Down syndrome markers third trimester
Sonographic identification of fetuses with Down syndrome in the third trimester: a matched control study
. 1999 May;93(5 Pt 1):702-6.
doi: 10.1016/s0029-7844(98)00492-x.
A C Ranzini 1 , E R Guzman, C V Ananth, D Day-Salvatore, A J Fisher, A M Vintzileos
Affiliations
Affiliation
- 1 The Center for Perinatal Health Initiatives, Department of Obstetrics, Gynecology, and Reproductive Sciences, University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School/St. Peter's Medical Center, New Brunswick, USA.
- PMID: 10912971
- DOI: 10.
1016/s0029-7844(98)00492-x
A C Ranzini et al. Obstet Gynecol. 1999 May.
. 1999 May;93(5 Pt 1):702-6.
doi: 10.1016/s0029-7844(98)00492-x.
Authors
A C Ranzini 1 , E R Guzman, C V Ananth, D Day-Salvatore, A J Fisher, A M Vintzileos
Affiliation
- 1 The Center for Perinatal Health Initiatives, Department of Obstetrics, Gynecology, and Reproductive Sciences, University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School/St. Peter's Medical Center, New Brunswick, USA.
- PMID: 10912971
- DOI: 10.
 1016/s0029-7844(98)00492-x
1016/s0029-7844(98)00492-x
Abstract
Objective: To determine sonographic findings in Down syndrome fetuses in the third trimester.
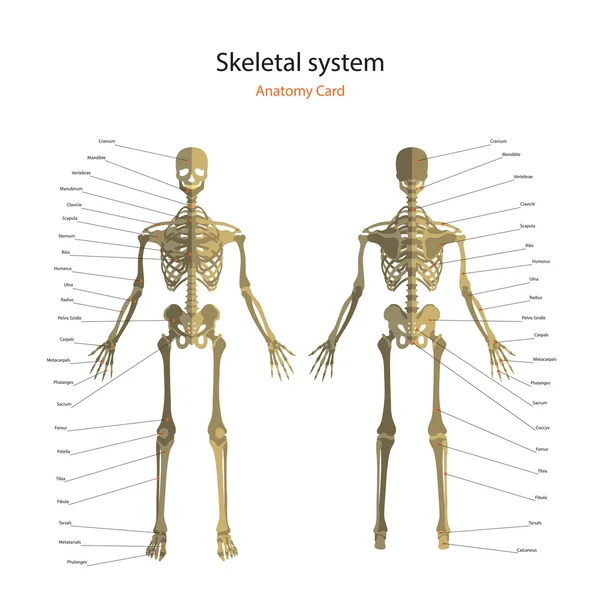
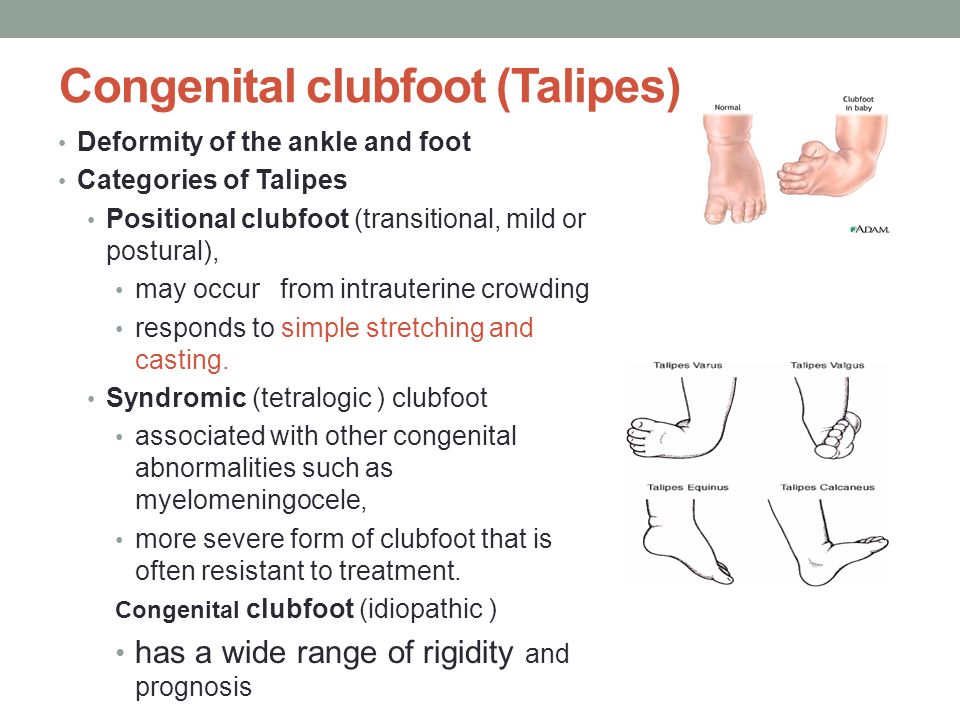
Methods: Down syndrome fetuses who had third-trimester ultrasound examinations between 25 and 41 weeks' gestation were matched for gestational age with three controls each. Fetal structural anomalies, Down syndrome dysmorphology markers (abnormal facial profile, sandal gap, tongue thrusting, clinodactyly, or hypoplastic middle phalanx of the fifth finger), and abnormal long-bone biometry (femur, humerus, tibia, and fibula; femur length to biparietal diameter ratio; and femur length to abdominal circumference ratio were abstracted from the ultrasound reports. The fetal face, hands, feet, profile, and cardiac outflow tracts are routinely evaluated in our center.
Results: Seventeen fetuses with Down syndrome who had third-trimester ultrasound evaluations were identified. Anomalies included cardiac defects (five), tongue thrusting (three), clinodactyly (three), abnormal profile (three), sandal gap (two), and duodenal atresia (two). Of the 17 fetuses, at least one long-bone abnormality was found in 13, at least one structural or biometric anomaly was found in 15, and at least two abnormal findings existed in 11. Abnormal ultrasound findings, including structural anomalies, short bones, and Down syndrome dysmorphology markers, were more common in cases than in matched controls.
Conclusion: At least one abnormal ultrasound finding was present in 15 of 17 fetuses, and abnormal bone measurements or ratios were discovered in 13 of 17. Abnormal long-bone biometry at third-trimester ultrasound should raise the suspicion of fetal Down syndrome.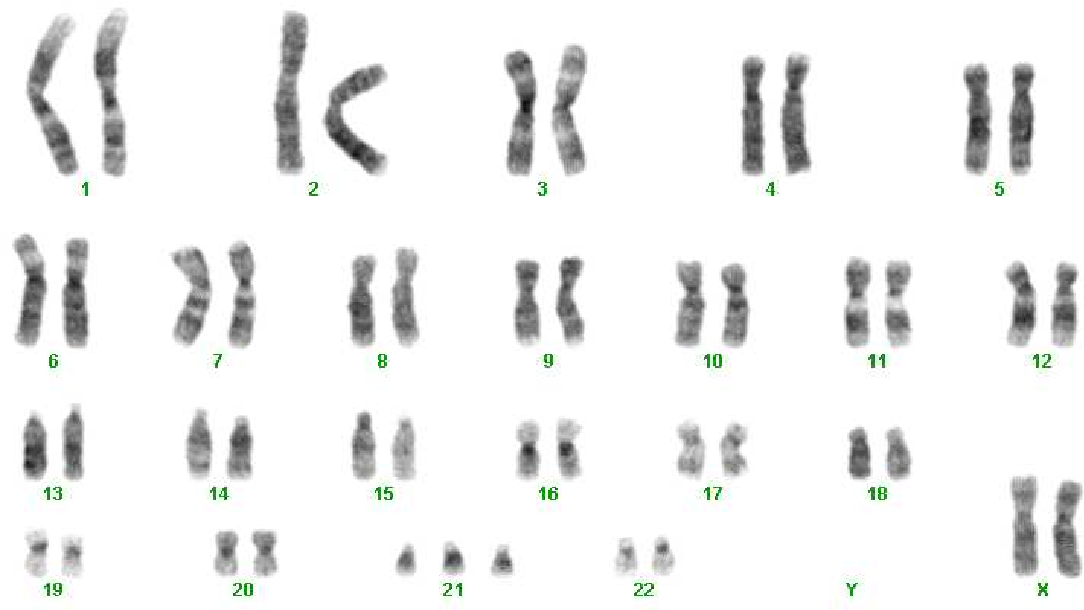
Similar articles
-
The use of second-trimester genetic sonogram in guiding clinical management of patients at increased risk for fetal trisomy 21.
Vintzileos AM, Campbell WA, Rodis JF, Guzman ER, Smulian JC, Knuppel RA. Vintzileos AM, et al. Obstet Gynecol. 1996 Jun;87(6):948-52. doi: 10.1016/0029-7844(96)00053-1. Obstet Gynecol. 1996. PMID: 8649704
-
Prenatal sonographic markers of trisomy 21.
Tongsong T, Wanapirak C, Sirichotiyakul S, Sirivatanapa P. Tongsong T, et al. J Med Assoc Thai. 2001 Feb;84(2):274-80. J Med Assoc Thai. 2001. PMID: 11336089
-
Adjusting the risk for trisomy 21 by a simple ultrasound method using fetal long-bone biometry.
Vintzileos AM, Egan JF, Smulian JC, Campbell WA, Guzman ER, Rodis JF. Vintzileos AM, et al. Obstet Gynecol. 1996 Jun;87(6):953-8. doi: 10.1016/0029-7844(96)00058-0. Obstet Gynecol. 1996. PMID: 8649705
-
The role of ultrasound in screening for fetal Down syndrome.
Egan JF. Egan JF. Curr Womens Health Rep. 2002 Feb;2(1):52-8. Curr Womens Health Rep. 2002. PMID: 12112983 Review.
-
Fetal ear length measurement: a useful predictor of aneuploidy?
Chitkara U, Lee L, Oehlert JW, Bloch DA, Holbrook RH Jr, El-Sayed YY, Druzin ML. Chitkara U, et al. Ultrasound Obstet Gynecol. 2002 Feb;19(2):131-5. doi: 10.1046/j.0960-7692.2001.00558.x. Ultrasound Obstet Gynecol. 2002. PMID: 11876803 Review.
See all similar articles
Publication types
MeSH terms
Ultrasound Markers for Down Syndrome
Back to Search Results
1/5/2021
Add to your favorites list
Author: Meaghan Shanahan, MD
Mentor: James F. Smith, MD, MA
Editor: Peter F. Schnatz, DO
Registered users can also download a PDF or listen to a podcast of this Pearl.
Log in now, or create a free account to access bonus Pearls features.
Download
Down Syndrome (trisomy 21) is the most common chromosomal disorder in live born infants. About 6,000 babies are born with Down Syndrome each year in the United States, or about 1 in every 700 births. There are multiple prenatal genetic screening strategies and diagnostic tests aimed at accurate prenatal identification of Down Syndrome and other aneuploidies.
Ultrasound is a key component of aneuploidy screening. Both major structural abnormalities and minor “soft markers” can be detected by ultrasound in fetuses affected with aneuploidies. Down Syndrome can include cardiovascular, central nervous, craniofacial, musculoskeletal, gastrointestinal, and urinary tract system anomalies. Major structural anomalies include duodenal atresia and cardiac anomalies such as septal defects, tetralogy of Fallot, and atrioventricular canal defects. These anomalies are not always detected by prenatal ultrasound screening.
Nuchal translucency (NT) can be assessed in the first trimester. NT reflects the subcutaneous fluid-filled space between the back of the fetal neck and the overlying skin. There is an association between increased NT measurement and risk of aneuploidies, including Down Syndrome, with the detection rate for Down Syndrome being 64-70%. A nuchal cystic hygroma represents pathologic nuchal edema and is associated with aneuploidy, including Down Syndrome, in about 50% of cases. A hypoplastic or absent nasal bone can be detected in the first trimester in 62-70% of fetuses with Down Syndrome, but is present in only 1% of normal fetuses.
A hypoplastic or absent nasal bone can be detected in the first trimester in 62-70% of fetuses with Down Syndrome, but is present in only 1% of normal fetuses.
In the second trimester, the most commonly assessed soft markers include echogenic intracardiac foci, pyelectasis, short femur length, choroid plexus cysts, echogenic bowel, thickened nuchal skin fold, and ventriculomegaly. While the likelihood ratios associated with the first four are generally less than 2, the likelihood ratios for echogenic bowel, thickened nuchal fold, and ventriculomegaly are all over 5. The predictive value for echogenic bowel, thickened nuchal fold, and ventriculomegaly, even when isolated, is sufficiently high to prompt further genetic counseling and offering additional aneuploidy screening or diagnostic testing. Findings with lower predictive values such as an isolated choroid plexus cyst, echogenic intracardiac focus, or pyelectasis may prompt aneuploidy screening if not already done. The probability of Down Syndrome is increased when multiple soft markers are present and may prompt diagnostic testing. As an isolated finding, an increased nuchal skin fold confers the highest risk of aneuploidy and is the most powerful second trimester ultrasound marker, with a likelihood ratio of 11-18 and > 99% specificity for Down Syndrome.
As an isolated finding, an increased nuchal skin fold confers the highest risk of aneuploidy and is the most powerful second trimester ultrasound marker, with a likelihood ratio of 11-18 and > 99% specificity for Down Syndrome.
Ultrasonography should not be used by itself to diagnose or exclude Down Syndrome. Sensitivity for detecting Down Syndrome is increased when ultrasound findings are interpreted in combination with serum analyte screening tests such as first and second trimester screening and integrated and sequential screening. Cell-free DNA has a detection rate for Down Syndrome of 99%. Diagnostic testing, such as amniocentesis or chorionic villus sampling, should be offered when screening test results are positive.
Further Reading:
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics; Committee on Genetics; Society for Maternal-Fetal Medicine. Screening for Fetal Chromosomal Abnormalities: ACOG Practice Bulletin, Number 226.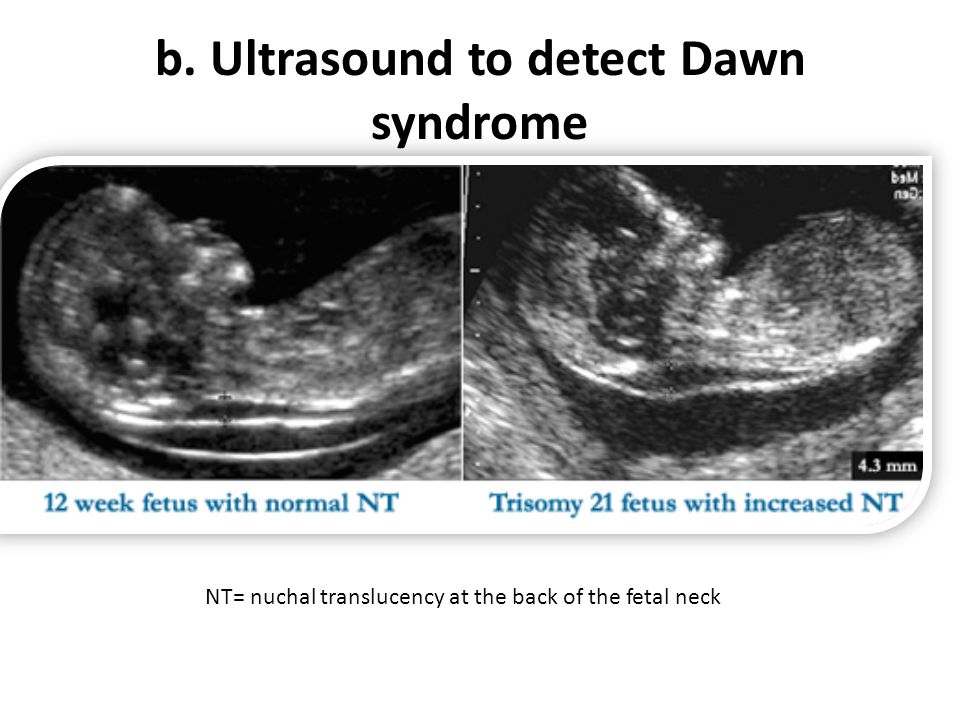 Obstet Gynecol. 2020 Oct;136(4):e48-e69. doi: 10.1097/AOG.0000000000004084. PMID: 32804883.
Obstet Gynecol. 2020 Oct;136(4):e48-e69. doi: 10.1097/AOG.0000000000004084. PMID: 32804883.
Committee on Practice Bulletins—Obstetrics and the American Institute of Ultrasound in Medicine. Practice Bulletin No. 175: Ultrasound in Pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-e256.
Initial approval: November 2017. Reaffirmed May 2019, Reaffirmed January 2021, Minor Revision July 2022
********** Notice Regarding Use ************
The Society for Academic Specialists in General Obstetrics and Gynecology, Inc. (“SASGOG”) is committed to accuracy and will review and validate all Pearls on an ongoing basis to reflect current practice.
This document is designed to aid practitioners in providing appropriate obstetric and gynecologic care. Recommendations are derived from major society guidelines and high-quality evidence when available, supplemented by the opinion of the author and editorial board when necessary. It should not be construed as dictating an exclusive course of treatment or procedure to be followed.
It should not be construed as dictating an exclusive course of treatment or procedure to be followed.
Variations in practice may be warranted when, in the reasonable judgment of the treating clinician, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology. SASGOG reviews the articles regularly; however, its publications may not reflect the most recent evidence. While we make every effort to present accurate and reliable information, this publication is provided “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. SASGOG does not guarantee, warrant, or endorse the products or services of any firm, organization, or person. Neither SASGOG nor its respective officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with this publication or reliance on the information presented.
Copyright 2022 The Society for Academic Specialists in General Obstetrics and Gynecology, Inc. All rights reserved. No re-print, duplication or posting allowed without prior written consent.
Back to Search Results
Prenatal Ultrasound Imaging for Down Syndrome
Author: Badar Bin Bilal Shafi
Introduction
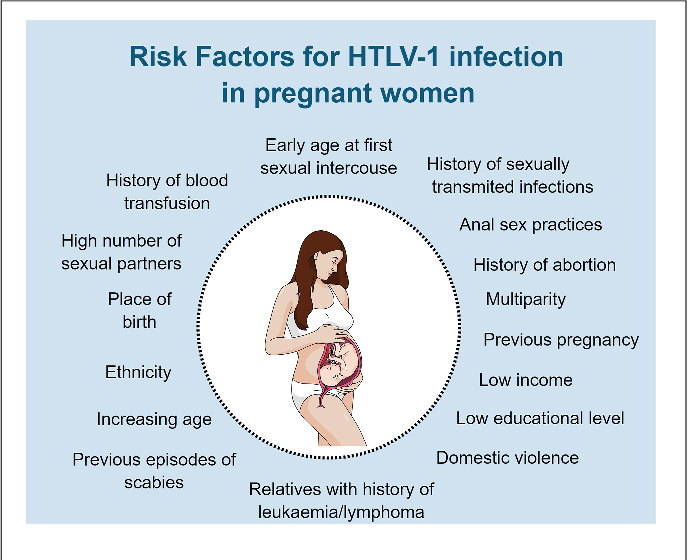
Down syndrome, also known as trisomy 21, is a congenital syndrome caused by the presence of an extra chromosome 21. The frequency in the population is about 1 in 800 live births, and each year about 6,000 babies are born with Down syndrome. Although the clinical manifestations of Down syndrome can vary, they are characterized by a number of serious disorders, including learning disabilities, congenital heart defects, duodenal atresia, seizures, leukemia, and early Alzheimer's disease. Approximately 50% of children with Down syndrome are born with a heart defect, most commonly with a hole in the septum.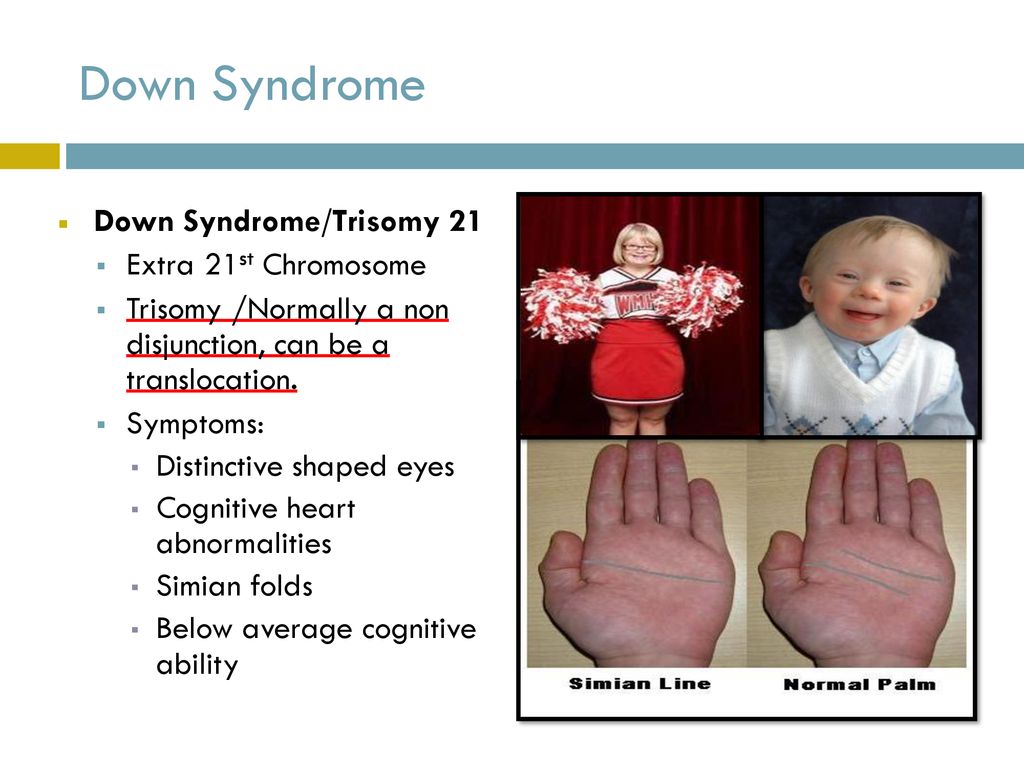 In addition, Hirschsprung's disease, which can cause bowel obstruction, is more common in children with Down syndrome than in other children.
In addition, Hirschsprung's disease, which can cause bowel obstruction, is more common in children with Down syndrome than in other children.
The diagnosis of Down's syndrome is based on the fetal karyotype, analyzed predominantly on fetal amniotic fluid cells collected by amniocentesis or chorionic villus sampling (CVS). Diagnostic tests are invasive and resource intensive, and may cause a risk of pain, infection, bleeding, fetal scarring, or fetal loss. Because of the risk of fetal loss inherent in these invasive methods, they are generally not recommended for all women. Screening consists in identifying patients at increased risk of chromosomal abnormalities, for whom diagnostic testing is then carried out.
Screening tests are non-invasive and usually painless tests done to assess the risk of a fetus developing Down syndrome. These tests do not provide a definitive answer as to whether a child has Down syndrome, but they are used to help parents and doctors decide whether diagnostic tests are warranted.
According to the American College of Obstetricians and Gynecologists, all women should be offered screening for aneuploidy before 20 weeks of gestation, and all pregnant women, regardless of age, should be able to have diagnostic testing.
Ultrasound
Ultrasound is the backbone of imaging, prenatal screening, and diagnosis of Down syndrome and is often used in conjunction with biochemical tests. Ultrasound in the second trimester helps to identify 60-91% of cases of Down syndrome, depending on the criteria used. The use of color Doppler increases sensitivity to detect cardiac malformations, including atrioventricular septal defect (AVSD), outflow anomalies, mitral and tricuspid regurgitation, and right-to-left heart chamber disproportion.
Ultrasound markers include determination of:
- collar space thickness;
- heart anomalies;
- duodenal atresia;
- short hip;
- shortened humerus;
- renal pyelectasis;
- missing nasal bone;
- hyperechoic bowel;
- choroid plexus cysts.
Evidence suggests that a careful combination of accurately performed non-invasive ultrasonography and maternal blood testing, ultimately followed by quantitative fluorescence polymerase chain reaction (QF-PCR), should reduce the need for conventional chromosome analysis, which is relatively expensive. time.
Genetic ultrasound evaluation index
In the proposed scoring system for detecting Down syndrome, the importance of marker clustering forms the basis of the index. So point values are assigned to individual markers based on their sensitivity and specificity in detecting the syndrome. The points scored by each fetus are used for the final score. One study proposed the following scoring system: neck crease = 2; major structural defect = 2; hip shortening, humerus shortening, and pyelectasis = 1 each. Selection of fetuses with a score of 2 or more identified 26/32 (81%) fetuses with Down syndrome, 9/9 (100%) fetuses with trisomy-18 and 2/2 (100%) fetuses with trisomy-13, but only 26/588 (4. 4%) normal fetuses were identified by this scoring system. For the 1/250 risk group, the use of an ultrasound score of 2 resulted in a positive predictive value of 6.87% for Down syndrome and 7.25% for all three trisomies.
4%) normal fetuses were identified by this scoring system. For the 1/250 risk group, the use of an ultrasound score of 2 resulted in a positive predictive value of 6.87% for Down syndrome and 7.25% for all three trisomies.
Technical Limitations
Combined first trimester screening in 11-week Down's Syndrome is better than quadruple second trimester screening. However, after 13 weeks, the results are similar to those of the quadruple screening in the second trimester. Down syndrome detection rates are high with staged, sequential screening and fully integrated screening with low false positive rates.
Nuchal Thickness Determination
Nuchal Thickness (NT) Determination is performed between 11 and 14 weeks of gestation and involves the use of ultrasound to measure the free space in the neck folds of a developing fetus. In fetuses with Down syndrome and other chromosomal abnormalities, fluid tends to accumulate at this site, causing the space to appear enlarged.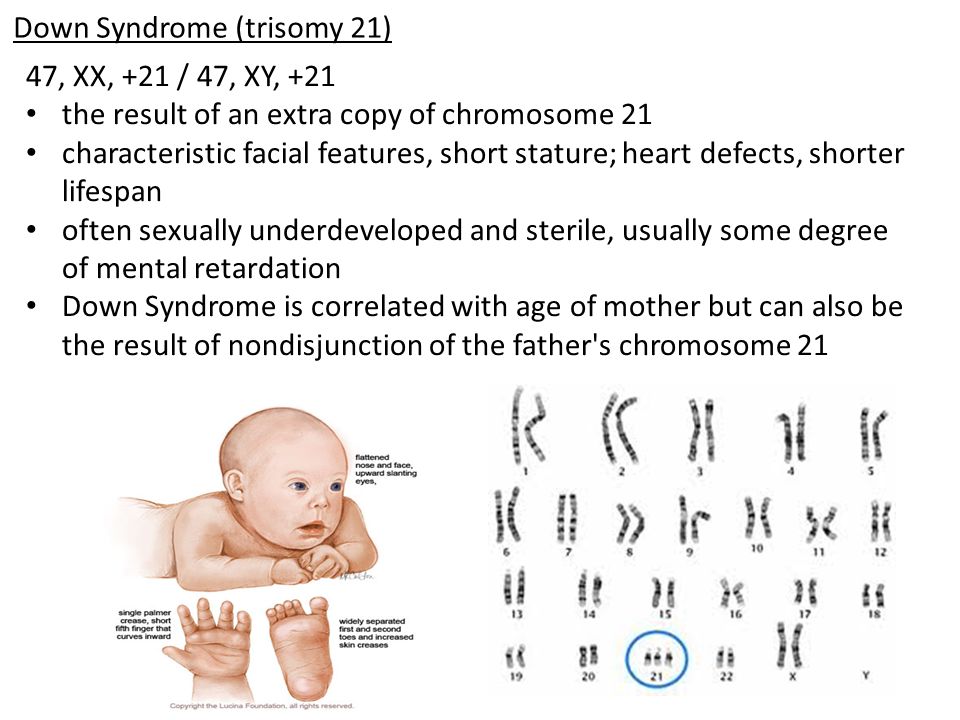 An increase is considered threatening when it exceeds 3 mm. This finding does not mean that the fetus has a chromosomal abnormality, but rather indicates that the risks of certain genetic disorders and birth defects, including Down syndrome, are increased. This measurement, taken together with the age of the mother and the gestational age of the fetus, can be used to calculate the likelihood that the fetus has Down syndrome. When an increased thickness of the collar space is detected, Down syndrome is detected in approximately 80% of cases.
An increase is considered threatening when it exceeds 3 mm. This finding does not mean that the fetus has a chromosomal abnormality, but rather indicates that the risks of certain genetic disorders and birth defects, including Down syndrome, are increased. This measurement, taken together with the age of the mother and the gestational age of the fetus, can be used to calculate the likelihood that the fetus has Down syndrome. When an increased thickness of the collar space is detected, Down syndrome is detected in approximately 80% of cases.
Axial prenatal ultrasonogram of the fetal head demonstrates thickening and translucence of the occipital muscles (arrow).
Longitudinal prenatal ultrasonogram showing nuchal thickening (arrow).
General ultrasound markers
The most common ultrasound marker is to determine the thickness of the collar space. Ultrasound findings in the second trimester, called "soft markers" because they can be transient, include cardiac abnormalities, duodenal atresia, missing nasal bone, shortened femur, shortened humerus, pyelectasis or hydronephrosis, hyperechoic bowel, and vascular cysts. plexus. An echogenic intracardiac focus (EIF) has also been identified as a mild marker of the second trimester. None of these markers are specific and no false positive rates have been reported.
plexus. An echogenic intracardiac focus (EIF) has also been identified as a mild marker of the second trimester. None of these markers are specific and no false positive rates have been reported.
Absence of the nasal bone is a powerful marker of Down syndrome. A short nasal bone is associated with an increased likelihood of Down syndrome in high-risk fetuses. The ratio of nasal thickness to nasal bone length (PT/NBL) has been found to be a valuable marker of first trimester screening for Down syndrome.
Prenatal ultrasound of the fetus at 21 weeks and 1 day of pregnancy shows a shortening of the length of the femur up to 27 mm.
Axial prenatal ultrasound of the head shows a choroid plexus cyst (arrow) in the lateral ventricle.
Axial prenatal abdominal ultrasound obtained at the level of the kidneys shows bilateral renal pyelectasis (arrows)
Coronal prenatal abdominal ultrasound shows bilateral renal pyelectasis (arrows).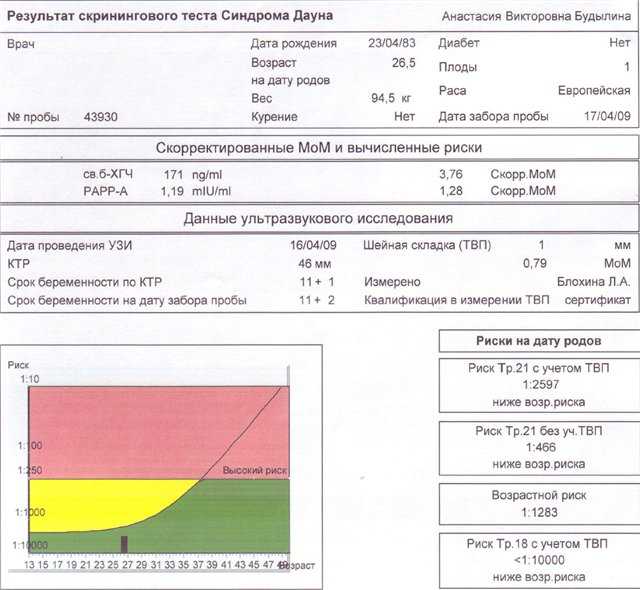
DO YOU CARE FOR YOUR ULTRASONIC MACHINE CORRECTLY?
Download the care guide now
Pelvic and cerebral diameters
Although pelvis and brain diameters are individual as markers of trisomy 21, a combination of measurements of transcerebellar diameter (TCD) and frontothalamic distance (FTD) can be better than measuring any of the parameters alone.
Down's syndrome patients have a large median iliac angle and a shortened median iliac length. The most pronounced differences are found on the median coccygeal crest. This observation suggests that the median coccygeal crest may be the optimal level for measuring iliac angle and length during prenatal diagnosis.
The iliac angle is significantly greater in second trimester fetuses with trisomy 21 than in euploid fetuses. The angle of the ilium varies with axial level, with the widest angle being at the highest level. Evidence supports measurement of the iliac angle at the highest level as a potential marker of Down syndrome on prenatal ultrasound.
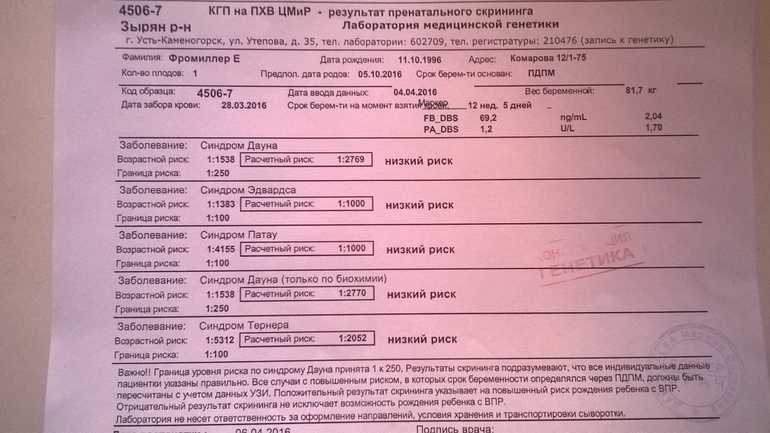
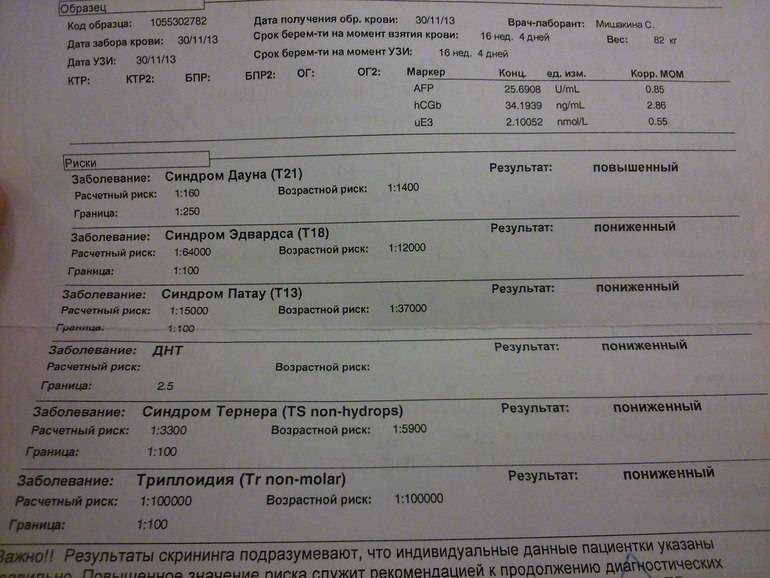
Prenatal screening for trisomies of the first trimester of pregnancy (Down syndrome), PRISCA
A non-invasive test that, based on certain laboratory markers and clinical data, allows using a computer program to calculate the likely risk of developing chromosomal diseases or other congenital anomalies of the fetus.
Due to limitations in the use of calculation methods for determining the risk of congenital fetal anomalies, it is not possible to calculate such risks in multiple pregnancies with 3 or more fetuses.
Russian synonyms
Biochemical screening of the 1st trimester of pregnancy, "double test" of the 1st trimester.
Synonyms English
Maternal Screen, First Trimester; Prenatal Screening I; PRISCA I (Prenatal Risk Calculation).
Research method
Solid-phase chemiluminescent enzyme immunoassay ("sandwich" method), immunochemiluminescent analysis.
Units of measurement
MIU/mL (milli-international unit per milliliter), IU/l (international unit per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for an examination?
- Eliminate fatty foods 24 hours before the test.
- Exclude physical and emotional overexertion within 30 minutes prior to the study.
- Do not smoke for 30 minutes before the test.
General information about the study
Down's disease is a chromosomal disease associated with a violation of cell division (meiosis) during the maturation of sperm and eggs, which leads to the formation of an additional 21st chromosome. The frequency in the population is 1 case per 600-800 births. The risk of a chromosomal abnormality increases with the age of the woman in labor and does not depend on the state of health of the mother of the child, environmental factors. Edwards syndrome (trisomy 18) and Patau syndrome (trisomy 13) are less related to maternal age, with a population frequency of 1 in 7,000 births. Accurate prenatal diagnosis of genetic diseases requires invasive procedures that are associated with a high likelihood of complications, therefore, safe research methods are used for mass screening to identify low or high risk of chromosomal abnormalities and assess the feasibility of further testing.
Edwards syndrome (trisomy 18) and Patau syndrome (trisomy 13) are less related to maternal age, with a population frequency of 1 in 7,000 births. Accurate prenatal diagnosis of genetic diseases requires invasive procedures that are associated with a high likelihood of complications, therefore, safe research methods are used for mass screening to identify low or high risk of chromosomal abnormalities and assess the feasibility of further testing.
Prenatal screening for first trimester trisomies is performed to determine the likely risk of fetal chromosomal abnormalities, trisomy 21 (Down syndrome), and trisomy 18 (Edwards syndrome) and trisomy 13 (Patau syndrome) between weeks 10 and 13 th week and 6 days of pregnancy. It is calculated using the PRISCA (Prenatal Risk Calculation) computer program developed by Typolog Software (Germany) and having an international certificate of conformity. For the study, the content of the free beta subunit of chorionic gonadotropin (hCG) and pregnancy-associated plasma protein A (PAPP-A) in the blood of a pregnant woman is determined.
PAPP-A ensures proper growth and development of the placenta. Its content in the blood increases with the course of pregnancy. The level of PAPP-A does not significantly depend on such parameters as the sex and weight of the child. In the presence of a chromosomal abnormality with fetal malformations, its concentration in the blood decreases significantly from the 8th to the 14th week of pregnancy. It decreases most sharply with trisomy on the 21st, 18th and 13th chromosomes. In Down syndrome, the PAPP-A level is an order of magnitude lower than in a normal pregnancy. An even sharper decrease in the concentration of PAPP-A in the mother's blood serum is observed if the fetus has a genetic pathology with multiple malformations - Cornelia de Lange syndrome. However, after 14 weeks of gestation, the value of determining PAPP-A as a risk marker for chromosomal abnormalities is lost, since its level then corresponds to the norm even in the presence of pathology.
For screening, clinical data (age of the pregnant woman, body weight, number of fetuses, presence and characteristics of IVF, mother's race, bad habits, presence of diabetes, medications taken), ultrasound data (coccyx-parietal size (CTE) and thickness collar space (NTP), the length of the nasal bone).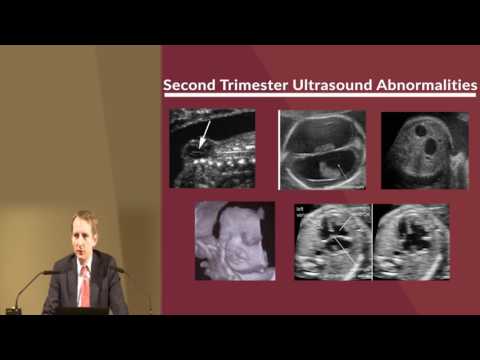 If ultrasound data is available, the gestational age is calculated by the CTE value, and not by the date of the last menstruation.
If ultrasound data is available, the gestational age is calculated by the CTE value, and not by the date of the last menstruation.
After the study and calculation of the risk, a scheduled consultation with an obstetrician-gynecologist is carried out.
The results of a screening study cannot serve as criteria for making a diagnosis and as a reason for artificial termination of pregnancy. Based on them, a decision is made on the advisability of prescribing invasive methods for examining the fetus. At high risk, additional examinations are necessary, including chorion puncture, amniocentesis with a genetic study of the material obtained.
What is research used for?
- For screening of pregnant women to assess the risk of fetal chromosomal pathology - trisomy 21 (Down syndrome), Edwards syndrome.
When is the test ordered?
- When examining pregnant women in the first trimester (the analysis is recommended at a gestational age of 10 weeks - 13 weeks 6 days), especially in the presence of risk factors for the development of pathology:
- over 35 years of age;
- history of miscarriage and severe pregnancy complications;
- chromosomal pathologies, Down's disease or congenital malformations in previous pregnancies;
- hereditary diseases in the family;
- past infections, radiation exposure, taking in early pregnancy or shortly before it drugs that have a teratogenic effect.

What do the results mean?
Reference values
- Pregnancy-associated plasma protein A (PAPP-A)
| Week of pregnancy | Reference values |
| 8th-9th | 0.17 - 1.54 MIU/ml |
| 9th-10th | 0.32 - 2.42 MIU/ml |
| 10-11th | 0.46 - 3.73 MIU/ml |
| 11-12th | 0.79 - 4.76 MIU/ml |
| 12-13th | 1. |
| 13th-14th | 1.47 - 8.54 MIU/ml |
- Free beta subunit of human chorionic gonadotropin (free beta hCG)
| Week of pregnancy | Reference values |
| 8th-9th | 23.65 - 162.5 ng/ml |
| 9th-10th | 23.58 - 193.13 ng/mL |
| 11-12th | 17.4 - 130.38 ng/mL |
| 12-13th | 13. |
| 13th-14th | 14.21 - 114.7 ng/mL |
| 14-15th | 8.91 - 79.44 ng/mL |
| 15-16th | 5.78 - 62.07 ng/mL |
| 16-17th | 4.67 - 50.05 ng/mL |
| 17-18th | 3.33 - 42.81 ng/mL |
| 18-19th | 3.84 - 33.3 ng/mL |
PRISCA calculates the probability of malformations based on the results of the pregnancy examination. For example, the ratio 1:400 shows that, according to statistics, one out of 400 pregnant women with similar values of indicators has a child with a corresponding malformation.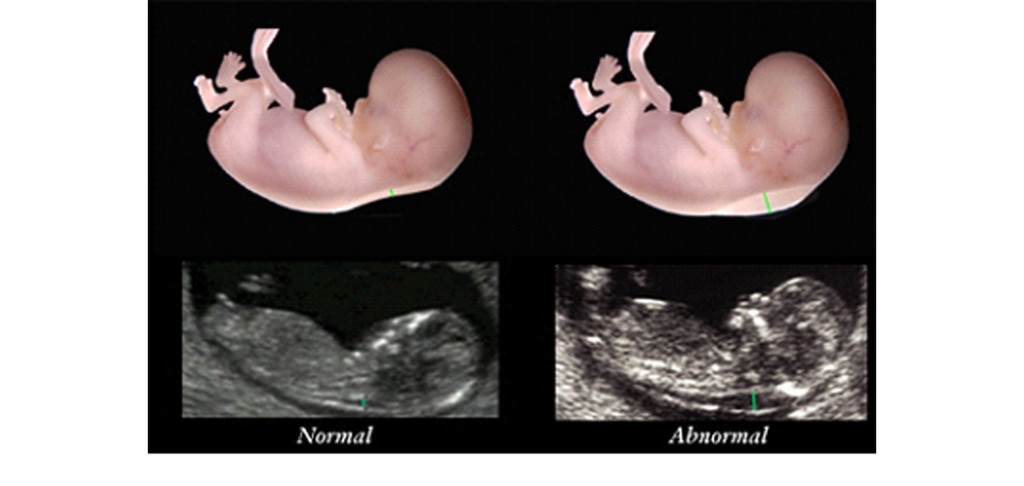
What can influence the result?
- The result is affected by the accuracy of the information provided and the conclusions of the ultrasound diagnosis.
- A false-positive result (high risk) in some cases may be associated with an increase in the beta subunit of chorionic gonadotropin against the background of placental dysfunction, the threat of abortion.
Important Notes
- The laboratory must have accurate data on gestational age and all factors needed to calculate rates. Incomplete or inaccurate data provided may cause serious errors in risk calculations.
The use of invasive diagnostic methods (chorionic biopsy, amniocentesis, cordocentesis) is not recommended if screening tests are normal and there are no changes on ultrasound. - The results of prenatal screening, even at a high calculated risk, cannot serve as a basis for artificial termination of pregnancy.
Also recommended
- Pregnancy - 1st trimester
- Beta subunit of human chorionic gonadotropin (beta hCG)
- Pregnancy-associated plasma protein A (PAPP-A)
- Alpha-fetoprotein (alpha-FP)
- Free estriol
- Placental lactogen
- Progesterone
- Cytological examination of the hormonal background (with the threat of termination of pregnancy, cycle disorders)
Who orders the examination?
Obstetrician-gynecologist, medical geneticist.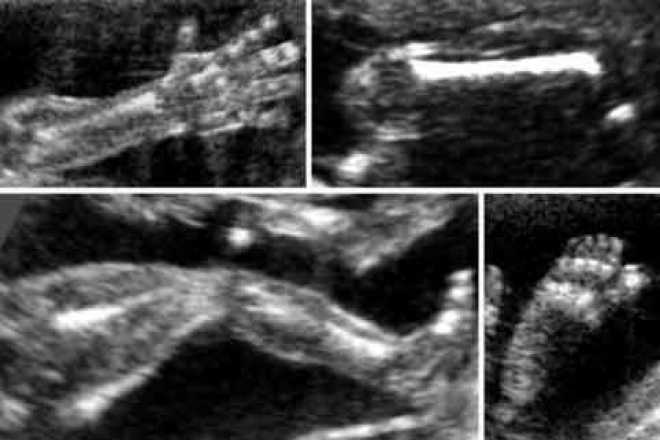
 03 - 6.01 MIU/ml
03 - 6.01 MIU/ml  43 - 128.5 ng/mL
43 - 128.5 ng/mL