What causes blindness at birth
Severe Visual Impairment and Blindness in Infants: Causes and Opportunities for Control
Middle East Afr J Ophthalmol. 2011 Apr-Jun; 18(2): 109–114.
doi: 10.4103/0974-9233.80698
,1,2,3 and 4
Author information Copyright and License information Disclaimer
Childhood blindness has an adverse effect on growth, development, social, and economic opportunities. Severe visual impairment (SVI) and blindness in infants must be detected as early as possible to initiate immediate treatment to prevent deep amblyopia. Although difficult, measurement of visual acuity of an infant is possible. The causes of SVI and blindness may be prenatal, perinatal, and postnatal. Congenital anomalies such as anophthalmos, microphthalmos, coloboma, congenital cataract, infantile glaucoma, and neuro-ophthalmic lesions are causes of impairment present at birth. Ophthalmia neonatorum, retinopathy of prematurity, and cortical visual impairment are acquired during the perinatal period. Leukocoria or white pupillary reflex can be cause by congenital cataract, persistent hyperplastic primary vitreous, or retinoblastoma. While few medical or surgical options are available for congenital anomalies or neuro-ophthalmic disorders, many affected infants can still benefit from low vision aids and rehabilitation. Ideally, surgery for congenital cataracts should occur within the first 4 months of life. Anterior vitrectomy and primary posterior capsulotomy are required, followed by aphakic glasses with secondary intraocular lens implantation at a later date. The treatment of infantile glaucoma is surgery followed by anti-glaucoma medication. Retinopathy of prematurity is a proliferation of the retinal vasculature in response to relative hypoxia in a premature infant. Screening in the first few weeks of life can prevent blindness. Retinoblastoma can be debulked with chemotherapy; however, enucleation may still be required. Neonatologists, pediatricians, traditional birth attendants, nurses, and ophthalmologists should be sensitive to a parent’s complaints of poor vision in an infant and ensure adequate follow-up to determine the cause.
 If required, evaluation under anesthesia should be performed, which includes funduscopy, refraction, corneal diameter measurement, and measurement of intraocular pressure.
If required, evaluation under anesthesia should be performed, which includes funduscopy, refraction, corneal diameter measurement, and measurement of intraocular pressure.
Keywords: Childhood Blindness, Congenital Anomalies, Congenital Cataract, Retinopathy of Prematurity
Visual impairment and blindness in children pose a special problem for ophthalmologists, as many eye care practitioners are not familiar with performing pediatric eye examinations and measuring visual acuity in infants. Infants are unable to verbalize their complaints, and history from parents and care takers may lack important details. The first year of life is also the time when the visual system develops and binocular vision is formed.1 If a visual deficit at this age is not treated in a timely manner, amblyopia and permanent visual deficit can occur. Hence, early diagnosis and prompt treatment is essential. The burden of blindness measured in blind-person years due to childhood blindness is second only to cataract – the most common cause of avoidable blindness in childhood. 2 Studies worldwide show that many of the causes of blindness in children are either preventable or treatable (ie, avoidable).3 Even children who have visual loss that cannot be clinically treated, can be helped with low vision devices and rehabilitation. Childhood blindness affects the individual, their family, and the community. Blindness also has implications for infants’ development, education, and future social, marital, and economic prospects. Nearly 75% of early learning comes from vision. Early onset visual loss can have profound consequences on a child’s motor, social, emotional, and psychological development.4
2 Studies worldwide show that many of the causes of blindness in children are either preventable or treatable (ie, avoidable).3 Even children who have visual loss that cannot be clinically treated, can be helped with low vision devices and rehabilitation. Childhood blindness affects the individual, their family, and the community. Blindness also has implications for infants’ development, education, and future social, marital, and economic prospects. Nearly 75% of early learning comes from vision. Early onset visual loss can have profound consequences on a child’s motor, social, emotional, and psychological development.4
The World Health Organization (WHO) classifies the causes of childhood blindness according to the anatomical site most affected and the underlying etiology.5 Visual loss in infants can be either prenatal (ie, occurring at the time of conception or during the intrauterine period) or postnatal (during or after birth). Prenatal causes are congenital anomalies – anophthalmos, microphthalmos, and coloboma; congenital cataract, retinal dystrophies such as Leber’s congenital amaurosis, infantile glaucoma, and congenital cloudy cornea. In the perinatal period (ie, from the 28th week of gestation through to 1-4 weeks after birth), the following conditions can occur: cortical impairment from birth asphyxia, ophthalmia neonatorum, and retinopathy of prematurity. Postnatal conditions (ie, those acquired after birth) are unusual during infancy. As retinoblastoma can be inherited as an autosomal dominant condition, it is considered a prenatal condition for the purposes of this paper.
In the perinatal period (ie, from the 28th week of gestation through to 1-4 weeks after birth), the following conditions can occur: cortical impairment from birth asphyxia, ophthalmia neonatorum, and retinopathy of prematurity. Postnatal conditions (ie, those acquired after birth) are unusual during infancy. As retinoblastoma can be inherited as an autosomal dominant condition, it is considered a prenatal condition for the purposes of this paper.
Leukocoria may be seen in early infancy can be due to congenital cataract, retinopathy of prematurity (ROP), persistent hyperplastic primary vitreous (PHPV) – anterior or posterior – retinoblastoma or rare genetic disorders such as Norrie’s disease. A leukocoria detected by parents in later infancy may be due to developmental cataract or retinoblastoma. Retinoblastoma is the most common childhood tumor presenting at the age of 12-15 months in bilateral cases and 18-24 months in unilateral cases; it can also develop much later in childhood. It is essential to examine children presenting with leukocoria under anesthesia due to the potentially serious underlying causes.
It is essential to examine children presenting with leukocoria under anesthesia due to the potentially serious underlying causes.
Congenital anomalies
Anophthalmos and microphthalmos are congenital anomalies in which the entire eyeball is entirely absent or smaller than normal from birth. Typical complete uveal coloboma is the most common congenital anomaly in which the embryonic fissure does not close completely by the sixth week of intrauterine life. Coloboma can cause severe visual loss if the defect involves the macula and/or optic nerve. Surveys from schools for the blind in many parts of Asia show that these congenital eye anomalies are a leading cause of blindness and severe visual impairment in children.6–9 These are difficult to research, even in countries with the best healthcare systems and expertise. In the majority of cases, even with in-depth molecular genetic testing and detailed investigation, no cause can be identified.10 This is because these anomalies are likely to be due to genes controlling eye development (which are largely unknown) and possibly, gene-environment interactions, reflecting similar processes elucidated for folic acid and spina bifida.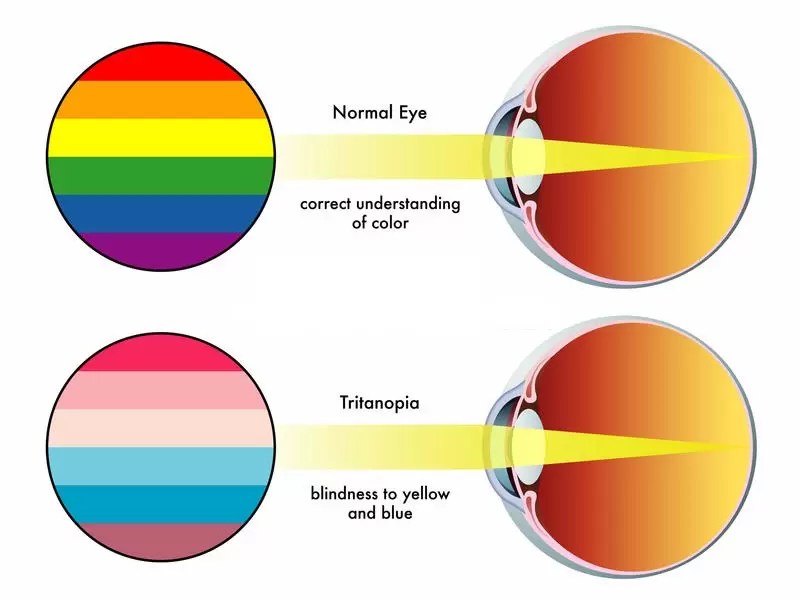 11 Even if an environmental agent (eg, folate) could be identified, the intervention would have to been extremely broad to have a measurable effect, be inexpensive and safe (as it would need to be given to large numbers of people) and be nonteratogenic – a difficult proposition in developing countries.
11 Even if an environmental agent (eg, folate) could be identified, the intervention would have to been extremely broad to have a measurable effect, be inexpensive and safe (as it would need to be given to large numbers of people) and be nonteratogenic – a difficult proposition in developing countries.
Medical therapy or surgery are rarely effective in congenital cases; however, refraction and low vision aids can help many of these cases.12 Many children with congenital defects can be taught to read print with low vision aids instead of Braille.
PHPV is a congenital anomaly in which the primary vitreous, which extends from the optic disc to the vitreous base at the posterior pole of the lens, persists into childhood.13 This anomaly can cause severe visual loss, and may be associated with microphthalmos. PHPV is usually unilateral, although bilateral cases can occur. Early vitrectomy can be attempted in eyes where the surrounding vitreous is clear and the retina fairly developed; however, the visual outcomes are often suboptimal.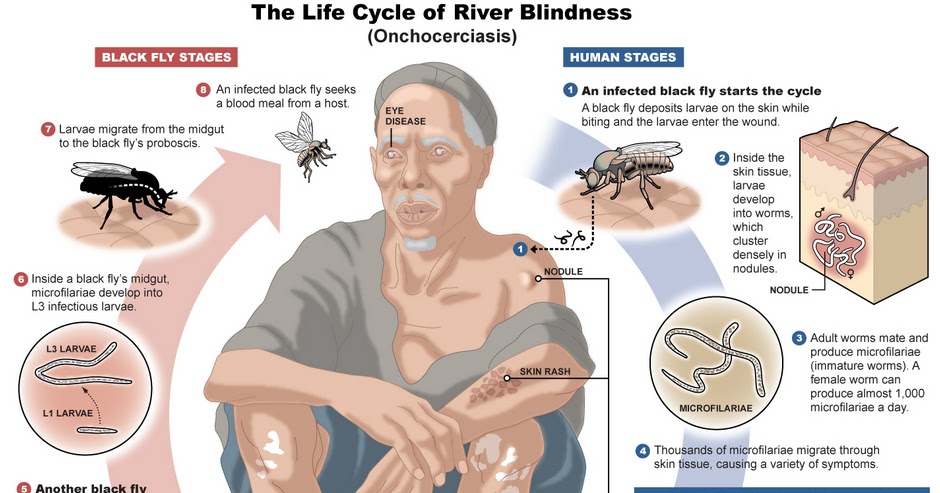 14
14
Infantile glaucoma
Infantile glaucoma can result in blindness without early intervention.15 Surgery followed by medication and optical aids is the treatment of choice. Numerous genes have been implicated and genetic counselling is essential if more than one sibling is affected.
Retinal dystrophies
Retinal dystrophies have variable genetic inheritance and are common in communities with high rates of consanguinity. Although the dystrophy may only give visual symptoms later in life, this is a common cause of blindness in children worldwide, particularly in Middle Eastern countries.16,17 Low vision aids are effective for navigation and reading for individuals affected with retinal dystrophies. Genetic counselling is required if more than one sibling is involved.
Leber’s congenital amaurosis is an autosomal recessive condition that manifests in infancy. The fundus may be normal or show peripheral chorioretinal atrophy and granularity with nystagmus.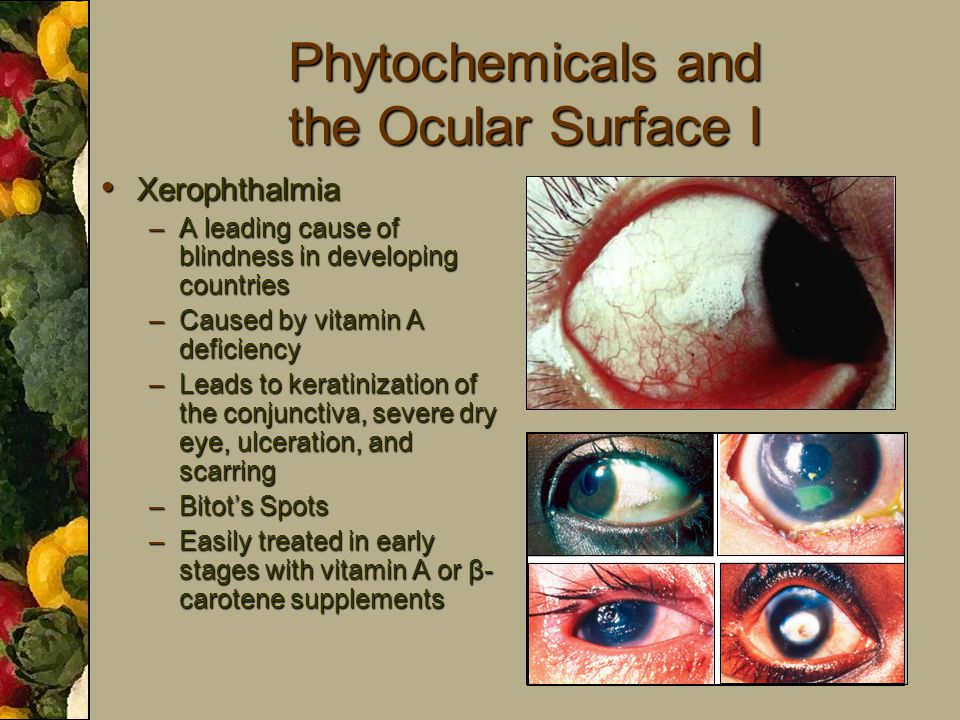 Oculodigital syndrome, in which the infant constantly rubs or presses on the eyes, which leads to enophthalmos, is common. Other common features include learning disability, deafness, and epilepsy. In Knobloch syndrome nystagmus, high myopia and late retinal detachment are seen. Oculocutaneous albinism, which may be X-linked or autosomal recessive, is detectable at birth. Ocular albinism affects only male infants due to the X-linked inheritance and is usually diagnosed at infancy. Achromatopsy is a rare autosomal recessive heterogeneous group of stationary retinal dystrophies characterized by reduced central vision, poor color vision, and normal fundus. The usual presentation is reduced vision, marked photophobia, and nystagmus in infancy. A macular cherry red spot could be due to Tay-Sachs disease, which is fatal by the second year of life or due to Niemann-Pick disease or Sandhoff disease.
Oculodigital syndrome, in which the infant constantly rubs or presses on the eyes, which leads to enophthalmos, is common. Other common features include learning disability, deafness, and epilepsy. In Knobloch syndrome nystagmus, high myopia and late retinal detachment are seen. Oculocutaneous albinism, which may be X-linked or autosomal recessive, is detectable at birth. Ocular albinism affects only male infants due to the X-linked inheritance and is usually diagnosed at infancy. Achromatopsy is a rare autosomal recessive heterogeneous group of stationary retinal dystrophies characterized by reduced central vision, poor color vision, and normal fundus. The usual presentation is reduced vision, marked photophobia, and nystagmus in infancy. A macular cherry red spot could be due to Tay-Sachs disease, which is fatal by the second year of life or due to Niemann-Pick disease or Sandhoff disease.
Congenital cataract
The birth prevalence of cataract is 3-5/1,000 live births.18 While monogenetic abnormalities, syndromes, metabolic disorders, genetic disorders, and congenital rubella syndrome are recognized causes of this condition, in the majority, the cause is unknown.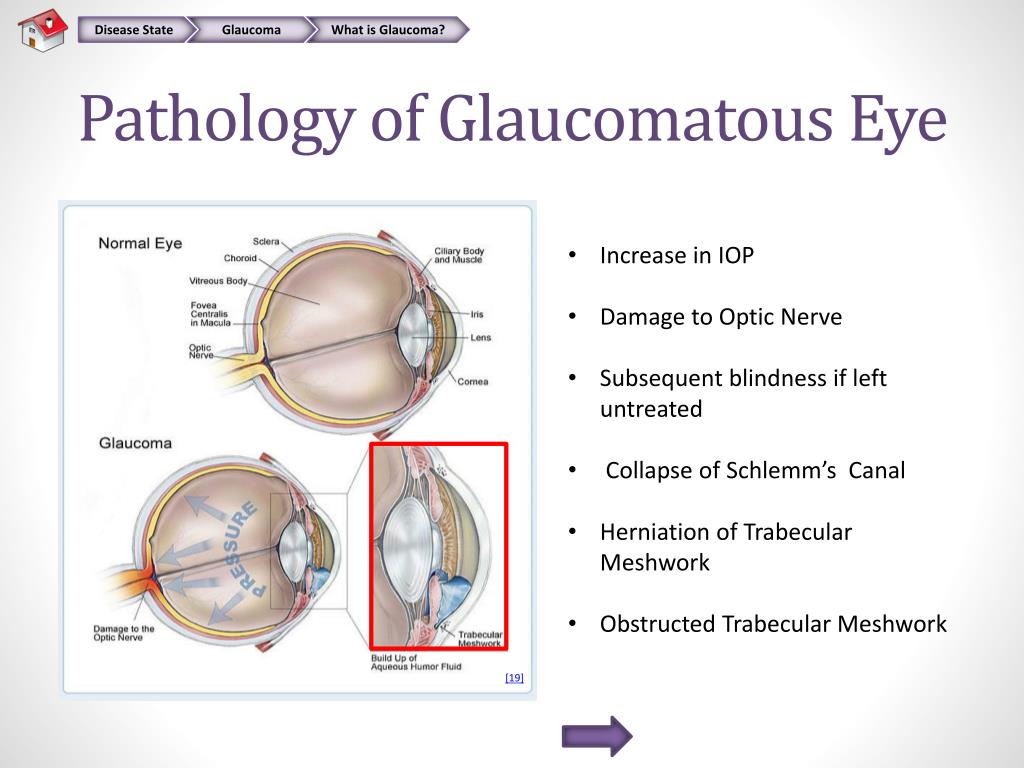 19 The importance of congenital cataract is increasing as a cause of blindness among children in developing countries, with other causes declining. There can be 2 years delay from cataract diagnosis to presentation for surgery.20 Early recognition and referral is essential to prevent development of dense amblyopia. However, the timing of intraocular lens (IOL) implantation remains controversial.21 Many experienced surgeons are implanting IOLs in very young children, ie, 12 months or older. While children with unilateral cataract have undergone IOL implantation at as early as 6 months of age, it is better to wait until 2 years of age for implanting IOLs in children with bilateral cataracts.21,22 In \ children where the risk of general anesthesia very high, bilateral surgery at the same visit is advisable; however, this should be an exception rather than the rule. There is almost a hundred percent posterior capsular opacification in pediatric eyes.
19 The importance of congenital cataract is increasing as a cause of blindness among children in developing countries, with other causes declining. There can be 2 years delay from cataract diagnosis to presentation for surgery.20 Early recognition and referral is essential to prevent development of dense amblyopia. However, the timing of intraocular lens (IOL) implantation remains controversial.21 Many experienced surgeons are implanting IOLs in very young children, ie, 12 months or older. While children with unilateral cataract have undergone IOL implantation at as early as 6 months of age, it is better to wait until 2 years of age for implanting IOLs in children with bilateral cataracts.21,22 In \ children where the risk of general anesthesia very high, bilateral surgery at the same visit is advisable; however, this should be an exception rather than the rule. There is almost a hundred percent posterior capsular opacification in pediatric eyes.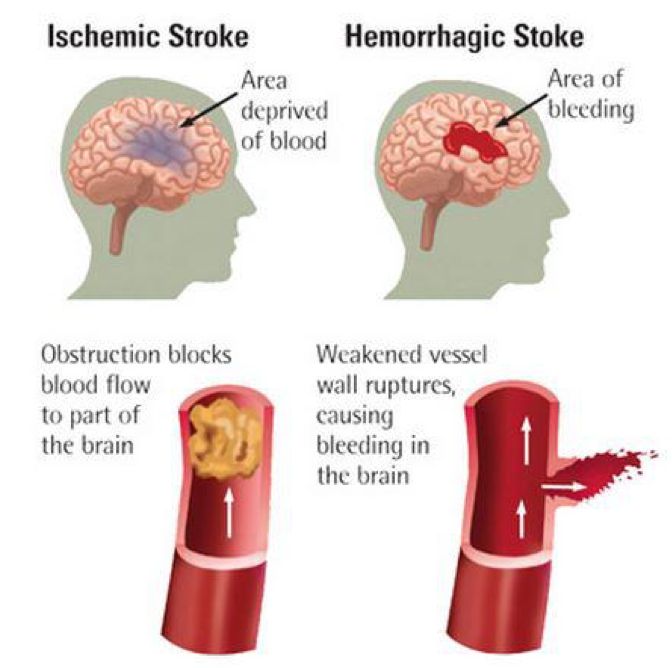 Experts recommend primary posterior capsulotomy and anterior vitrectomy in children up to the age of 6-7 years. At 6 years or older, the child can sit on a slit lamp for Nd:YAG laser capsulotomy after surgery, if required.21 The anterior vitrectomy removes the almost solid vitreous base, which can act as a scaffold for migrating lenticular cells. The pars plana approach has the advantage of keeping the primary incision and the anterior chamber free of vitreous, but this is technically demanding for anterior segment surgeons. Moreover, there is an exaggerated fear of suprachoroidal hemorrhage.23 Vitrectomy through limbal side ports is easier but the surgeon has to be meticulous in removing vitreous from the anterior chamber. The primary posterior capsulotomy can be performed before or after inserting the intraocular lens. There is a risk of the capsulotomy extending during the implantation of a foldable lens. An MVR blade may be used to make a ’nick’ below the implanted lens to later enlarge the opening with a vitrectors.
Experts recommend primary posterior capsulotomy and anterior vitrectomy in children up to the age of 6-7 years. At 6 years or older, the child can sit on a slit lamp for Nd:YAG laser capsulotomy after surgery, if required.21 The anterior vitrectomy removes the almost solid vitreous base, which can act as a scaffold for migrating lenticular cells. The pars plana approach has the advantage of keeping the primary incision and the anterior chamber free of vitreous, but this is technically demanding for anterior segment surgeons. Moreover, there is an exaggerated fear of suprachoroidal hemorrhage.23 Vitrectomy through limbal side ports is easier but the surgeon has to be meticulous in removing vitreous from the anterior chamber. The primary posterior capsulotomy can be performed before or after inserting the intraocular lens. There is a risk of the capsulotomy extending during the implantation of a foldable lens. An MVR blade may be used to make a ’nick’ below the implanted lens to later enlarge the opening with a vitrectors. 23 A-scan biometry and keratometry need to be performed under anesthesia. Hydrophobic acrylic or poly-methyl-methacrylate IOLs are best for infants. Generally, the target postoperative refraction is emmetropia by the age of 5-6 years. Aphakic glasses have to be corrected for near vision.
23 A-scan biometry and keratometry need to be performed under anesthesia. Hydrophobic acrylic or poly-methyl-methacrylate IOLs are best for infants. Generally, the target postoperative refraction is emmetropia by the age of 5-6 years. Aphakic glasses have to be corrected for near vision.
Pediatric cataract surgery is one step in a series of interventions required to rehabilitate vision.24 Postoperative management includes frequent steroid eye drops with cycloplegia, followed by early, accurate, and repeated refractions and treatment of amblyopia by patching the better seeing eye. Late complications of pediatric IOL implantation include opacification of the visual axis and glaucoma, the latter being particularly difficult to treat. Parents must be counselled about the need for regular ophthalmic examination, refraction, and intraocular pressure measurement. It is important to remember that aphakic/pseudophakic children need correction for near as well as distance, and many are able to tolerate executive bifocals very well.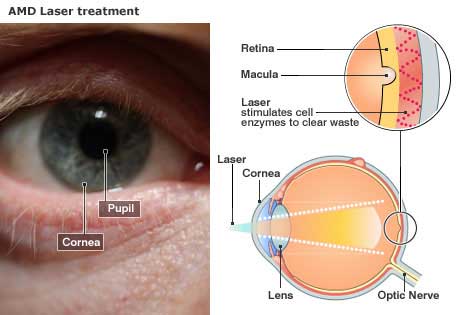 21,24
21,24
Retinoblastoma
Retinoblastoma is the most common intraocular malignancy in early childhood. It usually presents after infancy as leukocoria, esotropia, or masquerades as uveitis. Lesions detected early can be treated with chemotherapy with preservation of the globe; however, larger lesions may need enucleation.25,26 A prosthesis needs to be implanted in the child’s eye to prevent the contracture of the socket. A mule’s implant wrapped in a sclera shell or dermal fat grafts may be used for this purpose. Management with specialist tertiary oncology services is also advisable.
Ophthalmia neonatorum
This is an eminently preventable condition in which the eyes of the infant become infected in the birth passage during delivery. Credé’s prophylaxis and antenatal testing or treatment of sexually transmitted diseases during pregnancy can prevent the condition. Credé’s prophylaxis entails cleaning the infants’ eyes immediately after birth with instillation of a topical antibiotic (eg, tetracycline eye ointment) or antiseptic (eg, 2. 5% povidone iodine). Traditionally, a 2% solution of silver nitrate was used for Credé’s prophylaxis. The agent used depends on the local epidemiology of sexually transmitted diseases and the organism’s sensitivity to antibiotics. Treatment of ophthalmia neonatorum must entail systemic as well as topical treatment, to ensure treatment of extraocular sites of infection (eg, pneumonia).
5% povidone iodine). Traditionally, a 2% solution of silver nitrate was used for Credé’s prophylaxis. The agent used depends on the local epidemiology of sexually transmitted diseases and the organism’s sensitivity to antibiotics. Treatment of ophthalmia neonatorum must entail systemic as well as topical treatment, to ensure treatment of extraocular sites of infection (eg, pneumonia).
Retinopathy of prematurity
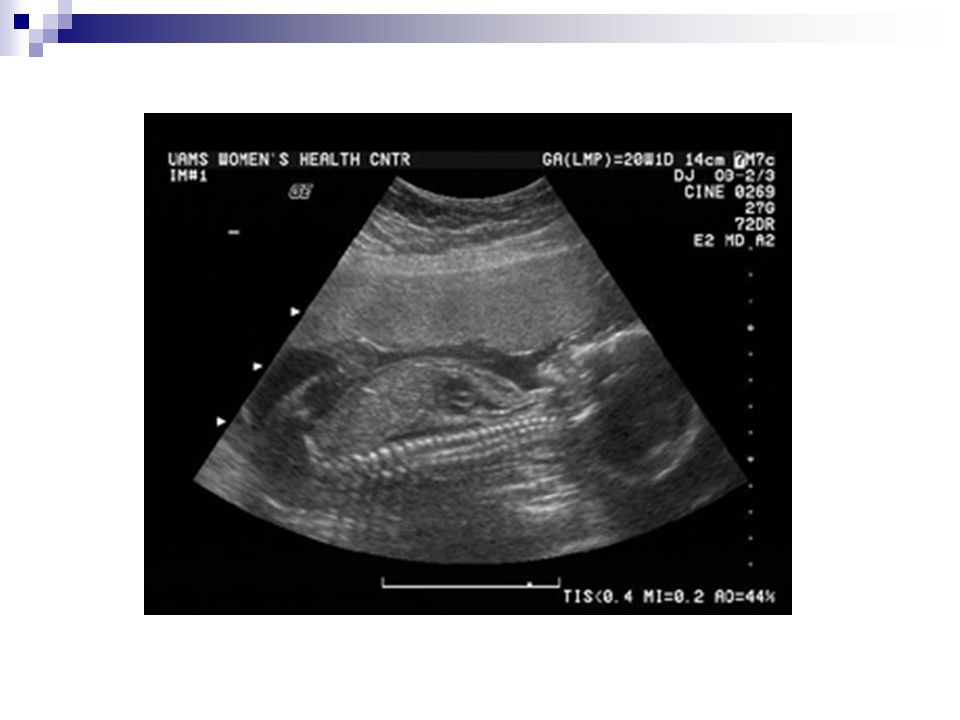
Retinopathy of prematurity (ROP) is responsible for up to 15% of all causes of blindness in developed countries and up to 60% in middle income countries.27 A number of risk factors are implicated in the development of ROP. However, the most commonly identified risk factors are the degree of immaturity measured by birth weight (BW), gestational age (GA), and prolonged exposure to supplementary oxygen.28 Paradoxically, the hyperbaric oxygen that saves an infant’s life, if not properly controlled and tapered, can cause blindness. There are several trials seeking to define safe upper and lower limits of arterial oxygen saturation.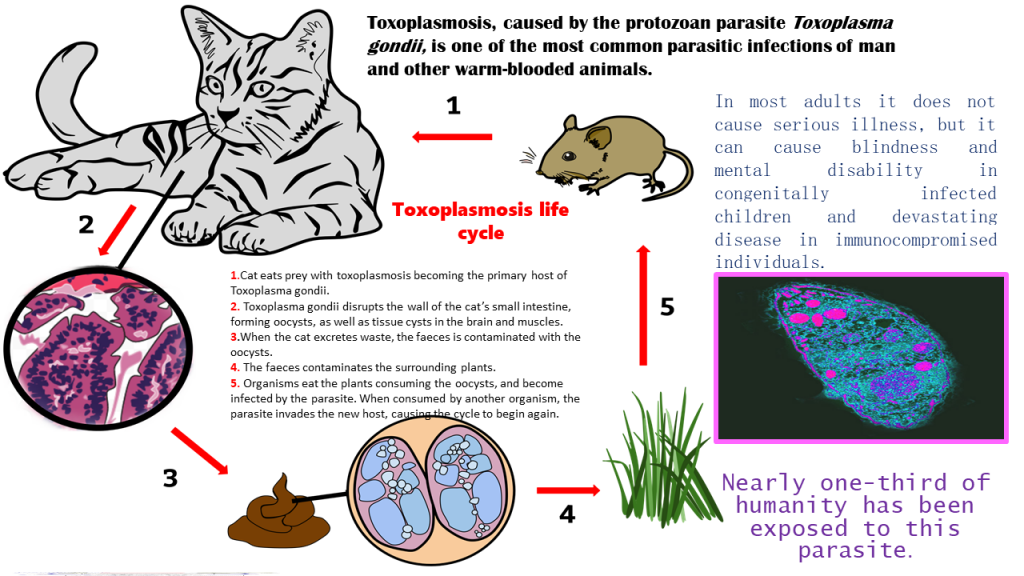 29 The improvement in neonatal care can lead to an increase in survival rates of premature infants in middle-income countries and major metropolises of even poorer countries. As a consequence, ROP has become a very important cause of childhood in these developing economies, where quality of neonatal care still needs to improve. The disease is classified by severity (stages I-V), by site (zones 1-3), and by extent (clock hours 1-12). While most developed countries screen infants by BW < 1,500 g,30 middle income and developing countries need larger BW criteria as infants weighing up to 2,500 g are developing severe ROP.31,32 Appropriate screening protocols ensure early detection in the first weeks of life so that treatment (peripheral ablation of avascular retina) with laser or cryotherapy can be provided. So far, there is no evidence provided by clinical trials that surgery is beneficial for cases in stages IV and V. Anti-vascular endothelial growth factors (VEGFs) are promising drugs for treatment of retinal proliferative diseases in adults.
29 The improvement in neonatal care can lead to an increase in survival rates of premature infants in middle-income countries and major metropolises of even poorer countries. As a consequence, ROP has become a very important cause of childhood in these developing economies, where quality of neonatal care still needs to improve. The disease is classified by severity (stages I-V), by site (zones 1-3), and by extent (clock hours 1-12). While most developed countries screen infants by BW < 1,500 g,30 middle income and developing countries need larger BW criteria as infants weighing up to 2,500 g are developing severe ROP.31,32 Appropriate screening protocols ensure early detection in the first weeks of life so that treatment (peripheral ablation of avascular retina) with laser or cryotherapy can be provided. So far, there is no evidence provided by clinical trials that surgery is beneficial for cases in stages IV and V. Anti-vascular endothelial growth factors (VEGFs) are promising drugs for treatment of retinal proliferative diseases in adults.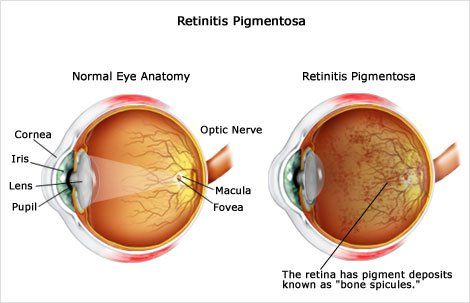 However, extreme caution is warranted in infants, as these drugs interfere with the normal development of vasculature elsewhere in the body and may impede development of the lungs and alveoli of the lungs, which are VEGF-sensitive and develop at the same time as does ROP.33 Premature infants are at increased risk of developing refractive errors, strabismus, amblyopia, and low vision; hence, long-term follow-up is recommended.
However, extreme caution is warranted in infants, as these drugs interfere with the normal development of vasculature elsewhere in the body and may impede development of the lungs and alveoli of the lungs, which are VEGF-sensitive and develop at the same time as does ROP.33 Premature infants are at increased risk of developing refractive errors, strabismus, amblyopia, and low vision; hence, long-term follow-up is recommended.
Optic nerve lesions and cerebral visual impairment
Optic nerve lesions and cerebral visual impairment are the most common causes of visual impairment in many developed countries34 where these are often a consequence of preterm birth.35 Birth asphyxia, which causes cerebral palsy, may affect the optic nerve and cause cortical visual impairment. Little can be done by way of medical treatment. Low vision aids and rehabilitation are often the only recourse. Often, such children are severely handicapped, which makes assessment and management even more challenging.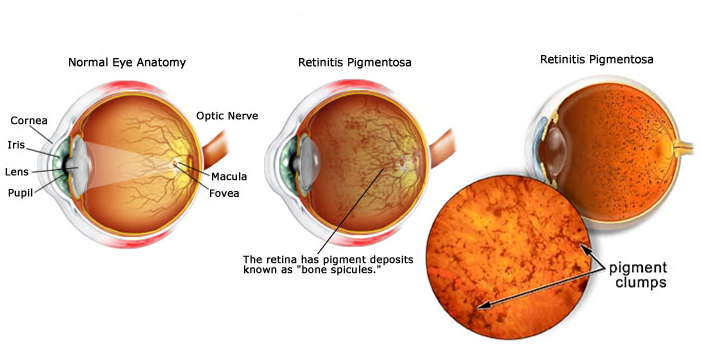
Keratomalacia cause by acute deficiency of vitamin A is very unusual in the first year of life, and most infants before the age of 9 months (when they are immunized) will have protective measles antibodies received from their mother. The common causes of blindness in childhood such as vitamin A deficiency, measles, trauma, and trachoma are uncommon in infancy. Unless the refractive error is very large [>3-4 diopter (D)], or is causing strabismus, spectacles are not required in infants. However, if the infant has low vision, even small refractive errors may need correction.
While evaluation of a visually impaired infant may seem challenging for the general ophthalmologist, the task is not that difficult. Infants are best examined in the position they are most comfortable – on their parents’ shoulders, in their laps, or cribs. We recommend not making the infant and parents wait in a busy waiting area. A separate area for breastfeeding is welcome, as this puts the mother and child at ease.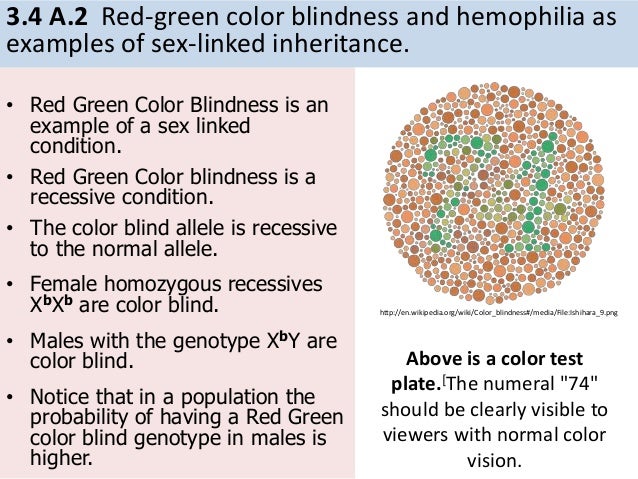 The infant can be examined for fixating and following of the flashlight. The ophthalmologist should also have a quick look at the cornea, anterior chamber, lens, and pupillary reflex. A handheld slit lamp is the best instrument for this component of the evaluation. The red reflex should be examined to rule out congenital cataract, advanced ROP, and other causes of leukocoria. If the child is uncooperative or distressed, the examination can be repeated after a few hours or next day after instilling atropine eye ointment to dilate the pupil. However, the drug may affect the pupil for a week. Cyclopentolate 0.1%, tropicamide 0.1%, and phenylephrine 2.5% eye drops may also be instilled, though there is a risk of toxicity due to systemic absorption. Cyclopentolate and tropicamide are parasympatholytic agents acting on sphincter pupillae, whereas phenylephrine is sympathomimetic acting on the dilator papillae muscle. The child can also be given 2.5 ml of phenergan syrup (properazine – a mild sedative and antihistamine combination) and then breastfed to lull it into sleep.
The infant can be examined for fixating and following of the flashlight. The ophthalmologist should also have a quick look at the cornea, anterior chamber, lens, and pupillary reflex. A handheld slit lamp is the best instrument for this component of the evaluation. The red reflex should be examined to rule out congenital cataract, advanced ROP, and other causes of leukocoria. If the child is uncooperative or distressed, the examination can be repeated after a few hours or next day after instilling atropine eye ointment to dilate the pupil. However, the drug may affect the pupil for a week. Cyclopentolate 0.1%, tropicamide 0.1%, and phenylephrine 2.5% eye drops may also be instilled, though there is a risk of toxicity due to systemic absorption. Cyclopentolate and tropicamide are parasympatholytic agents acting on sphincter pupillae, whereas phenylephrine is sympathomimetic acting on the dilator papillae muscle. The child can also be given 2.5 ml of phenergan syrup (properazine – a mild sedative and antihistamine combination) and then breastfed to lull it into sleep. This allows more detailed fundus and external ocular evaluation, and measurement of intraocular pressure by non-contact or Perkins (more accurate) tonometer. If a serious lesion such as retinoblastoma is suspected, an evaluation under anesthesia is essential for detailed examination of the fundus. The opportunity must be utilized not just to examine the fundus but to also perform tonometry, refraction, measurement of corneal diameter, and axial length.
This allows more detailed fundus and external ocular evaluation, and measurement of intraocular pressure by non-contact or Perkins (more accurate) tonometer. If a serious lesion such as retinoblastoma is suspected, an evaluation under anesthesia is essential for detailed examination of the fundus. The opportunity must be utilized not just to examine the fundus but to also perform tonometry, refraction, measurement of corneal diameter, and axial length.
Orthoptic evaluation of an infant requires patience. Jampolsky’s dictum of “one toy-one look” should be used to examine the infant’s ocular motility in the nine cardinal directions of gaze. An assortment of soft toys, brightly colored objects, and even mobile phones can be used to arouse the child’s interest. The objects should not make noise as the child will be attracted through the auditory and not the visual signals, which would defeat the purpose of the examination. Visual acuity can be formally assessed using forced preferential looking tests (eg, Cardiff cards), with the child sitting comfortably on a parent’s lap.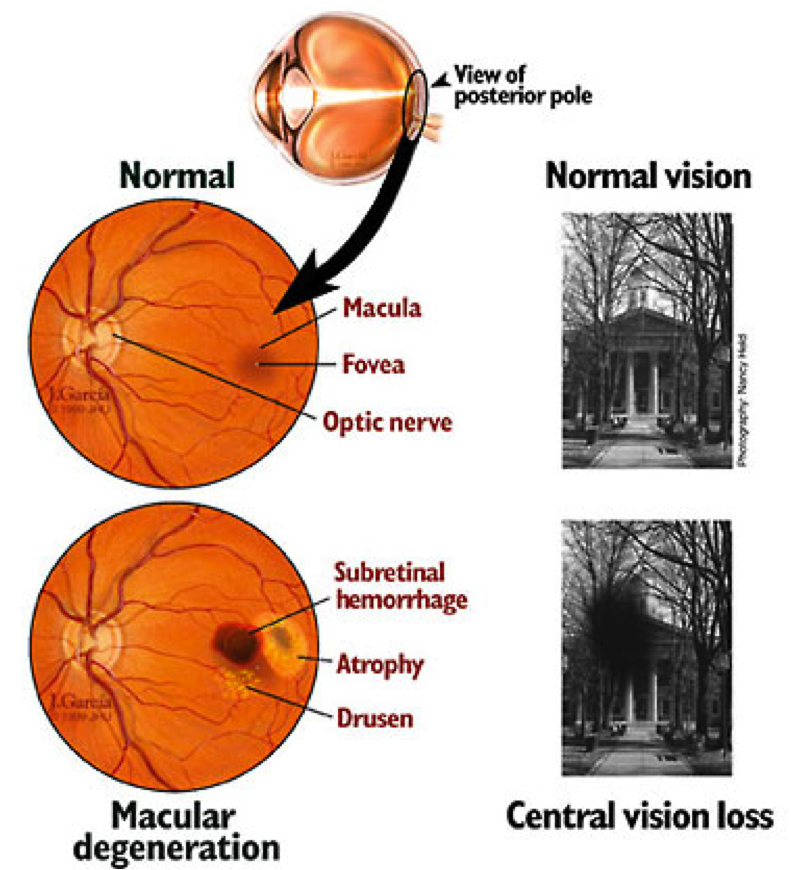 The test is based on the psychological percept that humans are attracted to novel stimuli. If the child is shown a line drawing at one end of the card sheet and the other end is kept blank, the child will divert its eyes to the drawing rather than the blank area. The line drawings are made progressively finer to estimate higher orders of form vision. Worth’s ivory fall test and small sweets commonly used to decorate cakes, “hundreds and thousands”, can also be used. The child picks up the small sweets if it is able to see them. At first, bilateral vision is tested followed by monocular testing. The mother should be asked to occlude the infant’s eyes one at a time, and report on the infant’s response. If the infant objects to occlusion of one eye, this may indicate the visual acuity of the other eye is poor.
The test is based on the psychological percept that humans are attracted to novel stimuli. If the child is shown a line drawing at one end of the card sheet and the other end is kept blank, the child will divert its eyes to the drawing rather than the blank area. The line drawings are made progressively finer to estimate higher orders of form vision. Worth’s ivory fall test and small sweets commonly used to decorate cakes, “hundreds and thousands”, can also be used. The child picks up the small sweets if it is able to see them. At first, bilateral vision is tested followed by monocular testing. The mother should be asked to occlude the infant’s eyes one at a time, and report on the infant’s response. If the infant objects to occlusion of one eye, this may indicate the visual acuity of the other eye is poor.
There is a narrow window of opportunity in treating a visually impaired infant. Binocular single vision develops by 6 months of life and a visual deficit, if not detected and treated in time, may leave the child bereft of stereopsis.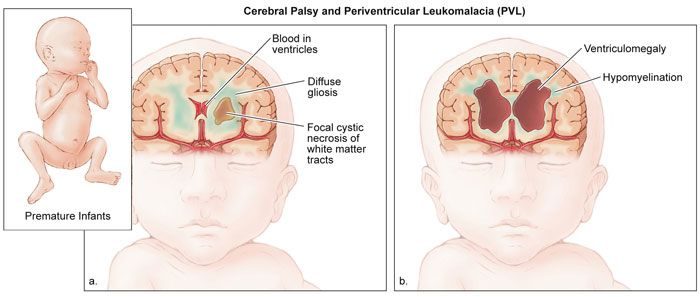 The amblyopia that develops from visual deprivation of early onset, irrespective of the cause, can be dense and difficult to treat.
The amblyopia that develops from visual deprivation of early onset, irrespective of the cause, can be dense and difficult to treat.
Pediatricians, general practitioners, and midwives should be educated and encouraged to perform the red reflex test. Using the direct ophthalmoscope, they should be taught to detect any opacity seen in the infant’s red reflex. All healthcare personnel working for the care of the infant should be sensitized to the eye conditions in infancy and on the causes of childhood blindness and visual impairment. Their training curricula should emphasize on the importance of early detection and treatment of such children. Training of midwives, traditional birth attendants, healthcare workers working for child health and immunization would be of immense help in early detection of such children.
The major barrier to accessing eye care services for infants is the absence of trained personnel who can diagnose a problem early. Developed countries have established referral systems between family practitioners, health visitors, neonatal units, and pediatric ophthalmology and retina specialist. However, pediatric eye care centers are rare in developing countries. There are financial and geographic barriers for many parents from poorer communities. Diagnostic, curative, and rehabilitative services may not be available in the region. Pediatric eye care interventions are also more expensive than adult treatment. For example, general anesthesia is often required for examination and treatment. This entails liaison with other medical practitioners such as pediatricians, anesthetists, and neonatologists. Another significant barrier is the lack of knowledge on the part of healthcare providers. Many healthcare workers, including physicians ask parents to wait until the child is older before any treatment can be given. Some physicians are unsure about what needs to be done. Others believe that the problem may resolve, as the child grows older or that a unilateral condition does not matter as long as the other eye is healthy. Due to these misconceptions, appropriate referral may too late if dense amblyopia has occurred.
However, pediatric eye care centers are rare in developing countries. There are financial and geographic barriers for many parents from poorer communities. Diagnostic, curative, and rehabilitative services may not be available in the region. Pediatric eye care interventions are also more expensive than adult treatment. For example, general anesthesia is often required for examination and treatment. This entails liaison with other medical practitioners such as pediatricians, anesthetists, and neonatologists. Another significant barrier is the lack of knowledge on the part of healthcare providers. Many healthcare workers, including physicians ask parents to wait until the child is older before any treatment can be given. Some physicians are unsure about what needs to be done. Others believe that the problem may resolve, as the child grows older or that a unilateral condition does not matter as long as the other eye is healthy. Due to these misconceptions, appropriate referral may too late if dense amblyopia has occurred.
Even when the infant has been referred for treatment appropriately, many parents believe that their infant is too small to undergo surgery or wear spectacles and, in some communities, visual loss in infants is not considered a priority for the family, especially for females.
However, a child who cannot be helped by medicine or surgery may still benefit from use of spectacles and/or low vision aids. Completely and irreversibly blind children can benefit by rehabilitation and special school education. This should be emphasized during parent counselling. Ophthalmologists should be nonjudgmental and empathetic while breaking the news about a potentially blinding condition. Ocular conditions, which have a genetic or familial basis, may be blamed on one of the parents. The ophthalmologist should spend some time with the parents to reassure, counsel, and suggest various alternatives that are available for the infant. It may take the parents some time to come to terms with their child’s visual loss. Frequent ophthalmic visits to confirm the level of vision and make a definitive diagnosis can be difficult for parents. A social worker or counsellor can establish a rapport with the parents or caretakers to ensure that they comply with the treatment as much as possible.
Frequent ophthalmic visits to confirm the level of vision and make a definitive diagnosis can be difficult for parents. A social worker or counsellor can establish a rapport with the parents or caretakers to ensure that they comply with the treatment as much as possible.
Blindness and severe visual impairment in infants is not that difficult to detect and diagnose. With proper care, most of these infants can be helped and formation of dense amblyopia prevented. Even if the ophthalmologist may not be able to help medically or surgically, optical aids and rehabilitation can help children reach their full capacity.
Source of Support: Nil
Conflict of Interest: None declared.
1. Day S. Normal and abnormal visual development. In: David T, editor. Pediatric ophthalmology. Section 1. Chapter 2. Oxford UK: Blackwell Science; 1997. pp. 13–28. [Google Scholar]
2. Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. [PMC free article] [PubMed] [Google Scholar]
Br J Ophthalmol. 1999;83:387–8. [PMC free article] [PubMed] [Google Scholar]
3. Gilbert C, Rahi JS, Quinn GE. Visual impairment and blindness in children. In: Jhonson GJ, Minassian D, Weale RA, West SK, editors. Epidemiology of Eye Disease. 2nd ed. London: Arnold publishers; 2003. pp. 260–86. [Google Scholar]
4. Dale N, Salt A. Early support developmental journal for children with visual impairment: The case for a new developmental framework for early intervention. Child Care Health Dev. 2007;33:684–90. [PubMed] [Google Scholar]
5. Gilbert C, Foster A, Negrel AD, Thylefors B. Childhood blindness: A new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71:485–9. [PMC free article] [PubMed] [Google Scholar]
6. Gogate P, Deshpande M, Sudrik S, Kishore H, Taras S, Deshpande M. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. [PMC free article] [PubMed] [Google Scholar]
7. Njuguna M, Msukwa G, Shilio B, Tumwesigye C, Courtright P, Lewallen S. Causes of severe visual impairment and blindness in children in schools for the blind in eastern Africa: Changes in the last 14 years. Ophthalmic Epidemiol. 2009;16:151–5. [PubMed] [Google Scholar]
Causes of severe visual impairment and blindness in children in schools for the blind in eastern Africa: Changes in the last 14 years. Ophthalmic Epidemiol. 2009;16:151–5. [PubMed] [Google Scholar]
8. Gogate P, Kishore H, Dole K, Shetty J, Gilbert C, Ranade S, et al. The pattern of childhood blindness in Karnataka, South India. Ophthalmic Epidemiol. 2009;16:212–7. [PubMed] [Google Scholar]
9. Sitorus RS, Abidin MS, Prihartono J. Causes and temporal trends of childhood blindness in Indonesia: Study at schools for the blind in Java. Br J Ophthalmol. 2007;91:1109–13. [PMC free article] [PubMed] [Google Scholar]
10. Shah SP, Taylor AE, Sowden JC, Ragge NK, Russell-Eggitt I, Rahi JS, et al. Anophthalmos, micophthalmos and typical coloboma in the United Kingdom: A prospective study of incidence and risk. Invest Ophthalmol Vis Sci. 2011;52:558–64. [PubMed] [Google Scholar]
11. Hornby SJ, Ward SJ, Gilbert CE. Hypothesis: Eye birth defects in humans may be caused by a recessively-inherited genetic predisposition to the effects of maternal vitamin A deficiency during pregnancy.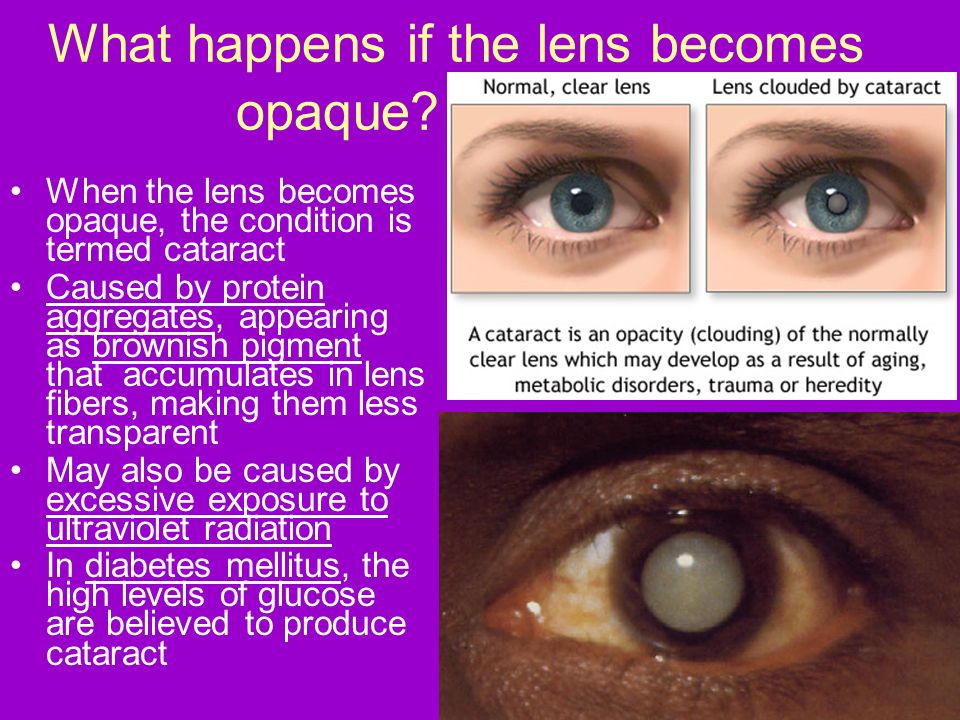 Med Sci Monit. 2003;9:HY23–6. [PubMed] [Google Scholar]
Med Sci Monit. 2003;9:HY23–6. [PubMed] [Google Scholar]
12. Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Requirements for optical services in children with microphthalmos, coloboma and microcornea in southern India. Eye. 2000;14:219–24. [PubMed] [Google Scholar]
13. Shastry BS. Persistent hyperplastic primary vitreous: Congenital malformation of the eye. Clin Exp Ophthalmol. 2009;37:884–90. [PubMed] [Google Scholar]
14. Walsh MK, Drenser KA, Capone A, Jr, Trese MT. Early vitrectomy effective for bilateral combined anterior and posterior persistent fetal vasculature syndrome. Retina. 2010;30:S2–8. [PubMed] [Google Scholar]
15. Mandal AK, Bhatia PG, Bhaskar A, Nutheti R. Long-term surgical and visual outcomes in Indian children with developmental glaucoma operated on within 6 months of birth. Ophthalmology. 2004;111:283–90. [PubMed] [Google Scholar]
16. Kotb AA, Hammouda EF, Tabbara KF. Childhood blindness at a school for the blind in Riyadh, Saudi Arabia. Ophthalmic Epidemiol. 2006;13:1–5. [PubMed] [Google Scholar]
Ophthalmic Epidemiol. 2006;13:1–5. [PubMed] [Google Scholar]
17. Cetin E, Yaman A, Berk AT. Etiology of childhood blindness in Izmir, Turkey. Eur J Ophthalmol. 2004;14:531–7. [PubMed] [Google Scholar]
18. Rahi JS, Dezateux C. British Congenital Cataract Interest Group. Measuring and interpreting the incidence of congenital ocular anomalies: Lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci. 2001;42:1444–8. [PubMed] [Google Scholar]
19. Rahi JS, Dezateux C. Congenital and infantile cataract in the United Kingdom: Underlying or associated factors. British Congenital Cataract Interest Group. Invest Ophthalmol Vis Sci. 2000;41:2108–14. [PubMed] [Google Scholar]
20. Mwende J, Bronsard A, Mosha M, Bowman R, Geneau R, Courtright P. Delay in presentation to hospital for surgery for congenital and developmental cataract in Tanzania. Br J Ophthalmol. 2005;89:1478–82. [PMC free article] [PubMed] [Google Scholar]
21. Wilson ME, Pandey SK, Thakur J. Paediatric cataract blindness in the developing world: Surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol. 2003;87:14–9. [PMC free article] [PubMed] [Google Scholar]
Paediatric cataract blindness in the developing world: Surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol. 2003;87:14–9. [PMC free article] [PubMed] [Google Scholar]
22. Ram J, Brar GS, Kaushik S, Sukhija J, Bandyopadhyay S, Gupta A. Primary intraocular lens implantation in the first two years of life: safety profile and visual results. Indian J Ophthalmol. 2007;55:185–9. [PubMed] [Google Scholar]
23. Gogate P. Complications of pediatric cataract surgery. Highlights Ophthalmol. 2009;37:12–5. [Google Scholar]
24. Gogate P, Khandekar R, Srisimal M, Dole K, Taras S, Kulkarni S, et al. Cataracts with delayed presentation. Are they worth operating upon? Ophthalmic Epidemiol. 2010;17:25–33. [PubMed] [Google Scholar]
25. Shields CL, Honavar SG, Meadows AT, Shields JA, Demirci H, Naduvilath TJ. Chemoreduction for unilateral retinoblastoma. Arch Ophthalmol. 2002;120:1653–8. [PubMed] [Google Scholar]
26. Honavar SG. Emerging options in the management of advanced intraocular retinoblastoma. Br J Ophthalmol. 2009;93:848–9. [PubMed] [Google Scholar]
Br J Ophthalmol. 2009;93:848–9. [PubMed] [Google Scholar]
27. Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, et al. ; For the International NO-ROP Group. Characteristics of babies with severe retinopathy of prematurity in countries with low, moderate and high levels of development: Implications for screening programmes. Pediatrics. 2005;115:e518–25. [PubMed] [Google Scholar]
28. McColm JR, Fleck BW. Retinopathy of prematurity: Causation. Semin Neonatol. 2001;6:453–60. [PubMed] [Google Scholar]
29. Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Support Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1970–9. [PMC free article] [PubMed] [Google Scholar]
30. Wilkinson AR, Haines L, Head K, Fielder AR. UK retinopathy of prematurity guideline. Early Hum Dev. 2008;84:71–4. [PubMed] [Google Scholar]
31. Vinekar A, Dogra MR, Sangtam T, Narang A, Gupta A. Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: Ten year data from a tertiary care center in a developing country. Indian J Ophthalmol. 2007;55:331–6. [PMC free article] [PubMed] [Google Scholar]
Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: Ten year data from a tertiary care center in a developing country. Indian J Ophthalmol. 2007;55:331–6. [PMC free article] [PubMed] [Google Scholar]
32. Shah PK, Narendran V, Kalpana N, Gilbert C. Severe retinopathy of prematurity in big babies in India: History repeating itself? Indian J Pediatr. 2009;76:801–4. [PubMed] [Google Scholar]
33. Darlow BA, Gilbert C, Quinn GE, Azad R, Ells AL, Fielder A, et al. Promise and potential pitfalls of anti-VEGF drugs in retinopathy of prematurity. Br J Ophthalmol. 2009;93:986. [PubMed] [Google Scholar]
34. Rudanko SL, Laatikainen L. Visual impairment in children born at full term from 1972 through 1989 in Finland. Ophthalmology. 2004;111:2307–12. [PubMed] [Google Scholar]
35. Rudanko SL, Fellman V, Laatikainen L. Visual impairment in children born prematurely from 1972 through 1989. Ophthalmology. 2003;110:1639–45. [PubMed] [Google Scholar]
What Causes Blindness at Birth? | For Eyes
People of all ages can endure issues with their eyesight, even infants.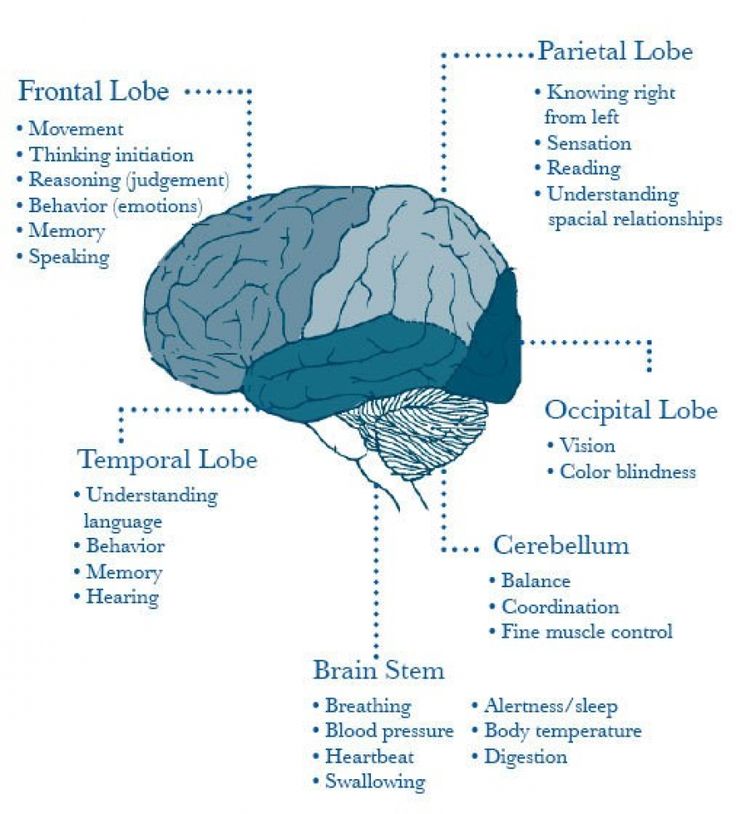 From obstacles during pregnancy to developmental problems, the reasons behind vision loss in babies can vary.
From obstacles during pregnancy to developmental problems, the reasons behind vision loss in babies can vary.
To find out more about what causes blindness at birth, keep reading. For Eyes is here to help.
What causes blindness at birth?
Like other age groups, newborns are not immune to blindness. Your little one’s eyes will need to be inspected from the time they’re born, such as for congenital cataracts, which may appear as unpigmented spots on your child’s eyes.
Congenital cataracts are a potential cause of vision loss in infants that can sometimes go undetected until your child is older, which is why every child needs an eye exam by 6 months of age. (The next eye exam should be at 3 years old and then again at age 6, with an appointment every year after into adulthood.)
What else causes blindness at birth? Issues with your child’s eye development or problems with the portion of the brain that controls vision may impact your child’s eyesight.
Another one of the potential causes of blindness in infants is retinopathy of prematurity (ROP), which affects the blood vessels in the retina. It most often impacts premature babies who are less than three pounds. When an infant is born early, their retina and blood vessels may not finish developing, which can inhibit oxygen absorption around the retina.
It most often impacts premature babies who are less than three pounds. When an infant is born early, their retina and blood vessels may not finish developing, which can inhibit oxygen absorption around the retina.
Due to this, the retina may be alerted to create new blood vessels. These can be delicate, and they tend to leak fluids, which can create marks and scars. The scars can yank on the retina as your child grows, which can make the retina move from its place behind the eye. Even if retinal detachment does not occur, your little one’s vision can still be impacted, usually making their direct line of sight blurry at the least.
According to the American Optometric Association (AOA), if your child has other health issues, they may have a higher chance of developing ROP. However, how much your little one weighs and when they’re born are some of the most significant risk factors.
What are the symptoms of blindness in babies?
From the day your child is born, it’s a good idea to watch for symptoms of blindness.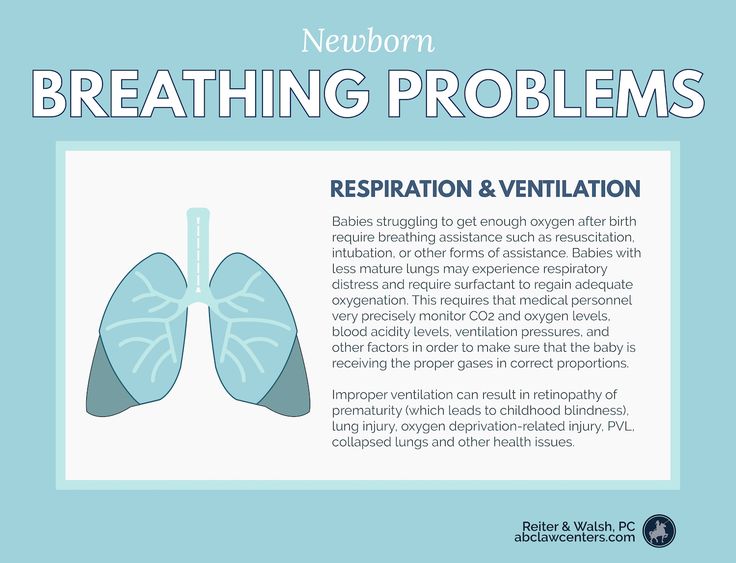 In babies, the way to do so is to work with an eye doctor, who will inspect how your child’s eyes function together and apart. They may also look at how your child’s eyes respond to light, which can indicate a vision concern if the light doesn’t seem to affect them.
In babies, the way to do so is to work with an eye doctor, who will inspect how your child’s eyes function together and apart. They may also look at how your child’s eyes respond to light, which can indicate a vision concern if the light doesn’t seem to affect them.
Here are some other common symptoms of blindness in babies and children:
- Discolored pupils
- Eye movement issues
- Light sensitivity
- Red eyes
- Touching the eyes often
Remember: These symptoms don’t always indicate oncoming blindness. When your little one is young, it can take time for their eyes to develop. If you notice any symptoms happening more often than usual, consult an Independent Doctor of Optometry in your area.
Summary: Blindness in Babies
Monitoring symptoms of blindness in babies and children is the best way to detect eye issues early on and get your child the right treatment. If your child exhibits any signs of eye issues, such as discoloration in the pupils or light sensitivity, we encourage you to reach out to an optometrist.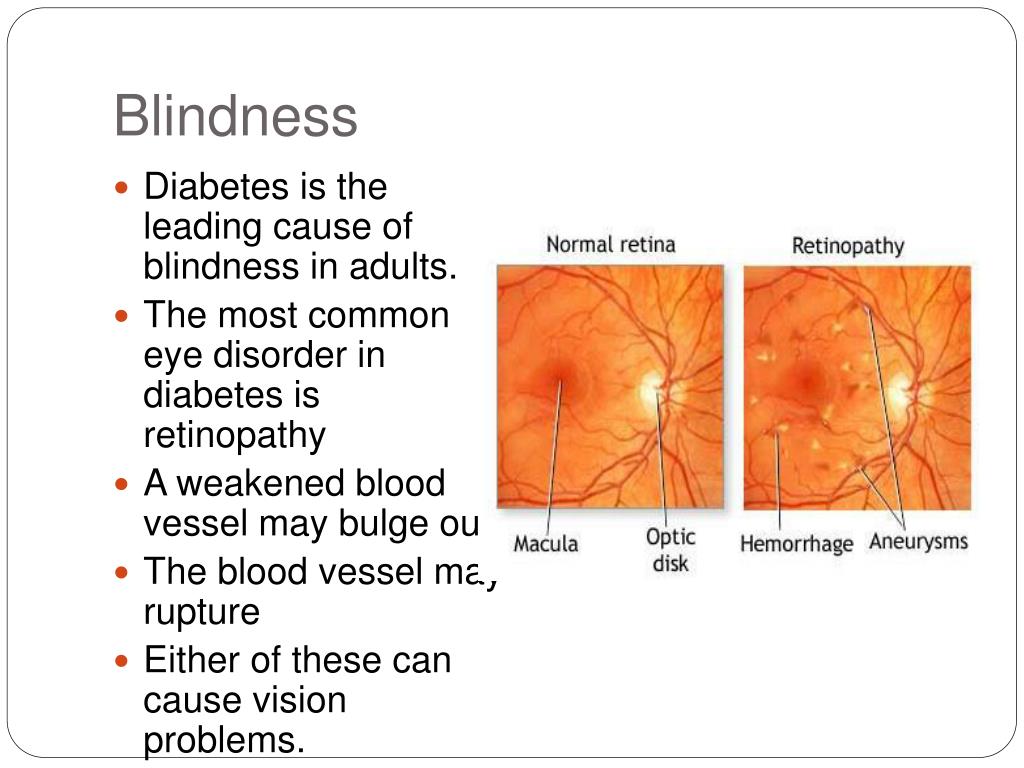
Are you curious about what causes blindness at birth? Two of the main conditions to watch for are congenital cataracts and ROP.
While these issues are by no means the only ones that can affect your baby’s eyes, they’re some important ones to monitor. By ensuring your little one gets a comprehensive eye exam by 6 months old, you can usually catch these conditions before they progress too much.
Book your eye exam at For Eyes
Have you had your annual comprehensive eye exam? Schedule an appointment with an Independent Doctor of Optometry at your local For Eyes.
Book an Exam
Kids Eye Health Eyeglasses eye doctor eye exam Eye Health eye pain question eye doctor symptoms eye eye eyewear routine eye exam birth BlindnessTOP 5 DISEASES THAT CAN MAKE BLIND
11/19/2019
The World Health Organization has designated November 13 as International Day for the Blind.
This date was chosen in honor of the birthday of Valentin Gayuy, a French teacher who, at his own expense, without anyone's help, opened the first school of sciences and crafts for blind children, created the uncial font for the blind and published books. Then he worked in Russia, St. Petersburg, where he created an institute for the blind.
Fortunately, now blindness is gradually receding under the onslaught of modern discoveries in medicine, but there are still diseases that can cause blindness. Igor Aznauryan, ophthalmologist, doctor of medical sciences, professor, founder of the Yasny Vzor children's eye clinic, will tell how ophthalmologists continue to fight these formidable enemies.
DIABETIC RETINOPATHY
Diabetes begins with elevated blood glucose levels and leads to various complications, the most severe of which is diabetic retinopathy. It is seen in 89-0% of diabetic patients. Because of this complication, increased vascular permeability develops, and everything that should remain in the vessel ends up in the perivascular space.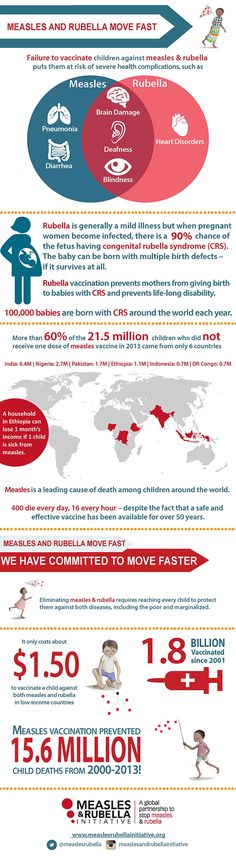 As a result, swelling and hemorrhages occur in the retina of the eye. The consequences are a pronounced decrease in visual acuity and blindness.
As a result, swelling and hemorrhages occur in the retina of the eye. The consequences are a pronounced decrease in visual acuity and blindness.
Diabetic retinopathy ranks first in the world in terms of the number of people blinded because of it. To save your eyesight, you need to immediately contact an endocrinologist and an ophthalmologist when diagnosing diabetes mellitus.
The endocrinologist will work on the normalization of blood sugar levels, prescribe a course of insulin intake and the necessary diet.
The ophthalmologist will monitor changes in the retina in order to timely detect the onset of the disease and begin conservative or surgical treatment.
GLAUCOMA
An ophthalmic disease that has not yet surrendered to ophthalmologists results in complete and incurable blindness if not caught in its early stages.
The insidiousness of glaucoma is that it can progress for a long time absolutely imperceptibly for a person. As a result, he comes to the doctor already at an extremely advanced stage, when tubular vision has formed. This means that peripheral vision is already completely absent.
As a result, he comes to the doctor already at an extremely advanced stage, when tubular vision has formed. This means that peripheral vision is already completely absent.
In glaucoma, there is an increase in intraocular pressure, which causes the death of optic nerve cells. Because of this, he can no longer transmit an image to the brain.
But if earlier glaucoma was a death sentence, now, with early detection, doctors can save a person's eyesight for many years - for example, Bono, the lead singer of U2, has been fighting this disease for almost 20 years and still sees the world.
The main thing is the rapid detection of the disease at the earliest stages. To do this, after 35 years of age, at least once a year, an ophthalmological examination with measurement of intraocular pressure should be performed. If it is elevated, the doctor will prescribe pressure-reducing drops, which must be strictly dripped into the eyes every day. There are also surgical and laser treatments for glaucoma.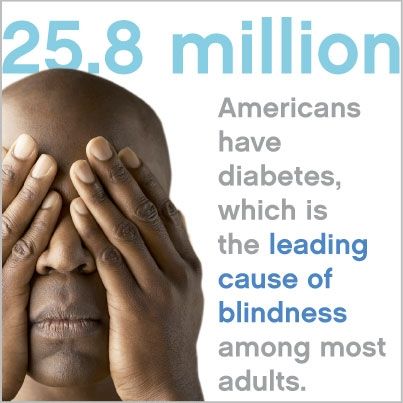
OPTItic atrophy
The death of the nerve fibers of the optic nerve leads to irreversible blindness. This disease remained a terrible sentence for a very long time - but now, with partial atrophy, when the surviving nerve fibers are preserved, vision can be preserved. Unfortunately, it cannot be improved, but the patient will see.
It is necessary to consult a doctor as soon as possible to identify the disease. To stop the process of atrophy and stabilize vision, many techniques have been developed - for example, drug therapy, which includes vasodilators, anti-atherosclerosis drugs, stimulants, and means to regulate blood clotting.
Ophthalmologists use ultrasound, the introduction of vitamin B, nicotinic acid, trypsin enzymes. Means for color and light stimulation, electro- and magneto-stimulating procedures, massage techniques, meso- and ozone therapy have been created.
There are also surgical methods to combat atrophy - the doctor injects the patient with a drug that replaces nerve tissue, or installs an electrical stimulator in the orbit of the eye for several years.
RETINOBLASTOMA
One of the most dangerous eye cancers appears in the first months or years of a child's life, but the disease is almost impossible to notice. The baby does not feel any pain or discomfort. Is that when photographing in his pupil there is a greenish cat glow.
If you notice something like this, immediately run with the child to the doctor. If you delay, you can lose not only your eyes (literally), but also your life - if the tumor metastasizes to the brain.
Alas, due to the invisibility of the tumor, most often parents bring the child to the doctor already in the later stages. To avoid such a situation - in the first years of a baby's life, visit an ophthalmologist every six months. Otherwise, if you're lucky, your baby will survive, but, like the actor Peter Falk, he will wear a glass prosthesis for the rest of his life and see with only one eye.
MELANOMA
Melanoma is not only the most insidious and dangerous skin cancer.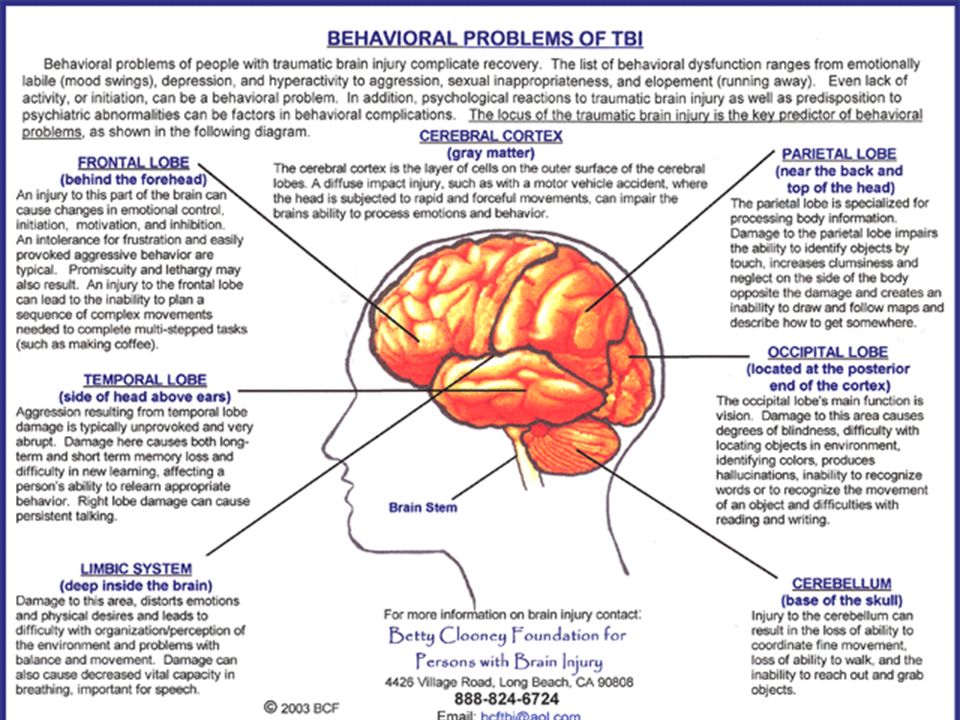 Since there is a large amount of melanin in the iris of the eye, melanocytes that produce it can become the basis for the development of melanoma.
Since there is a large amount of melanin in the iris of the eye, melanocytes that produce it can become the basis for the development of melanoma.
It affects the pupil, iris or sclera - the white shell of the eyeball. Often this happens completely unnoticed, and the patient comes to the doctor when the rapidly progressing disease reaches a critical stage. There are no preventive measures for melanoma of the eye - only constant attention.
If a pigment spot or dot suddenly appears in the eye, go to the ophthalmologist for an ultrasound of the eyeball as soon as possible. It is not only about vision, but also about saving life - this is a malignant, very rapidly developing tumor. Early detection of ocular melanoma is essential for successful treatment.
World of news, November 19, 2019
Common eye diseases
Cataract Cataract is a condition in which the lens of the eye loses its natural transparency and becomes cloudy. In most cases, this happens gradually, over many years. Additional factors in the development of cataracts include eye trauma, congenital cataracts, taking various medications, etc. The recommended treatment for cataracts is an operation in which the cloudy lens is removed and an artificial transparent lens is transplanted in its place, which remains in the eye forever. There is a wide range of lenses available for transplantation. Today, in some cases, it is even possible to get rid of myopia, hyperopia and astigmatism by transplanting a multifocal lens, which helps to see both far and near. GlaucomaGlaucoma or "lightning", also known as the "silent thief of vision", is an eye disease in which intraocular pressure rises, which can eventually lead to permanent blindness. The increased pressure inside the eye causes irreversible damage to the optic nerve and leads to a gradual reduction in the visual field.
Glaucoma can develop at any age, but its onset is most common around the age of 40, mostly in people with high blood pressure, diabetes, or nearsightedness, and in those who have had eye surgery.
For the treatment of patients with glaucoma, a drug method is used, including eye drops to reduce intraocular pressure and tablets. In addition, the patient may be scheduled for surgery or laser correction. Such treatment is designed to reduce intraocular pressure and stop the further development of the disease. The choice of treatment by a doctor depends on the type and stage of the disease, as well as on the patient's health status. If there is a glaucoma patient in your family, then other family members are at increased risk. Try to get tested as soon as possible and find out if other family members suffer from this disease. It is important to listen to the doctor's instructions, strictly follow the medication schedule and monitor the rate of development of the disease. Early detection and treatment will save your eyesight and allow you to return to your normal life in the shortest possible time.
Retinal atrophy
Retinal center atrophy (AMD - age-related macular degeneration) is the most common cause of vision loss among older adults in the Western world. This disease is associated with age-related degeneration of the macula or macula, which is located in the center of the retina and is responsible for central vision, which allows us to read, drive a car and distinguish objects. As a rule, the only symptom of this disease is a decrease in vision. But sometimes it can lead to a severe deterioration in vision and cause significant damage to the quality of life of patients. Sometimes patients see a reduced picture, and sometimes images of different sizes in different eyes. Regular eye examinations by a qualified ophthalmologist contribute to the early diagnosis of this condition. Diagnosis of retinal atrophy is based on examination of the fundus and is performed through various tests such as OCT (computed tomography, which scans the retina without the use of a contrast agent) and a picture of the retina after injection of a contrast agent. Although this disease almost never leads to complete blindness, it limits the sufferer from daily activities.
Therefore, early diagnosis of the disease is extremely important. Retinal atrophy is divided into two types: "dry" (lighter form) and "wet" (more severe form that threatens vision).
Methods of treatment
In mild cases, when it comes to the "dry" type of disease, treatment involves taking special vitamins that reduce the risk of deterioration to "wet". In the "wet" form of the disease, injections of Avastin or Lucentis into the vitreous are made. These drugs are directed against the growth factors of blood vessels, which are the causative agents of the disease, and also counteract retinal edema. In the clinics of the "Einaim" network, such types of treatment are prescribed both for private patients and members of health insurance funds.
Keratoconus Keratoconus (conical retina) is a disease of the cornea of the eye, which leads to a gradual change in its structure. The cornea becomes thinner in the center and in the lower part and takes on a conical shape. The disease may be hereditary or may be caused by such local factors as frequent rubbing of the eyes (for example, as a result of various allergic inflammations). A change in the structure of the cornea leads to the development of myopia and severe asymmetric astigmatism and the appearance of a blurry image that is poorly corrected with glasses. Keratoconus is diagnosed by scanning the cornea and measuring its thickness. The main condition for obtaining a sharp image is the symmetry and transparency of the cornea. Keratoconus develops when the cornea becomes thin. The change in the structure of the cornea is expressed in an increase in the cylinder, a gradual increase in numerical parameters and the lack of stability of the cornea. The image becomes blurred and distorted. The lack of sharpness and focus of vision cannot be completely corrected with glasses. Additional symptoms of the disease: deterioration in the ability to distinguish between color shades, scattering of light at night and the formation of light halos. In addition, a significant relationship was found between thin cornea and intraocular pressure. Since in some cases this disease is hereditary and its symptoms are detected during the test, it is recommended that the whole family be diagnosed.
Treatment methods: in the early stages of the disease, visual acuity can be corrected with glasses or soft or hard breathable contact lenses, which are made to order order. At later stages of the development of the disease, the patient needs surgery. There are several methods of treatment: at an intermediate stage, a corneal ring can be transplanted, which increases the stability of the cornea. In more severe cases, corneal implantation from a donor can be performed. If the disease progresses, it can be stopped by strengthening the cornea of the eye. The development of the disease can be stopped using a method called "cross linking" (Cross Linking), which involves a biochemical effect to harden the cornea. It does this by increasing intermolecular collagen bonds within the cornea. Who is the treatment for?1. At the late stage of keratoconus.2. In rare cases, complications after surgery to get rid of glasses.3. Liquefaction of the cornea of the eye.4. Edema of the endothelium of the cornea of the eye.
There is a keratoconus clinic at the Einaim Medical Center, in which comprehensive checks of the stage of the disease are performed. Based on these checks, each patient is offered the appropriate treatment for him.
Retinal detachment
If a tear or hole has formed in the retina, then fluid from the vitreous body or blood can penetrate through it under the retina. In this case, the retina peels off from the eyeball. A tear or hole in the retina may appear as flashes of light in the visual field. At a later stage in the development of this disease, a gray “curtain” may appear in front of the eye and a sudden sharp decrease in visual acuity. This process is painless and usually develops in only one eye. It should be noted that severe myopia is an additional risk factor that can lead to rupture and detachment of the retina. For patients with myopia greater than 6 diopters, annual retinal examinations are recommended. This check is performed by an eye doctor after pupil dilation.
Retinal detachment treatments:
When the retina is torn, laser surgery is usually performed, which is designed to prevent detachment. If retinal detachment has already occurred, then it can be returned to its place by injecting gas into the vitreous body or through surgery.
Diabetic retinopathy
This is an eye disease that affects diabetics and is characterized by damage to the retinal blood vessels. If it is not treated in a timely manner, it can cause severe damage to vision, up to blindness. Diabetic retinopathy primarily affects the small blood vessels of the retina, causing bleeding and secretions in the retina. In the later stages of the disease, new, abnormal blood vessels appear in the retina and vitreous. This leads to bleeding inside the vitreous body, which in turn causes a sharp and serious decrease in the sharpness of vision, and then - retinal detachment. Diabetes mellitus also increases the likelihood of diseases such as cataracts and glaucoma. The disease can be prevented or delayed by balancing blood sugar levels with medication, proper nutrition and weight loss in obese individuals, as well as by stabilizing blood pressure, fat content in the blood and, of course, smoking cessation. Diabetic retinopathy requires careful observation by an eye doctor every 3 to 12 months, depending on the severity of the disease. When signs of retinopathy and damage to blood vessels in the retina are detected, laser treatment is usually used to reduce swelling of the macula and central areas of the retina. Laser treatment is performed after pupil dilation and under local anesthesia with eye drops. In cases of chronic macular edema, steroid injections are also used to help absorb the edema into the vitreous. If there are signs of vitreous bleeding or retinal detachment, surgery is performed to drain blood from the vitreous or correct retinal detachment.
Pterygium
Pterygium is a benign pterygoid hymen that is formed as a result of thickening of the conjunctiva, the mucous membrane that covers the white of the eye. This hymen grows slowly over the years. If the hymen grows only in the white part of the eye, then it is called a "pinguecula". If the tissue begins to grow upward and capture the cornea of the eye, then this is pterygium. In any case, it contains more blood vessels than the surrounding tissues, and when these vessels dilate, redness appears. In cases where the hymen does not interfere with vision or approaches the center of the cornea, there is no need to remove it, since there is a risk that it will reappear. But if the hymen covers the visual axis of the eye or leads to deformation of the cornea to such an extent that it causes distortion of vision, then it can be removed with a surgical operation. In addition, sometimes this hymen is small, but it looks red, irritated and interferes with a person from an aesthetic point of view. In this case, you can consider removing it. The most advanced treatment for this disease today involves implanting the conjunctiva, which greatly reduces the risk of its recurrence.
Uveitis (uvetis) - inflammation of the tissues of the eye
There is a whole group of diseases that are characterized by inflammation of the choroid. This inflammation is classified according to its location in the eye and can be anterior, posterior, or involve the entire eye. Sometimes uveitis can affect several layers of tissue at the same time. It is diagnosed by a complete physical examination, as well as by serological and hematological blood tests and tomography of the eyes, head, and whole body (CT and X-ray). As a rule, uveitis is one of the manifestations of other diseases (for example, autoimmune and systemic diseases, in particular tuberculosis) with a parasitic infection caused by hereditary factors or trauma. Uveitis is treated with anti-inflammatory drugs.
Blepharitis
Blepharitis is a non-infectious inflammation of the edges of the eyelids that develops as a result of narrowing or blockage of the pores in the glands that secrete the fatty components of tears. As a result, the chemical composition of the secretions changes, bacterial growth increases and an inflammatory reaction develops at the edges of the eyelids. Blepharitis causes the following symptoms: dry eyes, redness, discharge on the eyelashes, tired eyes and sometimes a sensation of a "foreign body", tearing, thinning of the eyelashes or their growth inside the eye. This disease is common among people with oily skin and a tendency to develop pustules and acne, as well as among people suffering from dandruff, and among patients with skin diseases such as seborrhea or psoriasis. Treatment requires constant cleaning of the skin of the eyelids from secretions and maintaining proper eye hygiene the following means: compresses with hot water, massage of the eyelid on the surface of the eyeball, external cleaning of the edges of the eyelids with a special towel. Sometimes a doctor will recommend rubbing antibiotic ointment or taking antibiotics internally to change the viscosity of the fat layer and kill germs.
Barley (holazion)
The lesion, which in most cases is not infectious, but can become contaminated, causing pain and the appearance of an abscess. Treatment involves heating the affected area with a towel or cotton wool soaked in hot water for several minutes. This will help relieve pain and stop the inflammation in the eyes. In rare cases, the eye doctor may decide to surgically aspirate to remove the pus or to remove the infected area.
Corneal edema
One of the layers, which is part of the cornea of the eye, contains a layer of endothelial cells, which are responsible for the constant removal of fluids from the cornea and thereby prevent the appearance of edema. A healthy cornea contains about 2,500 endothelial cells per square millimeter, and they cannot multiply. Over the years, the number of endothelial cells naturally decreases. In diseases associated with eye atrophy, when the density of endothelial cells becomes below a certain level, corneal insufficiency is observed. This is mainly expressed in the fact that the fluid penetrates the cornea of \u200b\u200bthe eye and causes it to swell. In this case, the cornea becomes thick and cloudy. A decrease in the transparency of the cornea of the eye leads to a decrease in the sharpness of vision up to blindness. Additional factors that cause corneal edema include surgery and eye trauma.
Treatment: If the swelling persists and causes cloudiness of the cornea, which reduces the sharpness of vision, then a transplant is necessary. Before the transplant operation, treatment with salt water drops is prescribed as a temporary solution. These drops help drain fluid from the cornea. If all layers of the cornea are normal and transparent, and only the layer of endothelial cells is damaged, then only endothelial cell transplantation is performed, without replacing the entire cornea. Operations of this type do not leave stitches, and therefore recovery is faster.
Blockage of tear ducts in young children
The tear ducts must open after birth, and tears must pass through them from the eyes into the nasal cavity. Sometimes tear ducts remain clogged and prevent tears from flowing out normally. In case of blockage of the tear ducts, the lacrimal sac fills up, and the fluid accumulated in it becomes a life-giving environment for microbes. As a result, they multiply and cause inflammation, which is expressed in the release of pus, increased tearfulness and redness in the eyes. Treatment of this disease in children is carried out by prescribing local antibiotics and local massage, which are designed to help open blocked tear ducts. If this does not solve the problem, then the blocked ducts are surgically opened. If this blockage occurs in adults, surgery is usually done to create a bypass called a DCR. To do this, an incision is made in the nose or an endoscope is inserted. The operation is performed in cooperation with an ear-nose-throat doctor.
Nystagmus
Unwanted eye movements caused by a significant deterioration in vision at a very young age, when the relationship between the eyes and the brain should develop. Sometimes this disease can be treated with muscle transplant surgery, but even then minimal nystagmus remains.
Ptosis - drooping eyelid
Causes of this phenomenon include congenital drooping of the eyelid, drooping of the eyelid as a result of eye injury, heredity or weakness of the muscles of the eyelid as a result of growing up and aging. In about 25% of cases, drooping of the eyelid occurs in both eyes. In young children, this condition requires immediate treatment if the eyelid covers the visual axis and can lead to amblyopia ("lazy eye") if not corrected. Ptosis is treated with eyelid lift surgery.
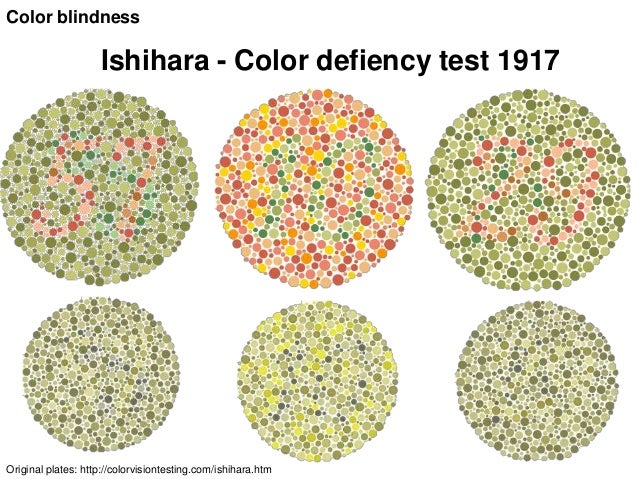
Impairment of color vision
Violation of color perception can be congenital or acquired as a result of damage to the optic nerve or injury to the retina. Congenital disorder is more common and more typical for boys than for girls - its frequency is 5 - 8% and 0.5%, respectively. It is important to note that the range of color perception impairment is very wide - from different levels of difficulty in distinguishing colors that look less bright, up to reduced vision.