Bulging veins in legs pregnancy
Hemorrhoids and Varicose Veins in Pregnancy
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What are hemorrhoids and varicose veins?
Hemorrhoids and varicose veins might seem to be two different, unrelated problems, but they're actually quite similar. And many women, especially those in the third trimester of pregnancy, have them.
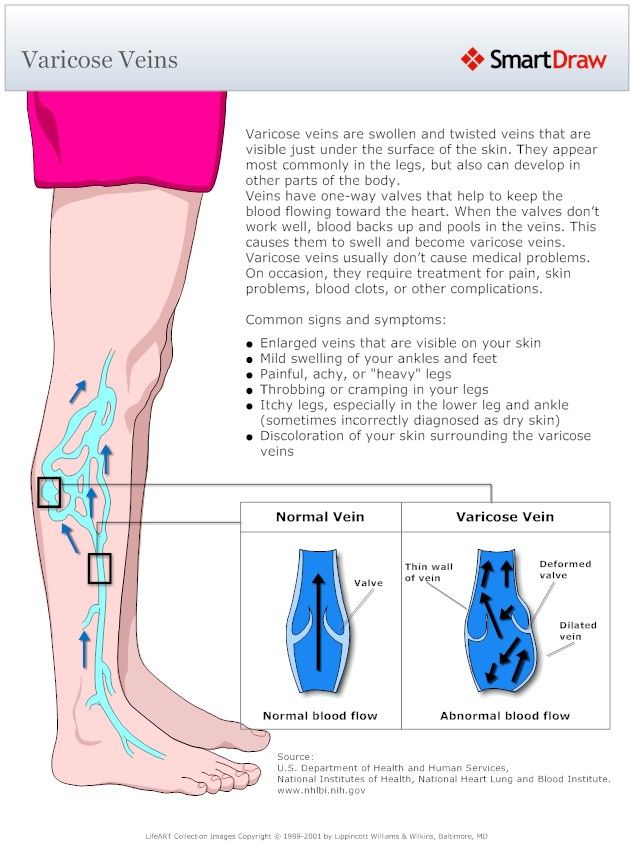
Both hemorrhoids and varicose veins are swollen, twisted veins. These veins are often in the legs, but they also can form in other parts of your body. When they form in the rectum, they're called hemorrhoids.
What causes hemorrhoids and varicose veins in pregnancy?
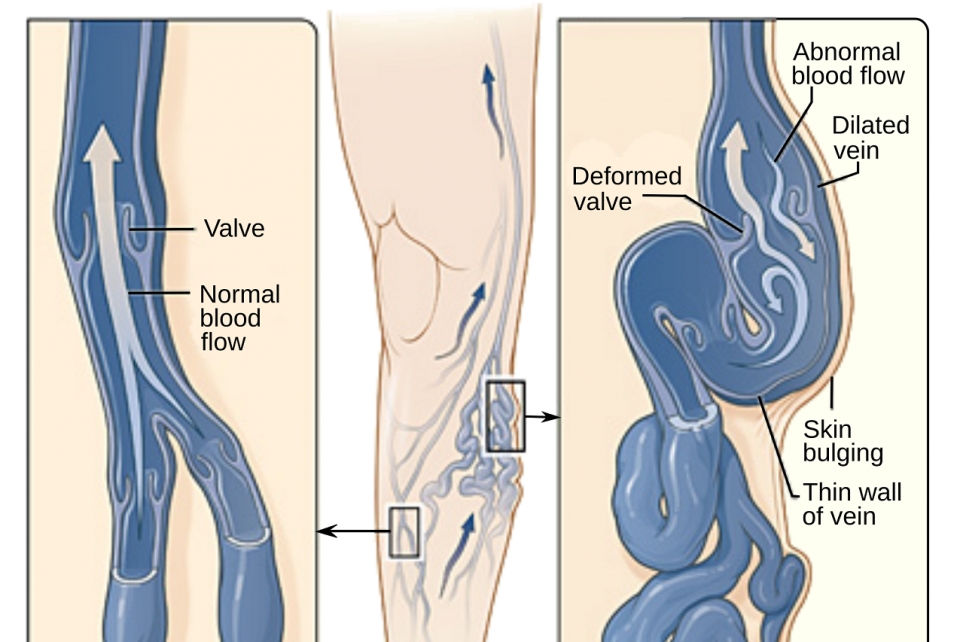
Normally, veins have one-way valves to help keep blood flowing toward the heart. Pressure or weakening of these valves allows blood to back up and pool in the veins. This causes them to enlarge and swell. Hemorrhoids result when rectal veins enlarge. Varicose veins occur when veins of the legs swell.
Many changes in pregnancy can increase the risk of hemorrhoids and varicose veins, such as:
- Increased blood volume, which enlarges the veins
- The heavy weight of the growing baby, which presses on the large blood vessels in the pelvis, altering blood flow
- Hormone changes affecting blood vessels, which can slow the return of blood to the heart and cause the smaller veins in the pelvis and legs to swell
Hemorrhoids can get worse with pushing or straining, especially with constipation. Being overweight and having hemorrhoids before pregnancy can also make them worse. Pushing during delivery tends to worsen hemorrhoids, too.
Varicose veins tend to run in families. Sitting or standing in one position for a long time may force the veins to work harder to pump blood to the heart. This can result in swollen, varicose veins and can also worsen existing hemorrhoids. Varicose veins can also occur in a woman's genital area.
What are the symptoms of hemorrhoids and varicose veins in pregnancy?
Hemorrhoids can be internal, forming inside the rectum, or external, located on the outside, around the anal opening. Internal hemorrhoids can sometimes bulge out through the anal opening. The most common symptom is bright red blood passed with a bowel movement. External hemorrhoids can be painful or itch and may bleed if irritated by straining or wiping.
Varicose veins often look like large, twisted, raised blue or purple veins on the legs–often on the backs of the calves or inside the legs. They may cause mild swelling in the ankles and feet or aching, heaviness, or throbbing in the legs. They can also cause leg cramps. If varicose veins occur in the genital area, they also appear as large, twisted, raised veins.
They may cause mild swelling in the ankles and feet or aching, heaviness, or throbbing in the legs. They can also cause leg cramps. If varicose veins occur in the genital area, they also appear as large, twisted, raised veins.
How are hemorrhoids and varicose veins in pregnancy diagnosed?
Your healthcare provider will examine your legs or rectal area to check for varicose veins or hemorrhoids.
How are hemorrhoids and varicose veins in pregnancy treated?
Hemorrhoids in pregnancy are a short-term problem, and they get better after your baby is born. Still, there are some things you can do to relieve the discomfort:
- To relieve pain, sit in a tub or sitz bath several times a day in plain, warm water for about 10 minutes each time. When you use a tub bath, don’t fill the tub all the way. Just put in enough warm water to sit in.
 That will direct blood flow to your rectum.
That will direct blood flow to your rectum. - Use ice packs or cold compresses to reduce swelling.
- Ask your healthcare provider about creams or other medicines, such as stool softeners, that are safe to use during pregnancy.
It’s important to prevent constipation by including lots of fiber and fluids in your diet.
Also try not to strain with bowel movements, and avoid sitting for a long time. Regular Kegel exercises can help improve muscle tone, These exercises involve squeezing and relaxing the muscles in your vaginal and rectal area.
Most varicose veins that develop during pregnancy get better within the first year after birth. But for now, limit standing or sitting for a long time without a break, and try not to cross your legs.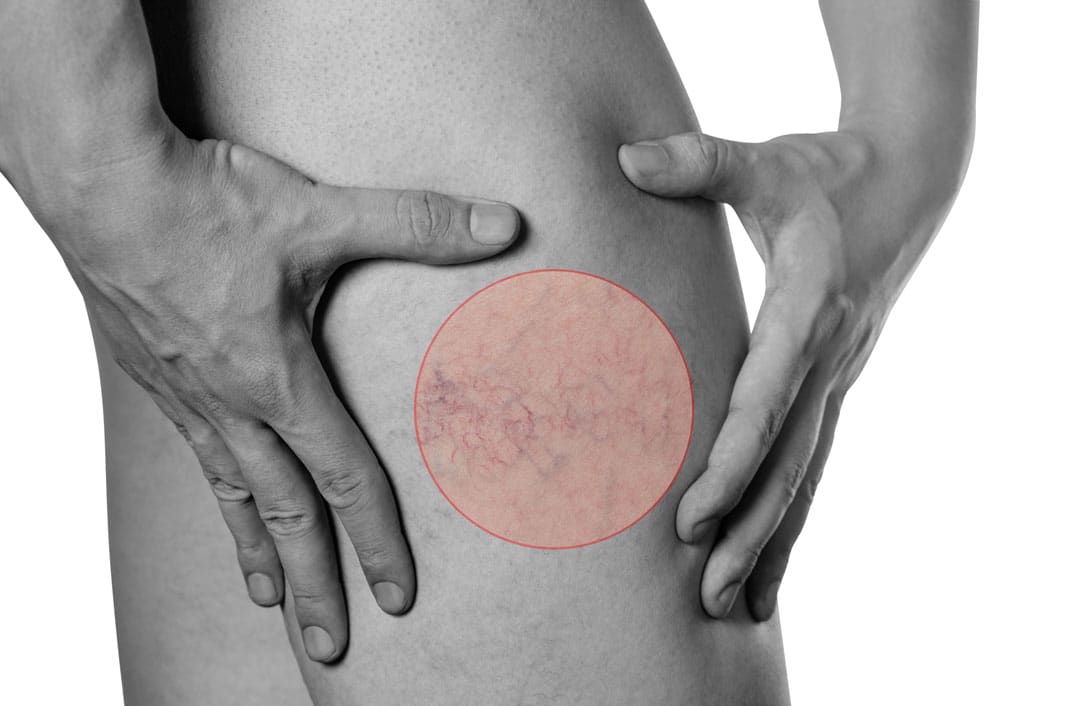 Also try to raise your legs and feet whenever you’re sitting or lying down.
Also try to raise your legs and feet whenever you’re sitting or lying down.
Avoid tight clothing around your waist, thighs, and legs, as it can worsen varicose veins.
Be sure to check with your provider if your symptoms worsen or you have excessive bleeding from hemorrhoids. And remember that these problems are usually short-term and get better after delivery with time and treatment.
What can I do to prevent hemorrhoids and varicose veins in pregnancy?
The best way to help prevent hemorrhoids during pregnancy is to prevent constipation. If you're constipated, don't strain during bowel movements.
Steps to help prevent varicose veins are the same as those used to decrease symptoms:
- Don't stand still or sit for long periods of time.
- Prop your feet up whenever possible.
- Don't wear tight clothes.
Key points about hemorrhoids and varicose veins in pregnancy
- Both hemorrhoids and varicose veins are swollen, twisted veins. These veins are often in the legs, but when they form in the rectum, they're called hemorrhoids.
- Many normal changes in pregnancy can increase the risk for hemorrhoids and varicose veins.
- Hemorrhoids and varicose veins in pregnancy are a short-term problem, and they get better after your baby is born.
- You can do things to ease the discomfort they can cause. These include sitz baths, ice packs, or cold compresses to reduce swelling and creams or other medicines, such as stool softeners, your healthcare provider may recommend.
- The best way to help prevent hemorrhoids during pregnancy is to prevent constipation. If you're constipated, don't strain during bowel movements.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.

- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Medical Reviewer: Irina Burd MD PhD
Medical Reviewer: Donna Freeborn PhD CNM FNP
Medical Reviewer: Heather M Trevino BSN RNC
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Varicose Veins and Your Pregnant Legs
Written by Nicklya Harris-Ray
In this Article
- What Are Varicose Veins?
- Varicose Veins Pregnancy Cause
- Varicose Veins Pregnancy Symptoms
- Pregnancy Varicose Veins Treatment
- How Can You Prevent Varicose Veins?
- Is a Hemorrhoid a Varicose Vein?
- Do Varicose Veins Go Away After Pregnancy?
Varicose veins are very common.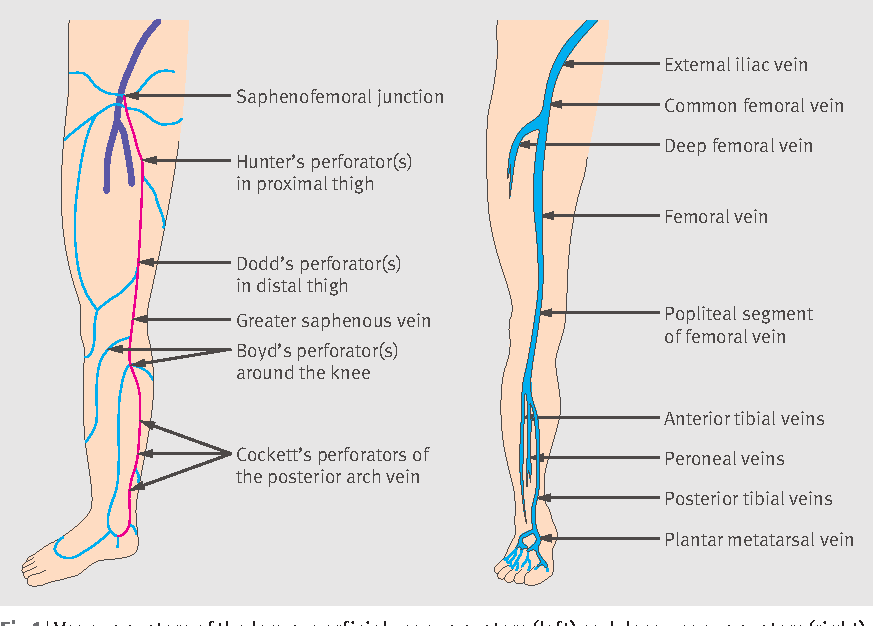 For most women, they are usually a harmless result of pregnancy. Pressure from the uterus on the circulatory system causes blood to back up on the way back to the heart from the legs. Such varicose veins can be easily managed and eventually should go away.
For most women, they are usually a harmless result of pregnancy. Pressure from the uterus on the circulatory system causes blood to back up on the way back to the heart from the legs. Such varicose veins can be easily managed and eventually should go away.
What Are Varicose Veins?
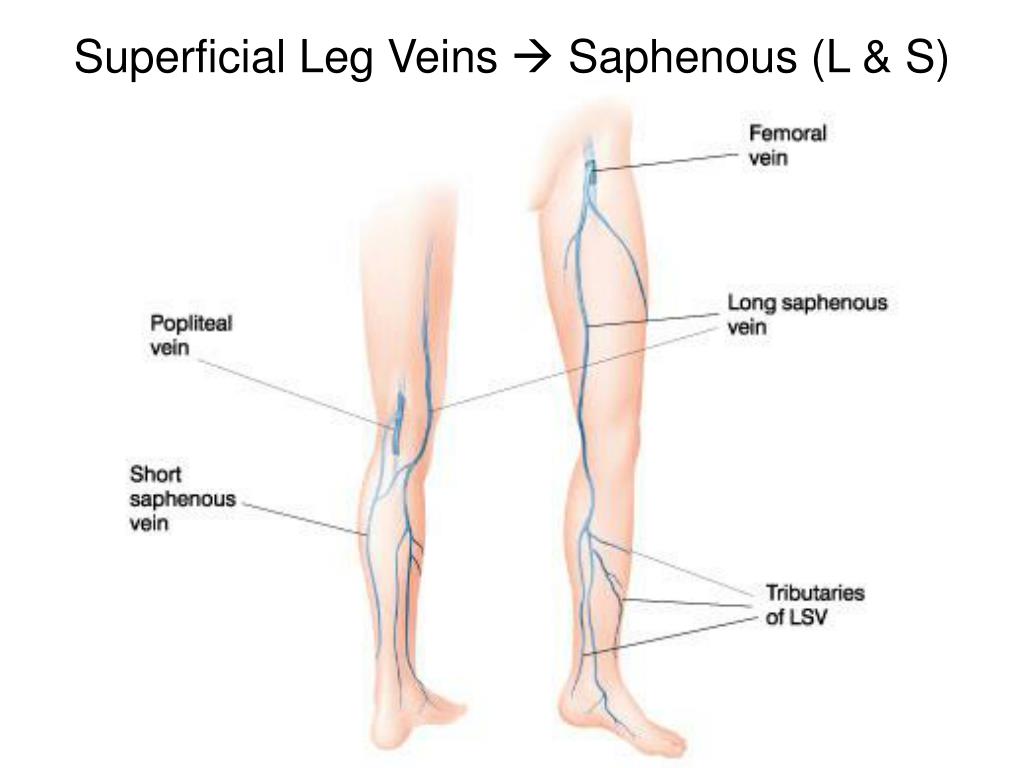
About half of women notice enlarged or abnormal dilation of the superficial veins of their legs while pregnant. These are varicose veins.
Superficial veins in the leg have one-way valves. They help to move blood up the leg against the pull of gravity to return blood to the heart. During pregnancy, many physiological changes occur, including the enlarging of those veins, which become visible. Another physiological change is the growth of the uterus, which affects the main blood vessels.
Varicose Veins Pregnancy Cause
Varicose veins are usually hereditary. Your mother may have had them too, and not much can be done to prevent them.
During pregnancy, blood volume in the body increases. It can increase by up to 20 percent. The number of veins remains the same, though, meaning that there is more work for your limited vascular system.
It can increase by up to 20 percent. The number of veins remains the same, though, meaning that there is more work for your limited vascular system.
Spikes in your hormones like progesterone, meanwhile, relax the ligaments of the pelvis and the muscle cells in the walls of the vein. This makes the upward movement of blood more difficult during pregnancy.
As a result, veins dilate, which places pressure on the valves. This causes the veins to dilate even more, making the valve almost useless.
The veins can become itchy and uncomfortable. Though usually found in the legs, varicose veins can also show up in the genital area and as hemorrhoids in the rectum.
Varicose Veins Pregnancy Symptoms
Varicose veins appear as twisted, large, raised bluish/purplish veins in the legs. They often appear on the inside of the legs or back of the calves. They may cause:
- Mild swelling in the feet or ankles
- Aching
- Throbbing in the legs
- Heaviness
They can cause leg cramps.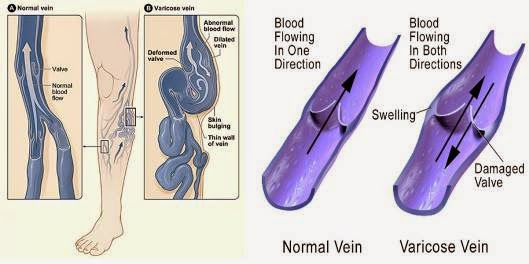 Some may also consider the veins a cosmetic issue. Regardless, you should let your OB-GYN know that you have them. This is especially important if they cause discomfort.
Some may also consider the veins a cosmetic issue. Regardless, you should let your OB-GYN know that you have them. This is especially important if they cause discomfort.
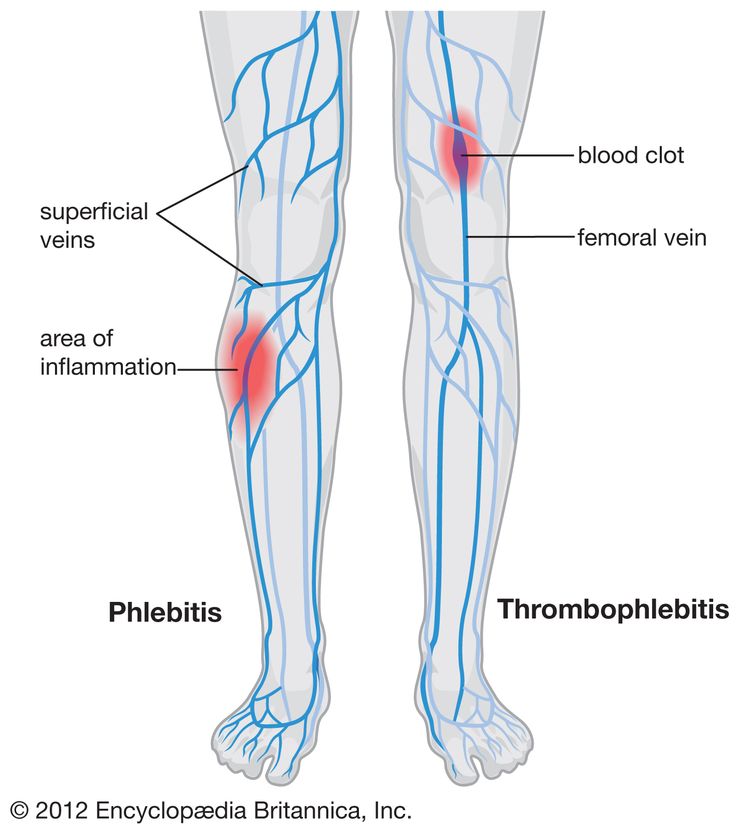
Rarely, venous insufficiency can occur. This is the failure of the veins to return the blood to the heart sufficiently, and therefore, the skin begins to break down. Other rare scenarios include inflammation of the veins, which causes extreme pain and possible blood clots.
Pregnancy Varicose Veins Treatment
Compression stockings are a good treatment and support for varicose veins. They come in many styles, strength levels, and sizes. They can be purchased online, but a prescription submitted by your doctor to a medical supply store can give you a stronger option. Just make sure they are not too strong.
The stockings are graded by pressure value with a measurement of millimeters of mercury (mmHg). Doctors recommend anywhere from 20 to 30 mmHg strength, which is considered moderate- to high-pressured. The lowest strength available is 8 15 mmHg.
The lowest strength available is 8 15 mmHg.
Warning: Some moms have tried horse chestnut extract (with esculin, which is poisonous, removed). Please note that eating the flower, raw bark, leaf, or seeds of this plant instead of the extract is poisonous and can be fatal. In fact, the safety of the use of horse chestnut extract, even with the poison parts removed, is unknown. So, it is best to avoid it while pregnant or breastfeeding. Doctors discourage the pursuit of elective surgery to get rid of the veins during pregnancy. The veins usually fade after birth.
How Can You Prevent Varicose Veins?
Several things can be done to avoid varicose veins, avoid making them worse, and reduce vein pain:
- Keep your feet elevated often.
- Engage in daily low-impact exercises with your doctor's approval.
- Take regular breaks and move back and forth as much as possible after extended periods of standing or sitting.
- Keep your legs uncrossed while sitting.
- Sleep with your body turned to the left side to keep pressure off the inferior vena cava, which is located on the right side of the body.
- Wear maternity hose that supports your legs.
You could try these practical adjustments as well:
- Decrease your intake of salt to minimize swelling of the veins.
- Drink a lot of water, and eat plenty of fiber to stop constipation.
- Avoid wearing high heels. It is wiser to wear flat shoes or low heel shoes because this exercises the calf muscles, aiding in better circulation.
Is a Hemorrhoid a Varicose Vein?
Both varicose veins and hemorrhoids are twisted, swollen veins. They are called hemorrhoids when they are found in the rectum. They can get worse with straining or pushing that comes with constipation. If you were overweight before pregnancy, hemorrhoids can become worse during pregnancy. Pushing during delivery makes them worse as well.
Hemorrhoids can form inside of the rectum internally or outside of the rectum externally around the anus.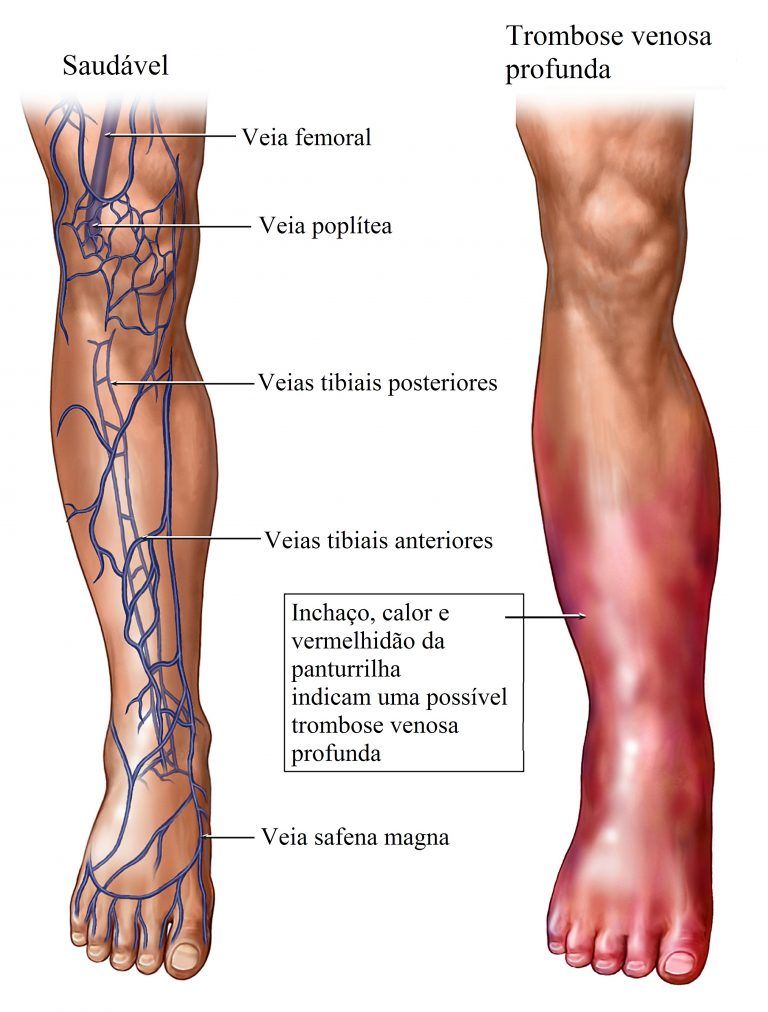 Internal hemorrhoids can grow and bulge through the opening of the anus. The bright red blood that appears during a bowel movement is the most common symptom of hemorrhoids. Hemorrhoids can be itchy, or they can be painful and bleed if they are irritated by wiping and straining.
Internal hemorrhoids can grow and bulge through the opening of the anus. The bright red blood that appears during a bowel movement is the most common symptom of hemorrhoids. Hemorrhoids can be itchy, or they can be painful and bleed if they are irritated by wiping and straining.
Do Varicose Veins Go Away After Pregnancy?
Varicose veins are usually harmless, though they could become uncomfortable and itchy. They typically go away within 3 months after giving birth. In the majority of cases, moms walk away from pregnancy with varicose veins that, if not completely gone, are less painful and prominent.
Again, varicose vein surgery is not suggested during pregnancy because they usually automatically improve after birth. However, if the veins become tender, warm, red, swollen, or if they bleed, you should immediately contact your doctor. If the skin of the leg thickens or changes color, or if you develop a rash, it is similarly important to seek medical attention.
Varicose veins during pregnancy - what to do and how to treat varicose veins in the legs
Varicose veins are persistent and irreversible enlargement resulting from pathological changes in the walls and valves of blood vessels. The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
Causes
The following reasons contribute to the occurrence of varicose veins during pregnancy:
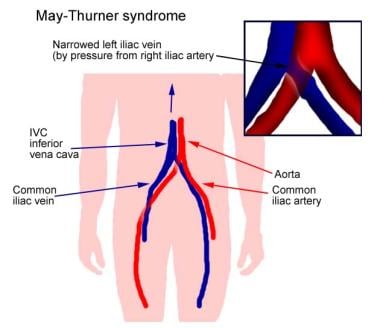
- Violation of the outflow of blood from the veins of the lower extremities. This is because the growing uterus presses on the inferior vena cava - a large abdominal vein that collects blood from the lower half of the trunk and lower extremities.
- During pregnancy, the blood is more viscous, flows more slowly, this also contributes to venous congestion.
- The increase in body weight during gestation increases the load on the legs.
The development of varicose veins is promoted by wearing high-heeled shoes, prolonged work in a standing position, lifting weights, and overweight.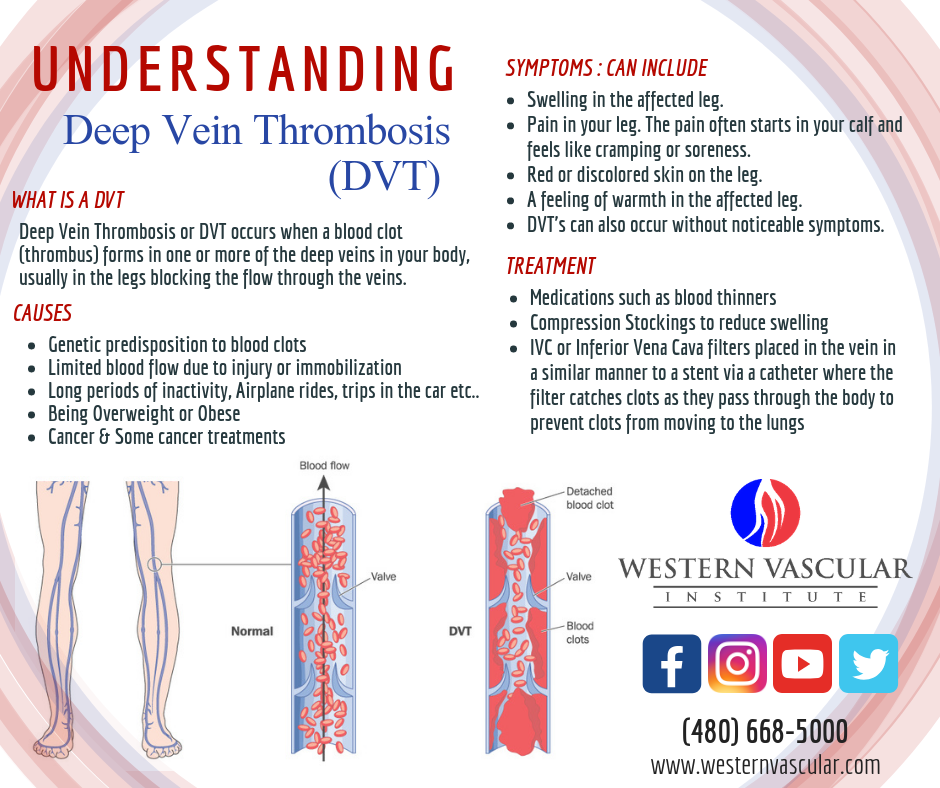
Symptoms
The first symptom is a visible increase in the vessels of the lower extremities. The veins are blue or purple, tortuous, protrude above the surface of the skin, may be serpentine or knobby (nodular) in shape. At the initial stage of the disease, a woman is only concerned about a cosmetic defect.
Other complaints follow. Edema appears, increasing in the evening and decreasing or completely disappearing after rest and a night's sleep. At night, convulsions may disturb. When walking, rapid fatigue is observed, there may be a feeling of fullness and pain.
Varicose veins of the lower extremities are observed in 50% of pregnant women, but not all of them suffer from true varicose veins, when irreversible changes appear in the venous wall. For most, the disease is functional in nature, that is, it is temporary, and after childbirth, when the factors that prevent normal venous outflow are eliminated, the tubes return to normal. This usually happens within a year.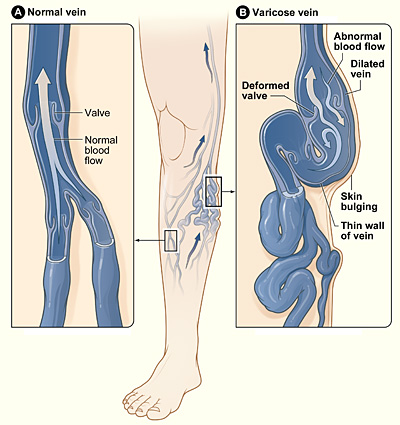
Regression does not occur if the predisposition is independent of pregnancy. In this case, close relatives usually have varicose veins, or the woman herself had some symptoms even before conception.
Diagnostics
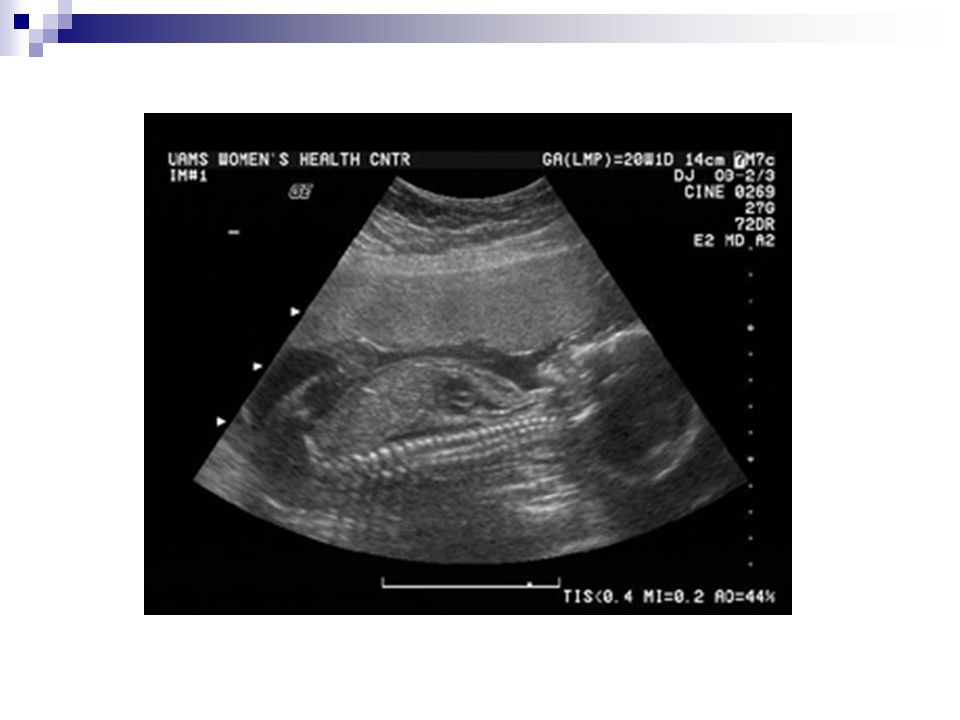
As you know, the “gold standard” for diagnosing pathology is ultrasound duplex scanning (USDS) of the veins of the lower extremities. This is a safe procedure for the expectant mother. Experienced obstetricians and gynecologists strongly recommend that pregnant women visit a phlebologist in the early stages of pregnancy, which contributes to the early prevention of complications of varicose veins in the postpartum period.
Stockings for varicose veins during pregnancy
During pregnancy, it is recommended to wear special compression (anti-varicose) tights and stockings. They need to be put on in a prone position, slightly lifting the leg up. There are 4 compression classes (pressure levels):
- 18-21 mmHg
- 23-32 mmHg
- 33-48 mmHg
- over 49 mmHg
During pregnancy, it is recommended to use compression class 1-2. The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
Tights should be specially designed for expectant mothers so that they do not put pressure on the growing belly, but support it.
How much to wear?
After 20 weeks, you need to wear a bandage. It supports the uterus and reduces pressure on the large vessels of the abdominal cavity, thereby improving the outflow of blood from the lower half of the body.
Compression underwear and a bandage should be bought in pharmacies, it is important to choose the right size for them.
Exercise
It is recommended to attend gymnastics for pregnant women or do exercises at home. Particularly good prevention of varicose veins are classes in the pool. Sports strengthen the walls of blood vessels and improve blood flow. In addition, gymnastics is the prevention of overweight.
A contrast shower on the calf muscles is useful.
If you think you have a predisposition to varicose veins, you should avoid saunas and thermal treatments.
As often as possible, try to give your legs an elevated position. Don't sit cross-legged for long periods of time.
Wear comfortable shoes with small heels.
You can use creams for pregnant women "to relieve fatigue from the legs", such creams usually contain plant substances that, with regular use, strengthen the walls of superficial veins.
Treatment
Treatment of true varicose veins is surgical. During pregnancy, surgical treatment is carried out only for emergency indications, in view of the development of complications (thrombophlebitis).
A modern method of treatment is sclerotherapy, when a chemical substance is injected into the lumen of the vein, which leads to sclerosis and closure of its lumen. Endovasal methods are also minimally invasive treatments performed on an outpatient basis (described in the relevant sections of our website).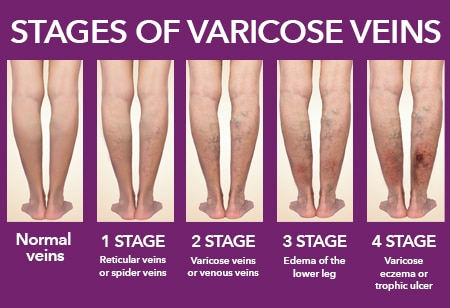 They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
All other methods are aimed only at preventing the disease from developing and temporarily reducing symptoms.
Most often, various ointments and gels are used, which are applied to the affected limb. For example, heparin-containing ointments reduce blood clotting and prevent the formation of blood clots. Venotonics (allowed only from the second trimester of pregnancy) have a decongestant and anti-inflammatory effect and strengthen the walls of blood vessels.
The diagnostic equipment used in our center has been tested in ROSTEST and has an appropriate conclusion about the absence of contraindications for use in pregnant women and children.
In the medical center "Yuzhny" they are very kind to expectant mothers and experienced phlebologists are well versed in the methods of diagnosing CVI and the secrets of preserving your beautiful legs after childbirth.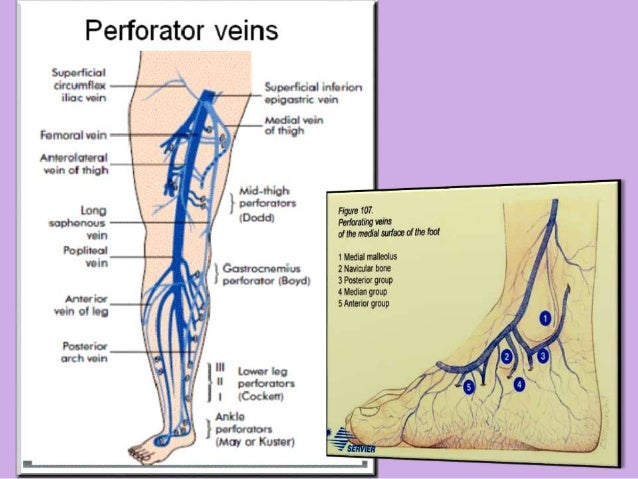
Varicose veins during pregnancy. Phlebologist's recommendations for pregnant women - Dobrobut clinic
Chronic venous insufficiency and pregnancy
Pregnancy is a wonderful, joyful and natural state. However, pregnancy does not always go smoothly. Hormonal changes in this period of life have a positive effect on a woman's body, protect it during this difficult period, but the same hormones can significantly complicate the work of other organs and systems. Connective tissue undergoes the greatest changes. This can cause various problems: pain in the lower back and joints, the appearance of "stretch marks" on the skin of the chest and abdomen, flat feet. In addition, 50% of women develop either dilated skin capillaries or varicose veins during their first pregnancy. With repeated pregnancies, this percentage increases, and the risk of thrombotic complications also increases sharply.
Nature took care that during childbirth the mother did not lose much blood.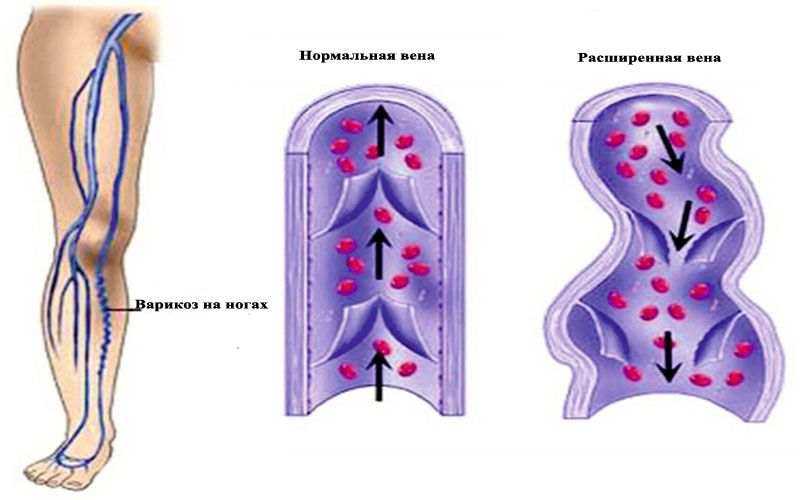 To do this, during pregnancy, under the influence of hormones, the blood becomes thicker. Thickening of the blood, as well as venous stasis, significantly increase the risk of blood clots in the veins. In a future mother, this risk is 3-5 times higher than in a non-pregnant mother. The formation of blood clots in the veins can cause a severe and sometimes fatal complication - pulmonary embolism, which threatens not only health, but also the life of the mother and unborn child. A high risk of thrombosis remains and is even especially dangerous within 6 weeks after childbirth, especially after a caesarean section or large blood loss during childbirth. Thus, pregnancy is actually a thrombogenic condition. This means that the normal changes that occur in the body during physiological pregnancy increase the likelihood of deep vein thrombosis.
To do this, during pregnancy, under the influence of hormones, the blood becomes thicker. Thickening of the blood, as well as venous stasis, significantly increase the risk of blood clots in the veins. In a future mother, this risk is 3-5 times higher than in a non-pregnant mother. The formation of blood clots in the veins can cause a severe and sometimes fatal complication - pulmonary embolism, which threatens not only health, but also the life of the mother and unborn child. A high risk of thrombosis remains and is even especially dangerous within 6 weeks after childbirth, especially after a caesarean section or large blood loss during childbirth. Thus, pregnancy is actually a thrombogenic condition. This means that the normal changes that occur in the body during physiological pregnancy increase the likelihood of deep vein thrombosis.
These changes are:
- Significant slowing of blood flow in the deep veins of the legs due to increased outflow of blood from the placental part of the uterus with overload of the iliac veins;
- Reducing the tone of the walls of the veins and their physiological expansion, which leads to natural valvular insufficiency and reverse blood flow;
- Increased pressure in the veins of the lower extremities by 2-3 times;
- Increased production of sex hormones - progesterone and relaxin, which directly affect elastic fibers and reduce the tone of vascular smooth muscles;
- Significant increase in the concentration of blood coagulation factors;
- Decreased fibrinolytic (dissolving of clots or blood clots) capacity of the blood at the end of pregnancy and in the first stage of labour;
- Entry into the blood of active substances after separation of the placenta
Obstruction of venous outflow from the lower extremities during pregnancy is due to a cascade of five mechanisms:
- Mechanical factor.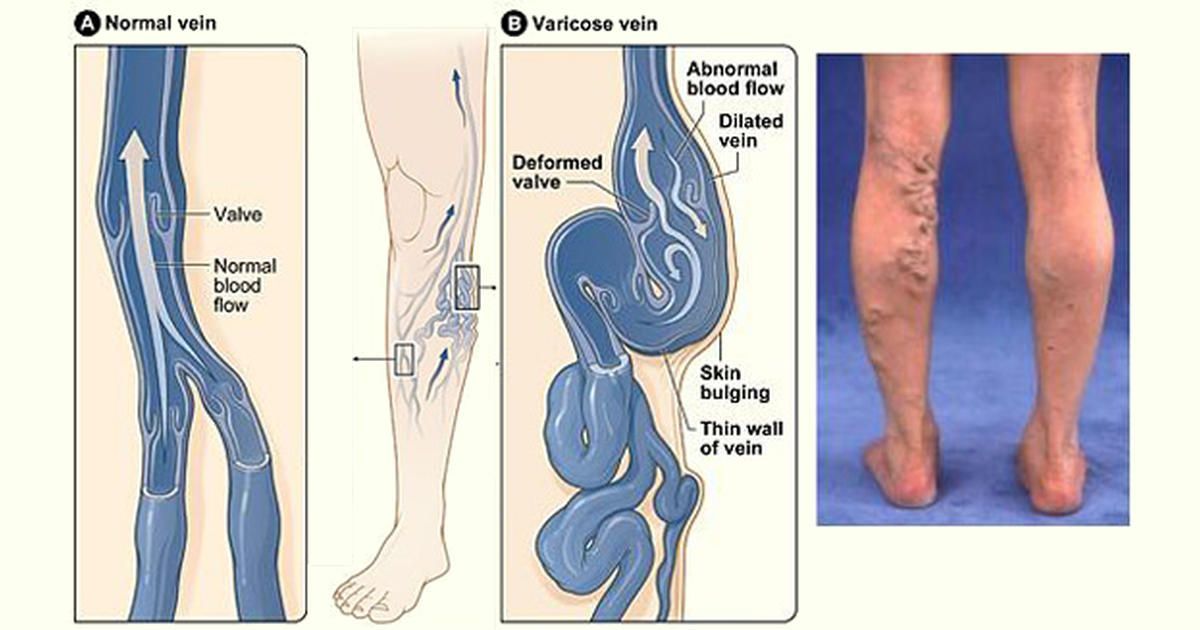 An enlarged uterus is an obstruction to circulation, as it compresses the inferior vena cava, pressing it against the spinal column and iliac muscle.
An enlarged uterus is an obstruction to circulation, as it compresses the inferior vena cava, pressing it against the spinal column and iliac muscle.
- Circulatory factor. An increase in blood volume and outflow of blood from the heart leads to an increase in the load on the veins and their expansion. This is especially important for the veins of the lower extremities and the vaginal area.
- Hormonal factors. Progesterone, due to its relaxing effect on smooth muscle fibers, leads not only to a decrease in the tone of the venous wall, but also to a decrease in the tone of the urethra, bladder and small intestine.
- Hemostatic factors. Changes in the hemostasis system always occur in the direction of increased clotting (increased fibrinogen levels, increased platelet activity and decreased fibrinolytic activity).
- Hemorheological factors. Increased blood viscosity despite decreased hematocrit
- Other contributing factors.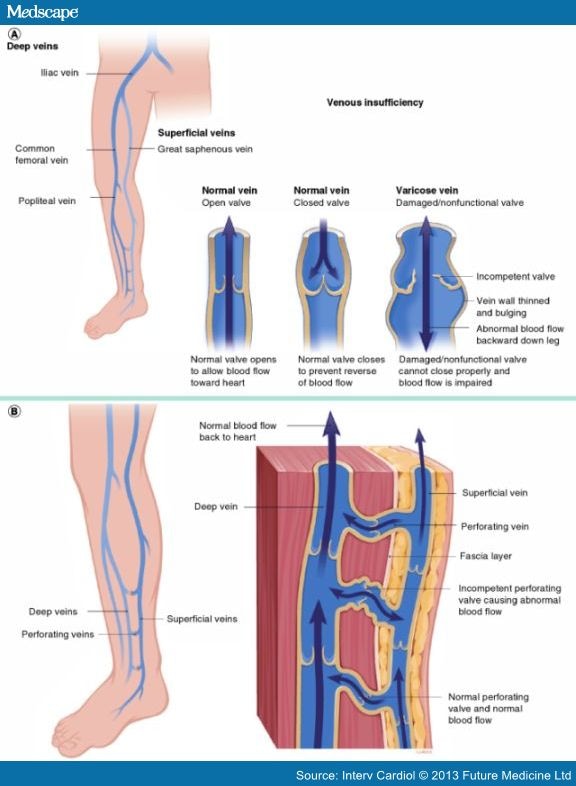 These factors include a strong family history, sedentary lifestyle, prolonged immobility at work, driving, excessively high or thin heels, obesity, hot baths, multiple or short pregnancies.
These factors include a strong family history, sedentary lifestyle, prolonged immobility at work, driving, excessively high or thin heels, obesity, hot baths, multiple or short pregnancies.
The danger increases from the 5th month of the first pregnancy, increases significantly with each subsequent. The triggering factor is the hormonal changes that occur in the body of a pregnant woman: the release of large amounts of female sex hormones, in particular, the hormones of the corpus luteum. In addition, the pregnant uterus grows and, gradually, more and more compresses the large veins located in the pelvis and abdominal cavity, creating obstacles to the outflow of venous blood from the lower extremities. As a result, there is stagnation of venous blood and an increase in pressure in the veins of the legs and small pelvis.
During pregnancy, a woman's body undergoes many changes. The hormone progesterone, which is responsible for the preservation and development of the fetus, affects not only the uterus, but also the veins, their smooth muscle cells, which reduces their tone. The influence of progesterone begins from the first days of conception and fetal development. A high level of the hormone leads to the development of degenerative changes in the elastic and collagen fibers, as a result of which the veins become less elastic and dilate. The process proceeds more quickly if the hormonal background was disturbed before pregnancy, and also if the woman took hormonal drugs, oral contraceptives.
The influence of progesterone begins from the first days of conception and fetal development. A high level of the hormone leads to the development of degenerative changes in the elastic and collagen fibers, as a result of which the veins become less elastic and dilate. The process proceeds more quickly if the hormonal background was disturbed before pregnancy, and also if the woman took hormonal drugs, oral contraceptives.
Varicose veins develop during pregnancy due to many factors. An increase in the volume of circulating blood leads to an increase in pressure on the vessels. Because of this, the veins suffer, since their wall has a lower density and elasticity compared to the arteries.
An increase in the size of the uterus puts pressure on the veins of the small pelvis, which leads to a delay in the outflow of blood from the legs to the upper region. For this reason, varicose veins of the lower extremities occur. An increase in pressure on the vessels of the lower extremities due to the constant weight gain of a pregnant woman.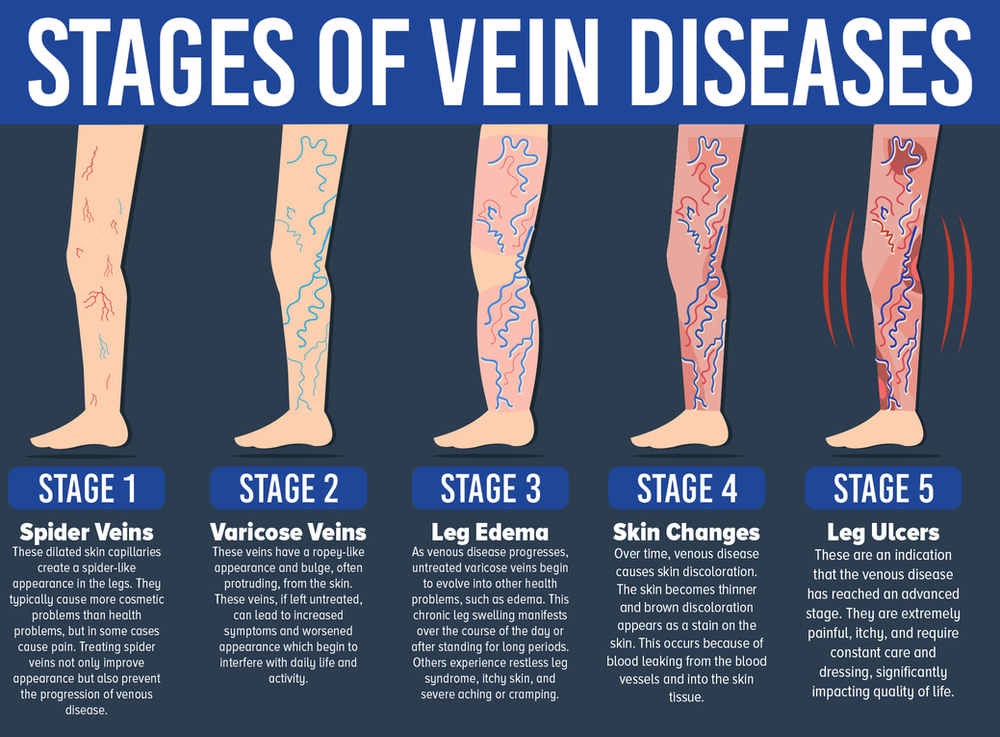 The saphenous veins, which are not surrounded by muscles, are most affected compared to the deep veins. They are most often subjected to varicose expansion, since their wall is not surrounded by an outer layer of the muscular frame.
The saphenous veins, which are not surrounded by muscles, are most affected compared to the deep veins. They are most often subjected to varicose expansion, since their wall is not surrounded by an outer layer of the muscular frame.
There are such forms of varicose veins in pregnant women:
- Varicose disease of the lower extremities
- Varicose veins of the small pelvis
- Varicose veins of the external genital organs
- Pelvic venous congestion syndrome
- Right ovarian vein syndrome
- Varicose ovarian veins (varicoovarium)
Currently, there are 2 variants of the course of varicose veins of the small pelvis: varicose veins of the perineum and vulva, as well as pelvic venous plethora syndrome. It should be emphasized that this division is rather arbitrary, since in more than 50% of cases, varicose veins of the perineum and vulva provoke a violation of the outflow from the small pelvis, and vice versa.
Varicose veins of the perineum and vulva
Occurs in 30% of women during pregnancy. The mechanisms of this condition are basically similar to those of varicose veins of the lower extremities. At the same time, the progressive varicose transformation of the perineal veins is aggravated by the compression of the main veins of the retroperitoneal space (iliac and inferior vena cava) by the pregnant uterus. Outside of pregnancy persists in 2-10% of cases.
Pelvic Congestion Syndrome
The variety of clinical manifestations and the imperfection of diagnostics disguise it as various forms of gynecological (inflammatory diseases of the uterus and its appendages, endometriosis), urological (cystitis), surgical (colitis, Crohn's disease, etc.) and even orthopedic (diseases of the hip joint) pathology.
This disease is associated with varicose veins of the venous plexuses of the ovaries and the broad ligament of the uterus. The main mechanism is valvular insufficiency of the ovarian veins, leading to a discharge of blood and an increase in pressure in the venous plexuses of the small pelvis. Predisposing factors may be retroflexion of the uterus, leading to bending of the broad ligament of the uterus, which impedes the outflow of venous blood, as well as various gynecological diseases (endometriosis, tumors of the uterus and ovaries). In recent years, the adverse effects of hormone therapy and contraception have been discussed. The influence of the hormonal background is evidenced by the fact that the manifestations of the syndrome of venous plethora of the small pelvis in the postmenopausal period become less pronounced.
Predisposing factors may be retroflexion of the uterus, leading to bending of the broad ligament of the uterus, which impedes the outflow of venous blood, as well as various gynecological diseases (endometriosis, tumors of the uterus and ovaries). In recent years, the adverse effects of hormone therapy and contraception have been discussed. The influence of the hormonal background is evidenced by the fact that the manifestations of the syndrome of venous plethora of the small pelvis in the postmenopausal period become less pronounced.
The clinical picture of the disease is quite characteristic and manifests itself as progressive varicose veins of the perineum, vulva, vagina, lower extremities (cosmetic defect) as the duration of pregnancy increases. Signs of such violations will be:
- Itching in the area of dilated veins.
- Feeling of heaviness and arching pains in the perineum, small pelvis, swelling of the external genitalia, lower extremities.
- Dyspareunia (pain during intercourse)
- Dysmenorrhea
- Severe premenstrual syndrome
- Pain on walking and exercise
- Pain along the veins
- General pain and aches in the legs
- Dysuric disorders.

- Fatigue.
- Development of acute varicothrombophlebitis and rupture of altered veins, which is accompanied by massive bleeding.
Thrombosis during pregnancy is a major clinical problem. This is due to the high frequency of this condition as a cause of maternal mortality (20% of all causes). As you know, during pregnancy there is a tenfold increase in the risk of thrombosis. The incidence of thrombosis is 0.7-4.2/1000 in pregnant women versus 1/10,000 in non-pregnant women of childbearing age.
The critical stage of the thrombotic process is pulmonary embolism, the most severe and very often fatal complication of thrombosis. PE is the leading cause of maternal death in obstetric practice in the West - 0.7 cases per 1000 births (from 11% to 27%). The probability of venous thromboembolic complications (VTO) during caesarean section is 3-6 times higher. The risk of VTE returns to non-pregnant levels 6 weeks postpartum.
The main risk factors for WTO include the following:
- Age (> 35)
- Caesarean section
- Weight > 80 kg
- Individual and family history of thrombosis
- Repeated births
- Ovarian hyperstimulation
- Long-term immobilization
- Varicose disease
- Thrombophilia
The complexity of the treatment of WTO during pregnancy is as follows:
- Direct dependence on gestational age (safe periods of pregnancy for active treatment tactics 7-8 weeks, 13-17 weeks, 23-27 weeks)
- Difficulty in choosing the type and dosage of anticoagulant
- High chance of miscarriage and/or complications
- The need to resolve the complex issue of choice of treatment tactics
- Ethical issue of choosing to preserve life
- Compliance problem with patient and her relatives
As for varicose disease of the lower extremities during pregnancy, this problem is very extensive and ambiguous.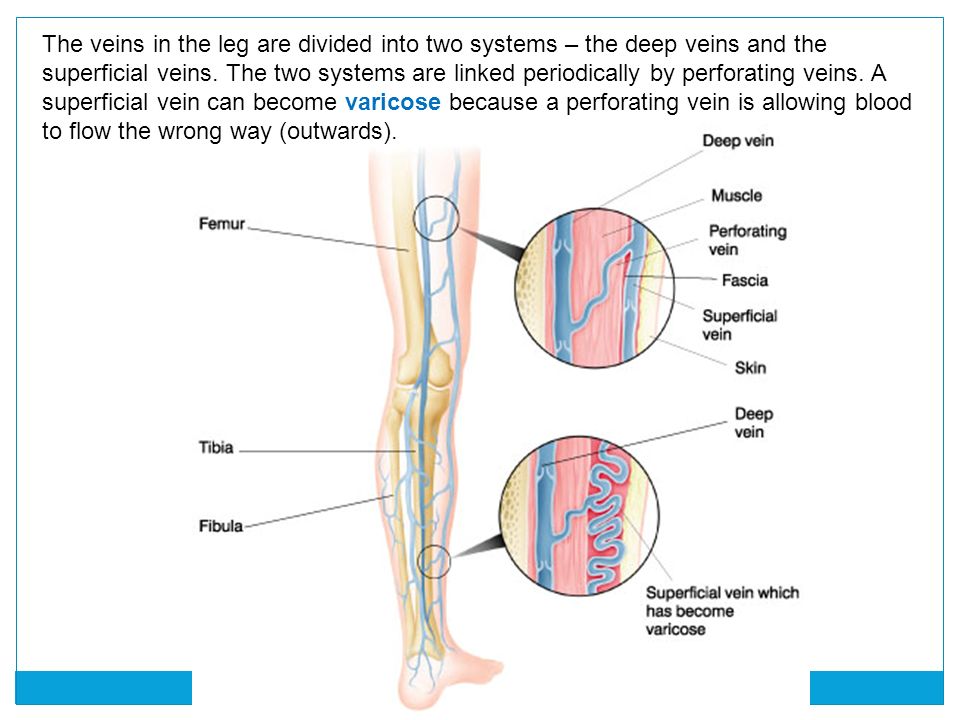 Patients with varicose veins who are planning a pregnancy should be clearly aware of the risks, adequately assess the danger that the disease carries not only for the mother, but also for the unborn child, so as not to then place all responsibility on doctors, who in this case will have very limited possibilities. Such responsibility, first of all, should lie with the parents of the unborn child. Experts always insist that varicose veins be cured before the pregnancy period, then there will be no corresponding risk.
Patients with varicose veins who are planning a pregnancy should be clearly aware of the risks, adequately assess the danger that the disease carries not only for the mother, but also for the unborn child, so as not to then place all responsibility on doctors, who in this case will have very limited possibilities. Such responsibility, first of all, should lie with the parents of the unborn child. Experts always insist that varicose veins be cured before the pregnancy period, then there will be no corresponding risk.
On the one hand, the presence of varicose veins is the main risk factor for the occurrence of WTO, i.e. There is a strong need for the prevention of such complications - surgical treatment. On the other hand, during pregnancy, the possibilities of surgical treatment are sharply limited by the safe terms of pregnancy. And if before pregnancy the patient has a fairly large choice in treatment methods, then if complications of varicose veins occur during pregnancy, such as thrombophlebitis, only a standard operation will be a possible method for removing veins, and this is general anesthesia and the need to prescribe medications, which is a direct threat to the fetus, and besides, a severe surgical injury, causing certain changes in the body, clearly not benefiting the pregnant woman and the fetus. In this case, modern low-traumatic methods of surgical treatment - EVLO and RFO will have a clear advantage, because. they do not require the use of general anesthesia and the appointment of a significant amount of medication, and also do not cause severe surgical trauma and are safe. However, in this variant, given the constant growth of the pregnant uterus and progressive changes in venous circulation with a sharp increase in pressure in the veins, the likelihood of a relapse of the disease is very high. An important factor will be certain conditions and technical possibilities for performing such an intervention.
In this case, modern low-traumatic methods of surgical treatment - EVLO and RFO will have a clear advantage, because. they do not require the use of general anesthesia and the appointment of a significant amount of medication, and also do not cause severe surgical trauma and are safe. However, in this variant, given the constant growth of the pregnant uterus and progressive changes in venous circulation with a sharp increase in pressure in the veins, the likelihood of a relapse of the disease is very high. An important factor will be certain conditions and technical possibilities for performing such an intervention.
Therefore, if a patient with varicose veins seeks help already during pregnancy, in most cases conservative methods of prevention are still prescribed, as a rule, compression therapy, taking phlebotropic drugs in safe periods of pregnancy, dynamic monitoring with an objective assessment of the condition. In the absence of complications during pregnancy, surgical treatment is prescribed after the period of breastfeeding. However, the high risk of VTO in varicose veins in pregnant women, even with compression therapy, remains, especially in the presence of several risk factors, which we mentioned above.
However, the high risk of VTO in varicose veins in pregnant women, even with compression therapy, remains, especially in the presence of several risk factors, which we mentioned above.
For example, the standard for preventing WTO in Europe in the presence of several risk factors for thrombosis, in the presence of varicose veins, is the appointment of daily injections of drugs that “thinn” the blood for the ENTIRE period of pregnancy! Is it really worth it not to operate on your varicose veins before pregnancy, using modern methods, quickly, painlessly, and then be absolutely calm both for yourself and for your unborn child ?!
So, the main measure to prevent the development of HTO in the presence of varicose veins is timely and adequate treatment (timely surgical treatment, adherence to the compression therapy regimen, correction of the rheological properties of blood and blood coagulation processes, active lifestyle).
The main simple preventive measures are as follows:
- Wear comfortable underwear;
- Limit physical activity while doing light exercise to keep fit, swimming
- Monitor nutrition by adding more fiber to the diet
- Sufficient liquid
- Walking in loose shoes, no more than 4 cm heel, comfortable, not tight clothing
- Do not take hot baths, do not go to the bathhouse, sauna
- Daily ascending contrast shower
- Active motor mode, avoid long periods of immobility, walking 2 h/d
- Perform special venous exercises
- Watch your weight
- Sleeping on the left side
- Wear compression stockings
- See a phlebologist
Given all of the above, our advice to pregnant women with varicose veins:
- wear compression stockings throughout your pregnancy;
- observe the active motor mode;
- see a phlebologist throughout pregnancy;
- strictly follow all recommendations of the specialist;
- at the first signs of deterioration - immediately seek help.