What causes failure to thrive
Failure to Thrive | Johns Hopkins Medicine
Failure to Thrive | Johns Hopkins MedicineWhat is failure to thrive?
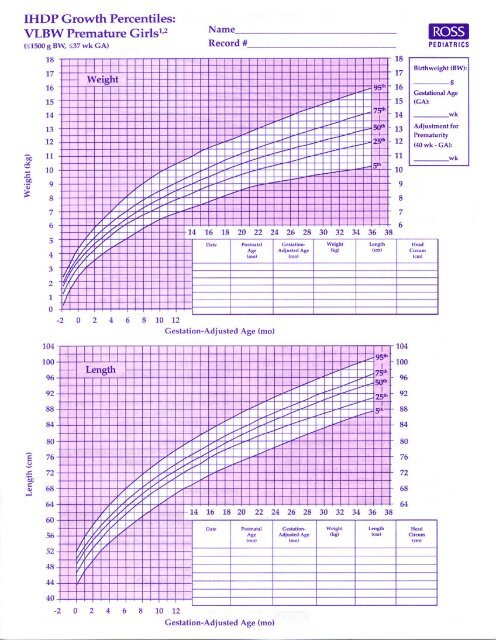
Children are diagnosed with failure to thrive when their weight or rate of weight gain is significantly below that of other children of similar age and sex. Infants or children that fail to thrive seem to be dramatically smaller or shorter than other children the same age. Teenagers may have short stature or appear to lack the usual changes that occur at puberty. However, there is a wide variation in what is considered normal growth and development.
Symptoms
In general, the rate of change in weight and height may be more important than the actual measurements.
Infants or children who fail to thrive have a height, weight and head circumference that do not match standard growth charts. The person's weight falls lower than the third percentile (as outlined in standard growth charts) or 20 percent below the ideal weight for their height. Growing may have slowed or stopped after a previously established growth curve.
The following are delayed or slow to develop:
Physical skills, such as rolling over, sitting, standing and walking
Mental and social skills
Secondary sexual characteristics (delayed in adolescents)
Diagnosis
It is important to determine whether failure to thrive results from medical problems or factors in the environment, such as abuse or neglect.
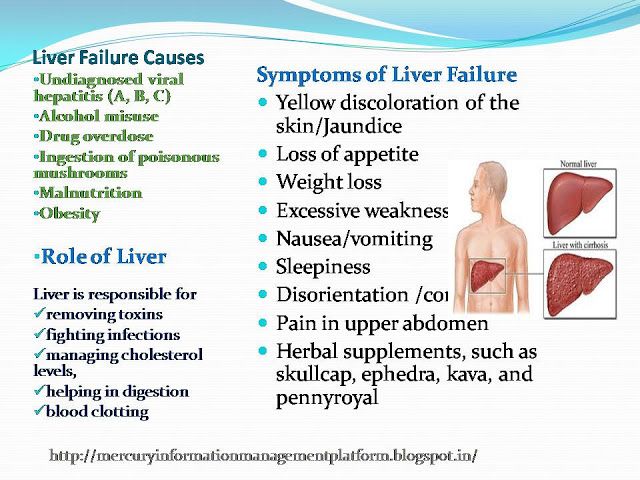
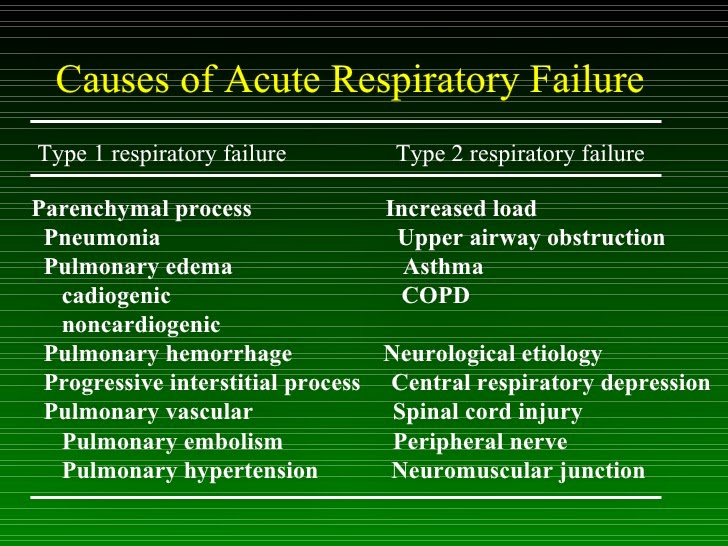
There are multiple medical causes of failure to thrive. These include:
Chromosome abnormalities, such as Down syndrome and Turner syndrome
Defects in major organ systems
Problems with the endocrine system, such as thyroid hormone deficiency, growth hormone deficiency or other hormone deficiencies
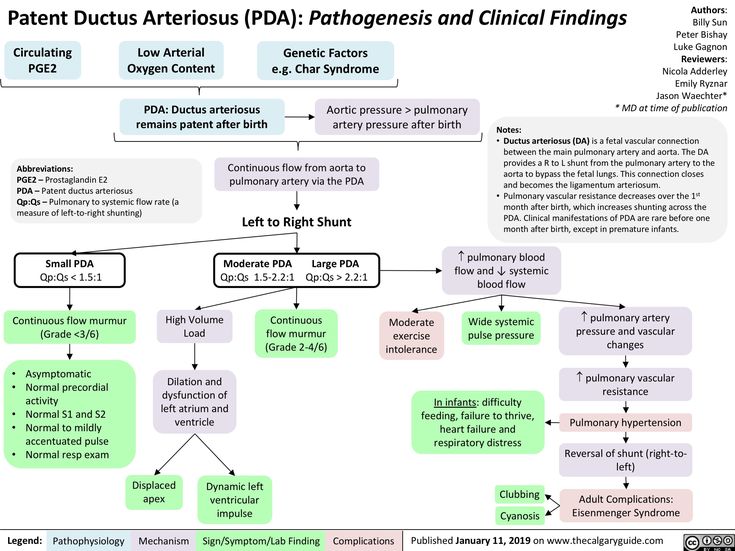
Damage to the brain or central nervous system, which may cause feeding difficulties in an infant
Heart or lung problems, which can affect how oxygen and nutrients move through the body
Anemia or other blood disorders
Gastrointestinal problems that result in malabsorption or a lack of digestive enzymes
Long-term gastroenteritis and gastroesophageal reflux (usually temporary)
Cerebral palsy
Long-term (chronic) infections
Metabolic disorders
Complications of pregnancy and low birth weight
Other factors that may lead to failure to thrive:
Emotional deprivation as a result of parental withdrawal, rejection or hostility
Economic problems that affect nutrition, living conditions and parental attitudes
Exposure to infections, parasites or toxins
Poor eating habits, such as eating in front of the television and not having formal meal times
Many times the cause cannot be determined.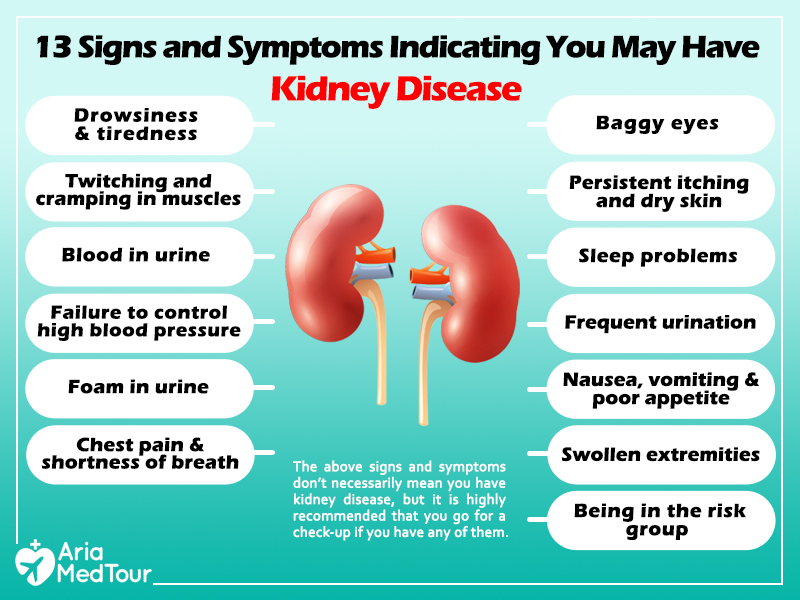
Treatment
The treatment depends on the cause of the delayed growth and development. Delayed growth due to nutritional factors can be resolved by educating the parents to provide a well-balanced diet.
If psychosocial factors are involved, treatment should include improving the family dynamics and living conditions. Parental attitudes and behavior may contribute to a child's problems and need to be examined. In many cases, a child may need to be hospitalized initially to focus on implementation of a comprehensive medical, behavioral and psychosocial treatment plan.
Do not give your child dietary supplements without consulting your physician first.
Related
-
Pediatric
Healthy Sleep Habits
-
Nutrition
Feeding Guide for the First Year
-
Preschooler Nutrition
Preschooler Nutrition
Related Topics
Failure to Thrive (for Parents)
What Is Failure to Thrive?
When growing kids don't gain weight as they should, it is called "failure to thrive.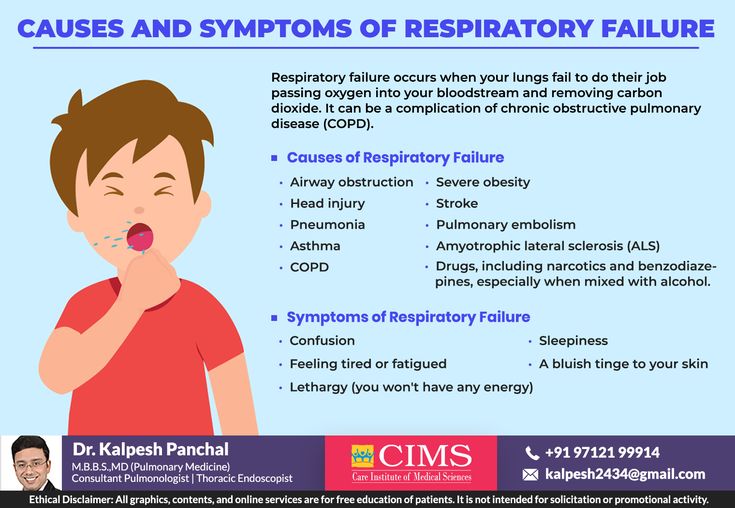 "
"
Failure to thrive is not a disease or disorder itself. Rather, it's a sign that a child is undernourished. In general, kids who fail to thrive are not getting enough calories to grow and gain weight in a healthy way. When kids can't gain weight, they also often may not grow as tall as they should.
Kids need to get enough calories to learn and develop well. So kids with failure to thrive might start to walk and talk later than other kids, and can have trouble learning in school.
What Causes Failure to Thrive?
Different things can cause failure to thrive, including:
- Not enough calories provided. Sometimes a parent or caregiver measures or mixes formula incorrectly, so an infant doesn't get enough calories. Problems with breastfeeding or starting solids also can cause failure to thrive. Some families have trouble affording enough food for their children. And sometimes parents miss their children's hunger cues.
- The child eats too little.
 Some children have trouble eating enough food. This might be due to a developmental delay, being a very picky eater, a medical condition that affects swallowing (like cerebral palsy or a cleft palate), or a condition like autism in which kids don't like eating foods with some textures or tastes.
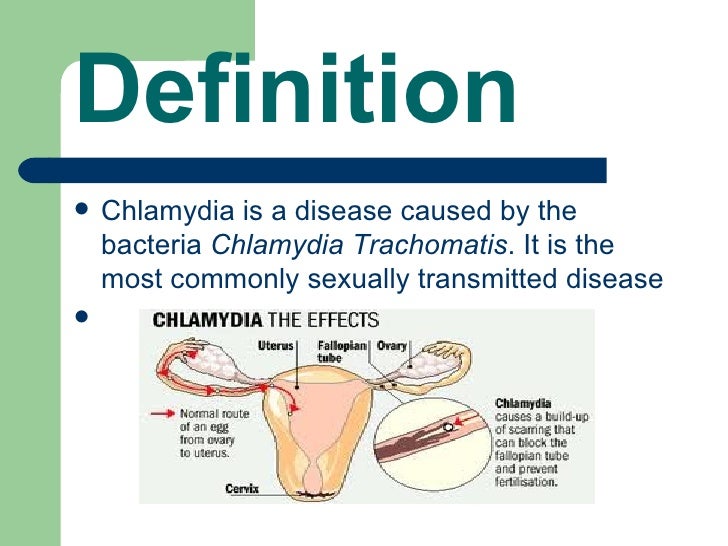
Some children have trouble eating enough food. This might be due to a developmental delay, being a very picky eater, a medical condition that affects swallowing (like cerebral palsy or a cleft palate), or a condition like autism in which kids don't like eating foods with some textures or tastes. - Health problems involving the digestive system. Problems with the digestive system can prevent a child from gaining weight. Conditions like gastroesophageal reflux (GER), chronic diarrhea, cystic fibrosis, chronic liver disease, and celiac disease can make it harder for kids to absorb enough nutrients and calories to gain weight.
- Food intolerance. A food intolerance means the body is sensitive to some foods. For example, milk protein intolerance means the body can't absorb foods such as yogurt and cheese, which could lead to failure to thrive.
- An ongoing medical condition. Kids with conditions involving the heart, lungs, or endocrine system might need more calories than other kids.
 It can be hard for some to eat enough.
It can be hard for some to eat enough. - Infections. The body can use up a lot of calories as it fights an infection. And kids who don't feel well might eat less than usual.
- Metabolic disorders. These are health conditions that make it hard for the body to break down, process, or take energy from food. They also can cause a child to eat poorly or vomit.
Sometimes a mix of things leads to failure to thrive. For instance, if a baby has severe GER and is reluctant to eat, feeding times can be stressful. The baby may be upset and frustrated, and the caregiver might not be able to get the baby to eat enough.
Other times, doctors aren't sure exactly what causes the problem.
How Is Failure to Thrive Diagnosed?
Many babies and kids go through brief periods when they don't gain as much weight as expected. But if a child continues to not gain enough weight or loses weight, doctors try to find out why.
They'll ask for a child's health history, including a feeding history.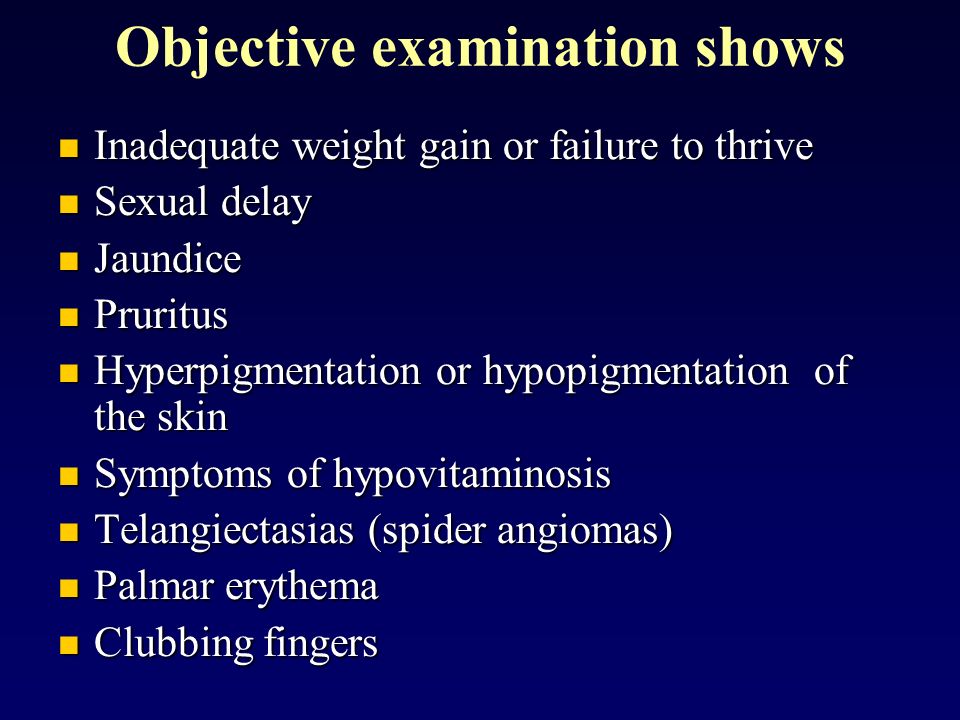 This helps them see if underfeeding, household stresses, or feeding problems might be causing the problem. A dietitian or other health care professional also may track the calories in a child's diet to make sure the child is getting enough.
This helps them see if underfeeding, household stresses, or feeding problems might be causing the problem. A dietitian or other health care professional also may track the calories in a child's diet to make sure the child is getting enough.
Doctors measure a child's weight, length, and head circumference at each well-child checkup and put the results on a growth chart. Children may have failure to thrive if they weigh less than most kids their age or aren't gaining weight as quickly as they should.
Doctors might order tests (such as blood tests or urine tests) to check for medical problems that could affect a child's weight and growth.
How Is Failure to Thrive Treated?
Treating kids who fail to thrive involves making sure they get the calories needed to grow. The care team also will address any causes for poor weight gain they find. A child's care team may include:
- the primary care doctor
- a registered dietitian
- occupational therapists to help with sensory or coordination problems
- speech therapists to help with any sucking or swallowing problems
- a social worker if a family has trouble getting enough food
- psychologists and other mental health professionals for any behavioral issues
- specialists (such as a cardiologist, neurologist, or gastroenterologist) to treat health conditions that could affect a child's weight
Usually, kids who have failure to thrive can be treated at home. They'll also have regular doctor visits to check on weight gain. Doctors often recommend high-calorie foods and, for babies, a high-calorie formula.
They'll also have regular doctor visits to check on weight gain. Doctors often recommend high-calorie foods and, for babies, a high-calorie formula.
Doctors also might recommend:
- spacing out meals to make sure children are hungry
- avoiding "empty" calories like juices and candies
- offering foods of certain textures if sensory issues are a problem
- other strategies depending what's causing the failure to thrive
Weight gain takes time, so it might be several months before a child is back in the normal range.
Some children with failure to thrive might need care in a hospital. They'll be fed and watched around the clock for several days (or longer) until they gain some weight. After leaving the hospital, the child will continue treatment at home.
How Can Parents Help?
It can be hard to learn that your child has failure to thrive. No matter what's causing it, there are ways to help and support your child. You can:
- Follow the advice from your doctor or the dietitian.

- Take your child to all recommended doctor visits.
- Call the doctor if your child develops new symptoms, like frequent diarrhea or vomiting.
- Learn about any medical conditions that the doctor finds in your child.
- Talk to the doctor or a therapist if you feel stressed or frustrated about problems with feeding your child.
Reviewed by: Larissa Hirsch, MD
Date reviewed: February 2020
causes of drowsiness, weakness and fatigue
Periods of moral fatigue occur even in stress-resistant people. By unconsciously pausing emotions, a person protects himself from the more severe consequences of mental stress. Therefore, a short-term decrease in social and psycho-emotional activity is considered the norm. We can talk about violations of mental health, if the depressed state drags on - indifference to life appears.
In clinical psychology and psychiatry, apathy is considered as an independent syndrome of loss of motivation or a symptom that accompanies mental disorders, addiction, neurological diseases.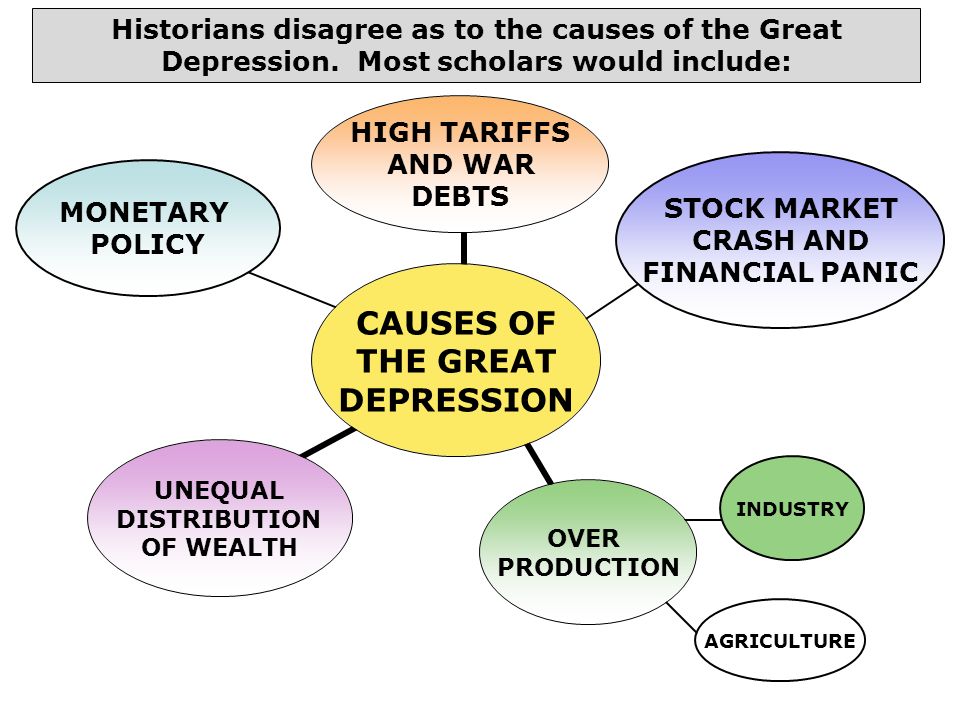 It is quite difficult to get out of this state without the help of a specialist. Especially if the situation is aggravated by misunderstanding of relatives. How does it manifest itself, why does apathy arise? Should she be treated with medication as a mental illness? We will answer these other questions in the article.
It is quite difficult to get out of this state without the help of a specialist. Especially if the situation is aggravated by misunderstanding of relatives. How does it manifest itself, why does apathy arise? Should she be treated with medication as a mental illness? We will answer these other questions in the article.
What is apathy?
Apathy and demoralization belong to a group of symptoms that combine deviations in the psychobehavioral, emotional, and cognitive spheres. There are several opinions about the typological affiliation of apathy in the structure of psychopathological disorders. Many experts characterize the apathetic state as the suppression of goal-directed behavior against the background of preserved intelligence and physical capabilities. Banal laziness and apathy are not identical concepts. A lazy person tries to avoid duties, but at the same time does not lose emotions, motivation for things that interest him. An apathetic patient lacks any initiative, cognitive activity and emotional response sharply decrease.
Along with mental and motor retardation, apathy is included in the symptom complex of depression. This allows us to classify the apathetic state as a psycho-emotional dysfunction:
- Anhedonia is the loss of the ability to experience positive emotions: pleasure, delight, joy. A person cannot enjoy pleasant things, people, situations. The brain refuses to act because it does not receive a “reward” in the form of positive emotions.
- Abulia - lack of will, psychological inability to perform actions, seek and make decisions. The patient does not lose consciousness, but cannot do anything.
Sustained decrease in mood (hypothymia), indifference to ongoing events are characteristic of different types of depressive disorders. With true major or minor depression, a person is haunted by feelings of guilt, obsessive negative thoughts about the past, present, and future. With apathetic depression, there is no concern about what happened, the desire to participate in what is happening, the motivation for life planning. A person does not care about either negative or positive events. Relatively speaking, the toggle switch "desires - feelings - interest" is turned off.
A person does not care about either negative or positive events. Relatively speaking, the toggle switch "desires - feelings - interest" is turned off.
Types of apathy
Many clinical cases are presented by passive apathetic depression. Loss of motivation is accompanied by severe symptoms that are noticeable to others. A person is changing before our eyes, without hiding it. From a sociable and hardworking employee, an attentive relative, he turns into a closed "beech", devoid of emotional reactions.
Active apathy is much less common. The patient loses interest in what is happening, loses the meaning of life, but diligently disguises it with imaginary activity. With difficulty, a person continues to perform daily duties, experiencing severe mental discomfort. This condition is considered more dangerous, since it gradually destroys the psyche, leads to the degradation of the personality, and provokes suicidal thoughts.
The difference between apathy and anhedonia is the lack of separation of life aspects. Anhedonia can be partial, that is, cover one side of life - social, physical or intellectual-aesthetic. An apathetic state is almost always total - a complete loss of interest in any aspect of life.
Anhedonia can be partial, that is, cover one side of life - social, physical or intellectual-aesthetic. An apathetic state is almost always total - a complete loss of interest in any aspect of life.
Causes of psycho-behavioral and emotional disorders
The basic trigger for apathetic depression in healthy people is mental exhaustion resulting from:
- occupational burnout;
- prolonged psychological stress;
- exhausting and unbearable loads against the background of lack of proper sleep;
- hypertrophied responsibility, perfectionism, "excellent student syndrome";
- long-term struggle with severe illness.
Post-traumatic stress disorder (PTSD) can cause lethargy. Indifference to the outside world develops against the background of psychotrauma. For example, the death of a loved one, a difficult divorce, loss of property. The degree of indifference depends on the personality accentuation - personal vulnerability to certain psychogenic factors.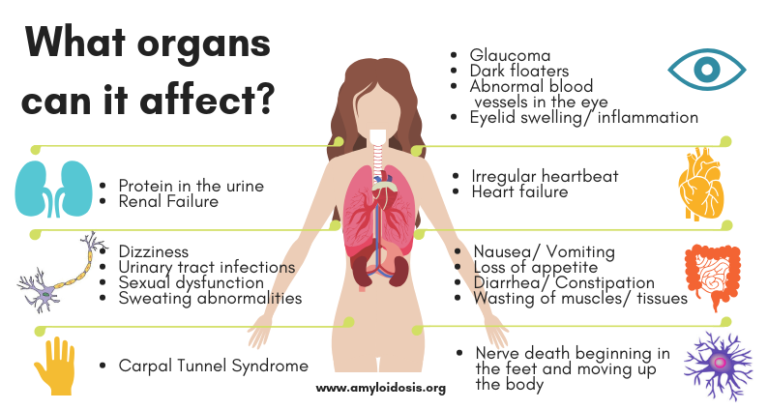 Etiologically, the condition is comparable to a protracted reactive psychosis - a distortion of the worldview in the patient's mind.
Etiologically, the condition is comparable to a protracted reactive psychosis - a distortion of the worldview in the patient's mind.
Other factors that provoke an indifferent attitude to life include:
- Shift in the level of hormones and neurotransmitters, damage to the frontal lobes of the brain. Changes are typical for infectious lesions of the membranes of the brain, craniocerebral injuries, neurogenic, endocrine diseases. Endogenous disorders play a leading role in the development of apathetic depression in women in the postpartum or menopausal period.
- Mental disorders. These are all types of schizophrenia, schizoid psychopathy, Alzheimer's disease, especially uncompensated forms (lack of treatment with specific drugs). The condition is complicated by the loss of the ability to separate the main from the secondary, to establish connections between phenomena.
- Addictions - alcoholism, drug addiction. The loss of motivation and the meaning of life is associated with severe withdrawal symptoms when alcohol and drugs are given up.
 The withdrawal syndrome is accompanied by a feeling of fear, irritability, psychosis, which is replaced by complete indifference.
The withdrawal syndrome is accompanied by a feeling of fear, irritability, psychosis, which is replaced by complete indifference. - Side effect of sleeping pills. Medicines inhibit the synaptic transmission of nerve impulses, so in the morning many people feel detached, indifferent.
In men, the causes of psycho-emotional dysfunction are more often associated with the professional sphere, in women - with interpersonal relationships, hormonal changes. Despite this, women are less prone to apathy. The gender imbalance is explained by the lability of the female psyche, the high involvement of women in social and family ties, and the excess of social roles.
Symptoms
In case of mental disorders, endogenous disorders, neurogenic diseases, addictions, apathy accelerates the impairment of cognitive functions and reduces the quality of life. Apathy is manifested by refusal of treatment. Melancholy grows, unwillingness to perform any actions - get out of bed, leave the house, wash, comb your hair.
In contrast to depressed patients, who usually acknowledge their hopelessness and the need for medical help, apathetic people rarely acknowledge their condition. The following symptoms help to suspect psycho-emotional dysfunction in a person:
- Detachment from family, social, professional problems. A person does not want to take part in discussions, take the initiative.
- Striving for loneliness, seclusion.
- Exhausted look - a haggard face, circles under the eyes, a detached look.
- Absence of emotional reactions. Do not cause reciprocal experiences sad or joyful news.
- Reticence, reticence, monotonous and poor speech. An apathetic patient avoids communication with relatives, colleagues, friends, easily breaks off old ties, refrains from making new acquaintances.
- Stingy facial expressions, gestures. A smile practically does not appear on the face, the movements are constrained, a little clumsy.
- Decreased appetite, physical activity.
 There is a retardation of attention, thinking.
There is a retardation of attention, thinking. - Changing habits. It includes giving up hobbies, participation in family and friendly gatherings.
In women, the symptoms of lethargy are reflected in appearance. They stop wearing make-up, dressing beautifully, because appearance, like everything else, ceases to be significant.
Internal state is characterized by:
- Chronic fatigue. Physical and moral weakness is always present (regardless of the time of day).
- Daytime sleepiness, decreased quality of night sleep. There are different types of insomnia - frequent awakenings at night, inability to fall asleep quickly.
- Oppression of sexuality. There is no libido, psychophysical pleasure from tactile sensations.
- Indifference to former pleasures. For example, a person refuses delicious food, outdoor recreation, SPA treatments, etc.
- Loss of desire to develop, contemplate the beautiful - listen to music, travel, watch movies, read books.
Psycho-emotional state affects physical health. There are regular headaches that are difficult to remove with painkillers. Aches in the bones, dyspepsia, problems with bowel movements appear, muscle tone decreases.
Treatment
When the psyche is not destroyed, and the patient himself is aware of the causes of apathy, rest, good sleep, healthy nutrition, and physical activity help to cope with indifference. If apathy continues for two weeks or more, specialist help is required. Therapy is aimed at stabilizing the functioning of the nervous system, restoring mental health, and maintaining physical fitness.
Comprehensive treatment includes:
- Medicines. Taking into account contraindications, age, severity of the disorder, tranquilizers, antidepressants, antipsychotics are prescribed. Special therapy can be supplemented by cardiological drugs, anti-pressure drugs.
- Psychological and psychotherapeutic assistance. To restore motivation, various methods and psychotechnics are used.
 Cognitive Behavioral Therapy - recognition and correction of behavioral attitudes. Gestalt therapy is the development of self-awareness (understanding, acceptance of one's state, liberation from it). Art therapy is the return of emotionality, the development of creativity. Personal growth training is the stimulation of the desire to return to the old life, to learn something new. At the first stage, classes are held one-on-one with a psychologist, at the second - in groups.
Cognitive Behavioral Therapy - recognition and correction of behavioral attitudes. Gestalt therapy is the development of self-awareness (understanding, acceptance of one's state, liberation from it). Art therapy is the return of emotionality, the development of creativity. Personal growth training is the stimulation of the desire to return to the old life, to learn something new. At the first stage, classes are held one-on-one with a psychologist, at the second - in groups. - Recovery of physical health. Includes sports, massage, walks in interesting places, a varied diet, taking vitamins, biologically active food supplements.
Treatment of apathy requires attention from relatives and friends. The support of relatives increases the effectiveness of the work of a psychologist, speeds up recovery. For this, family psychotherapy, family psychological counseling are provided. The involvement of relatives helps to find the root cause of an apathetic state, to form the correct behavior model to create a healthy environment in the family.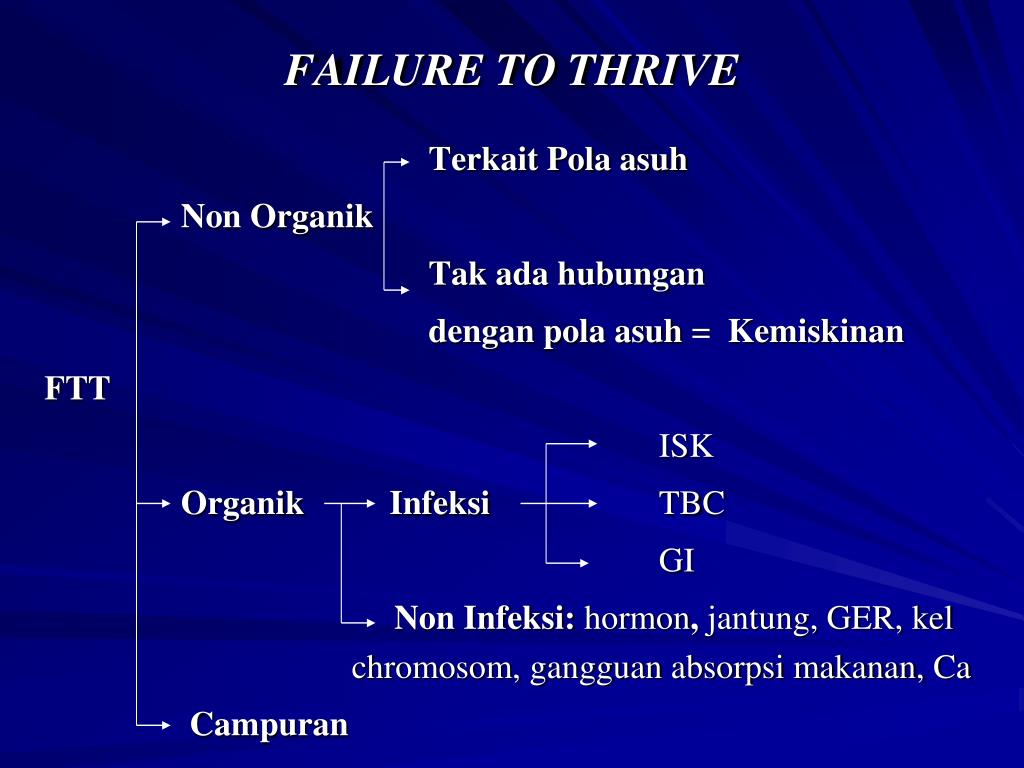
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find a country »
- A
- B
- C
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- Й
- К
- Л
- М
- Н
- О
- П
- Р
- С
- T
- U
- F
- x
- C 900 9
- Sh
- E
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.

- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, flatness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
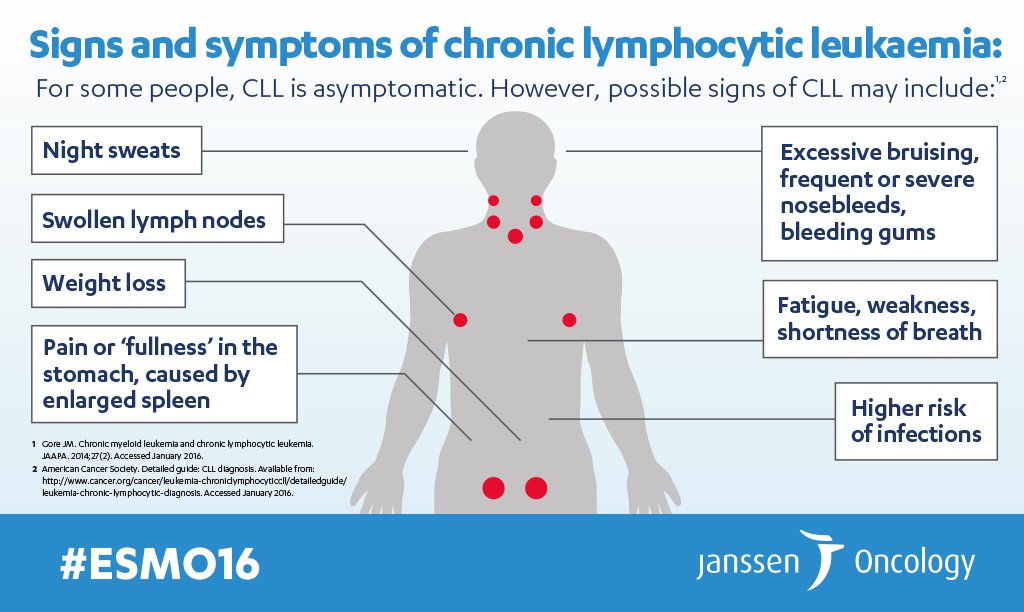
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).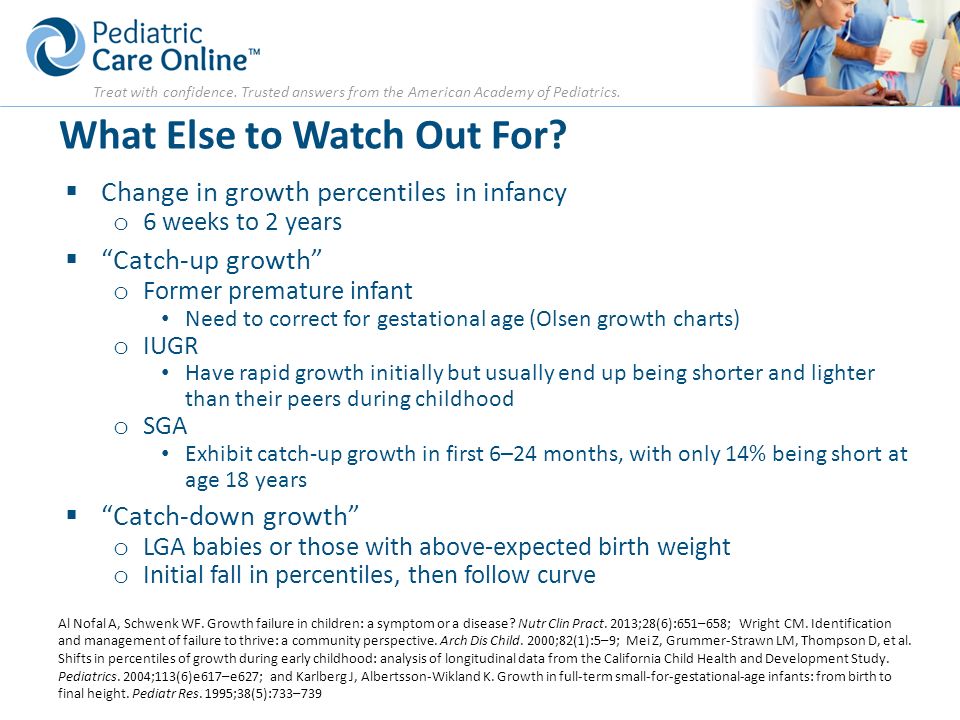 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.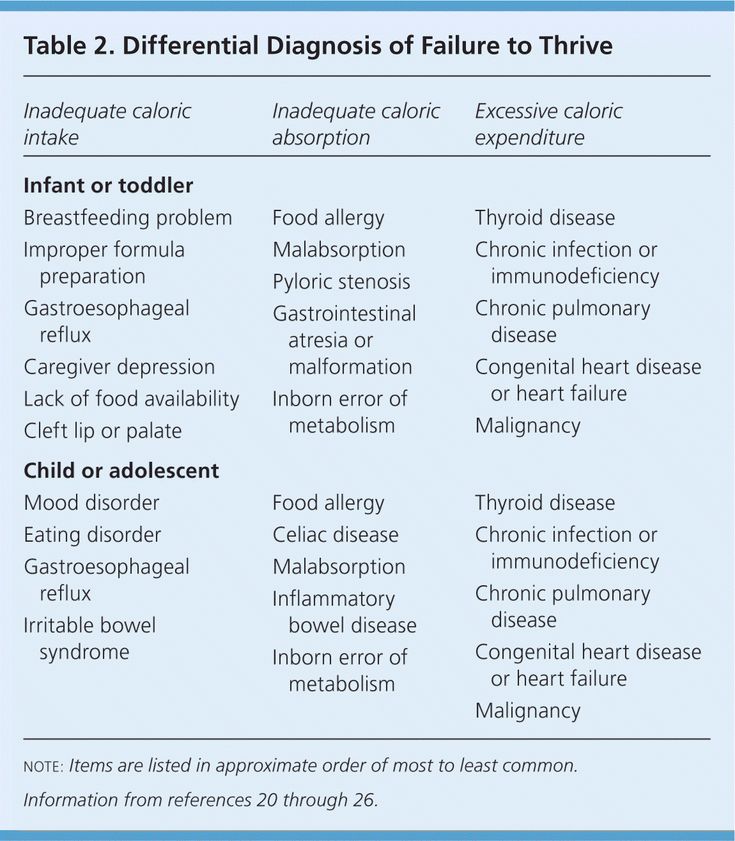
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
The vast majority of people with schizophrenia do not currently receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.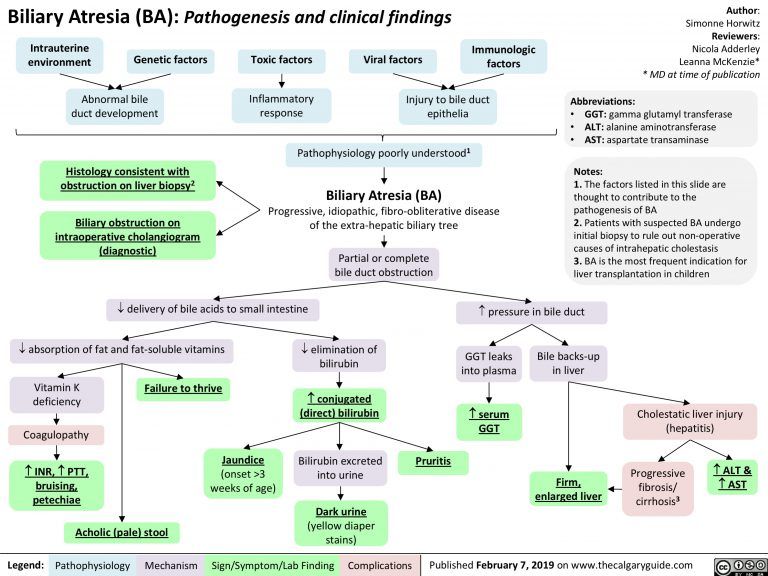 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).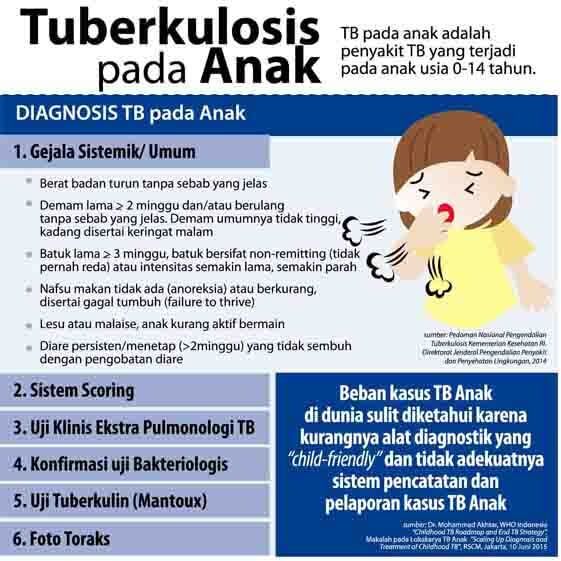 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.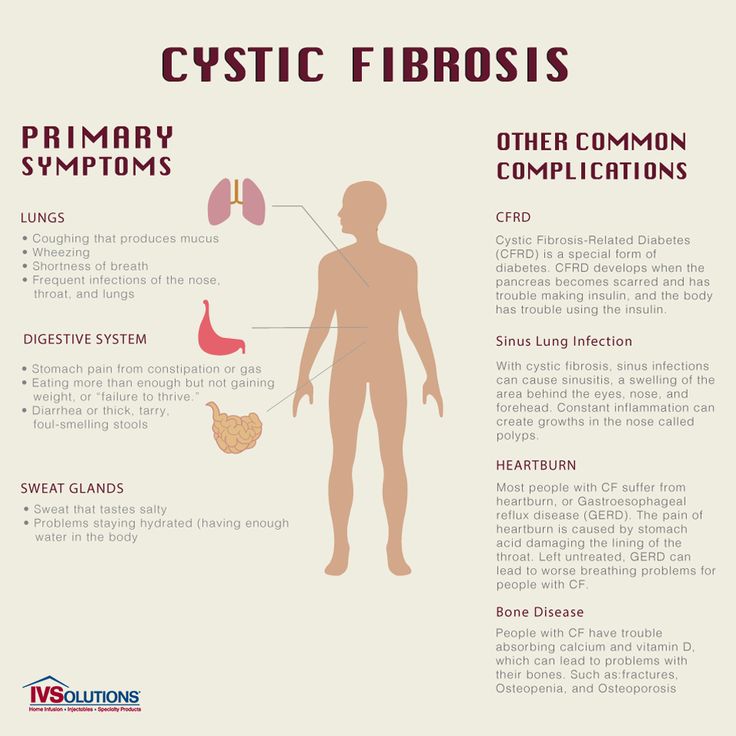 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.