Can you get an abortion at 16 weeks
Surgical Abortion (Second Trimester) | Conditions & Treatments
During the second trimester, 15 to 23 weeks after your last menstrual period, abortions are typically performed over a two-day period but don't require an overnight stay in the hospital. These procedures are known as dilation and evacuation (D&E).
On the first day, usually a Tuesday, you'll meet a health educator and doctor at the UCSF Women's Options Center to prepare for the procedure. This visit will take about two and a half hours.
The next day, you'll meet the doctor at UCSF Medical Center hospital at Mount Zion. This visit will take about four to five hours. In some cases, the procedure can be performed in one day for pregnancies 18 weeks or less, depending on the circumstances.
Cervical softening and dilating is performed with medication and small dilating sticks, called laminaria or Dilapan, that may be placed in the cervix, depending on the term of the pregnancy and your medical history. Laminaria are thin sticks made from a special seaweed material that widen as they absorb moisture from your body. Dilapan are synthetic sticks that work in the same way. The laminaria will stay in your cervix overnight and prepare your body for the next day's surgical procedure.
Preoperative Appointment
In a private exam room, you will learn about your procedure, undergo an exam and ultrasound, and receive oral medications that may include a pain reliever and anti-anxiety medication for relaxation, if laminaria is required for overnight dilation. If you're given medications, it's important that you follow the instructions provided by your doctor.
During the laminaria insertion, you'll be awake. If someone accompanies you, he or she can remain in the exam room, if you wish. The doctor will:
- Place a speculum to view inside your vagina.
- Clean the cervix with gauze soaked in soap.
- Apply numbing medication (local anesthesia) to the cervix.
- Insert laminaria (or Dilapan) into your cervix, the opening to the uterus.
 The laminaria insertion takes about five to 10 minutes.
The laminaria insertion takes about five to 10 minutes.
After the procedure, you will rest for a few minutes. You may experience cramping and spotting. You may get dressed when you feel able. We will give you detailed instructions on how to take care of your body overnight and how to prepare for the next day's procedure.
Someone must drive you home if you take anti-anxiety medications. Rest at home until the medications wear off.
Continue reading
Surgical Appointment
Don't eat for at least eight hours before your operating room procedure. You may drink clear liquids (such as water, broth or tea) up to three hours before your procedure.
The next day, you'll check in at the hospital reception area of UCSF Medical Center at Mount Zion, then go to the preoperative area, where you'll meet your doctor.
Medication will be administered intravenously (IV) in your arm to induce anesthesia or loss of consciousness. Most women fall asleep and don't remember the procedure. After you're well relaxed, the doctor will remove the laminaria and use suction and gynecological instruments to empty your uterus, with ultrasound guidance. You'll be in the operating room for about an hour, but the procedure may take from 15 to 45 minutes.
Most women fall asleep and don't remember the procedure. After you're well relaxed, the doctor will remove the laminaria and use suction and gynecological instruments to empty your uterus, with ultrasound guidance. You'll be in the operating room for about an hour, but the procedure may take from 15 to 45 minutes.
Recovery
In the recovery room, nurses will monitor you for about two hours. You may have some cramping and spotting. Before you return home, you'll receive antibiotics to prevent infection and instructions for postsurgical care.
The procedure and recovery period at the hospital takes about five hours in total.
Because of medications administered, you shouldn't drive until the medications wear off. Please make arrangements ahead of time for someone to take you home directly.
If you don't have anyone to accompany you home, contact Access, a women's health rights organization that may have a pro-choice volunteer driver to assist you. This must be coordinated with our clinic before your appointment, so please make arrangements as soon as possible.
You can expect to return to normal activities, such as work and school, the next day.
See our frequently asked questions about post-procedure care.
Follow-Up Visits
Unless you experience complications or have concerns, there's no need to return to the Women's Options Center. We recommend that you see your primary care doctor for regular evaluations.
Safety and Effectiveness
Second-trimester surgical abortion is one of the safest medical procedures. Although rare, possible complications include a blood clot in the uterus that can cause pain or require a repeat aspiration; infection, which is generally easily identified and treated; a tear in the cervix that can be easily repaired with suture; perforation; retained pregnancy tissue requiring repeat aspiration; and excessive bleeding requiring a transfusion.
Complications from a surgical abortion are considerably less frequent and less serious than those associated with giving birth.
Second Trimester Abortion Procedure | UCLA Health
During the second trimester, from 14 to 23 weeks and 6 days after your last menstrual period, abortions are typically performed over a two to three day period but don't require an overnight stay in the hospital. This procedure is known as a dilation and evacuation (D&E).
This procedure is known as a dilation and evacuation (D&E).
On the first day, you'll meet your medical team at the UCLA West Med Clinic to prepare for the procedure. This first visit typically takes about 3-4 hours.
On the day of the procedure, usually a Wednesday or a Friday, you'll meet the medical team at UCLA Ronald Reagan Medical Center. This visit will take about 6-8 hours.
Pre-Operative Appointment
In a private exam room, you will learn about your procedure, undergo an exam and ultrasound, and may receive oral pain/anxiety medications. You will receive prescriptions for pain medications and antibiotics. It is important that you follow the instructions provided by your doctor. You will have the option to discuss and choose a birth control method. You will also have the option to make arrangements for private cremation services if you choose.
Depending on your gestational age and medical history, cervical softening and dilating is performed with medication and/or small dilating sticks, called laminaria or Dilapan. Laminaria are thin sticks made from a special seaweed material that widen as they absorb moisture from your body. Dilapan are synthetic sticks that work in the same way. The dilators will stay in your cervix overnight, and allow the process of cervical dilation to happen slowly, which helps to prepare your body for the surgical procedure. Depending on your gestational age, you may come back for a second day of pre-op, during which the previous dilators will be removed and new ones will be put in. You may also receive an injection in the uterus that induces fetal demise.
Laminaria are thin sticks made from a special seaweed material that widen as they absorb moisture from your body. Dilapan are synthetic sticks that work in the same way. The dilators will stay in your cervix overnight, and allow the process of cervical dilation to happen slowly, which helps to prepare your body for the surgical procedure. Depending on your gestational age, you may come back for a second day of pre-op, during which the previous dilators will be removed and new ones will be put in. You may also receive an injection in the uterus that induces fetal demise.
During the dilator insertion, you'll be awake. The doctor will:
- Give you pain and/or anxiety medication to help with discomfort
- Place a speculum to view inside your vagina.
- Clean the cervix with gauze soaked in soap.
- Apply numbing medication (local anesthesia) to the cervix.
- Insert laminaria (or Dilapan) into your cervix, the opening to the uterus. The laminaria insertion takes about five to 10 minutes.

After the procedure, you will rest for a few minutes. You may experience cramping and spotting. You may get dressed when you feel able. Our nurse will give you detailed instructions on how to take care of your body overnight and how to prepare for the next day's procedure. She will also draw your blood as necessary.
Someone must drive you home if you take anti-anxiety or opiate pain medications. If needed, you and a support person can ride home together in an Uber/Lyft. Note: your driver/support person does NOT need to know you are having an abortion. They just need to be someone you can trust to get you home safely afterwards. We will not disclose your health information to anyone without your explicit consent. Rest at home until the medications wear off. It is recommended that you continue to relax at home for the rest of the day after your pre-op visit.
Surgical Appointment
Don't eat or drink after midnight on the day of your surgical procedure.
On the surgical day, you'll check-in at the hospital reception area at UCLA Ronald Reagan Medical Center then go to the pre-operative area, where you'll meet your medical team. They will begin to get you ready for the procedure.
Once you are in the procedure room, medication will be administered intravenously (IV) in your arm to induce anesthesia or loss of consciousness. Most patients fall asleep and don't remember the procedure. After you're well relaxed, the doctor will remove the laminaria and use gentle suction and gynecological instruments to empty your uterus, with ultrasound guidance. If you desired a contraceptive implant or intrauterine device, it will be placed in the operating room after your procedure. You'll be in the operating room for about an hour but the procedure will likely only take about 15 to 30 minutes.
Recovery
In the recovery room, nurses will monitor you for about two hours. You may have some cramping and spotting. The procedure and recovery period at the hospital usually takes about six to eight hours in total. Because of medications administered, you shouldn't drive until the medications wear off. Please make arrangements ahead of time for someone to take you home directly.You can expect to return to normal activities, such as work and school, the next day.
Because of medications administered, you shouldn't drive until the medications wear off. Please make arrangements ahead of time for someone to take you home directly.You can expect to return to normal activities, such as work and school, the next day.
If you don't have anyone to accompany you home, contact ACCESS Reproductive Justice, a reproductive rights organization that may have a pro-choice volunteer driver to assist you. This must be coordinated with our clinic before your appointment, so please make arrangements as soon as possible. ACCESS can be reached via phone call or text message at 800-376-4636. Their usual hours are Monday-Friday, 10:00 am to 4:00 pm PST.
Follow-Up Visits
You will have a follow up appointment one to two weeks after your procedure to confirm that your procedure is completed and that you are healing well. This visit is typically done via telehealth, though you can also be seen for an in-person evaluation. At this visit, you can also get a prescription for birth control.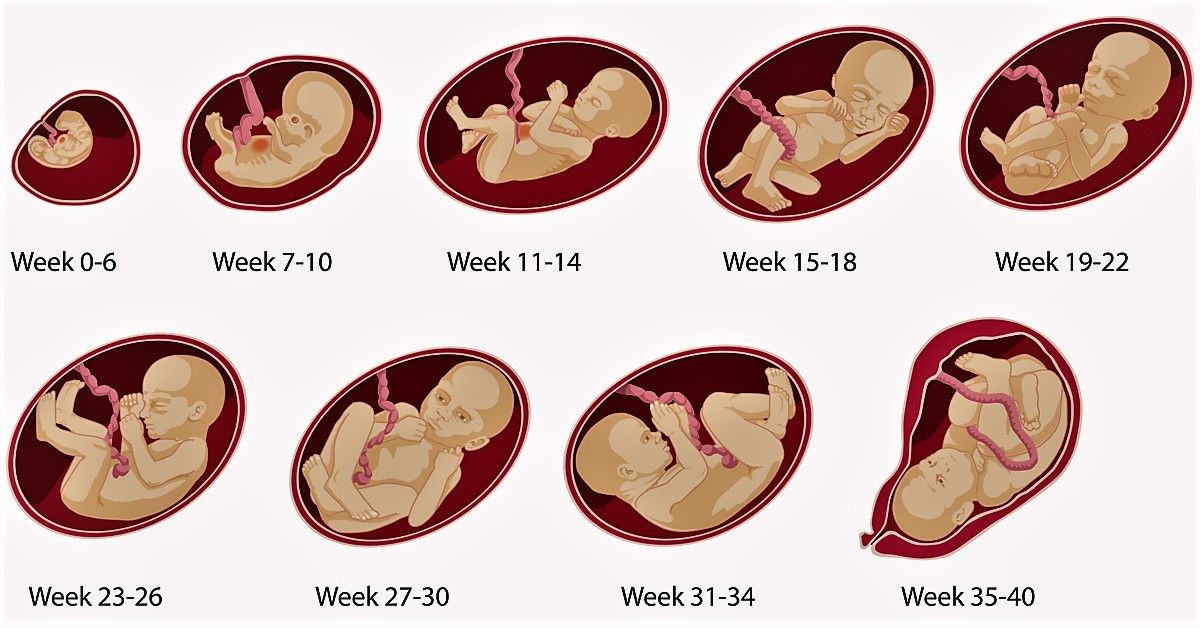
Safety and Effectiveness
Second trimester surgical abortion is one of the safest medical procedures. Although rare, possible complications include a blood clot in the uterus that can cause pain or require a repeat suction procedure; infection, which is generally easily identified and treated; a tear in the cervix that can be easily repaired with suture; perforation of the uterus; retained pregnancy tissue requiring a repeat suction procedure; and excessive bleeding requiring a transfusion. Complications from a surgical abortion are considerably rarer and much less serious than those associated with giving birth.
Termination of pregnancy at early and late stages
one Termination of pregnancy in the early and late stages
Early termination of pregnancy
Up to 12 weeks of pregnancy, a woman can have an abortion of her choice, for medical and social reasons. Early pregnancy can be terminated by both surgical and non-surgical methods. Surgical methods include vacuum aspiration and surgical abortion. Non-surgical methods include medical abortion.
Surgical methods include vacuum aspiration and surgical abortion. Non-surgical methods include medical abortion.
It is known that if for some reason a woman needs to get rid of an unwanted pregnancy, then it is best to do it in its early stages. However, situations are often created when a late abortion has to be done.
Late pregnancy termination
After 12 weeks of pregnancy, the possibility of abortion at the request of the woman herself is already excluded. Late abortion is performed only for medical or social reasons. The decision on the need for such an abortion is made by the medical council or the court.
The causes of late abortion can be: the death of the breadwinner during gestation, the social failure of the mother, the presence of a serious illness in the mother, pathology of the fetus.
Termination of pregnancy at 20 weeks is performed in inpatient or outpatient facilities only for medical reasons.
The presence of indications for late termination of pregnancy is established by a medical commission, which consists of an obstetrician-gynecologist, a specialist in the disease, and the head of a medical institution. If a mental or sexually transmitted disease becomes the cause of a late abortion, then the documentation is sent to the obstetric and gynecological institution.
If a mental or sexually transmitted disease becomes the cause of a late abortion, then the documentation is sent to the obstetric and gynecological institution.
Late abortions: types
At the late stage of pregnancy, the fetus is already formed, so the only possible way to remove it is surgery, artificial birth or caesarean section. Any surgical intervention should be performed only in specialized medical institutions that have the appropriate license.
Late abortions are carried out in strict accordance with established rules, namely:
If there is any doubt about the verdict of the doctors, a woman can always be re-examined at another clinic.
How the late abortion procedure works
The late abortion procedure usually takes about 3 days. During the first day, the cervix is dilated. However, the woman is prescribed anti-spasmodic drugs, which are designed to reduce pain. At the beginning of the 3rd day, a woman takes certain medications that start the process of childbirth. The uterus contracts and contractions begin.
The uterus contracts and contractions begin.
An obstetrician-gynecologist uses ultrasound to find out the position of the fetus and performs the necessary surgical procedures to extract it.
After that, the remains of the fetus and the placenta are taken out or sucked out with a special device. If the abortion turned out to be incomplete, then additionally the bottom of the uterus is scraped from blood clots and tissue remnants.
For more than 25 weeks' gestation, a caesarean section is performed.
Any abortion is a great stress for a woman's body, and, of course, it is better to try to avoid an unwanted pregnancy than to carry out such difficult interventions with a high risk of complications.
Literature
- Federal Law of the Russian Federation dated November 21, 2011 No323-F3 "On the Fundamentals of Protecting the Health of Citizens in the Russian Federation" (as amended).
- Dicke G.B., Yarotskaya V.A., Erofeeva A.
 V. Strategic assessment of policies, programs and services in the field of unplanned pregnancy, abortion and contraception in the Russian Federation (Joint study of the Ministry of Health and Social Development of the Russian Federation and WHO). reproduction problems. - 2010. - No3. - S. 92-97.
V. Strategic assessment of policies, programs and services in the field of unplanned pregnancy, abortion and contraception in the Russian Federation (Joint study of the Ministry of Health and Social Development of the Russian Federation and WHO). reproduction problems. - 2010. - No3. - S. 92-97. - Trubnikova L.I., Trubnikov V.C., Egorova O.A. Comparative characteristics of modern methods of terminating early pregnancy II Proceedings of the first regional forum "Mother and Child". - Kazan, 2007. - S. 346-347.
why terminate a pregnancy in the later stages and how it is done in Krasnoyarsk
“Like a bolt from the blue”
“We counted the fingers and toes, saw how the heart was beating. Then there was a short pause, and the doctor asked us to go for a walk so that the baby would roll over and he could finish the study. When we returned, there were already two doctors in the doctor's office. Now they were staring at the monitor together and trying to see something. I understood that there were some problems.
I understood that there were some problems.
And suddenly, like a bolt from the blue, the phrase sounded: “I can’t see the baby’s bladder. There is some kind of education, but what it is is too hard to understand ", - there are hundreds of stories with a similar beginning.
For many women, becoming a mother is a cherished dream. In most cases, pregnancy ends safely - the birth of a healthy baby. But sometimes families get a disappointing prognosis even at the stage of the first ultrasound and tests. Finding out that a child has serious illnesses is always difficult, especially if the health of the father and mother is all right and there are no prerequisites for terrible diagnoses.
Where to go, what to do, what decisions to make? These are only the first questions that arise in pregnant women who have received a poor prognosis.
It is not customary in society to discuss this topic. In our time, when the question of whether abortion is considered murder is still unresolved, the topic of late pregnancy termination, when the unborn child is not just an embryo, but already looks like a full-fledged baby, is painful even for the medical community.
"No error"
Memories of mothers who have experienced the loss of a child (from the forum of the charity foundation "Light in Hands"): "After 12 weeks, no one will terminate a pregnancy without a special consultation of doctors and a clearly established diagnosis. Needless to say, none of the doctors spoke to us normally, no one explained a clear sequence of actions, terms, risks, what does “abortion of pregnancy”, etc. mean in general?
Genetic abnormalities are detected at the stage of screenings of a pregnant woman, there are three in total. Screening is a set of studies that allows you to get the most complete information about the health of the fetus. If the ultrasound doctor has doubts during the examination, the patient is sent to the Medical Genetic Center.
“Of course, most of all we are tuned in to early diagnosis, namely, to identify some abnormalities up to 12 weeks, less often up to 21-22 weeks. But sometimes there are cases when deviations can be detected only in the second half of the term: usually this happens either when a woman registers late and has never been examined before, or when the pathology manifests itself late. Then a decision is already made on a more detailed examination and on the possible termination of such a pregnancy, ”said Tatyana Elizaryeva, head physician of the medical genetic center.
Then a decision is already made on a more detailed examination and on the possible termination of such a pregnancy, ”said Tatyana Elizaryeva, head physician of the medical genetic center.
The Medical Genetic Center of Krasnoyarsk sees patients from all over the Krasnoyarsk Territory. In the event that the doctor has doubts about the health of the child during the screening, the pregnant woman is sent for a more detailed examination
If the woman has passed all the examinations and the diagnosis is confirmed, she is invited to the medical commission of the genetic center. You can come to it either alone or with your husband or family members, usually the patient is asked how it is convenient for her. The commission includes several specialists: an ultrasound diagnostician, a neonatologist, an obstetrician-gynecologist, a doctor specializing in a particular pathology (cardiac surgeon, neurosurgeon, pediatric surgeon, etc.). There, the woman is told in detail about what is happening, what kind of pathology the child has, whether it can be treated and what kind of treatment it is.
“It is important to let a woman understand what she is facing and offer all possible options. If these are chromosomal disorders and an intellectual deficiency in the fetus, for example, Down's syndrome, we explain that a child can be born and, in the absence of any physical disabilities, even be able to develop - sit, perhaps write and draw, communicate a little. But we also make it clear that such a child will never be able to live independently, especially after the departure of parents or other guardians, such a child requires rather large financial costs, which not every family is ready for, such a child will always require more attention and strength, and for his parents will have to fight every step in his development. All this is necessary so that families understand what they are getting into in both cases. In any situation, we, as doctors, are obliged to respect their choice,” emphasizes Tatiana Elizarieva.
After a medical consultation, any couple has time to think and make an informed decision. Doctors note that today the equipment and technology of the medical genetic center excludes even the very possibility of making an incorrect diagnosis. In addition, in each case, the results of the tests are processed by several doctors, each giving an opinion and recommendations on pregnancy.
Doctors note that today the equipment and technology of the medical genetic center excludes even the very possibility of making an incorrect diagnosis. In addition, in each case, the results of the tests are processed by several doctors, each giving an opinion and recommendations on pregnancy.
“This is a forced measure”
Up to 22 weeks, pregnancy can be terminated, including by medication. The procedure is carried out in the Krasnoyarsk maternity hospital No. 4.
“Medical indications for termination of pregnancy from 12 to 22 weeks are fetal developmental anomalies that are incompatible with life and cannot be surgically corrected,” said Lyudmila Popova, chief physician of maternity hospital No. 4.
This is a chromosome analysis. In a healthy person, all chromosomes are paired, in the picture at number 21 there are three chromosomes instead of two. This is what Down syndrome looks like
According to doctors, a woman can choose to terminate her pregnancy or report it.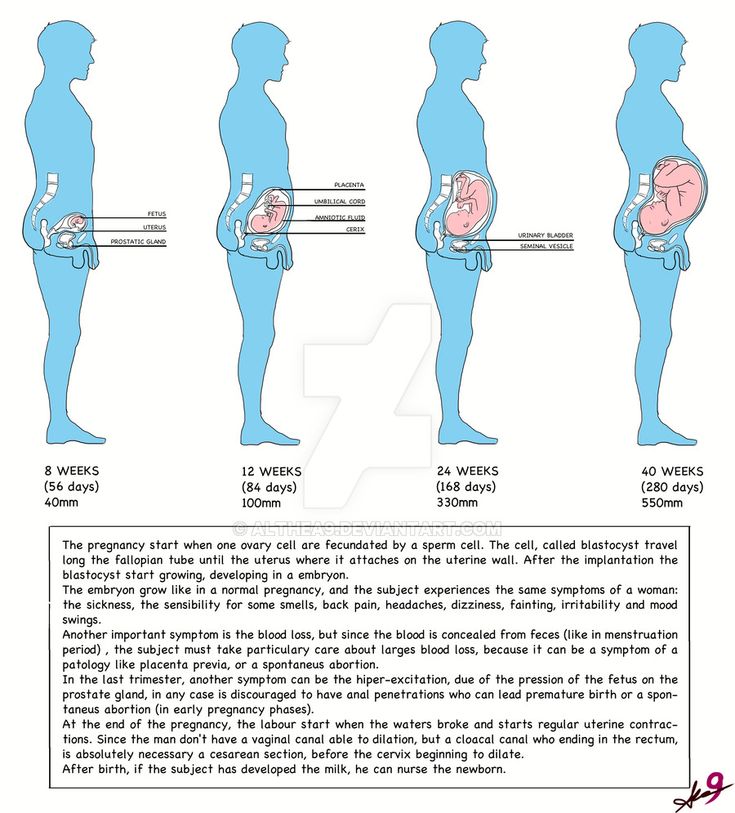 But often mothers do not fully realize what they doom themselves and their families to when they give birth to children with serious pathologies or non-viable ones.
But often mothers do not fully realize what they doom themselves and their families to when they give birth to children with serious pathologies or non-viable ones.
Memoirs of mothers who experienced the loss of a child from the forum of the charity fund "Light in Hands"): "The diagnosis was terrible, the doctors said that children with such pathologies are born dead or die in infancy. Realizing that losing a baby, a long-awaited daughter, after her birth would be simply fatal for me, I agreed to an abortion for medical reasons. To be honest, I still don’t understand if I did the right thing, and I blame myself that I went along with my relatives and doctors by agreeing to this abortion.”
“It's very hard to survive. Walk for 9 months and know that a child can die on the first or second day. What is more difficult: walking and knowing that it will be so, or terminating a pregnancy in the middle? Usually women agree with the opinion of doctors, but sometimes they still decide to leave the child, ”says Lyudmila Popova.
In general, most often, before the 22nd week, women agree and go for an abortion.
“This is not just an abortion at the request of a woman, this is a forced measure. Because then supporting the lives of these children is a colossal burden. It happens that mothers then refuse them, because they cannot cope, they give them to the Homes for the Disabled, and then the state takes care of these children, ”concluded Lyudmila Popova.
“After 22 weeks, this is already a full-fledged birth”
Until 2019, in the Krasnoyarsk Territory, pregnancy was not terminated at a later date (after 22 weeks of pregnancy) due to indications from the fetus (congenital malformations incompatible with life, which for some reason have not been previously identified). Women had only one way out - to give birth to a child with a pathology. And only at the end of 2018, the clinical protocol of the Ministry of Health of the Russian Federation "Artificial termination of pregnancy at a later date for medical reasons in the presence of fetal developmental anomalies" was approved, on the basis of which this medical technology was introduced in the Krasnoyarsk Regional Clinical Center for Maternal and Child Health.
The procedure for terminating a pregnancy at a later date is the same throughout Russia: an anesthetic is administered to the fetus in utero, after which the elimination (cardiac arrest) of the fetus is carried out, and labor is induced. The procedure is performed by an ultrasound doctor, an anesthesiologist, an anesthetist nurse and a laboratory assistant.
“Like any manipulation, the interruption procedure has certain risks associated with both the use of medications and the operation. Bleeding may develop, there may be negative consequences from drugs - side effects, allergies. Any intervention in a woman's body, even at the present stage of the development of medicine, is always a health risk that can lead to complete deprivation of reproductive function. Many couples decide to prolong the pregnancy, hoping for a miracle, for a diagnostic error, ”says Pavel Baurov, head of the advisory clinic at the Regional Clinical Center for Maternal and Childhood Welfare.

Head of the advisory polyclinic of the Regional Clinical Center for Maternal and Childhood Pavel Baurov
Women who refuse to terminate a pregnancy in case of medical indications, most often name their personal beliefs as the reasons, as well as their families. In the case when a decision is made to leave a non-viable child, the patient continues to be observed in the consultation.
How to survive the impossible
Late pregnancy termination is a severe psychological trauma. After the procedure itself, each woman is waiting for the rehabilitation process, a psychologist always works with her. Now there are such specialists at every antenatal clinic. A psychologist from the Center for Maternal and Childhood Welfare talks with a patient before and after the procedure.
“A woman in such a situation has a lot of difficult experiences. And one of the most difficult that appears at such moments is the feeling of guilt. Thoughts often arise in the mother’s head: “How could I allow this to be done?”, even if the situation is completely hopeless. The moment of choice also leaves an imprint - the woman still decides whether to terminate her pregnancy or keep it. Guilt, as a rule, is irrational, not corresponding to the real situation, ”the psychologist notes.
Thoughts often arise in the mother’s head: “How could I allow this to be done?”, even if the situation is completely hopeless. The moment of choice also leaves an imprint - the woman still decides whether to terminate her pregnancy or keep it. Guilt, as a rule, is irrational, not corresponding to the real situation, ”the psychologist notes.
Memories of mothers who have experienced the loss of a child (from the forum of the charitable foundation "Light in Hands"): “Two years have passed. And yes, we still gave birth to a child, a beautiful daughter. But there was not a day that I did not remember my first daughter. I wake up in the middle of the night and remember those days. I keep these memories as the only thing left of my child.”
Medical termination is exactly the same antenatal loss ( situation where the baby dies at during pregnancy — ed. ). A woman loses a baby for a long time, despite the fact that from the end of the first trimester she already perceives him as a person, interacts with him, communicates internally.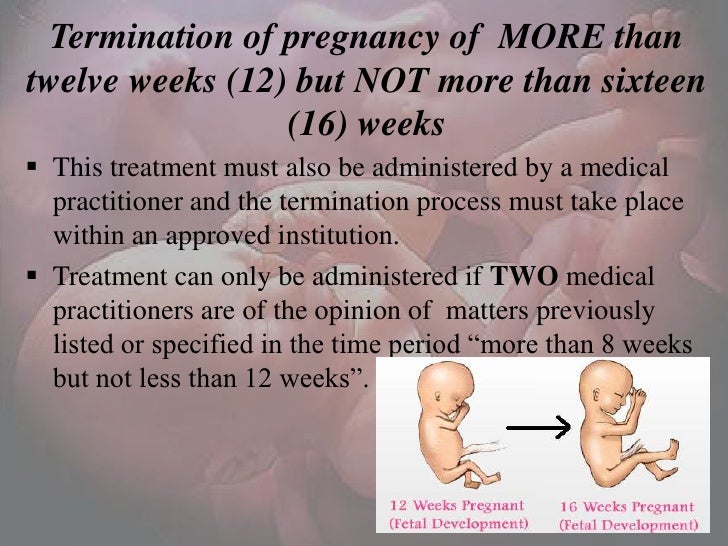
A psychologist has no influence on a woman's choice - such is the professional position. It helps to realize some things, provides psychological support. Sometimes the situation itself can be completely hopeless when a diagnosis of a pathology that is incompatible with life is made, but even this does not always affect the final choice of a couple. A psychologist helps to dispel any doubts, relieve tension and at least slightly alleviate the moment of suffering.
After the interruption, the woman goes through the process of mourning, as after any other loss. If adaptation is disrupted for too long and a person cannot live a full life, then psychologists talk about pathological mourning, which requires more serious treatment. It is very important that the environment of the woman also helps to survive the crisis.
“We, our society, unfortunately, no one taught empathy, and usually people feel discomfort next to those who have suffered a loss. As a rule, a woman's relatives think that the most important thing is that she stopped worrying about .This is where all these tips start: “stop crying”, “live on”, “get together”, and so on. But a woman doesn’t need this, she needs to live her grief, cry out her tears, she needs to speak out, ”says psychologist Svetlana Chursina.
Rehabilitation usually takes months, but even when a woman returned to normal life, this difficult moment will remain in her memory forever, it is impossible to erase it. From time to time, with tears, she will still remember her unborn baby.
Clinical psychologist of the Center for Maternal and Childhood Welfare Svetlana Chursina
Patients often ask the question: “What to do with the child? What will happen to him after I give birth to him?
“The doctor cannot insist, but still it is better if you look at the baby and say goodbye to him. It is better to keep some of his things related to pregnancy, ultrasound scans and so on. Firstly, the brain is arranged in such a way that until it sees it, it will not believe that this is final, therefore subconsciously it will not give you rest, there will always be doubts: “What if he were alive, but if he were healthy? “.Secondly, after some time, women who could not look at the child and say goodbye may regret it. Still, over time, this is perceived as the loss and death of a loved one, so you should not completely depersonalize the baby. But in any case, the choice is up to the woman herself. You can offer, but in no case insist,” advises Svetlana Chursina.
At the Center for Maternal and Child Health, a woman receives 1-2 consultations, after which the doctors recommend (if necessary) that she contact a psychologist at the antenatal clinic, or visit free support groups. In Russia, the charitable foundation "Light in Hands" works with mothers who have suffered perinatal loss. You can get advice and find out all the working conditions on the fund’s hotline.
Psychologists advise relatives, friends and colleagues to start from the desires of a woman - do not impose help, insist on talking if she does not want it. “Time heals” is one of the main principles of recovery, so the main thing is to give a woman this time.