Reason for random nose bleeds
Nosebleed causes & treatments | NHS inform
Most nosebleeds can be stopped without the need for medical attention, but occasionally further treatment may be required.
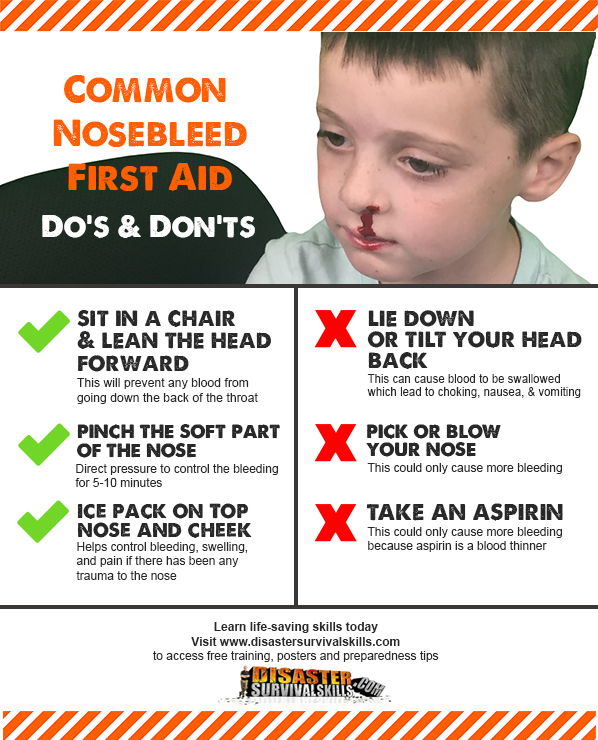
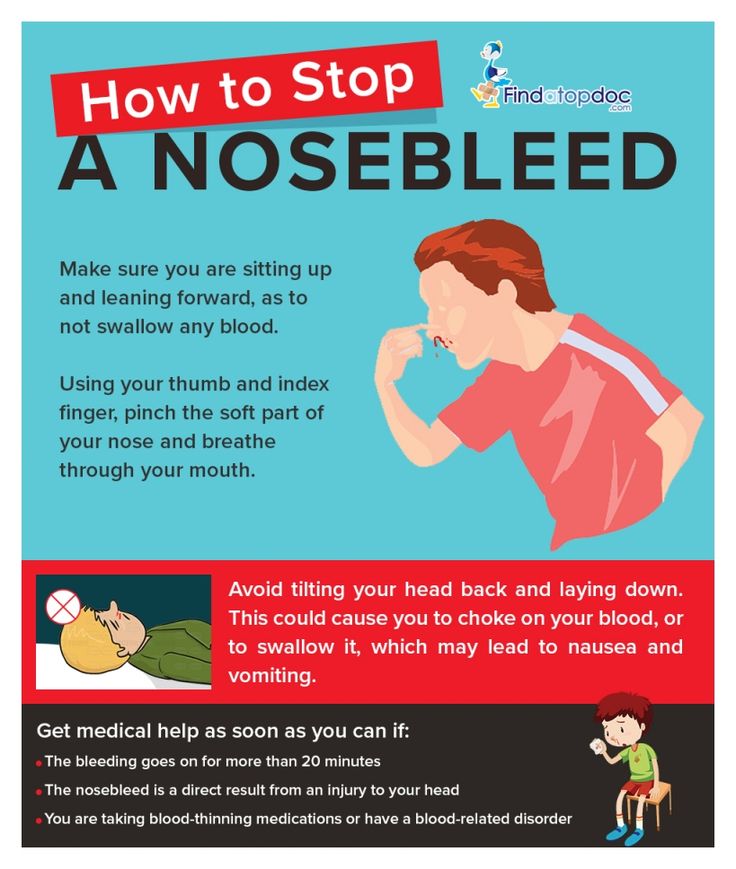
What to do
To stop a nosebleed:
- sit down and firmly pinch the soft part of your nose, just above your nostrils, for at least 10-15 minutes
- lean forward and breathe through your mouth – this will drain blood into your nose instead of down the back of your throat
- place an ice pack or bag of frozen vegetables covered by a towel on the bridge of your nose
- stay upright, rather than lying down as this reduces the blood pressure in the blood vessels of your nose and will discourage further bleeding
If the bleeding eventually stops, you won't usually need to seek medical advice. However, you should still follow the recovery advice outlined below.
When to seek medical advice
Contact your GP or call the NHS 111 service if:
- you're taking a blood-thinning medicine (anticoagulant) such as warfarin or have a clotting disorder such as haemophilia and the bleeding doesn't stop
- you have symptoms of anaemia such as heart palpitations, shortness of breath and a pale complexion
- a child under two years of age has a nosebleed (this is rare and there's a chance it's caused by something serious)
- you have nosebleeds that come and go regularly
Ask someone to drive you to your nearest accident and emergency (A&E) department or call 999 for an ambulance if:
- the bleeding continues for longer than 20 minutes
- the bleeding is heavy and you've lost a lot of blood
- you're having difficulty breathing
- you swallow a large amount of blood that makes you vomit
- the nosebleed developed after a serious injury, such as a car crash
Find your nearest A&E department
Medical treatment
If you see your GP or go to hospital with a nosebleed, you will be assessed to determine how serious your condition is and what's likely to have caused it. This may involve looking inside your nose, measuring your pulse and blood pressure, carrying out blood tests and asking about any other symptoms you have.
The main treatments that your GP or hospital doctor may use to stop your nose bleeding are described below.
Antibiotic ointment
Your doctor may prescribe an antibiotic ointment. This should be applied by squeezing a pea-sized amount onto the front of the nasal septum (wall between the nostrils).
This can reduce the inflammation and crusting in the nose and reduce the severity and frequency of nosebleeds.
Antibiotic ointment is particularly effective in children.
Cautery
If your doctor is able to identify exactly where the bleeding is coming from, they may carry out a minor procedure to seal the bleeding blood vessel by cauterising (burning) it.
This is normally done using a stick of a chemical called silver nitrate. A local anaesthetic will be sprayed into your nose to numb it and the silver nitrate stick will be held against the bleeding point for up to 10 seconds.
Nasal packing
If cautery is ineffective or your doctor is unable to identify a specific bleeding point, they may recommend packing your nose with gauze or special nasal sponges to stop the flow of blood by applying pressure to the source of the bleeding.
Packing will usually be carried out after local anaesthetic has been sprayed into your nose. The gauze or sponges often need to be left in place for 24-48 hours before being removed by a health professional. You'll usually need to be admitted to hospital to be monitored during this time.
Further treatment
If the treatments above don't help, you may be referred to a hospital specialist such as an ear, nose and throat (ENT) doctor for further treatment.
Additional treatments that may be used in hospital include:
- electrocautery – an electric current running through a wire is used to cauterise the blood vessel where the bleeding is coming from
- blood transfusions – a procedure to replace the blood you've lost
- tranexamic acid – medication that can reduce bleeding by helping your blood to clot
- packing under anaesthetic – your nose is carefully packed with gauze while you are unconscious from general anaesthetic
- ligation – an operation using small instruments to tie off bleeding blood vessels in the back of your nose
Recovery
Once your nose has stopped bleeding, you should follow the advice below to reduce the risk of your nose bleeding again and to stop you picking up an infection:
- avoid blowing or picking your nose, heavy lifting, strenuous exercise, lying flat, and drinking alcohol or hot drinks for 24 hours
- don't remove any crusts that form inside your nose – these may be unpleasant, but they're a useful part of the healing process
- if you need to sneeze, try to sneeze with your mouth open to reduce the pressure in your nose
- avoid people with coughs and colds
If you see a GP or a hospital doctor about your nosebleed, they may give you a prescription for an antiseptic nasal cream once the bleeding stops.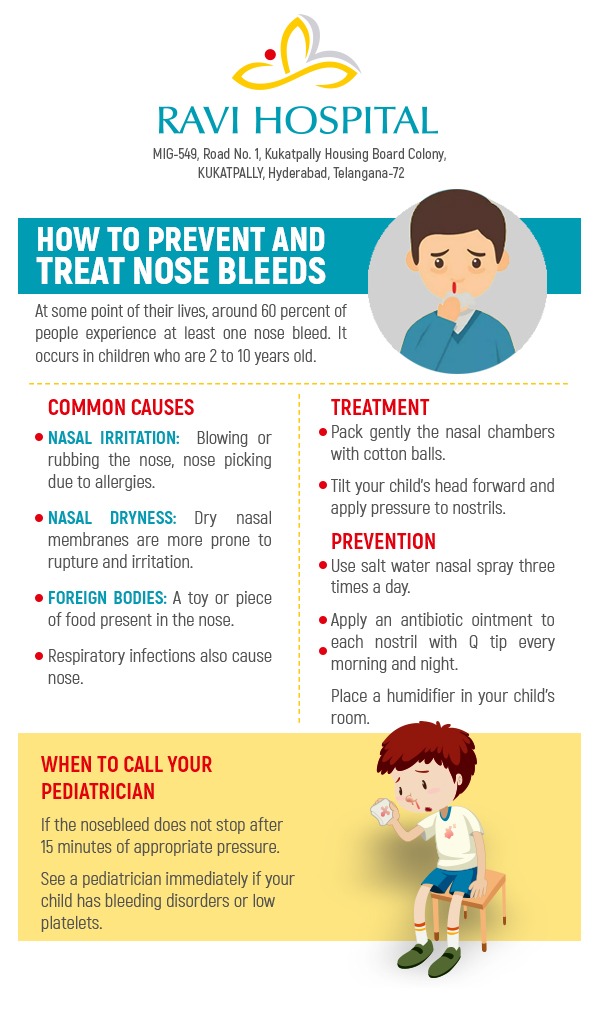 This should be applied to the inside of your nostrils several times a day for up to two weeks to help prevent further bleeding.
This should be applied to the inside of your nostrils several times a day for up to two weeks to help prevent further bleeding.
If your nose does start to bleed again, follow the first aid advice above and seek medical advice if the bleeding doesn't stop.
Iron deficiency anaemia - Illnesses & conditions
See all parts of this guide Hide guide parts
- 1. About iron deficiency anaemia
- 2. Causes of iron deficiency anaemia
-
3.
 Diagnosing iron deficiency anaemia
Diagnosing iron deficiency anaemia
- 4. Treating iron deficiency anaemia
- 5. Complications of iron deficiency anaemia
About iron deficiency anaemia
Iron deficiency anaemia is a condition where a lack of iron in the body leads to a reduction in the number of red blood cells.
Iron is used to produce red blood cells, which help store and carry oxygen in the blood. If you have fewer red blood cells than is normal, your organs and tissues won't get as much oxygen as they usually would.
There are several different types of anaemia, and each one has a different cause. Iron deficiency anaemia is the most common type.
Other types of anaemia can be caused by a lack of vitamin B12 or folate in the body – read more about vitamin B12 and folate deficiency anaemia.
Symptoms of iron deficiency anaemia
Many people with iron deficiency anaemia only have a few symptoms. The severity of the symptoms largely depends on how quickly anaemia develops.
You may notice symptoms immediately, or they may develop gradually if your anaemia is caused by a long-term problem, such as a stomach ulcer.
The most common symptoms include:
- tiredness and lack of energy (lethargy)
- shortness of breath
- noticeable heartbeats (heart palpitations)
- a pale complexion
Less common symptoms include:
- headache
- hearing sounds that come from inside the body, rather than from an outside source (tinnitus)
- an altered sense of taste
- feeling itchy
- a sore or abnormally smooth tongue
- hair loss
- a desire to eat non-food items, such as ice, paper or clay (pica)
- difficulty swallowing (dysphagia)
- painful open sores (ulcers) on the corners of your mouth
- spoon-shaped nails
When to see your GP
See your GP if you experience symptoms of iron deficiency anaemia. They should be able to diagnose the condition using a simple blood test.
They should be able to diagnose the condition using a simple blood test.
Read more about diagnosing iron deficiency anaemia
What causes iron deficiency anaemia?
There are many things that can lead to a lack of iron in the body. In men and post-menopausal women, the most common cause is bleeding in the stomach and intestines.
This can be caused by a stomach ulcer, stomach cancer, bowel cancer, or by taking non-steroidal anti-inflammatory drugs (NSAIDs).
In women of reproductive age, heavy periods and pregnancy are the most common causes of iron deficiency anaemia as your body needs extra iron for your baby during pregnancy.
Unless you're pregnant, it's rare for iron deficiency anaemia to be caused just by a lack of iron in your diet. However, if you do lack dietary iron, it may mean you're more likely to develop anaemia than if you have one of the problems mentioned above.
Read more about the causes of iron deficiency anaemia
How iron deficiency anaemia is treated
Treatment for iron deficiency anaemia involves taking iron supplements to boost the low levels of iron in your body. This is usually effective, and the condition rarely causes long-term problems.
This is usually effective, and the condition rarely causes long-term problems.
You'll need to be monitored every few months to check the treatment is working and your iron levels have returned to normal.
The underlying cause will need to be treated so you don't get anaemia again. Increasing the amount of iron in your diet may also be recommended.
Good sources of iron include:
- dark-green leafy vegetables, such as watercress and curly kale
- iron-fortified cereals or bread
- brown rice
- pulses and beans
- nuts and seeds
- meat, fish and tofu
- eggs
- dried fruit, such as dried apricots, prunes and raisins
Read more about treating iron deficiency anaemia
Further problems
If iron deficiency anaemia is left untreated, it can make you more susceptible to illness and infection, as a lack of iron affects the body's natural defence system (the immune system).
Severe iron deficiency anaemia may increase your risk of developing complications that affect the heart or lungs, such as an abnormally fast heartbeat (tachycardia) or heart failure, where your heart is unable to pump enough blood around your body at the right pressure.
Pregnant women with severe or untreated anaemia also have a higher risk of complications before and after birth.
Read more about the complications of iron deficiency anaemia
Causes of iron deficiency anaemia
Iron deficiency anaemia occurs when the body doesn't have enough iron, leading to the decreased production of red blood cells. Red blood cells carry oxygen around the body.
A lack of iron can be caused by several factors. Some of the most common causes of iron deficiency anaemia are outlined below.
Monthly periods
In women of reproductive age, periods are the most common cause of iron deficiency anaemia.
Usually, only women with heavy periods develop iron deficiency anaemia. If you have heavy bleeding over several consecutive menstrual cycles, it's known as menorrhagia.
Pregnancy
It's also very common for women to develop iron deficiency during pregnancy.
This is because your body needs extra iron to ensure your baby has a sufficient blood supply and receives necessary oxygen and nutrients.
Some pregnant women require an iron supplement, while others may need to increase the amount of iron in their diet.
Read more about vitamins and minerals in pregnancy
Gastrointestinal blood loss
The gastrointestinal tract is the part of the body responsible for digesting food. It contains the stomach and intestines.
Bleeding in the gastrointestinal tract is the most common cause of iron deficiency anaemia in men, as well as women who've experienced the menopause (when monthly periods stop).
Most people with gastrointestinal bleeding don't notice any obvious blood in their stools and don't experience any changes in their bowel habits.
Some causes of gastrointestinal bleeding are described below.
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs (NSAIDs) can cause bleeding in the stomach. Ibuprofen and aspirin are two commonly prescribed NSAIDs.
If your GP thinks your medication is causing gastrointestinal bleeding, they can prescribe a less harmful medicine. However, don't stop taking a medicine you've been prescribed unless your GP advises you to.
However, don't stop taking a medicine you've been prescribed unless your GP advises you to.
Stomach ulcers
The acid in your stomach, which helps your body digest food, can sometimes eat into your stomach lining. When this happens, the acid forms an open sore (an ulcer). This is also known as a stomach ulcer or a peptic ulcer.
Stomach ulcers can cause the stomach lining to bleed, which can lead to anaemia. In some cases, the bleeding can cause you to vomit blood or pass blood in your stools. However, if the ulcer bleeds slowly, you may not have any symptoms.
Gastrointestinal cancer
In a few cases, gastrointestinal bleeding can be caused by cancer, usually stomach cancer or bowel cancer.
When trying to establish the cause of anaemia, your GP will check for possible signs of cancer.
If your GP suspects cancer, you'll be referred to a gastroenterologist (a specialist in treating digestive conditions) for a more thorough examination. This means that if cancer is found, it can be treated as quickly as possible.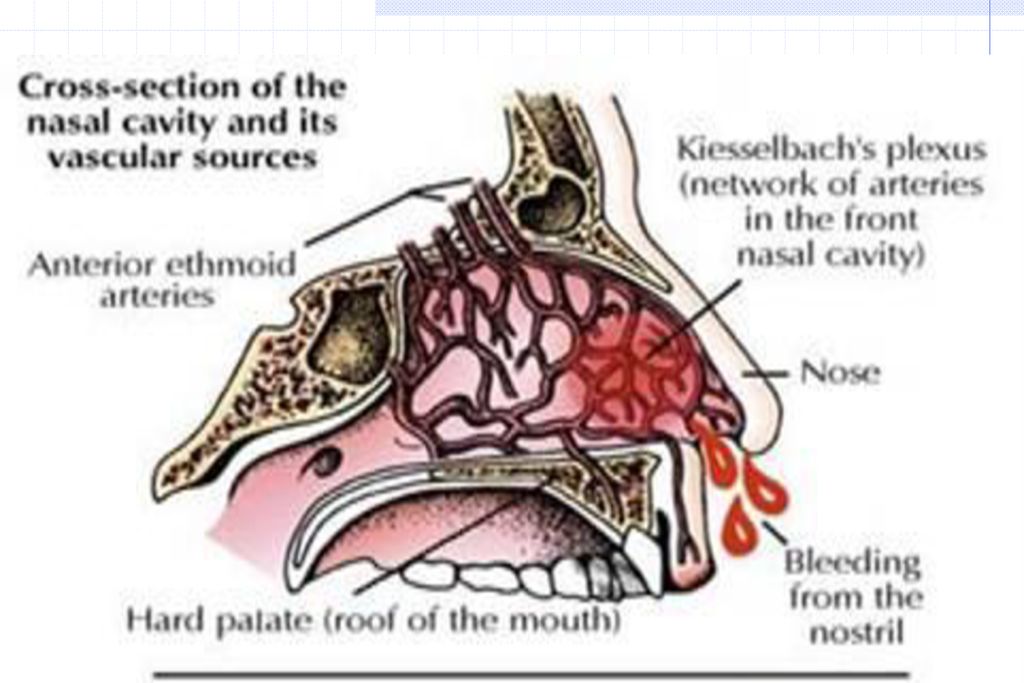
If you're 60 years old or over and have iron deficiency anaemia, your GP should refer you to a specialist to rule out bowel cancer. Your appointment with the specialist should be within two weeks of your GP referring you.
Angiodysplasia
Gastrointestinal bleeding can also be caused by a condition called angiodysplasia. This is the result of abnormal, fragile superficial blood vessels in the gastrointestinal tract, which can cause bleeding.
Chronic kidney disease
People with chronic kidney disease (CKD) often develop iron deficiency anaemia.
Most people with CKD who have iron deficiency anaemia will be given iron supplement injections, although daily tablets may be tried first.
You can read more about treating anaemia in people with CKD on the National Institute for Health and Care Excellence (NICE) website.
Other causes
Other conditions or actions that cause blood loss and may lead to iron deficiency anaemia include:
- inflammatory bowel disease – a condition that causes redness and swelling (inflammation) in the digestive system, such as Crohn's disease and ulcerative colitis
- oesophagitis – inflammation of the gullet (oesophagus) caused by stomach acid leaking through it
- schistosomiasis – an infection caused by parasites, mainly found in sub-Saharan Africa
- blood donation – donating a large amount of blood may lead to anaemia
- trauma – a serious accident, such as a car crash, may cause you to lose a large amount of blood
- nosebleeds – having regular nosebleeds may lead to anaemia, although this is rare
- haematuria (blood in your urine) – but this rarely causes anaemia and may be a symptom of another condition
Malabsorption
Malabsorption is when your body can't absorb iron from food, and is another possible cause of iron deficiency anaemia.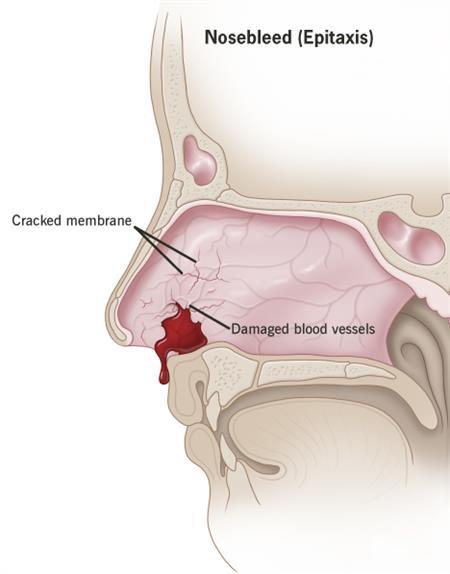
This may happen if you have coeliac disease, a common digestive condition where a person has an adverse reaction to gluten, or surgery to remove all or part of your stomach (gastrectomy).
Lack of iron in your diet
Unless you're pregnant, it's rare for iron deficiency anaemia to be caused solely by a lack of iron in your diet.
However, a lack of dietary iron can increase your risk of developing anaemia if you also have any of the conditions mentioned above.
Some studies suggest vegetarians or vegans are more at risk of iron deficiency anaemia because of the lack of meat in their diet.
If you are vegetarian or vegan, it is possible to gain enough iron by eating other types of food, such as:
- beans
- nuts
- dried fruit, such as dried apricots
- wholegrains, such as brown rice
- fortified breakfast cereals
- soybean flour
- most dark-green leafy vegetables, such as watercress and curly kale
If you're pregnant, you may need to increase the amount of iron-rich food you consume during pregnancy to help prevent iron deficiency anaemia.
Read more about vegetarian and vegan diets
Diagnosing iron deficiency anaemia
See your GP if you experience symptoms of iron deficiency anaemia, such as tiredness, shortness of breath and heart palpitations.
A simple blood test can usually confirm the diagnosis.
Your GP may also carry out a physical examination and ask you a number of questions to help determine the cause of your anaemia.
Blood test
To diagnose iron deficiency anaemia, a blood sample is taken from a vein in your arm and a full blood count is made. This means all the different types of blood cells in the sample will be measured.
If you have anaemia:
- your levels of haemoglobin – a substance that transports oxygen – will be lower than normal
- you'll have fewer red blood cells, which contain haemoglobin, than normal
- your red blood cells may be smaller and paler than usual
Your GP may also test for a substance called ferritin, a protein that stores iron.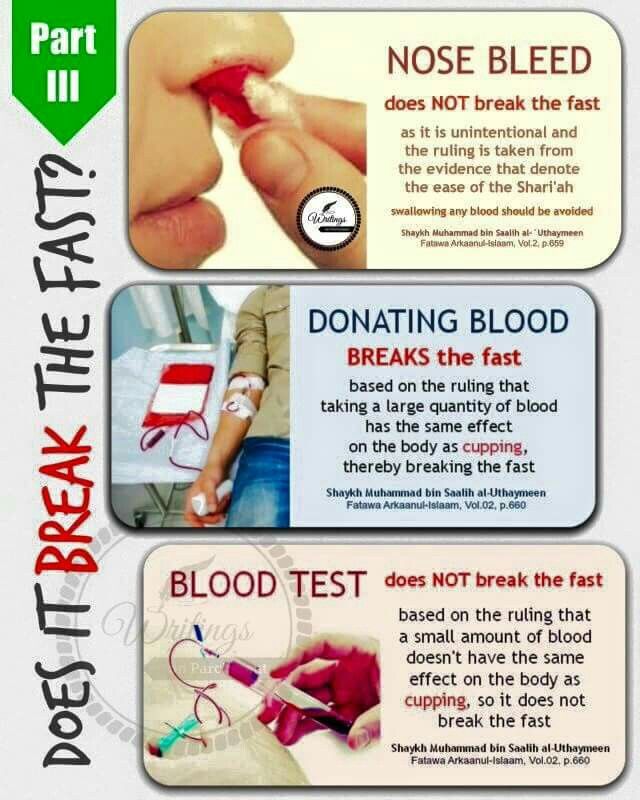 If your ferritin levels are low, it means there isn't much iron stored in your body and you may have iron deficiency anaemia.
If your ferritin levels are low, it means there isn't much iron stored in your body and you may have iron deficiency anaemia.
Read more about blood tests
Vitamin B12 and folate deficiency
If your GP thinks your anaemia may be the result of a vitamin B12 and folate deficiency, the levels of these substances may be tested. Folate works with vitamin B12 to help your body produce red blood cells.
Vitamin B12 and folate deficiency anaemia is more common in people who are over the age of 75.
Finding the cause
To determine the underlying cause of your anaemia, your GP may ask questions about your lifestyle and medical history. For example, they may ask you about:
- your diet – to see what you typically eat and whether this includes any iron-rich foods
- any medicines you take – to see if you've been regularly taking a type of medicine that can cause bleeding from the stomach and intestines (gastrointestinal bleeding), such as ibuprofen or aspirin
- your menstrual pattern – if you're a woman, your GP may ask if you've been experiencing particularly heavy periods
- your family history – you'll be asked if your immediate family has anaemia or a history of gastrointestinal bleeding or blood disorders
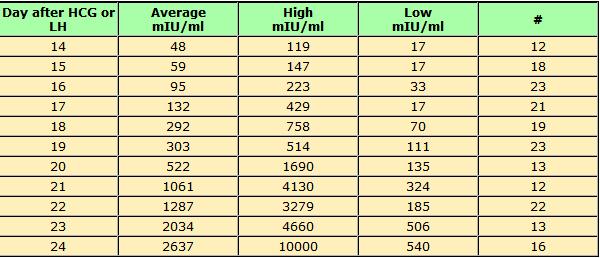
Iron deficiency anaemia is common during pregnancy.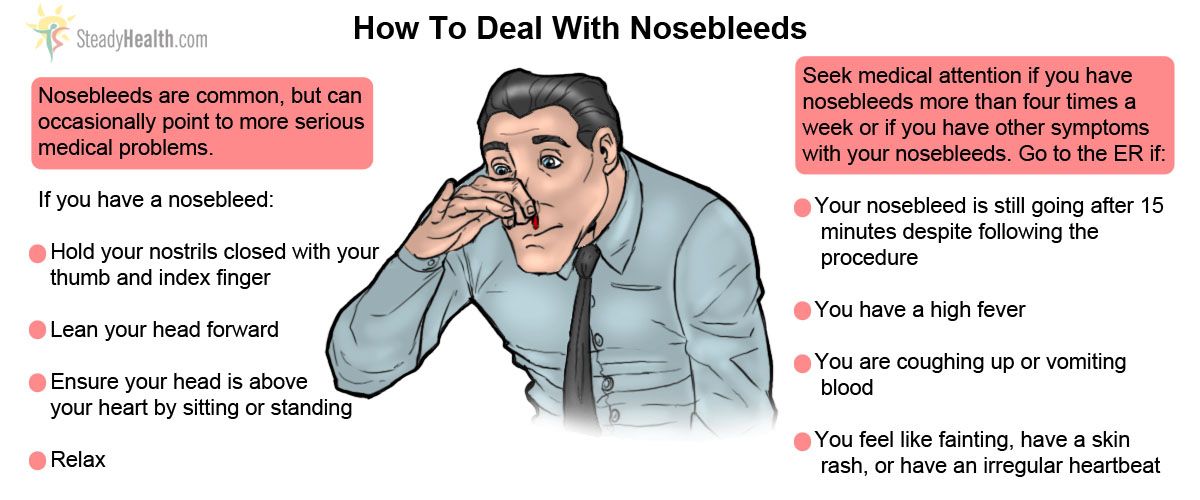 If you're pregnant, your GP will usually only look for an alternative cause if a blood test has identified a particularly low haemoglobin level, or if your symptoms or medical history suggest your anaemia may be caused by something else.
If you're pregnant, your GP will usually only look for an alternative cause if a blood test has identified a particularly low haemoglobin level, or if your symptoms or medical history suggest your anaemia may be caused by something else.
Physical examination
A physical examination will usually only be needed if the cause of your iron anaemia deficiency hasn't been identified by examining your medical history and asking you about your symptoms.
In such cases, your GP may:
- examine your stomach (abdomen) to check for any physical signs of gastrointestinal bleeding
- look for signs of heart failure, such as swollen ankles – heart failure can have some similar symptoms to iron deficiency anaemia
Two other possible types of physical examination you may have are explained below.
Rectal examination
A rectal examination is usually only needed if you're bleeding from your bottom. It's a common procedure that can help your GP find out if there's something in your gastrointestinal tract that's causing bleeding.
Your GP will insert a lubricated gloved finger into your bottom to feel for any abnormalities.
A rectal examination isn't something to be embarrassed about, as it's a procedure your GP will be used to doing. It shouldn't cause significant pain, but it may cause some slight discomfort – this will only last for a minute.
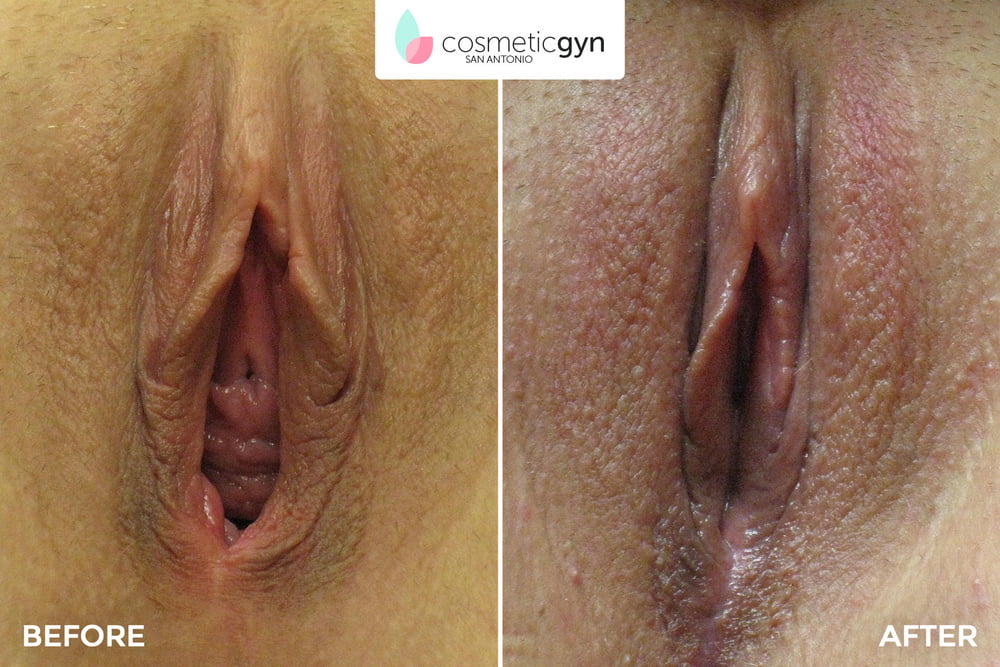
Pelvic examination
Women may have a pelvic examination if their GP thinks heavy menstrual bleeding (menorrhagia) may be the cause of their anaemia.
During a pelvic examination, your GP will examine your vulva and labia (external sex organs) for signs of bleeding or infection.
They may also examine you internally. This will involve your GP inserting lubricated gloved fingers into your vagina to feel whether your womb (uterus) is tender or enlarged.
A pelvic examination won't be carried out without your consent (permission), and you can choose to have someone with you.
Referral to a specialist
In some cases, your GP may refer you to a gastroenterologist, a specialist in treating digestive conditions.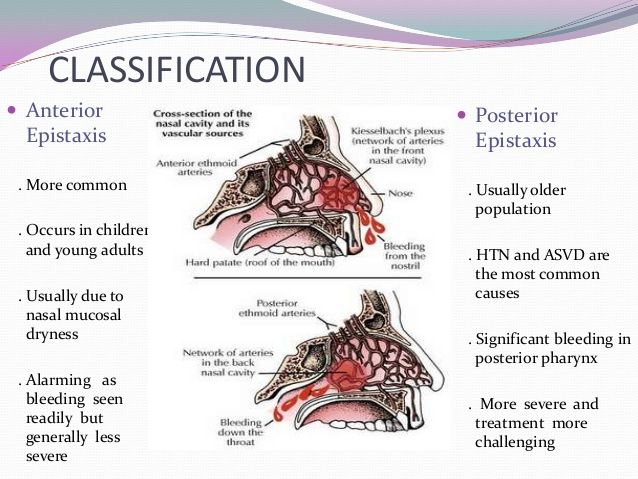 They'll carry out a more thorough examination.
They'll carry out a more thorough examination.
For example, you may be referred to a gastroenterologist if your GP can't identify a cause and you have a particularly low haemoglobin level, or if your GP thinks there's a possibility your symptoms could be caused by stomach cancer or bowel cancer, although this is unlikely.
If you're a woman with heavy periods, you may be referred to a gynaecologist if you don't respond to treatment with iron supplements.
Treating iron deficiency anaemia
Treatment for iron deficiency anaemia usually involves taking iron supplements and changing your diet to increase your iron levels, as well as treating the underlying cause.
Iron supplements
Your GP will prescribe an iron supplement to restore the iron missing from your body. The most commonly prescribed supplement is ferrous sulphate, which is taken as a tablet, usually twice a day.
Some people can experience side effects when taking iron supplements, including:
- abdominal (tummy) pain
- constipation or diarrhoea
- heartburn
- feeling sick
- black stools (faeces)
These side effects should settle down over time. However, your GP may recommend taking the tablets with food or shortly after eating if you have troublesome side effects.
However, your GP may recommend taking the tablets with food or shortly after eating if you have troublesome side effects.
Your GP may also advise you to only take one or two tablets a day, instead of three, if you're finding side effects difficult to cope with.
If you can't take ferrous sulphate because you get severe side effects, you may be prescribed a different iron supplement called ferrous gluconate.
This supplement should cause fewer side effects because it contains a less concentrated dose of iron. However, it may take longer for the iron levels in your body to be restored.
In a few cases – for example, if you have chronic kidney disease (CKD) – iron injections may be recommended instead of tablets.
As with all medications, it's important to store iron supplements out of the reach of children. An overdose of iron supplements in a young child can be fatal.
Dietary advice
If a lack of iron in your diet is thought to be contributing to your iron deficiency anaemia, your GP will tell you how to up your intake.
Iron-rich foods include:
- dark-green leafy vegetables, such as watercress and curly kale
- iron-fortified cereals or bread
- brown rice
- pulses and beans
- nuts and seeds
- white and red meat
- fish
- tofu
- eggs
- dried fruit, such as dried apricots, prunes and raisins
Your diet should include foods from all the major food groups to ensure it's healthy and balanced. In particular, food and drink containing vitamin C are important as vitamin C helps your body absorb iron.
However, consuming large amounts of some foods and drinks, as well as certain medicines, may make it harder for your body to absorb iron. These include:
- tea and coffee
- calcium – found in dairy products, such as milk
- antacids and proton pump inhibitors (PPIs) – medications used to relieve indigestion
- wholegrain cereals – although wholegrains are a good source of iron themselves, they contain phytic acid, which can stop your body absorbing iron from other foods and pills
You may be referred to a nutrition specialist called a dietitian if you're finding it difficult to include iron in your diet. They'll be able to give you detailed, personalised advice about how you can improve your diet.
They'll be able to give you detailed, personalised advice about how you can improve your diet.
Treating the underlying cause
Your GP will also need to ensure the underlying cause of your anaemia is treated so it doesn't happen again.
For example, if non-steroidal anti-inflammatory drugs (NSAIDs) are causing bleeding in your stomach, your GP may prescribe a different medicine to help minimise the risk of stomach bleeding.
Heavy periods can be treated with medication or – in particularly severe cases – surgery.
Monitoring
Your GP will ask you to return two to four weeks after you've started taking iron supplements to check how well you've responded to the treatment. You'll have a blood test to check your haemoglobin levels.
If your blood test results show an improvement, you'll be asked to continue taking iron supplements and return in two to four months for another blood test.
Once your haemoglobin levels and red blood cells are normal, your GP will usually recommend continuing to take iron supplements for three months to help build up the iron levels in your body.
After this, you should be able to stop taking the supplements, depending on the cause of your iron deficiency anaemia. Your condition will be monitored every three months over the course of a year, and again a year later.
Continuing treatment
Sometimes after a person's iron levels have been replenished, they start to fall again.
This could happen if you don't get enough iron in your diet, you're pregnant, or you have consistently heavy periods.
In such cases, you may be prescribed an ongoing iron supplement to help stop your anaemia returning. This will usually be a tablet, which you'll have to take once a day.
If treatment is ineffective
If your iron levels don't improve, your GP will ask how regularly you've been taking your iron supplements.
Some people are put off taking the medication because of the side effects. However, your condition won't improve if you don't take the supplements.
If you've been taking the supplements as prescribed and your iron levels still haven't improved, your GP may refer you to a specialist for an assessment.
Complications of iron deficiency anaemia
Iron deficiency anaemia rarely causes serious or long-term complications, although some people with the condition find it affects their daily life.
Some common complications are outlined below.
Tiredness
Iron deficiency anaemia can make you feel tired and lacking in energy (lethargic). This may result in you being less productive at work, and you may find it difficult to stay awake or not feel able to exercise regularly.
Increased risk of infections
Research has shown iron deficiency anaemia can affect your immune system – the body's natural defence system. This increases your vulnerability to infection.
Heart and lung problems
Adults with severe anaemia may be at risk of developing complications that affect their heart or lungs.
For example, you may develop tachycardia, which is an abnormally fast heartbeat, or heart failure, where the heart fails to pump enough blood around your body at the right pressure.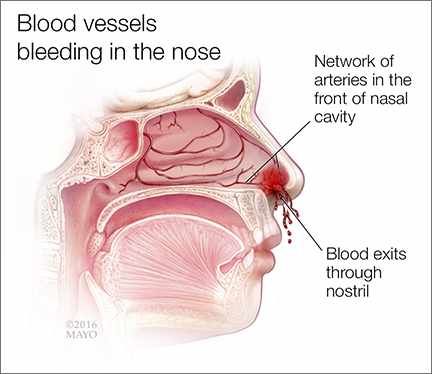
Pregnancy complications
Pregnant women with severe anaemia have an increased risk of developing complications, particularly during and after birth.
They may also develop postnatal depression, which some women experience after having a baby.
Research suggests babies born to mothers who have untreated anaemia are more likely to:
- be born prematurely – before the 37th week of pregnancy
- have a low birth weight
- have problems with iron levels themselves
- do less well in mental ability tests
Restless legs syndrome
Some cases of restless legs syndrome are thought to be caused by iron deficiency anaemia. Doctors often refer to this as secondary restless legs syndrome.
Restless legs syndrome is a common condition that affects the nervous system, and causes an overwhelming, irresistible urge to move the legs. It also causes an unpleasant feeling in the feet, calves and thighs.
Restless legs syndrome caused by iron deficiency anaemia can usually be treated with iron supplements.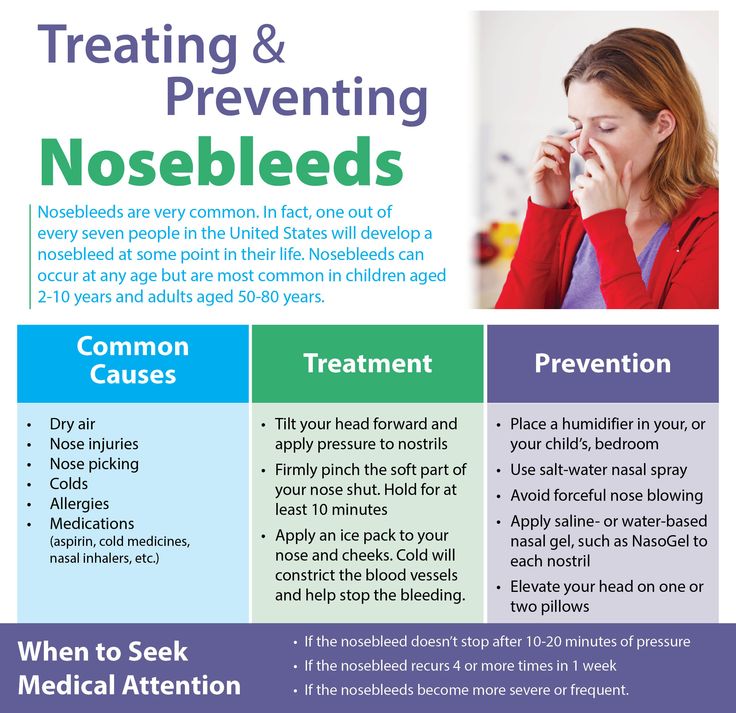
Epistaxis - City Hospital No. 40
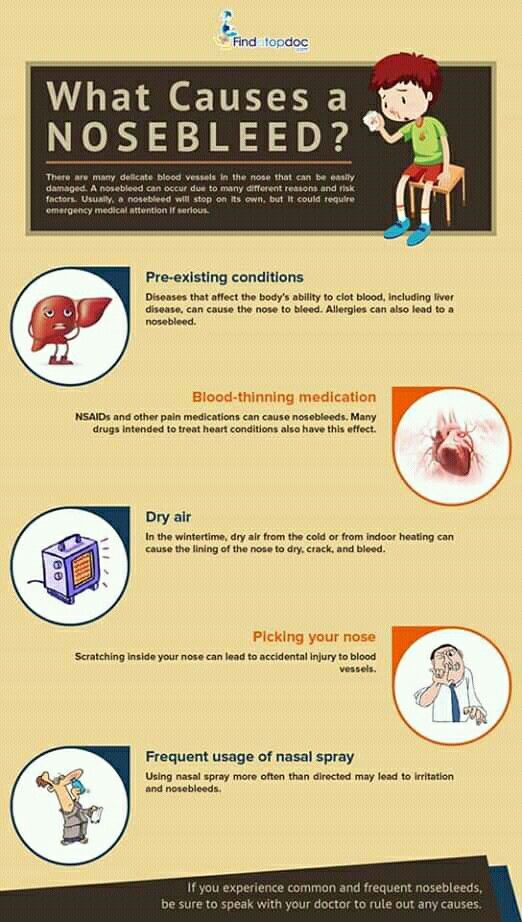
Nosebleed is a symptom of a local lesion of the nose or a general disease. The source of nosebleeds can be in different parts of the nose, but the most common bleeding site is the anteroinferior part of the nasal septum (Kisselbach's place). The most common cause of nosebleeds is trauma, which can be mild, causing minor bleeding, and major, with facial skeletal tissue damage, which can result in profuse, life-threatening bleeding.
The local cause of epistaxis can be surgical interventions, neoplasms, syphilitic or tuberculous ulcers.
Common causes of nosebleeds are diseases of the vascular system and blood (hypertension, heart defects, emphysema, diseases of the liver, spleen).
Severe bleeding from the nose occurs with hemorrhagic diathesis (hemophilia, hemorrhagic thrombasthenia, Werlhoff's disease, hemorrhagic vasculitis, etc.). The causes of nosebleeds in these diseases are heterogeneous: in some cases, the system of blood coagulation factors is disturbed, in others, the vascular wall is affected. Diseases of the hematopoietic organs (leukemia, reticulosis, etc.) can also be accompanied by bleeding from the nose.
Diseases of the hematopoietic organs (leukemia, reticulosis, etc.) can also be accompanied by bleeding from the nose.
Various other factors may play a role in the occurrence of nosebleeds:
- hypo- and beriberi;
- reduced atmospheric pressure;
- great physical exertion;
- body overheating, etc.
The discharge of blood from the nose in some patients begins unexpectedly, others note prodromal phenomena - headache, tinnitus, dizziness, itching or tickling in the nose. It must be borne in mind that blood can flow into the nose from other parts of the upper respiratory tract - the pharynx, larynx, trachea, lung, in rare cases from the middle ear through the auditory tube. With nosebleeds, the blood is clean, of a normal appearance, its flow down the back of the throat is clearly visible, especially when the head is thrown back.
Bleeding usually occurs from one side of the nose, but sometimes blood flows into the healthy side of the nose.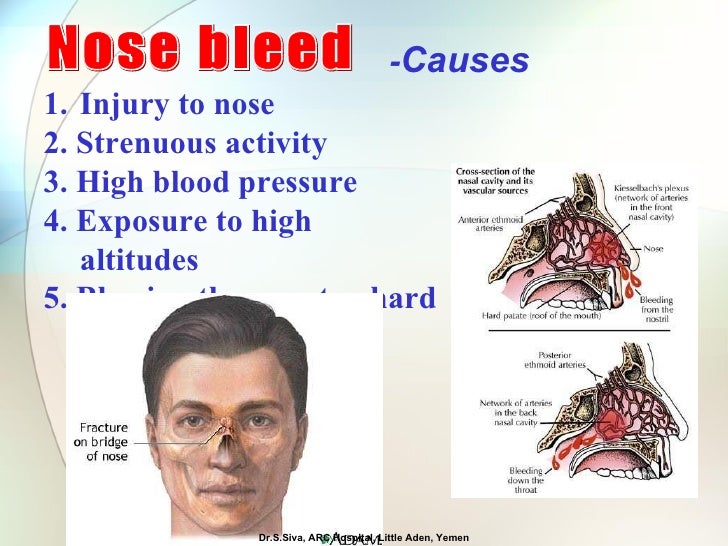 Distinguish:
Distinguish:
- insignificant;
- moderate;
- severe epistaxis.
Minor bleeding usually comes from the Kisselbach area: a few ml of blood is shed in drops for some time. Such bleeding often stops on its own. Outwardly harmless, but often recurring, long-term recurrent minor bleeding from the nose can have a particularly negative effect on a young organism.
Moderate epistaxis is characterized by more abundant bleeding (within 200 ml). At the same time, the change in hemodynamics is within the normal range.
In children and debilitated adults, external bleeding often does not give a complete picture of the true blood loss, since some of the blood flows into the throat and is swallowed. Insufficient assessment of this is fraught with serious complications: in such cases, profuse hematemesis usually occurs, blood pressure drops, and the pulse quickens.
With severe nosebleeds , the volume of blood lost per day exceeds 200 ml, sometimes reaching 1 liter or more. Such bleeding poses an immediate threat to life. Post-traumatic nosebleeds are often characterized not only by profuseness, but also by recurrence after a few days, and possibly even weeks. A large loss of blood during severe bleeding causes a drop in blood pressure, an increase in heart rate, a sharp general weakness, and sweating.
Such bleeding poses an immediate threat to life. Post-traumatic nosebleeds are often characterized not only by profuseness, but also by recurrence after a few days, and possibly even weeks. A large loss of blood during severe bleeding causes a drop in blood pressure, an increase in heart rate, a sharp general weakness, and sweating.
Treatment of nosebleeds
The simplest method of stopping nosebleeds is to introduce a ball of sterile cotton wool or gauze soaked in hydrogen peroxide solution into the anterior part of the bleeding half of the nose for 15-20 minutes. Stopping recurrent nosebleeds, as well as prolonged, massive bleeding, is carried out in a hospital using appropriate methods, such as cauterization of bleeding vessels, anterior and posterior nasal tamponade, if necessary, replenishment of the volume of circulating blood, erythrocytes, flooding of the body.
IMPORTANT!!! It must be remembered that repeated or recurrent nosebleeds are most often symptoms of any disease. Only a doctor can understand the causes of this condition, so the presence of bleeding is a mandatory indication for seeking medical help.
Only a doctor can understand the causes of this condition, so the presence of bleeding is a mandatory indication for seeking medical help.
Frequent nosebleeds: what are the causes and what to do?
Other related articles: otolaryngologist, therapist
-
"Sedentary" diseases
-
10 examinations
-
COVID-19
-
adenovirus infection
-
Adenoids
-
Angina
-
Anemia
-
Meniere's disease
-
Bronchitis
-
Bronchoscopy
-
Types of ELI tests
-
All about flu
-
Sinusitis
-
Nasal hemangioma
-
Hypertension
-
Flu and SARS
-
flu during pregnancy
Diarrhea (diarrhea)
-
Eustachitis
-
iron deficiency
-
Ear diseases
-
immunity to coronavirus
-
Nose curvature
-
Nosebleeds
-
Nosebleed
-
Laryngitis
-
Lungs after COVID
-
Treatment of adenoids
-
Lymphadenitis
-
ENT diseases in children
-
mastoiditis
-
Medical examinations
-
Uric acid
-
Runny nose
-
Nasal septum
-
Surveys in autumn
-
Complications after angina
-
Pneumonia
-
Defeat the Flu
-
Items in the nose
-
Taking antibiotics
-
Signs of COVID-19
-
Application of ozone
-
Washing lacunae
-
Rheumatism
-
Sinusitis
-
Vaccine testing
-
Tonsillitis
-
Tuberculosis
-
Sulfur Plug Removal
-
Tick bite
-
Bed bug bites
-
Pharyngitis
-
ferritin
-
Chronic fatigue
-
nasal endoscopy
Bleeding from the nose due to trauma usually does not raise questions, but if it occurs without any mechanical impact, and even more often, this should alert
What can be the causes of frequent nosebleeds and how they can be cured - tells otorhinolaryngologist of the clinic "Semeynaya" Olga Pavlovna Soloshenko.
If the bleeding does not occur from trauma and recurs periodically, it is better not to delay the visit to the ENT. After all, bleeding can be anterior and posterior - the second happens less often, but it is much more dangerous. With anterior bleeding, blood only goes out, with posterior bleeding, it flows into the mouth or stomach along the back of the pharynx. Posterior is usually caused by damage to larger vessels that are located deep in the nasal cavity. It is very difficult to stop back bleeding without a doctor.
Causes of nosebleeds:
- Injuries. Injury to the nose is often fraught with cartilage fractures. As a rule, this is accompanied by swelling and pain.
- High blood pressure. Very common cause. Due to a sharp jump, the walls of the capillaries easily burst. Pressure rises due to overload, as well as in the presence of diseases of the cardiovascular system.
- Sunstroke and any sudden increase in body temperature.
- Overwork.
- Hormonal changes. Bleeding may occur in women during the months of pregnancy or menopause, and in adolescents at puberty.
- Dry air. It causes dryness of the mucous membranes.
- Poor blood clotting.
- ENT diseases. Sinusitis, sinusitis, rhinitis - all of them can cause bleeding, especially with the constant use of drugs that thin the mucous membrane.
- Vascular problems. Even infectious diseases such as chickenpox, measles, influenza, etc. can lead to them.
- Polyps, adenoids, tumors. In addition to occasional bleeding, they simply make breathing difficult.
- Foreign body penetration - can damage mucous membranes and blood vessels.
- Deficiency of vitamins K, C and calcium.
First aid rules for nosebleeds:
- Lie down (or position the patient) with legs down
- Tilt your head forward
- Place a cold compress on the bridge of the nose for a few minutes
- Cover nose with hand or insert swab pre-moistened with hydrogen peroxide
- Drops for vasoconstriction can be instilled
Attention, this must not be done!
- Throwing the head back (contrary to popular belief) - blood can enter the respiratory tract
- Blow your nose - so as not to increase bleeding without it.
Which cases require an immediate call to a doctor and an ambulance
- In case of loss of consciousness
- For excessive bleeding
- Blood flows with clear fluid (this may occur after trauma and indicate a skull fracture)
- If vomiting of blood occurs (possibly indicating bleeding in the esophagus or stomach)
- Foamy blood (possible with lung injury)
- In a patient with diabetes mellitus
- If the patient is known to have poor blood clotting
Treatment
Treatment of bleeding is carried out in a complex manner. Often, an otorhinolaryngologist works in conjunction with a general practitioner, neurologist, endocrinologist, and hematologist.
At the first examination, the doctor determines the type of bleeding - anterior or posterior. Also, the patient is required to pass a general blood test and a coagulogram (analysis of blood coagulation indicators). In addition, it is important to measure the pressure, because if it is above the norm (the absolute norm is 120/80 mm Hg, but these figures change depending on age), the blood will not stop until it decreases.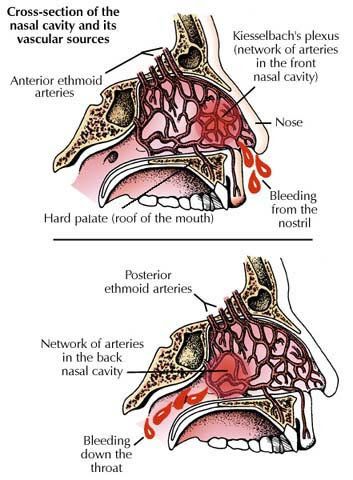
In case of significant blood loss, the patient may be left in the hospital.
As a treatment for bleeding, it is possible to pack the nasal cavity, cauterize vessels (with drugs, laser, ultrasound, etc.), remove polyps. If there is no result, surgical ligation of vessels in problem areas is performed. In addition, drugs are prescribed that increase blood clotting.
Prevention
- Taking drugs that strengthen the walls of blood vessels
- Nutrition rich in vitamins and minerals
- Air humidification during the heating season
- Injury Prevention
- Monitoring blood pressure and taking medications to lower it
Nosebleeds are not only unpleasant, but also dangerous. Therefore, as soon as it begins to bother you regularly, it is important to see a doctor as soon as possible. It is better to exclude all the most terrible causes of such a phenomenon as soon as possible and then it is already calmer to engage in further treatment.