimulation is the easiest way to control the position of the needle in order to confidently inject the drug into the target muscle group. Abbreviations m. levator ani, m. obturatorius internus under the action of electrical stimulation is determined by palpation per rectum. For this purpose, we used a domestically produced electromyostimulator.
Given the well-known difficulties in the use of botulinum toxin preparations, for myofascial blockades, we used a solution of novocaine 0.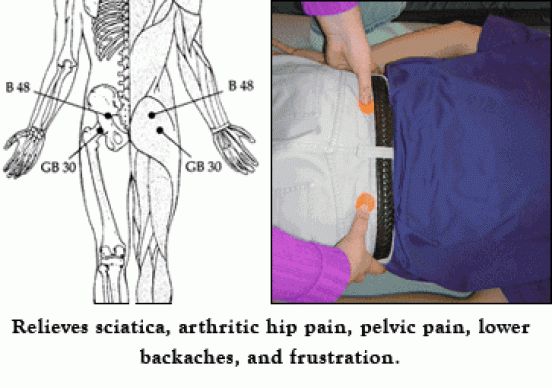 5% 40-80 ml with the addition of 2-4 mg of ropivacaine or lidocaine and 8 mg of dexamethasone. Blockades were performed with a frequency of 2 times a week for a total of 6 procedures and were supplemented with oral administration of gabapentin at a standard dosage (on the first day - 300 mg, on the second - 600 mg in 2 doses, on the third - 900 mg in 3 doses, a course of 2 months)
5% 40-80 ml with the addition of 2-4 mg of ropivacaine or lidocaine and 8 mg of dexamethasone. Blockades were performed with a frequency of 2 times a week for a total of 6 procedures and were supplemented with oral administration of gabapentin at a standard dosage (on the first day - 300 mg, on the second - 600 mg in 2 doses, on the third - 900 mg in 3 doses, a course of 2 months)
As clinical diagnostic criteria for improvement against the background of ongoing therapy, the following were taken: a decrease in the intensity of pain on an analog scale, a decrease in the total IPSS symptom index and an improvement in the quality of life, for patients with an established inflammatory process in the prostate gland - elimination of the pathogen during bacteriological examination of the secretion of the prostate gland, a decrease in the degree of inflammatory changes in the secretion of the prostate gland (less than 10 leukocytes in the field of view during microscopic examination of the secretion of the pancreas)
Statistical processing of the obtained data was carried out according to the Student's method, differences in indicators were considered significant at p<0. 05.
05.
Results and discussion
When analyzing the results, regardless of the presence or absence of an inflammatory process, the effect of pain on the total symptom score does not go beyond the accepted error, and the assessment of pain intensity is the same (Table 1).
Table 1. Baseline characteristics of study patient groups
Myofascial blockade + neuropathic pain therapy
%), in 18% of patients, pain was localized only in the perineum, and 10% of patients noted the migratory nature of pain, periodically occurring in different anatomical areas of the pelvis. The predominant localization of pain was in no way associated with the presence or absence of the inflammatory process. In the presence of inflammation in the prostate gland during bacteriological examination, the most common microorganisms found were: E. coli - 26.8%, Enterobacter spp. - 16.0%, Enterococcus spp. - 14.6% Staphylococcus spp. - 7.5%, Enterococcus faecalis - 6.3%.
- 7.5%, Enterococcus faecalis - 6.3%.
As for the diagnosis of myofascial syndromes, according to our observations, there was also no significant correlation of such symptoms with the inflammatory component in the prostate - positive results of varying severity were encountered approximately equally in both groups. It should be noted that the identification of muscle hypertonicity and trigger points is quite subjective, given the practical impossibility of any quantitative characterization of this condition.
We observed the most pronounced effect from myofascial blockades in patients of the third group, since it was in them that the clinical picture was to the greatest extent due to the muscular-tonic component (diagrams 1, 2). A decrease in the severity of the pain syndrome was noted, as a rule, after the first procedure, but it was rather short-lived, due to the short period of action of the drugs used. In the future, the duration and severity of the effect increased significantly, which, on the one hand, is associated with a cumulative effect, the specific mechanisms of which require clarification, but are presumably associated with gradually developing desensitization, and, on the other hand, with a course of gabapentin.
Diagram 1. Dynamics of the I-PSS index during treatment
Diagram 1 .1-PSS Index DYNAMICS DURING OF TREATMENT
9000
0
1 during treatment
Diagram 2. NRS index dynamics during of treatment
such in patients without inflammatory changes in the prostate gland. The effectiveness of blockades in this case confirms the presence of the myofascial component of the pain syndrome in chronic bacterial prostatitis, and the worse overall dynamics, compared with patients of the second group, is consistent with the well-known ideas about the complexity of antibiotic therapy for prostatitis and the need for a long course of antibiotics.
During the course of blockades, in several cases, prolonged pain was noted at the injection site; We did not observe more serious complications.
Conclusion
The problem of developing a unified approach to understanding CPPS is obviously far from being resolved - o6 this is evidenced by dozens of theories and hypotheses of its origin.
Progress in this area should be expected as the differential diagnosis of these conditions improves, the clinical classification of the disease becomes more detailed, and the accumulation of reliable clinical results characterizing the efficacy and safety of drugs. However, even now the correction of musculo-tonic disorders
in this syndrome, it should be recognized as an effective and safe method of therapeutic effect and this method should be recommended for inclusion in complex therapy for CPPS/chronic prostatitis.
1. Protopopova N.V., Kogan A.S., Semendyaev A.A., Bochkov V.V. Modern ideas about the etiology, pathogenesis, diagnosis and treatment of chronic pelvic pain in women. Bulletin of the VSNC SO RAMS. 2005;6(44):180-190.
2. Cab drivers S.B., Selitsky G.V., Kamchatnov P.R. Syndrome of chronic pelvic pain. Journal of Neurology and Psychiatry. S.S. Korsakov. 2011;111(5):71-74.
3. Stefanidi A.V. Myofascial chronic pelvic pain in women. Bulletin of the VSNC SO RAMS.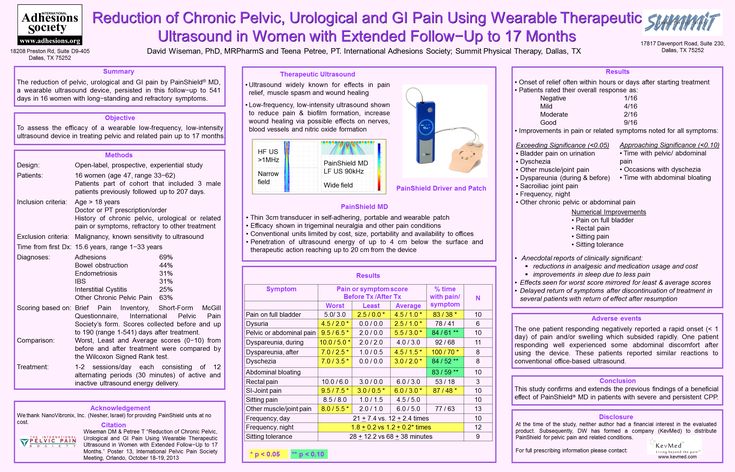 2006;5(51):176-180.
2006;5(51):176-180.
4. I. A. Apolikhina, Ya. B. Mirkin, I. A. Eizenach, O. Yu. Pelvic dysfunctions and pain syndromes in the practice of a urologist. Experimental and clinical urology. 2012;2:85-90
5. Sivkov A.V., Romikh V.V., Zakharchenko A.V. Category IIIB chronic prostatitis/chronic pelvic pain syndrome and sexual dysfunction. Andrology and genital surgery. 2015;16(4):18-26. DOI: 10.17650/2070-9781-2015-16-4-18-26
6. Kryuchkova M.N., Soldatkin V.A. Chronic pelvic pain syndrome: psychopathological aspects. Bulletin of Urology. 2017;5(1):52-63. DOI: 10.21886/2308-6424-2017-5-1-52-63
7. Cab drivers S.B., Kaprin A.D. Chronic pelvic pain syndrome: modern approaches to the problem. Materials of the Russian Congress "Men's Health" with international participation; June 16-18, 2010; M.
8. Kogan M.I., Belousov I.I., Bolotskov A.S. Arterial blood flow in the prostate in chronic pelvic pain syndrome/chronic prostatitis. Urology. 2011;3:22-28.
9. Mirkin Ya.B., Karapetyan A.V., Shumov S.Yu. Interstitial cystitis: discussion of pathogenesis, diagnosis and treatment. Part 1. Experimental and clinical urology. 2017;4:96-100.
Mirkin Ya.B., Karapetyan A.V., Shumov S.Yu. Interstitial cystitis: discussion of pathogenesis, diagnosis and treatment. Part 1. Experimental and clinical urology. 2017;4:96-100.
10. Strauss AC, Dimitrakov JD. New treatments for chronic prostatitis/chronic pelvic pain syndrome. Nat Rev Urol. 2010;7(3):127-35. DOI: 10.1038/nrurol.2010.4.
11. Bachar GN, Belenky A, Greif F, Atar E, Gat Y, Itkin M, Verstanding A. Initial experience with ovarian vein embolization for the treatment of chronic pelvic pain syndrome. Isr Med Assoc J. 2003;5(12):843-846. PMID: 14689749
12. Campbell-Walsh Urology. 11th Edition Review, 2nd Edition. 2016.
13. Bolotov A.V., Izvozchikov S.B. Gabapentin (Neurontin) in the treatment of neuropathic pelvic pain/pudendoneuropathy. Medical rehabilitation of patients with pathology of the musculoskeletal and supporting systems: Proceedings of the 7th city scientific and practical. conf.; December 20, 2006; M.
14. Engeler D (Chair), Baranowski AP, Borovicka J, Cottrell AM, Dinis-Oliveira P, Elneil S, Hughes J, Messelink EJ (Vice-chair), de C Williams AC.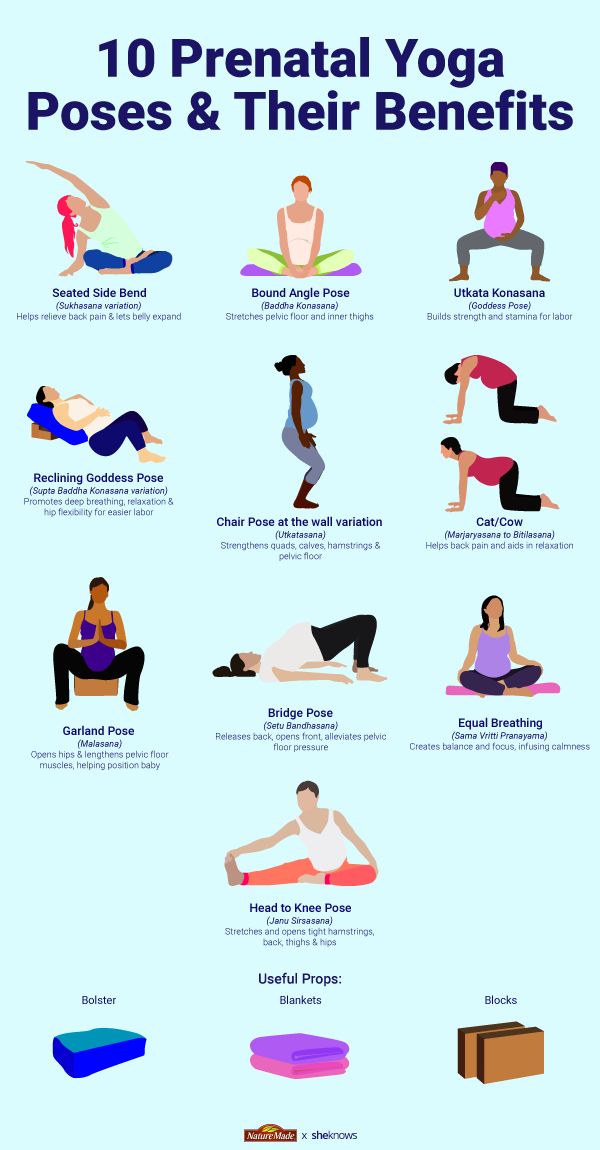 Guidelines Associates: Parsons B, Goonewardene S. EAU Guidelines on Chronic Pelvic Pain. European Association of Urology, 2018. Available at: https://uroweb.org/guideline/chronic-pelvic-pain/ Accessed 25.09..2018
Guidelines Associates: Parsons B, Goonewardene S. EAU Guidelines on Chronic Pelvic Pain. European Association of Urology, 2018. Available at: https://uroweb.org/guideline/chronic-pelvic-pain/ Accessed 25.09..2018
15. Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O'Leary MP, Pontari MA, McNaughton-Collins M, Shoskes DA, Comiter CV, Da???? a NS, Fowler JE Jr, Nadler RB, Zeitlin SI, Knauss JS, Wang Y, Kusek JW, Nyberg LM Jr, Litwin MS; Chronic Prostatitis Collaborative Research Network. Ciprofl oxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004;141(8):581-589. PMID: 15492337
16. Izvozchikov, SB Non-inflammatory syndrome of chronic pelvic pain in men: neurological aspects of the urological problem: Abstract of the thesis. dis. … cand. honey. science M.; 2007. Available at: http://medical-diss.com/medicina/nevospalitelnyy-sindrom-hronicheskoy-tazovoyboli-u-muzhchin-nevrologicheskie-aspekty-urologicheskoyproblemy Link active on 25.