How to tell if your child is emotionally disturbed
Does My Child Have an Emotional or Behavioral Disorder?
What To Look For
Among all the dilemmas facing a parent of a child with emotional or behavioral problems, the first question — whether the child’s behavior is sufficiently different to require a comprehensive evaluation by professionals — may be the most troublesome of all. Even when a child exhibits negative behaviors, members of a family may not all agree on whether the behaviors are serious.
For instance, children who have frequent temper outbursts or who destroy toys may appear to have a serious problem to some parents, while others see the same behavior as asserting independence or showing leadership skills.
Every child faces emotional difficulties from time to time, as do adults. Feelings of sadness, loss, or emotional extremes are part of growing up. Conflicts between parents and children are also inevitable as children struggle from the “terrible twos” through adolescence to develop their own identities. These are normal changes in behavior due to growth and development. Such problems can be more common in times of change for the family, such as the death of a grandparent or family member, a new child, or a move. Generally, these kinds of problems tend to fade on their own or with limited visits to a counselor or other mental health professional as children adjust to the changes in their lives.
At times, however, some children may develop inappropriate emotional and behavioral responses to situations in their lives that persist over time. The realization that a child’s behavior requires professional attention can be painful or frightening to parents who have tried to support their child, or it may be accepted and internalized as a personal failure by the parent.
Sometimes parents fear that their child may be inappropriately labeled. They have concerns that the array of medicines and therapies suggested are not always agreed upon by all professionals. Still others become alarmed after obtaining an evaluation for their child only to discover that the evaluator believed emotional disturbances originate in family dynamics and that “parenting skills” classes were the best way to address the problem.
While many parents will concede that they may need to learn new behavior management or communication techniques in order to provide a consistent and rewarding environment for their child, many also express deep anger about the blame that continues to be placed on families with children who behave differently.
Where To Start
Before seeking a formal mental health evaluation, parents may have tried to help their child by talking to friends, relatives, or the child’s school. They may try to discover whether others see the same problems and to learn what others suggest. Parents may feel that they also need help in learning better ways of supporting the child through difficult times and may seek classes to help them sharpen behavior management or conflict resolution skills. Modifications in a child’s routine at home or school may help to establish whether some "fine tuning” will improve performance or self-esteem.
If the problems a child is experiencing are seen as fairly severe and are unresponsive to interventions at school, in the community, or at home, a diagnostic evaluation by a competent mental health professional is probably in order. Evaluations provide information that, when combined with what parents know, may lead to a diagnosis of a mental health, emotional, or a behavioral disorder.
Evaluations provide information that, when combined with what parents know, may lead to a diagnosis of a mental health, emotional, or a behavioral disorder.
So what is that magical moment when parents should recognize their child’s behavior has surpassed the boundary of what all children do and has become sufficiently alarming to warrant a formal evaluation? There probably isn’t one. It is often a gradual awareness that a child’s emotional or behavioral development just isn’t where it should be that sends most parents on a quest for answers.
Perhaps the most important question of all for parents of school-age children to consider is, “How much distress is your child’s problem causing you, the child, or other members of the family?” If a child’s aggressive or argumentative behaviors, or sad or withdrawn behaviors are seen as a problem for a child, the school, or members of his or her family, then the child’s behaviors are a problem that should be looked at, regardless of their severity.
While there is no substitute for parental knowledge, certain guidelines are available to help families make the decision to seek an evaluation. In Help for Your Child: A Parent’s Guide to Mental Health Services, Sharon Brehm suggests three criteria to help in deciding whether a child’s behavior is normal or a sign that the youngster needs help:
- Duration of a troublesome behavior. Does it just go on and on with no sign that the child is going to outgrow it and progress to a new stage?
- Intensity of a behavior. While temper tantrums are normal in almost all children, some tantrums could be so extreme that they are frightening to parents and suggest that some specific intervention might be necessary. Parents should pay particular attention to their child’s feelings of despair or hopelessness; lack of interest in family, friends, school or other activities once considered enjoyable; or behaviors that are dangerous to the child or to others.
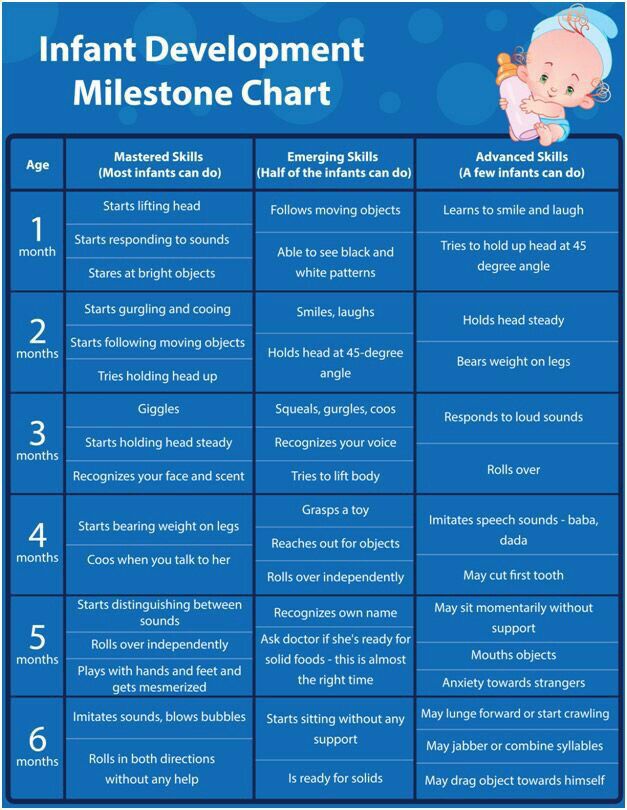
- Age of the child. Some behavior might be quite normal for a two-year-old, but observation of other children that age may lead to the conclusion that the behavior in question is not quite right for a five-year-old. Not all children reach the same emotional milestones at the same age, but extreme deviations from age-appropriate behaviors may well be cause for concern.
Attempts at self-injury or threats of suicide, violent behaviors, or severe withdrawal that creates an inability to carry on normal routines must be regarded as emergencies for which parents should seek immediate attention, through a mental health or medical clinic, mental health hotline, or crisis center.
Parents will also want to consider whether their child’s behavior could be influenced by other factors, such as:
- a specific physical condition (allergies, hearing problems, change in medication, etc.) that could be affecting the behavior;
- school problems (relationships or learning problems) that are creating additional stress;
- experimenting with drug use or alcohol for an adolescent or older teen; or
- changes in the family (divorce, new child, death) that may cause concern for the child.

Young Children
Special consideration needs to be given to identifying behaviors of concern in very young children. Their well-being is so connected with that of the family, that services must be developed with and directed to the family as a unit. The goal in evaluating and providing services to a young child should include helping families to articulate their own stresses and strengths. It is in the context of family that a child first explores his or her world, and learns to adapt to the varied demands of families and the world at large.
Historically, many professionals have been cautious to have a child “labeled and judged” at an early age because children are in a developmental period. On the other hand, the earlier that parents and professionals can intervene in the life of a young child with delays in emotional and behavioral development, the better it is for both the child and the family.
Early evaluation and intervention requires that parents be involved in both giving and receiving information about their child’s development.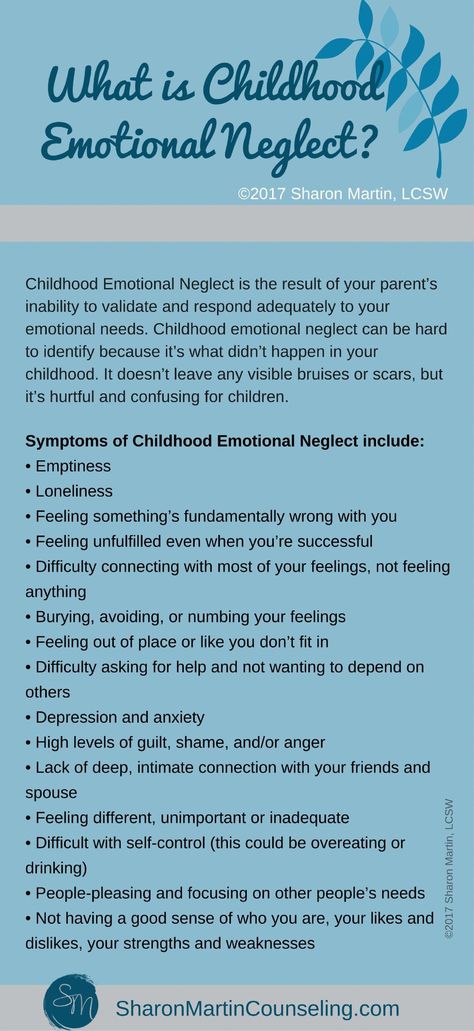 Interviews with families and observations of their child to assess how well he or she communicates, plays, relates to peers and adults, and is able to self-regulate behavior is useful in deciding whether the child has a developmental problem that needs attention.
Interviews with families and observations of their child to assess how well he or she communicates, plays, relates to peers and adults, and is able to self-regulate behavior is useful in deciding whether the child has a developmental problem that needs attention.
Most often, the first indications that an infant may be experiencing significant problems will be delays in normal development. An infant who is unresponsive to his or her environment (doesn’t show emotion such as pleasure or fear that is developmentally appropriate, doesn’t look at or reach for objects, or doesn’t respond to environmental changes such as sound or light), who is over responsive (easily startled, cries), or who shows weight loss or inadequate weight gain that is not explainable by a physical problem (failure to thrive), should have a thorough evaluation.
If parents have questions about their child’s development, they should call their child’s pediatrician or family physician. Many doctors who include young children in their practice will have materials available for parents on normal childhood development.
Toddlers may have a tremendous range of behaviors that would be considered developmentally appropriate. However, any significant delays (six months or more) in language development, motor skills, or cognitive development should be brought to the attention of the child’s pediatrician.
Children who become engrossed in self-stimulating behavior to the exclusion of normal activities or who are self-abusive (head banging, biting, hitting), who do not form affectionate relationships with care providers, such as regular babysitters or relatives they see often, or who repeatedly hit, bite, kick or attempt to injure others should be seen by their pediatrician or family physician and, if indicated, by a competent mental health professional.
Especially with a first child, parents may feel uneasy, uncomfortable, or even foolish about seeking an evaluation for their very young child. While sorting out problems from developmental stages can be quite tricky with infants and toddlers, early identification and intervention can significantly reduce the effects of abnormal psychosocial development. Careful observation of infants and toddlers as they interact with caregivers, their family, or their environment is one of the most useful tools that families or physicians have, since many mental health problems cannot be diagnosed in any other way.
Careful observation of infants and toddlers as they interact with caregivers, their family, or their environment is one of the most useful tools that families or physicians have, since many mental health problems cannot be diagnosed in any other way.
The Individuals with Disabilities Education Act of 2004 (IDEA) requires states to provide services for children from ages 3 through 21 who have disabilities. The section of the law that covers children birth through 2 is called Part C and recognizes the importance of families in meeting the needs of their young children. It requires that each state plan to provide early intervention services in collaboration with the main service providers for young children: human services, health, and education.
As of this writing, all states are receiving funds to provide services to infants and toddlers. Parents who have questions related to preschool or early intervention programs should call their local school district offices or their state Department of Education or Department of Health or Human Services for guidance.
Cultural Considerations
Evaluation of a child’s mental or emotional status is the key to developing appropriate school or mental health services. For children who are from diverse cultures, parents will want to know how, or if, those differences will affect evaluation results.
Tests, by their very nature, have been developed to determine differences between one child and another. If everyone taking a test scored the same, then the test would be of no use. What’s important, though, is that tests are used only in those areas they were designed to measure — such as depression or anxiety.
If the professional who is responsible for evaluation is not of the same cultural background as the child, parents should feel free to ask what his or her experiences have been in cross-cultural assessment or treatment. Professionals who are sensitive to issues of bias related to language, socioeconomic status, or culture in formal evaluation tools should willingly share such information with parents.
One way of minimizing the effects of cultural bias in obtaining an appropriate diagnosis is to use a multidisciplinary approach to evaluation involving persons from different backgrounds (teacher, therapist, parent, and social worker) in completing the evaluation. Several questions to consider are:
- Do the data and conclusions from various professionals agree?
- Did the professionals use family information about the child’s functioning at home and in the community to aid in making a diagnosis?
- Does the family believe the evaluation is accurate?
When a multidisciplinary approach is not practical or available, the person providing the evaluation should give the battery of tests following the procedures to reduce the effects of bias when making a determination that a child needs mental health services.
If children from specific ethnic or cultural groups appear to be overrepresented in a school or treatment program that has been selected or recommended for a child, parents should carefully examine the procedures for determining their child’s placement.
If parents decide that the placement decision was not influenced by racial or cultural bias, that perspective can increase confidence in the program selected for their child.
Seeking a Diagnostic Evaluation From a Medical Professional
Once parents have decided that their child or adolescent has behaviors that deserve at least a look by a medical professional, the question then becomes where to turn for a diagnostic evaluation.
A family doctor can rule out physical health issues, perform a basic mental health screening, and refer families to an appropriate child or adolescent psychologist, or psychiatrist. Also, many hospitals and most community mental health centers offer comprehensive diagnostic and evaluation programs for children and adolescents.
School districts also do mental health screenings during kindergarten roundup, and the results from that screening might help you decide to move forward with contacting your child’s pediatrician or another medical provider for a diagnostic evaluation.
Evaluations can be costly, but there are some supports available for families. Check with your insurance company to see if they will cover all or a portion of the costs of an evaluation, or Medical Assistance (Medicaid) may cover costs for eligible families.
Under the Affordable Care Act, marketplace health plans must cover preventative services for children at no charge, which includes behavioral assessments. For children eligible for Medicaid (Medical Assistance in Minnesota), the Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Program provides preventive health care, including screening (evaluation), diagnosis, and appropriate mental health services.
Under EPSDT, a screening is a comprehensive health evaluation, including the status of a child’s emotional health. A child is entitled to periodic screenings, or an inter-periodic screening (between normal screening times), whenever a physical or emotional problem is suspected, and to receive health services to address such problems from any Medicaid provider (public or private). Check with your state Medicaid office to get current information about the services under the EPSDT program.
Check with your state Medicaid office to get current information about the services under the EPSDT program.
Other parents, particularly those in rural areas, may want to first approach their county’s public health nurse, or family and human services agency. Either may be able to direct them to an evaluation program available in their area.
Community mental health centers are also a good source of help, and can be less expensive than seeking out a private doctor or mental health professional. Parents will want to ask for professional staff with experience in evaluating the mental health needs of children. If in doubt, ask for the credentials and expertise of the professional who is assigned to work with the child. Credentials should be offered and displayed in the professional’s workplace.
School-Linked Mental Health Services
Children and youth in Minnesota may have access to mental health supports at school through school-linked mental health services. It is not a requirement in Minnesota for schools to provide these services, but a grant program from the Children’s Mental Health Division at the Minnesota Department of Human Services has given some schools the opportunity to partner with community-based mental health providers so that students can have access to services at school. This partnership offers easier access for early intervention and treatment to prevent more serious mental illness, and offers students support in a natural, non-stigmatizing setting.
This partnership offers easier access for early intervention and treatment to prevent more serious mental illness, and offers students support in a natural, non-stigmatizing setting.
School-linked mental health services
Seeking a Free Comprehensive Special Education Evaluation for Services at School
There are federal and state laws that require certain services in school for children who have disabilities. The Individuals with Disabilities Education Act of 2004 (IDEA) is the federal law that addresses early intervention services for young children, as well as for school-age children who have disabilities. If your child needs more supports or services to help them be a successful learner, consider requesting an evaluation for special education from your school administrator.
The process of evaluation starts with Child Find, a process that requires schools to identify, locate, and evaluate students with disabilities who may need special education services and supports. An evaluation for special education is not the same as a diagnostic evaluation. A comprehensive special education evaluation determines if the student is in need of special education services (specially designed instruction and related services, and any necessary accommodations) due to their disability.
An evaluation for special education is not the same as a diagnostic evaluation. A comprehensive special education evaluation determines if the student is in need of special education services (specially designed instruction and related services, and any necessary accommodations) due to their disability.
If the child is determined to meet the criteria as a child with a disability under IDEA, the school will put together a team, which includes the parent, to develop and write an Individualized Education Plan (IEP). This is a legal agreement between the school district and the child and their parent(s) for the provision of special education services.
If the child is not determined to meet the criteria as a child with a disability under IDEA, parents may want to consider a 504 Plan. Section 504 of the Rehabilitation Act of 1973 is a federal civil rights law that says it is not legal to discriminate against people with disabilities in any program receiving federal funds.
In school, Section 504 can help children and youth who have a mental health or emotional disorder but are not eligible for special education. Schools must first determine whether the child’s impairment substantially limits their ability to learn, and then provide accommodations for that child. Accommodations can include such things as giving extra time to complete work, using headphones or going to a quiet place to help screen out noise. Section 504 helps children to succeed in the activities that are available to all students.
Schools must first determine whether the child’s impairment substantially limits their ability to learn, and then provide accommodations for that child. Accommodations can include such things as giving extra time to complete work, using headphones or going to a quiet place to help screen out noise. Section 504 helps children to succeed in the activities that are available to all students.
Signs of an Emotionally Disturbed Kid
TAMIYA KING
CLASS
Emotional disturbance is a condition that can sometimes mimic depression in children, and is recognized by the U.S. Department of Education as an educational disability. There are several behavioral and emotional indicators that a child is emotionally disturbed, and it's essential for parents and teachers to monitor these children closely to determine if the symptoms indicate other serious conditions.
Explore this article
- Aggressive Behavior
- Changes in Appetite
- Low Test Scores
- Loss of Energy and Interest in Activities
1 Aggressive Behavior
A child who is emotionally disturbed will likely exhibit aggressive behavior, and will often attempt to hurt others. According to the Sevier County Public School System, aggression is the symptom reported most commonly in children who are emotionally disturbed. A child's action often involves hitting or kicking other students, getting up from assigned seating even after being instructed repeatedly to stay seated, and stealing objects from the students or teacher's desk. While occasional aggressive behavior could simply be a sign that a child is unhappy with an isolated incident like moving to a new school or welcoming a new baby, this symptom is considered an emotional disturbance when it takes place over an extended period. The January 2010 issue of the Journal of Clinical Child and Adolescent Psychology also asserts that abused children often experience emotional disturbance and display it through aggressive actions; while little girls behaved equally as aggressive as those who had not been abused, boys who were abused were 50 percent more likely to get into fights, break objects and respond harshly to reprimands.
According to the Sevier County Public School System, aggression is the symptom reported most commonly in children who are emotionally disturbed. A child's action often involves hitting or kicking other students, getting up from assigned seating even after being instructed repeatedly to stay seated, and stealing objects from the students or teacher's desk. While occasional aggressive behavior could simply be a sign that a child is unhappy with an isolated incident like moving to a new school or welcoming a new baby, this symptom is considered an emotional disturbance when it takes place over an extended period. The January 2010 issue of the Journal of Clinical Child and Adolescent Psychology also asserts that abused children often experience emotional disturbance and display it through aggressive actions; while little girls behaved equally as aggressive as those who had not been abused, boys who were abused were 50 percent more likely to get into fights, break objects and respond harshly to reprimands.
2 Changes in Appetite
When a child begins eating much more or less than normal, this could be an indication of emotional disturbance, according to the Anne Arundel County Public School System. If this significant change in a child's eating habits begins to affect his educational performance, the symptom is considered a sign of emotional disturbance. For instance, poor nutrition will affect a child's ability to concentrate and absorb information. If a young student is eating too frequently, he may disrupt the class in the middle of instruction to demand food. Children may turn to food for comfort or avoid eating if they've lost interest in meal time. This could also be an indicator of depression. Again, if shifts in a child's appetite become constant, this means she is emotionally disturbed and counseling or treatment is necessary.
3 Low Test Scores
When a child scores significantly low on assessments designed to measure age-appropriate aptitude and comprehension, this can point to emotional disturbance. The Sevier County Public School District asserts that only 30 percent of emotionally disturbed children pass grade-level achievement tests on an average level. Data collected by the school district also asserts that in Florida 50 percent of students were not able to pass a functional test and 75 percent of emotionally disturbed teens failed the high school math competency test. The U.S. Office of Education estimates that around 2 percent of the student population suffers from emotional disturbance and are prone to these low test scores.
The Sevier County Public School District asserts that only 30 percent of emotionally disturbed children pass grade-level achievement tests on an average level. Data collected by the school district also asserts that in Florida 50 percent of students were not able to pass a functional test and 75 percent of emotionally disturbed teens failed the high school math competency test. The U.S. Office of Education estimates that around 2 percent of the student population suffers from emotional disturbance and are prone to these low test scores.
4 Loss of Energy and Interest in Activities
A child who is continually tired and no longer wants to participate in activities that she once enjoyed may be experiencing these symptoms because of emotional disturbance. When this lethargy or lack of interest affects academic performance and can't be attributed to a health condition or clinical depression, it is one sign of emotional disturbance. A child who exhibits this constant aversion to interactive activities like sports or crafts, or is always complaining of fatigue will likely exhibit withdrawn behavior and become disinterested in playing or talking to other students. This emotional disturbance sign could also be a sign of autism, so it's best to visit a behavior counselor with your child to have your little one further assessed and determine treatment.
This emotional disturbance sign could also be a sign of autism, so it's best to visit a behavior counselor with your child to have your little one further assessed and determine treatment.
references
- 1 NICHCY: Emotional Disturbance
- 2 Sevier.org: Definition of Seriously Emotionally Disturbed
About the Author
Tamiya King has been writing for over a decade, particularly in the areas of poetry and short stories. She also has extensive experience writing SEO and alternative health articles, and has written published interviews and other pieces for the "Atlanta Tribune" and Jolt Marketing. She possesses a Bachelor of Arts in English and is currently pursuing higher education to become a creative writing professor.
Related Articles
Emotional imbalance
Emotional imbalance Children are much more susceptible to mood swings than adults.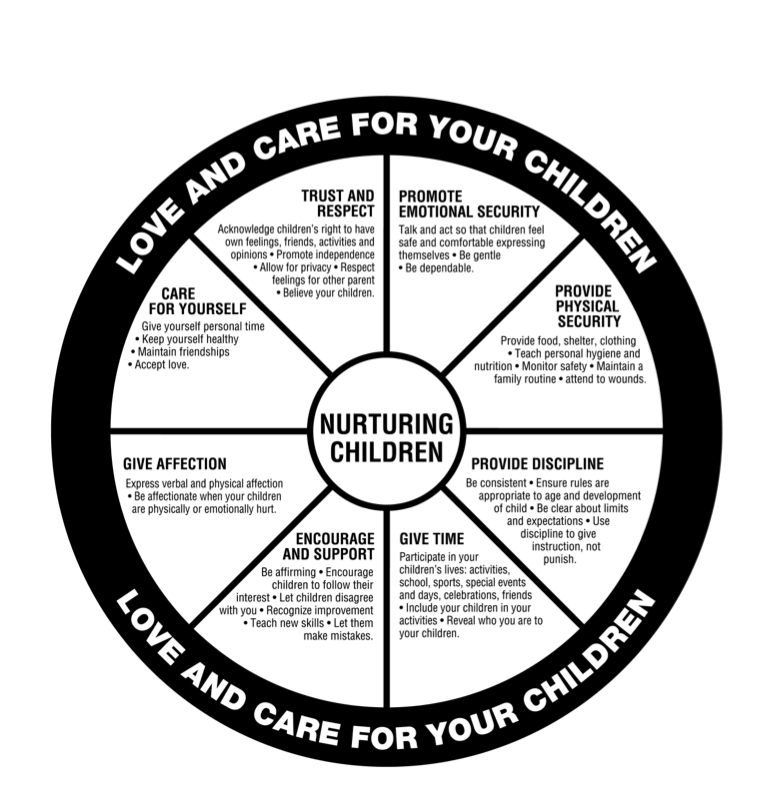 It is easy to cheer them up, but it is even easier to upset or offend them, since they almost completely do not yet know themselves and do not know how to control themselves. That is why they are able to experience a whole gamut of feelings and excitement in an unusually short period of time. A child who rolls on the floor with laughter may suddenly burst into tears or despair, and a minute later, with eyes still wet, laugh again contagiously. This behavior of children is completely normal. Besides, they have good days and bad days, just like we do. A child can be calm and thoughtful today or capricious and whimpering, and the next day - lively and cheerful. Sometimes we can explain his bad mood by fatigue or moving to a new place, upsets in kindergarten, malaise, jealousy of his younger brother ... In other words, we understand that his long-term bad mood is caused by anxiety due to some specific circumstance , and although we try our best to help the child get rid of him, it often happens that the feelings of the baby cause us complete bewilderment.
It is easy to cheer them up, but it is even easier to upset or offend them, since they almost completely do not yet know themselves and do not know how to control themselves. That is why they are able to experience a whole gamut of feelings and excitement in an unusually short period of time. A child who rolls on the floor with laughter may suddenly burst into tears or despair, and a minute later, with eyes still wet, laugh again contagiously. This behavior of children is completely normal. Besides, they have good days and bad days, just like we do. A child can be calm and thoughtful today or capricious and whimpering, and the next day - lively and cheerful. Sometimes we can explain his bad mood by fatigue or moving to a new place, upsets in kindergarten, malaise, jealousy of his younger brother ... In other words, we understand that his long-term bad mood is caused by anxiety due to some specific circumstance , and although we try our best to help the child get rid of him, it often happens that the feelings of the baby cause us complete bewilderment.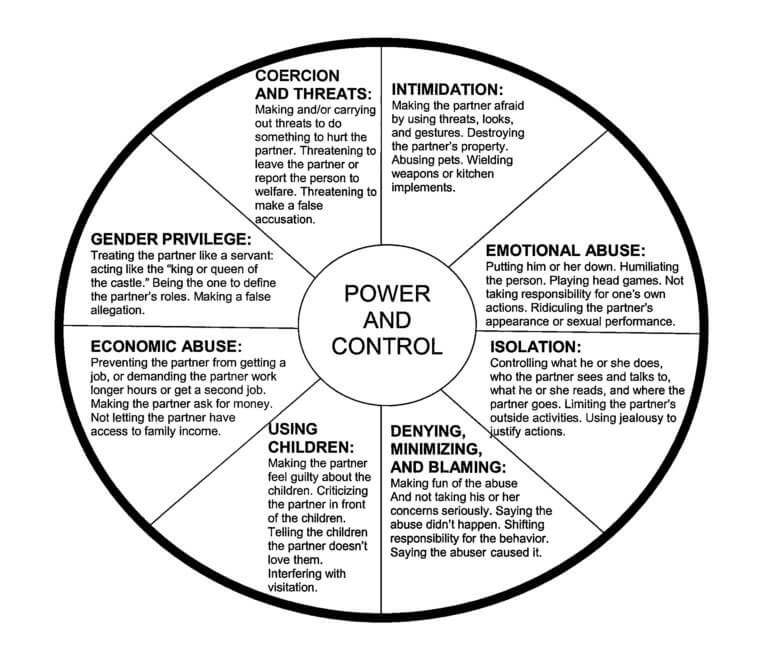
The fact is that no one can fully explain such emotional imbalance in children. Therefore, as long as the bad mood does not drag on for a long time - for example, for several days - and does not cross any boundaries, there is no need to worry. But if the child is in a depressed state for a very long time or abrupt and unexpected changes occur to him, it is better to seek the advice of a psychologist. If something constantly bothers the child, the specialist will be able to explain what we should do. If, on the contrary, everything is in order, he will calm us down and we will stop worrying. In general, it is better not to attach too much importance to changes in his mood and let the child find emotional stability on his own.
My daughter (she is six years old) is characterized by frequent mood swings and unreasonable tantrums. What should I do, should I seek help from a specialist?
It is very important that your daughter's emotional state be well. But in our time, more and more children are experiencing trouble in the emotional sphere. These include manifestations of aggressiveness, uncontrollability or anxiety, insecurity, a tendency to fear, isolation.
But in our time, more and more children are experiencing trouble in the emotional sphere. These include manifestations of aggressiveness, uncontrollability or anxiety, insecurity, a tendency to fear, isolation.
A direct consequence of high anxiety can be emotional imbalance: non-stop laughter or a stream of tears ... Very often these manifestations of emotional imbalance are aggravated precisely by experiencing the crisis of seven years. The child strives to become an adult, to participate in the life of adults, but does this in ways that are not quite adequate. Often he simply does not know how to prove himself in a new “adult” capacity, hence the “endless” tantrums, fits of uncontrollable laughter and other similar reactions. We, adults, strive in every possible way to suppress these manifestations and most often use shouting, reproaches, and punishments for this. As a result, until recently, such a sincere and direct child faces a wall of misunderstanding and, as a result, is increasingly moving away from his parents.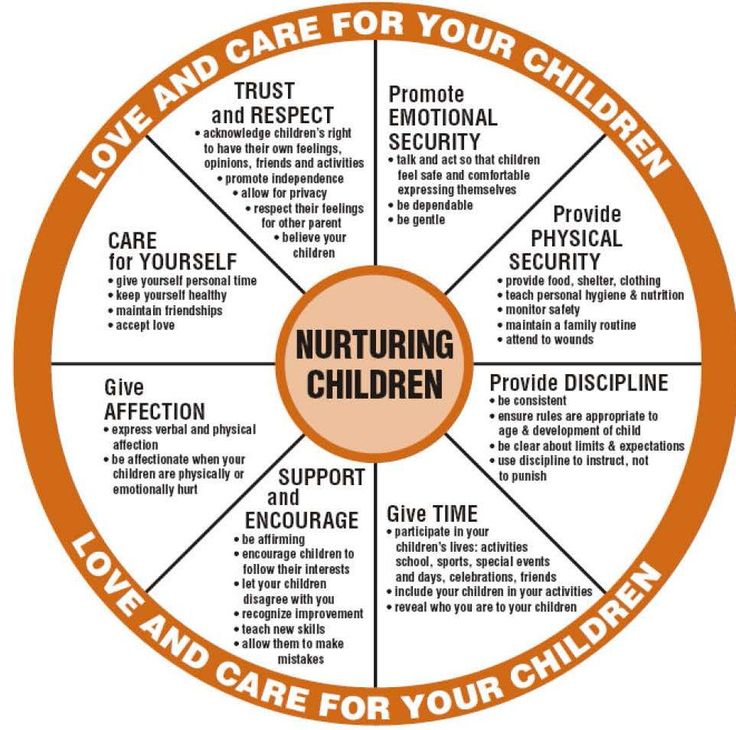
Recommendations to help improve interaction with a restless child:
- during the manifestation of strong emotions, try to distract him. To do this, you can offer him some interesting activity, ask an unexpected question;
- during an attack, take the child to the mirror and show how ugly the one who grimace or sobs looks;
- during an attack, do not lecture the child - he still does not hear you;
- try not to categorically forbid the child to do what he wants, but discuss and decide together whether it is possible to behave the way he wants; watch the tone of the presentation of demands or prohibitions, it should be friendly and explanatory, not imperative; try to always listen carefully to the child. If you can't hear him, he won't hear you either.
See book for details Korobitsyna E. V. Formation of positive relationships between parents and children aged 5-7 years: diagnostics, trainings, classes [Text]. - Volgograd: Teacher, 2009. - 133 p.
Shapiro EI 10 causes of bad behavior in children. Series “Oh, these kids! Secrets of education " [Text]. - St. Petersburg: Litera, 2012. - 64 p.
Danilina T.A., Zedgenidze V.Ya., Stepina N.M. In the world of children's emotions [Text]. – M.: Iris Press, 2004. – 16 p.
Yakovleva N.G. Psychological assistance to preschoolers. A book for parents and educators [Text]. - M.: Sphere, 2002. - 108 p.
Emotional disorders in children - ProMedicina Ufa
The child's emotions are connected with his inner world and various social situations, the experience of which causes him certain emotional states. As a result of a violation of social situations (changes in the daily routine, lifestyle, etc.), a child may experience a stressful state, affective reactions, and fear. This causes the negative well-being of the child, emotional distress.
Causes
Child psychologists believe that the main causes of emotional disorders in children can be: illnesses and stresses suffered in childhood; features of the physical and psycho-emotional development of the child, including delays, impairments or lags in intellectual development; microclimate in the family, as well as features of education; social and living conditions of the child, his close environment. Emotional disorders in children can also be caused by other factors. For example, films that he watches or computer games that he plays can cause psychological trauma to a child's body. Emotional disturbances in children appear most often in critical periods of development. A vivid example of such mentally unstable behavior is the so-called "transitional age".
Emotional disorders in children can also be caused by other factors. For example, films that he watches or computer games that he plays can cause psychological trauma to a child's body. Emotional disturbances in children appear most often in critical periods of development. A vivid example of such mentally unstable behavior is the so-called "transitional age".
Types of emotional disturbances
Euphoria - inadequately elevated, joyful mood. A child in a state of euphoria is characterized as impulsive, striving for dominance, impatient.
Dysphoria is a mood disorder, with a predominance of angry-dreary, gloomy-dissatisfied, with general irritability and aggressiveness. A child in a state of dysphoria can be described as sullen, angry, harsh, unyielding. Dysphoria is a type of depression.
Depression, in turn, is an affective state characterized by a negative emotional background and general passivity of behavior. A child with a low mood can be described as unhappy, gloomy, pessimistic.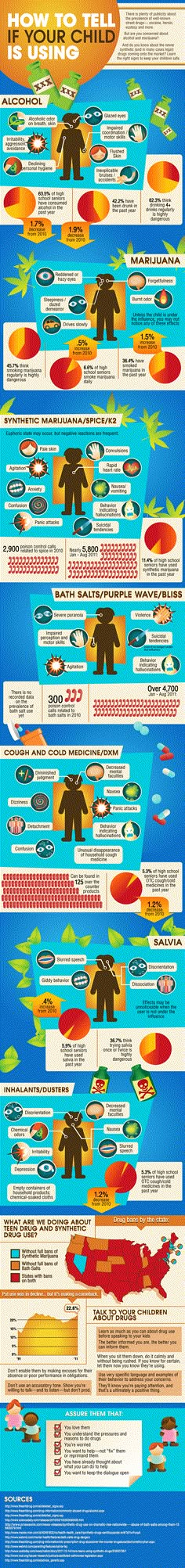
Anxiety syndrome is a state of causeless anxiety, accompanied by nervous tension, restlessness. An anxious child can be defined as insecure, constrained, tense. This syndrome is expressed in frequent mood swings, tearfulness, decreased appetite, thumb sucking, touchiness and sensitivity. Anxiety often turns into fears (phobias).
Fear is an emotional state arising from the realization of impending danger - imaginary or real. A child experiencing fear looks timid, frightened, withdrawn.
Apathy - an indifferent attitude to everything that happens, which is combined with a sharp drop in initiative. With apathy, the loss of emotional reactions is combined with the defeat or absence of volitional impulses. Only with great difficulty can one briefly disinhibit the emotional sphere, promote the manifestation of feelings.
Emotional dullness - characterized not only by the absence of emotions (for adequate or inadequate stimuli), but also by the impossibility of their appearance at all. The introduction of stimulant drugs leads to temporary non-objective motor excitation, but not to the appearance of feelings or contact.
The introduction of stimulant drugs leads to temporary non-objective motor excitation, but not to the appearance of feelings or contact.
Parathymia or inadequacy of emotions is a mood disorder in which the experience of one emotion is accompanied by an external manifestation of an emotion of the opposite valence. It should be noted that both parathymia and emotional dullness are characteristic of children with schizophrenia.
Attention deficit hyperactivity disorder (ADHD) is a combination of general motor restlessness, restlessness, impulsive behavior, emotional lability, and impaired concentration. It follows that the main features of this syndrome are distractibility of attention and motor disinhibition. Thus, a child suffering from ADHD is restless, does not complete the work he has begun, his mood quickly changes.
Aggression is a kind of provocative behavior aimed at attracting the attention of adults or peers. It can be physical, verbal (obscene language), indirect (displacement of an aggressive reaction to an outside person or object). It can manifest itself in the form of suspicion, resentment, negativism, feelings of guilt.
It can manifest itself in the form of suspicion, resentment, negativism, feelings of guilt.
In addition to the indicated groups of emotional disorders, emotional difficulties in communication can also be distinguished. They are represented in children by autistic behavior and difficulties in adequately determining the emotional states of people.
Treatment
Emotional disorders in children are treated in the same way as in adults: a combination of individual, family psychotherapy and pharmacotherapy gives the best effect.
The leading method of correcting emotional disturbances in childhood is the imitation of various emotional states by children. The significance of this method is due to a number of features:
1) active facial and pantomimic manifestations help prevent some emotions from developing into pathologies;
2) thanks to the work of the muscles of the face and body, an active discharge of emotions is ensured;
3) in children with voluntary reproduction of expressive movements, the corresponding emotions are revived and vivid memories of previously unreacted experiences can arise, which, in some cases, makes it possible to find the root cause of the child's nervous tension and level his real fears.