Pregnancy high thyroid levels
Thyroid Disease & Pregnancy | NIDDK
On this page:
- What role do thyroid hormones play in pregnancy?
- Hyperthyroidism in Pregnancy
- Hypothyroidism in Pregnancy
- Postpartum Thyroiditis
- Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
- Thyroid Disease and Eating During Pregnancy
- Clinical Trials
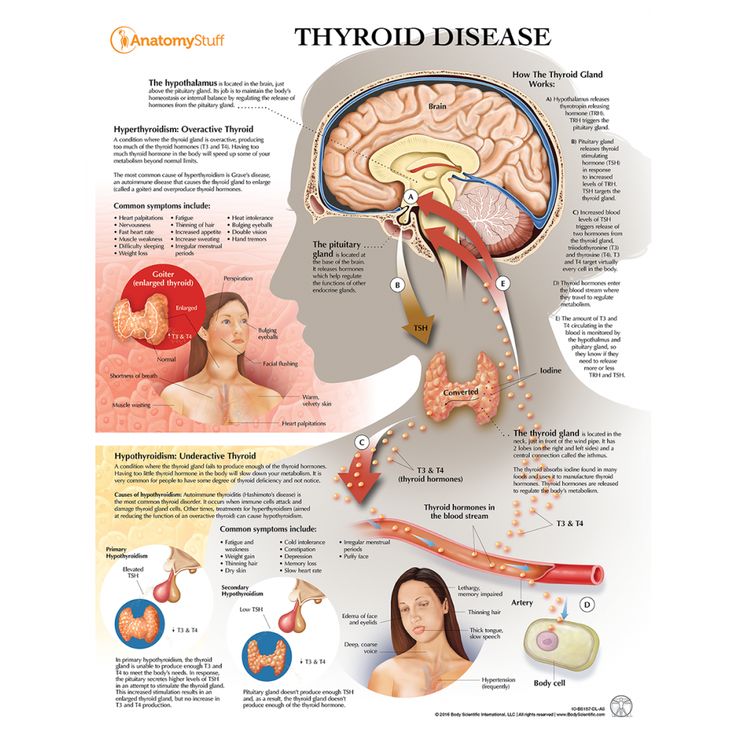
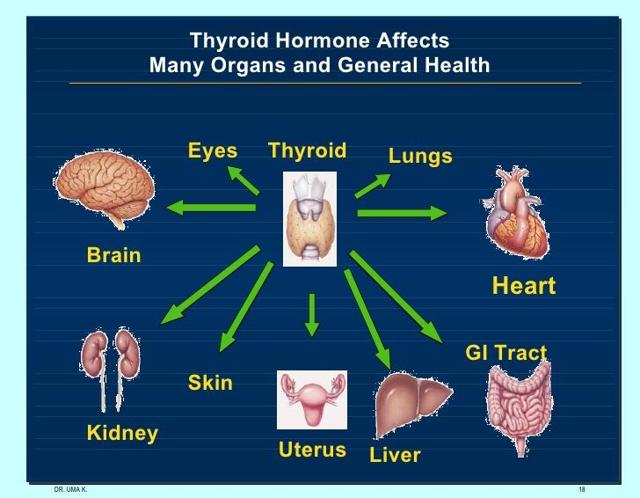
Thyroid disease is a group of disorders that affects the thyroid gland. The thyroid is a small, butterfly-shaped gland in the front of your neck that makes thyroid hormones. Thyroid hormones control how your body uses energy, so they affect the way nearly every organ in your body works—even the way your heart beats.
The thyroid is a small gland in your neck that makes thyroid hormones.Sometimes the thyroid makes too much or too little of these hormones. Too much thyroid hormone is called hyperthyroidism and can cause many of your body’s functions to speed up. “Hyper” means the thyroid is overactive. Learn more about hyperthyroidism in pregnancy. Too little thyroid hormone is called hypothyroidism and can cause many of your body’s functions to slow down. “Hypo” means the thyroid is underactive. Learn more about hypothyroidism in pregnancy.
If you have thyroid problems, you can still have a healthy pregnancy and protect your baby’s health by having regular thyroid function tests and taking any medicines that your doctor prescribes.
What role do thyroid hormones play in pregnancy?
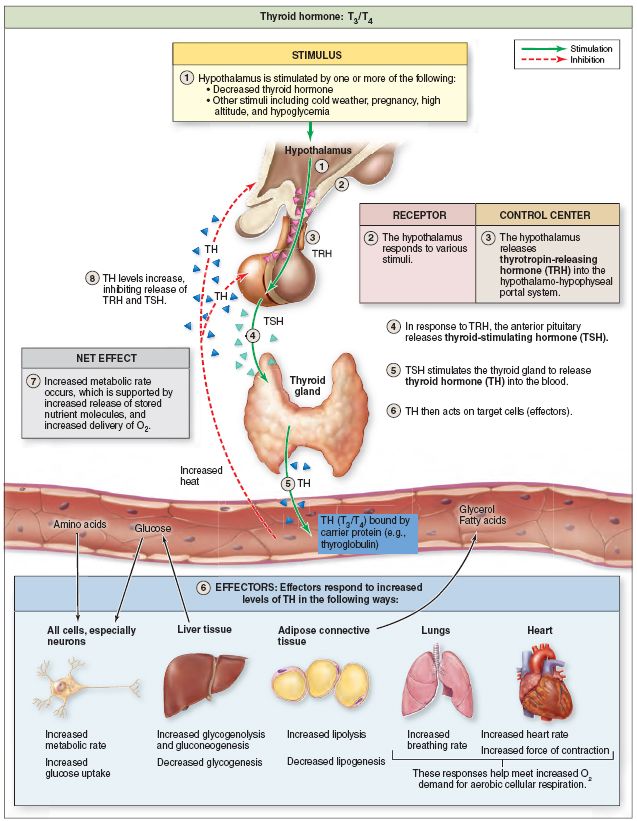
Thyroid hormones are crucial for normal development of your baby’s brain and nervous system. During the first trimester—the first 3 months of pregnancy—your baby depends on your supply of thyroid hormone, which comes through the placenta. At around 12 weeks, your baby’s thyroid starts to work on its own, but it doesn’t make enough thyroid hormone until 18 to 20 weeks of pregnancy.
Two pregnancy-related hormones—human chorionic gonadotropin (hCG) and estrogen—cause higher measured thyroid hormone levels in your blood. The thyroid enlarges slightly in healthy women during pregnancy, but usually not enough for a health care professional to feel during a physical exam.
The thyroid enlarges slightly in healthy women during pregnancy, but usually not enough for a health care professional to feel during a physical exam.
Thyroid problems can be hard to diagnose in pregnancy due to higher levels of thyroid hormones and other symptoms that occur in both pregnancy and thyroid disorders. Some symptoms of hyperthyroidism or hypothyroidism are easier to spot and may prompt your doctor to test you for these thyroid diseases.
Another type of thyroid disease, postpartum thyroiditis, can occur after your baby is born.
Hyperthyroidism in Pregnancy
What are the symptoms of hyperthyroidism in pregnancy?
Some signs and symptoms of hyperthyroidism often occur in normal pregnancies, including faster heart rate, trouble dealing with heat, and tiredness.
Other signs and symptoms can suggest hyperthyroidism:
- fast and irregular heartbeat
- shaky hands
- unexplained weight loss or failure to have normal pregnancy weight gain
What causes hyperthyroidism in pregnancy?
Hyperthyroidism in pregnancy is usually caused by Graves’ disease and occurs in 1 to 4 of every 1,000 pregnancies in the United States.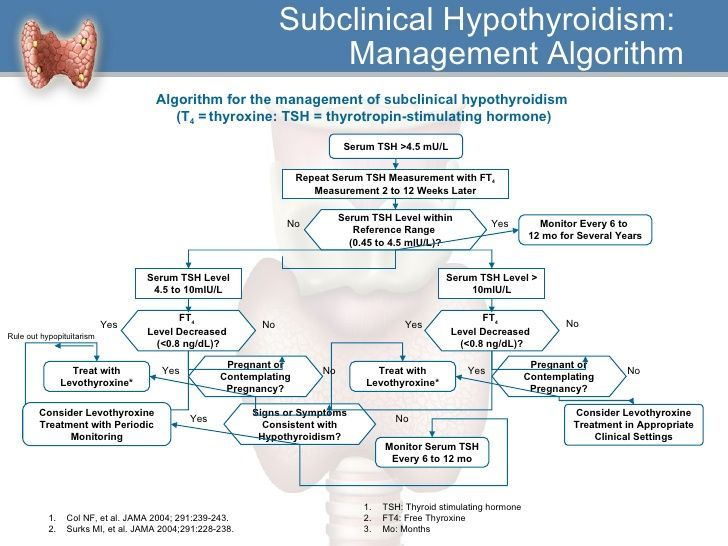 1 Graves’ disease is an autoimmune disorder. With this disease, your immune system makes antibodies that cause the thyroid to make too much thyroid hormone. This antibody is called thyroid stimulating immunoglobulin, or TSI.
1 Graves’ disease is an autoimmune disorder. With this disease, your immune system makes antibodies that cause the thyroid to make too much thyroid hormone. This antibody is called thyroid stimulating immunoglobulin, or TSI.
Graves’ disease may first appear during pregnancy. However, if you already have Graves’ disease, your symptoms could improve in your second and third trimesters. Some parts of your immune system are less active later in pregnancy so your immune system makes less TSI. This may be why symptoms improve. Graves’ disease often gets worse again in the first few months after your baby is born, when TSI levels go up again. If you have Graves’ disease, your doctor will most likely test your thyroid function monthly throughout your pregnancy and may need to treat your hyperthyroidism.1 Thyroid hormone levels that are too high can harm your health and your baby’s.
If you have Graves’ disease, your doctor will most likely test your thyroid function monthly during your pregnancy.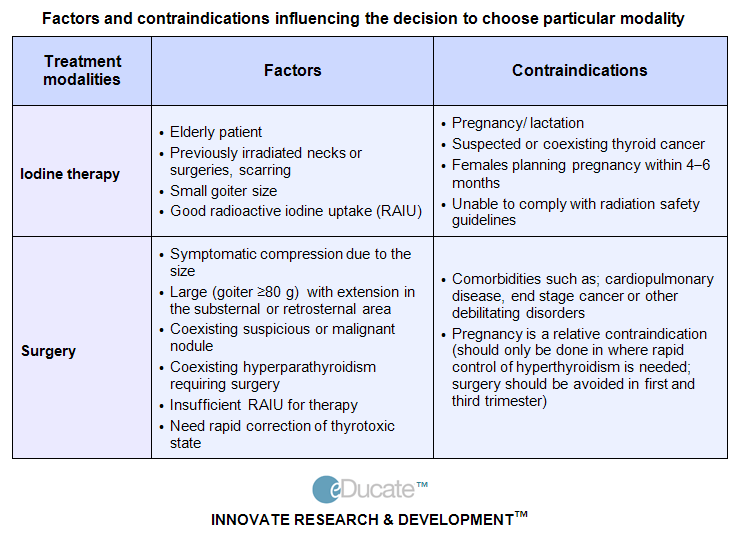
Rarely, hyperthyroidism in pregnancy is linked to hyperemesis gravidarum—severe nausea and vomiting that can lead to weight loss and dehydration. Experts believe this severe nausea and vomiting is caused by high levels of hCG early in pregnancy. High hCG levels can cause the thyroid to make too much thyroid hormone. This type of hyperthyroidism usually goes away during the second half of pregnancy.
Less often, one or more nodules, or lumps in your thyroid, make too much thyroid hormone.
How can hyperthyroidism affect me and my baby?
Untreated hyperthyroidism during pregnancy can lead to
- miscarriage
- premature birth
- low birthweight
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- thyroid storm—a sudden, severe worsening of symptoms
- congestive heart failure
Rarely, Graves’ disease may also affect a baby’s thyroid, causing it to make too much thyroid hormone. Even if your hyperthyroidism was cured by radioactive iodine treatment to destroy thyroid cells or surgery to remove your thyroid, your body still makes the TSI antibody. When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease so he or she can check your TSI levels. If they are very high, your doctor will monitor your baby for thyroid-related problems later in your pregnancy.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease.An overactive thyroid in a newborn can lead to
- a fast heart rate, which can lead to heart failure
- early closing of the soft spot in the baby’s skull
- poor weight gain
- irritability
Sometimes an enlarged thyroid can press against your baby’s windpipe and make it hard for your baby to breathe. If you have Graves’ disease, your health care team should closely monitor you and your newborn.
How do doctors diagnose hyperthyroidism in pregnancy?
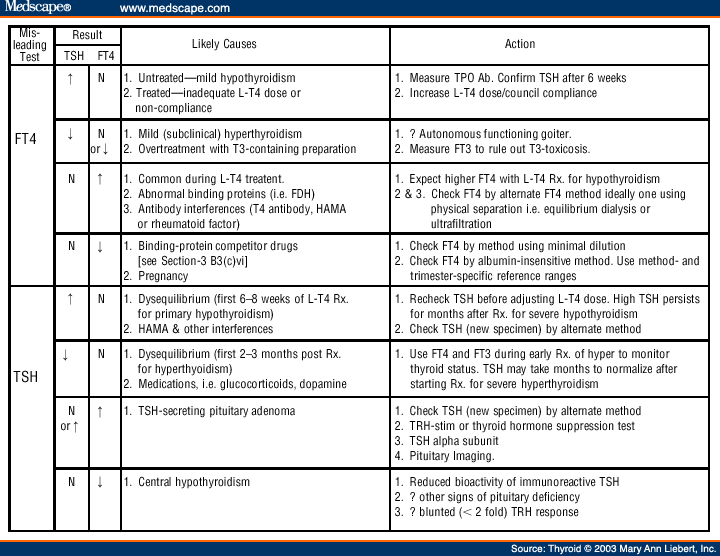
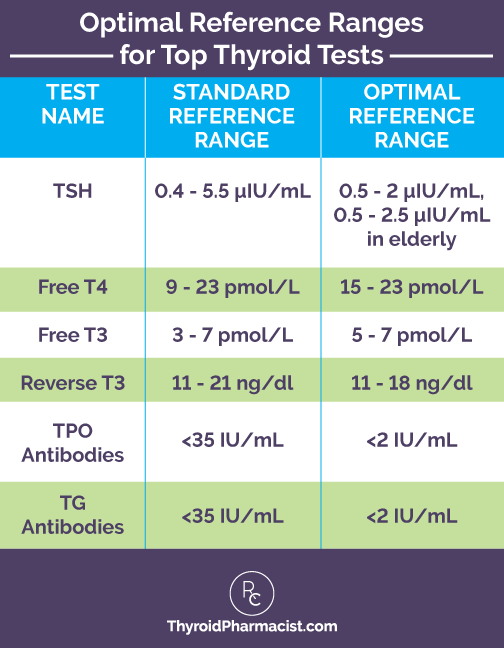
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for antibodies in your blood to see if Graves’ disease is causing your hyperthyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hyperthyroidism during pregnancy?
If you have mild hyperthyroidism during pregnancy, you probably won’t need treatment. If your hyperthyroidism is linked to hyperemesis gravidarum, you only need treatment for vomiting and dehydration.
If your hyperthyroidism is more severe, your doctor may prescribe antithyroid medicines, which cause your thyroid to make less thyroid hormone. This treatment prevents too much of your thyroid hormone from getting into your baby’s bloodstream. You may want to see a specialist, such as an endocrinologist or expert in maternal-fetal medicine, who can carefully monitor your baby to make sure you’re getting the right dose.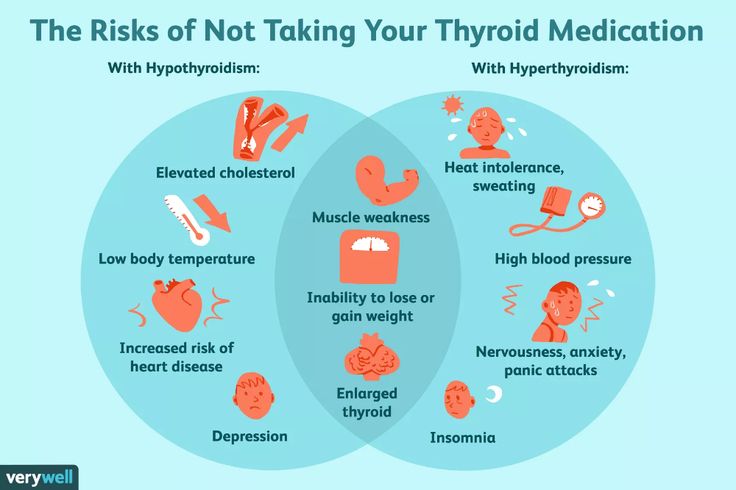
Doctors most often treat pregnant women with the antithyroid medicine propylthiouracil (PTU) during the first 3 months of pregnancy. Another type of antithyroid medicine, methimazole, is easier to take and has fewer side effects, but is slightly more likely to cause serious birth defects than PTU. Birth defects with either type of medicine are rare. Sometimes doctors switch to methimazole after the first trimester of pregnancy. Some women no longer need antithyroid medicine in the third trimester.
Small amounts of antithyroid medicine move into the baby’s bloodstream and lower the amount of thyroid hormone the baby makes. If you take antithyroid medicine, your doctor will prescribe the lowest possible dose to avoid hypothyroidism in your baby but enough to treat the high thyroid hormone levels that can also affect your baby.
Antithyroid medicines can cause side effects in some people, including
- allergic reactions such as rashes and itching
- rarely, a decrease in the number of white blood cells in the body, which can make it harder for your body to fight infection
- liver failure, in rare cases
Stop your antithyroid medicine and call your doctor right away if you develop any of these symptoms while taking antithyroid medicines:
- yellowing of your skin or the whites of your eyes, called jaundice
- dull pain in your abdomen
- constant sore throat
- fever
If you don’t hear back from your doctor the same day, you should go to the nearest emergency room.
You should also contact your doctor if any of these symptoms develop for the first time while you’re taking antithyroid medicines:
- increased tiredness or weakness
- loss of appetite
- skin rash or itching
- easy bruising
If you are allergic to or have severe side effects from antithyroid medicines, your doctor may consider surgery to remove part or most of your thyroid gland. The best time for thyroid surgery during pregnancy is in the second trimester.
Radioactive iodine treatment is not an option for pregnant women because it can damage the baby’s thyroid gland.
Hypothyroidism in Pregnancy
What are the symptoms of hypothyroidism in pregnancy?
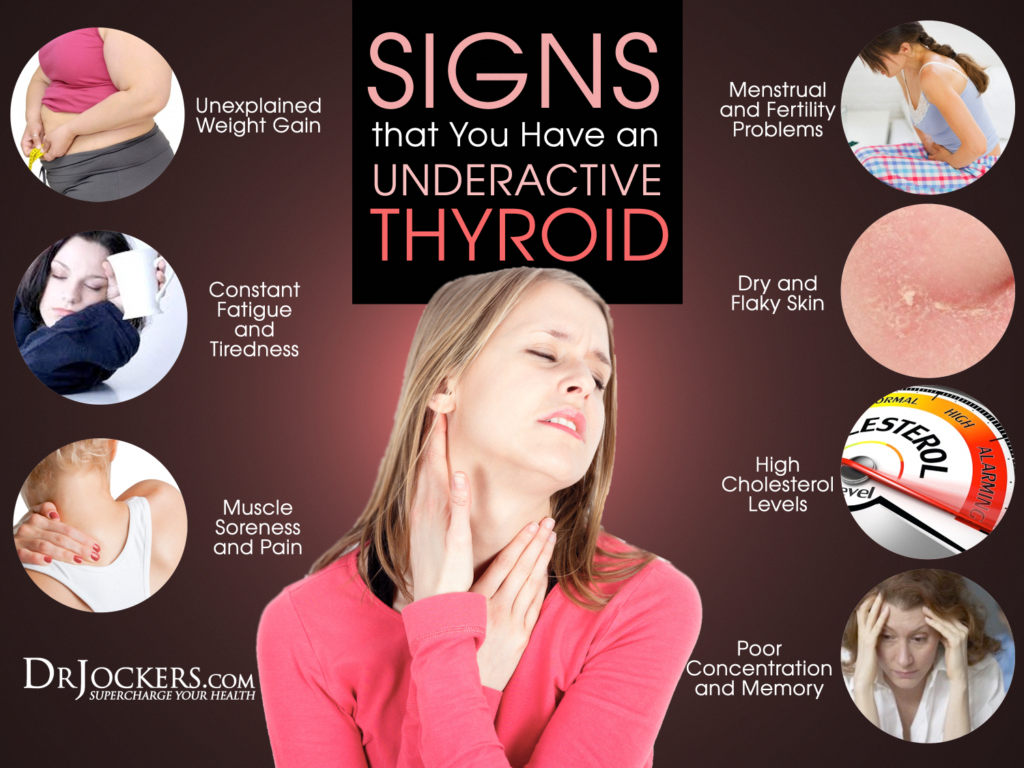
Symptoms of an underactive thyroid are often the same for pregnant women as for other people with hypothyroidism. Symptoms include
- extreme tiredness
- trouble dealing with cold
- muscle cramps
- severe constipation
- problems with memory or concentration

Most cases of hypothyroidism in pregnancy are mild and may not have symptoms.
What causes hypothyroidism in pregnancy?
Hypothyroidism in pregnancy is usually caused by Hashimoto’s disease and occurs in 2 to 3 out of every 100 pregnancies.1 Hashimoto’s disease is an autoimmune disorder. In Hashimoto’s disease, the immune system makes antibodies that attack the thyroid, causing inflammation and damage that make it less able to make thyroid hormones.
How can hypothyroidism affect me and my baby?
Untreated hypothyroidism during pregnancy can lead to
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- anemia
- miscarriage
- low birthweight
- stillbirth
- congestive heart failure, rarely
These problems occur most often with severe hypothyroidism.
Because thyroid hormones are so important to your baby’s brain and nervous system development, untreated hypothyroidism—especially during the first trimester—can cause low IQ and problems with normal development.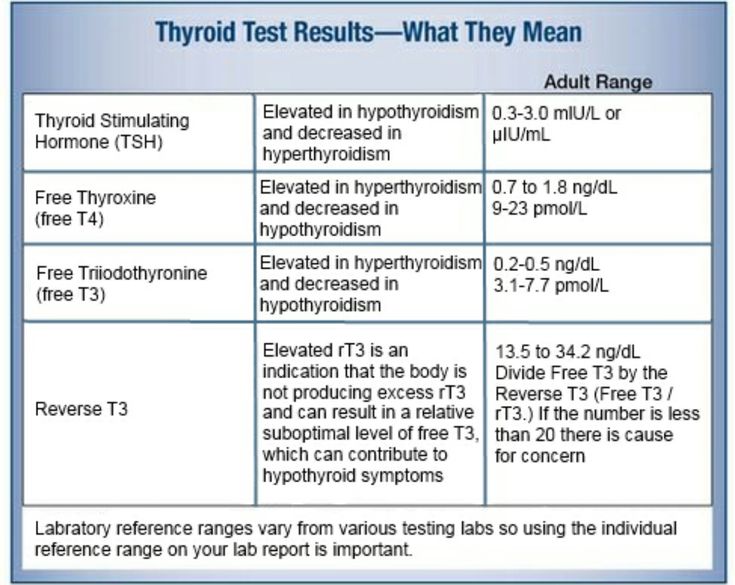
How do doctors diagnose hypothyroidism in pregnancy?
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for certain antibodies in your blood to see if Hashimoto’s disease is causing your hypothyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hypothyroidism during pregnancy?
Treatment for hypothyroidism involves replacing the hormone that your own thyroid can no longer make. Your doctor will most likely prescribe levothyroxine, a thyroid hormone medicine that is the same as T4, one of the hormones the thyroid normally makes. Levothyroxine is safe for your baby and especially important until your baby can make his or her own thyroid hormone.
Your thyroid makes a second type of hormone, T3. Early in pregnancy, T3 can’t enter your baby’s brain like T4 can. Instead, any T3 that your baby’s brain needs is made from T4. T3 is included in a lot of thyroid medicines made with animal thyroid, such as Armour Thyroid, but is not useful for your baby’s brain development.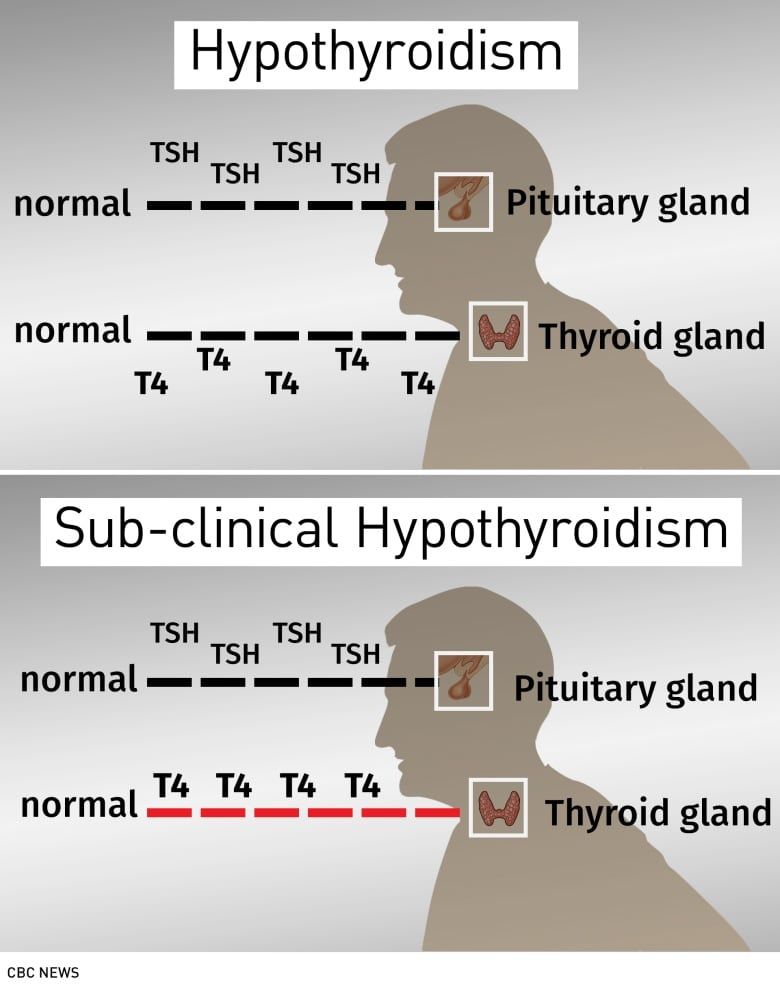 These medicines contain too much T3 and not enough T4, and should not be used during pregnancy. Experts recommend only using levothyroxine (T4) while you’re pregnant.
These medicines contain too much T3 and not enough T4, and should not be used during pregnancy. Experts recommend only using levothyroxine (T4) while you’re pregnant.
Some women with subclinical hypothyroidism—a mild form of the disease with no clear symptoms—may not need treatment.
Your doctor may prescribe levothyroxine to treat your hypothyroidism.If you had hypothyroidism before you became pregnant and are taking levothyroxine, you will probably need to increase your dose. Most thyroid specialists recommend taking two extra doses of thyroid medicine per week, starting right away. Contact your doctor as soon as you know you’re pregnant.
Your doctor will most likely test your thyroid hormone levels every 4 to 6 weeks for the first half of your pregnancy, and at least once after 30 weeks.1 You may need to adjust your dose a few times.
Postpartum Thyroiditis
What is postpartum thyroiditis?
Postpartum thyroiditis is an inflammation of the thyroid that affects about 1 in 20 women during the first year after giving birth1 and is more common in women with type 1 diabetes. The inflammation causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage raises the hormone levels in your blood, leading to hyperthyroidism. The hyperthyroidism may last up to 3 months. After that, some damage to your thyroid may cause it to become underactive. Your hypothyroidism may last up to a year after your baby is born. However, in some women, hypothyroidism doesn’t go away.
The inflammation causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage raises the hormone levels in your blood, leading to hyperthyroidism. The hyperthyroidism may last up to 3 months. After that, some damage to your thyroid may cause it to become underactive. Your hypothyroidism may last up to a year after your baby is born. However, in some women, hypothyroidism doesn’t go away.
Not all women who have postpartum thyroiditis go through both phases. Some only go through the hyperthyroid phase, and some only the hypothyroid phase.
What are the symptoms of postpartum thyroiditis?
The hyperthyroid phase often has no symptoms—or only mild ones. Symptoms may include irritability, trouble dealing with heat, tiredness, trouble sleeping, and fast heartbeat.
Symptoms of the hypothyroid phase may be mistaken for the “baby blues”—the tiredness and moodiness that sometimes occur after the baby is born. Symptoms of hypothyroidism may also include trouble dealing with cold; dry skin; trouble concentrating; and tingling in your hands, arms, feet, or legs.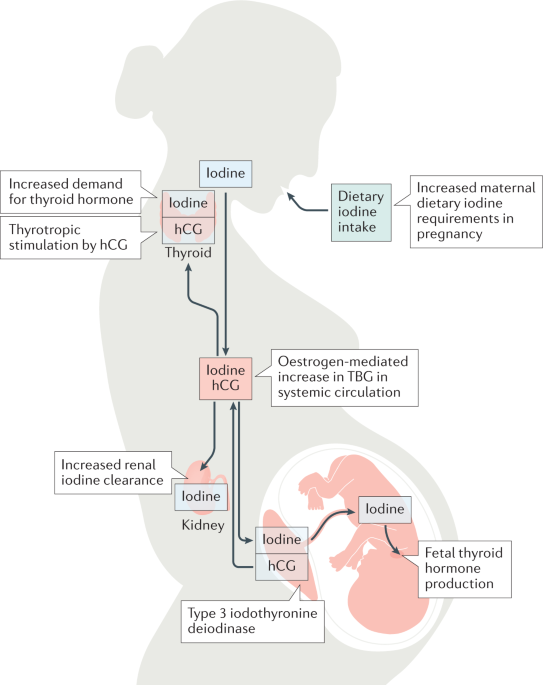 If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
What causes postpartum thyroiditis?
Postpartum thyroiditis is an autoimmune condition similar to Hashimoto’s disease. If you have postpartum thyroiditis, you may have already had a mild form of autoimmune thyroiditis that flares up after you give birth.
Postpartum thyroiditis may last up to a year after your baby is born.How do doctors diagnose postpartum thyroiditis?
If you have symptoms of postpartum thyroiditis, your doctor will order blood tests to check your thyroid hormone levels.
How do doctors treat postpartum thyroiditis?
The hyperthyroid stage of postpartum thyroiditis rarely needs treatment. If your symptoms are bothering you, your doctor may prescribe a beta-blocker, a medicine that slows your heart rate. Antithyroid medicines are not useful in postpartum thyroiditis, but if you have Grave’s disease, it may worsen after your baby is born and you may need antithyroid medicines.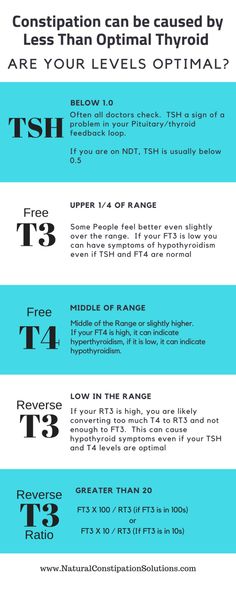
You’re more likely to have symptoms during the hypothyroid stage. Your doctor may prescribe thyroid hormone medicine to help with your symptoms. If your hypothyroidism doesn’t go away, you will need to take thyroid hormone medicine for the rest of your life.
Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
Certain beta-blockers are safe to use while you’re breastfeeding because only a small amount shows up in breast milk. The lowest possible dose to relieve your symptoms is best. Only a small amount of thyroid hormone medicine reaches your baby through breast milk, so it’s safe to take while you’re breastfeeding. However, in the case of antithyroid drugs, your doctor will most likely limit your dose to no more than 20 milligrams (mg) of methimazole or, less commonly, 400 mg of PTU.
Thyroid Disease and Eating During Pregnancy
What should I eat during pregnancy to help keep my thyroid and my baby’s thyroid working well?
Because the thyroid uses iodine to make thyroid hormone, iodine is an important mineral for you while you’re pregnant.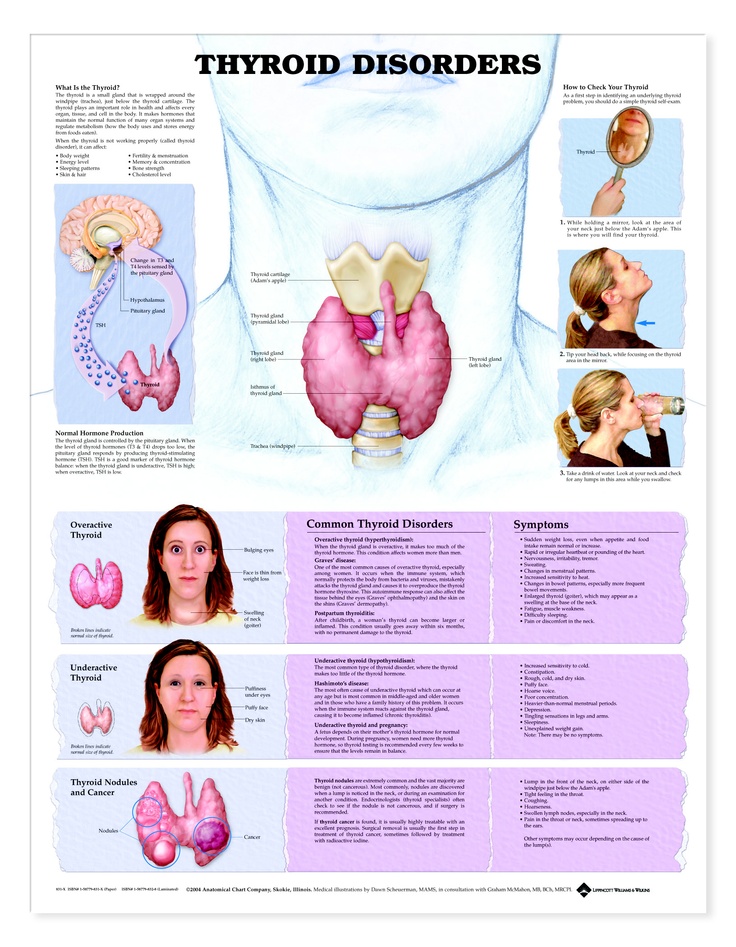 During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.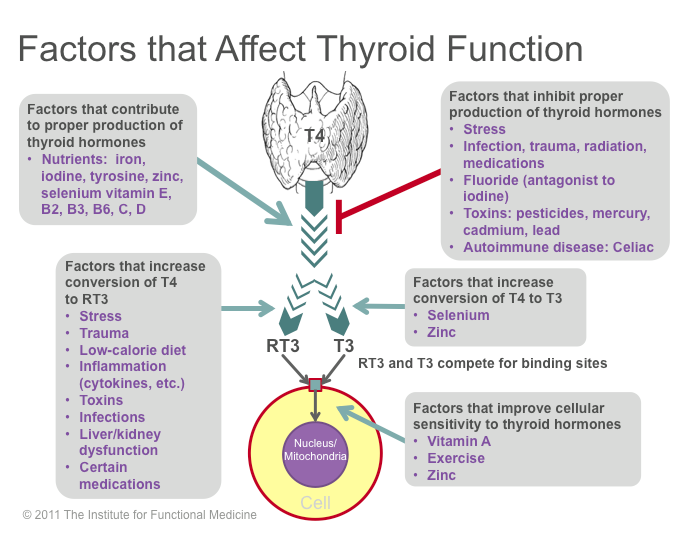
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov.
References
Thyroid conditions during pregnancy | March of Dimes
The thyroid makes hormones that help your body work. If it makes too little or too much of these hormones, you may have problems during pregnancy.
Untreated thyroid conditions during pregnancy are linked to serious problems, including premature birth, miscarriage and stillbirth.
If your thyroid condition is treated during pregnancy, you can have a healthy pregnancy and a healthy baby.
Ask your health care provider if your thyroid medicine is safe to take during pregnancy and breastfeeding. Your medicine or dose may need to change.
What is the thyroid?
The thyroid is a tiny, butterfly-shaped gland in your neck. A gland is an organ that makes substances that help your body work. The thyroid makes hormones (chemicals) that play a big role in your health. For example, thyroid hormones can affect your heart rate (how fast your heart beats) and your metabolism (how well and fast your body processes what you eat and drink).
Sometimes the thyroid gland makes too much or too little of certain hormones. When this happens, you have a thyroid disorder. Some women have a thyroid disorder that begins before pregnancy (also called a pre-existing condition). Others may develop thyroid problems for the first time during pregnancy or soon after giving birth.
With treatment, a thyroid condition may not cause any problems during pregnancy.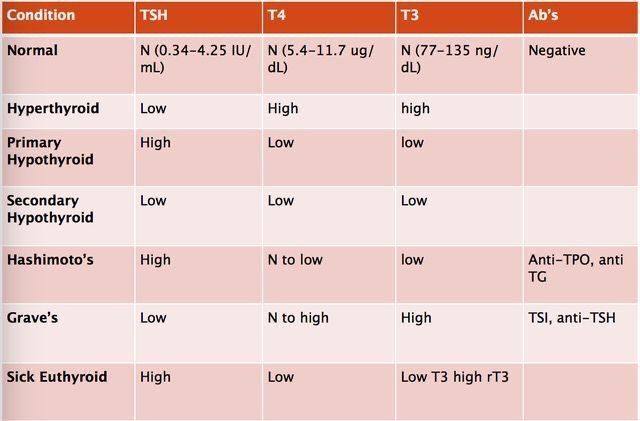 But untreated thyroid conditions can cause problems for you and your baby during pregnancy and after birth.
But untreated thyroid conditions can cause problems for you and your baby during pregnancy and after birth.
What are the main kinds of thyroid conditions?
There are two main kinds of thyroid conditions:
- Hyperthyroidism (“hyper” means too much). This is when the thyroid is overactive and makes too much thyroid hormone. This condition can cause many of your body’s functions to speed up. Hyperthyroidism during pregnancy usually is caused by an autoimmune disorder called Graves’ disease. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake. If you have Graves’ disease, your immune system makes antibodies that cause your thyroid to make too much thyroid hormone. In rare cases, hyperthyroidism is linked to a severe form of morning sickness called hyperemesis gravidarum (excessive nausea and vomiting during pregnancy). Also in rare cases, hyperthyroidism can be caused by thyroid nodules.
 These are lumps in your thyroid that make too much thyroid hormone.
These are lumps in your thyroid that make too much thyroid hormone. - Hypothyroidism (“hypo” means too little or not enough). This is when the thyroid is underactive and doesn’t make enough thyroid hormones, so many of your body’s functions slow down. Hypothyroidism during pregnancy usually is caused by an autoimmune disorder called Hashimoto’s disease. When you have Hashimoto’s disease, your immune system makes antibodies that attack your thyroid and damage it so it can’t produce thyroid hormones.
If you have a thyroid condition during pregnancy, treatment can help you have a healthy pregnancy and a healthy baby.
How are thyroid conditions during pregnancy diagnosed?
Health care providers don’t usually test your thyroid before or during pregnancy unless you’re at high risk of having a thyroid condition or you have signs or symptoms of one. If you have signs or symptoms of a thyroid condition, especially during pregnancy, tell your provider.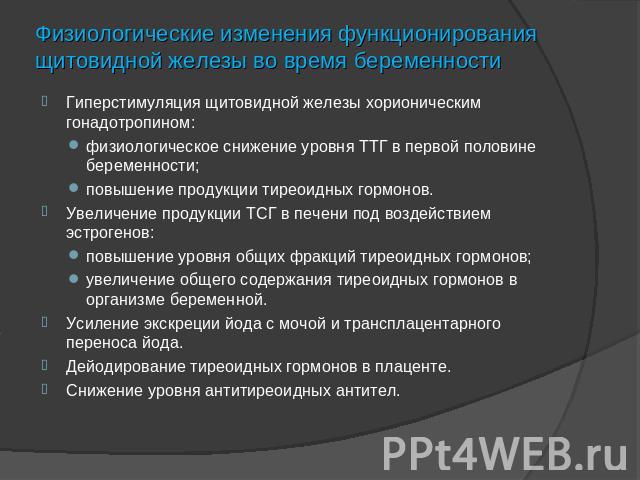 Signs of a condition are things someone else can see or know about you, like that you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Signs and symptoms of thyroid conditions may appear slowly over time. Many are signs and symptoms of other health conditions, so having one doesn’t always mean you have a thyroid problem.
Signs of a condition are things someone else can see or know about you, like that you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Signs and symptoms of thyroid conditions may appear slowly over time. Many are signs and symptoms of other health conditions, so having one doesn’t always mean you have a thyroid problem.
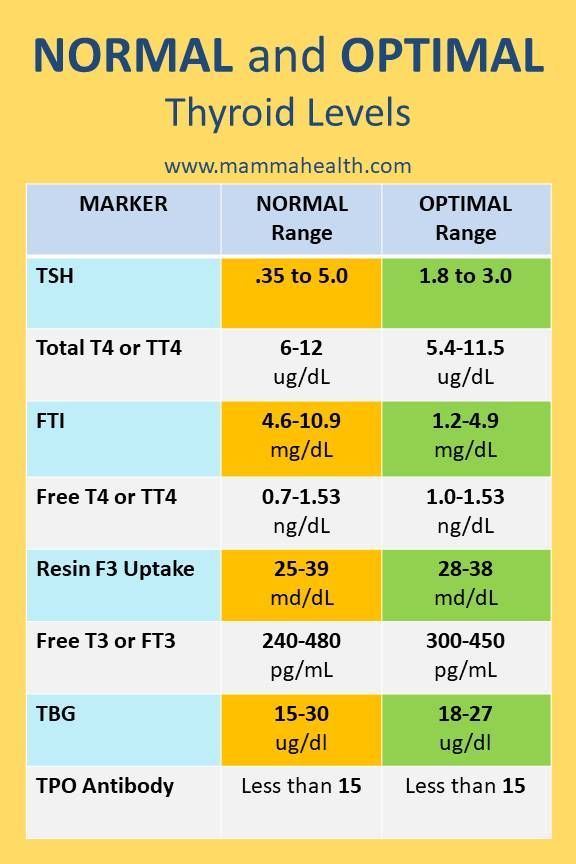
Your provider gives you a physical exam and a blood test to check for thyroid conditions. The blood test measures the levels of thyroid hormones and thyroid stimulating hormone (also called TSH) in your body. TSH is a hormone that tells your thyroid gland to make thyroid hormones. If you think you may have a thyroid condition, ask your provider about testing.
Are you at risk for having a thyroid condition during pregnancy?
You’re at higher risk for a thyroid condition during pregnancy than other women if you:
- Are currently being treated for a thyroid condition or you have thyroid nodules or a goiter.
 A goiter is a swollen thyroid gland that can make your neck look swollen.
A goiter is a swollen thyroid gland that can make your neck look swollen. - Have had a thyroid condition in the past (including after giving birth), or you’ve had a baby who had a thyroid condition
- Have an autoimmune disorder or you have a family history of autoimmune thyroid disease, like Graves’ disease or Hashimoto’s disease. Family history means that the condition runs in your family (people in your family have or have had the condition). Use the March of Dimes family health history form and share it with your provider. The form helps you keep a record of any health conditions and treatments that you, your partner and everyone in both of your families has had. It can help your provider check for health conditions that may affect your pregnancy. If you have a family history of thyroid or autoimmune conditions, ask your provider about testing.
- Have type 1 diabetes. Diabetes is a condition in which your body has too much sugar (called glucose) in the blood. Type 1 diabetes is a kind of preexisting diabetes, which means you have it before you get pregnant.
 If you have type 1 diabetes, your pancreas stops making insulin. Insulin is a hormone that helps keep the right amount of glucose in your body.
If you have type 1 diabetes, your pancreas stops making insulin. Insulin is a hormone that helps keep the right amount of glucose in your body. - Have had high-dose neck radiation or treatment for hyperthyroidism. Radiation is a kind of energy. It travels as rays or particles in the air.
If you’ve had a thyroid condition or think you’re at risk for having a thyroid condition, ask your provider about testing.
What are signs and symptoms of hypothyroidism?
Hyperthyroidism that’s untreated or not treated correctly is linked to problems for women and babies during pregnancy and after birth.
Problems for women can include:
- Preeclampsia. This is a serious blood pressure condition that can happen after the 20th week of pregnancy or after giving birth (also called postpartum preeclampsia). It’s when a woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working normally.
 Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy.
Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. - Pulmonary hypertension. This is a kind of high blood pressure that happens in the arteries in your lungs and on the right side of your heart.
- Placental abruption. This is a serious condition in which the placenta separates from the wall of the uterus before birth. The placenta grows in your uterus (womb) and supplies the baby with food and oxygen through the umbilical cord.
- Heart failure. This is when your heart can’t pump enough blood to the rest of your body.
- Thyroid storm. This is when your symptoms suddenly get much worse.
 It’s a rare, but life-threatening condition during pregnancy. Pregnant women who have thyroid storm are at high risk of heart failure.
It’s a rare, but life-threatening condition during pregnancy. Pregnant women who have thyroid storm are at high risk of heart failure.
Problems for babies can include:
- Premature birth. This is birth that happen too early, before 37 weeks of pregnancy.
- Goiter
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
- Thyroid problems. Antibodies that cause Graves’ disease cross the placenta during pregnancy. If you have Graves’ disease during pregnancy, your baby is at risk for thyroid conditions during and after birth. If you had treatment for Graves’ disease with radioactive iodine before pregnancy, your baby is at risk for Graves’ disease.
- Miscarriage or stillbirth. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
How can hypothyroidism affect pregnancy?
Untreated hypothyroidism during pregnancy is linked to problems for women and babies during pregnancy and after birth.
Problems for women can include:
- Anemia. This is when you don’t have enough healthy red blood cells to carry oxygen to the rest of your body.
- Gestational hypertension. This is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth.
- Preeclampsia
- Placental abruption
- Postpartum hemorrhage (also called PPH). This when a woman has heavy bleeding after giving birth. It’s a serious but rare condition. It usually happens within 1 day of giving birth, but it can happen up to 12 weeks after having a baby.
- Myxedema, a rare condition caused by severe, untreated hypothyroidism that can cause you to go into a coma and can cause death
- Heart failure.
 This is when your heart doesn’t pump blood as well as it should. Heart failure cause by hypothyroidism is rare.
This is when your heart doesn’t pump blood as well as it should. Heart failure cause by hypothyroidism is rare.
Problems for babies can include:
- Infantile myxedema, a condition that’s linked to severe hypothyroidism. It can cause dwarfism, intellectual disabilities and other problems. Dwarfism (also called little people) is a condition in which a person is very short (less than 4 feet 10 inches as an adult). Intellectual disability causes a lower-than-average intelligence and a lack of skills needed to function in daily life.
- Low birthweight.
- Problems with growth and brain and nervous system development. The nervous system is made up of your brain, spinal cord and nerves. Your nervous system helps you move, think and feel. Untreated hypothyroidism, especially when it happens during the first trimester, can cause low IQ in a baby.
- Thyroid problems. This is rare, but it can happen in babies of women with Hashimoto’s disease because the antibodies can cross the placenta during pregnancy.
- Miscarriage or stillbirth
What is postpartum thyroiditis?
In about 1 to 21 in 100 women (1 to 21 percent), the thyroid becomes swollen in the first year after giving birth. This is an autoimmune condition called postpartum thyroiditis. It can cause your thyroid to be overactive, underactive and even a combination of both.
How are thyroid conditions treated during pregnancy and while breastfeeding?
Many medicines used to treat thyroid conditions during pregnancy are safe for your baby.
Thyroid medicines can help keep the right level of thyroid hormones in your body. Your provider gives you blood tests during pregnancy to check your TSH and T4 levels to make sure your medicine is at the right amount (also called dose). T4 is a hormone made by your thyroid.
If you’re taking medicine for a thyroid condition before pregnancy, talk to your provider before you get pregnant. Your provider may want to adjust or change your medicine to make sure it’s safe for your baby. If you’re already taking thyroid medicine when you get pregnant, keep taking it and talk to your provider about it as soon as possible.
Treating hyperthyroidism. If you have mild hyperthyroidism, you may not need treatment. If it’s more severe, you may need to take an antithyroid medicine. This medicine causes your thyroid to make less thyroid hormone.
Most providers treat pregnant women with an overactive thyroid with antithyroid medicines called propylthiouracil in the first trimester and methimazole in the second and third trimesters. The timing of these medicines is important. Propylthiouracil after the first trimester can lead to liver problems. And methimazole in the first trimester may increase the risk of birth defects. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops, or how the body works.
Providers sometimes use radioactive iodine to treat hyperthyroidism.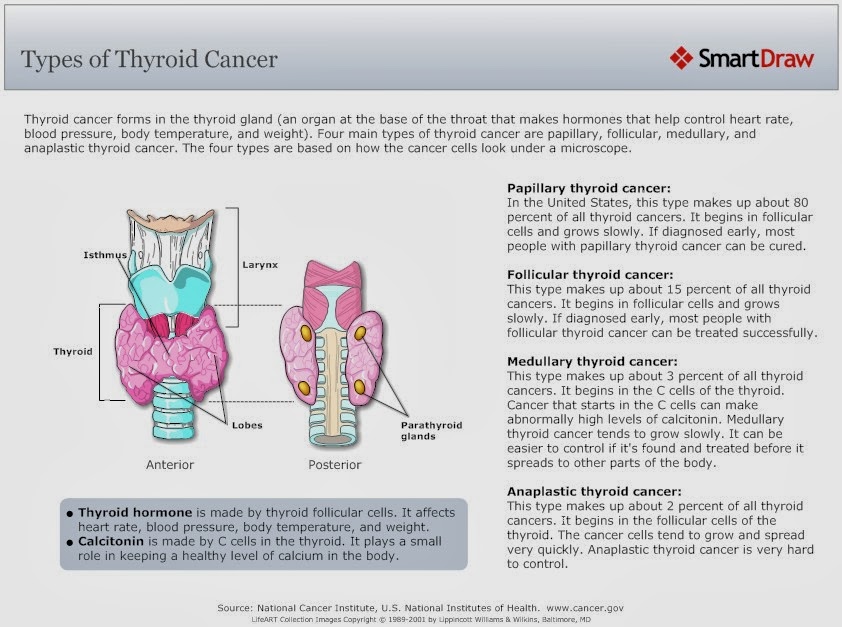 Pregnant women shouldn’t take this medicine because it can cause thyroid problems in the baby.
Pregnant women shouldn’t take this medicine because it can cause thyroid problems in the baby.
Antithyroid medicines are safe to take at low doses while you’re breastfeeding.
Treating hypothyroidism. Levothyroxine is the most common medicine used to treat an underactive thyroid during pregnancy. Levothyroxine replaces the thyroid hormone T4, which your own thyroid isn’t making or isn’t making enough of. It’s safe to take this medicine during pregnancy. Thyroid medicines that contain the T3 hormone aren’t safe to use during pregnancy.
If you had hypothyroidism before getting pregnant, you most likely need to increase the amount of medicine you take during pregnancy. Talk to your health care provider about your medicine as soon as you find out you’re pregnant. Your provider can check to make sure you’re taking the right dose by checking your TSH levels during pregnancy.
Talk to your provider about taking levothyroxine or other medicine to treat hypothyroidism while breastfeeding.
More information
- American Thyroid Association[AC18]
- MotherToBaby
Last reviewed: February, 2019
See also: Prescription medicine during pregnancy
Changes in thyroid function during pregnancy
O.V. Ushakova, D.V. Pozdnyakova, A.M. Volokhova, N.N.
Municipal budgetary healthcare institution "Clinical Diagnostic Center" of the Health Department of the Administration of Khabarovsk
Summary: The aim of the study is to assess the prevalence of changes in thyroid function in pregnant women.
The study showed that in the first trimester only 45.6% of cases during pregnancy have a normal functioning of the thyroid gland.
In 39.6% of cases, there was an increase in thyroid function. The average TSH level in women in the second group was 0.08±0.01 μIU/ml, free T4 - 29.2±0.8 pmol/l. Taking into account the absence of a thyrotoxicosis clinic, this condition was regarded as transient gestational thyrotoxicosis due to the production of chorionic gonadotropin by the placenta, therefore, thyrostatics were not treated.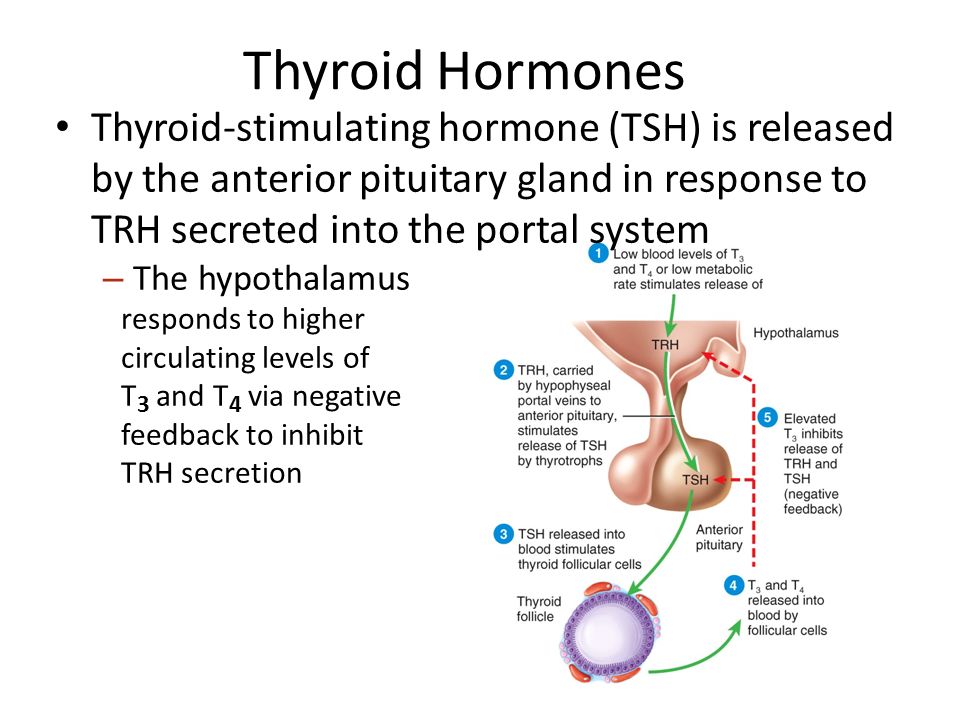 In the second trimester, the levels of thyroid hormones in women of this group were restored to normal values.
In the second trimester, the levels of thyroid hormones in women of this group were restored to normal values.
Subclinical hypothyroidism occurs in 12% of women.
Key words: pregnancy, gestational thyrotoxicosis, subclinical hypothyroidism.
Summary: A research objective – to estimate the prevalence of changes of function of a thyroid gland at pregnant women.
Research showed that in the first trimester only at 45.6% of cases during pregnancy function is noted normal functioning of a thyroid gland.
In 39.6% of cases increase of function of a thyroid gland was noted. The average value of the level of TTG at women in the second group made 0.08±0.01 mkME/ml, free T4 – 29.2±0.8 pmol/l the accounting of absence of clinic thyrotoxicosis, this condition was regarded as passing gestational thyrotoxicosis, caused by production of a horionichesky gonadotrophin by a placenta therefore treatment by the tireostatiky wasn't carried out.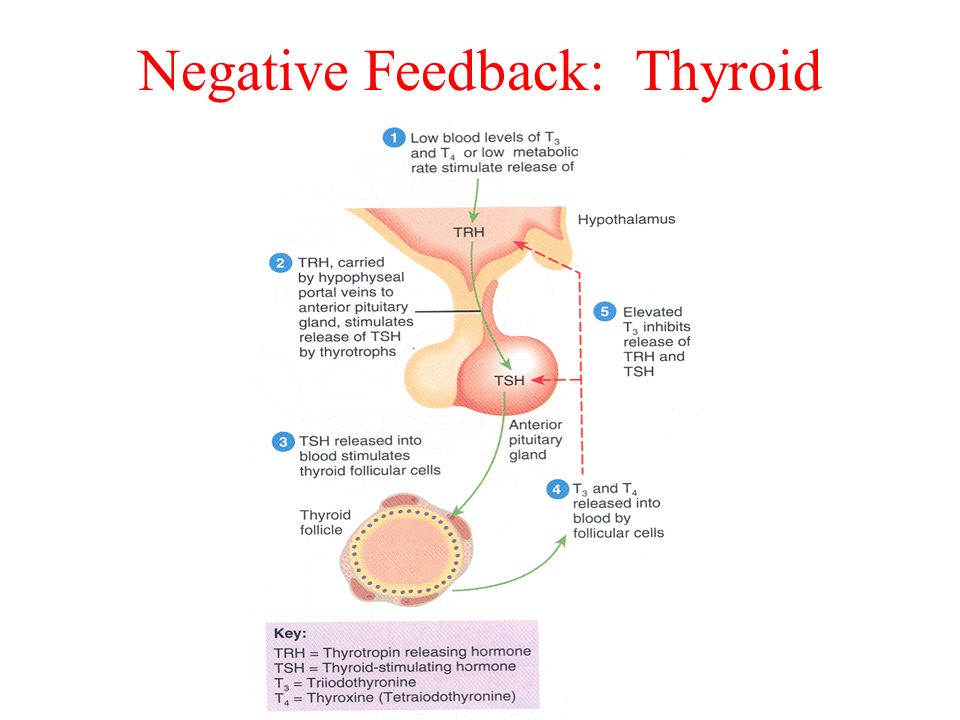 In the second trimester indicators of levels of hormones of a thyroid gland at women of this group were restored to normal values.
In the second trimester indicators of levels of hormones of a thyroid gland at women of this group were restored to normal values.
In 12% of cases at women the subclinical hypothyroidism meets.
Keywords: pregnancy, gestational hyperthyroidism, subclinical hypothyroidism.
Introduction:
In the context of deteriorating somatic and reproductive health of women, the most promising issues are early diagnosis, prevention and correction of conditions leading to the development of a threat of miscarriage, the birth of a healthy child. The course of pregnancy, the physical development of the child, and his intellectual potential depend on how effectively the thyroid gland produces thyroid hormones during pregnancy. During pregnancy, the level of thyroid hormones should increase by 30-50%. At this time, a temporary endocrine organ is formed in women - the placenta, which secretes chorionic gonadotropin, placental lactogen, estriol, estradiol, progesterone into the woman's body.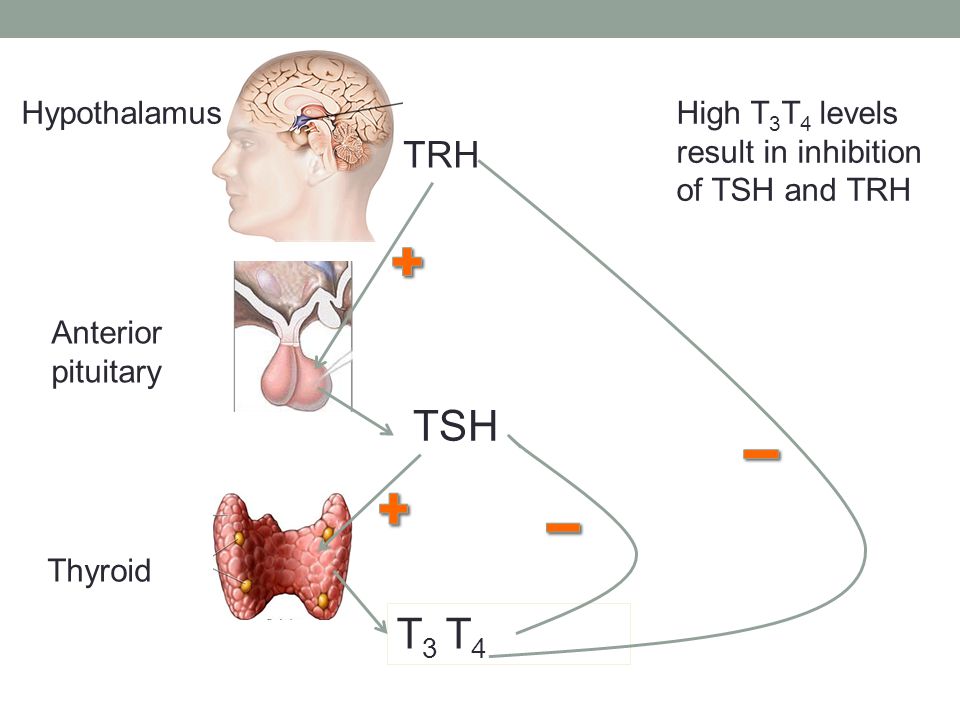 Produced in the first trimester of pregnancy, human chorionic gonadotropin has a structural similarity with thyroid-stimulating hormone (TSH), which allows stimulating thyroid function. From its influence, the level of the hormone T4f increases. and the level of TSH decreases, up to the development of gestational thyrotoxicosis with clinical manifestations. The next mechanism for stimulating thyroid function is an increase in the formation of thyroxin-binding globulin (TSG) under the influence of placental estrogens, which leads to an increase in blood levels of T3 and total T4, resulting in the level of T4f. decreases, stimulating the production of TSH levels and further stimulation of the thyroid gland.
Produced in the first trimester of pregnancy, human chorionic gonadotropin has a structural similarity with thyroid-stimulating hormone (TSH), which allows stimulating thyroid function. From its influence, the level of the hormone T4f increases. and the level of TSH decreases, up to the development of gestational thyrotoxicosis with clinical manifestations. The next mechanism for stimulating thyroid function is an increase in the formation of thyroxin-binding globulin (TSG) under the influence of placental estrogens, which leads to an increase in blood levels of T3 and total T4, resulting in the level of T4f. decreases, stimulating the production of TSH levels and further stimulation of the thyroid gland.
In addition, during pregnancy, as a result of increased glomerular filtration and renal clearance of iodine, the transplacental transfer of iodine to the fetus, a relative iodine deficiency develops in the woman's body, which also helps to stimulate the function of the thyroid gland.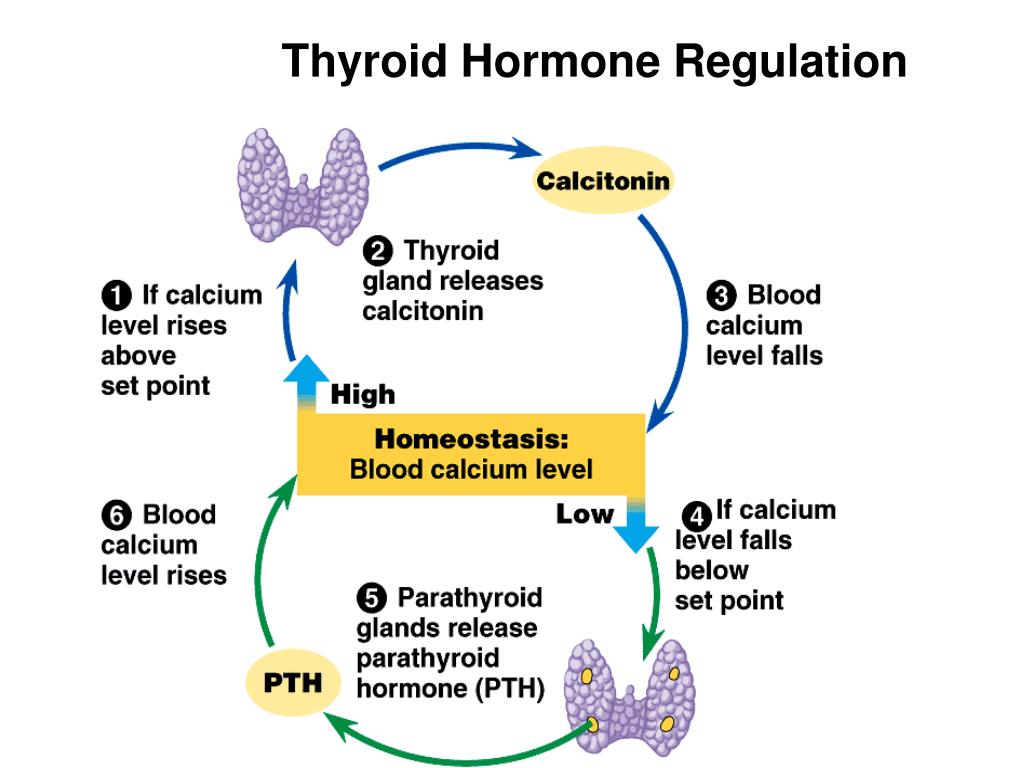
It is known that in the first trimester the thyroid gland of the fetus is just being formed, and its development will be carried out exclusively under the influence of the mother's thyroid hormones. The presence of both overt and subclinical hypothyroidism in the mother can have irreversible consequences for the development of the fetus and its brain functions.
Study aims to evaluate the prevalence of changes in thyroid function in pregnant women.
Materials and methods: study of the level of thyroid hormones TSH and T4f. was conducted in 414 pregnant women aged 18 to 38 years who were registered in the first trimester, and in 98 pregnant women who were registered in the second trimester. The examination was carried out in the clinical diagnostic laboratory of the municipal budgetary healthcare institution "Clinical Diagnostic Center" of the Health Department of the Administration of Khabarovsk.
Statistical analysis was carried out using a package of standard statistical programs: Office 2000 and Statistica 6. 0 for Windows.
0 for Windows.
Results and discussion
The functional activity of the thyroid gland according to the literature is determined by the level of TSH: euthyroid - TSH 0.4–4.0 µIU/ml; hyperthyroid - TSH less than 0.4 μIU / ml; hypothyroid - TSH more than 4.0 μIU / ml. For the correct interpretation of laboratory parameters reflecting the activity of the thyroid gland, the combined determination of the level of TSH and free T4 is important. The determination of total T4 and T3 is not informative, since during pregnancy their levels are always increased by 1.5 times
The study showed (Table 1) that in 45.6% of the total number of pregnant women examined in the first trimester, the level of TSH and free T4 remained within the normal range. In other cases, there was a deviation in the level of TSH and T4sv. both in combination and for each type of hormones from established norms (Table 2). So the level of TSH in the first trimester of pregnancy was reduced in combination with an increased level of free T4 in 39.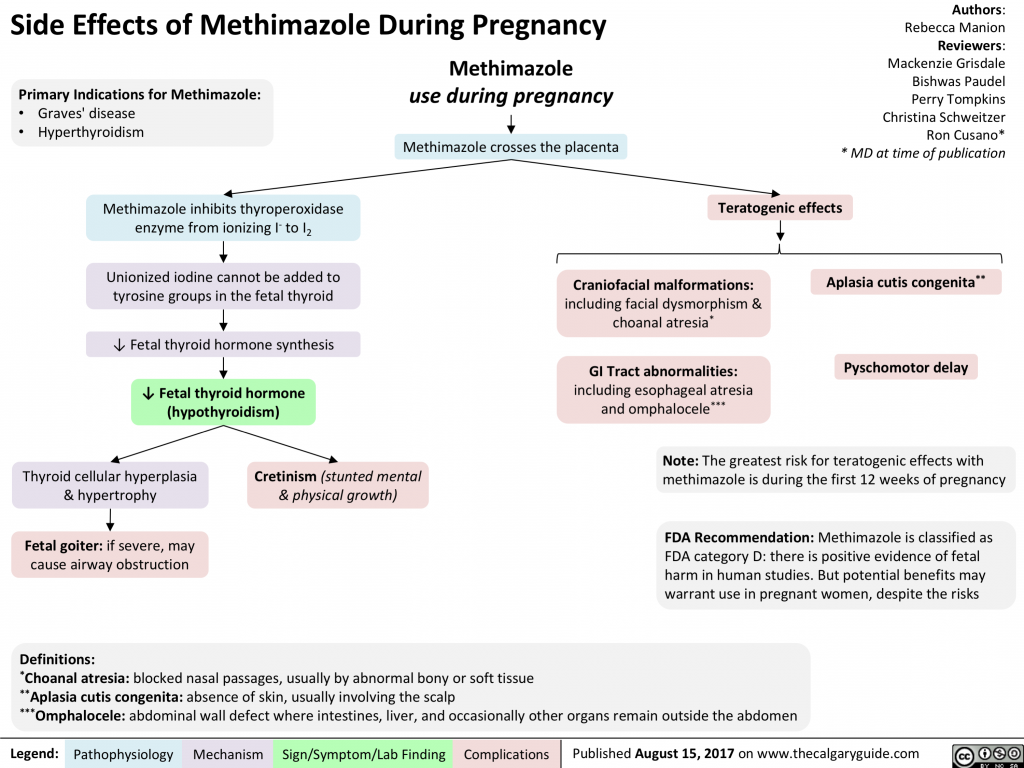 6% of the total number of women examined. In 12% of pregnant women out of the total number of those examined, an increase in the level of TSH was noted above the norm without a change in the level of free T4, in 2.8% of cases there was an isolated decrease in the level of free T4.
6% of the total number of women examined. In 12% of pregnant women out of the total number of those examined, an increase in the level of TSH was noted above the norm without a change in the level of free T4, in 2.8% of cases there was an isolated decrease in the level of free T4.
Thus, depending on the state of thyroid function, three groups of women were identified: the first group of women in a euthyroid state, the second group - a group of women with increased thyroid function, the third group of women with reduced thyroid function.
The average TSH level in women in the second group was 0.08±0.01 μIU/ml, free T4 - 29.2±0.8 pmol/l. This condition was regarded as transient gestational thyrotoxicosis due to the production of chorionic gonadotropin by the placenta. When examining women, dynamic monitoring of them, it was noted that the change in thyroid function was not manifested by clinical signs of thyrotoxicosis, was not accompanied by vomiting, the level of free T4 on average exceeded the normal value by 1.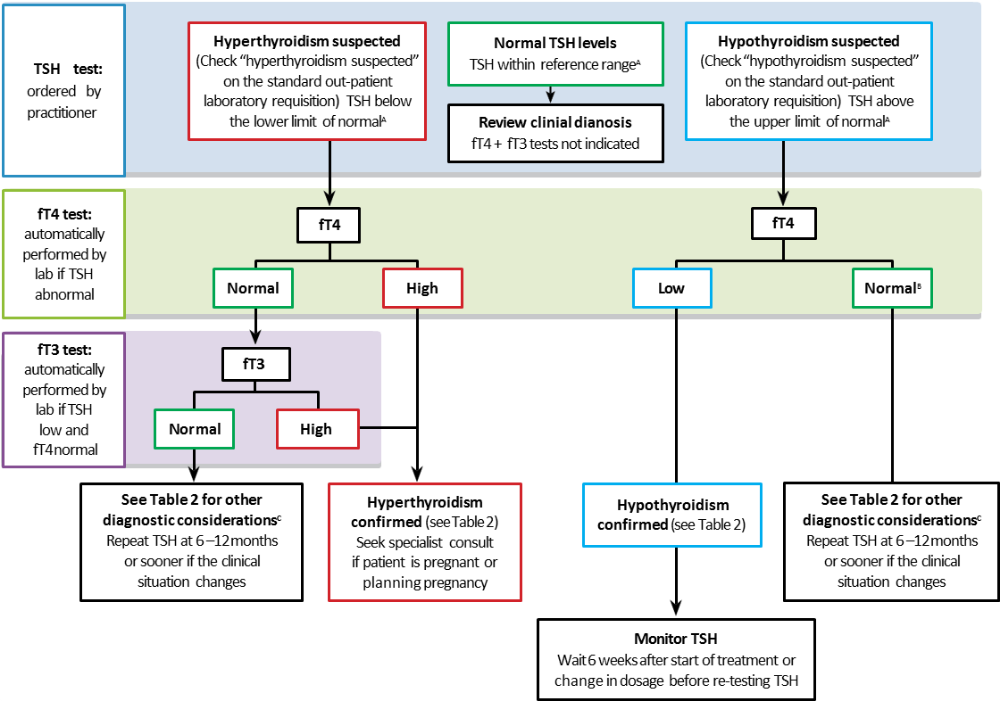 2 times, therefore, treatment with thyreostatics was not prescribed.
2 times, therefore, treatment with thyreostatics was not prescribed.
During the re-examination in the second trimester, there was a normalization of indicators characterizing the function of the thyroid gland. The average TSH level in women of this group was 0.4±0.08 μIU/ml, free T4 - 21±0.7 pmol/l.
The average TSH level in women in the third group was 5.1±0.09 µIU/ml, free T4 level was 18±0.04 pmol/l. This condition was regarded as subclinical hypothyroidism, in connection with which the women were prescribed levothyroxine replacement therapy with maintenance of TSH levels in the first trimester up to 2.5 µIU/ml, in the second trimester up to 3 µIU/ml.
Among women registered for pregnancy in the second trimester (Table 3), in 93.9% of cases of the total number of studies, the level of TSH and free T4 was within normal limits. The average level of TSH was 1.2±0.04 µIU/ml, free T4 was 19.2±0.4 pmol/l.
In 6.1% of cases, an elevated TSH level was noted with free T4 levels within the normal range.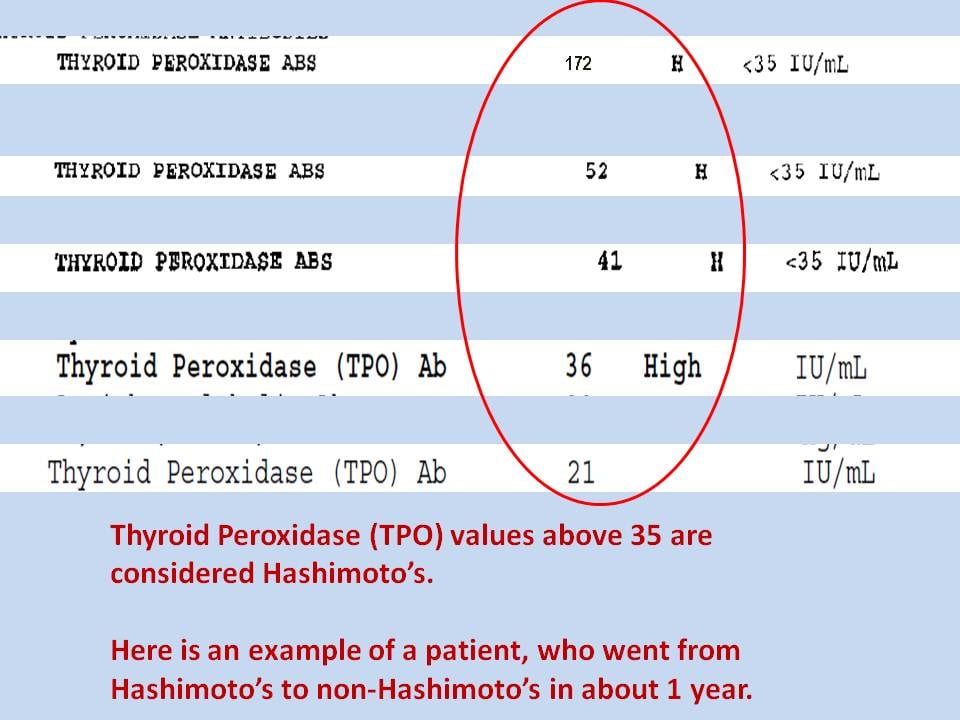 The average TSH level in women of this group was 4.9±0.08 µIU/ml, free T4 level was 16.7±0.07 pmol/l. This group of women was prescribed l-thyroxine at a dose that allows maintaining the recommended TSH level within 3 µIU/ml.
The average TSH level in women of this group was 4.9±0.08 µIU/ml, free T4 level was 16.7±0.07 pmol/l. This group of women was prescribed l-thyroxine at a dose that allows maintaining the recommended TSH level within 3 µIU/ml.
Subsequently, in women receiving replacement therapy with l-thyroxine, a deviation during pregnancy, childbirth was not observed.
For the full physiological adaptation of the thyroid gland during pregnancy, due to the developing iodine deficiency state, all women were prescribed potassium iodide at a dose of mcg per day for preventive purposes.
Conclusions:
- Pregnancy is a provoking factor in the development of changes in thyroid function. At 396% of cases in the first trimester develop transient gestational thyrotoxicosis.
- In the second trimester of pregnancy in women with transient gestational thyrotoxicosis in the first trimester, thyroid function returns to normal.
- The combination of hypothyroidism and pregnancy is relatively rare.
 When examining pregnant women according to the MBUZ CDC, hypothyroidism was detected in 12% of cases among pregnant women.
When examining pregnant women according to the MBUZ CDC, hypothyroidism was detected in 12% of cases among pregnant women.
Literature:
1. Dedov I.I. Melnichenko G.A., Pronin V.S. and others. Clinic and diagnosis of endocrine disorders: Educational and methodological guide. - M., 2005.
2. Dedov I.I., Melnichenko G.A., Andreeva V.N. Rational pharmacotherapy of diseases of the endocrine system and metabolic disorders: A guide for practitioners / Ed. ed. I.I. Dedova, G.A. Melnichenko. - M.: Litera, 2006.
3. Sviridov N.Yu. Questions of therapy of hypothyroidism // Russian Medical Journal - 2012 - No. 13 - p. 633 – 637.
4. Helen E. Turner, John A. H. Wass. Oxford Handbook of Endocrinology and Diabetes. second edition. Oxford, University Press - 2009- P.1-83.
5. Nohr S.B., Laurberg P. Opposite variations in maternal and neonatal thyroid function induced by iodine supplementation during pregnancy // J. Clin. Endocrinol.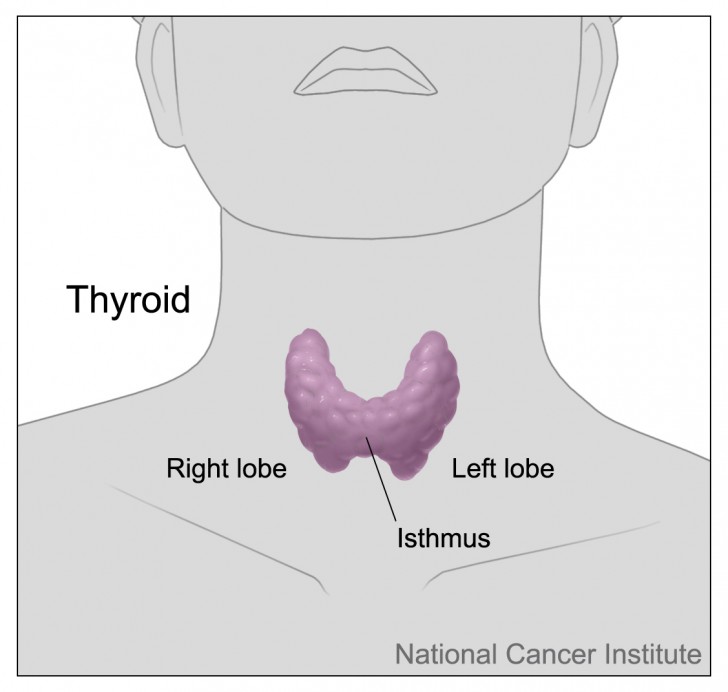 Metab. - 2000 - Vol. 85-P. .
Metab. - 2000 - Vol. 85-P. .
Table 1
Thyroid hormone levels in pregnant women in the first trimester (n=414)
| TSH ˂ 0.2 μIU/ml | TSH 04-4 µIU/ml | TSH ˃ 4 µIU/ml | T4 St. 10-23.2pmol/l | T4sv. ˃23.2 pmol/l | T4 St. ˂ 10 pmol/l | ||||||
| Abs. | % | Abs. | % | Abs. | % | Abs. | % | Abs. | % | Abs. | % |
| 164 | 39.6 | 189 | 45.6 | 49 | 12 | 189 | 45.6 | 164 | 39. | 12 | 2.8 |
Table 2
Structure of changes in the level of thyroid hormones in pregnant women registered in the first trimester (n=414)
| Indicators | Number of pregnant women | |
| Abs. | % | |
| TSH 04-4 μIU / ml + T4 St. 10-23.2pmol/l | 189 | 45.6 |
| TSH ˂ 0.2 µIU/ml + T4F. ˃23.2 pmol/l | 164 | 39.6 |
| TSH ˃ 4 μIU / ml + T4 St. 10-23.2pmol/l | 49 | 12 |
| T4 St. ˂ 10 pmol/l | 12 | 2.8 |
8)
| Indicators | Number of pregnant women | |
| Abs. | % | |
| TSH 04-4 μIU / ml + T4 St. 10-23.2pmol/l | 92 | 93.9 |
| TSH ˃ 4 μIU / ml + T4 St. 10-23.2pmol/l | 6 | 6.1 |
Severe hypothyroidism in pregnant women article on the website of the Preobrazhenskaya Clinic
Severe hypothyroidism (reduced thyroid function) in women is one of the common causes of infertility.
Also, relatively rarely, thyroid hormone deficiency occurs during pregnancy, which can adversely affect the course of pregnancy and the formation of the fetus.
The reasons
During pregnancy, the need for thyroid hormones (thyroid hormones) increases, which are necessary for the normal development of the fetus. The development of thyroid hormone deficiency is facilitated by relative iodine deficiency, which is characteristic of residents of endemic regions and the presence of latent (subclinical) hypothyroidism (decreased thyroid function) before pregnancy.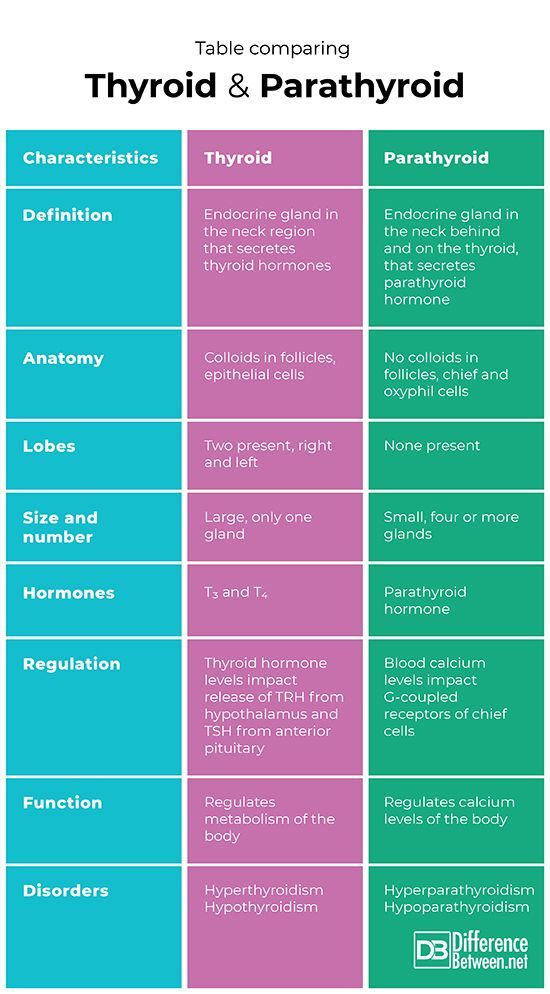
Symptoms of hypothyroidism during pregnancy:
Symptoms of the disease are nonspecific and often go unnoticed or are regarded as manifestations of pregnancy.
- general weakness
- drowsiness
- dry skin
- hair loss
- locks
- frequent infections
- slow heart rate - less than 60 beats / min.
Why is hypothyroidism dangerous for a pregnant woman:
- Adverse effects on the development of the central nervous system of the fetus and possible impairment of the mental activity of the child subsequently.
- Violation of the formation of the thyroid gland of the fetus - congenital hypothyroidism in a child
- Hypothyroidism increases the risk of spontaneous abortion and stillbirth.
- Pregnancy often complicated by anemia, pre-eclampsia
- Weak labor activity
- Bleeding in the postpartum period
Diagnosis of hypothyroidism during pregnancy:
To diagnose thyroid hormone deficiency during pregnancy (1 time per trimester) and timely treatment, it is necessary to determine the level of thyroid-stimulating hormone - TSH.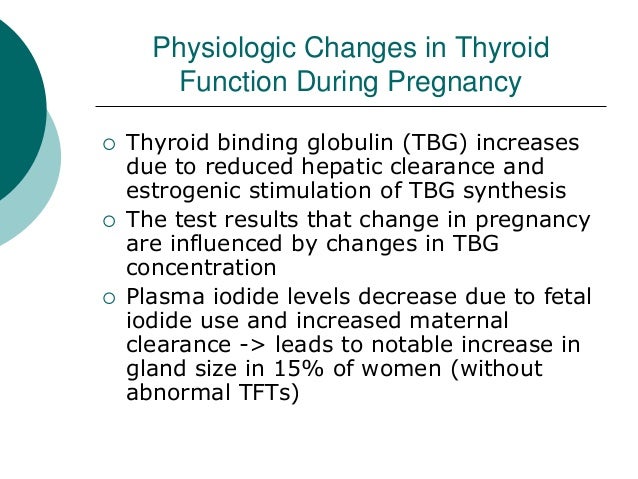
 6
6