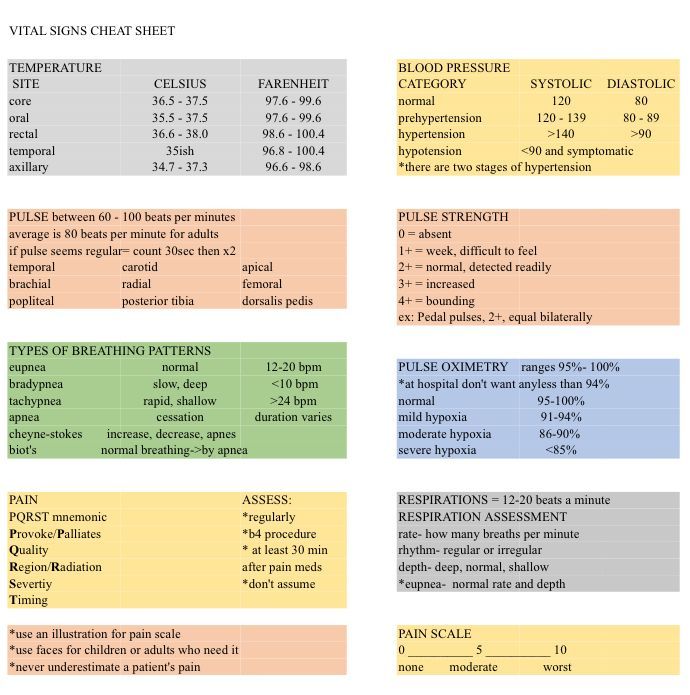
How many rescue breaths per minute for a child with pulse
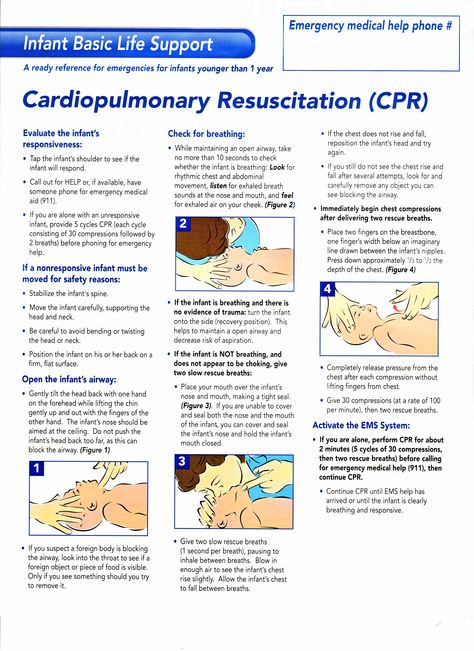
BLS Infant and Child Algorithm
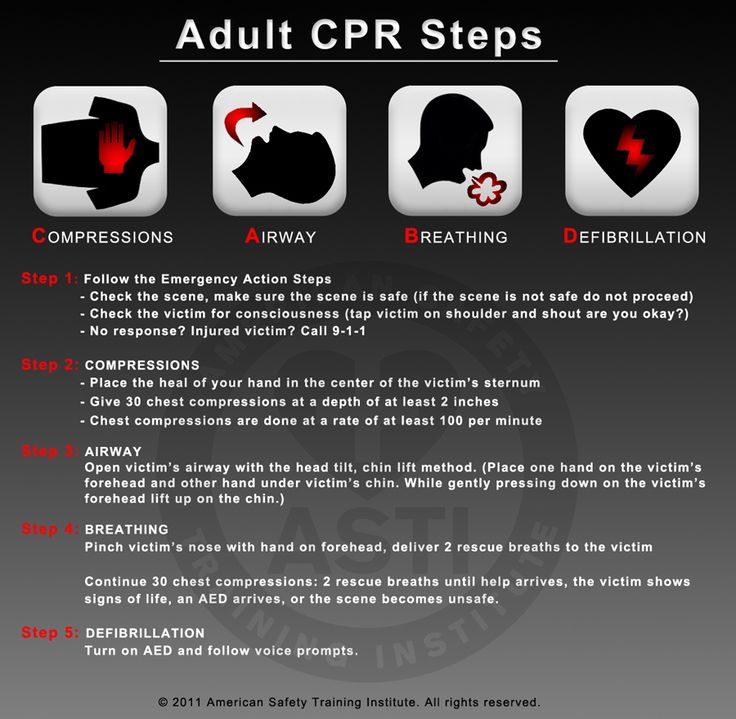
1. Secure the scene. This means pulling the victim out of standing water, traffic, or other dangerous situation. You should be safe before you begin Basic Life Support
2. Check for a response. If the victim is unresponsive and has abnormal respirations (no respirations or gasping/agonal breathing) activate EMS, yell for help, and send someone for an AED. Use a cell phone if one is available.
3. For no longer than 10 seconds, check for a pulse at the carotid or femoral artery. A heart rate of less than 60 beats per minute is considered cardiac arrest in children and infants.
If there is a pulse and breathing, continue to monitor and support breathing.
If there is a pulse and no/abnormal breathing, start rescue breathing (1 breath every 2-3 seconds).
If there is no pulse and no/abnormal breathing:
- Start high-quality CPR
- Compress to at least one-third of the anterior-posterior diameter or about 2 inches
- Allow the chest to fully recoil
- Continue CPR for 2 minutes OR until AED is on, powered up, and ready for use.
- Single rescuer: 30 compressions to 2 breaths, 100-120 compressions per minute
- Two rescuers: 15 compressions to 2 breaths, 100-120 compressions per minute
- If help is not available, leave the child to get help and an AED
- Check heart rhythm using AED
- Follow instructions on AED, deliver shock as needed
BLS
Certification
- 100% Online Training
- Unlimited Exam Retakes
- 2 Year Certification
- Guaranteed Acceptance
- Money Back Guarantee
View Course
ACLS
Certification
- 100% Online Training
- Unlimited Exam Retakes
- 2 Year Certification
- Guaranteed Acceptance
- Money Back Guarantee
View Course
PALS
Certification
- 100% Online Training
- Unlimited Exam Retakes
- 2 Year Certification
- Guaranteed Acceptance
- Money Back Guarantee
View Course
NEONATAL
Resuscitation
- 100% Online Training
- Unlimited Exam Retakes
- 2 Year Certification
- Guaranteed Acceptance
- Money Back Guarantee
View Course
All certifications are 100% Online and Accepted or your money back
- Latest ECC & ILCOR Guidelines
- No Skills Test Required
- 24/7 Online Access
- Instant Card Access
- 2 Year Certification
- 100% Money Back Guarantee
Rescue Breathing for Adults and Children: Step-by-Step Guide
Rescue breathing is a type of first aid that’s given to people who have stopped breathing. During rescue breathing, you blow air into a person’s mouth to supply them with vital oxygen.
During rescue breathing, you blow air into a person’s mouth to supply them with vital oxygen.
Rescue breathing can be done alone or as a part of cardiopulmonary resuscitation (CPR). The technique used can vary based on whether it’s being performed on an adult or a child.
In this article, we’ll discuss the rescue breathing technique in more detail, when it’s needed, and how it differs from CPR.
Oxygen is essential for life. When you breathe, oxygen enters your bloodstream through tiny air sacs in your lungs called alveoli. Once in your bloodstream, oxygen can travel to every part of your body.
Rescue breathing is a first aid technique that’s done when someone has stopped breathing (also known as respiratory arrest). Rescue breathing is also referred to as mouth-to-mouth resuscitation.
Situations that may cause breathing to stop can include the following:
- an injury due to a fall, car accident, or electrical shock
- near-drowning
- a stroke
- something stuck in the windpipe
- conditions that make it difficult to breathe, such as pneumonia, asthma, or chronic obstructive pulmonary disorder (COPD)
- a drug or alcohol overdose
- an inhalation injury from breathing in smoke or chemical fumes
When you perform rescue breathing, you gently blow air into a person’s mouth.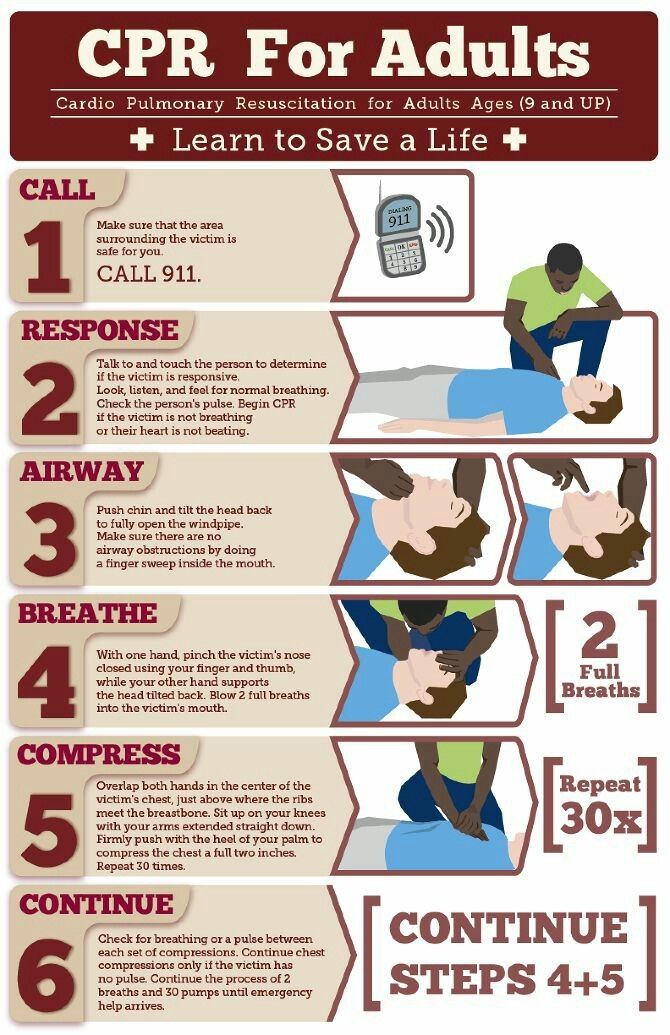 This helps supply them with vital oxygen until medical help arrives.
This helps supply them with vital oxygen until medical help arrives.
Rescue breaths can be given alone or as a part of CPR. Because of this, you may be wondering how the two are different.
Rescue breaths can be given alone when a person has a pulse but isn’t breathing. CPR is done when a person’s heartbeat and breathing have stopped. CPR involves cycles of chest compressions and rescue breathing.
It’s not uncommon for cardiac arrest (stopping of the heartbeat) to happen shortly after respiratory arrest. Because of this, you may find that giving CPR is more common in an emergency situation as opposed to giving rescue breaths alone.
There are some instances where rescue breathing isn’t recommended. This is most applicable when rescue breathing is given as a part of CPR.
The American Heart Association (AHA) updated their CPR guidelines in 2010. In these new guidelines, the AHA recommends:
- People without CPR training give hands-only CPR.
 This is CPR that uses only chest compressions without rescue breaths. In this situation, you’d give quick, uninterrupted chest compressions until help arrives.
This is CPR that uses only chest compressions without rescue breaths. In this situation, you’d give quick, uninterrupted chest compressions until help arrives. - Chest compressions come before rescue breathing. You may have heard of the ABCs of first aid, which stands for airway, breathing, and compressions. This acronym has now been updated to CAB (compressions, airway, breathing), with chest compressions ahead of breathing.
These changes came about because the process of opening the airway and effectively giving rescue breaths can take up vital time. Under the new guidelines, promptly starting chest compressions can help pump still-oxygenated blood to the body’s tissues.
Research supports these changes. For example, a 2017 review found that, when CPR is given by a bystander, just giving chest compressions increased survival compared to CPR that involved both chest compressions and rescue breathing.
Step 1: Call 911
If you encounter someone who is unresponsive and isn’t breathing, call 911.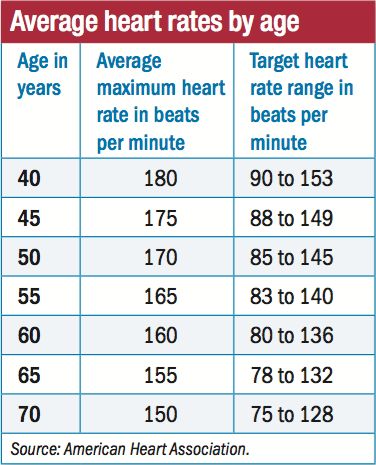 If you’re in a group, ask another person to call while you proceed to the next step.
If you’re in a group, ask another person to call while you proceed to the next step.
Important notes: In a situation where someone has a pulse but isn’t breathing, it’s important to be aware of the following:
- Someone who isn’t breathing or isn’t breathing well may make occasional gasping sounds. This isn’t the same thing as normal breathing.
- Respiratory arrest can sometimes happen before cardiac arrest. If at any point you notice that the person’s pulse has stopped, begin CPR immediately.
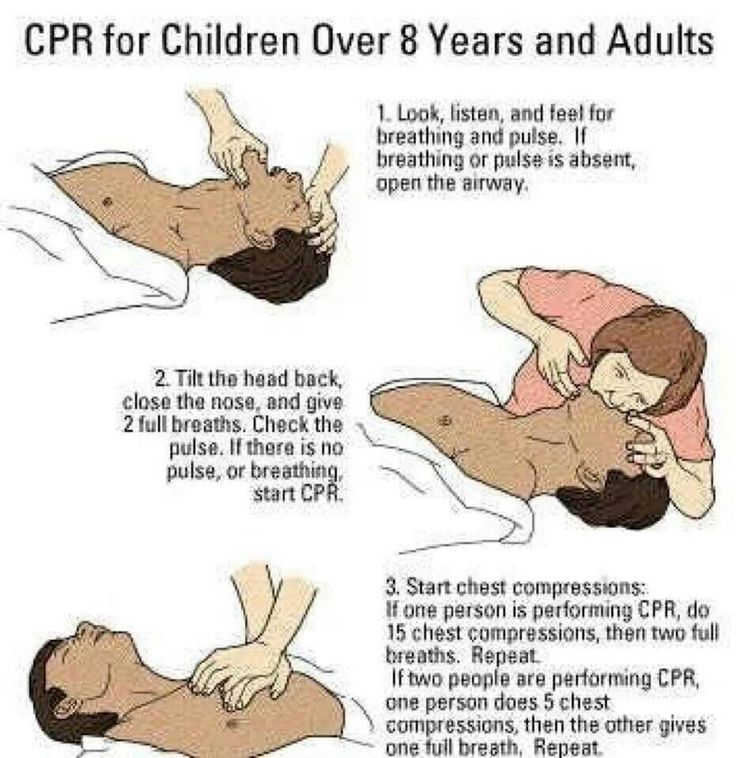
Step 2: Open the airway
To effectively give rescue breaths, it’s essential that the person’s airway is open and clear. To open a person’s airway, do the following:
- Place your hand on their forehead.
- Gently tilt their head back.
- Use the fingers of your other hand to carefully lift their chin upward.
Step 3: Give rescue breaths
Now that the airway is open, you can proceed to give rescue breaths. To do this:
To do this:
- Use the fingers of one hand to pinch the person’s nostrils shut. This helps to prevent air from escaping through their nose.
- Cover their mouth with yours, forming a seal so that air doesn’t escape.
- Give rescue breaths by gently breathing into their mouth. A rescue breath should last about 1 second. Aim to give a rescue breath every 5 to 6 seconds. This is about 10 to 12 breaths per minute.
- Check to see if the person’s chest rises as you give the first rescue breath. If it doesn’t, repeat step 2 (open the airway) before giving additional rescue breaths.
- Continue giving rescue breaths until emergency medical services (EMS) arrives or the person begins breathing normally on their own.
Important note: It’s also possible to give rescue breaths mouth-to-nose. This is an option when a person’s mouth is too injured to effectively give rescue breaths using a mouth-to-mouth technique.
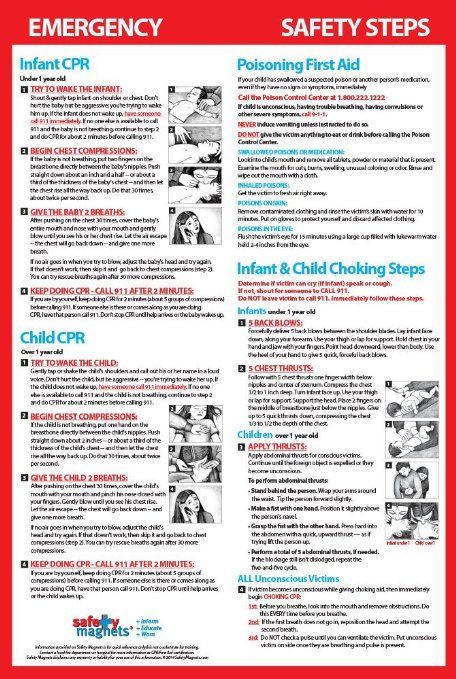
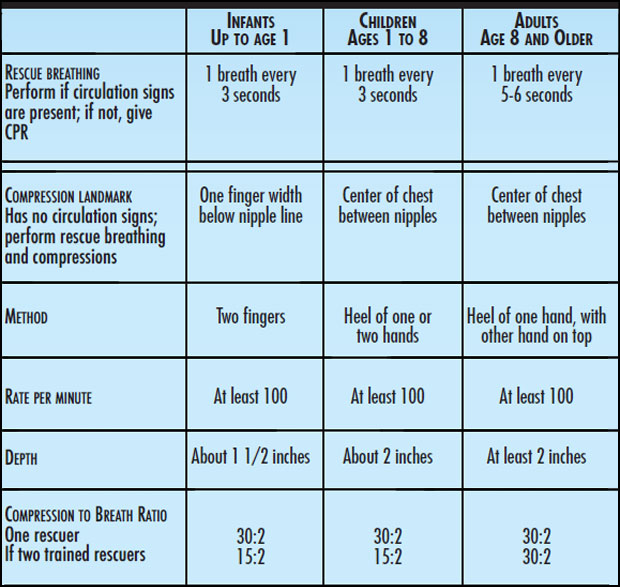
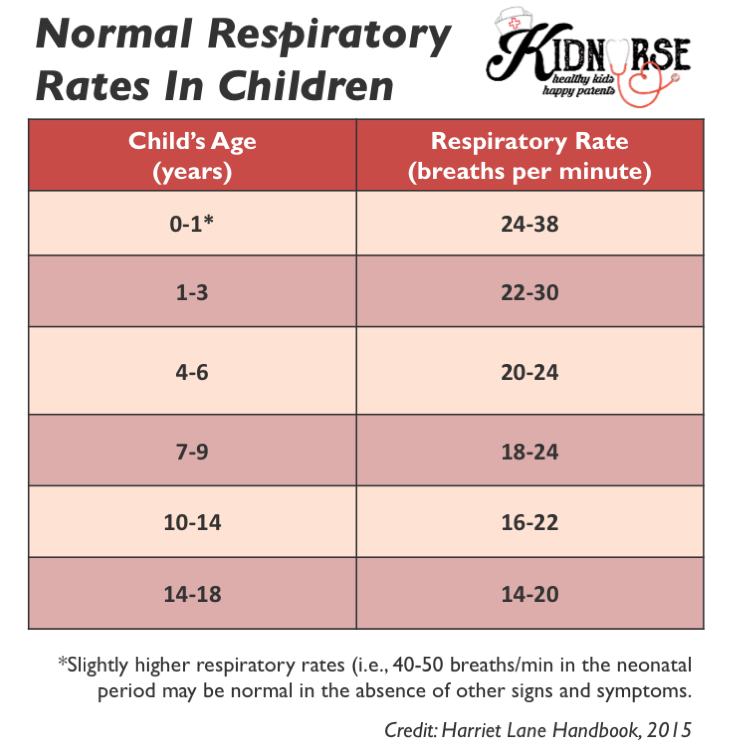
The steps for rescue breathing on a child or infant are similar to those for adults. However, there are some important things to be aware of.
However, there are some important things to be aware of.
Technique
The technique used for rescue breaths can depend on the size of the child:
- Infants and small children. Form a seal around both the mouth and nose when giving rescue breaths. If it’s difficult to form a good seal this way, try a mouth-to-nose or mouth-to-mouth technique instead.
- Older children. Use the mouth-to-mouth technique.
Frequency of breaths
The number of breaths given per minute is slightly higher for children and infants than for adults.
Aim to give 12 to 20 rescue breaths per minute for a child or infant that isn’t breathing. This is about 1 rescue breath every 3 to 5 seconds.
If you’d like to be trained in CPR and rescue breathing, consider checking out classes offered by the American Red Cross or American Heart Association.
Local resources like schools and fire departments may have classes as well.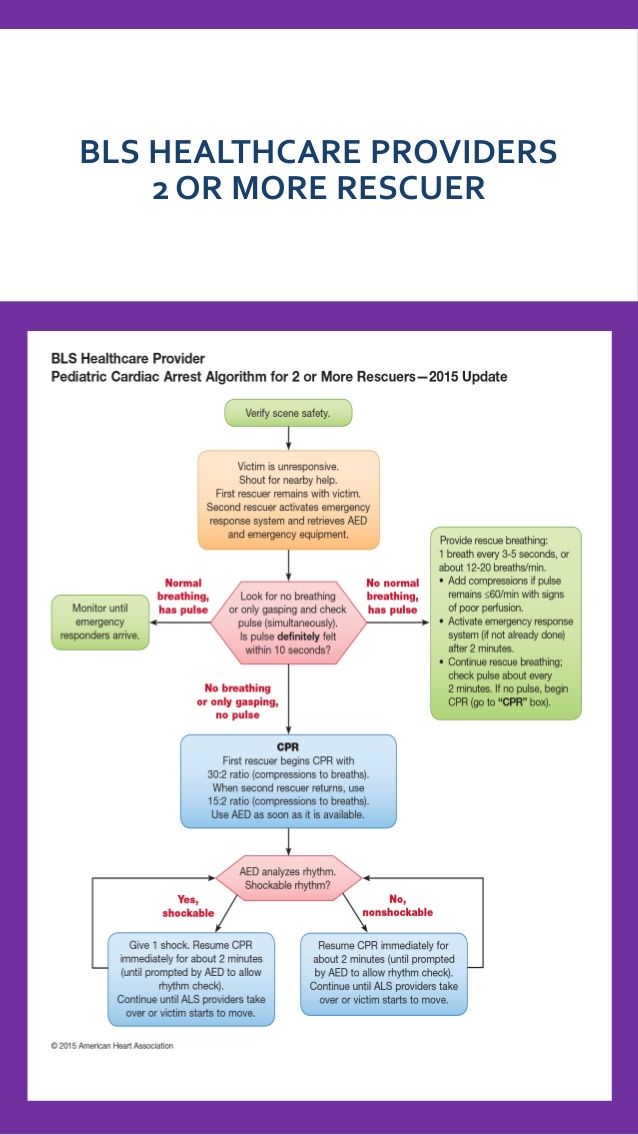
Rescue breathing is a type of first aid that’s used if someone has stopped breathing. During rescue breathing, you gently breathe into a person’s mouth every few seconds. This helps provide them with oxygen until help arrives. Rescue breathing isn’t the same as CPR.
CPR is done when a person isn’t breathing and doesn’t have a pulse. It involves cycles of chest compressions and rescue breathing. However, it’s recommended that individuals that aren’t trained in CPR only give chest compressions, without rescue breathing, if someone doesn’t have a heartbeat.
First aid | VCERM them. A.M. Nikiforov EMERCOM of Russia in St. Petersburg
Patients
Make an appointment
The ability to provide first aid is an elementary but very important skill. In an emergency, he can save someone's life. Here are 10 basic first aid skills. In this section, you will learn what to do in case of bleeding, fractures, poisoning, frostbite, and other emergencies. You will also learn about common mistakes that can put the victim's life in serious danger.
You will also learn about common mistakes that can put the victim's life in serious danger.
First aid is a set of urgent measures aimed at saving a person's life. An accident, a sudden attack of illness, poisoning - in these and other emergencies, competent first aid is needed.
According to the law, first aid is not medical - it is provided before the arrival of doctors or the delivery of the victim to the hospital. First aid can be provided by anyone who is at a critical moment next to the victim. For some categories of citizens, first aid is an official duty. We are talking about police officers, traffic police and the Ministry of Emergency Situations, military personnel, firefighters.
First aid algorithm
In order not to get confused and competently provide first aid, it is important to follow the following sequence of actions:
- Make sure you are safe and do not endanger yourself when giving first aid.
- Ensure the safety of the victim and others (eg, remove the victim from a burning car).
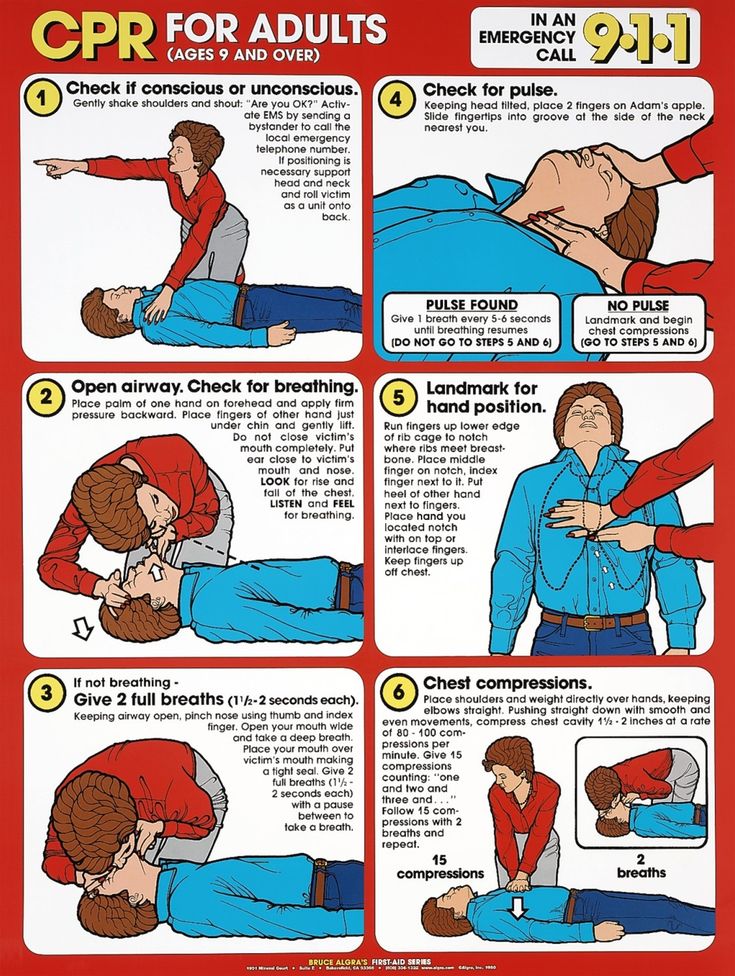
- Check for signs of life (pulse, respiration, pupillary reaction to light) and consciousness in the victim. To check for breathing, you need to tilt the victim's head back, bend over to his mouth and nose and try to hear or feel breathing. To detect the pulse, it is necessary to attach the fingertips to the carotid artery of the victim. To assess consciousness, it is necessary (if possible) to take the victim by the shoulders, shake gently and ask a question.
- Call specialists: 112 - from a mobile phone, from a landline - 03 (ambulance) or 01 (rescuers).
- Provide emergency first aid. Depending on the situation, this may be:
- restoration of airway patency;
- cardiopulmonary resuscitation;
- stop bleeding and other measures. - Provide the victim with physical and psychological comfort, wait for the arrival of specialists.
CPR
Artificial lung ventilation (ALV) is the introduction of air (or oxygen) into the respiratory tract of a person in order to restore natural ventilation of the lungs.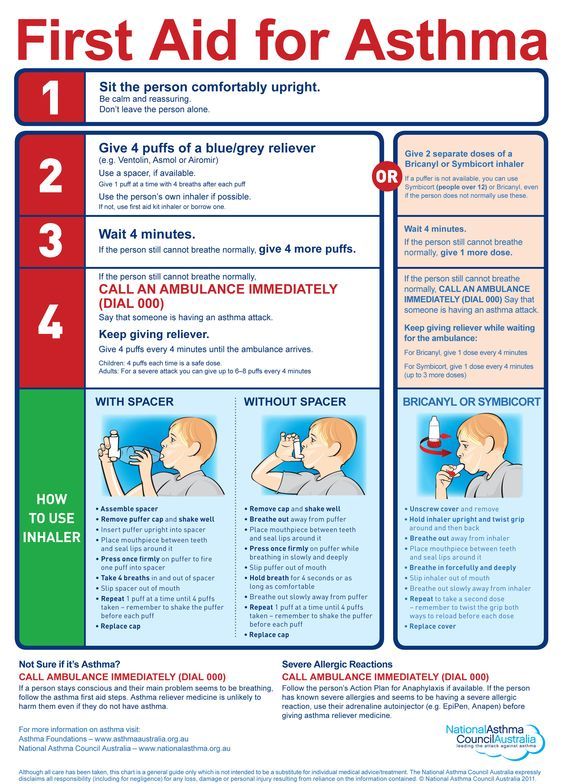 Refers to elementary resuscitation measures.
Refers to elementary resuscitation measures.
Typical situations requiring mechanical ventilation:
- car accident;
water incident;
electric shock and others.
There are various ways to ventilate. Mouth-to-mouth and mouth-to-nose artificial respiration is considered the most effective in providing first aid to a non-specialist.
If no natural respiration is detected on examination, immediately administer artificial respiration.
Mouth-to-mouth resuscitation technique
- Maintain a clear upper airway. Turn the head of the victim to one side and use your finger to remove mucus, blood, foreign objects from the oral cavity. Check the victim's nasal passages, clean them if necessary.
- Tilt the victim's head back while holding the neck with one hand.
Do not change the position of the victim's head in case of a spinal injury!
- Place a tissue, handkerchief, piece of cloth or gauze over the victim's mouth to protect yourself from infections.
 Pinch the victim's nose with your thumb and forefinger. Inhale deeply, press your lips tightly against the victim's mouth. Exhale into the victim's lungs.
Pinch the victim's nose with your thumb and forefinger. Inhale deeply, press your lips tightly against the victim's mouth. Exhale into the victim's lungs. The first 5-10 breaths should be fast (20-30 seconds), then 12-15 breaths per minute.
- Watch the movement of the victim's chest. If the victim's chest rises when inhaling air, then you are doing everything right.
Chest compressions
If there is no pulse with breathing, chest compressions should be performed.
An indirect (closed) heart massage, or chest compression, is the compression of the muscles of the heart between the sternum and the spine in order to maintain the circulation of a person during cardiac arrest. Refers to elementary resuscitation measures.
Attention! It is impossible to carry out a closed heart massage in the presence of a pulse.
Chest Compression Technique
- Lay the victim on a flat, hard surface. Do not perform chest compressions on a bed or other soft surfaces.
- Locate the affected xiphoid process. The xiphoid process is the shortest and narrowest part of the sternum, its end.
- Measure 2-4 cm upward from the xiphoid process - this is the point of compression.
- Place the base of your hand on the compression point. In this case, the thumb should point either to the chin or to the stomach of the victim, depending on the location of the resuscitator. Place the other hand on top of one hand, fold your fingers into the lock. Pressing is carried out strictly with the base of the palm - your fingers should not come into contact with the victim's sternum.
- Perform rhythmic chest thrusts strongly, smoothly, strictly vertically, with the weight of the upper half of your body. Frequency - 100-110 pressures per minute. In this case, the chest should sag by 3–4 cm.
For infants, chest compressions are performed with the index and middle fingers of one hand. Teenagers - with the palm of one hand.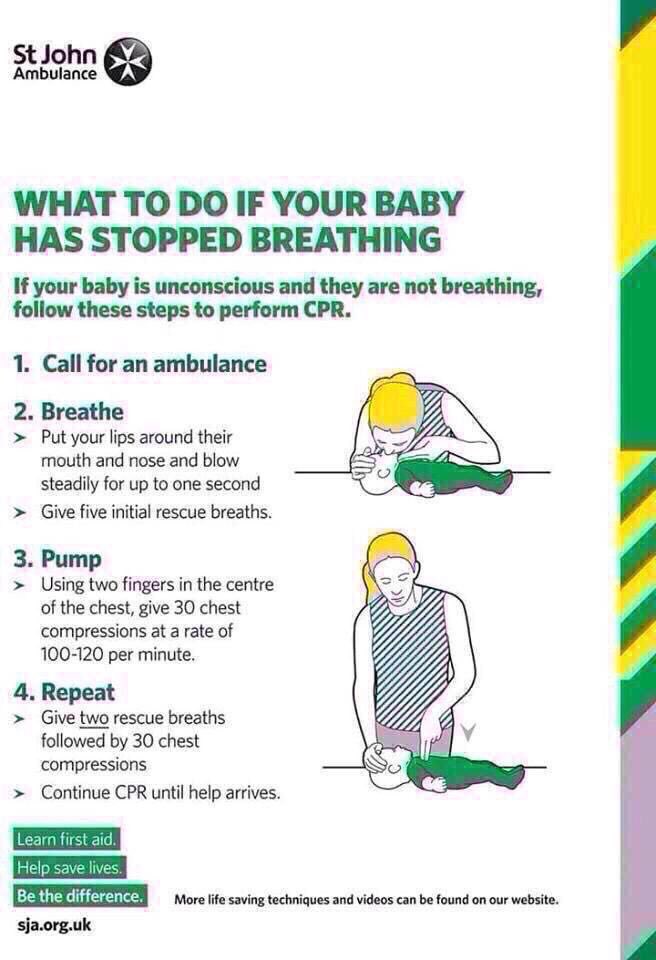
If ventilatory support is given concurrently with chest compressions, every two breaths should be alternated with 30 chest compressions.
Harm: chest compressions can break ribs, therefore broken bones can easily damage lungs and heart.
Correct: chest compressions are performed only after you have made sure that the victim has no pulse and breathing, and there is no doctor nearby. While one person is doing a heart massage, someone else must call an ambulance. Massage is performed in rhythm - 100 compressions in 1 minute. In the case of children, chest compressions are performed with the fingers in a different rhythm. After the heart starts, start performing artificial respiration. Alternative method: 30 compressions and 2 breaths, then repeat compressions and 2 breaths again.
In the event of an accident, do not remove the victim from the car and do not change his position
Harm: death is most often caused by trauma or fracture of the spine.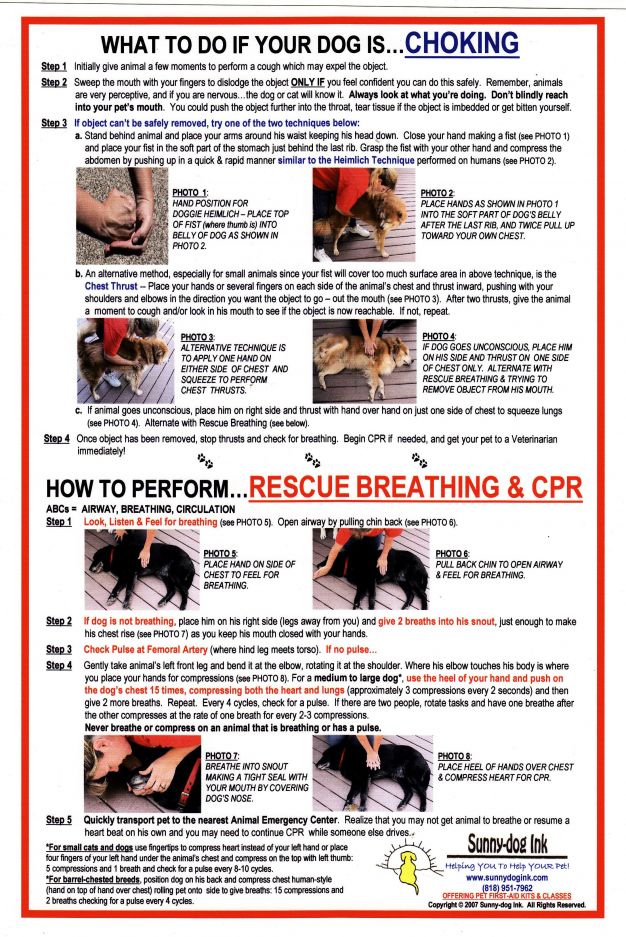 Even the most insignificant movement, caused by helping the victim to lie down more comfortably, can kill or make a person disabled.
Even the most insignificant movement, caused by helping the victim to lie down more comfortably, can kill or make a person disabled.
Correct: call an ambulance immediately after an injury if there is concern that the victim may have a head, neck, or spine injury. At the same time, monitor the patient's breathing until the arrival of doctors.
Fractures
Fracture - violation of the integrity of the bone. A fracture is accompanied by severe pain, sometimes fainting or shock, bleeding. There are open and closed fractures. The first is accompanied by a wound of soft tissues, bone fragments are sometimes visible in the wound.
Fracture First Aid Technique
- Assess the severity of the victim's condition, determine the location of the fracture.
- If there is bleeding, stop it.
- Determine if it is possible to move the victim before the arrival of specialists.
Do not carry or change position in case of spinal injury!
- Immobilize the bone in the area of the fracture - immobilize.
 To do this, it is necessary to immobilize the joints located above and below the fracture.
To do this, it is necessary to immobilize the joints located above and below the fracture. - Apply a splint. As a tire, you can use flat sticks, boards, rulers, rods, etc. The tire must be tightly, but not tightly fixed with bandages or plaster.
For a closed fracture, immobilization is performed over clothing. With an open fracture, you can not apply a splint to places where the bone protrudes outward.
Stopping bleeding with a tourniquet can lead to limb amputation
Harm: squeezing of the limbs is the result of incorrect or unnecessary application of the tourniquet. Tissue necrosis occurs due to a violation of blood circulation in the limbs, because the tourniquet does not stop the bleeding, but completely blocks the circulation.
Correct: Apply a clean cloth or sterile gauze dressing to the wound and hold it in place. Until the doctors arrive, this will be enough. Only with severe bleeding, when the risk of death is higher than the risk of amputation, is it permissible to use a tourniquet.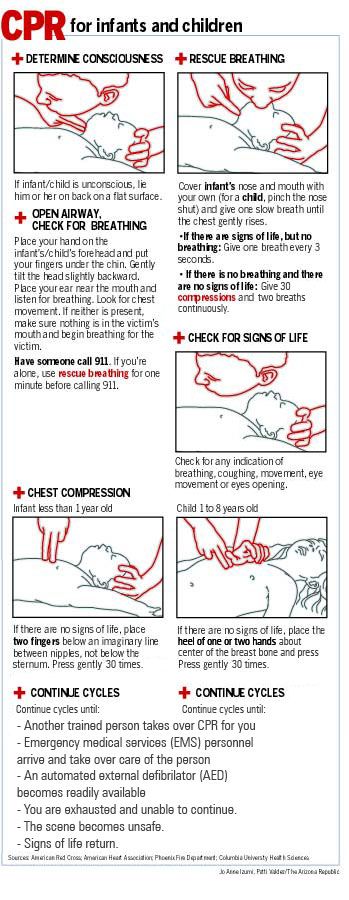
Tourniquet application technique
- Apply a tourniquet to clothing or padding just above the wound.
- Tighten the tourniquet and check the pulsation of the vessels: the bleeding should stop, and the skin below the tourniquet should turn pale.
- Bandage the wound.
- Record the exact time the tourniquet was applied.
A tourniquet may be applied to limbs for a maximum of 1 hour. After its expiration, the tourniquet must be loosened for 10-15 minutes. If necessary, tighten again, but no more than 20 minutes.
In case of bleeding from the nose, do not tilt your head back or lie down on your back
Harm: The pressure rises sharply when the head is thrown back or lying on the back during a nosebleed. Blood can enter the lungs or cause vomiting.
Correct: Keeping your head straight will speed up the pressure reduction. Apply something cold to your nose.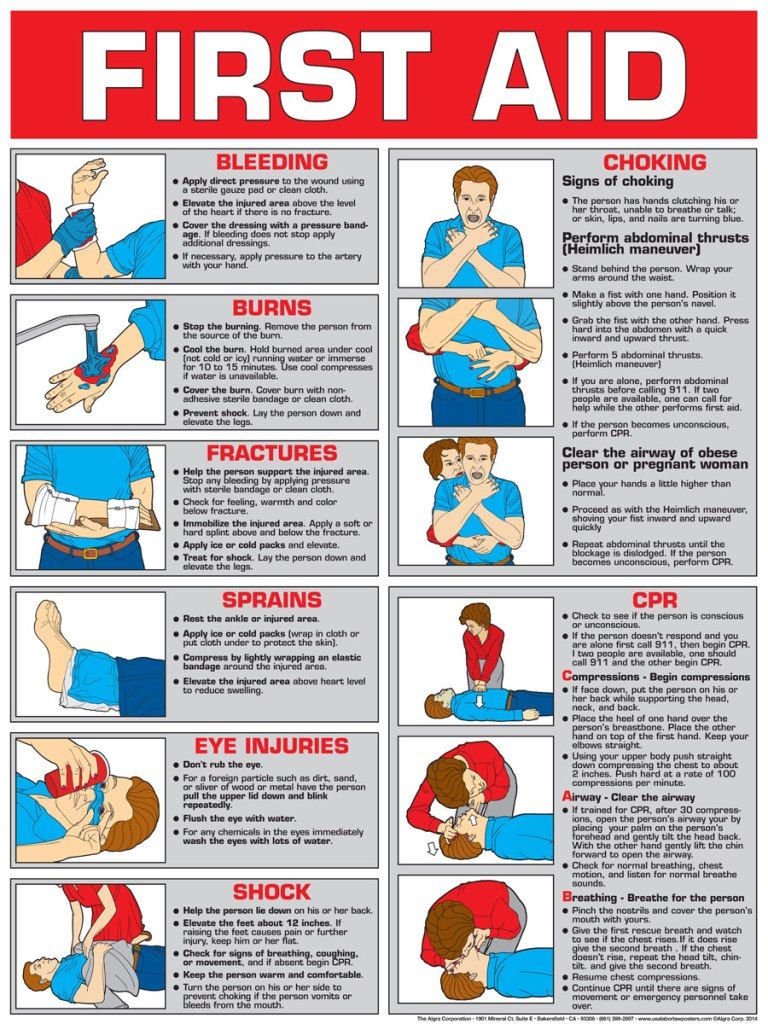 Close the nostrils alternately for 15 minutes each, with your index finger and thumb. Breathe through your mouth during this time. Repeat this technique if the bleeding does not stop. If bleeding continues, seek immediate medical attention.
Close the nostrils alternately for 15 minutes each, with your index finger and thumb. Breathe through your mouth during this time. Repeat this technique if the bleeding does not stop. If bleeding continues, seek immediate medical attention.
Use of drugs that cause vomiting
Harm: drugs that induce vomiting, burn the esophagus and cause poisoning by vomit if inhaled.
Correct: call an ambulance if you suspect poisoning. Describe the symptoms of poisoning by phone and remember the manipulations and actions that the dispatcher will recommend to you. Do not evaluate the severity of poisoning on your own and do not look for advice on the Internet - intoxication with vitamins or alcohol is very dangerous. A lethal outcome is possible in a short time if you do not seek medical help in time.
Fainting
Fainting is a sudden loss of consciousness due to a temporary interruption of cerebral blood flow. In other words, it is a signal to the brain that it lacks oxygen.
In other words, it is a signal to the brain that it lacks oxygen.
It is important to distinguish between normal and epileptic syncope. The first is usually preceded by nausea and dizziness.
The pre-fainting state is characterized by the fact that a person rolls his eyes, becomes covered with cold sweat, his pulse weakens, his limbs become cold.
Typical syncope situations:
- fright
- excitement
- stuffiness and others
If the person has fainted, put him in a comfortable horizontal position and provide fresh air (unbutton clothes, loosen belt, open windows and doors). Sprinkle cold water on the face of the victim, pat him on the cheeks. If you have a first-aid kit on hand, give a cotton swab moistened with ammonia to sniff.
If consciousness does not return after 3-5 minutes, call an ambulance immediately.
When the victim comes to, give him some strong tea.
Do not put a spoon into the mouth of a person who is having a seizure.
 And do not take out his tongue
And do not take out his tongue
Harm: A person in a fit can swallow or choke on an object that is inserted into the mouth to protect the tongue.
As correct: Seizure results in blue or violent startling. By itself, the body cannot harm itself, and the attacks end on their own. It is better to call a doctor, and make sure that the person does not harm himself and can breathe freely. Nothing will happen to the language. A person will not swallow it, and biting the tongue is not dangerous. Lay the patient on his side immediately after the attack.
Burns
A burn is damage to body tissues caused by high temperatures or chemicals. Burns vary in degrees as well as types of damage. According to the last reason, burns are distinguished:
- thermal (flame, hot liquid, steam, incandescent objects)
- chemical (alkalis, acids)
- electrical
- beam (light and ionizing radiation)
- combined
In case of burns, the first step is to eliminate the effect of the damaging factor (fire, electric current, boiling water, and so on).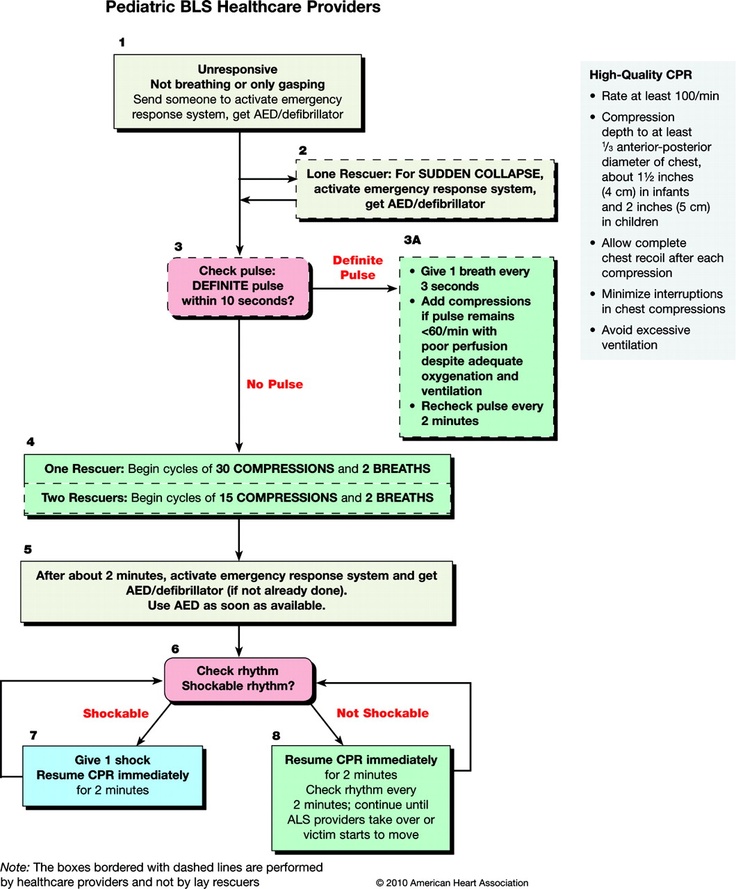
Then, in case of thermal burns, the affected area should be freed from clothing (gently, without tearing off, but cutting off the adherent tissue around the wound) and, for the purpose of disinfection and pain relief, irrigate it with a water-alcohol solution (1/1) or vodka.
Do not use oily ointments and greasy creams - fats and oils do not reduce pain, do not disinfect the burn, and do not promote healing.
After irrigate the wound with cold water, apply a sterile dressing and apply ice. Also, give the victim warm salted water.
Use dexpanthenol sprays to promote healing of minor burns. If the burn covers an area of more than one palm, be sure to consult a doctor.
Treatment with iodine, rubbing alcohol and washing wounds with hydrogen peroxide are sometimes dangerous
Harm: connective tissue is destroyed by hydrogen peroxide, thus the wound heals much longer. Alcohol, iodine and brilliant green burn intact cells and provoke a painful shock or burn on contact with the wound.
How to: Rinse the wound with clean water (boiled if possible), then treat the wound with an antibiotic ointment. Don't put on a bandage or plaster unnecessarily. A bandaged wound heals much longer.
First aid for drowning
- Remove victim from water.
A drowning man grabs everything that comes to hand. Be careful: swim up to him from behind, hold him by the hair or armpits, keeping your face above the surface of the water.
- Lay the victim on his knee with his head down.
- Clean mouth of foreign bodies (mucus, vomit, algae).
- Check for signs of life.
- In the absence of a pulse and breathing, immediately start ventilation and chest compressions.
- After recovery of breathing and cardiac activity, lay the victim on his side, cover him and keep him comfortable until the arrival of medical personnel.
Hypothermia and frostbite
Hypothermia is a drop in human body temperature below the norm necessary to maintain normal metabolism.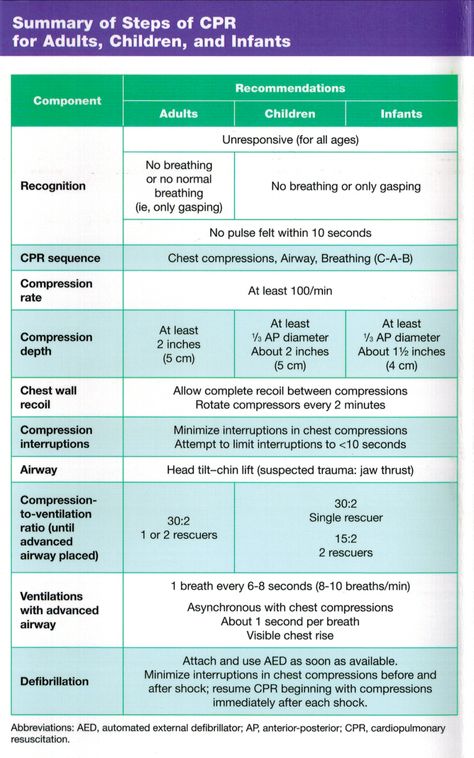
Hypothermia First Aid
- Bring the casualty into a warm room or cover with warm clothing.
- Do not rub the victim, let the body gradually warm up on its own.
- Give victim warm drink and food.
Do not use alcohol!
Hypothermia is often accompanied by frostbite, that is, damage and necrosis of body tissues under the influence of low temperatures. Frostbite is especially common in the fingers and toes, nose and ears, parts of the body with reduced blood supply.
Causes of frostbite - high humidity, frost, wind, immobility. Aggravates the condition of the victim, as a rule, alcohol intoxication.
Symptoms:
- cold feeling
- tingling in the frostbitten part of the body
- then numbness and loss of sensation
First aid for frostbite
- Keep victim warm.
- Remove any frozen or wet clothing from him.
- Do not rub the victim with snow or a cloth, as this will only injure the skin.
- Cover the frostbitten area.
- Give victim hot sweet drink or hot food.
Poisoning
Poisoning is a disorder of the body's vital functions resulting from the ingestion of a poison or toxin. Depending on the type of toxin, poisoning is distinguished:
- carbon monoxide
- pesticides
- alcohol
- drugs
- food and other
First aid measures depend on the nature of the poisoning. The most common food poisoning is accompanied by nausea, vomiting, diarrhea and stomach pain. In this case, the victim is recommended to take 3-5 grams of activated charcoal every 15 minutes for an hour, drink plenty of water, refrain from eating and be sure to consult a doctor.
In addition, accidental or intentional drug poisoning and alcohol intoxication are common.
In these cases, first aid consists of the following steps:
- Rinse the victim's stomach.
 To do this, make him drink several glasses of salted water (for 1 liter - 10 g of salt and 5 g of soda). After 2-3 glasses, induce vomiting in the victim. Repeat these steps until the vomit is "clean".
To do this, make him drink several glasses of salted water (for 1 liter - 10 g of salt and 5 g of soda). After 2-3 glasses, induce vomiting in the victim. Repeat these steps until the vomit is "clean". Gastric lavage is possible only if the victim is conscious.
- Dissolve 10-20 tablets of activated charcoal in a glass of water and give it to the victim to drink.
- Wait for the specialists to arrive.
Make an appointment
GBOUDPORO "TsPK" - Rostov-on-Don - Main
Distance learning
Professional retraining
Professional training
Master classes
Teachers of teachers, educators
Teaching of the population
24 November 24-Conference "Epidemiological Security"
9000 October 8 - World Day of Hospice and Palliative Care
June 19 - Day of the Medical Worker
Congratulation of the Governor of the Rostov Region on the Day of the Medical Worker
June 12 — Day of Russia
×
joomla/registry/src/Format/Json.
 php:78 Stack trace: #0 /var/www/cpk/data/www/cpkmed.ru/libraries/vendor/joomla/registry/src/Registry.php(370): Joomla\Registry\Format\Json->stringToObject('{"show_title" :"...', Array) #1 /var/www/cpk/data/www/cpkmed.ru/libraries/vendor/joomla/registry/src/Registry.php(76): Joomla\Registry\Registry->loadString('{"show_title":" ...') #2 /var/www/cpk/data/www/cpkmed.ru/components/com_content/models/article.php(165): Joomla\Registry\Registry->__construct('{"show_title":"...' ) #3 /var/www/cpk/data/www/cpkmed.ru/libraries/src/MVC/View/HtmlView.php(425): ContentModelArticle->getItem() #4 /var/www/cpk/data/www/cpkmed.ru/components/com_content/views/article/view.html.php(42): Joomla\CMS\MVC\View\HtmlView->get('Item' ) #5 /var/www/cpk/data/www/cpkmed.ru/libraries/src/MVC/Controller/BaseController.php(672): ContentViewArticle->display() #6 /var/www/cpk/data/www/cpkmed.ru/components/com_content/controller.php(118): Joomla\CMS\MVC\Controller\BaseController->display(true, Array) #7 /var/www/cpk/data/www/cpkmed.
php:78 Stack trace: #0 /var/www/cpk/data/www/cpkmed.ru/libraries/vendor/joomla/registry/src/Registry.php(370): Joomla\Registry\Format\Json->stringToObject('{"show_title" :"...', Array) #1 /var/www/cpk/data/www/cpkmed.ru/libraries/vendor/joomla/registry/src/Registry.php(76): Joomla\Registry\Registry->loadString('{"show_title":" ...') #2 /var/www/cpk/data/www/cpkmed.ru/components/com_content/models/article.php(165): Joomla\Registry\Registry->__construct('{"show_title":"...' ) #3 /var/www/cpk/data/www/cpkmed.ru/libraries/src/MVC/View/HtmlView.php(425): ContentModelArticle->getItem() #4 /var/www/cpk/data/www/cpkmed.ru/components/com_content/views/article/view.html.php(42): Joomla\CMS\MVC\View\HtmlView->get('Item' ) #5 /var/www/cpk/data/www/cpkmed.ru/libraries/src/MVC/Controller/BaseController.php(672): ContentViewArticle->display() #6 /var/www/cpk/data/www/cpkmed.ru/components/com_content/controller.php(118): Joomla\CMS\MVC\Controller\BaseController->display(true, Array) #7 /var/www/cpk/data/www/cpkmed.