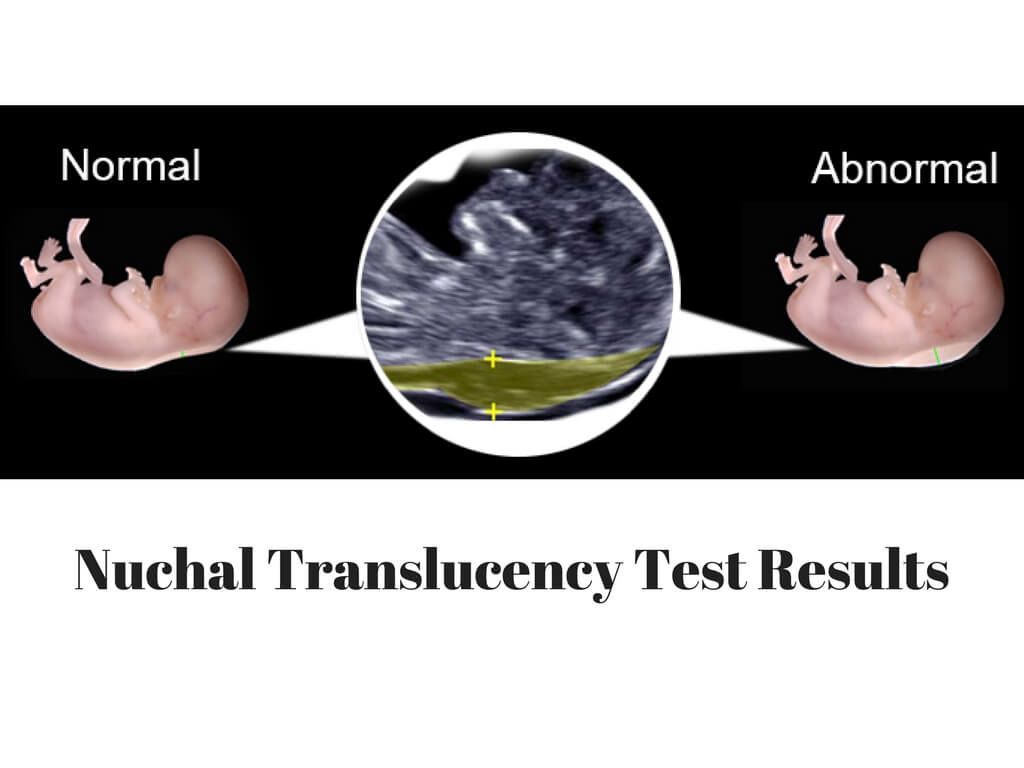
Nuchal translucency meaning
Nuchal translucency test
Medical Tests
Definition
The nuchal translucency test measures the nuchal fold thickness. This is an area of tissue at the back of an unborn baby's neck. Measuring this thickness helps assess the risk for Down syndrome and other genetic problems in the baby.
Alternative Names
Nuchal translucency screening; NT; Nuchal fold test; Nuchal fold scan; Prenatal genetic screening; Down syndrome - nuchal translucency
How the Test is Performed
Your health care provider uses abdominal ultrasound (not vaginal) to measure the nuchal fold. All unborn babies have some fluid at the back of their neck. In a baby with Down syndrome or other genetic disorders, there is more fluid than normal. This makes the space look thicker.
A blood test of the mother is also done. Together, these two tests will tell if the baby could have Down syndrome or another genetic disorder.
How to Prepare for the Test
Having a full bladder will give the best ultrasound picture. You may be asked to drink 2 to 3 glasses of liquid an hour before the test. DO NOT urinate before your ultrasound.
How the Test will Feel
You may have some discomfort from pressure on your bladder during the ultrasound. The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
Why the Test is Performed
Your provider may advise this test to screen your baby for Down syndrome. Many pregnant women decide to have this test.
Nuchal translucency is usually done between the 11th and 14th week of pregnancy. It can be done earlier in pregnancy than amniocentesis. This is another test that checks for birth defects.
Normal Results
A normal amount of fluid in the back of the neck during ultrasound means it is very unlikely your baby has Down syndrome or another genetic disorder.
Nuchal translucency measurement increases with gestational age. This is the period between conception and birth. The higher the measurement compared to babies the same gestational age, the higher the risk is for certain genetic disorders.
The measurements below are considered low risk for genetic disorders:
- At 11 weeks -- up to 2 mm
- At 13 weeks, 6 days -- up to 2.8 mm
What Abnormal Results Mean
More fluid than normal in the back of the neck means there is a higher risk for Down syndrome, trisomy 18, trisomy 13, Turner syndrome, or congenital heart disease. But it does not tell for certain that the baby has Down syndrome or another genetic disorder.
If the result is abnormal, other tests can be done. Most of the time, the other test done is amniocentesis.
Risks
There are no known risks from ultrasound.
References
Chaveeva P, Agathokleous M, Nicolaides KH. Fetal aneuploidies. In: Coady AM, Bower S, eds. Twining's Textbook of Fetal Abnormalities. 3rd ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2015:chap 2.
Walsh JM, D'Alton ME. Nuchal translucency. In: Copel JA, D'Alton ME, Feltovich H, et al, eds. Obstetric Imaging: Fetal Diagnosis and Care. 2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
Review Date: 04/19/2018
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.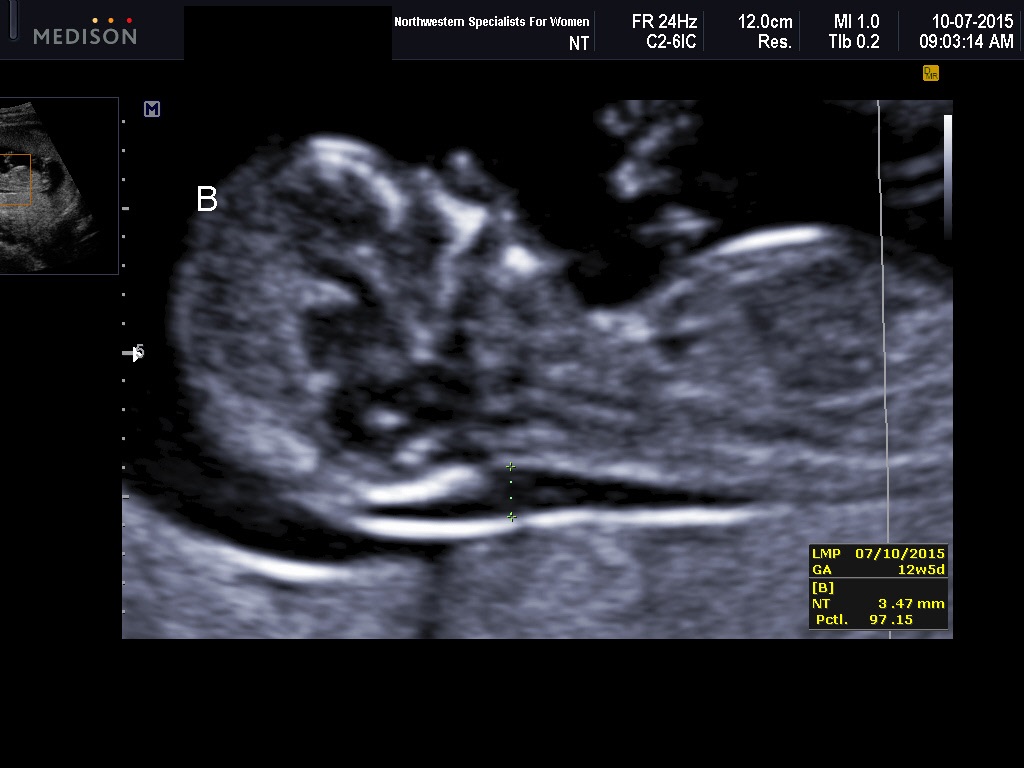 D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.
NT Scan During Pregnancy: What Your Results Mean
Written by Cheryl Whitten
In this Article
- What Is an NT Scan for Down Syndrome?
- What Does an NT Scan Check For?
- What Happens at a Nuchal Translucency Scan?
- What Are the Risks of an NT Scan?
- Is an NT Scan Necessary?
- What Do Your NT Scan Results Mean?
- What Happens if an NT Scan Is Abnormal?
- The Takeaway
If you’re pregnant, your doctor might have mentioned an NT scan or first-trimester screening. An NT scan is a simple test that shows your baby’s risk for some genetic conditions.
What Is an NT Scan for Down Syndrome?
An NT scan, or nuchal translucency scan, is a non-invasive ultrasound screening for Down syndrome and other genetic conditions during pregnancy. It’s usually done between weeks 11 and 14 of pregnancy.
Some people also have blood tests done at the same time that look for certain hormones and proteins, including:
- Free beta-human chorionic gonadotropin, or b-hCG
- Pregnancy-associated plasma protein-A, or PAPP-A
- Alpha-fetoprotein, or AFP
All pregnant people have these hormones and proteins, but the levels can be higher or lower than average when the baby has Down syndrome or other disorders. These screenings together are called the combined or integrated first-trimester screening.
What Does an NT Scan Check For?
All unborn babies have a skin fold, called a nuchal fold, at the back of the neck that holds fluid. Babies with certain genetic conditions have more fluid than normal, and the nuchal fold is thicker.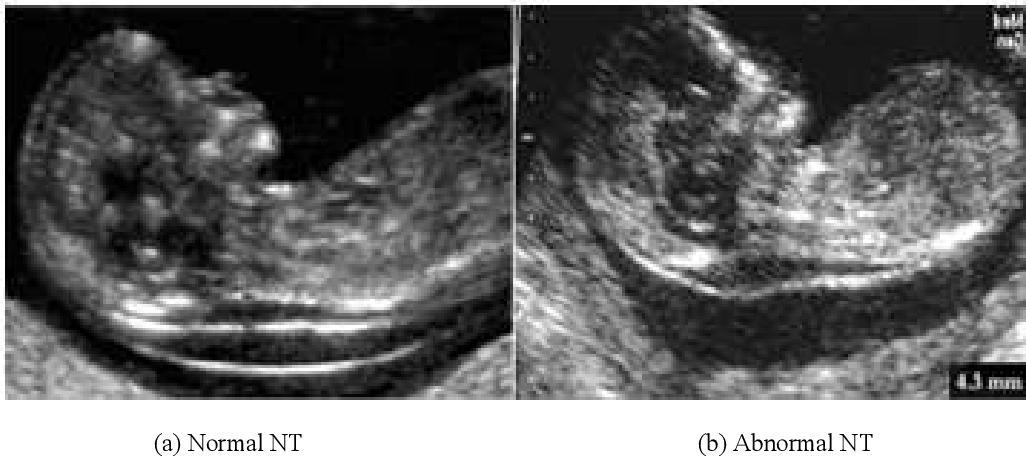
An NT scan measures this fold to check for the risk of genetic conditions like:
Down syndrome. Down syndrome, or trisomy 21, is a genetic disorder where babies have an extra 21st chromosome. Chromosomes are packages of genes that tell the body how to grow. An extra chromosome changes how the brain and body develop and can cause intellectual and physical disability, birth defects, and health problems.
Trisomy 13 and 18.Trisomy 13 and trisomy 18 happen when babies have an extra copy of either chromosome 13 or chromosome 18, respectively. These genetic disorders cause serious birth defects and intellectual disability, often leading to early death.
Turner syndrome. A baby with Turner syndrome is missing all of or part of the X chromosome. This only affects babies with X chromosomes and can cause growth problems and heart and ovary defects at birth.
Congenital heart disease.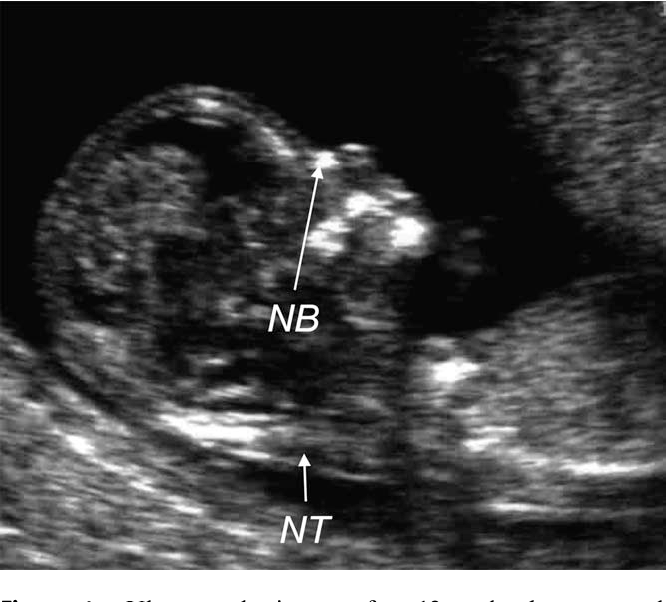 Babies with congenital heart disease are born with heart defects that change how blood flows through the heart. Some defects are life-threatening, and some don’t cause any problems.
Babies with congenital heart disease are born with heart defects that change how blood flows through the heart. Some defects are life-threatening, and some don’t cause any problems.
An NT scan doesn’t diagnose or confirm any of these disorders, though. Instead, it tells you whether your baby has a higher risk of having one of these conditions.
Since an NT scan is an ultrasound, your doctor might also check for other things, including:
- How your baby is growing
- How many babies you’re carrying
- Whether multiple babies share a placenta
- Exactly how far along you are in your pregnancy
What Happens at a Nuchal Translucency Scan?
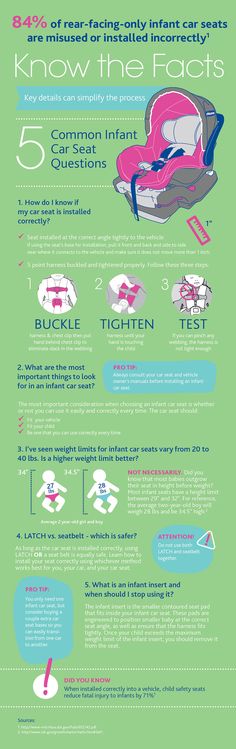
An NT scan is a routine ultrasound. You need to have a full bladder, so the ultrasound technician will ask you to drink 2 to 3 glasses of water an hour before the scan. You can’t urinate before the test, so you might feel full and uncomfortable.
During the test, you'll lay down on a table and the technician will put gel on your lower belly. They'll move a wand across your abdomen and take some pictures. Once they have the pictures, your scan will be done, and you can go back to your regular activities. A radiologist will read the scans and send the results to your doctor.
They'll move a wand across your abdomen and take some pictures. Once they have the pictures, your scan will be done, and you can go back to your regular activities. A radiologist will read the scans and send the results to your doctor.
What Are the Risks of an NT Scan?
There are no known risks for an NT scan. Ultrasounds are safe and non-invasive, and you can’t feel the ultrasound waves. You might feel some pressure as the technician moves the wand around your belly. This is normal and helps get the best view of your baby.
Is an NT Scan Necessary?
NT scans are optional. You have the option of getting this test early in your pregnancy, which will give you results early on. Early results can help you plan for the possibility of caring for a child with disabilities.
You can also decline this test. If you think it would cause too much stress, or if it won’t change how you manage your pregnancy or plan for your child, you might decide against it.
What Do Your NT Scan Results Mean?
The skin fold grows as unborn babies grow, so the test measures the thickness of the skin fold and compares it to babies of the same age in the womb. If the measurement is higher than the average measurement, then the risk for some genetic conditions is higher.
If the measurement is higher than the average measurement, then the risk for some genetic conditions is higher.
What is the NT scan normal range? At 11 weeks, the skin fold measures up to 2 mm. At 13 weeks and 6 days, it can be up to 2.8 mm. If your baby’s measurements are within this range, they have a low chance of having Down syndrome or other genetic disorders.
What is an abnormal NT scan measurement? An abnormal measurement is when the skin fold measure is larger than the normal range of up to 2 mm at 11 weeks or 2.8 mm at 13 weeks 6 days.
Your doctor will consider the measurements along with your age and your blood tests. While testing only shows the chances of having a condition, an NT scan with bloodwork can correctly predict genetic conditions in 85% of cases. About 5% of test results are false positives, which means they incorrectly suggest a higher chance.
What Happens if an NT Scan Is Abnormal?
If your NT scan has abnormal measurements, your doctor might suggest more testing.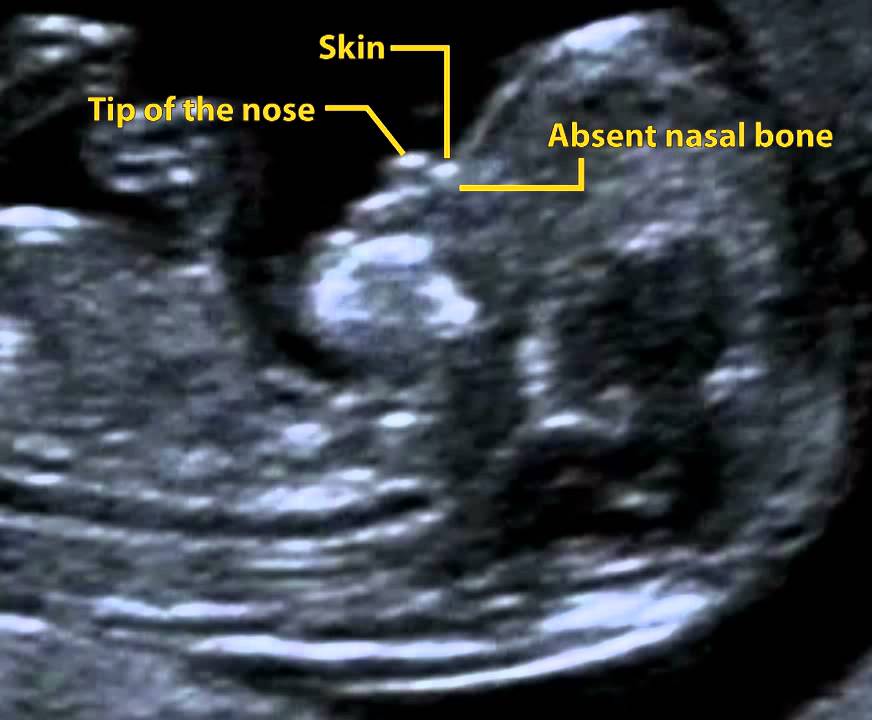 These tests can include:
These tests can include:
- Chorionic villus sampling, where they test a tiny piece of the placenta
- Amniocentesis, where they test a small amount of amniotic fluid from your uterus
- Prenatal cell-free DNA (cfDNA) screening, where they take some of your blood and look at your baby’s DNA
These tests do have a risk of causing pregnancy loss, so your doctor will go over the risks and benefits for your situation. If you decide to have the test, your doctor will discuss your results with you and help you understand what they mean.
The Takeaway
An NT scan is a safe and routine — but optional — ultrasound scan that can help predict the chances of your baby having Down syndrome. It’s sometimes done along with bloodwork in your first trimester.
Ultrasound diagnosis of Down syndrome and other chromosomal abnormalities
- Fetal ultrasound is the main method for diagnosing the likelihood of Down syndrome
- Basic ultrasound markers of Down syndrome
- Signs of Down syndrome with ultrasound in the second trimester of pregnancy
- How else can you determine the risk of having a baby with Down syndrome
Down's syndrome is a relatively common congenital pathology caused by the presence of an extra chromosome in 21 pairs.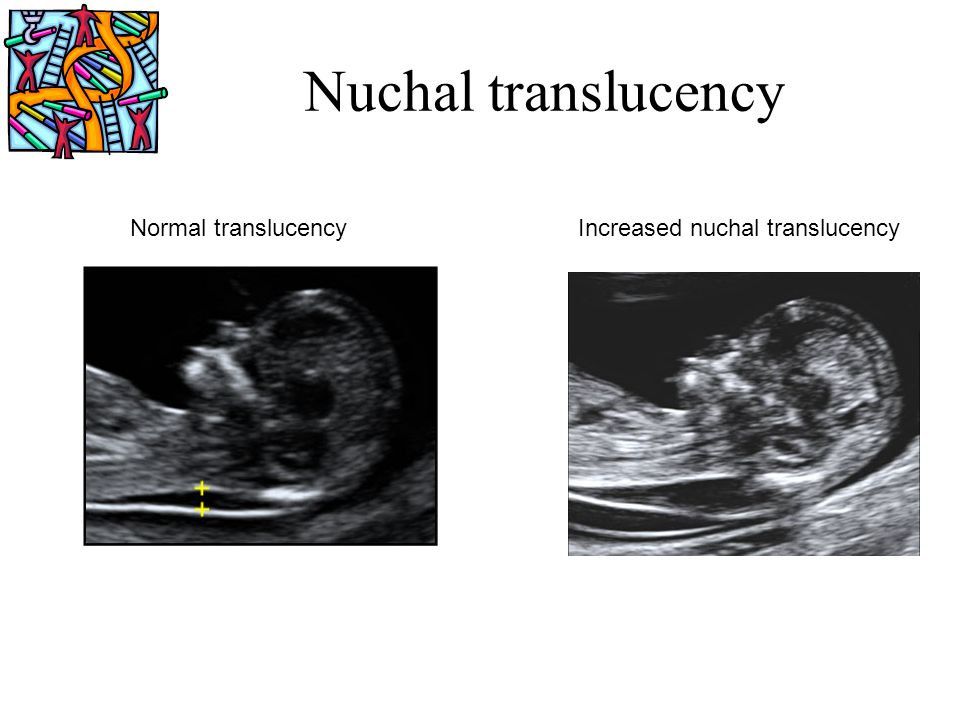 Down syndrome is also called trisomy on chromosome 21. Of all the chromosomal abnormalities, this pathology is the most well-known for a wide range of people.
Down syndrome is also called trisomy on chromosome 21. Of all the chromosomal abnormalities, this pathology is the most well-known for a wide range of people.
Down's syndrome is associated with many significant malformations. Such as, for example, congenital heart defects, duodenal atresia (a condition where part of the small intestine does not develop), an increased risk of developing acute leukemia (leukemia). About 50% of children with this condition are born with heart defects, the most common of which is a ventricular septal defect. Another disease that is often observed in such children is Hirschsprung's disease - an aganglionic area of the large intestine, leading to the development of intestinal obstruction.
Screening tests during pregnancy are used to assess the risk of having a baby with Down syndrome. These tests are painless and non-invasive (do not cause damage to the tissues of the pregnant woman and fetus), but do not accurately judge the presence or absence of congenital pathology.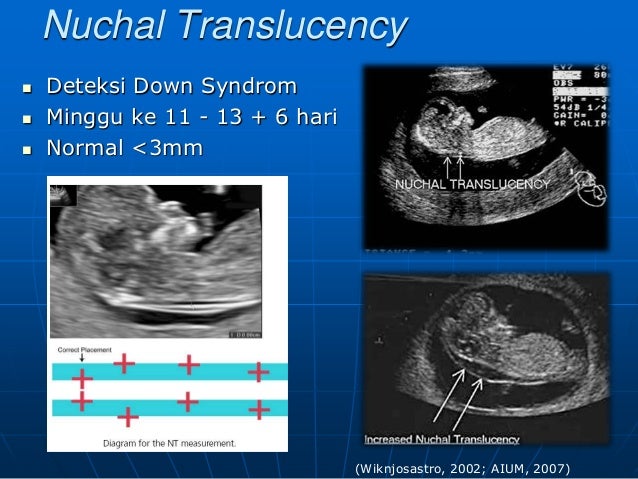 Nevertheless, their widespread use makes it possible to suspect risks and recommend invasive procedures. Invasive diagnostic methods include interventions performed under ultrasound guidance - amniocentesis, chordocentesis and chorionic villus sampling.
Nevertheless, their widespread use makes it possible to suspect risks and recommend invasive procedures. Invasive diagnostic methods include interventions performed under ultrasound guidance - amniocentesis, chordocentesis and chorionic villus sampling.
Fetal ultrasound is the main way to diagnose the likelihood of Down syndrome
Fetal ultrasound to detect developmental abnormalities is called ultrasound screening. Most often, ultrasound screening is combined with biochemical blood tests of a pregnant woman, and such a study is called combined screening. Depending on the choice of criteria, the probability of detecting Down syndrome in the second trimester is 60-91%. The use of color Doppler technology for ultrasound screening makes it possible to detect defects in the fetal heart and increases the accuracy of diagnosis.
Major ultrasound markers of Down syndrome
Ultrasound markers are ultrasound measurements that are most likely to be associated with a high chance of having Down syndrome in the fetus.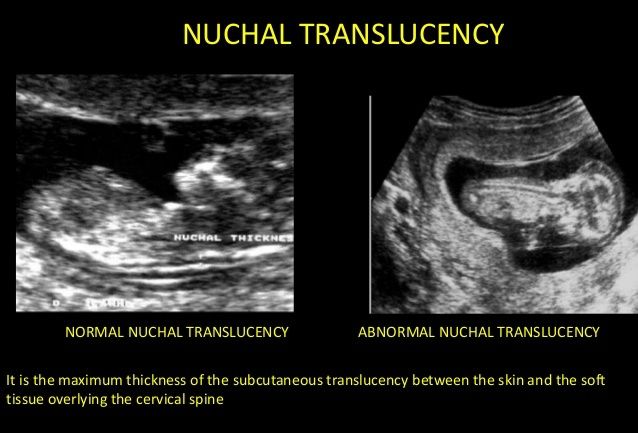 None of these markers is specific, that is, inherent only in this pathology. The following indicators are taken into account: the thickness of the collar space (75% of sensitivity), the absence of the nasal bone (58%), heart defects, short femurs and humeri, hyperechoic intestines, choroid plexus cysts, echogenic foci in the heart, signs of duodenal atresia . Of course, none of these markers is an absolute sign of a chromosomal abnormality.
None of these markers is specific, that is, inherent only in this pathology. The following indicators are taken into account: the thickness of the collar space (75% of sensitivity), the absence of the nasal bone (58%), heart defects, short femurs and humeri, hyperechoic intestines, choroid plexus cysts, echogenic foci in the heart, signs of duodenal atresia . Of course, none of these markers is an absolute sign of a chromosomal abnormality.
Measuring the thickness of the nuchal space
The nuchal space (cervical fold) is the area between the folds of fetal tissues, which is transparent on ultrasound, located below the occiput in the area of neck formation. In children with chromosomal abnormalities, such as Down's syndrome or trisomy 18, fluid accumulates in this place. The measurement of this space is carried out from 11 to 14 weeks during the ultrasound of pregnancy in the first trimester. Measurements obtained at this time are the most significant for predicting the individual risk of developing fetal chromosomal abnormalities.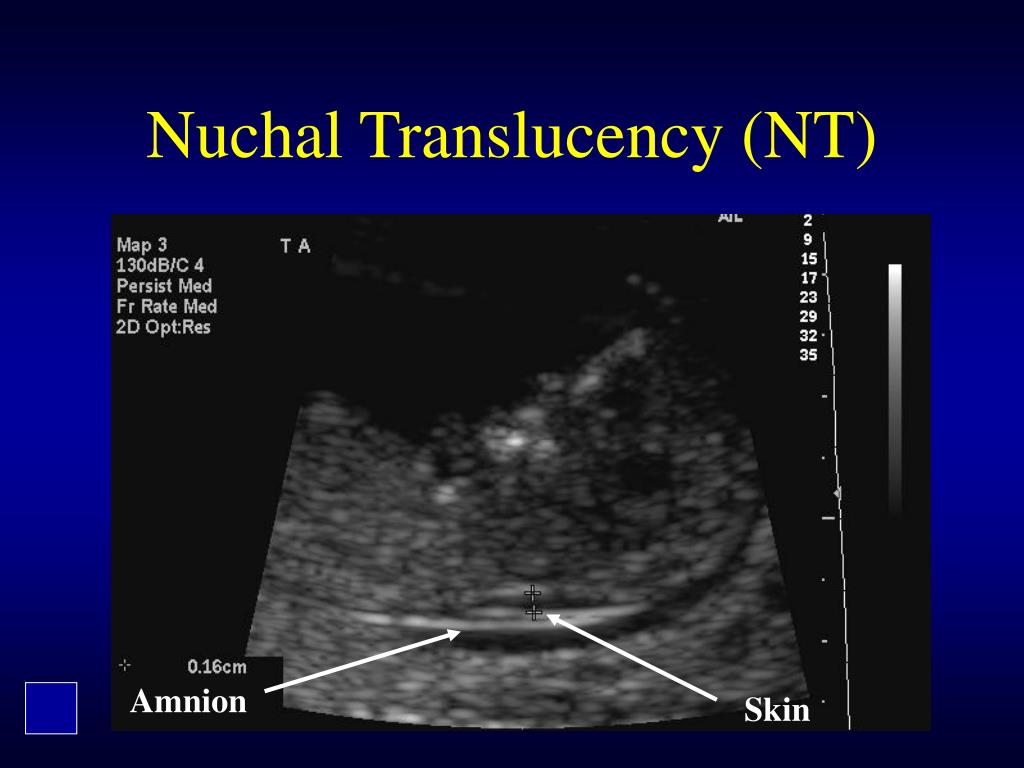 The thickness of the collar space more than 3 mm is taken as an indicator of an increased likelihood of genetic defects in the fetus. The increase in the collar space does not mean that the fetus necessarily has Down syndrome, but if we take into account the gestational age of the fetus on which measurements were taken, the age of the mother and biochemical screening indicators, the probability of a correct diagnosis becomes higher than 80%. Although nuchal thickness screening is one of the most important tests for detecting chromosomal abnormalities, there are biases. The error arises due to violations of the measurement technique. This applies not only to measurements of the collar space, but also to the nasal bone. There are errors due to the human factor. The correct measurement technique and the experience of the ultrasound specialist are very important.
The thickness of the collar space more than 3 mm is taken as an indicator of an increased likelihood of genetic defects in the fetus. The increase in the collar space does not mean that the fetus necessarily has Down syndrome, but if we take into account the gestational age of the fetus on which measurements were taken, the age of the mother and biochemical screening indicators, the probability of a correct diagnosis becomes higher than 80%. Although nuchal thickness screening is one of the most important tests for detecting chromosomal abnormalities, there are biases. The error arises due to violations of the measurement technique. This applies not only to measurements of the collar space, but also to the nasal bone. There are errors due to the human factor. The correct measurement technique and the experience of the ultrasound specialist are very important.
Fetal Pelvis and Brain Measurements
In fetuses with trisomy 21, ultrasonography may show cerebellar hypoplasia (reduction in size) and a reduction in the frontal lobe.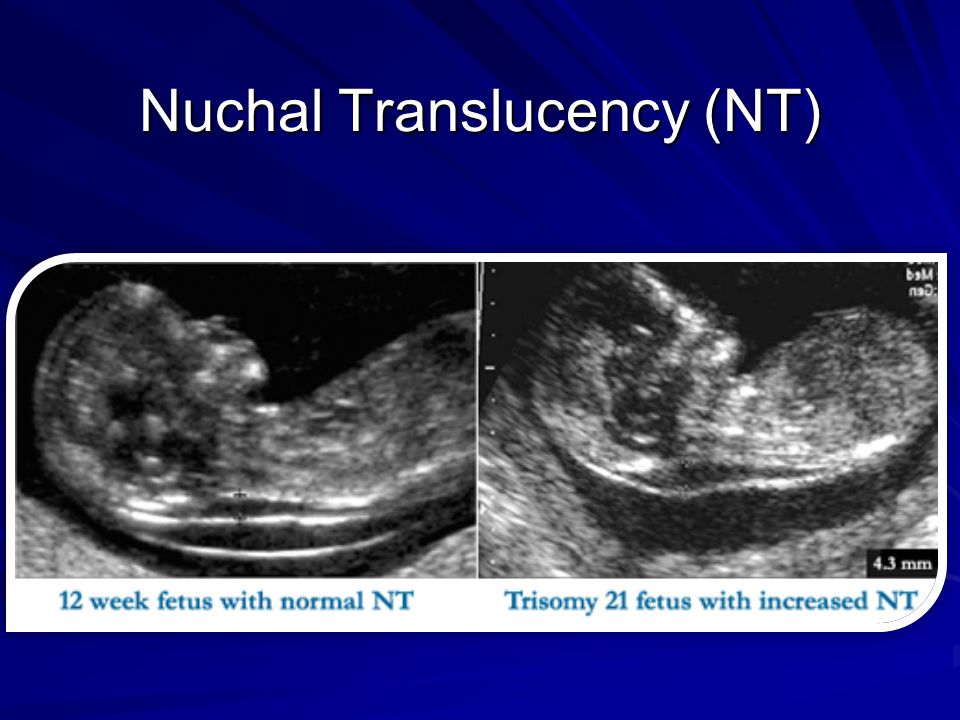 These facts are used to assess the likelihood of Down syndrome. The combination of a shortened transverse size of the cerebellum and a decrease in the fronto-thalamic distance is of greater importance for the diagnosis of this chromosomal anomaly than measuring each distance of intracerebral structures separately.
These facts are used to assess the likelihood of Down syndrome. The combination of a shortened transverse size of the cerebellum and a decrease in the fronto-thalamic distance is of greater importance for the diagnosis of this chromosomal anomaly than measuring each distance of intracerebral structures separately.
In a fetus with Down's syndrome during ultrasound, the length of the iliac bones is clearly reduced and the angle between these bones is increased. This can be measured most clearly at the level of the middle of the sacrum in cross section.
Signs of Down's syndrome during ultrasound in the second trimester of pregnancy
Ultrasound of the fetus in the second trimester of pregnancy can reveal such abnormalities as a violation of the formation of bones of the skeleton, expansion of the collar space by more than 5 mm, the presence of heart defects, expansion of the renal pelvis (pyeloectasia ), echogenicity of the intestine, cysts of the choroid plexus of the brain.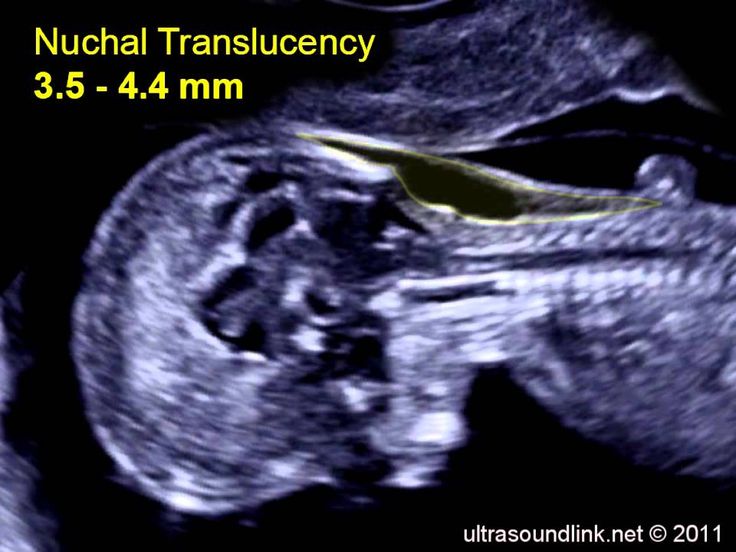 Moreover, only heart defects, disorders of skeletal formation and expansion of the collar space are independent risk factors.
Moreover, only heart defects, disorders of skeletal formation and expansion of the collar space are independent risk factors.
The use of only one of the measurements in assessing the probability of the presence of chromosomal abnormalities of the fetus, for example, determining the thickness of the collar space or measuring the iliac angle, is less accurate than taking into account the totality of measurements.
Another way to determine the risk of having a baby with Down syndrome
In addition to ultrasound signs, biochemical screening in the first and second trimester is used to determine the degree of risk. In this case, the blood of a pregnant woman is examined. The best results are obtained by combining ultrasonic and biochemical signs. If the combination of factors is threatening, a decision may be made to conduct invasive methods for diagnosing Down syndrome and other chromosomal abnormalities. Invasive techniques consist in obtaining particles of the skin or blood of the fetus, followed by genetic analysis. These methods are 100% reliable. At the same time, even complete well-being during screening in the first and second trimester using ultrasound and biochemical markers cannot guarantee the absence of chromosomal abnormalities in the fetus. The choice and determination of the sufficiency of diagnostic methods is carried out taking into account the age of the parents, family history and the presence of abnormalities during previous pregnancies.
These methods are 100% reliable. At the same time, even complete well-being during screening in the first and second trimester using ultrasound and biochemical markers cannot guarantee the absence of chromosomal abnormalities in the fetus. The choice and determination of the sufficiency of diagnostic methods is carried out taking into account the age of the parents, family history and the presence of abnormalities during previous pregnancies.
We carry out all types of ultrasound diagnostics:
- 3D and 4D ultrasound during pregnancy
- Fetometry data at various times
- Ultrasound diagnostics of Down syndrome and other chromosomal abnormalities
- Evaluation of the correct development of the fetus by ultrasound
Ultrasound during pregnancy
- Hydrotubation (echohydrotubation): examination of the patency of the fallopian tubes (ultrasonic hysterosalpingoscopy)
- Transvaginal
- Ovaries
- Uterus
- Mammary glands
Female ultrasound
- Duplex Scan
- Cerebral vessels
- Neck vessels (duplex angioscanning of the main arteries of the head)
- Veins of the lower extremities
Vascular ultrasound
- Transrectal (trusion): prostate
- Scrotum (testicles)
- Vessels of the penis
Male ultrasound
- Appendicitis
- Abdomen
- Gallbladder
- Stomach
- Intestines
- Bladder
- Soft tissue
- Pancreas
- Liver
- Kidney
- Joints
- Thyroid
- Echocardiography (ultrasound of the heart)
Organ ultrasound
- Varicose veins: ultrasound diagnosis of varicose veins
- Hypertension: Ultrasound diagnosis of hypertension
- Thrombosis: ultrasound diagnosis of vein thrombosis
- Ultrasound diagnosis of chronic pancreatitis
- for kidney stones
- for cholecystitis
Ultrasound diagnostics of diseases
- Hip joints in newborns (if hip dysplasia is suspected)
Pediatric ultrasound
Risk group
Necessary understand that the probability of detection pathology and the development of this pathology - it's not the same thing.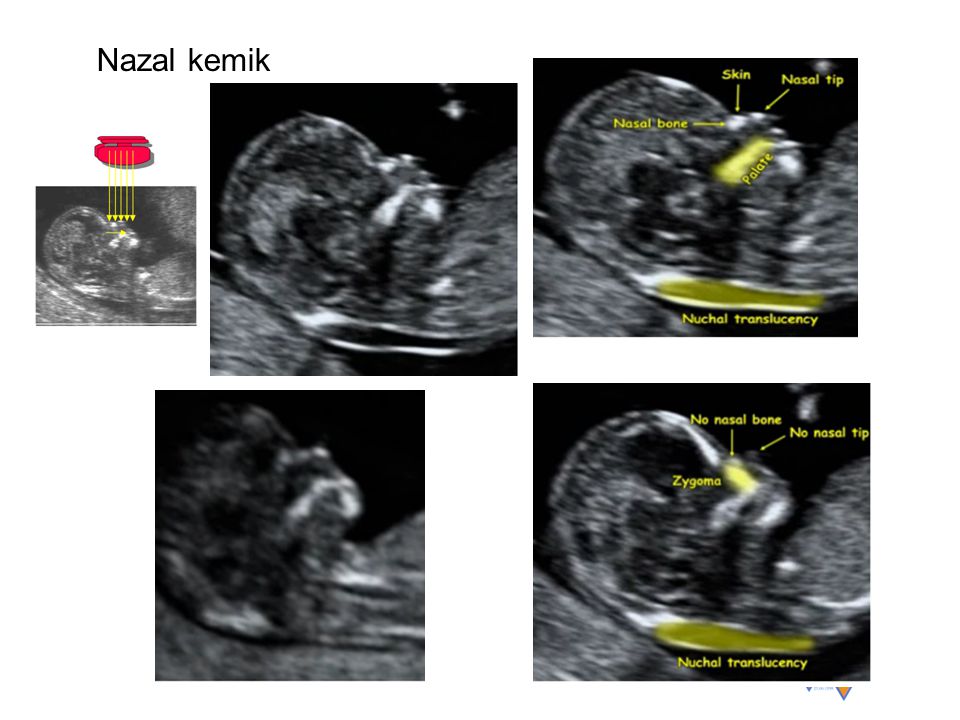 Elevated detection the risk of any deviation from the normal course of pregnancy or normal fetal development which is not a diagnosis. Pregnant women in the group risk, special additional research to confirm or rule out pathology. When is research done?
Elevated detection the risk of any deviation from the normal course of pregnancy or normal fetal development which is not a diagnosis. Pregnant women in the group risk, special additional research to confirm or rule out pathology. When is research done?
IN I trimester prenatal screening it is recommended to carry out on the 10-14th week pregnancy (optimally - on the 11-13th week). In II trimester examination can be done with 14th to 20th week (optimally - on the 16th-18th week).
Time screening studies also chosen randomly. Wherein a combination of factors is taken into account. Firstly, this is the maximum information indicators, secondly, gestational age, where additional research will be the safest for woman and child.
Simultaneous using another simple and available method - ultrasonic research - helps to increase accuracy and reliability of prenatal diagnostics. Screening includes ultrasound examination in I trimester of pregnancy (11-13 weeks). During this period, the number fetuses in the uterus and their viability, specifying the gestational age (according to coccyx-parietal size - KTR), gross malformations are excluded and chromosomal markers are determined fetal pathology (collar thickness space, presence or absence nasal bone). The term "thickness collar space "many synonyms found in literature or the conclusion of ultrasound specialists: TVP, cervical transparency, width of the cervical folds, collar zone, NT. In any case, we are talking about the accumulation subcutaneous fluid on the posterior surface fetal neck. Measure the thickness of this layer possible only in I trimester of pregnancy (until the 14th week), since at a later date this the fluid is usually resorbed. Normally, TVP should be no more than 2.7 mm. An increase in this size is typical for Down syndrome. Also, with this pathologies are often not visualized nasal bones in the fetus.
The term "thickness collar space "many synonyms found in literature or the conclusion of ultrasound specialists: TVP, cervical transparency, width of the cervical folds, collar zone, NT. In any case, we are talking about the accumulation subcutaneous fluid on the posterior surface fetal neck. Measure the thickness of this layer possible only in I trimester of pregnancy (until the 14th week), since at a later date this the fluid is usually resorbed. Normally, TVP should be no more than 2.7 mm. An increase in this size is typical for Down syndrome. Also, with this pathologies are often not visualized nasal bones in the fetus.
Necessary know that the concentration of b-hCG, PAPP, estriol and AFP in the blood can change not only with chromosomal pathology and DZNT, but also with other pathology pregnancy: threatened miscarriage or spontaneous abortion, intrauterine developmental delay or death of the fetus, placental insufficiency, late toxicosis (gestosis). Also on the value of biochemical parameters affects the intake of progestogens (Dufaston, Utrozhestan), multiple pregnancy.
Compare the results are the same, but performed in different laboratories incorrect, since the units of measurement and the norms often do not match. It's connected with the fact that for research These laboratories use different test systems. And to calculate the risks pathology at present there are several special programs with their own standards. And the results such an important examination as prenatal screening (wherever it is completed), should be able to assessed by any gynecologist. That's why received data is transferred to MoM (special coefficient). MoM norms for any biochemical markers, and also for collar thickness space (TVP) - from 0.5 to 2.0.
For adjusting the MoM value and calculating individual risk are taken into account factors such as the number of fruits, body weight of a pregnant woman, racial affiliation, smoking, sugar diabetes, use of ancillary reproductive technologies (IVF). Taking into account of this data is carried out individually MoM correction, resulting in "adjusted MoM value". Exactly it is then used to calculate individual risks. That's why everything the above factors should be shown on the referral form. How a separate risk factor is taken into account the age of the expectant mother. This is due to the fact that after 35 years the probability of being born child with Down syndrome increases.
Exactly it is then used to calculate individual risks. That's why everything the above factors should be shown on the referral form. How a separate risk factor is taken into account the age of the expectant mother. This is due to the fact that after 35 years the probability of being born child with Down syndrome increases.
I trimester II trimester Pregnancy (weeks) 10-14 weeks (optimal - 11-13) 14-20 weeks (optimally - 16-18) Biochemical markers (blood test) Free b-hCG PAPP-A AFP Free estriol L-hCG Basic ultrasound markers KTP
TVP
nasal bone
Calculation risk of chromosomal abnormalities in the fetus carried out in the laboratory using special programs and is indicated in figures. There is a threshold risk, which is 1:250. It means that statistical probability of birth a child with a chromosomal abnormality (Down syndrome, Edwards syndrome) accounts for 1 case out of 250. Comparison the result obtained with a threshold value allows you to highlight women risk groups, which should be additional research has been carried out.