Breast milk production tips
Low Milk Supply | WIC Breastfeeding Support
Many moms worry about low milk supply, but most of the time your body makes exactly what your baby needs, even if you don't realize it. There are also ways to tell if your baby is getting enough milk. If you aren't making enough, there are ways you can build your supply. And your WIC breastfeeding staff is always there to help!
Am I Making Enough Milk?
First, look for these signs that your baby is getting enough milk. For example, pay attention to the number of wet and dirty diapers and your baby's weight gain.
Things you should NOT worry about:
- How your breasts feel. Your breasts will feel softer and less full as your milk supply adjusts to your baby's needs. This does not mean you have low supply.
- If your baby nurses for shorter periods of time, such as only 5 minutes on each breast.
- If your baby's feeds are bunched together. This is called cluster feeding and happens when your baby starts nursing more often and for longer.
This can happen in the evenings or because of growth spurts.
- Not getting much milk when you express. Your baby is much more effective than a pump or hand expression at getting out milk. Find tips to help you pump.
If you are still concerned, talk to your baby's doctor about their growth.
Causes of Low Milk Supply
While most moms make plenty of milk, some do have low milk supply. This might happen if you:
- Limit your baby's breastfeeding sessions. Remember, the more you feed on demand, the more milk you make.
- Give your baby infant formula instead of breastfeeding.
- Introduce solid foods before baby is 4-6 months old.
- Take certain birth control pills or other medicine.
- Don't get enough sleep.
- Drink alcohol or smoke.
- Have had breast surgery.
Talk to your doctor if you have hepatitis B or C, herpes, or diabetes. These conditions may also affect milk supply.
Increasing Your Milk Supply
Breastfeeding frequently—especially in the first hours, days, and weeks—is the main way to increase your milk supply. Your body will make milk to meet your baby's demand.
Try these tips to help you make more milk:
- Breastfeed every time your baby is hungry. In the early weeks, your baby will eat 8-12 times every 24 hours. It's best not to put your baby on a strict feeding schedule. Follow your baby's cues, and let your baby tell you when it's time to eat.
- Make sure your baby is latching well.
- Offer both breasts at each feeding. Let your baby finish the first side, then offer the other side.
- Empty your breasts at each feeding.
 Hand express or pump after a feeding to draw out all the milk and signal your body to make more.
Hand express or pump after a feeding to draw out all the milk and signal your body to make more. - Avoid bottles and pacifiers in the early weeks. Feed your baby from your breast whenever you can.
- Get plenty of sleep, and eat a healthy diet.
- Pump or express your milk. Pumping or expressing milk frequently between nursing sessions, and consistently when you're away from your baby, can help build your milk supply.
- Relax and massage. Relax, hold your baby skin-to-skin, and massage your breasts before feeding to encourage your milk to let down.
- Take care of yourself. Get plenty of rest, eat well, drink enough fluids, and let others help you.
Consider Charting Your Progress
Record how often your baby is breastfeeding, for how long, and on which sides. If you are supplementing with infant formula, record how much your baby is getting and decrease the infant formula as your milk supply increases. WIC breastfeeding staff can help you determine how much infant formula your baby needs.
WIC breastfeeding staff can help you determine how much infant formula your baby needs.
Still Have Questions?
Contact your WIC breastfeeding expert. They can talk to you about supply concerns and give you tips to increase your supply to meet your baby's needs.
Breastfeeding: Tips to Increase Your Milk Supply l University Hospitals l Northeast Ohio
Signs That a Breastfed Baby Is Being Well Nourished
- Your baby nurses at least 8 to 16 times in 24 hours, or every 2 to 3 hours. Your baby may be fussy once or twice a day. At these times, he or she wants to nurse often for several hours before seeming full. This is called cluster feeding.
- Your baby wets at least 6 cloth or 5 disposable diapers and has at least 1 bowel movement in 24 hours. This occurs by 1 week of age.
- You can hear your baby swallow milk while nursing or you can feel your baby swallow when lightly touching his or her throat.
- Your breasts seem softer after nursing.

- Your baby gains 4 to 8 ounces a week after the first week. There is no need to weigh your baby at home. Your baby’s doctor will do this for you. You may notice that your baby has outgrown his or her clothing.
- Your baby has regained his/her birthweight by 10 to 14 days after birth.
Factors Which Can Cause Your Milk Supply to Decrease
- Your baby feeds fewer than 8 to 16 times in 24 hours. Milk production is affected by how well the breast is drained.
- Your baby has a very weak suck, or has an improper latch.
- Giving bottles of formula or water after nursing. Most babies will suck on a bottle after nursing. This just means they need to suck. It does not mean they are still hungry. Babies cry or fuss for many reasons, such as being tired, bored, wet, hot or cold.
- Giving solid foods too early and/or before you breastfeed. Most babies do not need solid foods for the first 6 months if they are breastfeeding 8 to 16 times a day.

- Smoking can cause a decreased milk supply and interfere with the letdown reflex. Here are some things you should do:
- Try to quit or cut down.
- Smoke after nursing, not before.
- Don’t smoke in the same room with your baby.
- Beginning birth control pills too soon can decrease your milk supply. Wait at least 6 weeks before taking birth control pills and then use only the mini-pill (Progestin). If you still notice a decrease in your milk supply, talk to your doctor about other birth control options. Other medications may also affect milk supply. Check with your doctor. (Refer to PI-682, Breastfeeding and Birth Control: You Have Options.)
- Mothers who are exhausted may notice a decrease in milk supply. To keep yourself from getting too tired:
- Sleep or relax when your baby sleeps.
- Eat balanced diet that includes high-protein food.
- Drink when you are thirsty so that your urine is pale yellow in color.
 Both under and excessive over hydration can decrease milk supply.
Both under and excessive over hydration can decrease milk supply. - Take an iron supplement if your healthcare provider says you are anemic.
- Talk with your doctor or nurse midwife about the need for vitamin supplement.
- Accept help when it is offered.
- Use nipple shields and pacifiers with caution.
- A breast flange that is too small or too large in size can hurt your milk supply.
- Pregnancy
- Breast reduction surgery may reduce milk supply.
If You Notice Your Milk Supply Is Low
You can increase your milk supply by:
- Nursing your baby often. Nurse every 2 hours during the day and every 3 to 4 hours at night (at least 8 to 16 times in 24 hours). If your baby will not nurse, use a good quality double electric breast pump to increase milk production. Pumping after breastfeeding signals your body to produce more milk.
- Nurse your baby at least 15 minutes at each breast.
 Do not limit nursing time. If your baby falls asleep after one breast, wake him or her and offer the second breast. A few babies may benefit from nursing at one breast per feeding to increase the fat content of the feeding. Switch nursing- switching breasts several times during a feeding has been shown to increase milk supply.
Do not limit nursing time. If your baby falls asleep after one breast, wake him or her and offer the second breast. A few babies may benefit from nursing at one breast per feeding to increase the fat content of the feeding. Switch nursing- switching breasts several times during a feeding has been shown to increase milk supply. - Gently massage breast before and during feedings.
- Use relaxation techniques to reduce stress and promote the flow of breast milk.
- Provide skin to skin time with your baby for about 20 minutes after feeds. This “kangaroo care” has been shown to increase milk supply.
- Be sure baby is positioned and latched correctly.
- Offer both breasts at each feeding.
- Try breast compression during the feeding to help drain the breast.
- Pump immediately after breastfeeding during the day. Rest at night. Some mothers find that they get more milk if they pump for 5 minutes, rest for 5 minutes, and pump for another 10 minutes.
Talk to your doctor about using medication or the herb fenugreek.
Works Cited
Wambach, Karen and Riordan, Jan “Breastfeeding and Human Lactation”, Fifth edition, Jones & Bartlett, 2016.
Breastfeeding | Tervisliku toitumise informatsioon
According to the Nordic Nutrition Guidelines based on research and advice from the WHO, only breast milk is the optimal nutrition for the first six months of a child's life.
A healthy child does not need any other fluids or supplements.
An exception is vitamin D, which pediatricians recommend giving as a fat-soluble supplement from the second week of life for the first two years at 10 micrograms (5 drops, or 500 IU) per day to ensure better skeletal development during a period of rapid growth. If a breastfeeding mother is a vegan or vegetarian, she should ensure that her baby is getting enough vitamin B12 to avoid deficiency.
From the second half of the year, continuing breastfeeding, you should gradually begin to give solid food even if the child grows well and on milk alone.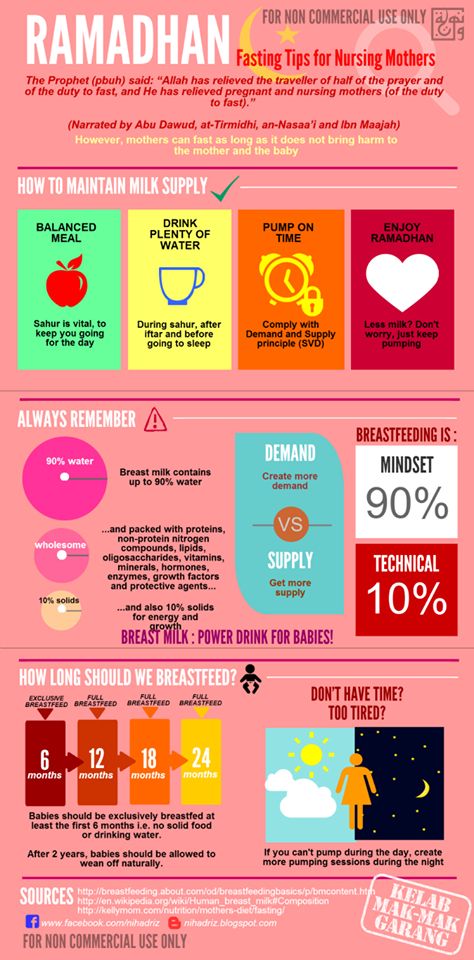 A gradual transition to family food should begin at the end of the first year of life. A one-year-old child should receive half of the energy from breast milk, half from spoon-feeding, mainly vegetables and fruits, cereals and meat. You can continue breastfeeding as long as it is comfortable for both mother and baby.
A gradual transition to family food should begin at the end of the first year of life. A one-year-old child should receive half of the energy from breast milk, half from spoon-feeding, mainly vegetables and fruits, cereals and meat. You can continue breastfeeding as long as it is comfortable for both mother and baby.
Nature is an amazing creator of food for a baby.
The mother's breast produces just the right product for a rapidly growing and developing baby. Breastfeeding soothes the baby, promotes the development of his oral cavity and the formation of bite. Breast milk is always at the right temperature, always clean and cheap. Feeding does not require any aids, you can feed your baby almost anywhere. All components of breast milk are easily absorbed and accepted by the baby and support its overall development. Breast milk is rich in nutrients and bioactive compounds such as vitamins, minerals, fatty acids, and immune factors that have been shown to be beneficial to human health. Breast milk differs during one feed, during the day, in summer and winter, and constantly changes with the age of the child.
Breast milk differs during one feed, during the day, in summer and winter, and constantly changes with the age of the child.
There is strong evidence that breastfeeding protects against overweight and many infections (ear, respiratory and digestive tract infections) in infancy and early childhood. Breast milk contains many protective factors that are thought to have an immunological effect for several years after breastfeeding has ended. Breastfeeding is likely to have a positive effect on a child's IQ and cognitive development, and this effect is related to the duration of breastfeeding. It is also considered likely that breastfeeding has a protective role against celiac disease if, even when the child receives breast milk, small amounts of gluten-containing foods are given to him. Comparing breastfed versus non-breastfed infants suggests a protective effect of breastmilk against type 1 and type 2 diabetes. There are indications that breastfeeding may reduce the risk of overweight and cardiovascular disease in adulthood.
Since breastfeeding is part of the normal postnatal process, it is also ideal for women. Feeding promotes faster uterine contraction and postpartum recovery.
When normal nutrition is continued, body weight decreases faster after pregnancy, since the body of a woman additionally spends more than 500 kcal on the production of breast milk. Certain foods (nuts, halva), as a rule, do not lead to an increase in the amount of breast milk, but only contribute to weight gain.
The amount of breast milk does not depend on the amount of food consumed by the mother. It depends on the frequency of breast emptying, the duration of feeding and the effectiveness of the sucking technique of the child. Pregnant women should not be without food for more than 12 hours. Otherwise, ketone bodies are formed in the blood, which are dangerous for the fetal brain. The situation can threaten the life of the fetus if the mother has not eaten for more than 20 hours.
Breastfeeding is an energy intensive process and many breastfeeding mothers are encouraged to increase their energy intake. However, in the case of a positive energy balance and low physical activity, there is a risk of overweight during the feeding period. To avoid postpartum weight gain, it is recommended to increase physical activity rather than decrease it during the feeding period. Nursing mothers have a lower risk of developing breast and uterine cancer at a young age, and the risk of osteoporosis later in life also decreases. During the feeding period, it is recommended to consume amounts of liquid proportional to the amount of milk produced. The amount of 750 ml of breast milk during the first six months increases the need for fluid in a nursing mother by about 600-700 ml per day.
Feeding creates a particularly close relationship with the baby, nighttime feedings are more comfortable, and studies show that breastfeeding mothers are less likely to experience postpartum depression.
98% of women can breastfeed, however, according to Estonian statistics, only 40% of our children receive breast milk at the age of 6 months. Many common myths about breast milk and breastfeeding can also prevent successful feeding.
Golden rules for feeding:
- The whole body is turned towards the mother, the mother supports the child behind the back (not behind the head!), pressing his stomach tightly to her own, maintaining closeness.
- Before taking the breast, the baby's nose is at the nipple.
- The child's jaw and nose are pressed against the chest, the lower lip is turned down, the cheeks are puffed out.
- Sucking alternates with swallowing.
- If the mother is sitting while breastfeeding, the baby should be on a cushion so that the mother can sit as freely and relaxed as possible, with a straight back, leaning on something, neck and shoulders relaxed.
- The child asks for breasts at least eight times a day and calms down after feeding.
- Every day the child urinates profusely and in the first month of life begins to poop at least once a day.
- Monthly weight gain of the child is at least 500-600 grams, the child grows in length, and every month his head circumference increases.
Sometimes breastfeeding may be contraindicated for health reasons of the mother or child. Then, during the first year of life, the child should be given milk mixtures and make sure that they are prepared in strict accordance with the instructions on the package. It is impossible to give cow's milk to a baby in the first year of life.
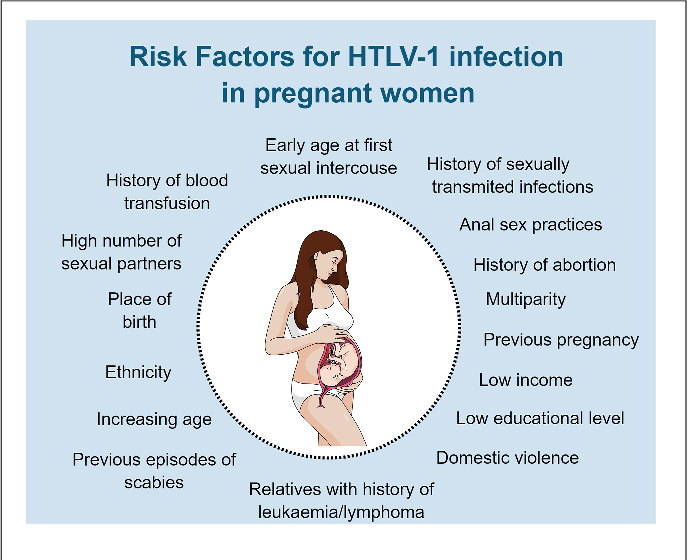
Do not breastfeed if:
- Baby has a rare metabolic disorder - galactosemia,
- The mother has a dangerous infectious disease: HIV, AIDS or acute incurable tuberculosis,
- The mother must take medicines that pass into milk - for example , anti-cancer, lithium, ergotamine, methotrexate, tranquilizers or sleeping pills,
- Mother is addicted to drugs.

Feeding may be difficult if:
- Women has a rare lack of glandular tissue or damage to the nerves of the nipple due to trauma or surgery that change the taste of breast milk, can reduce the amount and cause anxiety in the baby,
- The baby has health problems (cleft lip or palate, Down's syndrome, serious heart disease),
- The child has a very severe allergy.
In case of problems, contact your midwife or family doctor. In maternity hospitals, you can get help with consultations on feeding, you can also consult by phone.
Ida-Tallinn Central Hospital Breastfeeding Advice Center open on weekdays from 10:00 to 14:00, telephone 6207453 or 53041783
Tel.0082 – 666 5829
How can breastfeeding mothers increase their milk supply? - an article in the blog of the medical center Health for Children in Moscow
Breastfeeding is the key to good health and mental peace of the child for years to come.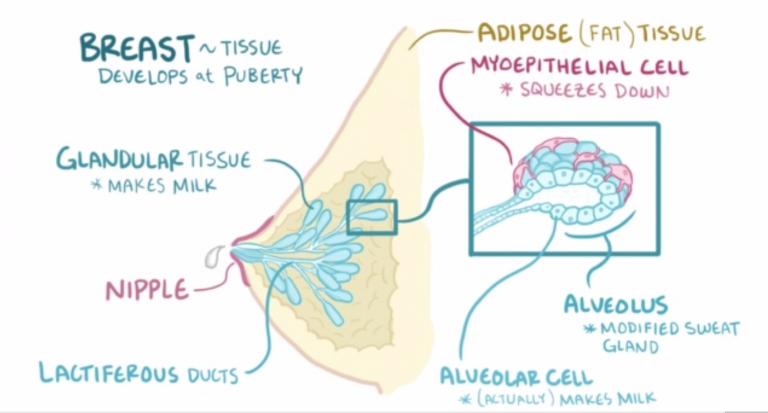 But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your baby. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your baby. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
The problem of lack of milk can occur both in the early neonatal period, when lactation is becoming established, and later, for example, during lactation crises, which can occur at certain periods of time (3-6 weeks, 3-4 months, 6 months), as well as after temporary weaning during the mother’s illness or the need to take certain medications that are incompatible with breastfeeding.
Ways to increase lactation:
- Feeding on demand , especially in early lactation. Frequent feedings in the first weeks of life are essential for maximizing the number of prolactin receptors to ensure sufficient milk production in the long term.
 Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth. If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months.
Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth. If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months. - Proper breastfeeding. The baby must include both the nipple and areola. His mouth should be wide open with his lower lip turned outward
- You can use post-feeding pumping which will increase milk production. And at the same time, freeze milk to create a reserve in case the mother leaves or a case of illness in which it is necessary to interrupt breastfeeding.
- Rational nutrition of a nursing woman. The menu should contain cereals, vegetables, fish, meat, eggs, fruits, dairy products are better than sour-milk, a small amount of nuts is acceptable. The use of strict hypoallergenic diets in a woman without an allergic history is unacceptable.
 Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk.
Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk. - Drinking enough liquid - water, green tea, compotes, fruit drinks. Drinks should preferably be warm or hot. It is recommended to take liquid 20-40 minutes before feeding.
- Avoid alcohol, nicotine, including passive smoking.
- Compliance with the rest regimen , psycho-emotional peace, positive attitude. This is largely determined by the attitude of close people who can help a nursing mother in household chores, caring for other children, etc.
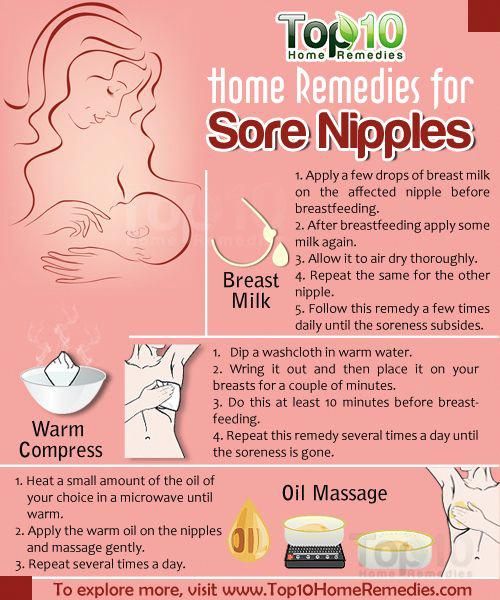
- Warm shower, light breast massage just before feeding.
- If you still need supplementary feeding, then it is better to give it with a pipette, spoon, syringe without a needle.
- Pharmacy products: Laktogon, Femilak. From herbs, galega, cumin, anise are considered safe. However, relying only on these funds is not worth it if the above points are not observed.