Reasons for emergency c-section
Why They're Needed and What to Expect
Congratulations, you’re expecting! This exciting time includes a lot of changes for you, as well as planning for the arrival of your baby and the not-so-distant future. It can also mean lots of anxiety and trying to make your birth plan just right.
Sometimes we plan, and the universe gently smiles. For many reasons, your birth plan may change — sometimes in regards to its smaller details, and other times in regards to its bigger ones, including how you want to give birth.
Whether your plans are for a vaginal birth or scheduled cesarean delivery (also called a C-section), both of these options will be off the table if you need an emergency C-section.
Don’t worry. You and your baby are in expert hands. Although almost 32 percent of births in the United States occur by C-section, you’re less likely to need an emergency C-section, which only happens when it’s the safest option for you and your baby.
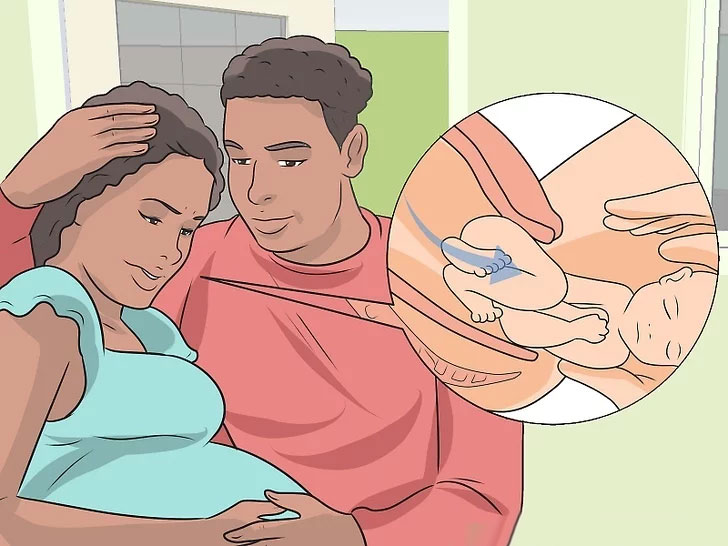
An emergency C-section is one that happens very quickly due to immediate concern for the health of the mother and/or baby. The goal is that no more than 30 minutes pass between the decision to perform an emergency C-section and delivery, but it can take up to 75 minutes.
Any kind of C-section is a major surgery that requires a room full of healthcare professionals and a great deal of organizing. This means that when a patient needs an emergency C-section, a lot of doctors and nurses have to get ready faster than normal.
You can end up having an emergency C-section even if you already had a scheduled, planned, or even unplanned C-section in the works. All of these are sometimes called medical C-sections, as they happen for health reasons. In comparison, an elective C-section is one that you choose to have.
What’s the difference between the types of C-sections?
- Scheduled C-section. This is when you and your doctor decide that it’s safest for you and your baby to deliver via C-section, potentially because you’ve had a C-section before. Your doctor will schedule a C-section date around your estimated delivery date, possibly months in advance.

- Unplanned C-section. This is when you were planning to have a vaginal birth, but a little while before your delivery your doctor decides that a C-section is best for you and your baby. This decision can be made a few weeks, days, or even hours before you’re about to give birth. With an unplanned C-section, there’s no emergency, but the change in plans is made to get you and baby onto the safest birth route.
- Emergency C-section. This happens when delivery must occur urgently to make sure both you and baby are safe. This can happen whether you’re planning to have a vaginal birth or a C-section.
They might seem like the same thing, but not all C-section experiences are created equal. Your experience, as well as the actual procedure for an emergency C-section, will be different than those of a scheduled or unplanned C-section.
What will happen during an emergency C-section?
One main difference is how you might be prepared for it.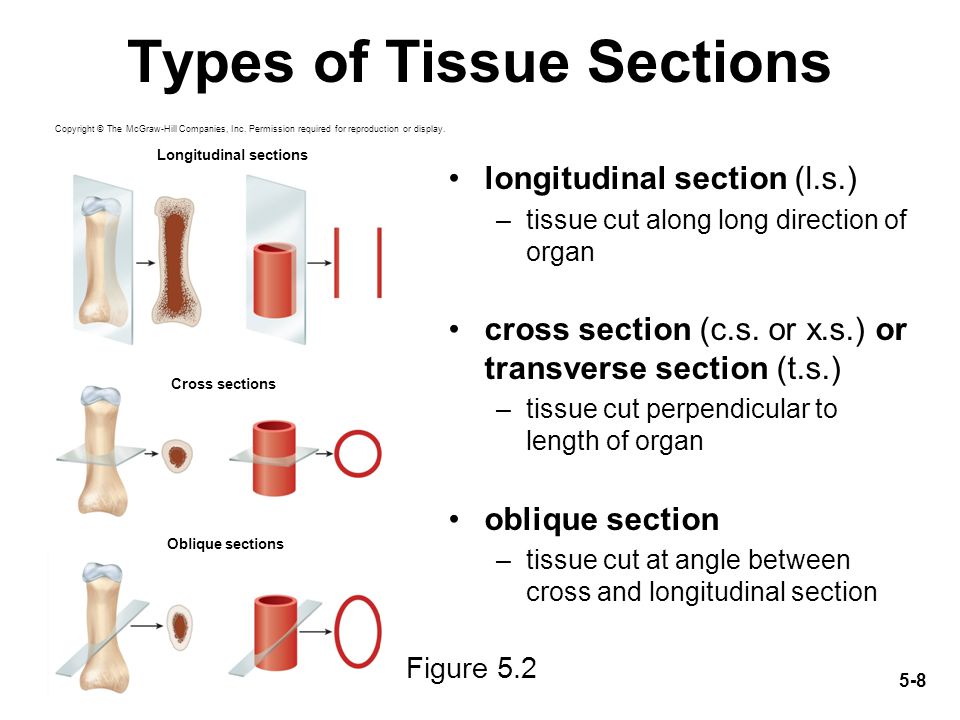 Everything must move quickly, including administering pain medications and getting the baby delivered.
Everything must move quickly, including administering pain medications and getting the baby delivered.
Most scheduled C-sections are performed with local or regional numbing (anesthesia). This means you’ll still be awake, but you won’t feel pain during the procedure. Local anesthesia is usually administered via a spinal injection, and this can take time.
In an emergency C-section, the timing and details of your situation, along with hospital policies, can affect your options for anesthesia.
Your doctor and the anesthesiologist may decide that there’s time to administer a spinal injection. Or, you may already have an epidural in place, which helps with the surgery preparations. However, depending on multiple factors, some of these options may not be possible.
Alternatively, you may have general anesthesia, using both injected and inhaled drugs to make sure you’re pain-free during the surgery. This will allow the C-section to happen more quickly, but this combination means you’re not able to be awake during the procedure.
Another difference may be the incision used during the surgery. In non-emergency C-sections, a horizontal (bikini) cut is typically performed. If you’re at term, you’ll likely have this type of incision, even in an emergency.
However, during an emergency surgery in which your baby’s health needs immediate attention, the surgeon may opt to use a vertical incision on your uterus to get to your baby faster. This type of incision may be necessary in cases of preterm birth, as well as due to adhesions from previous surgeries or fibroids that may be in the way of the uterus.
Again, this is dependent on the circumstances of your birth. Your surgeon’s training, as well as your and your baby’s health needs, are taken into consideration.
The reasons you might need an emergency C-section are also different than the reasons you might have a scheduled C-section.
Basically, an emergency C-section means that your baby isn’t cooperating with the planned exit or decides they want to come out before a scheduled or unplanned C-section. It may also mean that your health is a concern and waiting for progress isn’t the right choice.
It may also mean that your health is a concern and waiting for progress isn’t the right choice.
In most cases, there’s nothing you or your doctor can do to change the need for an emergency C-section.
The following are several reasons why this might happen:
Very long labor
Prolonged or delayed labor is when labor goes on for much longer than normal. This can sometimes cause health problems for both baby and mom. Prolonged labor is the most common reason for an emergency C-section. About 8 percent of pregnant women who are about to give birth have a prolonged labor.
When this happens, your doctor may decide that it’s much healthier for you and your baby to have an emergency C-section than to try to deliver vaginally. You might have a prolonged labor because:
- Your labor didn’t really start. Sometimes you’ve had contractions for ages, but they don’t seem to be doing anything. Plus, you may not be dilating as you should.
- Your labor stalls.
 Everything might be on track as you start having contractions and even begin dilating, but then everything stops. Sometimes this happens because your baby’s head cannot fit through your pelvis.
Everything might be on track as you start having contractions and even begin dilating, but then everything stops. Sometimes this happens because your baby’s head cannot fit through your pelvis.
Baby’s position
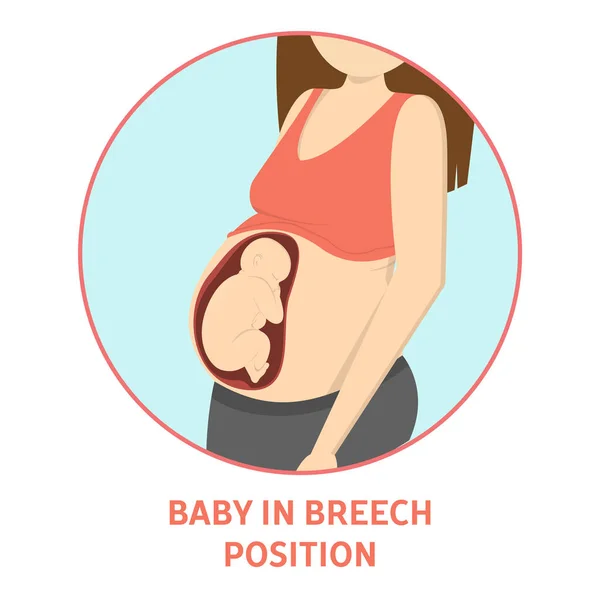
Your baby’s position might have already been a concern when your labor began, or an external cephalic version might have seemed successful, only to have baby return to a breech position at the last minute. Whatever the circumstances, labor may not progress as expected if your little one can’t be coaxed into turning around into a cooperative position.
If your baby is positioned with their behind first (breech), feet first, or stretched out sideways straight across your stomach (transverse), a vaginal delivery may not be possible. Your doctor may try to coax baby into position by turning your baby under controlled conditions, but this doesn’t always work.
Exhaustion
Sometimes all the pushing and trying in the world doesn’t seem like enough. Your doctor may have pulled out all the stops, even trying a vacuum-assisted delivery, to no avail.
Your doctor may have pulled out all the stops, even trying a vacuum-assisted delivery, to no avail.
At this stage you’ve likely been pushing for ages and are too exhausted to push any more. Your health may begin to show signs of distress, suggesting continued pushing is not an option.
At the same time, the fetal monitor might show that your baby’s heart is beating too fast or too slow. Your doctor may decide that it’s no longer safe for you and your baby to keep this up.
Health condition
If mama has a health condition or infection that comes up during labor, an emergency C-section might be recommended. For example, a herpes infection or other infection in the vaginal area can suddenly become active and harm the baby.
Alternatively, if your blood pressure or heart rate gets too high, it may not be a good idea to keep pushing. Also, if you have any kind of sudden heart or brain health issue, you may need an emergency C-section.
Tangled umbilical cord
If the umbilical cord gets compressed, tangled, or tries to come out before your baby, you’ll likely need an emergency C-section.
A prolapsed umbilical cord is a very rare complication that happens when the cord slides into the birth canal ahead of your baby. When this happens there’s a risk that it’ll be squeezed too much while your baby is trying to make their grand entrance. This can cut off baby’s blood supply.
Similarly, your baby might not be getting enough oxygen if the umbilical cord gets kinked or tangled like a garden hose.
Placental problems
Like the umbilical cord, the placenta can also complicate delivery.
Part or all of the placenta can come away from the lining of the womb. This is called placental abruption. When this happens your baby can’t get the necessary nutrients and oxygen inside the womb, and you may need an emergency C-section.
Womb tear
In very rare cases, the increased pressure on your body during birth can tear or rupture the womb. Having had a prior C-section increases your risk. If you have a womb or uterus tear (uterine rupture), you’ll need an emergency C-section.
Most of the risks of an emergency C-section are similar to those of any type of C-section.
Risks to your health include:
- an infection inside the womb or at the opening site
- opening or splitting stitches
- injury to the organs, nerves, or blood vessels near the uterus
- blood loss during the surgery
- heavy bleeding afterward
- blood clots
- a reaction to the anesthesia
- not being able to deliver vaginally in the future
Risks to your baby’s health include:
- accidental injury during the C-section
- temporary breathing problems for a few days after birth
There are also some risks to consider after the delivery is over.
If you’re asleep for the emergency C-section, you’ll likely not be able to have skin-to-skin contact with your baby right after birth. Also, the effects of the medications you were administered might make breastfeeding challenging for a while.
This does not mean that breastfeeding or bonding is impossible. You can begin a solid and satisfying breastfeeding relationship after an emergency delivery. Know that support is available, and you can work with a lactation consultant and your provider to meet your goals.
You can begin a solid and satisfying breastfeeding relationship after an emergency delivery. Know that support is available, and you can work with a lactation consultant and your provider to meet your goals.
You may also be at higher risk of post-traumatic stress and its related effects. It’s important to spend time caring for yourself and your mental health. Discuss any issues or concerns you have with your provider or a mental health professional.
Like other major surgeries, you’ll need time to rest and recover after any kind of C-section. This could mean bed rest and not being able to climb stairs or lift anything heavy for a while.
It’s important to avoid putting too much pressure on the incision site to help it heal well. You might not be able to pick up or hold your baby for too long if you’re sore. You’ll need to change the bandages and see your doctor for follow-up visits to make sure the area is not infected.
You’ll also likely need a dose of antibiotics to prevent infection. And if you need pain meds to stay comfortable, you may not be able to breastfeed your little one until you stop taking them. Ask your doctor about when it’s safe to breastfeed.
And if you need pain meds to stay comfortable, you may not be able to breastfeed your little one until you stop taking them. Ask your doctor about when it’s safe to breastfeed.
Also, unlike other C-sections and most surgeries, your doctor decided to do an emergency C-section at the eleventh hour. This means you may not have felt emotionally or mentally prepared for it.
Again, an emergency C-section may lead to post-traumatic stress disorder (PTSD). Talk to your doctor if you’re having difficulty dealing with your birth experience or feel you may have postpartum depression.
You might need an emergency C-section if your doctor decides that it’s the best option for you to deliver a healthy baby, and the need may arise due to a number of reasons.
Neither you nor your doctor can control this outcome. While a C-section might be a major detour from your birth plan, the important thing is that you and your baby remain healthy and safe.
Why They're Needed and What to Expect
Congratulations, you’re expecting! This exciting time includes a lot of changes for you, as well as planning for the arrival of your baby and the not-so-distant future. It can also mean lots of anxiety and trying to make your birth plan just right.
It can also mean lots of anxiety and trying to make your birth plan just right.
Sometimes we plan, and the universe gently smiles. For many reasons, your birth plan may change — sometimes in regards to its smaller details, and other times in regards to its bigger ones, including how you want to give birth.
Whether your plans are for a vaginal birth or scheduled cesarean delivery (also called a C-section), both of these options will be off the table if you need an emergency C-section.
Don’t worry. You and your baby are in expert hands. Although almost 32 percent of births in the United States occur by C-section, you’re less likely to need an emergency C-section, which only happens when it’s the safest option for you and your baby.
An emergency C-section is one that happens very quickly due to immediate concern for the health of the mother and/or baby. The goal is that no more than 30 minutes pass between the decision to perform an emergency C-section and delivery, but it can take up to 75 minutes.
Any kind of C-section is a major surgery that requires a room full of healthcare professionals and a great deal of organizing. This means that when a patient needs an emergency C-section, a lot of doctors and nurses have to get ready faster than normal.
You can end up having an emergency C-section even if you already had a scheduled, planned, or even unplanned C-section in the works. All of these are sometimes called medical C-sections, as they happen for health reasons. In comparison, an elective C-section is one that you choose to have.
What’s the difference between the types of C-sections?
- Scheduled C-section. This is when you and your doctor decide that it’s safest for you and your baby to deliver via C-section, potentially because you’ve had a C-section before. Your doctor will schedule a C-section date around your estimated delivery date, possibly months in advance.
- Unplanned C-section. This is when you were planning to have a vaginal birth, but a little while before your delivery your doctor decides that a C-section is best for you and your baby.
 This decision can be made a few weeks, days, or even hours before you’re about to give birth. With an unplanned C-section, there’s no emergency, but the change in plans is made to get you and baby onto the safest birth route.
This decision can be made a few weeks, days, or even hours before you’re about to give birth. With an unplanned C-section, there’s no emergency, but the change in plans is made to get you and baby onto the safest birth route.
- Emergency C-section. This happens when delivery must occur urgently to make sure both you and baby are safe. This can happen whether you’re planning to have a vaginal birth or a C-section.
They might seem like the same thing, but not all C-section experiences are created equal. Your experience, as well as the actual procedure for an emergency C-section, will be different than those of a scheduled or unplanned C-section.
What will happen during an emergency C-section?
One main difference is how you might be prepared for it. Everything must move quickly, including administering pain medications and getting the baby delivered.
Most scheduled C-sections are performed with local or regional numbing (anesthesia). This means you’ll still be awake, but you won’t feel pain during the procedure. Local anesthesia is usually administered via a spinal injection, and this can take time.
This means you’ll still be awake, but you won’t feel pain during the procedure. Local anesthesia is usually administered via a spinal injection, and this can take time.
In an emergency C-section, the timing and details of your situation, along with hospital policies, can affect your options for anesthesia.
Your doctor and the anesthesiologist may decide that there’s time to administer a spinal injection. Or, you may already have an epidural in place, which helps with the surgery preparations. However, depending on multiple factors, some of these options may not be possible.
Alternatively, you may have general anesthesia, using both injected and inhaled drugs to make sure you’re pain-free during the surgery. This will allow the C-section to happen more quickly, but this combination means you’re not able to be awake during the procedure.
Another difference may be the incision used during the surgery. In non-emergency C-sections, a horizontal (bikini) cut is typically performed. If you’re at term, you’ll likely have this type of incision, even in an emergency.
If you’re at term, you’ll likely have this type of incision, even in an emergency.
However, during an emergency surgery in which your baby’s health needs immediate attention, the surgeon may opt to use a vertical incision on your uterus to get to your baby faster. This type of incision may be necessary in cases of preterm birth, as well as due to adhesions from previous surgeries or fibroids that may be in the way of the uterus.
Again, this is dependent on the circumstances of your birth. Your surgeon’s training, as well as your and your baby’s health needs, are taken into consideration.
The reasons you might need an emergency C-section are also different than the reasons you might have a scheduled C-section.
Basically, an emergency C-section means that your baby isn’t cooperating with the planned exit or decides they want to come out before a scheduled or unplanned C-section. It may also mean that your health is a concern and waiting for progress isn’t the right choice.
In most cases, there’s nothing you or your doctor can do to change the need for an emergency C-section.
The following are several reasons why this might happen:
Very long labor
Prolonged or delayed labor is when labor goes on for much longer than normal. This can sometimes cause health problems for both baby and mom. Prolonged labor is the most common reason for an emergency C-section. About 8 percent of pregnant women who are about to give birth have a prolonged labor.
When this happens, your doctor may decide that it’s much healthier for you and your baby to have an emergency C-section than to try to deliver vaginally. You might have a prolonged labor because:
- Your labor didn’t really start. Sometimes you’ve had contractions for ages, but they don’t seem to be doing anything. Plus, you may not be dilating as you should.
- Your labor stalls. Everything might be on track as you start having contractions and even begin dilating, but then everything stops.
 Sometimes this happens because your baby’s head cannot fit through your pelvis.
Sometimes this happens because your baby’s head cannot fit through your pelvis.
Baby’s position
Your baby’s position might have already been a concern when your labor began, or an external cephalic version might have seemed successful, only to have baby return to a breech position at the last minute. Whatever the circumstances, labor may not progress as expected if your little one can’t be coaxed into turning around into a cooperative position.
If your baby is positioned with their behind first (breech), feet first, or stretched out sideways straight across your stomach (transverse), a vaginal delivery may not be possible. Your doctor may try to coax baby into position by turning your baby under controlled conditions, but this doesn’t always work.
Exhaustion
Sometimes all the pushing and trying in the world doesn’t seem like enough. Your doctor may have pulled out all the stops, even trying a vacuum-assisted delivery, to no avail.
At this stage you’ve likely been pushing for ages and are too exhausted to push any more. Your health may begin to show signs of distress, suggesting continued pushing is not an option.
Your health may begin to show signs of distress, suggesting continued pushing is not an option.
At the same time, the fetal monitor might show that your baby’s heart is beating too fast or too slow. Your doctor may decide that it’s no longer safe for you and your baby to keep this up.
Health condition
If mama has a health condition or infection that comes up during labor, an emergency C-section might be recommended. For example, a herpes infection or other infection in the vaginal area can suddenly become active and harm the baby.
Alternatively, if your blood pressure or heart rate gets too high, it may not be a good idea to keep pushing. Also, if you have any kind of sudden heart or brain health issue, you may need an emergency C-section.
Tangled umbilical cord
If the umbilical cord gets compressed, tangled, or tries to come out before your baby, you’ll likely need an emergency C-section.
A prolapsed umbilical cord is a very rare complication that happens when the cord slides into the birth canal ahead of your baby. When this happens there’s a risk that it’ll be squeezed too much while your baby is trying to make their grand entrance. This can cut off baby’s blood supply.
When this happens there’s a risk that it’ll be squeezed too much while your baby is trying to make their grand entrance. This can cut off baby’s blood supply.
Similarly, your baby might not be getting enough oxygen if the umbilical cord gets kinked or tangled like a garden hose.
Placental problems
Like the umbilical cord, the placenta can also complicate delivery.
Part or all of the placenta can come away from the lining of the womb. This is called placental abruption. When this happens your baby can’t get the necessary nutrients and oxygen inside the womb, and you may need an emergency C-section.
Womb tear
In very rare cases, the increased pressure on your body during birth can tear or rupture the womb. Having had a prior C-section increases your risk. If you have a womb or uterus tear (uterine rupture), you’ll need an emergency C-section.
Most of the risks of an emergency C-section are similar to those of any type of C-section.
Risks to your health include:
- an infection inside the womb or at the opening site
- opening or splitting stitches
- injury to the organs, nerves, or blood vessels near the uterus
- blood loss during the surgery
- heavy bleeding afterward
- blood clots
- a reaction to the anesthesia
- not being able to deliver vaginally in the future
Risks to your baby’s health include:
- accidental injury during the C-section
- temporary breathing problems for a few days after birth
There are also some risks to consider after the delivery is over.
If you’re asleep for the emergency C-section, you’ll likely not be able to have skin-to-skin contact with your baby right after birth. Also, the effects of the medications you were administered might make breastfeeding challenging for a while.
This does not mean that breastfeeding or bonding is impossible. You can begin a solid and satisfying breastfeeding relationship after an emergency delivery. Know that support is available, and you can work with a lactation consultant and your provider to meet your goals.
You may also be at higher risk of post-traumatic stress and its related effects. It’s important to spend time caring for yourself and your mental health. Discuss any issues or concerns you have with your provider or a mental health professional.
Like other major surgeries, you’ll need time to rest and recover after any kind of C-section. This could mean bed rest and not being able to climb stairs or lift anything heavy for a while.
It’s important to avoid putting too much pressure on the incision site to help it heal well. You might not be able to pick up or hold your baby for too long if you’re sore. You’ll need to change the bandages and see your doctor for follow-up visits to make sure the area is not infected.
You might not be able to pick up or hold your baby for too long if you’re sore. You’ll need to change the bandages and see your doctor for follow-up visits to make sure the area is not infected.
You’ll also likely need a dose of antibiotics to prevent infection. And if you need pain meds to stay comfortable, you may not be able to breastfeed your little one until you stop taking them. Ask your doctor about when it’s safe to breastfeed.
Also, unlike other C-sections and most surgeries, your doctor decided to do an emergency C-section at the eleventh hour. This means you may not have felt emotionally or mentally prepared for it.
Again, an emergency C-section may lead to post-traumatic stress disorder (PTSD). Talk to your doctor if you’re having difficulty dealing with your birth experience or feel you may have postpartum depression.
You might need an emergency C-section if your doctor decides that it’s the best option for you to deliver a healthy baby, and the need may arise due to a number of reasons.
Neither you nor your doctor can control this outcome. While a C-section might be a major detour from your birth plan, the important thing is that you and your baby remain healthy and safe.
Emergency caesarean section | CryoCenter
With the help of an emergency caesarean section, a baby is born in a situation where childbirth cannot be quickly resolved through the natural birth canal without harm to mother and child. On the part of the mother, indications for surgery are cases when, due to a particular disease, childbirth poses a threat to her health, and with indications from the fetus, cases when the birth act is a burden for him, which can lead to birth trauma, birth in asphyxia ( state of acute oxygen deficiency).
This occurs in the following situations.
Clinically narrow pelvis. In this case, with normal dimensions of the pelvis, which were determined during pregnancy, at the time of delivery, it turns out that the internal dimensions of the pelvis do not correspond to the dimensions of the fetal head. This is found out when the contractions are already in full swing, the cervix has dilated, but the head, despite good labor activity and attempts that have already begun, does not move along the birth canal. This is possible in cases where the size of the fetal head is large relative to the size of the bone pelvis:
This is found out when the contractions are already in full swing, the cervix has dilated, but the head, despite good labor activity and attempts that have already begun, does not move along the birth canal. This is possible in cases where the size of the fetal head is large relative to the size of the bone pelvis:
- there is an anatomical narrowing or abnormal shape of the bony pelvic ring,
- with large fetal sizes - when the head does not configure, that is, the bones of the skull are not able to overlap each other, as is normal (the reason for this is post-term pregnancy),
- when the fetal head is inserted into the pelvis not in the smallest size, but unbends on the way to the pelvic bones, for example, so that it is not the back of the fetus's head, as is the case in most cases, but the face.
If a clinically narrow pelvis is suspected, the woman is observed for an hour: if the head does not advance, a caesarean section is performed.
Premature discharge of amniotic fluid and lack of effect from labor induction. Normally, amniotic fluid is poured out at the end of the first stage of labor, i.e., when the cervix is already open. In the case when the waters poured out before the onset of contractions, they speak of premature rupture of amniotic fluid. Further events can develop according to different scenarios. Along with the outpouring of water, regular labor activity can begin, but it also happens that contractions do not begin. Then the methods of artificial labor induction are used, for this purpose PROSTAGLANDINS AND OXYTOCIN are administered intravenously - drugs that contribute to the onset of labor. This is necessary because after the opening of the fetal bladder, the fetus is no longer protected from the penetration of infection by the membranes and cannot be in the uterine cavity for more than 24 hours after the outflow of amniotic fluid, as this is fraught with the development of infectious and inflammatory complications, both in the mother and in fetus. If, under the influence of drugs, labor activity does not begin, then a caesarean section is performed.
If, under the influence of drugs, labor activity does not begin, then a caesarean section is performed.
Anomalies in the development of labor, not amenable to drug therapy. These most often include the weakness of labor activity. At the same time, the strength of the contractions is insufficient, the contractions are not long. The main reasons leading to weakness of labor activity are as follows:
- excessive neuropsychic stress (excitement, negative emotions),
- violation of the endocrine glands, - pathological changes in the uterus (endomyometritis (inflammation of the uterus) in the past, defective scar on the uterus, malformations of the uterus, uterine fibroids),
- overdistension of the uterus due to polyhydramnios, multiple pregnancies, large fetuses,
- with congenital reduced excitability of the muscle cells of the uterus - other reasons.
For the treatment of weakness of labor, drugs are used that are administered intravenously using a dropper. When using these drugs, the doctor examines the woman in labor at certain intervals, observes the speed at which the cervix opens. If the uterus does not respond to the administered drugs, then they say that rhodostimulation is ineffective. In this case, you also have to resort to operative delivery.
When using these drugs, the doctor examines the woman in labor at certain intervals, observes the speed at which the cervix opens. If the uterus does not respond to the administered drugs, then they say that rhodostimulation is ineffective. In this case, you also have to resort to operative delivery.
Acute fetal hypoxia. During childbirth, the condition of the fetus is monitored as carefully as the health of the mother. How the baby feels can be judged by several indicators. The first is the fetal heart rate. Normally, the baby's heart beats at a frequency of 140 - 160 beats per minute, during a contraction, the heartbeat quickens to 180 beats per minute. The heartbeat of the fetus during childbirth is recorded using a special device - a heart monitor and recorded on tape. The doctor can also determine the fetal heart rate with a stethoscope. A deviation in the fetal heartbeat may indicate that the baby does not have enough oxygen. Another indicator of the baby's condition is the nature of the amniotic fluid. Normally the water is clear. When the color of the water changes during childbirth from light green to dark brown, one can also talk about the occurrence of acute oxygen deficiency. The change in the nature of the amniotic fluid is due to the appearance of the original feces - meconium.
Normally the water is clear. When the color of the water changes during childbirth from light green to dark brown, one can also talk about the occurrence of acute oxygen deficiency. The change in the nature of the amniotic fluid is due to the appearance of the original feces - meconium.
In case of acute fetal hypoxia, when the condition of the baby deteriorates sharply during childbirth, the immediate completion of labor is required, since in conditions of oxygen deficiency the fetus will die inside the uterus.
Placental abruption. Violation of the connection between the placenta and the uterine wall is accompanied by bleeding, which adversely affects both the condition of the woman and the condition of the fetus. The root cause of premature abruption of the placenta is not always possible to establish. This can be caused by both mechanical trauma during a blow and a fall, as well as diseases of various organs and systems (hypertension, kidney disease, etc. ), anomalies in the development of the uterus, polyhydramnios, multiple pregnancies, and a short umbilical cord. Other reasons are possible.
), anomalies in the development of the uterus, polyhydramnios, multiple pregnancies, and a short umbilical cord. Other reasons are possible.
Placental abruption causes bleeding. Depending on how the placenta exfoliates - from the edge or in the center, blood may leak out or accumulate between the placenta and the wall of the uterus. In any case, due to blood loss, the condition of both the mother and the baby quickly and progressively worsens. To avoid negative consequences, it is necessary to immediately end the birth by surgery.
Threatening or incipient uterine rupture. Uterine rupture is an extremely rare injury. This condition can be caused by a discrepancy between the size of the fetus and the mother's pelvis (clinically narrow pelvis), as well as previous operations (caesarean section, operations to remove myomatous nodes). The contractions become frequent, very painful, the pain in the lower abdomen becomes permanent, the uterus does not relax between contractions. With the completed rupture in the mother and fetus, signs of acute blood loss are determined. In this case, only a timely operation can save the life of the mother and fetus.
With the completed rupture in the mother and fetus, signs of acute blood loss are determined. In this case, only a timely operation can save the life of the mother and fetus.
Presentation and prolapse of the umbilical cord. There are cases when the loops of the umbilical cord are presented in front of the head or the pelvic end of the fetus, that is, they will be born first, or the loops of the umbilical cord fall out before the birth of the head. This can occur with polyhydramnios. This leads to the fact that the loops of the umbilical cord are pressed against the walls of the pelvis by the head of the fetus, blood circulation between the placenta and the fetus stops. This situation also requires immediate surgical intervention.
Severe preeclampsia. Preeclampsia is a pathology of the second half of pregnancy, which is characterized by an increase in blood pressure, a violation of the kidneys, which is expressed in the appearance of protein in the urine, as well as the presence of edema. The operation is performed with a persistent increase in blood pressure during childbirth to high numbers, which is not regulated by medication, as well as with the progression of the disease, which is expressed by the appearance of seizures. In this case, there is a spasm of the vessels of the pregnant woman, including the vessels that feed the placenta.
The operation is performed with a persistent increase in blood pressure during childbirth to high numbers, which is not regulated by medication, as well as with the progression of the disease, which is expressed by the appearance of seizures. In this case, there is a spasm of the vessels of the pregnant woman, including the vessels that feed the placenta.
Emergency surgery requires minimal preparation. First, hygienic treatment is performed. If the pregnant woman ate a few hours before the operation, then the stomach is washed and the probe is left in the stomach to avoid bronchospasm from getting vomit into the respiratory tract. The patient is administered sedative drugs intravenously, which has a positive effect on her psychological state, and also accelerates and deepens the action of the anesthetic that will be administered during anesthesia. Empty the bladder. To perform a caesarean section, the consent of the mother to the operation is required, which is reflected in the history of childbirth even in emergency situations.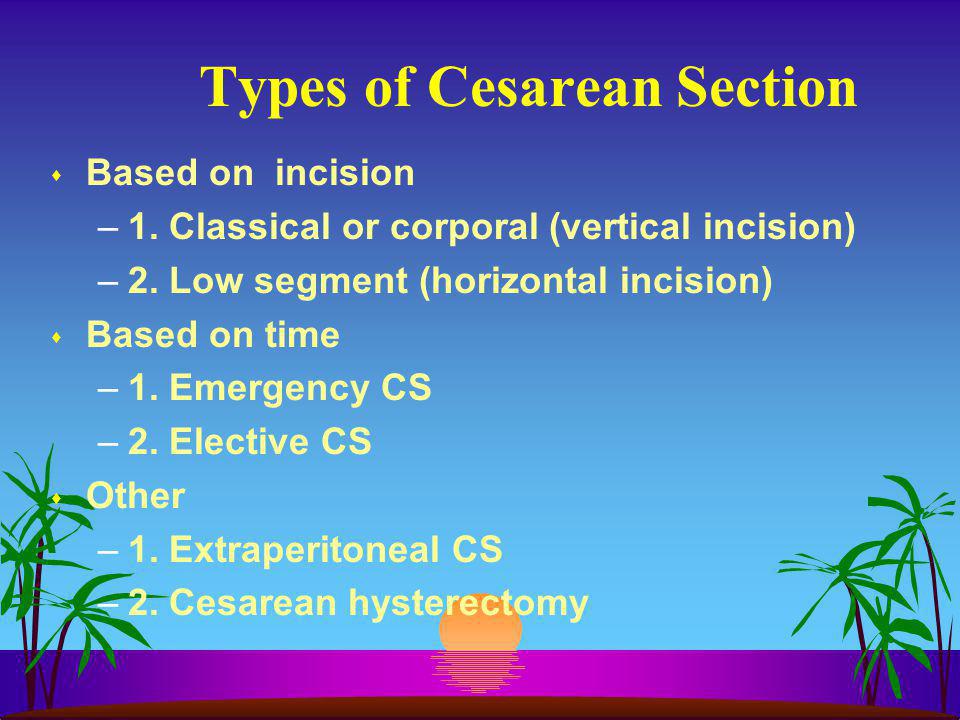
Pain relief during an emergency caesarean section . Since the current situation requires an early resolution, methods of anesthesia are used that can be implemented as soon as possible. That is why for pain relief during emergency caesarean section operations, the so-called GENERAL ANESTHESIA is used more often than during planned operations. At the same time, the woman is in an unconscious state, an apparatus for artificial respiration is used.
Since epidural anesthesia takes 15 to 30 minutes to relieve pain, in emergency operations this method of anesthesia is used only when the catheter has been inserted into the space above the dura mater, even during childbirth. In this case, the woman remains conscious.
SPINAL ANESTHESIA may be used during emergency surgery. With this method, as with epidural anesthesia, an injection is made in the back in the lumbar region, the anesthetic is injected into the spinal space. Anesthesia begins to work within the first 5 minutes, which allows you to quickly start the operation. As with epidural anesthesia, only the lower part of the body is anesthetized, the woman remains conscious.
As with epidural anesthesia, only the lower part of the body is anesthetized, the woman remains conscious.
Natalia Epifanova, obstetrician-gynecologist, PhD
Magazine "9 Months", 2004, No. 7. www.9months.ru
Up Features of the operation ›
Caesarean section: only when necessary | Blog
Most pregnant women want natural childbirth, but there are mothers-to-be who are so afraid of pain that they prefer a caesarean section.
Is it possible to do this operation "at will"?
Indeed, there was a period of literally "fashion" for caesarean section, and this trend was observed in many developed countries of the world: women preferred birth through caesarean sections because of the fear of painful natural childbirth.
However, like any operation, caesarean section is associated with certain risks, after which a recovery period is required, so doctors do not recommend caesarean section without indications from the mother or child.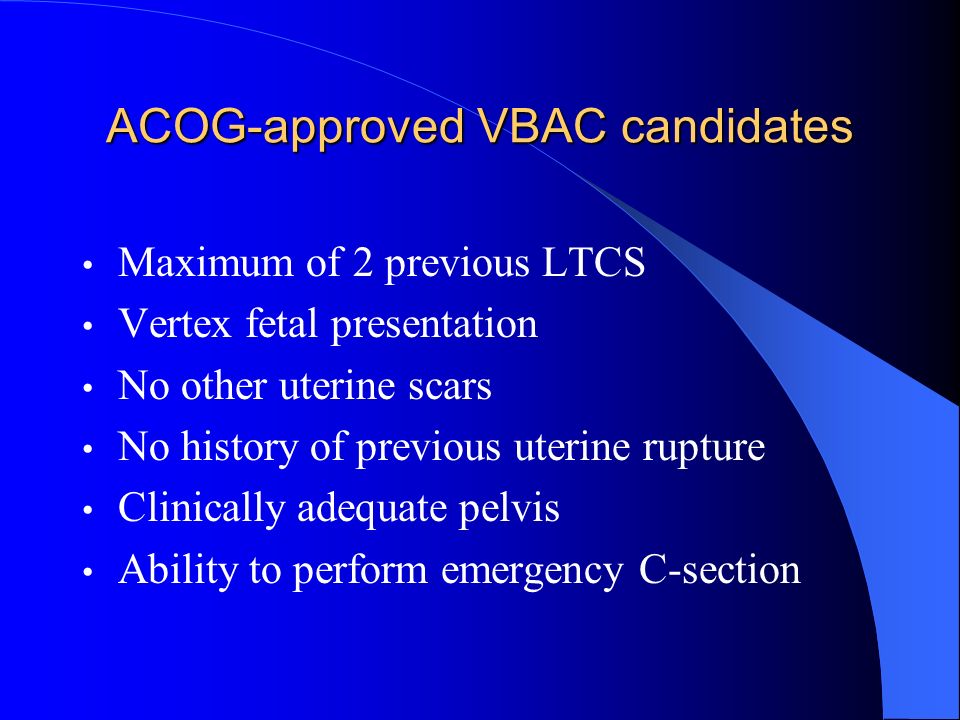
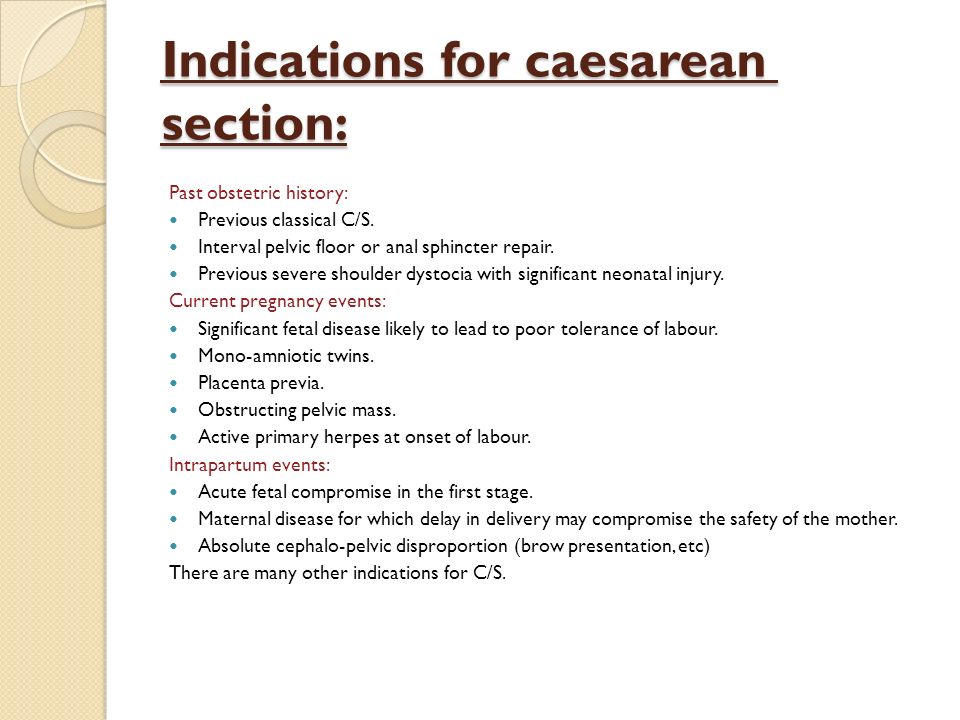
Elective caesarean section performed at:
- Multiple pregnancy;
- Previa or placental abruption;
- Narrow pelvis pregnant;
- An inconsistent scar on the uterus from a previous caesarean section or other operations;
- Deformed pelvic bones, tumors, malformations of the uterus or vagina;
- Large fetal mass, transverse fetal position;
- Severe forms of gestosis, cardiovascular diseases, oncological neoplasms of any localization;
- Risk of retinal detachment and rupture during attempts.
Indications for emergency caesarean section:
- Absence of labor activity after premature discharge of amniotic fluid and lack of response to its stimulation, weakness of labor activity;
- Oxygen starvation (hypoxia) of the fetus;
- Placental abruption and other causes.
Often, a caesarean section is performed for a combination of several indications. The fact that pregnancy resulted from IVF is not in itself an indication for a caesarean section!
The fact that pregnancy resulted from IVF is not in itself an indication for a caesarean section!
All cases involving planned and emergency caesarean section are provided for in the Order of the Ministry of Health of Ukraine No. 997 dated 12/27/2011 "Clinical protocol for obstetric care" Caesarean section ".
How is caesarean section anesthetized? epidural anesthesia.The woman is conscious, the child, after removal from the uterine cavity, is given to the father or another close person who can be present at the birth of the child by caesarean section (unless, of course, there is a need for resuscitation for the newborn).0003
Usually a day after the operation, a young mother stays in the postoperative department, and then in the postpartum ward with her newborn baby.
He has been taking painkillers and antibiotic therapy for several days. However, this is not a contraindication for breastfeeding - it is recommended to apply the baby to the breast as soon as possible after the caesarean section, usually on the second day after it.
As already mentioned, caesarean section is associated with risks for the mother and the newborn. For the mother, this is the risk of repeated surgical interventions, the likelihood of a planned cesarean section during the next birth, as well as such rare complications as bladder damage, damage to the ureter, and some others.
Immediately after surgery, a woman naturally complains of pain, 9% of new mothers experience pain in the wound area for several months after surgery, there is a higher risk of blood loss and infection. For babies born by caesarean section, the most common complications are respiratory disorders (3.5%) and skin lesions (2%).
On average, 12-27% of deliveries in Ukrainian maternity hospitals are performed by caesarean section. All of them are done according to absolute or relative indications. If at some point a woman feels that a caesarean section is a way to avoid pain during childbirth, doctors offer a safer solution: natural labor pain relief.