Pregnancy and blood work
Routine Tests During Pregnancy | ACOG
Acquired Immunodeficiency Syndrome (AIDS): A group of signs and symptoms, usually of severe infections, in a person who has human immunodeficiency virus (HIV).
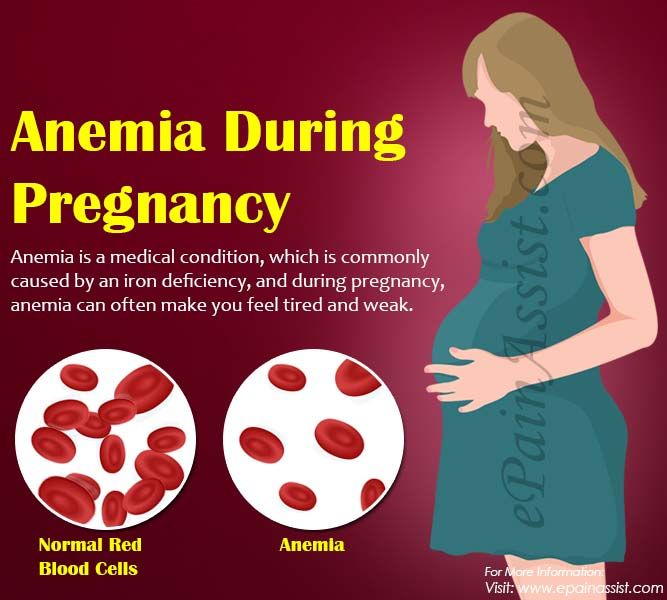
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Antibiotics: Drugs that treat certain types of infections.
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Bacteria: One-celled organisms that can cause infections in the human body.
Birth Defects: Physical problems that are present at birth.
Cells: The smallest units of structures in the body.
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Chlamydia: A sexually transmitted infection caused by bacteria. This infection can lead to pelvic inflammatory disease and infertility.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.
Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gene: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
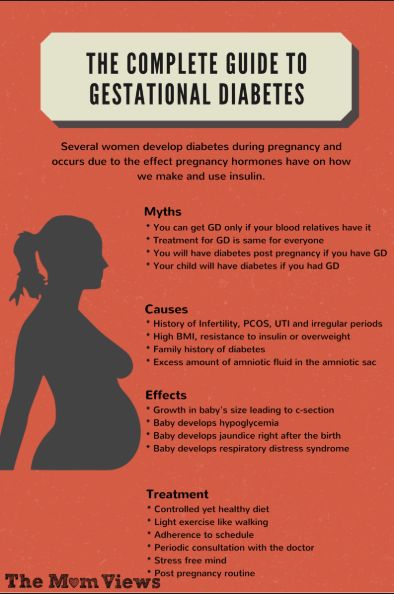
Gestational Diabetes: Diabetes that arises during pregnancy.
Glucose: A sugar in the blood that is the body’s main source of fuel.
Gonorrhea: A sexually transmitted infection that can lead to pelvic inflammatory disease, infertility, and arthritis.
Group B Streptococcus (GBS): A type of bacteria that many people carry normally and can be passed to the fetus at the time of delivery. GBS can cause serious infection in some newborns. Antibiotics are given during labor to women who carry the bacteria to prevent newborn infection.
Hepatitis B: An infection caused by a virus that can be spread through blood, semen, or other body fluid infected with the virus.
Hepatitis C: An infection caused by a virus that can be spread through infected blood.
Human Immunodeficiency Virus (HIV): A virus that attacks certain cells of the body’s immune system. If left untreated, HIV can cause acquired immunodeficiency syndrome (AIDS).
Immune: Protected against infectious disease.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.
Measles–Mumps–Rubella (MMR) Vaccine: A shot given to protect against measles, mumps, and rubella. The shot contains live viruses that have been changed to not cause disease. The shot is not recommended for pregnant women.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
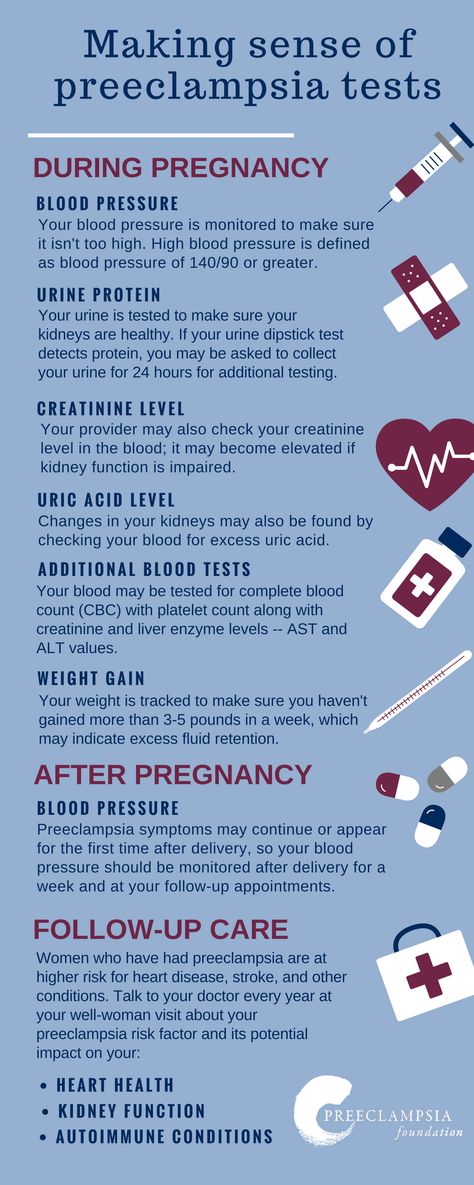
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Rectum: The last part of the digestive tract.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rubella: A virus that can be passed to the fetus if a woman becomes infected during pregnancy. The virus can cause miscarriage or severe birth defects.
Sexually Transmitted Infections (STIs): Infections that are spread by sexual contact. Infections include chlamydia, gonorrhea, human papillomavirus (HPV), herpes, syphilis, and human immunodeficiency virus (HIV, the cause of acquired immunodeficiency syndrome [AIDS]).
Syphilis: A sexually transmitted infection (STI) that is caused by an organism called Treponema pallidum. This infection may cause major health problems or death in its later stages.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Tuberculosis (TB): A disease that affects the lungs and other organs in the body. TB is caused by bacteria.
TB is caused by bacteria.
Urinary Tract Infection (UTI): An infection in any part of the urinary system, including the kidneys, bladder, or urethra.
Vaccine: A substance that helps the body fight disease. Vaccines are made from very small amounts of weak or dead agents that cause disease (bacteria, toxins, and viruses).
Vagina: A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
Common Tests During Pregnancy | Johns Hopkins Medicine
-
Genetic Screening
-
First Trimester
-
Second Trimester
-
Ultrasound
-
Amniocentesis
-
Chorionic Villus Sampling
-
Fetal Monitoring
-
Glucose
-
Group B Strep Culture
Your health care provider may recommend a variety of screenings, tests and imaging techniques during your pregnancy. These tests are designed to provide information about the health of your baby and may help you optimize your child’s prenatal care and development.
These tests are designed to provide information about the health of your baby and may help you optimize your child’s prenatal care and development.
Genetic Screening
Many genetic abnormalities can be diagnosed before birth. Your doctor or midwife may recommend genetic testing during pregnancy if you or your partner has a family history of genetic disorders. You may also choose to have genetic screening if you have had a fetus or baby with a genetic abnormality.
Examples of genetic disorders that can be diagnosed before birth include:
-
Cystic fibrosis
-
Duchenne muscular dystrophy
-
Hemophilia A
-
Polycystic kidney disease
-
Sickle cell disease
-
Tay-Sachs disease
-
Thalassemia
The following screening methods are available during pregnancy:
-
Alpha-fetoprotein (AFP) test or multiple marker test
-
Amniocentesis
-
Chorionic villus sampling
-
Cell-free fetal DNA testing
-
Percutaneous umbilical blood sampling (withdrawing a small sample of the fetal blood from the umbilical cord)
-
Ultrasound scan
First Trimester Prenatal Screening Tests
First trimester screening is a combination of fetal ultrasound and maternal blood testing. This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
First trimester screening includes:
-
Ultrasound for fetal nuchal translucency. Nuchal translucency screening uses an ultrasound to examine the area at the back of the fetal neck for increased fluid or thickening.
-
Ultrasound for fetal nasal bone determination. The nasal bone may not be visualized in some babies with certain chromosome abnormalities, such as Down syndrome. This screen is performed using an ultrasound between 11 and 13 weeks gestation.
-
Maternal serum (blood) tests. These blood tests measure two substances found in the blood of all pregnant women:
-
Pregnancy-associated plasma protein A. A protein produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.

-
Human chorionic gonadotropin. A hormone produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
When used together as first trimester screening tests, nuchal translucency screening and maternal blood tests have a greater ability to determine if the fetus might have a birth defect, such as Down syndrome (trisomy 21) and trisomy 18.
If the results of these first trimester screening tests are abnormal, genetic counseling is recommended. Additional testing, such as chorionic villus sampling, amniocentesis, cell-free fetal DNA or other ultrasounds, may be needed for an accurate diagnosis.
Second Trimester Prenatal Screening Tests
Second trimester prenatal screening may include several blood tests called multiple markers. These markers provide information about your potential risk of having a baby with certain genetic conditions or birth defects. Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
-
AFP screening. Also called maternal serum AFP, this blood test measures the level of AFP in your blood during pregnancy. AFP is a protein normally produced by the fetal liver that is present in the fluid surrounding the fetus (amniotic fluid). It crosses the placenta and enters your blood. Abnormal levels of AFP may indicate:
-
A miscalculated due date, as the levels vary throughout pregnancy
-
Defects in the abdominal wall of the fetus
-
Down syndrome or other chromosomal abnormalities
-
Open neural tube defects, such as spina bifida
-
Twins (more than one fetus is producing the protein)
-
-
Estriol.
 This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health.
This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health. -
Inhibin. This is a hormone produced by the placenta.
-
Human chorionic gonadotropin. This is also a hormone produced by the placenta.
Abnormal test results of AFP and other markers may mean that additional testing is needed. An ultrasound is used to confirm the milestones of your pregnancy and to check the fetal spine and other body parts for defects. An amniocentesis may be needed for an accurate diagnosis.
Since multiple marker screening is not diagnostic, it is not 100 percent accurate. It helps determine who in the population should be offered additional testing during pregnancy. False-positive results may indicate a problem when the fetus is actually healthy. On the other hand, false-negative results indicate a normal result when the fetus actually does have a health problem.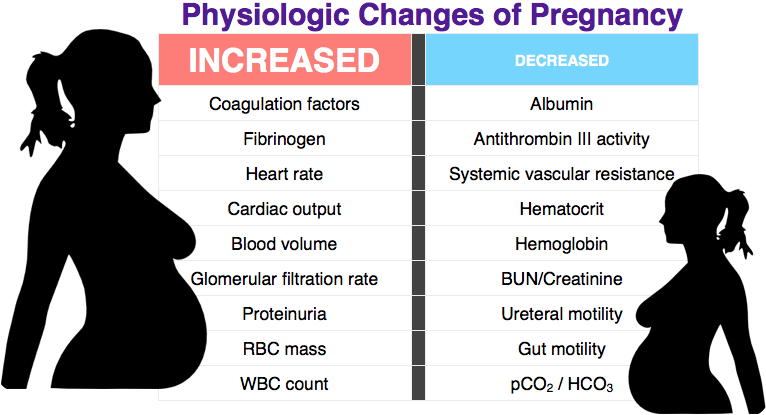
When you have both first and second trimester screening tests performed, the ability of the tests to detect an abnormality is greater than using just one screening independently. Most cases of Down syndrome can be detected when both first and second trimester screenings are used.
Ultrasound
An ultrasound scan is a diagnostic technique that uses high-frequency sound waves to create an image of the internal organs. A screening ultrasound is sometimes done during the course of your pregnancy to check normal fetal growth and verify the due date.
When are ultrasounds performed during pregnancy?
Ultrasounds may be done at various times throughout pregnancy for several reasons:
First Trimester
-
To establish the due date (this is the most accurate way of determining the due date)
-
To determine the number of fetuses and identify placental structures
-
To diagnose an ectopic pregnancy or miscarriage
-
To examine the uterus and other pelvic anatomy
-
To detect fetal abnormalities (in some cases)
Midtrimester (also called the 18- to 20-week scan)
-
To confirm the due date (a due date set in the first trimester is rarely changed)
-
To determine the number of fetuses and examine the placental structures
-
To assist in prenatal tests, such as an amniocentesis
-
To examine the fetal anatomy for abnormalities
-
To check the amount of amniotic fluid
-
To examine blood flow patterns
-
To observe fetal behavior and activity
-
To measure the length of the cervix
-
To monitor fetal growth
Third Trimester
-
To monitor fetal growth
-
To check the amount of amniotic fluid
-
To conduct the biophysical profile test
-
To determine the position of the fetus
-
To assess the placenta
How is an ultrasound scan performed?
Two types of ultrasounds can be performed during pregnancy:
-
Abdominal ultrasound.
 In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image.
In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image. -
Transvaginal ultrasound. In a transvaginal ultrasound, a smaller ultrasound transducer is inserted into your vagina and rests against the back of the vagina to create an image. A transvaginal ultrasound produces a sharper image than an abdominal ultrasound and is often used in early pregnancy.
Which ultrasound imaging techniques are available?
There are several types of ultrasound imaging techniques. As the most common type, the 2-D ultrasound provides a flat picture of one aspect of the baby.
If more information is needed, a 3-D ultrasound exam can be done. This technique, which provides a 3-D picture, requires a special machine and special training. The 3-D image allows the health care provider to see the width, height and depth of the images, which can be helpful during the diagnosis.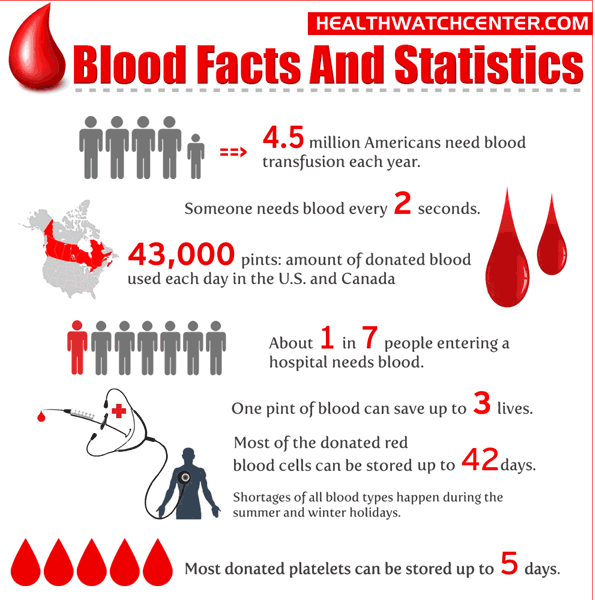 The 3-D images can also be captured and saved for later review.
The 3-D images can also be captured and saved for later review.
The latest technology is 4-D ultrasound, which allows the health care provider to visualize the unborn baby moving in real time. With 4-D imaging, a three-dimensional image is continuously updated, providing a “live action” view. These images often have a golden color, which helps show shadows and highlights.
Ultrasound images may be captured in still photographs or on video to document findings.
What are the risks and benefits of ultrasound imaging?
Fetal ultrasound has no known risks other than mild discomfort due to pressure from the transducer on your abdomen or in your vagina. No radiation is used during the procedure.
Transvaginal ultrasound requires covering the ultrasound transducer in a plastic or latex sheath, which may cause a reaction in women with a latex allergy.
Ultrasound imaging is constantly being improved and refined. As with any test, the results may not be completely accurate.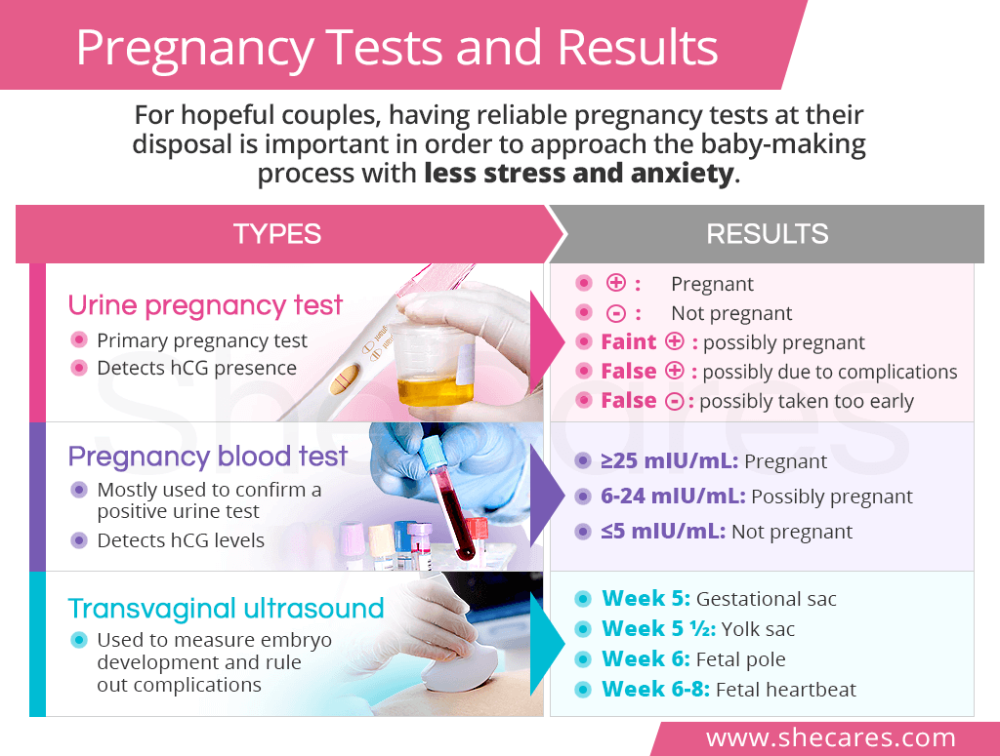 However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
Fetal ultrasound is sometimes offered in nonmedical settings to provide keepsake images or videos for parents. While the ultrasound procedure itself is considered safe, it is possible that untrained personnel may miss an abnormality or give parents false assurances about their baby’s well-being. It is best to have an ultrasound performed by trained medical personnel who can correctly interpret the results. Talk with your doctor or midwife if you have questions.
Amniocentesis
An amniocentesis involves taking a small sample of the amniotic fluid that surrounds the fetus. It is used to diagnose chromosomal disorders and open neural tube defects, such as spina bifida.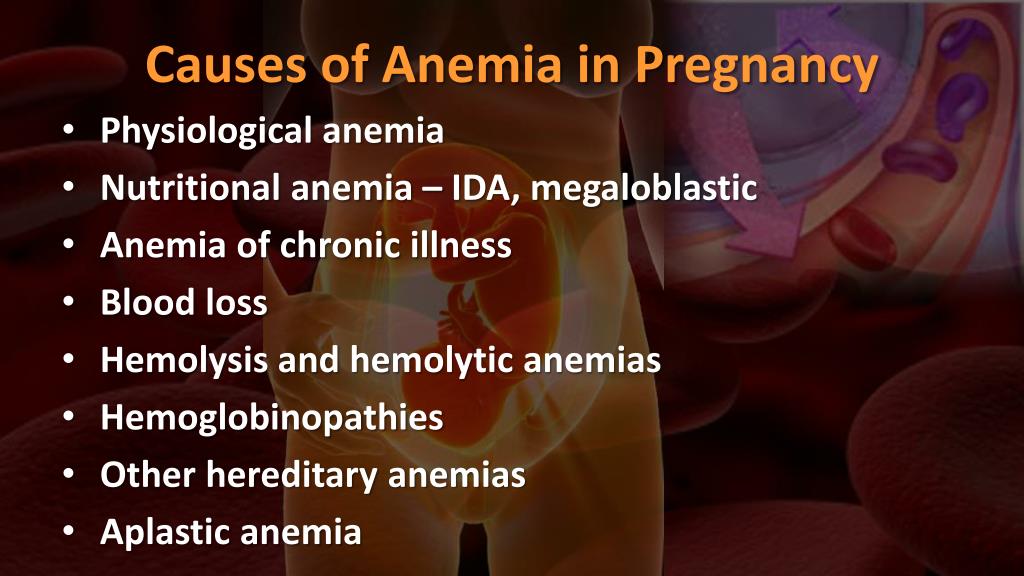 Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Who is an ideal candidate for amniocentesis?
An amniocentesis is generally offered to women between the 15th and 20th week of pregnancy who have an increased risk of chromosomal abnormalities. Candidates include women who will be over age 35 at the time of delivery or those who have had an abnormal maternal serum screening test.
How is an amniocentesis performed?
An amniocentesis involves inserting a long, thin needle through your abdomen into the amniotic sac to withdraw a small sample of amniotic fluid. The amniotic fluid contains cells shed by the fetus, which contain genetic information. Although specific details of each procedure may vary, a typical amniocentesis follows this process:
-
Your abdomen will be cleansed with an antiseptic.
-
Your doctor may or may not give a local anesthetic to numb the skin.

-
Your doctor will use ultrasound technology to help guide a hollow needle into the amniotic sac. He or she will withdraw a small sample of fluid for lab analysis.
You may feel some cramping during or after the amniocentesis. Strenuous activities should be avoided for 24 hours following the procedure.
Women who are pregnant with twins or other higher-order multiples need sampling from each amniotic sac to study each baby. Depending on the position of the baby and placenta, amount of fluid, and woman’s anatomy, sometimes the amniocentesis cannot be done. The fluid is then sent to a genetics lab so that the cells can grow and be analyzed. AFP is also measured to rule out an open neural tube defect. Results are usually available in about 10 days to two weeks, depending on the lab.
Chorionic Villus Sampling (CVS)?
CVS is a prenatal test that involves taking a sample of some of the placental tissue. This tissue contains the same genetic material as the fetus and can be tested for chromosomal abnormalities and some other genetic problems. Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
How is CVS performed?
CVS may be offered to women with an increased risk of chromosomal abnormalities or who have a family history of a genetic defect that is testable from the placental tissue. CVS is usually performed between the 10th and 13th week of pregnancy. Although exact methods may vary, the procedure involves the following steps:
-
Your doctor will insert a small tube (catheter) through your vagina and into your cervix.
-
Using ultrasound technology, your doctor will guide the catheter into place near the placenta.
-
Your doctor will remove some tissue using a syringe on the other end of the catheter.
Your doctor may also choose to perform a transabdominal CVS, which involves inserting a needle through your abdomen and into your uterus to sample the placental cells. You may feel some cramping during and after either type of CVS procedure. The tissue samples are sent to a genetic lab for growth and analysis. Results are usually available in about 10 days to two weeks, depending on the lab.
What if CVS is not possible?
Women with twins or other higher-order multiples usually need sampling from each placenta. However, because of the complexity of the procedure and the positioning of the placentas, CVS is not always feasible or successful with multiples.
Women who are not candidates for CVS or who did not get accurate results from the procedure may require a follow-up amniocentesis. An active vaginal infection, such as herpes or gonorrhea, will prohibit the procedure. In other cases, the doctor may take a sample that does not have enough tissue to grow in the lab, generating incomplete or inconclusive results.
Fetal Monitoring
During late pregnancy and labor, your doctor may want to monitor the fetal heart rate and other functions. Fetal heart rate monitoring is a method of checking the rate and rhythm of the fetal heartbeat. The average fetal heart rate is between 120 and 160 beats per minute. This rate may change as the fetus responds to conditions in the uterus. An abnormal fetal heart rate or pattern may mean that the fetus is not getting enough oxygen or indicate other problems. An abnormal pattern also may mean that an emergency cesarean delivery is needed.
How is fetal monitoring performed?
Using a fetoscope (a type of stethoscope) to listen to the fetal heartbeat is the most basic type of fetal heart rate monitoring. Another type of monitoring is performed with a hand-held Doppler device. This is often used during prenatal visits to count the fetal heart rate. During labor, continuous electronic fetal monitoring is often used. Although the specific details of each procedure may vary, standard electronic fetal monitoring follows this process:
-
Gel is applied to your abdomen to act as a medium for the ultrasound transducer.

-
The ultrasound transducer is attached to your abdomen with straps so it can transmit the fetal heartbeat to a recorder. The fetal heart rate is displayed on a screen and printed onto special paper.
-
During contractions, an external tocodynamometer (a monitoring device that is placed over the top of the uterus with a belt) can record the pattern of contractions.
When is internal fetal monitoring needed?
On occasion, internal fetal monitoring is needed to provide a more accurate reading of the fetal heart rate. Your bag of waters (amniotic fluid) must be broken and your cervix must be partially dilated to use internal monitoring. Internal fetal monitoring involves inserting an electrode through the dilated cervix and attaching the electrode to the scalp of the fetus.
Glucose Testing
Glucose testing is used to measure the level of sugar in your blood.
A glucose challenge test is usually conducted between 24 and 28 weeks of pregnancy. Abnormal glucose levels may indicate gestational diabetes.
Abnormal glucose levels may indicate gestational diabetes.
What is involved in a glucose challenge test?
The initial one-hour test is a glucose challenge test. If the results are abnormal, a glucose tolerance test is needed.
How is a glucose tolerance test performed?
You may be asked to only drink water on the day the glucose tolerance test is given. Although the specific details of each procedure may vary, a typical glucose tolerance test includes the following steps:
-
An initial fasting sample of blood will be drawn from your vein.
-
You will be given a special glucose solution to drink.
-
Blood will be drawn at various times over the course of several hours to measure the glucose levels in your body.
Group B Strep Culture
Group B streptococcus (GBS) is a type of bacteria found in the lower genital tract of about 20 percent of all women. While a GBS infection does not usually cause problems in women before pregnancy, it can cause serious illness in mothers during pregnancy. GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies contract the infection during pregnancy or from the mother’s genital tract during labor and delivery.
The Centers for Disease Control and Prevention recommends screening all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks gestation. The treatment of mothers with certain risk factors or positive cultures is important to reduce the risk of transmission of GBS to the baby. Babies whose mothers receive antibiotic treatment for a positive GBS test are 20 times less likely to develop the disease than those without treatment.
Blood test for pregnancy in the early stages - why you need and how to donate blood
Blood test for pregnancy is a procedure that is necessary to identify existing pathologies. It also allows you to determine the very presence of pregnancy, since it detects the presence in the blood of a woman of a hormone called "chorionic gonadotropin" (hCG).
It also allows you to determine the very presence of pregnancy, since it detects the presence in the blood of a woman of a hormone called "chorionic gonadotropin" (hCG).
In a situation where conception has not occurred, this substance is not produced in the patient's body, since its appearance is associated with the formation of the chorion. This is the tissue that occurs between the endometrium and the zygote after the attachment of a fertilized egg to the wall of the uterus.
Reasons for testing
A blood test can show pregnancy as early as six days after a successful conception. Whereas a standard pregnancy test in some cases can give incorrect results. Therefore, tests during pregnancy are prescribed to determine such conditions as:
- Establishment of the actual fact of conception
- Assessment of hormonal background for failures
- Tracking abnormal pregnancy types:
- Frozen - in this case, at a certain stage, the embryo stops its development
- Ectopic - in this situation, the zygote is not attached to the wall of the uterus, but in the fallopian tube
Also, a blood test shows the presence of infections, other types of body dysfunctions and diseases such as:
- Cytomegalovirus
- Diphtheria
- Tetanus
- Herpes
- Chlamydia
- Hepatitis
- Ureaplasmosis
- HIV
- Mycoplasmosis
- Syphilis
- Leptospirosis
- Chlamydia
Any of these diseases is a danger not only to the body of the woman herself, but also to her unborn child. Therefore, if there are deviations in the results of the blood test, the doctor sends the patient for an additional examination.
Therefore, if there are deviations in the results of the blood test, the doctor sends the patient for an additional examination.
Changes in hCG during pregnancy
After the physical onset of conception, the level of hCG in the female body begins to rise, and every two to three days its concentration almost doubles. It reaches its highest level at 8-11 weeks, and then it begins to gradually decrease.
The first analysis can be taken on the 6th day of the expected delay, but the result will be more accurate on the 11-12th day. Therefore, doctors recommend undergoing a blood test two to three times (every two days later).
Monitoring the level of hCG allows you to monitor the dynamics of pregnancy, the appearance of pathologies, etc.:
- In ectopic pregnancy, the level of the hormone practically does not increase
- If the development of the embryo has stopped, then the level of hCG drops from the moment of its death
Usually the result of the analysis is compared with a special table. In the first or second weeks, the concentration of hCG can range from 25 to 700 units, at the peak of the value it can reach 18,000–240,000 units, and at the end of the gestational age - 2,179-60,000 units.
In the first or second weeks, the concentration of hCG can range from 25 to 700 units, at the peak of the value it can reach 18,000–240,000 units, and at the end of the gestational age - 2,179-60,000 units.
After establishing the fact of conception, the doctor refers the patient to other blood tests:
- General
- Biochemical
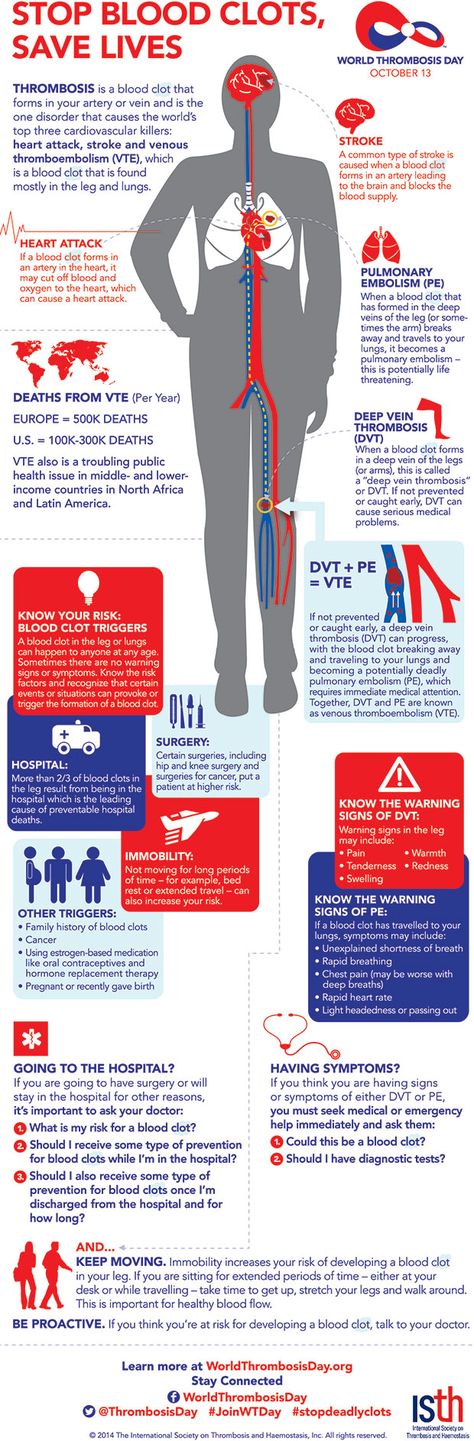
- For clotting
- For hepatitis and HIV
- For TORCH infections
- For genetic pathologies
- For Rh factor and blood group (if not previously determined)
- For the content of hormones produced by the thyroid gland
- Antiphospholipid syndrome
- For STDs
Causes of deviation from the norm of the hormone hCG
Normally, after the onset of pregnancy, the level of human chorionic gonadotropin should gradually increase. If it decreases, then the doctor may assume the presence of such problems as:
- In the early stages:
- Fetal death
- Probability of spontaneous termination of pregnancy
- Missing embryo in ovum
- Late term:
- Placental abruption
In some cases, a low level of hCG may be associated with an incorrectly calculated gestational age. Therefore, in order to determine the exact cause of low hormone levels, early pregnancy tests are usually performed, as well as several types of other examinations.
Therefore, in order to determine the exact cause of low hormone levels, early pregnancy tests are usually performed, as well as several types of other examinations.
Causes of an increase in hCG levels
In the results of blood tests, the level of hCG can be seriously higher than normal for the following reasons:
- Presence of toxicosis
- More than one fetus
- Occurrence of hydatidiform mole
- Presence of genetic problems
- Complication due to diabetes mellitus
The level of human chorionic gonadotropin can be increased not only due to pregnancy, but also due to some abnormalities:
- Extremely high hCG levels due to hormonal drugs
- The presence of a malignant neoplasm in various organs (kidneys, gastrointestinal tract, uterus, lungs, etc.)
- Preservation of an unstable hormonal background as a result of an abortion
In rare cases, in the presence of serious hormonal disorders, men can also be found to have elevated levels of hCG.
Preparation for procedure
The following preparations are required before taking hCG tests for pregnant women:
- Fasting for 7-8 hours before the procedure
- Limiting the intake of any liquid a few hours before the examination
Also tell your doctor if you are taking any medications.
Statistics show that the highest concentration of hCG in the blood is observed in the first half of the day, so the doctor usually prescribes such an analysis in the morning.
If the recommendations are not followed, the study may show an unreliable result, so additional procedures will have to be carried out.
How blood sampling is performed
Blood tests for pregnant women are taken from a vein in the area located on the inside of the arm at the elbow. The procedure is as follows:
- The patient sits on a couch or chair and exposes her left or right arm
- Medic applying a tourniquet above the elbow
- After that, the woman performs several clenching of the palm into a fist
- The doctor lubricates the area of the future puncture with a disinfectant
- He then inserts the needle into the vein and fills the syringe (about 10 ml of blood is needed for the test)
- After that, the tourniquet is removed, and a cotton swab is applied to the puncture area, which the patient must hold with her arm bent at the elbow (this helps to stop the release of fluid from the wound)
After these manipulations, the blood in the test tube is sent to the laboratory for analysis. The results of the analysis can be transferred directly to the attending physician, or issued to the patient. A woman can independently compare these indicators with the values in the tables, but it is recommended to entrust this process to professionals.
The results of the analysis can be transferred directly to the attending physician, or issued to the patient. A woman can independently compare these indicators with the values in the tables, but it is recommended to entrust this process to professionals.
Advantages of the procedure at MEDSI
- Highly qualified doctors work in the clinics, who not only develop comprehensive examination and treatment programs, but also help to properly prepare for childbirth in case of pregnancy
- Special consultation mechanisms have been established for prospective parents
- Clinics have their own laboratory for receiving and checking tests, which allows you to get an accurate result in the shortest possible time
- For examinations and therapy, modern devices from leading manufacturers from countries such as Japan, USA, Germany, etc. are used.
- Originator drugs (not generics) are used
To make an appointment, call 8 (495) 7-800-500 or contact one of the many registries located in Moscow, the region and regions of the Russian Federation.
Do not delay treatment, see a doctor now:
- Pregnancy test
- Gynecological appointment
- Planning and management of pregnancy
- Reproductive health
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measuring height, body weight, determining body mass index), measuring the size of the pelvis, examining the cervix in the mirrors, bimanual vaginal study | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. 5. Dry processing of seams (if any). |
 General (clinical) blood test.
General (clinical) blood test. 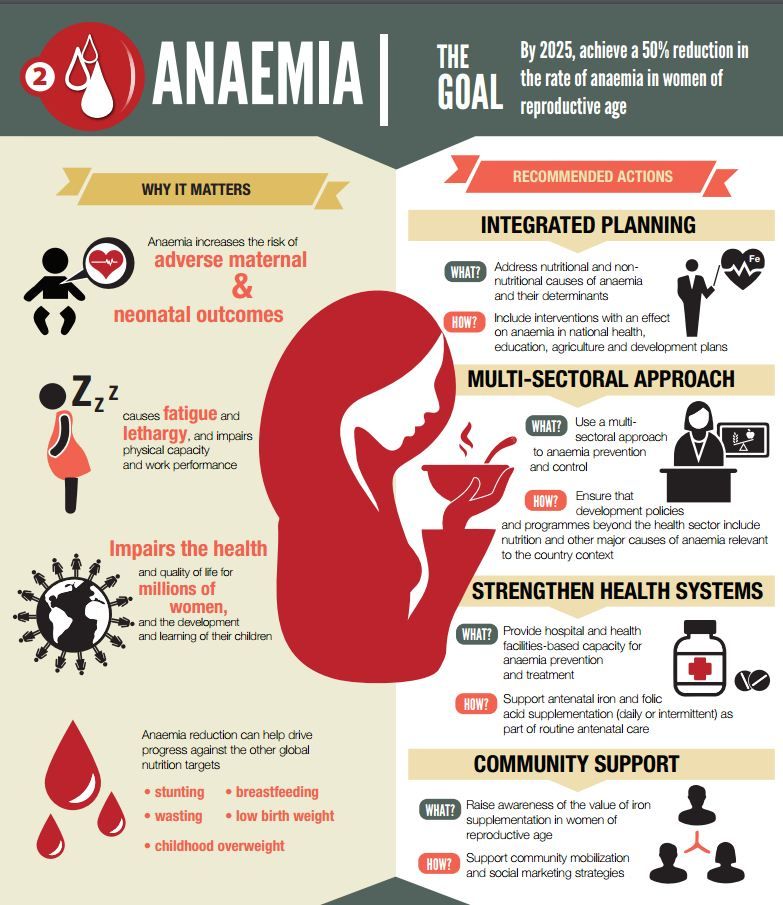
 General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 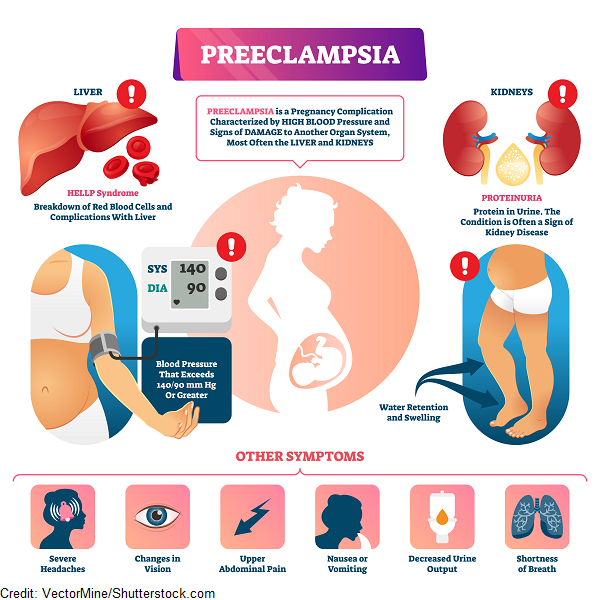 Inspections and consultations:
Inspections and consultations: