Donated breast milk safety
Use of Donor Human Milk
The benefits of breastfeeding are well established, and breastfeeding is strongly recommended by healthcare professionals and the U.S. Department of Health and Human Services. Information on breastfeeding can be found at:
- HHS Breastfeeding
- CDC Breastfeeding
- USPSTF 2014 Guide to Clinical Preventive Services on Breastfeeding Counseling
- American Academy of Pediatrics Guidelines
In some situations, instead of breastfeeding parents may look for alternative sources of human breast milk to feed their babies.
Consult a healthcare provider first
The choice to feed a baby human milk from a source other than the baby’s mother should be made in consultation with the baby’s healthcare provider, because the nutritional needs of each baby depend on many factors including the baby’s age and health.
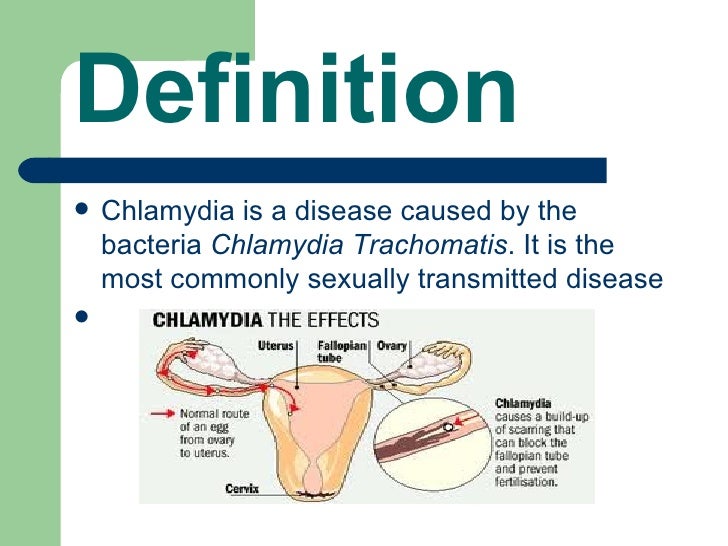
Consider the possible safety risks
If you are considering feeding a baby with human milk from a source other than the baby’s mother, you should know that there are possible health and safety risks for the baby. Risks for the baby include exposure to infectious diseases, including HIV, to chemical contaminants, such as some illegal drugs, and to a limited number of prescription drugs that might be in the human milk, if the donor has not been adequately screened. In addition, if human milk is not handled and stored properly, it could, like any type of milk, become contaminated and unsafe to drink.
FDA recommends against feeding your baby breast milk acquired directly from individuals or through the Internet
When human milk is obtained directly from individuals or through the Internet, the donor is unlikely to have been adequately screened for infectious disease or contamination risk. In addition, it is not likely that the human milk has been collected, processed, tested or stored in a way that reduces possible safety risks to the baby.
FDA recommends that if, after consultation with a healthcare provider, you decide to feed a baby with human milk from a source other than the baby’s mother, you should only use milk from a source that has screened its milk donors and taken other precautions to ensure the safety of its milk.
There are human milk banks that take voluntary steps to screen milk donors, and safely collect, process, handle, test, and store the milk. In a few states, there are required safety standards for such milk banks. FDA has not been involved in establishing these voluntary guidelines or state standards.
You can contact your state’s department of health to find out if it has information on human milk banks in your area. Another source of information is the Human Milk Banking Association of North America (HMBANA), a voluntary professional association for human milk banks (http://www.hmbana.org/ ). HMBANA issues voluntary safety guidelines for member banks on screening donors, and collecting, processing, handling, testing and storing milk.
Donor Milk Safety and Screening • Mothers' Milk Bank Northeast
Mothers’ Milk Bank Northeast follows strict screening, processing, and dispensing guidelines established by the Human Milk Banking Association of North America (HMBANA) in consultation with the Centers for Disease Control, Food and Drug Administration, New York State Department of Health, and the blood and tissue banking industries.
Milk Donors
Milk donors are healthy, lactating women with surplus milk, and babies of any age. Bereaved and surrogate mothers may also donate. Donors are not paid; they give their milk for altruistic reasons only, which eliminates incentives to tamper with milk or provide inaccurate health information.
Donor screening
- Detailed oral and written medical and lifestyle histories, based on blood donation screening
- Physician letters confirming health of donor mother and her child
- Blood tests to detect HIV 0, 1 & 2, HTLV 1 & 2, hepatitis B & C, and syphilis
- Many medications (prescription, over-the-counter, herbal, mega-dose vitamins) are cause for deferral
- We are in ongoing communication with donors about medications, illnesses, and other questions
Ineligibility
Some conditions that disqualify women from milk donation:
- Positive blood test result for HIV, HTLV, hepatitis B or C, or syphilis
- She or her sexual partner is at risk for HIV
- Tobacco products, illegal drugs, daily use of more than 1 alcohol serving (waiting period required for alcohol)
- She or her sexual partner has received a blood transfusion or blood products in the 6 months prior to milk collection
- She or her sexual partner has received an organ or tissue transplant in the last 12 months
- Potential exposure to Creutzfeldt-Jakob disease
Acceptable medications
Many medications are acceptable for use while others require a specific deferral period [the day(s) that the medication is taken, plus a waiting period following the last dose to allow the drug to clear from the body]. Medication standards are reviewed and updated regularly in accordance with new research and information. Among the medications generally acceptable are plain acetaminophen, ibuprofen (up to 1,200 mg/day), cough drops, nasal sprays, and topical medications.
Medication standards are reviewed and updated regularly in accordance with new research and information. Among the medications generally acceptable are plain acetaminophen, ibuprofen (up to 1,200 mg/day), cough drops, nasal sprays, and topical medications.
Laboratory Processing
Donor milk arrives frozen and is carefully logged and stored. Milk from 2-4 donors is thawed overnight in a refrigerator, pooled, carefully mixed to ensure an even distribution of milk components, and poured into bottles by trained technicians in our FDA-regulated laboratory.
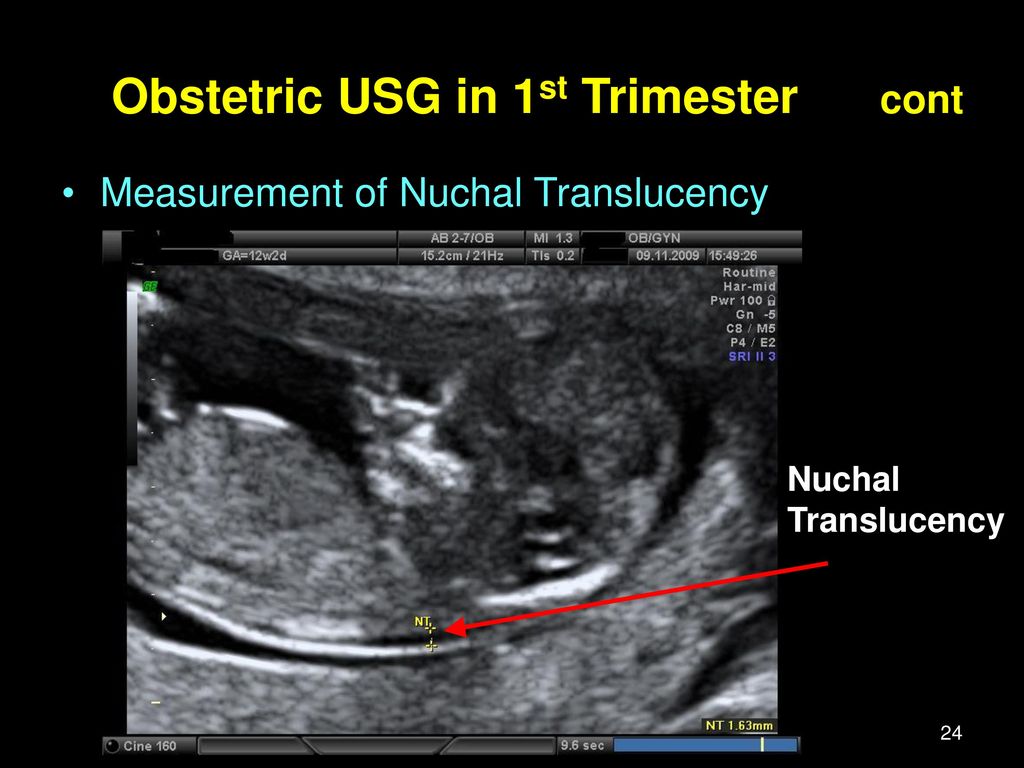
Pasteurization
Trays of milk bottles are heated in a shaking water bath using the Holder Method of pasteurization (62.5◦C for 30 minutes). Pasteurization eliminates bacteria while retaining the majority of the milk’s beneficial components. Cytomegalovirus (CMV) is among the pathogens destroyed during pasteurization. Pasteurized milk is quick-cooled, then frozen at -20◦C.
Testing
Pre-pasteurization: Every new donor’s milk undergoes a pre-pasteurization culture to screen for heat-resistant pathogens. Testing is repeated every 3 months.
Testing is repeated every 3 months.
Post-pasteurization: One bottle from each pasteurized tray is sent to an independent laboratory for microbiological cultures to verify zero growth of bacteria after the heating process. Any milk with a positive culture is discarded and not dispensed.
Storage and Shipping
Each bottle is labeled with an expiration date 1 year after the earliest pump date in the batch. Milk is shipped overnight in coolers with dry ice to arrive frozen by 10:30 am the following day.
These multiple overlapping screening and safety steps ensure that pasteurized donor human milk is safe for the most vulnerable infants. In over 40 years of modern milk banking there has never been a documented case of an infant being harmed by donor milk.
Mothers’ Milk Bank Northeast: Safe. Trusted. Lifesaving.
On the safety of donor breast milk and methods of ensuring it
Research results suggest that the risks to a child's health are significantly higher when feeding with formula than with donor milk, but it is important to observe the principles of safe exchange of donor milk. If you are getting milk from an unreliable source, then Holder pasteurization is an effective way to kill all known microbial agents in donor milk, as scientific research backs it up. (1.3, 11.14)
If you are getting milk from an unreliable source, then Holder pasteurization is an effective way to kill all known microbial agents in donor milk, as scientific research backs it up. (1.3, 11.14)
What if the donor mother suddenly falls ill?
Firstly, many diseases are not transmitted through milk, and for those that can be transmitted, the route of transmission of infection through it is far from the main one, that is, it is more likely to become infected in other ways, and not by drinking breast milk.
Secondly, along with the disease, antibodies begin to be produced that help protect the child's body from infection, which also enter the milk - this is the so-called passive immunity, a wonderful natural mechanism.
In newborns who do not receive breast milk, passive immunity, that is, antibodies obtained in utero, persists up to 3-6 months. With breast milk, the baby's body receives additional, very important portions of antibodies.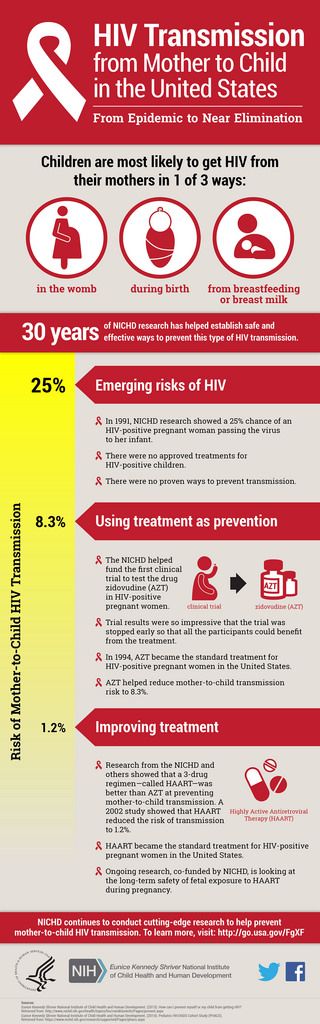 Thus, the milk itself protects the child from diseases.
Thus, the milk itself protects the child from diseases.
An additional mechanism for protecting children is the passage of breast milk through the stomach, which has an acidic environment. Breastfed babies are known to have lower acidity values (stomach contents are more acidic), while formula-fed babies are higher.
Thirdly, the course of an infectious disease includes the so-called latent, incubation period, during which the isolation of the infectious agent is already taking place, and it is theoretically possible for pathogens to enter the milk, but even if they are not neutralized by the components of the milk itself and the acidic environment of the stomach, there are simple and reliable ways to neutralize them
|
Viruses and bacteria |
Penetration into milk | Pathogen exposure | |||
| Cooling | Freezing | Holder pasteurization | Fast heating | ||
| HIV** (4. | YES through damaged nipples | Saved | Saved | destroys | destroys |
| Hepatitis A | DOES NOT PENETRATE | It is pointless to study exposure, since the virus does not pass into milk | |||
| Hepatitis B** (5) | Possibly through damaged nipples | Saved | Saved | destroys | Most likely retained |
| Hepatitis C** | Few, not proven through damaged nipples. The virus is inactivated in the stomach | Less resistant than hepatitis B virus | Less resistant than hepatitis B virus | destroys | May be retained |
| T-cell leukemia virus** (9) | YES | destroys | destroys | destroys | No data |
| Cytamegalovirus | YES (in the acute phase of the disease - in the analysis of IgM | destroys after 7 days in the refrigerator | destroys after 3 days of freezing | destroys | No data |
| NONE (if carrier - IgG only in analysis) | |||||
| Human papillomavirus (2) | DOES NOT PENETRATE | It is pointless to study exposure, since the virus does not pass into milk | |||
| Mycobacterium tuberculosis***** | Possibly | No growth or reproduction, pathogen persists | No growth or reproduction, pathogen persists | destroys | No data |
| Herpes simplex virus*** | Through affected nipples | No data | No data | destroys | No data |
| Staphylococcus**** (13) | YES | No data | Reduces | destroys | destroys |
| Streptococcus**** | Possibly | No data | Decreases | destroys | destroys |
| Escherichia coli**** | YES | No data | reduces | destroys | destroys |
| Candida fungi | Through affected nipples | Saved | May be retained | destroys | May be retained |
| Salmonella ****** | YES | Saved ****** | Saved ****** | May not completely kill Salmonella | Destroys most of |
*The table is based on reliable data from various sources available online
** Donation is contraindicated
*** Donation is contraindicated during an exacerbation
**** There is a study in which doctors fed raw milk containing staphylococcus and other bacteria to children and did not find any negative effects
* **** In addition, in Russia, doctors prohibit breastfeeding for mothers with the following diseases: eclampsia, severe bleeding during childbirth and in the postpartum period, an open form of tuberculosis, a state of severe decompensation in chronic diseases of the heart, lungs, kidneys, liver, hyperthyroidism, acute mental illness, especially dangerous infections (typhoid, cholera), herpetic eruptions on the nipple of the breast (before their aftercare), HIV infection, acute hepatitis A. In hepatitis B and C, feeding is carried out through special silicone pads. (Source) Thus, the probability that a dairy mother is sick with one of these diseases is practically zero.
In hepatitis B and C, feeding is carried out through special silicone pads. (Source) Thus, the probability that a dairy mother is sick with one of these diseases is practically zero.
****** Salmonellosis is a disease with striking characteristic symptoms. In addition, it is physically very difficult to express and store milk with symptoms of salmonellosis: fever, vomiting and diarrhea. Make sure the donor mom was healthy when she expressed her milk (the first of the 4 safety principles of informal milk exchange).
******* By analogy with animal milk, no information was found for breast milk.
If the nursing mother has started taking any medication, you can independently test the medication for compatibility with breastfeeding and make sure it is safe.
Thus, if a donor mother falls ill, the first thing to do is to understand whether something special needs to be done. In most cases, you don't need to do anything extra.
Note that, according to a study (10), yeast and mold content is higher in pasteurized, processed milk than in unpasteurized milk. Therefore, it is recommended to keep the expressed milk at room temperature or in the refrigerator for some time before freezing, allowing the microorganisms and active cells present in the milk to carry out a natural protective reaction.
Therefore, it is recommended to keep the expressed milk at room temperature or in the refrigerator for some time before freezing, allowing the microorganisms and active cells present in the milk to carry out a natural protective reaction.
Let's say you get milk from an unreliable source and want to be on the safe side.
The first step of protection is cooling or freezing milk. This prevents the reproduction of spore-forming bacteria, destroys some viruses, in particular, according to many sources, even cytomegalovirus. The second step is heating the donor milk: pasteurization or rapid heating. The most gentle way to disinfect milk while retaining many of its useful components is rapid heating (6,7,8)
So, firstly, not all pathogens are transmitted with breast milk. Secondly, if the principles of safe exchange of donor milk are observed, pathogenic microorganisms do not reach the baby receiving it, and thirdly, antibodies produced in response to an infection in a milk mother remain in the milk in one quantity or another and protect the baby.
1. Pasteurized Donor Human Milk Maintains Microbiological Purity for 4 Days at 4°C. Vickers AM1, Starks-Solis S2, Hill DR3, Newburg DS4.
2. Inactivation of high-risk human papillomaviruses by Holder pasteurization: implications for donor human milkbanking. Donalisio M, Cagno V, Vallino M, Moro GE, Arslanoglu S, Tonetto P, Bertino E, Lembo D.
3. Heating-induced bacteriological and biochemical modifications in human donor milk after holder pasteurisation. de Segura AG1, Escuder D, Montilla A, Bustos G, Pallás C, Fernández L, Corzo N, Rodríguez JM.
4. Effect of flash-heat treatment on antimicrobial activity of breastmilk. Chantry CJ1, Wiedeman J, Buehring G, Peerson JM, Hayfron K, K'Aluoch O, Lonnerdal B, Israel-Ballard K, Coutsoudis A, Abrams B.
5 Hepatitis B viral markers in banked human milk before and after Holder pasteurization . de Oliveira PR1, Yamamoto AY, de Souza CB, de Araújo NM, de Andrade Gomes S, Heck AR, de Castro Figueiredo JF, Mussi-Pinhata MM.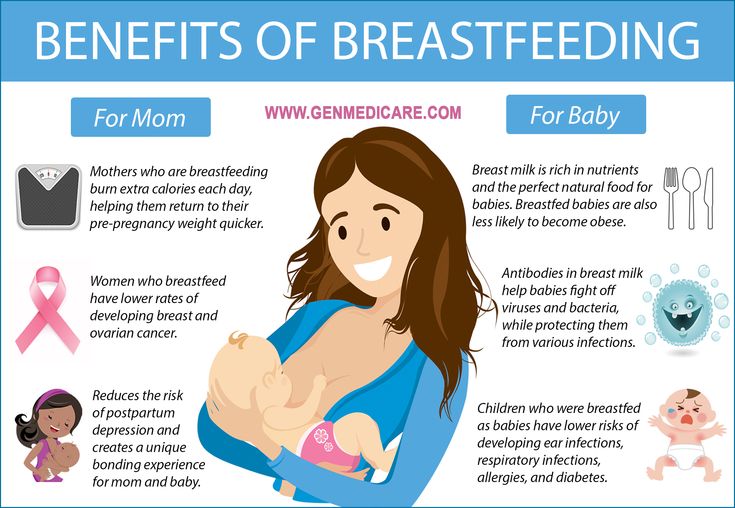
6 Effects of different CMV-heat-inactivation-methods on growth factors in human breast milk. Goelz R1, Hihn E, Hamprecht K, Dietz K, Jahn G, Poets C, Elmlinger M.
7 Antimicrobial and antiviral effect of high temperature short-time (HTST) pasteurization applied to human milk. Terpstra FG1, Rechtman DJ, Lee ML, Hoeij KV, Berg H, Van Engelenberg FA, Van't Wout AB.
8 Bacterial safety of flash-heated and unheated expressed breastmilk during storage. Israel-Ballard K1, Coutsoudis A, Chantry CJ, Sturm AW, Karim F, Sibeko L, Abrams B.
9 Long-term serological outcome of infants who received frozen-thawed milk from human T-lymphotropic virustype-I positive mothers. Ando Y1, Ekuni Y, Matsumoto Y, Nakano S, Saito K, Kakimoto K, Tanigawa T, Kawa M, Toyama T.
10 [Microbiological quality of human milk from a Brazilian milk bank]. [Article in Portuguese]
11 Donor milk: what's in it and what's not. Tully DB1, Jones F, Tully MR.
12 Pretoria pasteurisation: a potential method for the reduction of postnatal mother to child transmission of the human immunodeficiency virus. Jeffery BS1, Mercer KG.
Jeffery BS1, Mercer KG.
13 Microbiological study of breast milk with special reference to its storage in milk bank. Deodhar L1, Joshi S.
14 Microbial contaminants and antimicrobial properties of human milk. May JT1.
15 Transmission of Salmonella enterica serotype typhimurium DT104 to infants through mother's breast milk. Qutaishat SS1, Stemper ME, Spencer SK, Borchardt MA, Opitz JC, Monson TA, Anderson JL, Ellingson JL.
Polina Lykova, doctor, lactation consultant, member of the CMPF, mother of three children
Remote Milk - Blood5
Breast milk donation is practiced all over the world. It has been more or less organized in Russia since 2014, but so far this niche is still wild and more like a quest. Women donate their milk to other families for free, solve the problems of its safety themselves, and resist aggressive advertising of artificial mixtures. And every now and then they are forced to pull their community in social networks out of the ban for a photo of breastfeeding.
“I am looking for a breadwinner with accommodation for a year in the near Moscow region,” I read on eva.ru, “the payment is very generous.” “Gee,” follows the answer from ivolga, “you won’t find it, I give my head off for cutting off. Feed with donor milk. But where to get it? And why, if in the nearest store you can pick up a mixture for a child? And what is the market for donor breast milk anyway? How is it arranged? To understand this, Krov5 spoke with members of the Dairy Mom volunteer movement and pediatricians.
Complex matter
The advantages of breast milk over formula are not disputed even by manufacturers of artificial nutrition.
“No formula based on cow's or goat's milk, which usually contains only 40-50 components, will ever come close to the composition of a woman's breast milk,” explains Krov5 Anton Olenev, chief freelance specialist in obstetrics and gynecology at the Moscow Department of Health.
According to him, breast milk contains leukocytes, stem cells, more than 20 types of amino acids, more than a thousand proteins that strengthen the immune system and protect brain neurons. The intestinal microflora of a child is supported by more than 200 types of complex sugars. More than 40 enzymes speed up chemical reactions in the child's body. Milk contains hormones, antibodies, vitamins and minerals, long-chain fatty acids, 1400 microRNA species that regulate gene expression.
“Almost 30% of the cellular composition of milk consists of stem cells, whose importance to science has yet to be determined,” says Olga Lukoyanova, one of the leading Russian neonatologists, pediatrician, MD, leading researcher at the Laboratory of Healthy and Sick Child Nutrition at the Moscow National Medical Center (NMIC) children's health. – Babies who are breastfed are less likely to develop inflammatory diseases such as otitis media and infectious diseases of the gastrointestinal tract.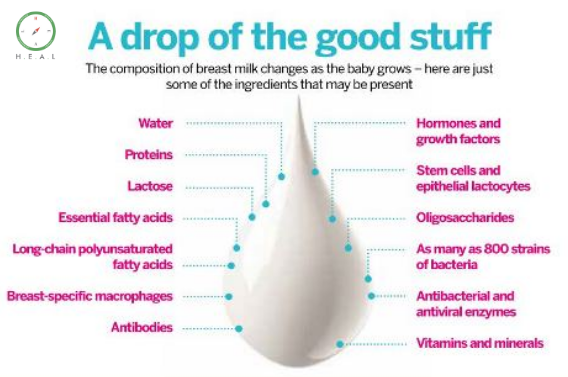
The advantage is obvious, but sometimes breastfeeding is not possible due to life circumstances. For example, because of the illness of the mother. Or a woman's unwillingness to endure the hardships of feeding. In such situations, the World Health Organization (WHO) recommends that donor breast milk be used first.
Experiences and Practices
Illustration: Future King Louis XIV in the arms of his nurse. Unknown AuthorIn Brazil, USA, Canada, Israel, Italy, Finland and some other countries there are breast milk banks, both public and private. They take milk from the population, process it and thus guarantee safety.
Brazil is the world leader in this field, with 210 such banks in the country. For comparison, the Association of Breast Milk Banks of North America has 13 organizations. The benefits of these institutions are enormous. In Brazil, in the five years since the creation of the first donor milk bank, infant mortality has fallen by 73%.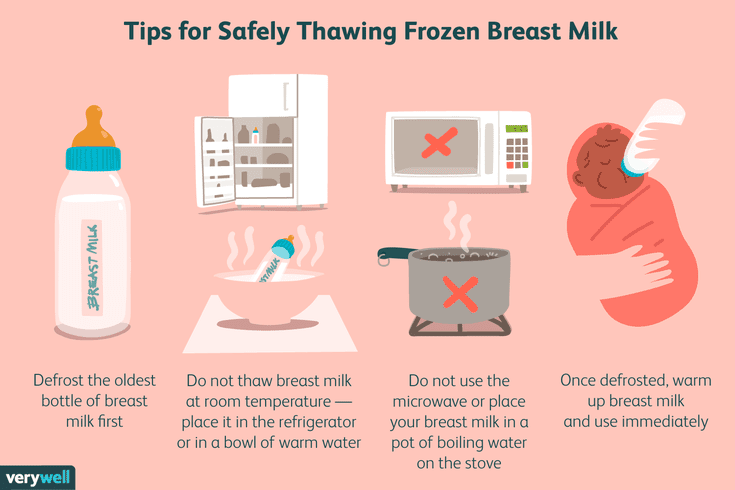 Since 2005, the country has celebrated Breast Milk Donor Day (May 19), and since 2010 a number of European countries have joined this initiative.
Since 2005, the country has celebrated Breast Milk Donor Day (May 19), and since 2010 a number of European countries have joined this initiative.
In Russia, the first donor milk bank appeared in Moscow in 2014, on the basis of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences. The next one is in Ufa, at the Republican Children's Clinical Hospital. And one more in 2019year at the Regional Perinatal Center in Chelyabinsk.
Donors in them are carefully examined, milk is checked and pasteurized on special equipment to prevent bacteria and viruses. Only all these institutions are of a stationary type, they serve only their patients, so their throughput is low. For clarity: in the first year of operation, only 50 children received donor milk from the Moscow bank.
And what about the rest who need it?
Mother will support
Photo: Andrey Karelin. Mother, child and nurse
Mother, child and nurse Those who did not immediately go to the store for formula, begin their participation in the quest, that is, the search for breast milk on the Internet. In many countries there are informal communities for the exchange of donor milk. True, official structures do not recommend contacting them. The same American Food and Drug Administration (FDA), the Association of Breast Milk Banks in North America and a similar association in Europe oppose informal exchange. But this is just a recommendation. Moreover, from organizations interested in receiving breast milk in their banks - their financing is tied to this. Public donor organizations explain such statements as competition for breast milk and insist that donation should be available to everyone.
In Russia, in addition to the three mentioned banks, breast milk donation has been promoted since 2013 by the Dairy Mom volunteer movement. Key principle: milk should only be free.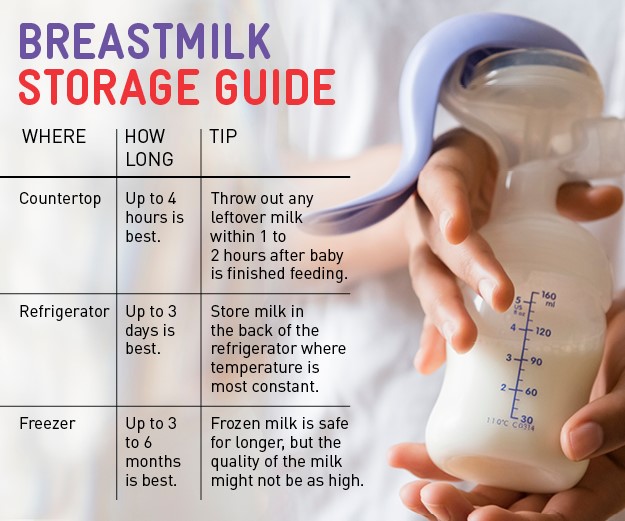 Since the lack of benefits excludes fakes, fraud and the risk of exploiting the body of a nursing woman.
Since the lack of benefits excludes fakes, fraud and the risk of exploiting the body of a nursing woman.
The history of the creation of "Dairy Mom" began with the fact that the psychologist Olga Rodicheva was looking for a breast milk donor for her third child. She posted a request on the Internet, left her contacts, and she received a wave of messages from other women with words of both support and criticism. “You are so brave, and I am afraid to openly admit that I do not have enough milk,” wrote one mother. “Ugh, how disgusting, you are not a mother!” another was outraged.
- When there is one letter in the mail - from a woman from Tver who wants to give milk, and another - from a mother who writes: "I live in Tver, but I don’t know how to find milk here", somehow not humanly there was no way to connect them,” Olga recalls. - At first, my like-minded people and I did it manually, simply sending each other the addresses of mothers. Then we had a community in LiveJournal, where we posted their contacts. But they stuffed bumps and realized that it was impossible to openly publish contacts. So we got a closed database, and then we moved to a separate site.
Then we had a community in LiveJournal, where we posted their contacts. But they stuffed bumps and realized that it was impossible to openly publish contacts. So we got a closed database, and then we moved to a separate site.
Dairy Mom unites Russian-speaking residents from 435 settlements in 25 countries, including the states of Asia, Africa, and South America.
To imagine the scale, suffice it to say that thanks to the activities of the “Dairy Mom”, about 4.5 tons of donor breast milk is annually transferred to needy babies.
About 30 volunteers do all the maintenance of the processes between the buttons on the site "Give milk" and "Find milk". They also maintain pages on social networks, translate scientific articles and lectures into Russian, publish educational materials on the topic of milk donation, and organize educational webinars.
To receive or donate milk, a person fills out a form on the site and leaves his contacts. From the chatbot, the answer comes instantly, from the moderators - within a day. This speed of response is explained by the fact that, as a rule, they are mothers with small children, and they also live in different time zones.
From the chatbot, the answer comes instantly, from the moderators - within a day. This speed of response is explained by the fact that, as a rule, they are mothers with small children, and they also live in different time zones.
“This is professional volunteering in a way,” says Olga. – There are those who help us pay for the domain and hosting, sometimes we buy articles in scientific journals, pay for webinars. However, we do not have any centralized support, because we are not registered as an NPO, we do not have an accountant, a current account, and stable income. In principle, this is not necessary. Everything works like that. But we will be very happy to help you to upgrade our old site.
Special circumstances
Photo: 1900. A woman is feeding a child Milk donors are, without a doubt, altruists: they are driven by the desire to help their neighbor. After all, pumping, storing and transferring milk is work, time that they spend free of charge.
“There was a desire to help,” Tatyana Makarova briefly answered Krov5's question about how she came to milk donation. And this answer is typical for the majority. “I found out about this practice by accident, my friends and relatives were shocked, no one knew that this happens,” says the donor under the nickname tanyatabachnik. “I helped a mother of twins who didn’t have enough milk for two.”
Often people come up with the idea of becoming a milk donor because of hyperlactation: there is so much milk that even when expressed, it no longer fits in the freezer, and it is a pity to throw it away.
“I helped several families,” writes Irina le-Deygen. “My first extra supply of milk was taken by my family for my adopted daughter.”
Alisa Gavrilova was a donor for half a year, and it was an unforgettable experience: “The mother I supported is a hero. Every week she went for milk to three families from different cities. Her baby was premature and using breast milk instead of formula helped her deal with her guilt."
Her baby was premature and using breast milk instead of formula helped her deal with her guilt."
Mom under the name Olga Loukkonen came to the donation paradoxically: after an unsuccessful attempt to become a recipient. Living in Spain, she wrote a request to Dairy Mom. The donor was found 75 km from her house, but the three-month-old daughter refused to accept someone else's milk, and the woman tried to induce lactation in herself. The attempt turned out to be so successful that after two weeks she clicked on the “Gift Milk” button on the Dairy Mom website - and those who wanted to receive it were immediately found.
“In my practice, there was a woman who had a large supply of milk, but the baby did not survive, and it was important for her to give this milk,” says Tatyana Lebedeva, a breastfeeding specialist from the Rostov region, a teacher at the Association of Breastfeeding Consultants. “We also had a woman who died in childbirth, and seven volunteer moms collected milk that another volunteer took to the grandmother for this woman’s child. We later induced lactation on this grandmother - yes, it is possible to induce lactation in nulliparous women. In general, I hope that milk donation will become the norm in our country.
We later induced lactation on this grandmother - yes, it is possible to induce lactation in nulliparous women. In general, I hope that milk donation will become the norm in our country.
By the way, about the norm: for eight years of work, the volunteers of the "Dairy Mom" noted an unusual phenomenon for which there is no explanation yet.
- Usually the demand for milk exceeds the supply, Olga Rodicheva notes. - In Moscow - significantly. But there is an amazing city of Chelyabinsk, it is the only one on the planet where the situation is reversed: there are more mothers who are ready to share milk than those who would like to take it.
The residents of Chelyabinsk themselves - local doctors and psychologists, with whom Krov5 talked - find it difficult to explain this phenomenon.
“I would even say that we have almost no milk donation,” says Ksenia Vlasova, a pediatrician at the Healthy Child medical center in Chelyabinsk. - It is more developed in Moscow, St. Petersburg. In my practice, I have not come across recipients of donor milk, but I see intolerance to mixtures in about half of the children on artificial nutrition.
- It is more developed in Moscow, St. Petersburg. In my practice, I have not come across recipients of donor milk, but I see intolerance to mixtures in about half of the children on artificial nutrition.
Milk Way
Illustration: Leonid Pasternak. To relatives. 1891Still, for breast donation to become the norm, several key issues need to be addressed. The main one is the safety of donor milk.
“We don't exchange other bodily fluids with strangers at the subway, for example, blood,” says pediatrician Olga Lukoyanova from the National Medical Research Center for Children's Health. – I am not against donor exchange, but the process should be controlled by specialists. Sharing milk over the Internet is dangerous because it can contain human T-cell leukemia, cytomegalovirus, HIV and hepatitis A, B, C, streptococci, staphylococci, Pseudomonas aeruginosa…
If we turn to the past, beautiful women of 20–35 years old with a cheerful character and “developed mental abilities” were traditionally hired as nurses, since it was believed that both beauty and intelligence were transmitted with milk.
Nowadays, there are no less myths about the superpowers of breast milk, but more in the genre of horror stories. There is, for example, a prejudice that all viruses and pathogenic bacteria that a nursing woman has are transmitted with milk.
– If you wash your hands, use clean dishes and follow simple hygiene rules according to the protocol of the Academy of Breastfeeding Medicine, then little is passed through breast milk, says Tatyana Lebedeva. - And from the dangerous that can be transmitted, pasteurization helps.
Ideally, breast milk should be pasteurized on specialized equipment under the supervision of professionals. And in this sense, the ideal solution to the problem, according to Olga Rodicheva, would be the development of existing donor milk banks in the country. For example, on their basis it would be possible to provide the population with paid services of pasteurization and health screening of donors. As a result, host families will be confident in the biological safety of the product, and banks will receive money for development.
As a result, host families will be confident in the biological safety of the product, and banks will receive money for development.
- It would be a real cooperation, - Olga Rodicheva is sure. - When in one place the donor could be screened, and the host family could order pasteurization. And most importantly, such cooperation with informal networks and banks themselves will attract more donors. But such decisions can only be made at a high level - in the Ministry of Health. So far there is little hope. We tried to make friends with milk banks, but they don't want to be friends with us. And I do not believe that the situation will change in the near future.
Another myth interferes with the development of milk donation: that milk from a non-relative is not suitable for a child.
- Pasteurized donor milk may not be suitable only in case of allergies to specific products, - explains Tatyana Lebedeva. “There are no complications from it.
“There are no complications from it.
- In the entire history of breast exchange in the world, we do not know of a single case when a child fell ill or died from donor milk, but we constantly hear about the dangers, - adds Olga Rodicheva. – Breast milk does not belong to the biohazard category of liquids (representing a biological hazard. – Blood5). And I consider unacceptable the attitude of some officials towards informal donors as obviously stupid, unthinking women. It seems to them that since women themselves are responsible for their children, run an informal milk exchange, negotiate among themselves without medical officials, then everyone will die.
The situation worsens as soon as money is involved. For decades, formula milk manufacturers and breastfeeding advocates have clashed over the ethics of formula nutrition advertising. In 1981, the manufacturers themselves supported the adoption of the International Code of Marketing of Infant Formula at the World Health Assembly of WHO, which recommends the complete elimination of formula advertising. Since then, 65 countries have adopted laws based on this document. This code had little effect on Russia.
Since then, 65 countries have adopted laws based on this document. This code had little effect on Russia.
The Milk Mom movement is also working on this issue. It has taken on the mission to become the representative of IBFAN in Russia, the International Infant Food Surveillance Network for Infants and Young Children, which fights primarily against the aggressive marketing of milk formulas and advocates for informing the population about infant nutrition.
- We consider it our merit that on the websites of some pediatricians there are now no advertisements for formula manufacturers, - says Olga Rodicheva. – Of course, many people do not like our work. This is a loss of sponsors, money, but we are heard by talented doctors, scientists, officials who are trying to tighten laws regarding the advertising of mixtures.
In addition, the Dairy Mom community has launched a project where they publish photos of breastfeeding mothers to show that breastfeeding a child in a public place is normal.
 12)
12)