Pregnancy safe lice treatment
Head Lice | InfantRisk Center
Pregnancy Breastfeeding
Head lice or Pediculus humanus capitis, attack as many as 12 million children every year. Lice are spread by direct contact with infested hair. Sharing combs, brushes, beds, and hats may also contribute to the spread of these parasites. Lice infestations in the U.S. are more frequent in girls and lead to stigma and absenteeism from school or day care.1, 2
The life cycle of a louse is divided into three stages. The female adult louse lays eggs (nits) that hatch after eight or nine days. The young louse (nymph) matures into adulthood within nine to twelve days. The adult louse usually lives about one month and feeds on human blood. Adult lice are usually tan to grey in color and two to three millimeters in length. Nits are usually yellow to white in color and are less than one millimeter in size. Lice typically die after one or two days without access to a blood meal. Lice do not appear to cause disease but subsequent bacterial infections may occur from scratching.
Signs and symptoms of head lice include tickling on the scalp, difficulty sleeping, and excessive scratching. Diagnosis can be difficult as a louse moves quickly and blends in with the hair shaft. Nits are typically found around 5 millimeters from the scalp during active infestations. All family members should be evaluated for lice if one child has an infestation.
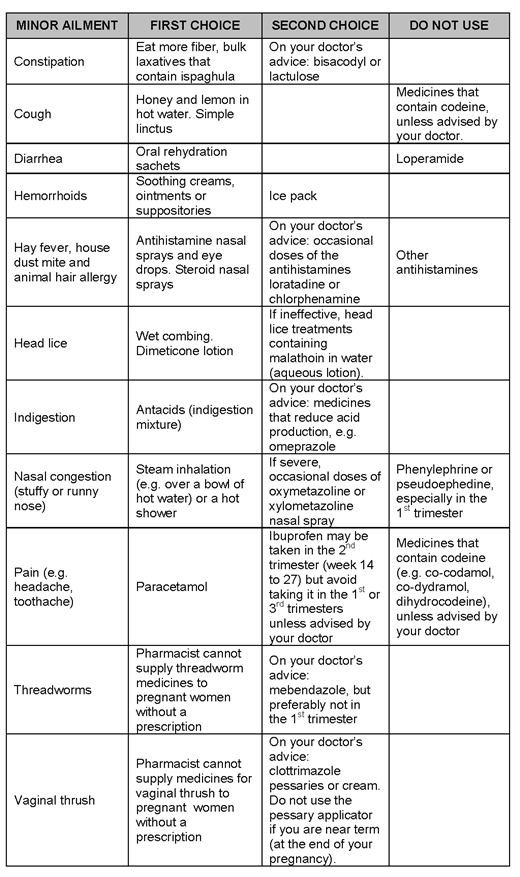
Head lice during pregnancy and breastfeeding can be treated with pediculicides including permethrin, malathion, and ivermectin. There are studies providing evidence that these agents do not increase the risk of birth defects.3-5 They are also unlikely to pass into the milk of breastfeeding mothers in clinically relevant amounts. Permethrin is preferred for breastfeeding and pregnant mothers because it is non-toxic, and there is minimal absorption through the skin (<2%).6 However, at least one additional treatment is usually required to completely treat the infestation.
Newly approved Sklice Lotion (0. 5% ivermectin) may be used in children who are six months and older. A recent study has suggested that a single topical application of ivermectin kills most of the lice.7 The researchers found that 94.9% of ivermectin treated patients were louse free one day after application and there was significant reduction in itching between day one and day two in the ivermectin group, as compared with the control group. The proportion of head louse free patients in the ivermectin group was 85.2% on day eight and 73.8% on day fifteen. The continued efficacy of treatment with topical ivermectin two weeks after a single treatment suggests that this formulation has activity against louse eggs. Another recent laboratory study has also suggested this. In this study, ivermectin was applied to head louse ova and, although the ova subsequently hatched, all the released nymphs quickly died. The nymphal mortality was attributed to ivermectin induced mouthpart paralysis, which severely limited or completely prevented the nymphs from feeding.
5% ivermectin) may be used in children who are six months and older. A recent study has suggested that a single topical application of ivermectin kills most of the lice.7 The researchers found that 94.9% of ivermectin treated patients were louse free one day after application and there was significant reduction in itching between day one and day two in the ivermectin group, as compared with the control group. The proportion of head louse free patients in the ivermectin group was 85.2% on day eight and 73.8% on day fifteen. The continued efficacy of treatment with topical ivermectin two weeks after a single treatment suggests that this formulation has activity against louse eggs. Another recent laboratory study has also suggested this. In this study, ivermectin was applied to head louse ova and, although the ova subsequently hatched, all the released nymphs quickly died. The nymphal mortality was attributed to ivermectin induced mouthpart paralysis, which severely limited or completely prevented the nymphs from feeding. 8
8
Regardless of what medication is used, if any, some careful infection-control measures are necessary to prevent re-infestation. Ova can hide under fingernails and toenails, so careful cleaning and treatment of those areas is important. Wash bedding, clothes, and hats in hot water, and with a hot air cycle in the dryer. Items that cannot be laundered may be dry cleaned or placed in sealed, plastic bags for two weeks to allow time for all lice life cycles to be completed. Vacuuming floors and furniture to remove infested hair is also recommended.
Each involved member of the household should also take time to wet comb their hair. This is a mechanical removal of lice via straining with a fine-toothed comb. Metal combs seem to be more effective than plastic for this purpose. To perform this maneuver, the hair should be wet with an added lubricant such as hair conditioner or olive oil. The hair should be brushed or combed to remove tangles. Insert the comb near the crown of the head until it touches the scalp gently. Draw it firmly down and examine the comb for lice after each stroke. The entire head should be combed systematically at least twice. Repeat the combing until no lice are found in each session.
Draw it firmly down and examine the comb for lice after each stroke. The entire head should be combed systematically at least twice. Repeat the combing until no lice are found in each session.
If no pediculicide is used, repeat sessions may be necessary every three to four days for several weeks. It is somewhat uncertain how effective wet combing is when used in place of topical insecticides. Existing studies have used flawed methodology and have produced contradictory results.
Sonia Shoukat, MD
Thomas W. Hale, Ph.D.
James Abbey, MD
References:
- Frankowski BL, Weiner LB, Committee on School Health the Committee on Infectious Diseases. American Academy of P. Head lice. Pediatrics. Sep 2002;110(3):638-643
- Gordon SC. Shared vulnerability: a theory of caring for children with persistent head lice. The Journal of school nursing : the official publication of the National Association of School Nurses.
 Oct 2007;23(5):283-292
Oct 2007;23(5):283-292 - Kennedy D, Hurst V, Konradsdottir E, Einarson A. Pregnancy outcome following exposure to permethrin and use of teratogen information. American journal of perinatology. Feb 2005;22(2):87-90
- Pacque M, Munoz B, Poetschke G, Foose J, Greene BM, Taylor HR. Pregnancy outcome after inadvertent ivermectin treatment during community-based distribution. Lancet. Dec 15 1990;336(8729):1486-1489
- Thomas DC, Petitti DB, Goldhaber M, Swan SH, Rappaport EB, Hertz-Picciotto I. Reproductive outcomes in relation to malathion spraying in the San Francisco Bay Area, 1981-1982. Epidemiology. Jan 1992;3(1):32-39
- Pharmaceutical manufacturer prescribing information. 2003
- Pariser DM, Meinking TL, Bell M, Ryan WG. Topical 0.5% ivermectin lotion for treatment of head lice. The New England journal of medicine. Nov 2012;367(18):1687-1693
- Strycharz JP, Berge NM, Alves AM, Clark JM. Ivermectin acts as a posteclosion nymphicide by reducing blood feeding of human head lice (Anoplura: Pediculidae) that hatched from treated eggs.
 Journal of medical entomology. Nov 2011;48(6):1174-118
Journal of medical entomology. Nov 2011;48(6):1174-118
Common Conditions
Safety of Topical Medications for Scabies and Lice in Pregnancy
1. Arya V, Molinaro MJ, Majewski SS, Schwartz RA. Pediatric scabies. Cutis. 2003;71:193–6. [PubMed] [Google Scholar]
2. Tajirian A, Schwartz R. Scabies and pediculosis: Biologic cycle and diagnosis. In: Micali G, editor. Videodermatoscopy in Clinical Practice. New York: Informa Healthcare; 2010. pp. 7–10. [Google Scholar]
3. Micali G, Lacarrubba F, Massimino D, Schwartz RA. Dermatoscopy: Alternative uses in daily clinical practice. J Am Acad Dermatol. 2011;64:1135–46. [PubMed] [Google Scholar]
4. Nutanson I, Steen C, Schwartz RA. Pediculosis corporis: An ancient itch. Acta Dermatovenerol Croat. 2007;15:33–8. [PubMed] [Google Scholar]
5. Nutanson I, Steen CJ, Schwartz RA, Janniger CK. Pediculus humanus capitis: An update. Acta Dermatovenerol Alp Pannonica Adriat. 2008;17:147–54. 156-7, 159. [PubMed] [Google Scholar]
6. Hall CM, Milligan DW, Berrington J. Probable adverse reaction to a pharmaceutical excipient. Arch Dis Child Fetal Neonatal Ed. 2004;89:F184. [PMC free article] [PubMed] [Google Scholar]
Hall CM, Milligan DW, Berrington J. Probable adverse reaction to a pharmaceutical excipient. Arch Dis Child Fetal Neonatal Ed. 2004;89:F184. [PMC free article] [PubMed] [Google Scholar]
7. Fölster-Holst R, Rufli T, Christophers E. Treatment of scabies with special consideration of the approach in infancy, pregnancy and while nursing. Hautarzt. 2000;51:7–13. [PubMed] [Google Scholar]
8. Mytton OT, McGready R, Lee SJ, Roberts CH, Ashley EA, Carrara VI, et al. Safety of benzyl benzoate lotion and permethrin in pregnancy: A retrospective matched cohort study. BJOG. 2007;114:582–7. [PubMed] [Google Scholar]
9. Mattison D. Clinical Pharmacology During Pregnancy. 1st ed. London, UK: Academic Press; 2012. [Google Scholar]
10. Schaefer C, Peters P, Miller R. Drugs During Pregnancy and Lactation. 3rd ed. London, UK: Academic Press; 2014. [Google Scholar]
11. Leuschner J. Reproductive toxicity studies of D-camphor in rats and rabbits. Arzneimittelforschung. 1997;47:124–8. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
12. Alakilli SY. Evaluation of camphor mutagenicity in somatic cells of pregnant rats. Asian J Biotechnol. 2009;1:111–7. [Google Scholar]
13. Weiss J, Catalano P. Camphorated oil intoxication during pregnancy. Pediatrics. 1973;52:713–4. [PubMed] [Google Scholar]
14. Heinonen O, Slone D, Shapiro S. Birth Defects and Drugs in Pregnancy: Maternal Drug Exposure and Congenital Malformations. Littleton, MA: Publishing Sciences Group; 1977. [Google Scholar]
15. Alsaad AM, Fox C, Koren G. Toxicology and teratology of the active ingredients of professional therapy MuscleCare products during pregnancy and lactation: A systematic review. BMC Complement Altern Med. 2015;15:40. [PMC free article] [PubMed] [Google Scholar]
16. Roth MM. Pregnancy dermatoses: Diagnosis, management, and controversies. Am J Clin Dermatol. 2011;12:25–41. [PubMed] [Google Scholar]
17. Briggs G. Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014. [Google Scholar]
10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014. [Google Scholar]
18. Chi CC, Wang SH, Wojnarowska F, Kirtschig G, Davies E, Bennett C. Safety of topical corticosteroids in pregnancy. Cochrane Database Syst Rev. 2015;10:CD007346. [PMC free article] [PubMed] [Google Scholar]
19. Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54:1–15. [PubMed] [Google Scholar]
20. Alabdulrazzaq F, Koren G. Topical corticosteroid use during pregnancy. Can Fam Physician. 2012;58:643–4. [PMC free article] [PubMed] [Google Scholar]
21. Chi CC, Kirtschig G, Aberer W, Gabbud JP, Lipozencic J, Kárpáti S, et al. Evidence-based (S3) guideline on topical corticosteroids in pregnancy. Br J Dermatol. 2011;165:943–52. [PubMed] [Google Scholar]
22. Schuster O, Menke G, Czichowsky H, Loew D. Pharmacokinetics of crotamiton following topical application to healthy male volunteers. J Dermatolog Treat. 1992;3:57–60. [Google Scholar]
[Google Scholar]
23. Wolverton SE. Comprehensive Dermatologic Drug Therapy. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012. [Google Scholar]
24. Diamantis SA, Morrell DS, Burkhart CN. Treatment of head lice. Dermatol Ther. 2009;22:273–8. [PubMed] [Google Scholar]
25. Murase JE, Heller MM, Butler DC. Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. J Am Acad Dermatol. 2014;70:401.e1–14. [PubMed] [Google Scholar]
26. Hay RJ, Steer AC, Engelman D, Walton S. Scabies in the developing world – Its prevalence, complications, and management. Clin Microbiol Infect. 2012;18:313–23. [PubMed] [Google Scholar]
27. DPT Laboratories. Sklice package insert. 2012. [Last accessed on 2016 Mar 05]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202736s000lbl.pdf .
28. Pacqué M, Muñoz B, Poetschke G, Foose J, Greene BM, Taylor HR. Pregnancy outcome after inadvertent ivermectin treatment during community-based distribution.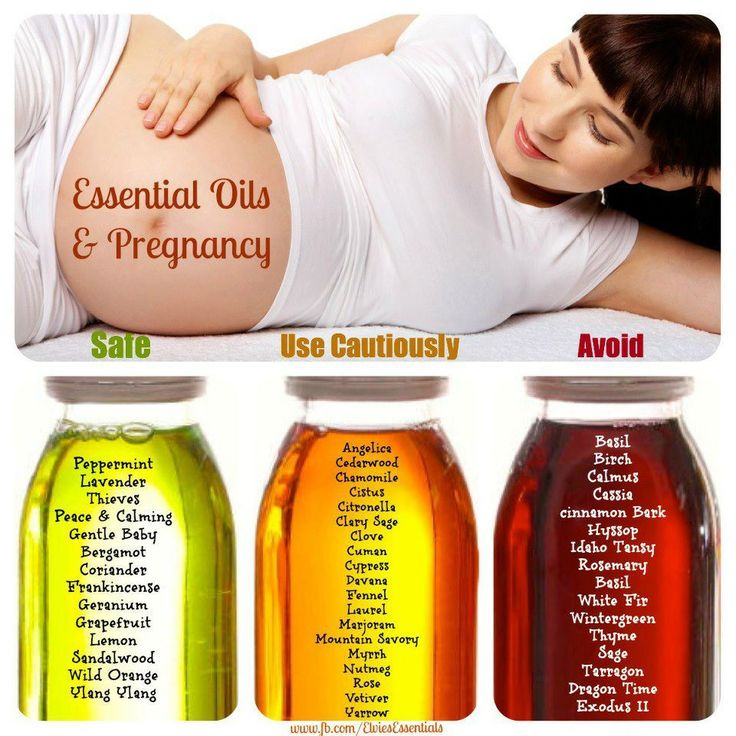 Lancet. 1990;336:1486–9. [PubMed] [Google Scholar]
Lancet. 1990;336:1486–9. [PubMed] [Google Scholar]
29. Chippaux JP, Gardon-Wendel N, Gardon J, Ernould JC. Absence of any adverse effect of inadvertent ivermectin treatment during pregnancy. Trans R Soc Trop Med Hyg. 1993;87:318. [PubMed] [Google Scholar]
30. Leachman SA, Reed BR. The use of dermatologic drugs in pregnancy and lactation. Dermatol Clin. 2006;24:167–97, vi. [PubMed] [Google Scholar]
31. Dourmishev AL, Dourmishev LA, Schwartz RA. Ivermectin: Pharmacology and application in dermatology. Int J Dermatol. 2005;44:981–8. [PubMed] [Google Scholar]
32. Morton Grove Pharmaceuticals. Lindane package insert. 2007. [Last accessed on 2015 Feb 26]. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=770415b2-4555-4abc-b5d6-c67dfb07ab30 .
33. Sircar S, Lahiri P. Lindane (gamma-HCH) causes reproductive failure and fetotoxicity in mice. Toxicology. 1989;59:171–7. [PubMed] [Google Scholar]
34. Palmer AK, Bottomley AM, Worden AN, Frohberg H, Bauer A. Effect of lindane on pregnancy in the rabbit and rat. Toxicology. 1978;9:239–47. [PubMed] [Google Scholar]
Effect of lindane on pregnancy in the rabbit and rat. Toxicology. 1978;9:239–47. [PubMed] [Google Scholar]
35. Palmer AK, Cozens DD, Spicer EJ, Worden AN. Effects of lindane upon reproductive function in a 3-generation study in rats. Toxicology. 1978;10:45–54. [PubMed] [Google Scholar]
36. FDA. Lindane Assessment Memorandum. 2003. [Last accessed on 2016 Feb 26]. Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM110853 .
37. Tyler KH. Dermatologic therapy in pregnancy. Clin Obstet Gynecol. 2015;58:112–8. [PubMed] [Google Scholar]
38. Taro Pharmaceuticals. Ovide package insert. 2011. [Last accessed on 2016 Feb 26]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018613s017lbl.pdf .
39. Grether JK, Harris JA, Neutra R, Kizer KW. Exposure to aerial malathion application and the occurrence of congenital anomalies and low birthweight. Am J Public Health. 1987;77:1009–10. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
40. Thomas D, Goldhaber M, Petitti D, Swan S, Rappaport E, Hertzpicciotto I. Reproductive outcomes in women exposed to malathion. Am J Epidemiol. 1990;132:794–5. [Google Scholar]
41. Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell NP, Barr DB, et al. Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect. 2004;112:1116–24. [PMC free article] [PubMed] [Google Scholar]
42. Eskenazi B, Marks AR, Bradman A, Harley K, Barr DB, Johnson C, et al. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect. 2007;115:792–8. [PMC free article] [PubMed] [Google Scholar]
43. Nash B. Extracts from “Best Treatments”: Treating head lice. Br Med J. 2003;326:1256. [PMC free article] [PubMed] [Google Scholar]
44. Lee A, Inch S, Finnigan D. Therapeutics in Pregnancy and Lactation. Abingdon, OX: Radcliffe Medical Press; 2000. [Google Scholar]
Abingdon, OX: Radcliffe Medical Press; 2000. [Google Scholar]
45. Rubin PC, Ramsey M. Prescribing in Pregnancy. Oxford, UK: Wiley; 2008. [Google Scholar]
46. Connolly M. Recommended management of head lice and scabies. Prescriber. 2013;24:17–29. [Google Scholar]
47. Rungsiprakarn P, Laopaiboon M, Sangkomkamhang US, Lumbiganon P. Pharmacological interventions for generalised itching (not caused by systemic disease or skin lesions) in pregnancy. Cochrane Database Syst Rev. 2016;2:CD011351. [PMC free article] [PubMed] [Google Scholar]
48. Perrigo Pharmaceuticals. Permethrin package insert. 2015. [Last accessed on 2016 Mar 05]. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=bdb796aa-a7d1-4476-988f-2b4a9519788f .
49. Kennedy D, Hurst V, Konradsdottir E, Einarson A. Pregnancy outcome following exposure to permethrin and use of teratogen information. Am J Perinatol. 2005;22:87–90. [PubMed] [Google Scholar]
50. Hengge UR, Currie BJ, Jäger G, Lupi O, Schwartz RA. Scabies: A ubiquitous neglected skin disease. Lancet Infect Dis. 2006;6:769–79. [PubMed] [Google Scholar]
Scabies: A ubiquitous neglected skin disease. Lancet Infect Dis. 2006;6:769–79. [PubMed] [Google Scholar]
51. Wozniacka A, Hawro T, Schwartz RA. Bullous scabies: A diagnostic challenge. Cutis. 2008;82:350–2. [PubMed] [Google Scholar]
52. Lin AN, Reimer RJ, Carter DM. Sulfur revisited. J Am Acad Dermatol. 1988;18:553–8. [PubMed] [Google Scholar]
53. Karthikeyan K. Treatment of scabies: Newer perspectives. Postgrad Med J. 2005;81:7–11. [PMC free article] [PubMed] [Google Scholar]
54. Díaz M, Cazorla D, Acosta M. Efficacy, safety and acceptability of precipitated sulphur petrolatum for topical treatment of scabies at the city of Coro, Falcon State, Venezuela. Rev Invest Clin. 2004;56:615–22. [PubMed] [Google Scholar]
55. Parapro LLC. Natroba package insert. 2014. [Last accessed on 2016 Mar 05]. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=fa90ccc8-2df0-49f7-8878-2b33e34cd272 .
56. Cole SW, Lundquist LM. Spinosad for treatment of head lice infestation. Ann Pharmacother. 2011;45:954–9. [PubMed] [Google Scholar]
Ann Pharmacother. 2011;45:954–9. [PubMed] [Google Scholar]
Treatment of head lice during pregnancy
As you know, pregnancy is not a diagnosis, but a temporary state of a woman, during which she enjoys future motherhood. But sometimes, the mood can be overshadowed by an annoying nuisance - pediculosis. Exactly. Unfortunately, pregnancy does not protect the expectant mother from parasites. And therefore, she, like many other people, can become infected with them.
But unlike ordinary people, pregnant women have to deal with lice in a slightly different way.
How to cure pediculosis in a pregnant woman
It is a well-known fact that during pregnancy the treatment of pediculosis is hampered by the fact that it is impossible to use certain drugs, since their chemical composition can harm not only parasites, but also the woman herself and her fetus. Therefore, in this case, you need to show maximum patience, and try to start the fight mechanically.
Mechanical lice removal
To do this, you can use a special fine-toothed comb with a white cloth. Carefully combing out the parasites, they must be destroyed immediately in order to prevent any attempts to escape. However, getting rid of nits is not so easy. They are too tenacious and hold well on the roots of the hair. To destroy them, you can use special irons to straighten your hair. Warming them up to a certain temperature, strand by strand should be carried out from the very roots to the very tips. True, this can harm the already weakened hair of a pregnant woman. Therefore, if you do not want to take risks, use some folk methods.
Carefully combing out the parasites, they must be destroyed immediately in order to prevent any attempts to escape. However, getting rid of nits is not so easy. They are too tenacious and hold well on the roots of the hair. To destroy them, you can use special irons to straighten your hair. Warming them up to a certain temperature, strand by strand should be carried out from the very roots to the very tips. True, this can harm the already weakened hair of a pregnant woman. Therefore, if you do not want to take risks, use some folk methods.
Folk therapy for head lice
In order to get rid of lice during pregnancy, you can use safe remedies for head lice, which were used by our mothers and grandmothers. The list of these preparations consists of:
- apple cider vinegar;
- cranberry juice;
- decoction of wormwood;
- parsley juice;
- tar and dust;
- also, olive or butter.
However, here, as in the previous version, in order to * cure pediculosis * you will have to try hard, showing stamina and endurance. Why? Because no matter which of the above options you choose, you will have to repeat the manipulations at least three times. But on the other hand, neither you nor the child can be harmed by such treatment in any way.
Why? Because no matter which of the above options you choose, you will have to repeat the manipulations at least three times. But on the other hand, neither you nor the child can be harmed by such treatment in any way.
Another thing is when all efforts go down the drain. In this case, you will have to discard all stereotypes and boldly go to the nearest pharmacy.
Medical treatment of lice in pregnant women
If no previously tried methods could save you from unwanted parasites, you have no choice but to buy a modern remedy for lice, which will surely help you forget about this trouble. This may be a drug such as: Permethrin or Melatinone. Both of them are very effective, safe, and most importantly, enjoy a good reputation and great popularity.
Creative treatment for head lice during pregnancy
Contrary to the fact that there is a belief that during the period when a woman is in an "interesting position" she can neither dye nor cut her hair, many people forget about these ancient traditions. And regarding such a problem as lice, this solution becomes a lifeline.
And regarding such a problem as lice, this solution becomes a lifeline.
The most ordinary hair dye will help not only to remove parasites once and for all, but also improve hair color!
Comments
folk methods and mechanical methods
During the period of expectation of a child, the female body becomes especially susceptible to various pathologies, including the penetration of parasites.
Pediculosis is a serious problem for the mother-to-be, since most medicines are not allowed to be used. And then the question of what and how to get rid of lice and nits during pregnancy becomes especially relevant.
Lice in pregnant women
How to remove lice from a pregnant woman without harm to her health is a rather complicated problem, but it can be solved. After all, lice cause concern both from a physical point of view and from a moral one, and when it comes to pregnancy, then everything is much more complicated.
Women in this period are suspicious and vulnerable, and such problems usually cause them a feeling of fear for the future baby, as well as a feeling of embarrassment and inconvenience. What to do if a pregnant woman has lice, you need to know in order to quickly and safely eliminate them. To do this, you can use some herbal preparations, mechanical means, as well as methods from traditional medicine.
What to do if a pregnant woman has lice, you need to know in order to quickly and safely eliminate them. To do this, you can use some herbal preparations, mechanical means, as well as methods from traditional medicine.
Article contents
- Sources of infection
- Danger of pediculosis during pregnancy
- What means can be used from parasites during pregnancy
- Medicines for lice
- Mechanicals
- Tips for the choice of a comb
- Folk Methods
- Conclusion
Pedical disease among children attending kindergartens and schools. Therefore, if a pregnant woman has an older child of this age, then you should check for the presence of parasites in him, and also notify educators or teachers about the problem in the team, if such an assumption is confirmed.
Lice
Other possible sources of infection:
- Public transport.
- Polyclinic.
- Hairdresser.

- Swimming pool, etc.
Attention! Infection with lice is possible only through close contact with the carrier of these parasites, or when using his personal belongings, such as a comb, towel, clothing, etc.
Read also: Lice in children: the main causes pregnancy
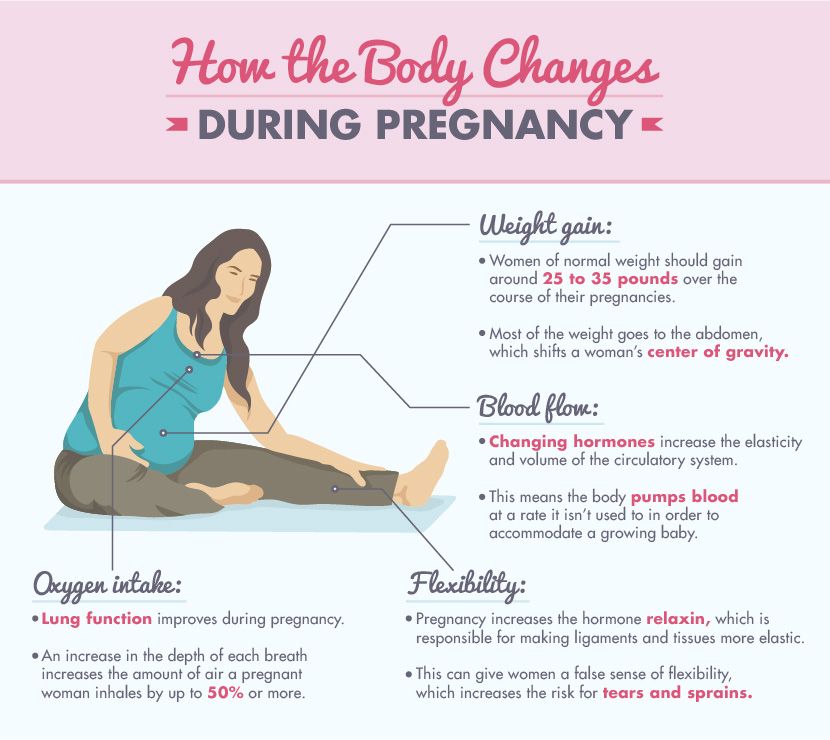
The presence of lice on the head causes intense itching, which makes the expectant mother very nervous and irritable. This negatively affects her well-being, disrupts normal sleep and appetite.
Such stressful situations are contraindicated for pregnant women. Moreover, discomfort arises not only in the physical sense, but also in the psychological one, the very fact of the presence of insects in the hair causes a lot of negative emotions.
Risk of head lice during pregnancy
Another problem is the intensive scratching of the scalp until the appearance of wounds and damage through which infection can enter the body and develop inflammatory processes.
Therefore, it is important to keep your hands clean, cut your nails short and try not to scratch your head, and also find out exactly how you can treat head lice in a pregnant woman, which remedy is the safest and most effective.
Which remedies can be used against parasites during pregnancy
Most medicines for head lice during pregnancy are contraindicated due to high toxicity, pungent odor, harmful substances that can penetrate the mother's body and, accordingly, the child through the placenta. Therefore, it is important to decide what exactly can be used to treat pediculosis in pregnant women so as not to harm health.
To do this, you can consult a doctor, try to comb out insects with a comb, or use traditional methods. However, among the drugs there are effective herbal remedies that are acceptable for use in women in an interesting position. Before using them, you should carefully read the instructions to make sure that there are no contraindications.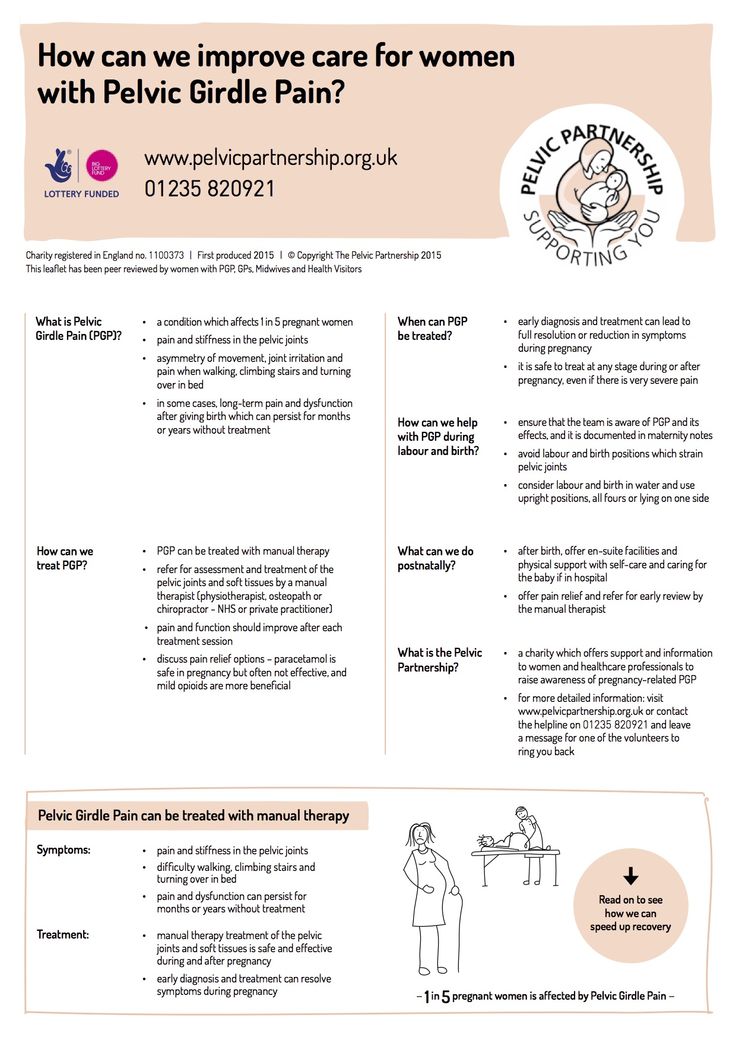
So, how to get rid of lice in a pregnant woman? There are three main ways:
- Medicinal - safe drugs;
- Mechanical - combing out parasites with a special comb;
- Folk - with the help of improvised means.
Medicines for lice
Conventional medicines for nits and lice are contraindicated in pregnant women due to the concentration of active substances in them that have a toxic effect on the body. There are other drugs without the content of such components:
- Delacet.
- Nyx cream.
- Shampoo Pedilin.
- Nittifor solution.
- Medifox solution.
- Nude Spray.
- Shampoo Paranit.
- Oil preparation D-95.
Delacet
Important! You can not use these drugs for pregnant women without the recommendation of a doctor, since there are no medicines that are absolutely safe for health.

Mechanical
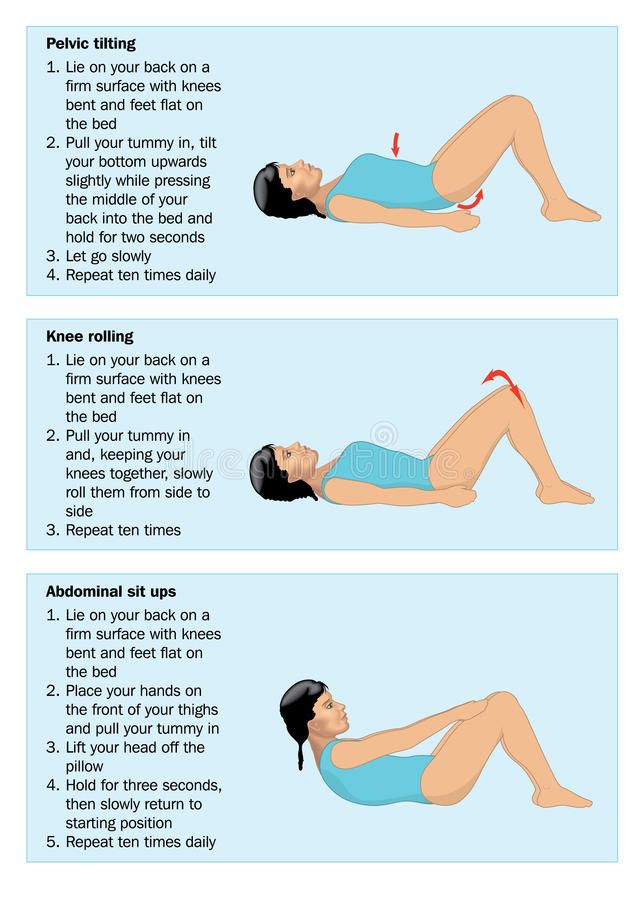
The most harmless remedy for lice for pregnant women is the mechanical combing of parasites and their eggs with a special fine comb.
The procedure is carried out in stages:
- Thoroughly wash your hair with shampoo, normal or anti-lice. If the hair is long, then it is advisable to cut it shorter.
- Apply any vegetable oil to the hair to facilitate glide and simplify the procedure.
- Tilt your head forward and begin to carefully comb the curls from the roots. In the process, you need to periodically rinse the comb to eliminate dead insects.
After combing, rinse your hair again with shampoo, after which you can rinse your hair with water acidified with vinegar. This procedure should be carried out daily to shorten the treatment time.
The main advantage of mechanical elimination of parasites is the ability to remove not only adults, but also nits that are firmly attached to the hair and are resistant to many drugs.
Comb Selection Tips
Many people prefer using the comb as the safest, chemical-free maternity lice and nit remedy. The comb for combing out insects should be frequent, with special notches on the teeth made of medical steel. The name of the most popular head parasite comb is Antive.
RobiComb electronic comb for lice and nits
There are also more modern devices, such as the RobiComb electric comb, which is distinguished by the presence of a special detector for finding insects. When using it, when a louse gets into the teeth of the device, it starts to emit intermittent signals. Robocomb is very convenient for preventive checks, as well as for follow-up checks after head lice treatment.
Traditional methods
Treatment of lice in a pregnant woman is desirable to carry out folk methods in combination with mechanical combing. But it must be borne in mind that not all means can be used by expectant mothers. For example, hellebore water against lice, kerosene is contraindicated.
But it must be borne in mind that not all means can be used by expectant mothers. For example, hellebore water against lice, kerosene is contraindicated.
The most effective recipes:
- Treat the head with freshly squeezed cranberry juice, rub it thoroughly into the roots, spread over the entire length of the hair, put on a plastic cap. You can wash it off after a few hours, then comb out the immobile parasites with a comb.
- Soak hair with apple cider vinegar or grape vinegar, minding the scalp, then put on a polyethylene cap. Wash off after 3-3.5 hours.
- Periodically wash your hair not with shampoo, but with laundry or tar soap.
- Pass the onion head through a meat grinder, mix with vegetable oil and apply this mixture on the head, wrap with polyethylene. After an hour, you can wash off and get rid of dead insects.
- Lighten or simply recolor your hair.
- Take a little olive oil, add a few drops of lavender, geranium and tea tree essential oils to it, then carefully treat the entire head and hair with the resulting composition, paying special attention to the area behind the ears, the back of the head and temples.

- Prepare a decoction of bitter wormwood, apply it to the hair and scalp for one hour.
- Pour boiling water over burdock leaves, cool, mix with essential oils (geranium, lavender) and apply to hair, put on a plastic cap. Wash off after 1.5 hours.
- Spray head with hydrogen peroxide diluted with water.
- Every day, style your hair with a flat iron. Insects are killed by exposure to high temperatures.
- Rub parsley juice on the scalp.
- Prepare a decoction of wild rosemary with the addition of bitter wormwood, treat the entire scalp and wrap it with plastic wrap. Wash off after 2 hours.
- Apply Vaseline to your hair, put on a cap and go to bed. In the morning, wash your hair and remove dead insects.
- Wash hair with dust soap.
- Bring pomegranate juice with mint leaves to a boil, treat skin and hair.
- Pass a few lemons through a meat grinder, pour boiling water, cool and rub into the scalp, distribute through the hair.