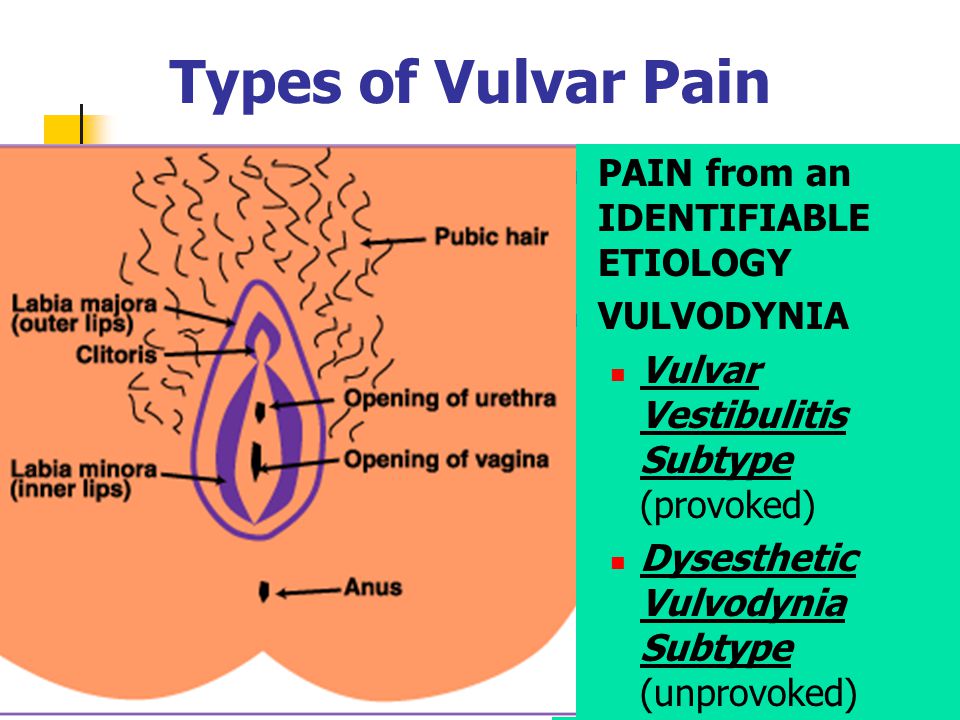
Irritated vulva during pregnancy
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women. Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.

- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.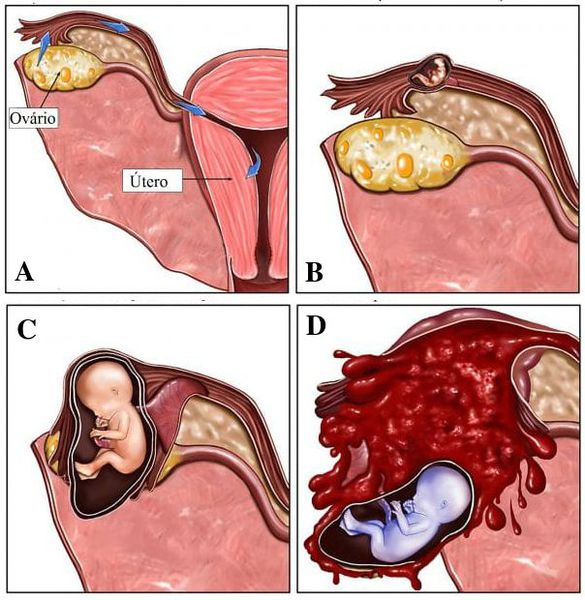
Vaginal thrush during pregnancy | Pregnancy Birth and Baby
Vaginal thrush during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Most women experience occasional bouts of a common yeast infection known as vaginal thrush. It causes itching, irritation and swelling of the vagina and surrounding area, sometimes with a creamy white cottage cheese-like discharge.
Vaginal thrush is fairly harmless, but it can be uncomfortable and it can keep coming back, which is known as recurrent thrush.
Thrush is a yeast infection, usually caused by a yeast-like fungus called 'Candida albicans'.
Many women have Candida in their vagina without it causing any symptoms. Hormones in vaginal secretions and 'friendly' vaginal bacteria keep the fungus under control. Problems arise when the natural balance in the vagina is upset and Candida multiplies.
Problems arise when the natural balance in the vagina is upset and Candida multiplies.
Vaginal thrush can sometimes be passed on during sex but is not considered a sexually transmitted infection (STI). However, if you have thrush it’s best to avoid having sex until you’ve completed a course of treatment and the infection has cleared up.
During pregnancy
You are more at risk of getting thrush while you're pregnant. Changes in the levels of female hormones, such as oestrogen, increase your chances of developing thrush and make it more likely to keep coming back.
There is no evidence that thrush affects your chances of getting pregnant.
If you're pregnant or breastfeeding and you have thrush, you should avoid taking oral anti-thrush treatments. Instead, use vaginal pessaries, plus an anti-thrush cream if necessary.
Treatment
If you have thrush and you're pregnant or breastfeeding, you should always visit your doctor rather than buying anti-thrush medication over the counter from a pharmacy.
You won’t be prescribed oral treatment because it may affect your baby. An anti-thrush pessary, such as clotrimazole, nystatin or miconazole will probably be prescribed to be used for about 3 to 7 days.
If you're pregnant, take care when inserting a pessary because there's a risk of injuring your cervix (neck of the womb). To reduce the risk, it may be better to insert the pessaries by hand instead of using the applicator.
If you have symptoms around your vulva, such as itching and soreness, you may also be prescribed an anti-thrush cream.
Not all of these products are safe to use at different stages of pregnancy, so it's important to talk to your doctor and pharmacist before using any products.
What can I do to prevent vaginal thrush?
There are a number of simple things you can do:
- Wear cotton or silk underwear rather than synthetics and change daily. Wear tights or stockings for as short a time as possible.
- Wash underwear in hot water and pure soap and double rinse to make sure any irritants are removed before you wear them.
- Change out of damp swimming costumes or sports clothes as soon as possible after swimming or exercise.
- If using pads, change them regularly and avoid perfumed or deodorised pads.
- Avoid tight fitting clothes such as jeans as this creates a moist, warm environment that encourages the overgrowth of bacteria and yeasts.
- Never douche — except if it is specifically prescribed by a doctor to treat an infection. Douching increases your risk of vaginal irritation and is not recommended during pregnancy. A healthy vagina does not need a vaginal deodorant.
- Avoid using soaps, bubble baths, bath salts, perfumes and perfumed talcs around the vaginal area. And never ever use anything harsh such as disinfectants — even diluted, near your vagina.
- A gentle moisturiser like aqueous cream may be advised. Use water or soap substitutes to wash the area.
- Always wipe from the front to the back after going to the toilet since this stops bowel organisms being swept into the vagina.
 Don’t use perfumed toilet paper because it can cause irritation.
Don’t use perfumed toilet paper because it can cause irritation.
Sources:
Mater Mother’s Hospital (Pregnancy – information for women and families), MotherSafe: NSW Medications in Pregnancy and Breastfeeding Service (Thrush in pregnancy), Women and Children’s Health Network (Common health problems in pregnancy – vaginal thrush)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
Need more information?
Thrush | SA Health
Thrush or Candidiasis is a common vaginal infection, caused by an overgrowth of yeasts and is not considered to be a sexually transmitted infection
Read more on SA Health website
Vaginal discharge during pregnancy
Almost all women have more vaginal discharge in pregnancy as it helps prevent any infections travelling up from the vagina to the womb.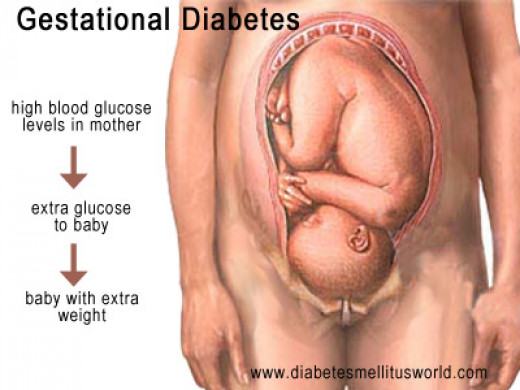
Read more on Pregnancy, Birth & Baby website
Contraception: vaginal ring - MyDr.com.au
The vaginal ring (brand name NuvaRing) is a type of hormonal contraception. When used properly, the vaginal ring is an effective and safe way of preventing pregnancy.
Read more on myDr website
Urinary tract infections (UTIs) during pregnancy
A urinary tract infection (UTI) is the most common bacterial infection women get in pregnancy, but there are ways to lower the risk of developing one.
Read more on Pregnancy, Birth & Baby website
Gestational diabetes: Q and A - MyDr.com.au
Gestational diabetes is a form of diabetes that develops during pregnancy.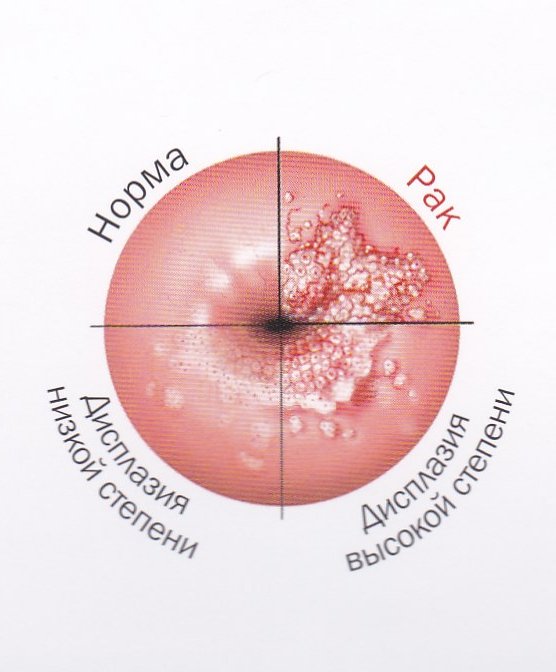 It is different from having known diabetes before pregnancy and then getting pregnant.
It is different from having known diabetes before pregnancy and then getting pregnant.
Read more on myDr website
Anatomy of pregnancy and birth - perineum and pelvic floor
The perineum – the skin between the vagina and anus - stretches during childbirth and can sometimes tear. Learn here how to prepare the perineum for the birth.
Read more on Pregnancy, Birth & Baby website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
STIs and pregnancy
Sexually transmitted infections (STIs), if left untreated, can cause serious problems for both mother and child.
Read more on Pregnancy, Birth & Baby website
Episiotomy
An episiotomy is a procedure performed during labour to assist with the delivery of your baby.
Read more on Pregnancy, Birth & Baby website
Menstrual cycle: normal - MyDr.com.au
All you need to know about periods, including what's normal and what's not. Plus, see what happens inside your body during the different phases of a normal menstrual cycle.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.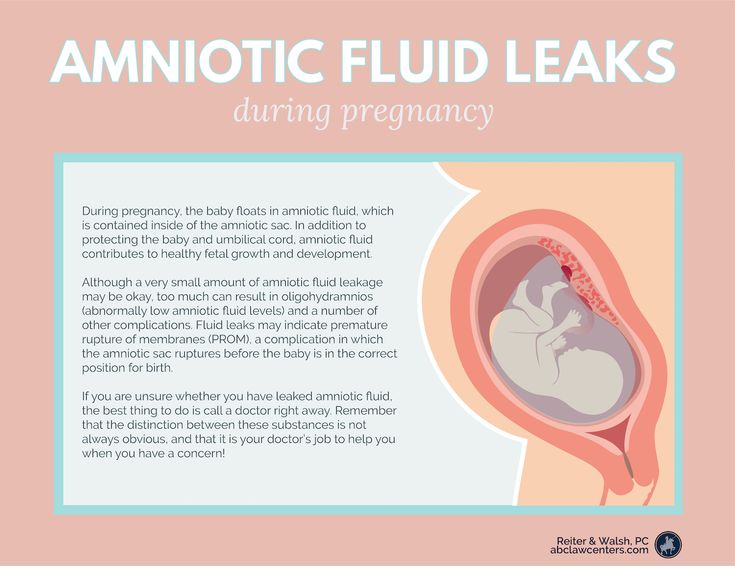
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
why does it occur and how to solve the problem?
Pregnancy is one of the important and responsible stages in a woman's life. In most cases, this is 9 months of anxious waiting to meet your baby. However, during pregnancy, a woman's body undergoes major hormonal changes and pleasant emotions can go hand in hand with painful and uncomfortable sensations in different areas of the body. Including unpleasant symptoms may appear in the intimate area.
Discomfort in the vagina often manifests itself in the form of itching, burning, irritation and swelling. The main thing, when these symptoms appear, is to understand that it is necessary to establish their cause and eliminate it as soon as possible, because there are risks of harming the health of the fetus.
Various sexual infections can affect the appearance of discomfort in the perineum. Unfortunately, during pregnancy, a woman is prone to various infectious diseases. As mentioned above, bearing a baby causes a restructuring of the hormonal background in a woman's body: the level of the hormone progesterone rises and the activity of the immune system naturally decreases, which creates favorable conditions for the exacerbation of chronic infections and the emergence of new ones.
How dangerous is the development of infectious diseases of the vagina and vulva during the bearing of a baby? Normally, during pregnancy, the amniotic bladder and water, as well as the mucous plug of the cervix, protect the fetus from various infections and bacteria, so your unborn baby is safe.
The presence in the body of a woman in an interesting position of an infectious disease and the lack of necessary therapy can adversely affect the course of pregnancy.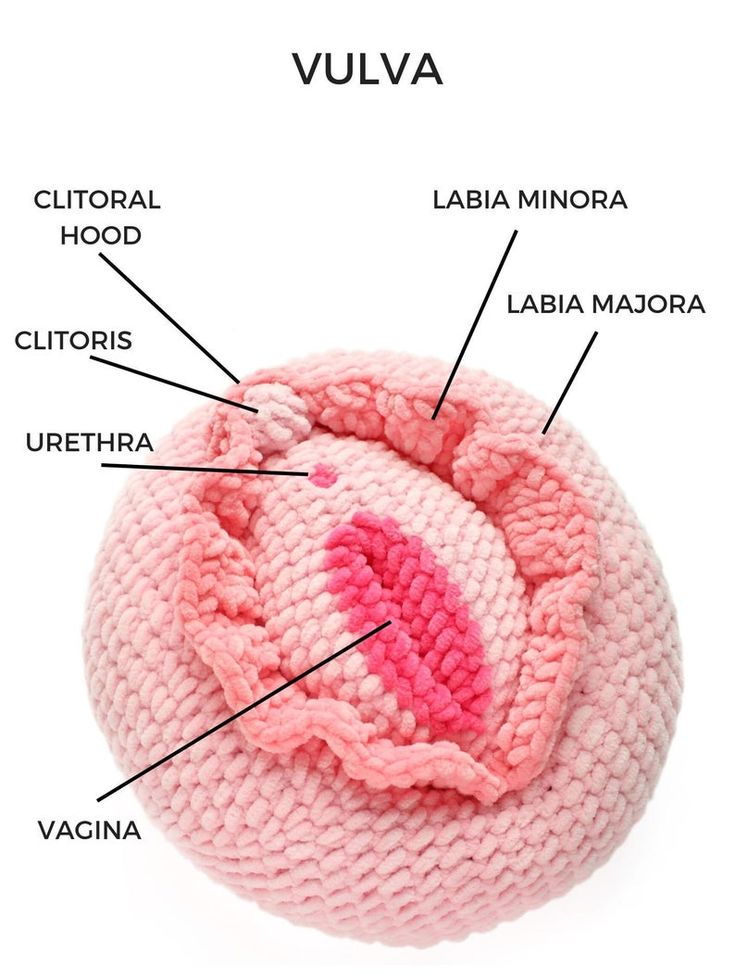 For example, an untreated infection can lead to damage to the membranes, the fluid in which the unborn child is located, and the fetus itself.
For example, an untreated infection can lead to damage to the membranes, the fluid in which the unborn child is located, and the fetus itself.
There is also a high probability of physical contact of the child with the infection during passage through the birth canal. Therefore, in case of any discomfort in the intimate area during pregnancy, you should consult a specialist.
You can suspect the appearance of an infection of the vagina and vulva by a series of symptoms: cramps, itching, burning. Often, sexual infections provoke colpitis - inflammation of the mucous membrane of the vagina and the vaginal part of the cervix. By itself, colpitis often causes discomfort in the groin of pregnant women. It can be provoked not only by sexual infections, but also by endocrine or chronic diseases, stress, lack of hygiene.
Bacterial vaginosis can also cause discomfort. This pathology, caused by a decrease in the number of lactobacilli in the vagina, as a result, their place is taken by other microorganisms that are always present in the vagina, but in excess lead to the development of dysbiosis. Bacterial vaginosis can occur without symptoms, but sometimes it occurs with clinical manifestations. It is usually accompanied by discomfort, as well as vaginal discharge that is white, gray, or yellow-green in color with an unpleasant "fishy" odor.
Bacterial vaginosis can occur without symptoms, but sometimes it occurs with clinical manifestations. It is usually accompanied by discomfort, as well as vaginal discharge that is white, gray, or yellow-green in color with an unpleasant "fishy" odor.
Bacterial vaginosis also adversely affects the course of pregnancy, can provoke inflammation of the pelvic organs, premature birth, chorioamnionitis - inflammation of the amniotic membranes and infection of the amniotic fluid.
Itching in the intimate area during pregnancy can appear with vulvovaginal candidiasis - infection of the mucous membranes of the vulva and vagina with yeast-like fungi of the genus Candida. It should be noted that the first episode of the incidence of vulvovaginal candidiasis is observed during pregnancy. This is due to changes in hormonal levels, reduced immunity. This disease, in addition to discomfort in the groin area, itching and burning, is characterized by: moderate hyperemia, white and thick discharge like cottage cheese, sour smell from the vagina, pain during sexual intercourse and urination.
However, itching and burning are not always symptoms of serious pathologies. Occasionally, discomfort can occur with the use of poorly fitting underwear or aggressive pH soaps.
Feeling discomfort in the groin, you should consult with a specialist. The specialist can conduct an examination, collect an anamnesis and prescribe, if necessary, laboratory and / or other diagnostic tests. All this will help to establish a diagnosis and choose an individual treatment regimen.
In order to prevent the appearance of discomfort in the intimate area and not spoil the pleasant waiting time for the addition, it is necessary to follow preventive recommendations.
- It is necessary to carry out external hygiene of the intimate area. Normally 2 times a day - no more and no less. Frequent washing can lead to “overdrying” of the skin and mucous membranes of the intimate area, and a lack of hygiene can lead to the development of various inflammations.
 You should not self-douche or vaginal lavage unless recommended by a specialist in your particular case.
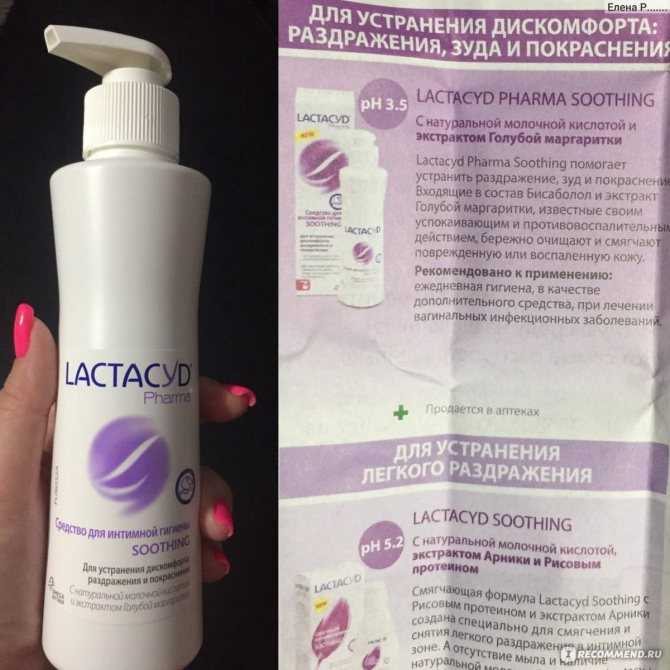
You should not self-douche or vaginal lavage unless recommended by a specialist in your particular case. - Choose a quality cleanser. Ideally, this should be a hypoallergenic product that is dermatologically tested, contains lactic acid and components that care for the skin of the genital organs. Epigen Intim Gel is ideal for daily hygiene of the inguinal zone during pregnancy and after childbirth. Epigen Intim gel contains activated glycyrrhizic and lactic acids in its composition. Its pH is slightly acidic, which corresponds to the normal acid-base balance of the skin of the intimate area. The tool helps to eliminate discomfort (irritation) due to wearing panty liners or not very comfortable underwear. It has a very pleasant aroma and helps to neutralize unpleasant odors in the intimate area with constant use.
- Abandon synthetic underwear in favor of natural fabrics. Cotton panties do not create a "greenhouse effect", especially in the heat.
Treatment of discomfort in the intimate area will be different.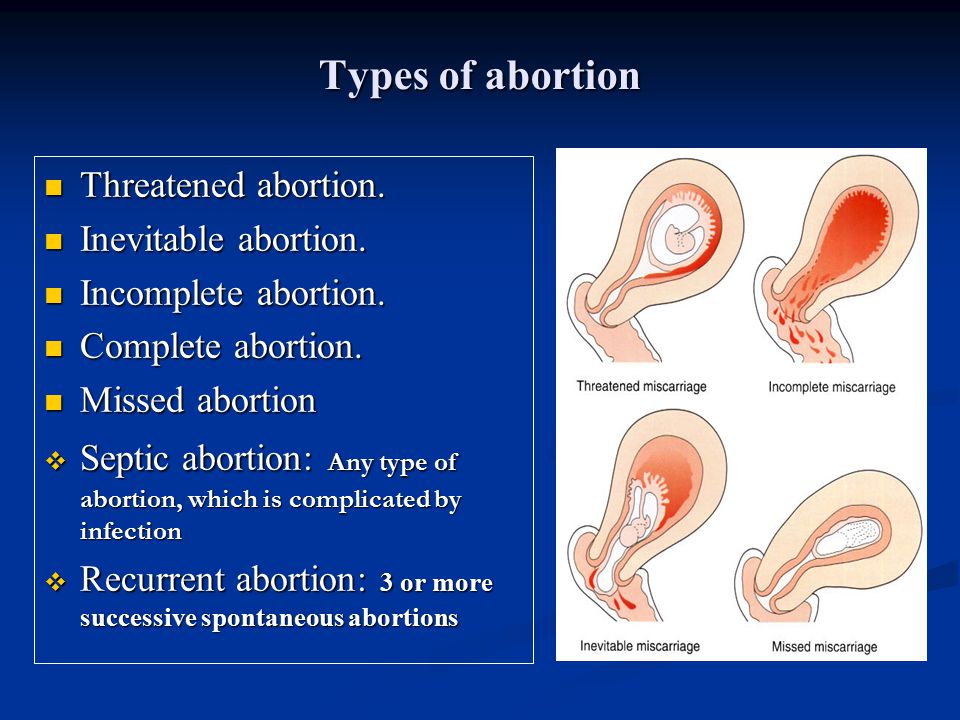 The diagnosed disease will influence the choice of therapy. Spray Epigen Intim can be included in the complex treatment of diseases accompanied by discomfort - nonspecific colpitis (vaginitis), bacterial vaginosis, thrush, herpes.
The diagnosed disease will influence the choice of therapy. Spray Epigen Intim can be included in the complex treatment of diseases accompanied by discomfort - nonspecific colpitis (vaginitis), bacterial vaginosis, thrush, herpes.
Spray Epigen Intim
More
Buy
Epigen Intim Spray
The drug has antipruritic and anti-inflammatory action. Thanks to the active ingredient - activated glycyrrhizic acid, Epigen Intim spray helps to eliminate itching and irritation. It also helps to eliminate inflammation, swelling and redness of tissues. The drug is also able to increase the local immunity of the vagina, by stimulating the production of its own interferons. Spray Epigen Intim promotes healing and restoration of the integrity of the damaged mucosa, due to which the protective function of the mucosa will be restored and the number of lactobacilli will increase.
The drug is successfully used to treat viral infections (caused by the human papillomavirus, genital herpes), diseases associated with a decrease in local immunity (nonspecific vaginitis, thrush, bacterial vaginosis), etc. It can be used to treat exacerbations in conjunction with antiviral, antifungal and antimicrobial drugs, and for the prevention of these vaginal infections.
It can be used to treat exacerbations in conjunction with antiviral, antifungal and antimicrobial drugs, and for the prevention of these vaginal infections.
more
By the way, while carrying a baby, the use of many drugs sold in pharmacies is limited or prohibited.
But Epigen Intim spray is approved for use in pregnant and lactating women and is dispensed without a doctor's prescription. The drug is applied both externally and intravaginally, depending on the disease.
In the presence of itching, burning, irritation and swelling in the groin area, a woman feels as uncomfortable as possible. Intimate discomfort can bring especially many experiences to women during pregnancy. To minimize the risks of discomfort, try to follow the simple rules indicated in the article. When discomfort appears in the perineum, the most correct thing is to visit a specialist and not self-medicate, since now you are responsible not only for yourself, but also for the unborn baby.
COLPITIS DURING PREGNANCY
During pregnancy, a woman, as a rule, takes special care of her health and reacts anxiously to every unusual symptom.
Unusual discharge and discomfort in the genital area are often the cause of the expectant mother's panic. Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
Vaginitis during pregnancy is a good reason to immediately contact a gynecologist and start treating this dangerous pathology. Diagnose the disease and determine how to treat colpitis during pregnancy without harming the mother and baby, qualified gynecologists will prompt.
Symptoms of colpitis during pregnancy
First of all, it should be determined that vaginitis or colpitis is an inflammatory disease that involves the mucous membranes of the vagina.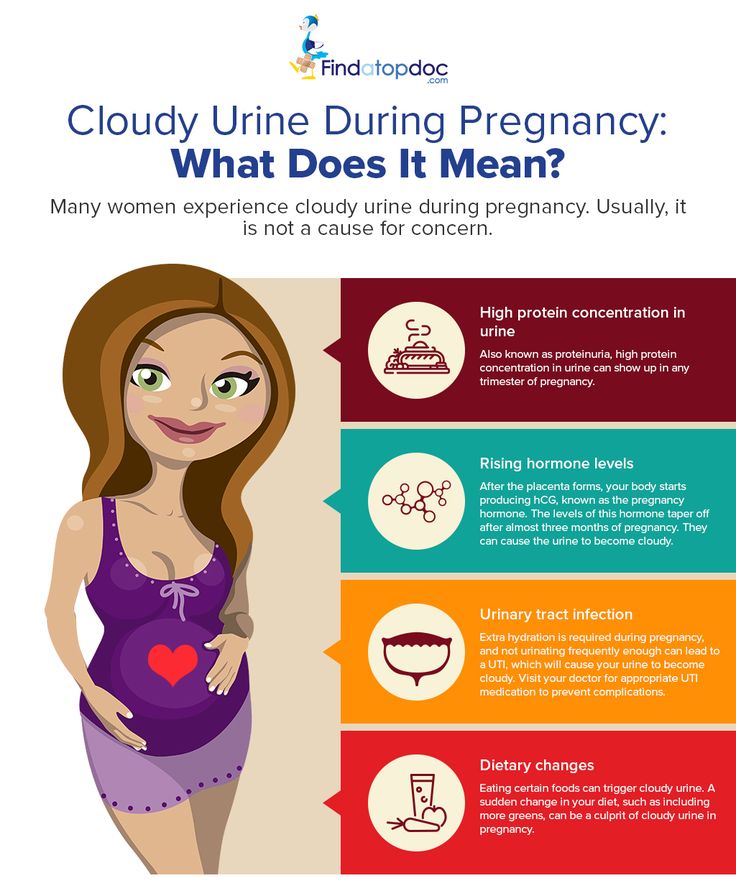 The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia. In this case, inflammation can be seen with the naked eye.
The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia. In this case, inflammation can be seen with the naked eye.
The characteristic signs of colpitis during pregnancy do not differ from the symptoms of a non-pregnant woman:
- itching and burning in the vaginal area - the inflammatory process irritates the delicate mucous membranes, which causes discomfort and sometimes pain in the vaginal walls;
- pain in the lower abdomen - this symptom is especially frightening for pregnant women, but it is not associated with uterine tone, as many assume, but with tissue inflammation;
- the appearance of specific discharge - the discharge during colpitis during pregnancy is very abundant and may have a different color and consistency. Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
- swelling and redness of the genital organs - patients often notice hyperemia and swelling of the labia and clitoris, which become more sensitive and cause discomfort to the woman.
Acute vaginitis during pregnancy is accompanied by severe symptoms, which should make the patient seek professional help. This will help protect the child from possible negative consequences.
Causes and types of vaginitis during pregnancy
Inflammation of the mucous membranes of the vagina is usually of an infectious nature. This becomes possible due to vaginal dysbacteriosis, which often accompanies the period of pregnancy. Hormonal changes and high loads on all organs of the expectant mother cause a decrease in the body's defenses, which provokes an infectious and inflammatory process. In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
It is interesting that depending on the cause of the development of the disease, its symptoms and manifestations may differ:
- candidal colpitis - accompanied by abundant cheesy discharge and severe itching of the genital organs, which manifests itself even at rest;
- emphysematous colpitis - a very common type of vaginitis in pregnant women. Pathology is accompanied by the formation of small watery vesicles on the surface of the mucous membranes of the genital organs. This form of colpitis resolves on its own in 2-3 weeks after childbirth;
- Trichomonas colpitis - a very dangerous form of pathology that develops when Trichomonas enters the vaginal environment.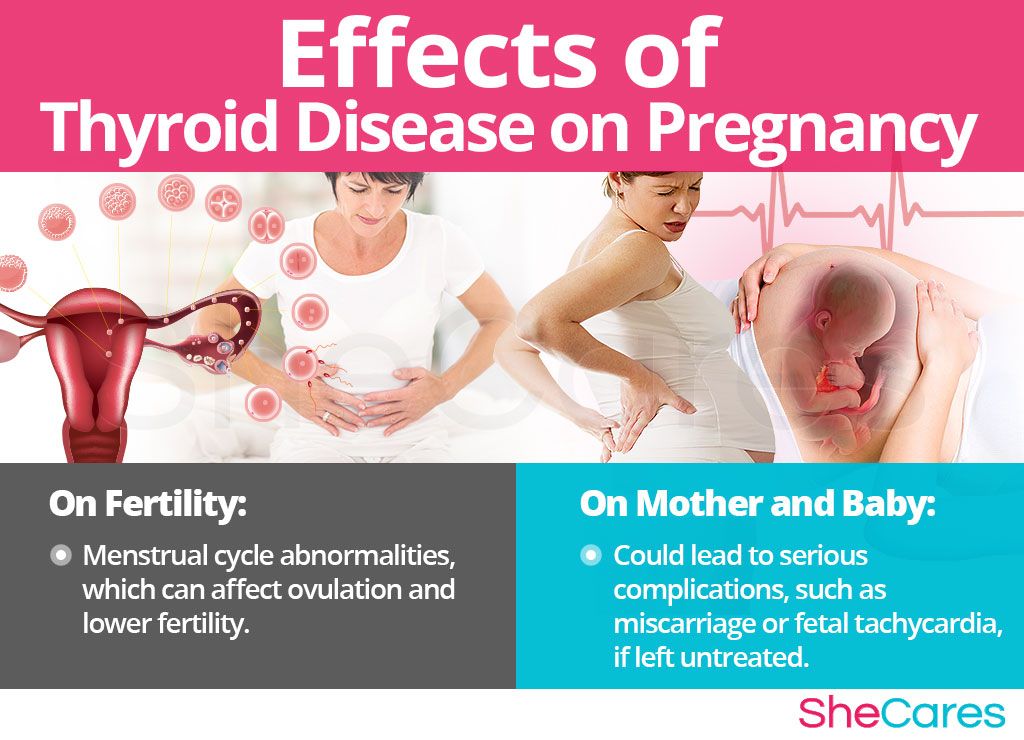 Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Concomitant conditions for the development of colpitis in a pregnant woman, in addition to a decrease in immunity, may be allergic reactions, microtrauma of the vagina, non-observance of personal hygiene, the presence of chronic diseases.
Colpitis during pregnancy: consequences for the child
Inflammation of the mucous membranes of the vagina poses a threat not only to the health of the expectant mother, but also to the baby. The ascending route of infection can lead to pregnancy abnormalities such as polyhydramnios, premature birth, and infection of the amniotic fluid. Vaginitis is especially dangerous during childbirth, when the baby passes through an infected maternal birth canal. At at this moment there is a high probability of infection newborn.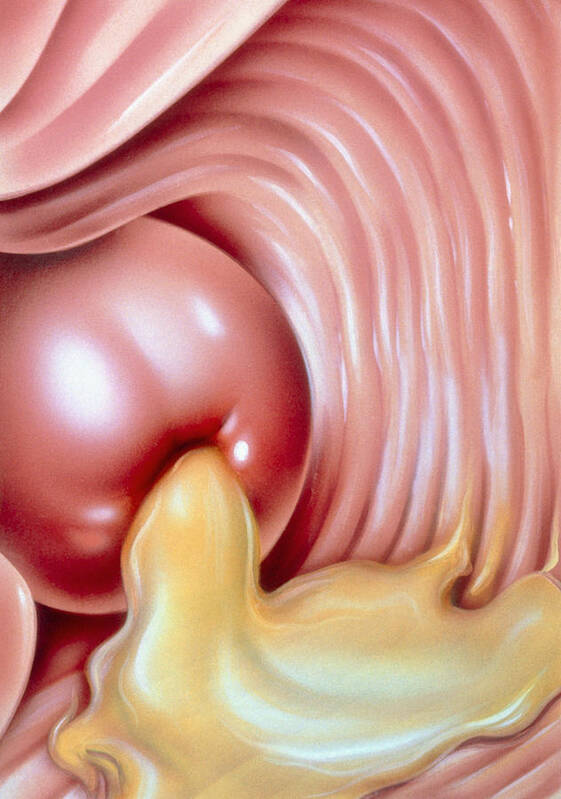
Interestingly, colpitis after pregnancy can go away on its own, but this happens relatively rarely. The development of colpitis after childbirth is most often provoked by trauma to the vaginal membranes during delivery. In connection with this fact, doctors recommend abstaining from sexual activity for the first weeks after childbirth. Violating this prohibition, a woman increases the risk of developing colpitis after childbirth.
Treatment of colpitis during pregnancy
Diagnosis of the disease involves a standard gynecological examination and colposcopy. This research method makes it possible to visualize the surface of the mucous membrane of the walls of the vagina and assess their condition. During the examination, the doctor takes a smear for analysis. The study of biological material is carried out by bacterioscopic and bacteriological methods.
Treatment of colpitis in pregnant women requires a rational approach to prescribing antibiotics.