Molar pregnancy awareness
Molar pregnancy - Better Health Channel
The term gestational trophoblastic disease (GTD) covers several pregnancy conditions that involve the placental tissue turning cancer-like, or cancers originating from placental tissue. In Australia, this condition occurs in one in every 600 to 1000 pregnancies.
The main types of GTD are hydatidiform mole (also known as molar pregnancy; this is the most common form) and gestational trophoblastic neoplasia (also known as persistent gestational trophoblastic disease or persistent GTD).
Molar pregnancy is a form of abnormal pregnancy, in which the formed placental-like tissue sometimes invades the wall of the uterus. In most cases, the woman miscarries and passes the mole from her body, or it is removed with a surgical procedure called a dilatation and curettage (D&C). This procedure is also known as an evacuation of the uterus.
If treated early, molar pregnancy is 100 per cent curable.
The cause of molar pregnancy is unknown, but a key risk factor is maternal age. Women aged less than 20 years or more than 40 years are most at risk.
Symptoms of molar pregnancy
The symptoms of molar pregnancy can include:
- vaginal bleeding during early pregnancy
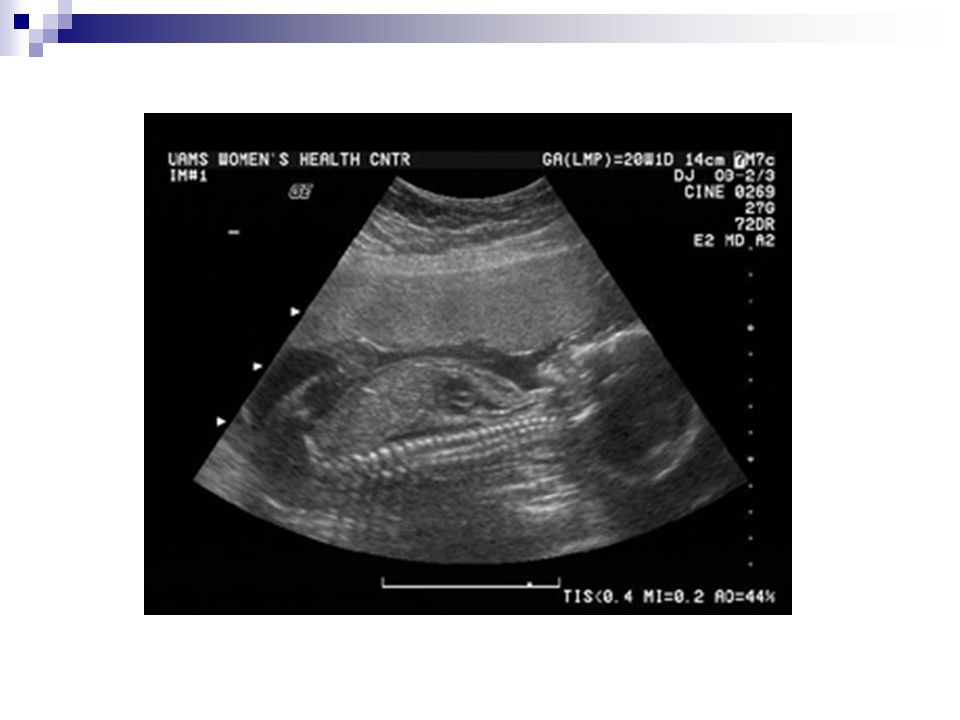
- abnormal appearance of the uterine cavity at the first ultrasound (called a ‘snowstorm’ pattern).
More rarely, when a diagnosis is not made until later gestation, symptoms include:
- a uterus larger than expected
- no foetal movement
- no foetal heartbeat
- extremely severe morning sickness
- high blood pressure (hypertension) – early onset of gestational hypertensive diseases.
Risk factors for molar pregnancy
The cause of molar pregnancy is unknown, but risk factors include:
- maternal age of less than 20 or more than 40 years
- race – Asian women are at increased risk
- dietary deficiencies including lack of folate, beta-carotene or protein
- prior history of gestational trophoblastic disease – the recurrence rate is one in 100.

Formation of a molar pregnancy
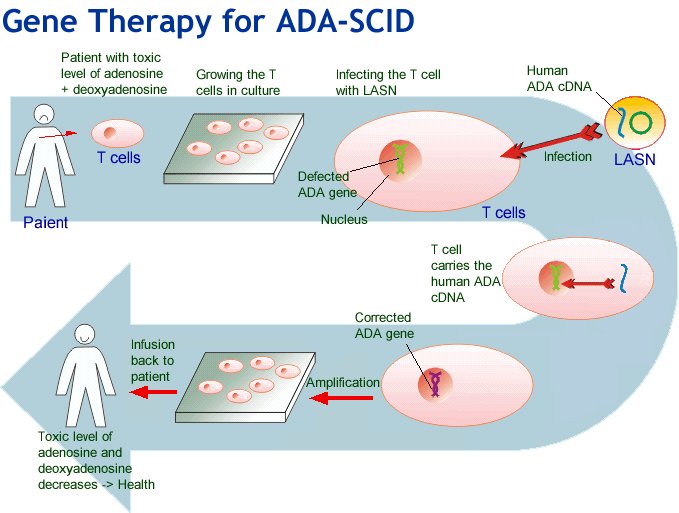
After fertilisation, developing cells split into two broad groups – one group becomes the fetus and the other becomes the placenta. The placenta has millions of tiny finger-like projections (villi) that are designed to ‘dig in’ to the womb wall and tap into the mother’s blood supply.
There are two forms of molar pregnancy – complete mole and partial mole. In complete molar pregnancies, there is no foetus, and the placenta grows abnormally. The villi swell and look like little blisters. These blisters are called a hydatidiform mole.
In partial molar pregnancies there is some development of the fetus but it is not normal and cannot survive.
When a woman has a molar pregnancy she experiences the symptoms of pregnancy because the placenta continues to make the pregnancy hormone human chorionic gonadotrophin (hCG). However, the level of hCG is usually higher than normal, which explains why morning sickness can be sometimes more severe than usual.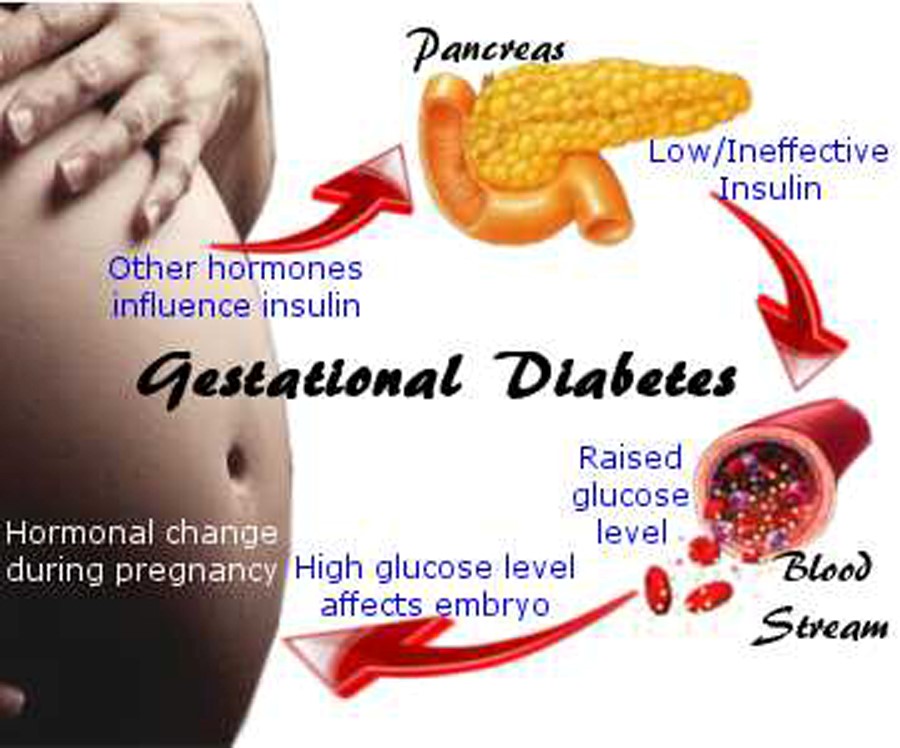 In some cases, the morning sickness is so severe that hospitalisation is needed.
In some cases, the morning sickness is so severe that hospitalisation is needed.
Complications of molar pregnancy
Molar pregnancy is usually diagnosed early with minimal symptoms, but if diagnosis is delayed the following complications can arise:
- haemorrhage
- ovarian cysts
- breathlessness (when it spreads to the lungs)
- pre-eclampsia (toxaemia of pregnancy), involving high levels of certain substances in the blood that raise blood pressure and affect the kidneys and (sometimes) liver function
- excess thyroid hormone production, which causes heart palpitations and other thyroid hormone effects.
If a molar pregnancy is not treated or does not miscarry completely it can progress and cause a range of serious conditions (known as gestational trophoblastic neoplasia), including:
- persistent GTD – persistent growth of the abnormal placental tissue
- invasive mole – the tumour spreads into the wall of the uterus
- metastatic mole – molar cells migrate to other organs of the body and cause secondary tumours.
 The lungs are common sites for metastatic moles
The lungs are common sites for metastatic moles - gestational choriocarcinoma – a rapidly spreading type of cancer that can travel to any part of the body via the blood vessels or lymphatic system.
Diagnosis of molar pregnancy
Molar pregnancy is diagnosed using:
- Medical history, which could include current pregnancy or recent childbirth, miscarriage or abortion
- physical examination
- blood test to check for high levels of the pregnancy hormone hCG
- ultrasound (the most common imaging tool used)
- other scans including x-rays, computed tomography (CT) or magnetic resonance imaging (MRI) if it is thought the cancer may have spread to other areas of the body.
Molar pregnancy can be hard to diagnose because:
- A woman who experiences a miscarriage will not know whether or not she passed a hydatidiform mole unless the aborted tissue is examined in a laboratory.
- If recent pregnancy, labour and birth were normal, there is often no reason to suspect molar pregnancy until symptoms become apparent.

Treatment of molar pregnancy
Promptly treated, molar pregnancies are curable in 100 per cent of cases. Treatment options depend on various factors, including whether or not the tumour has spread to other areas of the body, but could include:
- dilatation and curettage (D&C) – the cervix is gently opened and the uterine contents are removed (evacuated)
- hysterectomy – if a woman doesn’t want any more children, the surgical removal of her uterus may be recommended.
Further treatment is required in 10 per cent of all cases.
Molar pregnancy can persist (continue) after an evacuation procedure. There is a 15 to 25 percent chance of a complete mole persisting, and a 0.5 to 4 per cent chance of a partial mole persisting, so regular monitoring of your hCG levels is required.
The primary test is a blood test for hCG, but sometimes the 24-hour collection of urine can be used to measure hCG levels.
If the hCG level does not fall or continues to rise, or if further tests such as x-rays and scans show that spread has occurred and you are diagnosed with persistent GTD, you will need chemotherapy.
It is important to strictly avoid pregnancy until your hCG level has returned to normal, because a normal pregnancy will produce hCG and make the monitoring blood tests ineffective.
If you need chemotherapy, avoid becoming pregnant for the first year after completion of the treatment so that your hCG blood tests are effective, and to avoid harm to your developing baby.
In Victoria, all women with a hydatidiform mole pregnancy are registered on the Royal Women’s Hospital’s Gestational Trophoblastic Disease Registry. Follow-up is monitored and support is available for women with this diagnosis.
Queensland also has a state registry but in other states in Australia, care is usually provided by a specialist gynaecologist.
Where to get help
- Your GP (doctor)
- Gestational Trophoblastic Disease Registry, Royal Women’s Hospital Tel. (03) 8345 2620
- Women’s health clinic
- Sexual Health Victoria (SHV). To book an appointment call SHV Melbourne CBD Clinic: (03) 9660 4700 or call SHV Box Hill Clinic: (03) 9257 0100 or (free call): 1800 013 952.
 These services are youth friendly.
These services are youth friendly. - Cancer Council Victoria Tel. 13 11 20
Molar pregnancy - Symptoms and causes
Overview
A molar pregnancy is a rare complication of pregnancy. It involves unusual growth of cells called trophoblasts. These cells typically become the organ that feeds a growing fetus. That organ also is known as the placenta.
There are two types of molar pregnancy — complete molar pregnancy and partial molar pregnancy. In a complete molar pregnancy, the placental tissue swells and appears to form fluid-filled cysts. There is no fetus.
In a partial molar pregnancy, the placenta might have both regular and irregular tissue. There may be a fetus, but the fetus can't survive. The fetus usually is miscarried early in the pregnancy.
A molar pregnancy can have serious complications, including a rare form of cancer. A molar pregnancy requires early treatment.
Products & Services
- Book: Your Guide to Miscarriage and Pregnancy Loss
Symptoms
Molar pregnancy
Molar pregnancy
During a molar pregnancy, the placenta doesn't form typically.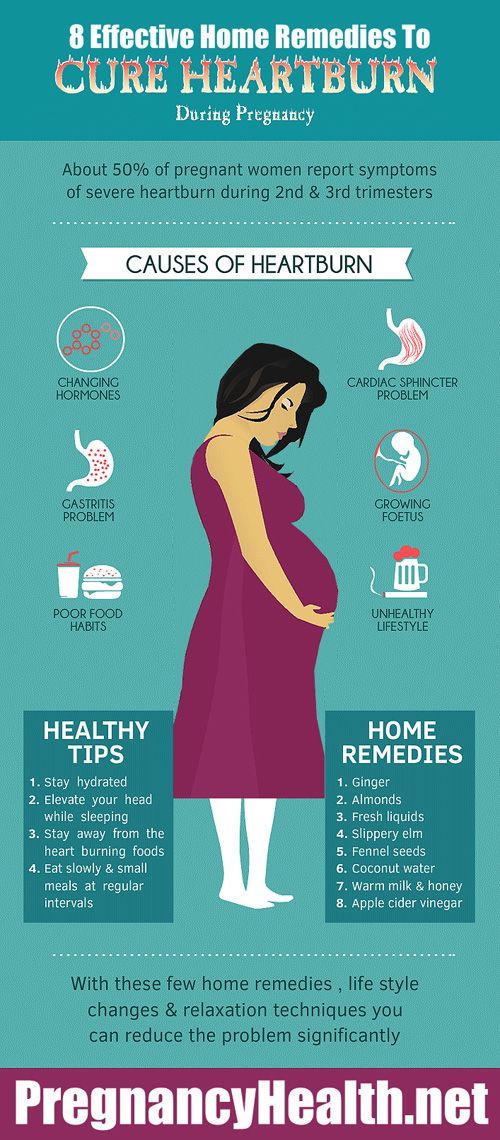 It can look like a mass of cysts. The fetus either doesn't form or doesn't form regularly and can't survive.
It can look like a mass of cysts. The fetus either doesn't form or doesn't form regularly and can't survive.
A molar pregnancy may seem like a regular pregnancy at first. But most molar pregnancies cause symptoms that can include:
- Dark brown to bright red bleeding from the vagina during the first three months
- Severe nausea and vomiting
- Sometimes grapelike cysts that pass from the vagina
- Pelvic pressure or pain
Because of improved ways of detecting a molar pregnancy, most are found in the first trimester. If it is not found in the first three months, symptoms of a molar pregnancy might include:
- A uterus growing quickly and being too large early in the pregnancy
- Preeclampsia — a condition that causes high blood pressure and protein in the urine — before 20 weeks of pregnancy
- Ovarian cysts
- Overactive thyroid, also known as hyperthyroidism
Request an Appointment at Mayo Clinic
Causes
An egg fertilized atypically causes a molar pregnancy. Human cells usually have 23 pairs of chromosomes. In a typical fertilization, one chromosome in each pair comes from the father, the other from the mother.
Human cells usually have 23 pairs of chromosomes. In a typical fertilization, one chromosome in each pair comes from the father, the other from the mother.
In a complete molar pregnancy, one or two sperm fertilize an egg. The chromosomes from the mother's egg are missing or don't work. The father's chromosomes are copied. There's none from the mother.
In a partial or incomplete molar pregnancy, the mother's chromosomes are present, but the father supplies two sets of chromosomes. The embryo then has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father's genes.
Risk factors
Factors that can contribute to a molar pregnancy include:
- Earlier molar pregnancy. If you've had one molar pregnancy, you're more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 people.
- Age of the mother. A molar pregnancy is more likely in people older than age 43 or younger than age 15.

Complications
After removing a molar pregnancy, molar tissue might remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). GTN happens more often in complete molar pregnancies than it does in partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, the mole that causes the molar pregnancy goes deep into the middle layer of the uterine wall. This causes bleeding from the vagina.
Persistent GTN is usually treated with chemotherapy. Another treatment possibility is removal of the uterus, also known as hysterectomy.
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs.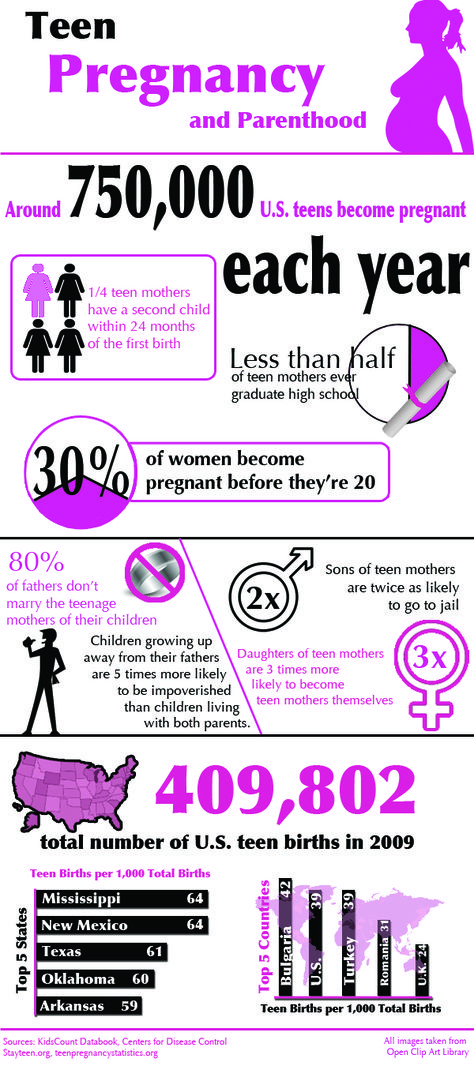 Choriocarcinoma is usually successfully treated with chemotherapy. A complete molar pregnancy is more likely to have this complication than is a partial molar pregnancy.
Choriocarcinoma is usually successfully treated with chemotherapy. A complete molar pregnancy is more likely to have this complication than is a partial molar pregnancy.
Prevention
If you've had a molar pregnancy, talk to your pregnancy care provider before trying to get pregnant again. You might want to wait six months to one year. The risk of having another molar pregnancy is low, but it's higher once you've had a molar pregnancy.
During future pregnancies, a care provider may do early ultrasounds to check your condition and make sure the baby is developing.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
How to diagnose a molar pregnancy - advice from an obstetrician
Quick navigation
Molar pregnancy (molar pregnancy) is a rare complication of pregnancy and a type of gestational trophoblastic disease, when the fertilization of an egg by a sperm cell occurs incorrectly and creates abnormal cells inside the uterus . This pathology is rare, and according to statistics, for every 590 pregnancies, there is about 1 case of a molar pregnancy. Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist.
This pathology is rare, and according to statistics, for every 590 pregnancies, there is about 1 case of a molar pregnancy. Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist.
Causes
Molar pregnancy is caused by an imbalance in the genetic material (chromosomes) during pregnancy. This usually occurs when an egg that contains no genetic information is fertilized by a sperm (complete molar pregnancy) or when a normal egg is fertilized by two sperm (partial molar pregnancy).
Mole risk factors
All pregnant women have a risk of developing a molar pregnancy, but this risk is very small.
Age. Researchers have found that certain types of molar pregnancies are more common in certain age groups. Complete molar pregnancies are more common in mothers over 45 years of age. The risk is moderately increased in young adolescents. Age does not affect the risk of partial molar pregnancies.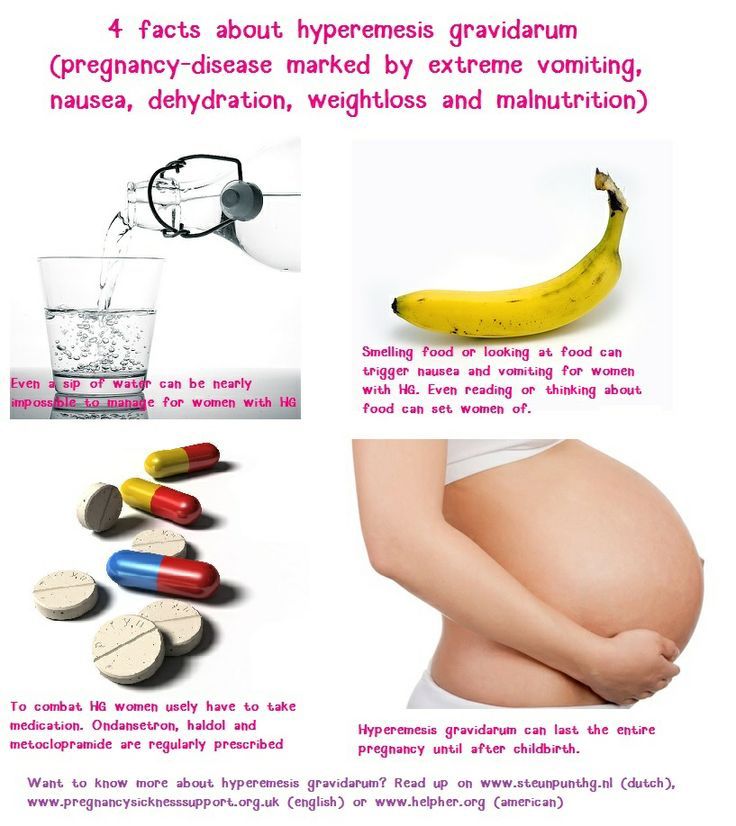
Previous molar pregnancy. If a woman has already had one molar pregnancy, she has a 1 in 100 chance of having a recurrence. If a woman has had two or more molar pregnancies, the risk of another pregnancy with this condition is higher, about 15 to 20 out of 100.
Symptoms of molar pregnancy
Vaginal bleeding
Vaginal bleeding is the most common symptom of molar pregnancy. Bleeding can occur during normal pregnancy and is not always serious, but the woman should immediately inform the gynecologist or midwife about it. Women with a mole are more likely to develop blood clots or a watery brown vaginal discharge. In some pregnant women, pieces of molar tissue come out, which can look a bit like small bunches of grapes. Bleeding caused by a mole usually starts between 6 and 12 weeks of gestation.
The following symptoms are rare. This is because most hydatidiform moles are detected and corrected during routine ultrasound examinations performed in early pregnancy. In some women with a complete hydatidiform mole, the abdomen may expand faster than in a normal pregnancy. In women with partial hydatidiform mole, the uterus and abdomen may be smaller than expected for this stage of pregnancy.
In some women with a complete hydatidiform mole, the abdomen may expand faster than in a normal pregnancy. In women with partial hydatidiform mole, the uterus and abdomen may be smaller than expected for this stage of pregnancy.
Nausea is common in normal pregnancies, but may be more severe and more frequent with mole. This is called hyperemesis.
Anemia means that the patient has few red blood cells in her body. If a woman is losing blood due to vaginal bleeding, her red blood cell count may decrease. Due to anemia, the patient may feel constant fatigue and shortness of breath.
Pre-eclampsia is a complication that can occasionally occur during the last 3 months of a normal pregnancy. The main symptoms are high blood pressure and protein in the urine. In rare cases, with a hydatidiform mole, preeclampsia can be obtained much earlier.
An overactive thyroid is a rare symptom of molar pregnancy. The medical term for this is hyperthyroidism.
Molar pregnancy stages
staging is a system doctors use to describe the size of a tumor and whether it has spread. Gynecologists usually remove abnormal molar tissue during pregnancy from the uterus. If the levels of a hormone called hCG return to normal shortly after the mole is removed, then the doctor does not need to stage the mole. In most women, the hCG level practically disappears within 4-6 weeks after the removal of the hydatidiform mole. Once the molar tissue has left the uterus, it cannot produce hCG. Thus, in addition to subsequent blood and urine tests to check for molar tissue return, the woman will not need additional tests.
Gynecologists usually remove abnormal molar tissue during pregnancy from the uterus. If the levels of a hormone called hCG return to normal shortly after the mole is removed, then the doctor does not need to stage the mole. In most women, the hCG level practically disappears within 4-6 weeks after the removal of the hydatidiform mole. Once the molar tissue has left the uterus, it cannot produce hCG. Thus, in addition to subsequent blood and urine tests to check for molar tissue return, the woman will not need additional tests.
If the hCG level remains high or rises, this may be a sign that abnormal cells are still present in the uterus. The cells may spread to deeper layers of the uterus or other parts of the body. Gynecologists call this persistent trophoblastic disease. In this case, the woman will need additional tests to determine the stage of the tumor.
Survival of hydatidiform mole
Almost all women with hydatidiform mole recover. Doctors remove all of the abnormal molar tissue with surgery, and most women don't need further treatment. In a small number of patients, some abnormal cells remain and may spread to deeper layers of the uterus or other parts of the body. This is called persistent trophoblastic disease. Chemotherapy can usually completely rid a woman of all abnormal cells.
In a small number of patients, some abnormal cells remain and may spread to deeper layers of the uterus or other parts of the body. This is called persistent trophoblastic disease. Chemotherapy can usually completely rid a woman of all abnormal cells.
Molar Pregnancy Diagnosis
When a woman is pregnant, the placenta produces the hormone human chorionic gonadotropin (hCG) to help the baby develop. The placenta releases hCG into the bloodstream, and the body gets rid of the rest in the urine. HCG is produced during molar pregnancy, but is at a much higher level than normal. Thus, routine blood tests during pregnancy may reveal a mole.
Women usually have a routine ultrasound at 12 weeks pregnant. Molar pregnancies may show a characteristic "blizzard appearance" on scans. An ultrasound scan is a good way to diagnose complete molar pregnancies, but it is not as good at detecting partial molar pregnancies. A partial molar pregnancy can still be detected by a blood test.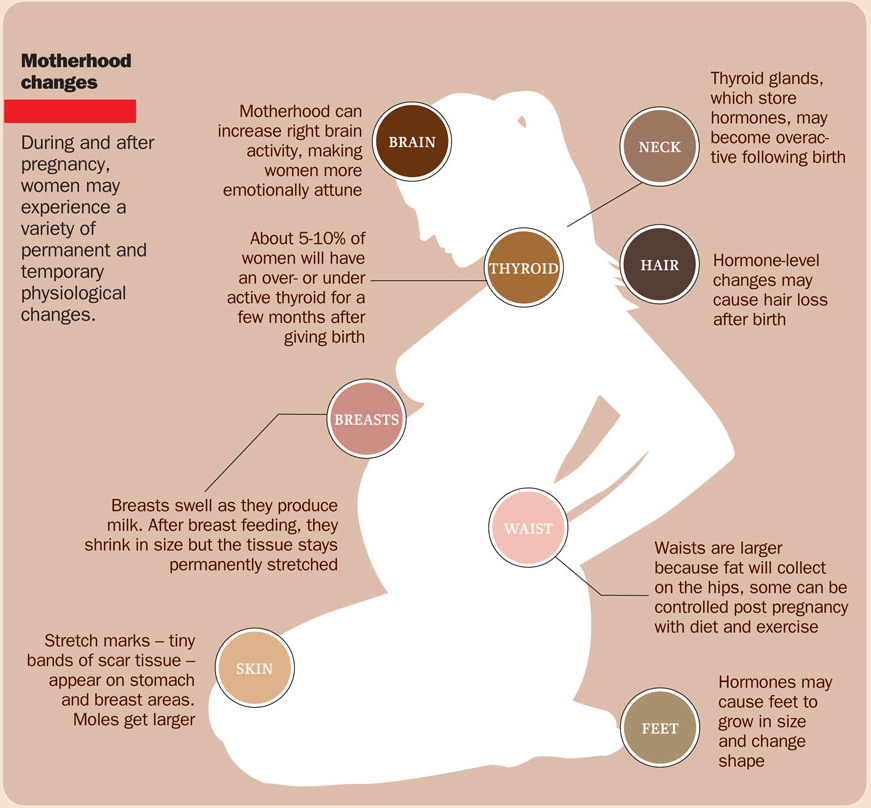
Diagnosis after a miscarriage or abortion
A doctor will usually examine the tissues of the placenta and fetus if a woman has had a miscarriage in the hospital or an abortion. These checks may reveal abnormal mole cells. If positive, the woman will need treatment to remove molar tissue from the uterus.
Treatments for hydatidiform mole
There are various surgical options for removing a molar pregnancy.
Mole surgery
Most women have a minor operation under general anesthesia to remove molar tissue from the uterus. The operation is called dilation and suction evacuation. The surgeon uses a thin tube to gently suck out the molar tissue. Sometimes they may also use a sharp instrument to cut tissue from the uterine lining. This is called expansion and scraping. This treatment removes all of the molar tissue for most women.
Removal of the uterus (hysterectomy)
The surgeon may suggest removal of the uterus (hysterectomy) instead of removing just the molar tissue.
Drug treatment to remove molar tissue
Some women with partial mole are given drug treatment to make the uterus contract and get rid of the abnormal cells.
Author: Belyakov Nikolai Grigorievich
Specialization: Pediatrician
Where does the reception: Clinic General Medical Center (GMC), St. Petersburg
Share:
The best specialists in St. Petersburg with a rating of 4.5+
Veromey Dominika Tadeushevna
Specialization: Therapist, Gynecologist, Obstetrician-gynecologist
Medical experience: since 201023 Where does the appointment: Dr. Pel's Clinic
Andreeva Oksana Sergeevna
Specialization: Ultrasound doctor, Gynecologist, Obstetrician-gynecologist
Medical experience: since 1998
Where does the appointment: Dr. Pel's Clinic
Evgeniya Kaminskaya
Specialization: Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 1994
Where he meets: Clinic of Dr. Pel, IEM Medical Center, Medical College
Pel, IEM Medical Center, Medical College
Golotina Maria Vladimirovna
Specialization: Ultrasound doctor, Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 2008
Where does the appointment: Dr. Pel's Clinic
Literature:
- Beskova T.K., Kalinin A.V. Study of the immune status in patients with hydatidiform mole // Journal "A and G" 1981. No. 9.
- Davydova M.A., Kalelyushnik N.L., Osipov R.A. Progressive form of hydatidiform drift//Kazan medical journal 1979 (1).
- Kalinin A.V. Clinical and morphological features of hydatidiform mole and its prognosis // Abstract of the discussion for the degree of candidate of medical sciences. 1982.
- I. Persianinov L.S., Demidov V.N. Ultrasonic diagnostics in obstetrics. — M.: Medicine. - 1980. —- 335 S.
- Kosenko IA, Bakinovskaya IE Ultrasound diagnosis of trophoblastic tumors of the uterus.
 Minsk: Medicine, 2005.-75p.
Minsk: Medicine, 2005.-75p.
Latest diagnostic articles
Radiation therapy
Radiation therapy is a treatment that uses radiation to kill cancer cells. This therapy is most often prescribed by oncologists for the treatment of oncological diseases.
Read more
Is MRI harmful to health
When making an MRI appointment, the patient sometimes has questions about the safety of the examination: “Is there any harm from MRI for the body, what is the danger of magnetic resonance imaging, and how often can MRI be done. Let's figure it out.
Read more
Principles of operation of MRI, ultrasound, CT, X-ray and PET
In modern medicine, thanks to advances in technology, there is a wide range of diagnostic equipment that helps doctors in the early detection of diseases and pathological disorders. In this article we will talk about the principles of operation of MRI, ultrasound, CT,
Read more
MRI during pregnancy
Since every day MRI technology provides doctors of St. Petersburg medical centers with an increasing range of diagnostic capabilities, it is being actively used in pediatrics, prenatal diagnostics in pregnant women and oncology. As soon as a woman finds out that she will become a mother, she immediately has the question of what procedures she can do and which are contraindicated. Almost all pregnant women know that they are strictly forbidden to take x-rays and can undergo ultrasound.
Petersburg medical centers with an increasing range of diagnostic capabilities, it is being actively used in pediatrics, prenatal diagnostics in pregnant women and oncology. As soon as a woman finds out that she will become a mother, she immediately has the question of what procedures she can do and which are contraindicated. Almost all pregnant women know that they are strictly forbidden to take x-rays and can undergo ultrasound.
Read more
Woman thought she was pregnant but ended up giving birth to a cancerous tumor
stories
cognitive
diseases
people
12/01/2017
14254
Lauren Knowles, from Aberdeen, Scotland, was heartbroken when she discovered in her seventh week of pregnancy that her unborn child was actually a terminal illness.
At the age of 27, Lauren was beside herself with happiness when a pregnancy test came back positive, but her happiness turned into horror when, at the seventh week of pregnancy, her body suddenly became covered with spots
Immediately after the spots appeared, the doctors sent Lauren for an examination, which showed that the woman was experiencing a so-called molar pregnancy.
A molar pregnancy, also known as a hydatidiform mole, is a pregnancy failure that causes abnormal growth of placental tissue in a woman's uterus.
Simply put, this is when a fertilized cell is defective, as a result of which a placenta begins to form with a fetus that does not develop due to the lack of the necessary chromosomes - a full mole, or vice versa, the fetus has too many chromosomes, because of which it begins develop abnormally and cannot survive - partial mole.
Both of these cases are accompanied by abnormal growth of the placenta.
Lauren was unfortunate to face one of these cases, but unfortunately, her misfortunes did not end there. Doctors later confirmed that her molar pregnancy was also accompanied by cancerous cells. This disease is called trophoblast and is also known as placental cancer.
Although the cancerous tissue was removed, the tumor continued to grow at an alarming rate and Lauren had to undergo chemotherapy, which led to hair loss
"The tumor grew in my stomach like a baby, my body produced the same hormones and all my pregnancy tests were always positive," Lauren said.
"I didn't think it could be cancer, but when I started bleeding in the seventh week of my pregnancy, I had an additional examination," she continued.
[region:bone:inline_1]
Doctors performed a double scan of Lauren's abdomen to confirm the diagnosis
What Lauren said:
"It was only then that the doctors told me it was a molar pregnancy. I didn't even know what it was, so they gave me a newsletter, and the more I read it, the stronger my heart went to the heels."
"My tumor was cancerous, so I started mild chemotherapy, but the tumor continued to grow."
"It was terrible and one day when I was swinging my son on the swing in the park, I looked down and saw that I was covered in blood."
"I was rushed to the hospital, where I underwent 6 cycles of highly toxic chemotherapy that caused me to lose all my hair in a week."
After five months of treatment, in April 2015, Lauren's health began to deteriorate sharply, but the usual trip to the toilet turned out to be an unexpected surprise for her:
I went to the hospital toilet.
"
"When I was sitting in the toilet, I felt that I had to push something out of myself, and it was very painful. After a lot of pain, I got up, looked into the toilet, and saw a large dark mass there."
"It was a huge relief for me, and I knew it was the end. I was so happy that the tumor was finally out of me."
The doctors said that Lauren's next pregnancy could be complicated or the woman would never be able to have children at all, but in any case, they advised parents to continue trying no earlier than a year after getting rid of the tumor.
Lauren was able to conceive after a one-year hiatus 3 months after resuming her attempts to have a baby
"Throughout my pregnancy, I was terrified that she would be molar again, so I couldn't enjoy the feeling of having a baby."
"During the first scan, we saw a beating heart and I couldn't stop crying because I didn't believe it was really happening."
"Indy [daughter's name] was born 5 weeks premature and had to have an emergency c-section.