How is hiv transmitted from mother to child during pregnancy
Preventing Perinatal Transmission of HIV
Preventing Perinatal Transmission of HIV
Last Reviewed: August 18, 2021
Key Points
- Perinatal transmission of HIV is when HIV is passed from a woman with HIV to her child during pregnancy, childbirth (also called labor and delivery), or breastfeeding (through breast milk). Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
- Women should get tested for HIV before they become pregnant or as early as possible during each pregnancy. The earlier HIV is detected, the sooner HIV medicines can be started.
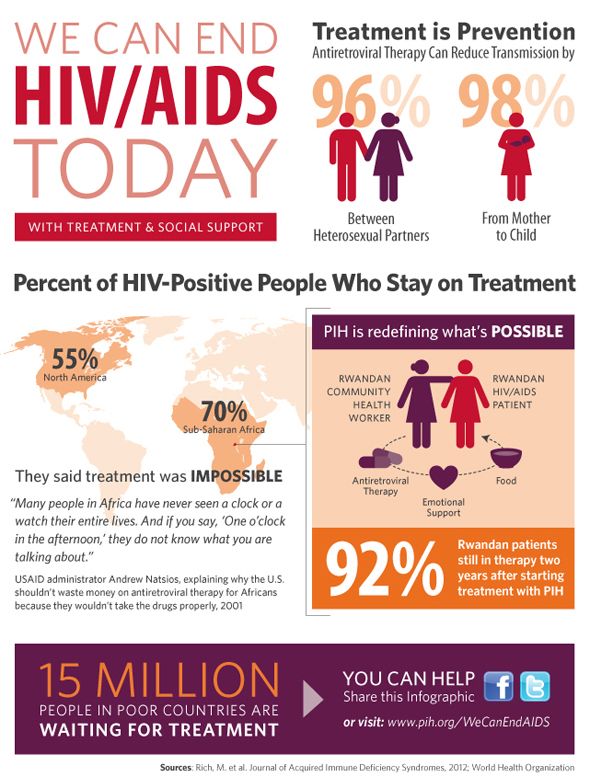
- The use of HIV medicines and other strategies have helped lower the rate of perinatal transmission of HIV to 1% or less in the United States and Europe. (HIV medicines are called antiretrovirals.)
- Pregnant women with HIV should take HIV medicines throughout pregnancy and childbirth to prevent perinatal transmission of HIV.
A scheduled cesarean delivery (sometimes called a C-section) can reduce the risk of perinatal transmission of HIV in women who have a high viral load (more than 1,000 copies/mL) or an unknown viral load near the time of delivery.
- After birth, babies born to women with HIV should receive HIV medicines to reduce the risk of perinatal transmission of HIV. Several factors determine what HIV medicines babies receive and how long they receive the medicines.
- Despite ongoing maternal use of HIV medicines after childbirth, a woman with HIV can still pass HIV to her baby while breastfeeding. In the United States, infant formula is a safe and readily available alternative to breast milk. For these reasons, women with HIV who live in the United States should not breastfeed their babies.
What is perinatal transmission of HIV?
Perinatal transmission of HIV is when HIV is passed from a woman with HIV to her child during pregnancy, childbirth (also called labor and delivery), or breastfeeding (through breast milk). Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
The use of HIV medicines and other strategies have helped to lower the rate of perinatal transmission of HIV to 1% or less in the United States and Europe. (HIV medicines are called antiretrovirals.)
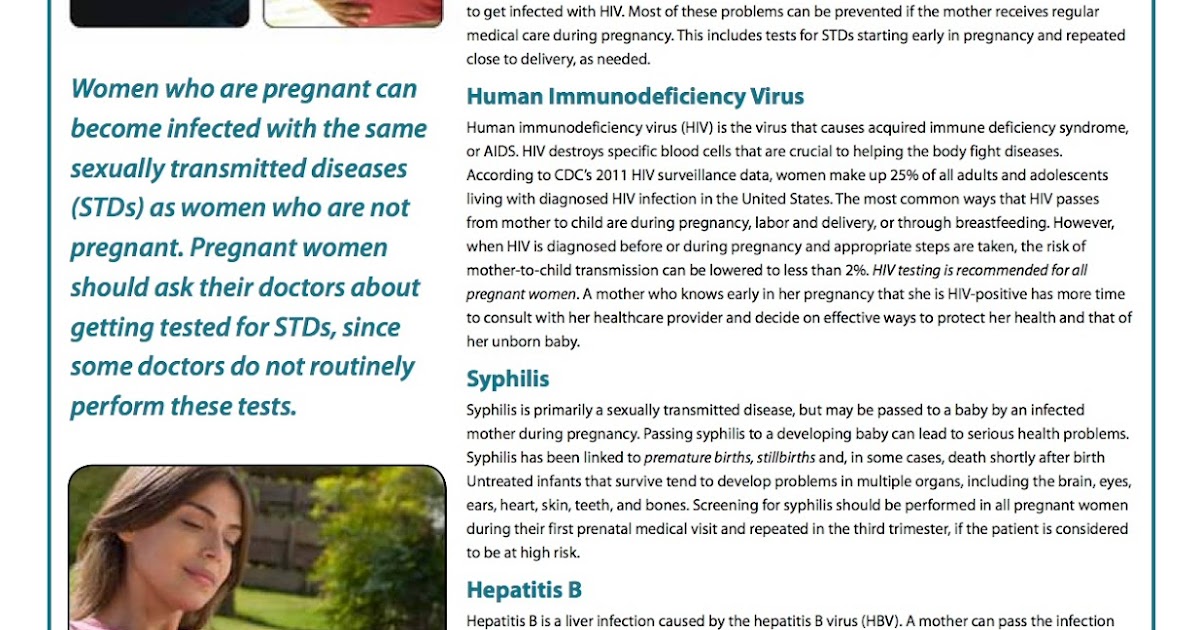
Is HIV testing recommended for pregnant women?
The Centers for Disease Control and Prevention (CDC) recommends that all women get tested for HIV before they become pregnant or as early as possible during each pregnancy. The earlier HIV is detected, the sooner HIV medicines can be started.
All women who are pregnant or trying to get pregnant should encourage their partners also to get tested for HIV and, if possible, screened for other sexually transmitted diseases (STDs). STDs can increase viral loads in people with HIV. If any partner has HIV, that partner should take HIV medicine as prescribed to stay healthy and prevent transmission.
How do HIV medicines prevent perinatal transmission of HIV?
Pregnant women with HIV should take HIV medicines to reduce the risk of perinatal transmission of HIV.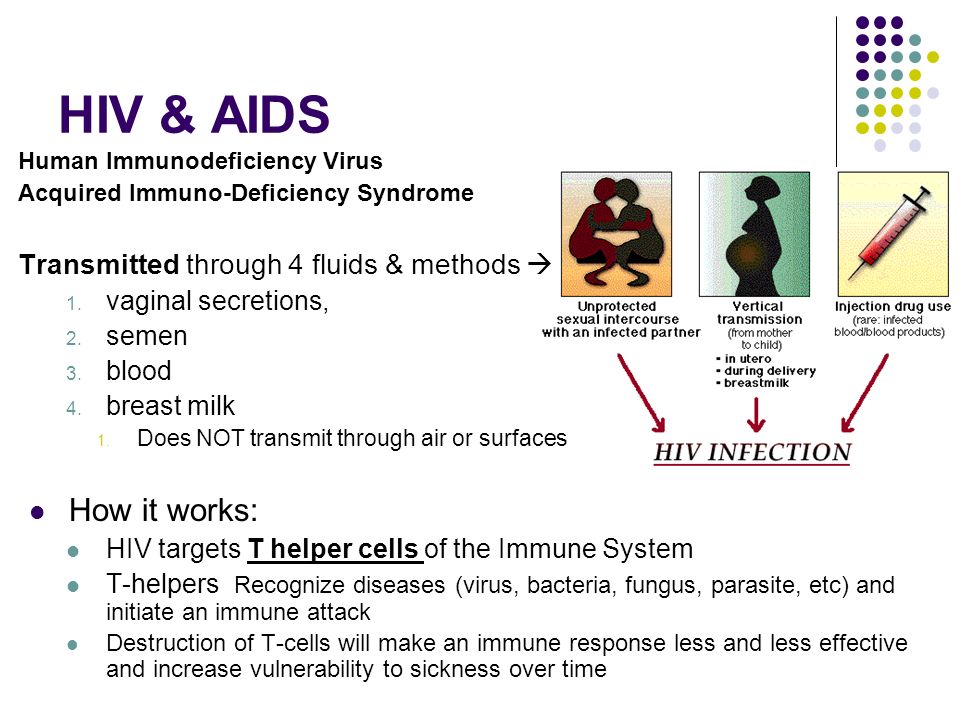 When started early, HIV medicines can be more effective at preventing perinatal transmission of HIV. Women with HIV who are trying to conceive should start HIV medicines before they become pregnant to prevent perinatal transmission of HIV. Pregnant women with HIV should take HIV medicines throughout pregnancy and childbirth to prevent perinatal transmission of HIV. HIV medicines also protect the woman’s health.
When started early, HIV medicines can be more effective at preventing perinatal transmission of HIV. Women with HIV who are trying to conceive should start HIV medicines before they become pregnant to prevent perinatal transmission of HIV. Pregnant women with HIV should take HIV medicines throughout pregnancy and childbirth to prevent perinatal transmission of HIV. HIV medicines also protect the woman’s health.
HIV medicines, when taken as prescribed, prevent HIV from multiplying and reduce the amount of HIV in the body (called the viral load). An undetectable viral load is when the level of HIV in the blood is too low to be detected by a viral load test. The risk of perinatal transmission of HIV during pregnancy and childbirth is lowest when a woman with HIV has an undetectable viral load. Maintaining an undetectable viral load also helps keep the mother-to-be healthy.
Some HIV medicines used during pregnancy that pass from the pregnant woman to her unborn baby through cesarean delivery (sometimes called a C-section) can reduce the risk of perinatal transmission of HIV in women who have a high viral load (more than 1,000 copies/mL) or an unknown viral load near the time of delivery.
After birth, babies born to women with HIV receive HIV medicines to reduce the risk of perinatal transmission of HIV. Several factors determine what HIV medicines babies receive and how long they receive the medicines.
Are HIV medicines safe to use during pregnancy?
Most HIV medicines are safe to use during pregnancy. In general, HIV medicines do not increase the risk of birth defects. Health care providers discuss the benefits and risks of specific HIV medicines when helping women with HIV to decide which HIV medicines to use during pregnancy or while they are trying to conceive.
Are there other ways to prevent perinatal transmission of HIV?
Despite ongoing maternal use of HIV medicines after childbirth, a woman with HIV can still pass HIV to her baby while breastfeeding. In the United States, infant formula is a safe and readily available alternative to breast milk. For these reasons, women with HIV who live in the United States should not breastfeed their babies. Women with HIV can talk to their health care providers to discuss alternative options for feeding before their babies are born or even if they are already breastfeeding.
For these reasons, women with HIV who live in the United States should not breastfeed their babies. Women with HIV can talk to their health care providers to discuss alternative options for feeding before their babies are born or even if they are already breastfeeding.
Additionally, babies should not eat food that was pre-chewed by a person with HIV.
Where can I learn more about preventing perinatal transmission of HIV?
Read the following HIVinfo fact sheets:
- HIV Medicines During Pregnancy and Childbirth
- Preventing Perinatal Transmission of HIV After Birth
This fact sheet is based on information from the following sources:
From CDC:
- HIV and Pregnant Women, Infants, and Children
From the Department of Health and Human Services:
- Recommendations for the Use of Antiretroviral Drugs in Pregnant Women with HIV Infection and Interventions to Reduce Perinatal HIV Transmission in the United States:
- Introduction
- General Principles Regarding Use of Antiretroviral Drugs During Pregnancy: Overview and Teratogenicity
- Counseling and Managing Women Living with HIV in the United States Who Desire to Breastfeed
- Management of Infants Born to Women with HIV Infection: Antiretroviral Management of Newborns with Perinatal HIV Exposure or HIV Infection
Also see the HIV Source collection of HIV links and resources.
Preventing Perinatal Transmission of HIV
Skip to Main Content
HIV SERVICES LOCATOR
Content From: HIV.gov•Updated: June 14, 2022•4 min read
Topics
Can a Pregnant Person Transmit HIV to Their Baby?
Yes. An HIV-positive person can transmit HIV to their baby any time during pregnancy, childbirth, or breastfeeding. But that doesn’t mean that you can’t have children.
Treatment with a combination of HIV medicines (called antiretroviral therapy or ART) can prevent transmission of HIV to your baby and protect your health.
How Can You Prevent Transmitting HIV to Your Baby?
If you are HIV-positive, there are several steps you can take to reduce your risk of transmitting HIV to your baby.
Get Tested for HIV As Soon As Possible to Know Your Status
- If you are pregnant or planning to get pregnant, get tested for HIV as early as possible during each pregnancy.
 Knowing your HIV status gives you powerful information.
Knowing your HIV status gives you powerful information. - If you learn you have HIV, the sooner you start treatment the better—for your health and your baby’s health and to prevent transmitting HIV to your partner.
- If you learn you don’t have HIV, but you are at increased risk of acquiring it, get tested again in your third trimester.
- You should also encourage your partner to get tested for HIV.
HIV-negative but at Risk? Take Medicine to Prevent HIV
- If you have a partner with HIV and you are considering getting pregnant, talk to your health care provider about pre-exposure prophylaxis (PrEP).
- PrEP is medicine people at risk for HIV take to prevent getting HIV from sex or injection drug use. PrEP can stop HIV from taking hold and spreading throughout your body.
- PrEP may be an option to help protect you and your baby from getting HIV while you try to get pregnant, during pregnancy, or while breastfeeding. Find out if PrEP is right for you.
- If your partner has HIV, also encourage them to get and stay on HIV medicine. This will keep them healthy and help prevent them from transmitting HIV to you.
HIV-positive? Take Medicine to Treat HIV
- Taking HIV medicine reduces the amount of HIV in your body (your viral load) to a very low level, called viral suppression. If your viral load is so low that a standard lab test can’t detect it, this is called having an undetectable viral load. Taking HIV medicine and getting and keeping an undetectable viral load is the best thing you can do to stay healthy and prevent transmission to your baby.
- If you have HIV and take HIV medicine as prescribed throughout your pregnancy and childbirth and give HIV medicine to your baby for 4 to 6 weeks after giving birth, your risk of transmitting HIV to your baby can be less than 1%.
- If your HIV viral load is not adequately reduced by HIV medicine, a cesarean delivery (sometimes called a C-section) can also help prevent HIV transmission.

- Taking HIV medicine substantially reduces, but does not eliminate, the risk of transmitting HIV through breastfeeding. The current recommendation in the United States is to avoid breastfeeding.
- Taking HIV medicine also protects your HIV-negative partner. People with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load can live long and healthy lives and will not transmit HIV to their HIV-negative partners through sex.
Are HIV Medicines Safe for You to Use During Pregnancy?
Most HIV medicines are safe to use during pregnancy. Talk with your health care provider about the benefits and risks of specific HIV medicines when deciding which HIV medicines to use during pregnancy or while you are trying to get pregnant.
Can You Breastfeed if You Have HIV?
The current recommendation in the United States is that people with HIV should not breastfeed or pre-chew food for their babies.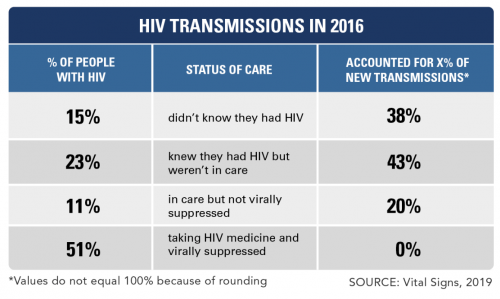 In the United States, infant formula is a safe and readily available alternative to breast milk. Keeping an undetectable viral load substantially reduces, but does not eliminate, the risk of transmitting HIV through breastfeeding. If you have questions about breastfeeding or desire to breastfeed, talk to your health care provider about infant feeding options. Learn more about HIV and breastfeeding here.
In the United States, infant formula is a safe and readily available alternative to breast milk. Keeping an undetectable viral load substantially reduces, but does not eliminate, the risk of transmitting HIV through breastfeeding. If you have questions about breastfeeding or desire to breastfeed, talk to your health care provider about infant feeding options. Learn more about HIV and breastfeeding here.
What Should You Ask Your Health Care Provider About Having a Baby?
You might ask your health care provider some of these questions:
- What is the safest way to conceive?
- Will HIV cause problems for me during pregnancy or delivery?
- Will my HIV treatment cause problems for my baby?
- What are the pros and cons of taking HIV medicine while I am pregnant?
- Is my viral load undetectable?
- How do I avoid transmitting HIV to my partner(s), surrogate, or baby during conception, pregnancy, and delivery?
- What medical and community programs and support groups can help me and my baby?
- What birth control methods are best for me?
If you or your partner has HIV and is thinking about getting pregnant, you should talk to your health care provider as soon as possible about taking PrEP.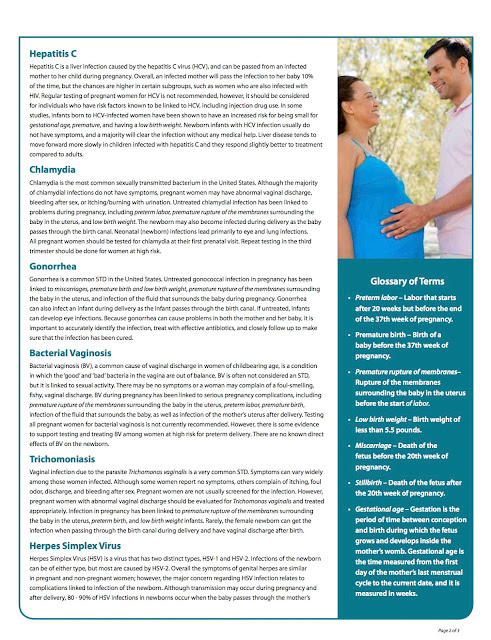 If you’re not already taking it, PrEP may be an option to help protect you or your partner from getting HIV while you or your partner try to get pregnant, during pregnancy, or while breastfeeding.
If you’re not already taking it, PrEP may be an option to help protect you or your partner from getting HIV while you or your partner try to get pregnant, during pregnancy, or while breastfeeding.
Adopting a baby is also an option for people with HIV who want to begin or expand their families. The Americans with Disabilities Act does not allow adoption agencies to discriminate against individuals or couples with HIV.
Related HIV.gov Blogs
Topics
Additional Resources
Pregnancy and childbirth with HIV
Pregnancy and childbirth are often associated with many questions and concerns. When pregnancy occurs against the background of HIV infection, there are even more questions.
First and foremost, if a woman with HIV finds out about her pregnancy, or a girl finds out about her positive HIV status and about her pregnancy at the same time, then you should contact the AntiAIDS Center as soon as possible!
Taking ARVs can conceive, bear and give birth to a healthy baby! The risk of transmitting HIV to him will be minimal. This is true for discordant couples (when only one of the partners is living with HIV) and when both partners are HIV positive. It is important to take ART correctly and achieve an undetectable viral load in the mother, as well as apply other preventive measures.
This is true for discordant couples (when only one of the partners is living with HIV) and when both partners are HIV positive. It is important to take ART correctly and achieve an undetectable viral load in the mother, as well as apply other preventive measures.
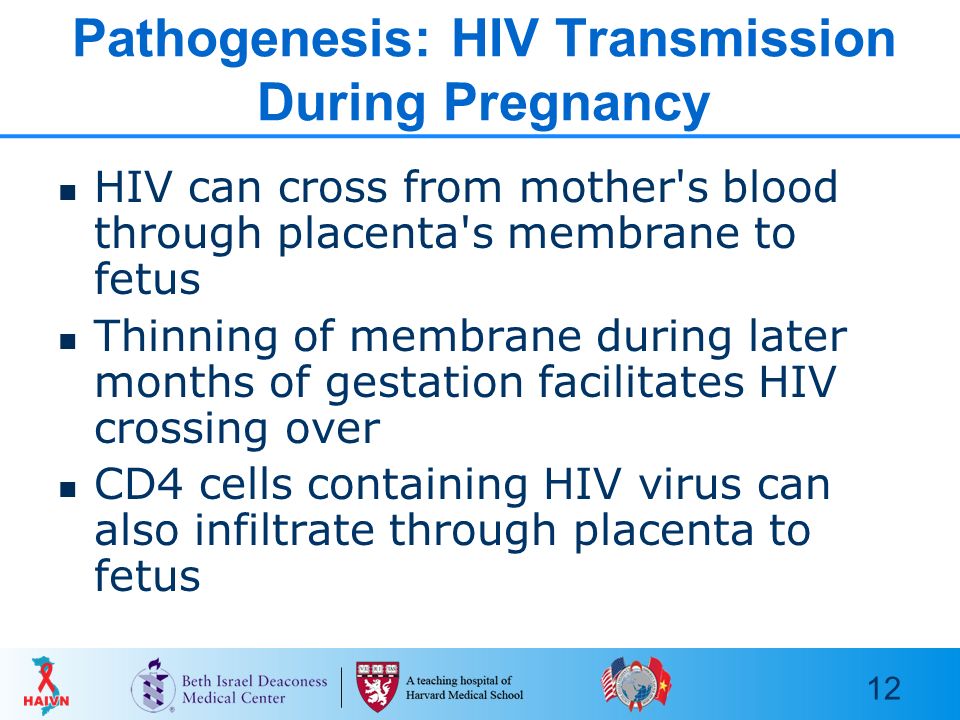
How can HIV be transmitted from mother to child? It can be transmitted through blood, vaginal secretions and breast milk. The risk of intrauterine transmission increases in late pregnancy and during childbirth. During childbirth, the child comes into contact with the mother's blood and vaginal discharge, from which the virus can enter the child's body through microtraumas on the child's skin.
HIV does not cross the placenta well and is rarely transmitted during early pregnancy. If at the time of conception a woman did not take ARVT, this does not mean that the child will be infected. But it is important to start taking ART as early as possible in order to achieve an undetectable viral load by late pregnancy and childbirth.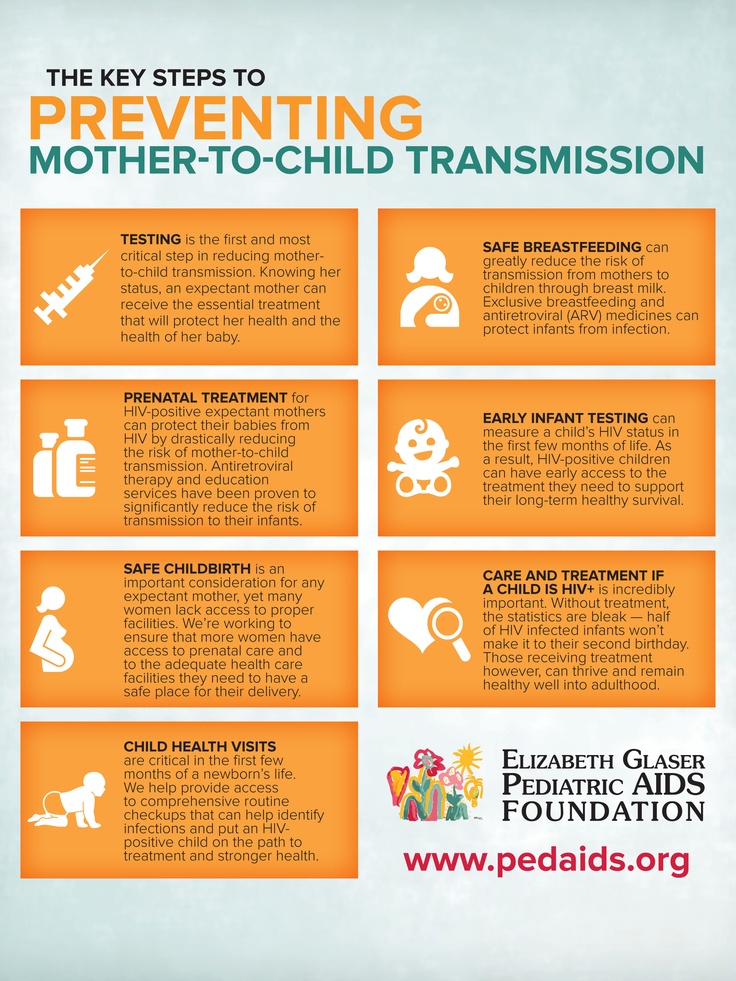 And breastfeeding will need to be abandoned completely, even when taking ART.
And breastfeeding will need to be abandoned completely, even when taking ART.
Is pregnancy safe for a mother with HIV? With the right ARV therapy, pregnancy will be almost indistinguishable from pregnancy with HIV-negative status.
There are special recommendations for discordant couples where only one parent is HIV positive.
If the mother is HIV-negative and the father is HIV-positive, conception will carry the risk of infection for the mother. Sustained suppression of the viral load in the father is a prerequisite for conceiving a child. To eliminate the risk of infection of the mother, it is necessary to resort to the following methods:
- Semen cleaning. Viral particles are found only in the seminal fluid, but not in the spermatozoa themselves. Therefore, it is possible to separate the spermatozoa from the seminal fluid, test them for the absence of viral particles, and then insert them into the vagina.
- IVF (in vitro fertilization).
 In this case, the mother's egg is fertilized with purified father's sperm "in vitro" and then the resulting embryo is implanted in the uterus.
In this case, the mother's egg is fertilized with purified father's sperm "in vitro" and then the resulting embryo is implanted in the uterus.
In almost 100% of cases, when using these methods, the risk of infection, both mother and child, is eliminated.
If the mother is HIV-positive and the father is HIV-negative, then the safest way is to inject semen into the vagina using an ordinary plastic syringe without a needle. It can be collected using a condom (no spermicidal lubricant) or a clean plastic biomaterial container. The collected sperm is injected with a syringe deep into the vagina on the days of ovulation. The risk of infection for the father is completely absent.
How safe is ARV therapy during pregnancy? ARV therapy is very important for the birth of a healthy child. But expectant mothers may have questions about how safe it is during pregnancy.
Modern antiretroviral therapy has a very good safety profile for both mother and child. After numerous clinical studies, many ARV drugs have been proven safe - they do not affect the growth and development of the child and do not threaten the normal course of pregnancy.
After numerous clinical studies, many ARV drugs have been proven safe - they do not affect the growth and development of the child and do not threaten the normal course of pregnancy.
The doctor always selects a specific regimen, taking into account other features of the mother's health and the course of pregnancy. Nevertheless, it is important for the expectant mother to carefully monitor her condition, regularly take prescribed tests and visit a doctor!
When should I start ART? If a woman was not taking ART before pregnancy, it is usually started at 13–14 weeks of gestation. By this time, the formation of the main organs of the fetus is completed, and the risks of influencing the development of the child become minimal. But, if the mother has a very low CD4 count or a very high viral load, therapy is started immediately.
It is dangerous to delay the start of therapy beyond the 14th week. To protect the baby from HIV infection, a sustained low maternal viral load must be achieved by the time of birth. If it was not possible to start therapy in a timely manner, it should be done in any case, as soon as such an opportunity arises.
If it was not possible to start therapy in a timely manner, it should be done in any case, as soon as such an opportunity arises.
If you are already taking antiretroviral drugs and are planning a pregnancy, be sure to discuss this with your doctor! The doctor may suggest changing the regimen. It may turn out that your regimen already consists of drugs that are allowed during pregnancy, then nothing will have to be changed.
If the regimen does need to be changed, it is safest to first ensure that the new regimen is well tolerated and produces sustained viral load suppression, and then plan pregnancy. This usually becomes clear within 1-3 months of starting a new regimen.
Is there a need for special prevention of HIV transmission to the child after childbirth?
Prevention by taking ART. Babies born to mothers with HIV, regardless of the mother's viral load at the time of birth, are usually given prophylactic ARVs for several weeks. Therapy begins immediately after childbirth, the scheme and dosage is selected by the doctor individually.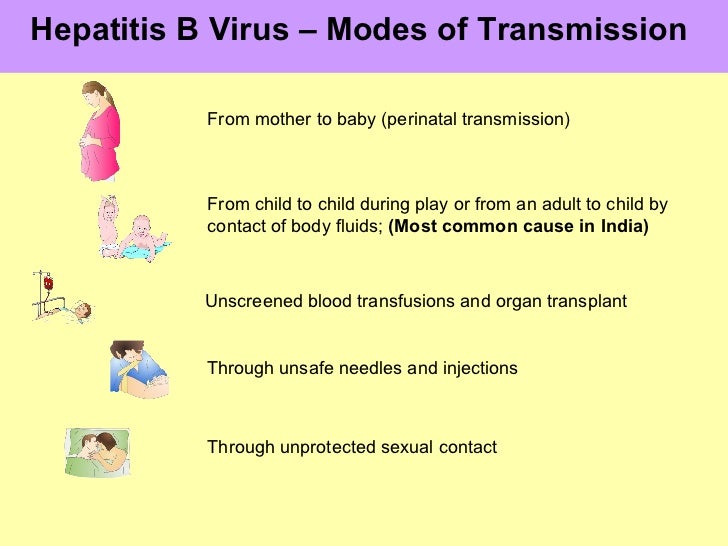
Breastfeeding should be completely avoided. HIV is found in breast milk, and can also be transmitted to the child through microtrauma and cracked nipples. You can’t apply a baby to an empty breast either - even when there is no milk, the risk of transmitting the virus through microcracks in the nipple remains. You can't feed with expressed milk either.
If a mother is diagnosed with HIV already during breastfeeding, it should be stopped. The child is prescribed a prophylactic course of antiretroviral drugs and is tested for HIV infection.
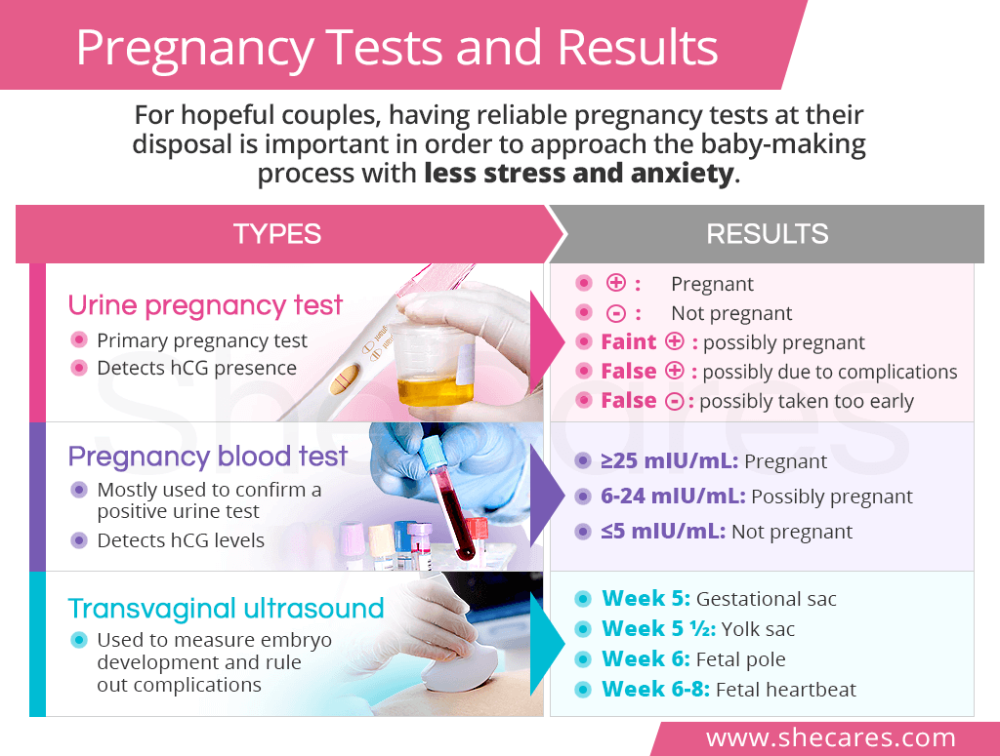
When can you know for sure that HIV infection has not been passed on to a child? Children are tested by PCR - it allows you to detect virus RNA in the blood. PCR is usually performed in the first two days after birth, then a month later, and then another three months later. Maternal antibodies completely disappear from the child's blood by 18 months - at this age, ELISA is done.
A negative PCR result on the second day after birth indicates that the baby was NOT infected during pregnancy.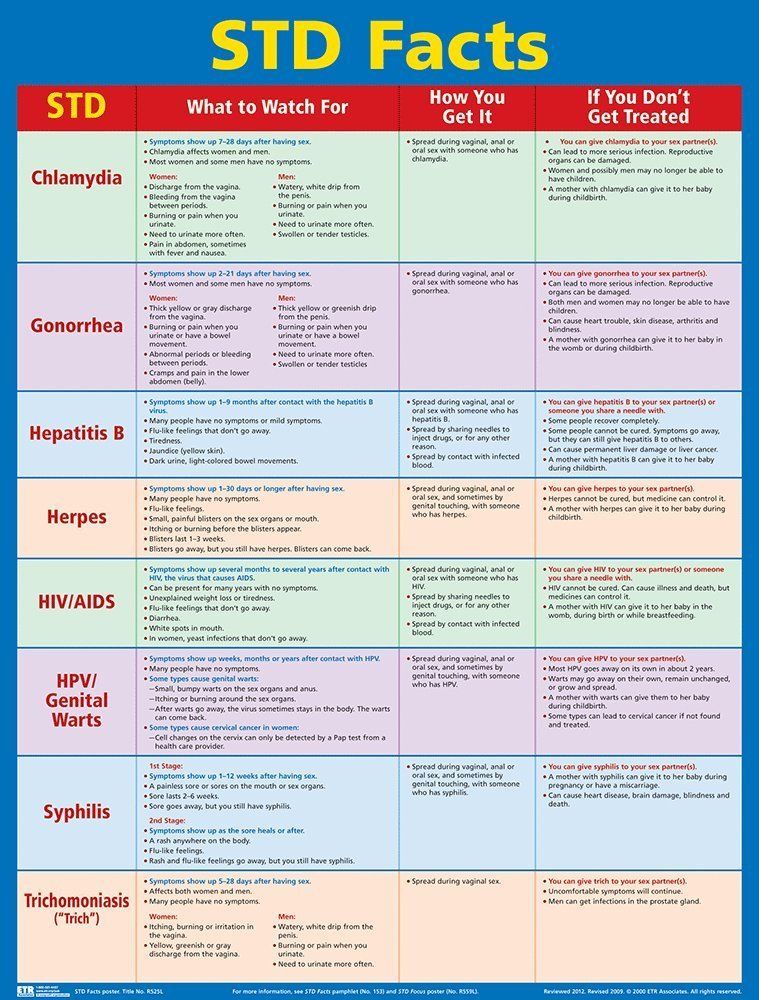 A negative PCR after one month indicates that the baby most likely did NOT become infected during delivery. A negative PCR after 4 months of age indicates that the child is almost certainly NOT infected with HIV. The final confirmation of this is a negative ELISA result at 1.5 years.
A negative PCR after one month indicates that the baby most likely did NOT become infected during delivery. A negative PCR after 4 months of age indicates that the child is almost certainly NOT infected with HIV. The final confirmation of this is a negative ELISA result at 1.5 years.
A positive result of any PCR test indicates that the child may have been infected with HIV. In this case, additional studies are carried out to finally confirm the diagnosis. If HIV is still transmitted to the child, he is prescribed ARV therapy, which will allow him to live a long, fulfilling life and have his own children in the future.
Remember that it is possible to give birth to a healthy baby with HIV! To do this, you need to contact the local Anti-AIDS Center, follow the doctor's recommendations, take ARV therapy correctly and apply preventive measures.
HIV and pregnancy
Every pregnant woman registered with the antenatal clinic must be tested for HIV twice - at the first visit and in the third trimester. If a positive or doubtful test for antibodies to HIV is detected, the woman is immediately sent for a consultation to the AIDS Center to clarify the diagnosis.
If a positive or doubtful test for antibodies to HIV is detected, the woman is immediately sent for a consultation to the AIDS Center to clarify the diagnosis.
Mother-to-child transmission of HIV is possible during pregnancy, more often during late pregnancy, during childbirth and while breastfeeding.
Without preventive measures, the risk of HIV transmission is up to 30%. The risk of infection of the child increases if the mother was infected within six months before the onset of pregnancy or during pregnancy, and also if the pregnancy occurred in the late stages of HIV infection. The risk increases with a high viral load (the amount of virus in the blood) and low immunity. An increase in the risk of infection of the child occurs with repeated pregnancies.
With proper preventive measures, the risk of mother-to-child transmission of HIV infection is reduced to 2%.
In this brochure you will find information on how to reduce the risk of infection of a child and on the terms of dispensary observation of a child at the AIDS Center.
Reducing the risk of mother-to-child transmission of HIV infection
When contacting the AIDS Center, a pregnant woman receives advice from an infectious disease specialist, an obstetrician-gynecologist, a pediatrician; passes all the necessary tests (viral load, immune status, etc.), after which the issue of prescribing antiretroviral (ARV) drugs to the woman is decided. When ARV drugs are taken correctly, the amount of virus in the blood decreases and the risk of passing HIV to an unborn child is reduced. The choice of the regimen and the term of prescription of ARV drugs is decided individually. The safety of their use for the fetus and the pregnant woman herself has been proven. The medicines are given out free of charge according to the prescriptions of the doctors of the AIDS Center.
The effectiveness of drugs should be checked by the end of pregnancy (viral load laboratory test).
A pregnant woman must continue to be observed at the antenatal clinic at the place of residence.
Prevention of mother-to-child transmission of HIV includes 3 stages:
1 stage. Taking medication by a pregnant woman. Prevention should be started as early as possible, preferably from 13 weeks of gestation, with three drugs and continued until delivery.
Stage 2. Intravenous administration of an ARV drug to a woman during childbirth (“dropper”).
Stage 3. Taking medications for a newborn baby. Taking drugs by a child begins in the first 6 hours after birth (no later than 3 days). Most children receive zidovudine syrup at a dose of 0.4 ml per 1 kg of body weight twice a day (every 12 hours) for 28 days. In special cases, the doctor can add 2 more drugs to the child for prevention: viramune suspension - 3 days, epivir solution - within one week.
Births take place in maternity hospitals where the woman lives. Maternity hospitals in the Kostroma region are provided with all the necessary ARV drugs for prevention.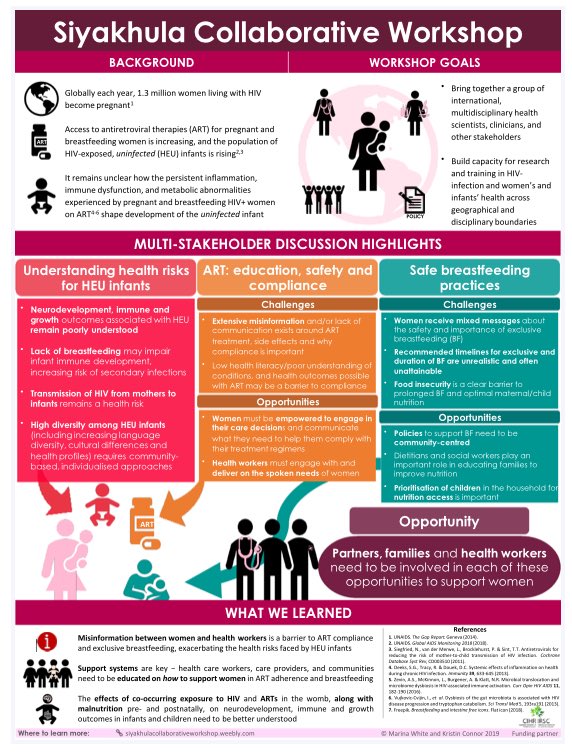 The method of delivery (natural childbirth or caesarean section) is chosen by the general decision of the infectious disease specialist and obstetrician-gynecologist.
The method of delivery (natural childbirth or caesarean section) is chosen by the general decision of the infectious disease specialist and obstetrician-gynecologist.
Breastfeeding is one of the ways of transmission of HIV infection (not only breastfeeding, but also feeding with expressed milk).
Without exception, women with HIV should not breastfeed!
Timing of examination of children born to HIV-infected mothers in the first year of life.
Until the age of 1 year, the child is examined three times:
- In the first 2 days after birth, blood is taken in the maternity hospital for HIV testing by PCR (detects virus particles) and ELISA (detects antibodies - protective proteins produced by the human body for the presence of infection ) for delivery to the AIDS Center.
- At 1 month of life - blood is taken for HIV by PCR in a children's clinic or hospital, in the HIV prevention office at the place of residence (if you have not donated blood at the place of residence, this will need to be done at the AIDS Center at 2 months).

- At 4 months of life - you must come to the AIDS Center to examine the child by a pediatrician and test the blood for HIV by PCR. Also, the doctor may prescribe additional tests for your child (immune status, hematology, biochemistry, hepatitis C, etc.).
If you miss one of the examination dates, do not postpone it until a later time. At the age of 1 month and up to 1 year of life, the child must be tested for HIV by PCR at least 2 times!
What do the test results mean?
Positive blood test for HIV antibodies
All children of HIV-positive mothers are also positive from birth, and this is normal! The mother passes on her proteins (antibodies) in an attempt to protect the baby. Maternal antibodies should leave the blood of a healthy child by 1.5 years (on average).
Positive PCR result
This test directly detects the virus itself, which means that a positive PCR may indicate a possible infection of the child. An urgent appearance of the child in the AIDS Center for rechecking is required.
An urgent appearance of the child in the AIDS Center for rechecking is required.
Negative PCR
A negative result is the best result! Virus not detected.
- A negative PCR on the second day of a child's life indicates that the child most likely did not become infected during pregnancy.
- Negative PCR at 1 month of life says that the child was not infected during childbirth. The reliability of this analysis at the age of one month is about 93%.
- Negative PCR over the age of 4 months - the child is not infected with a probability of almost 100%.
Examinations of children from 1 year of age.
If a child already has a negative blood test for HIV by PCR, the main method of research from the age of 1 year is the determination of antibodies to HIV in the child's blood. The average age when the child's blood is completely "cleared" of maternal proteins is 1.5 years.
- At the age of 1, the child donates blood for antibodies to HIV at the AIDS Center or at the place of residence.
 If a negative test result is obtained, repeat after 1 month and the child can be deregistered ahead of schedule. A positive or questionable result for HIV antibodies requires a retake after 1.5 years.
If a negative test result is obtained, repeat after 1 month and the child can be deregistered ahead of schedule. A positive or questionable result for HIV antibodies requires a retake after 1.5 years. - Over the age of 1.5 years, one negative HIV antibody test is enough to deregister the child if there are previous tests.
Deregistration of children
- Age of the child is over 1 year;
- Presence of two or more negative PCR tests over 1 month of age;
- Two or more negative HIV antibody test results over 1 year of age;
- Not breastfeeding in the last 12 months.
Confirmation of the diagnosis of HIV infection in a child
Confirmation is possible at any age from 1 to 12 months with two positive HIV PCR results.
In children older than 1.5 years, the diagnostic criteria are the same as for adults (presence of a positive blood test for antibodies to HIV).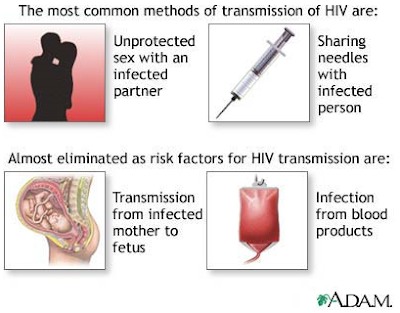
The diagnosis is confirmed only by specialists from the AIDS Center.
Children with HIV infection are constantly under the supervision of a pediatrician of the AIDS Center, as well as in the children's polyclinic at the place of residence. HIV infection may be asymptomatic, but there comes a time when the doctor will prescribe treatment for the child. Modern drugs can suppress the immunodeficiency virus, thereby eliminating its effect on the body of a growing child. Children with HIV can lead a full life, visit any children's institutions on a general basis.
Vaccination
Children of positive mothers are vaccinated like all other children according to the national calendar, but with two exceptions:
- The polio vaccine must be inactivated (not live).
- Permission for BCG vaccination (vaccination against tuberculosis), which is usually given in the maternity hospital, you will receive from the pediatrician of the AIDS Center
Pediatric department phone: 8-9191397331 (from 0900 to 1500 except Thursdays).