Baby has red arms like sunburn
Serious childhood rashes | Pregnancy Birth and Baby
Serious childhood rashes | Pregnancy Birth and Baby beginning of content8-minute read
Listen
Take your child to the doctor urgently if they have a rash together with a high temperature, cold or cough symptoms, or swollen neck glands.
Key facts
- Many rashes are harmless, but a rash on your child’s skin might indicate a serious condition that requires urgent medical treatment.
- You can protect your child from some of these diseases, including measles, chickenpox and some types of meningococcal disease, with routine immunisations.
- You should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms, or swollen neck glands.
- If your child has a meningococcal rash, go immediately to the closest hospital emergency department.
Is my child’s rash serious?
Many rashes are harmless, but a rash on your child’s skin might indicate a serious condition that requires medical treatment. You should take your child to the doctor if they have a rash together with a high temperature, cold or cough symptoms, or swollen neck glands.
You can protect your child against some of these diseases, including measles, chickenpox and some types of meningococcal disease, with routine vaccination.
Learn more about common childhood rashes that are not serious.
What is meningococcal rash?
If you think your child might have meningococcal rash, seek medical attention immediately or call triple zero (000) and ask for an ambulance.
Meningococcal rash is a sign that your child is infected with meningococcal bacteria, which is not common but very serious. This is a medical emergency, as meningococcal disease can be life threatening.
This is a medical emergency, as meningococcal disease can be life threatening.
A meningococcal rash appears as tiny red or purple pinpricks that spread into blotches. The rash is a non-blanching rash. This means that when you press on the rash it doesn’t disappear.
Your child might also:
- have a fever
- refuse to eat or drink
- be unhappy or drowsy
- be sensitive to light
- have pale or blotchy skin
These symptoms can appear before the rash.
If your child has meningococcal disease, they will likely be admitted to hospital so they can be monitored and given intravenous (IV) antibiotics.
What is measles?
Measles is a highly contagious viral disease that can lead to serious complications. It is rare in Australia, but travellers from overseas or unvaccinated people can spread measles. You can protect your child from catching measles by making sure they are up to date with their regular childhood vaccinations.
At first, measles can seem like just a cold. Your child might have a cough and sore, watery eyes. They might also have tiny white spots inside their mouth. After 3 or 4 days, a rash of red, slightly raised spots appears. These are not itchy.
Call your doctor if you think your child may have measles. To avoid infecting others, your doctor may ask you to come to the clinic when other patients are not are around. They may also take you and your child to a separate room.
Talk to your pharmacist or doctor about treatments that can treat the fever, coughing and other symptoms.
Children with measles are contagious for a week after the spots appear. During this time, keep your child home from childcare or school, and away from other people as much as possible.
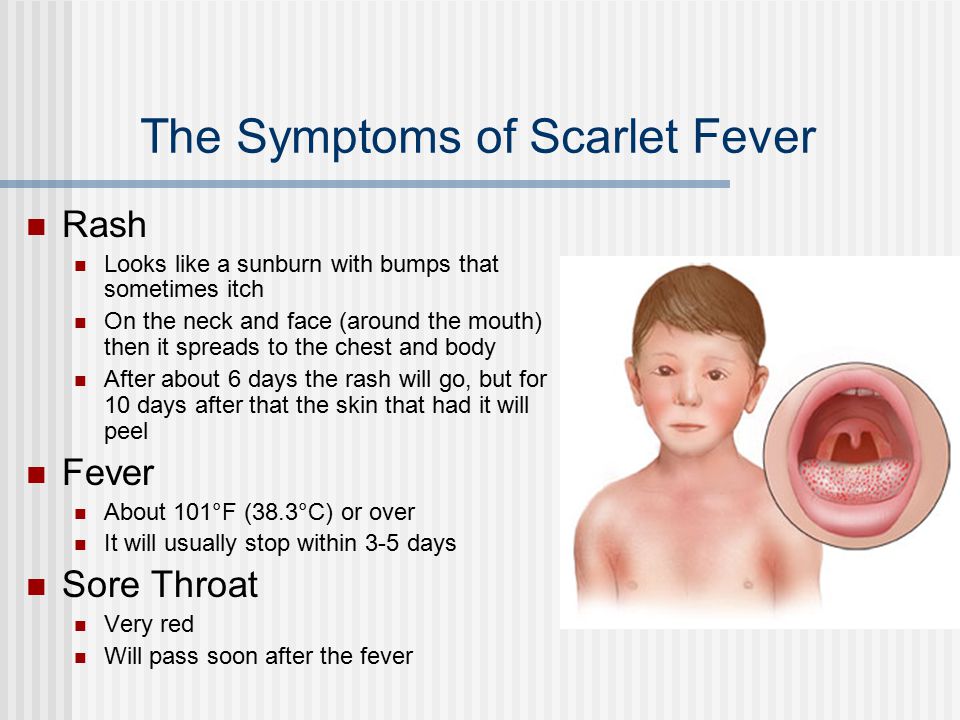
What is scarlet fever?
Scarlet fever is a contagious infection of the throat caused by the bacteria Group A streptococcus. Scarlet fever can easily be treated with antibiotics. Antibiotics will help prevent the bacteria from spreading to other parts of the body and causing serious health problems.
Antibiotics will help prevent the bacteria from spreading to other parts of the body and causing serious health problems.
Scarlet fever usually begins with a sore throat, fever, swollen tonsils and swollen glands in the neck. Within 1 to 2 days, a rough, red rash that looks like sunburn develops on the body and limbs. It usually lasts 3 to 5 days. Your child might also develop a very red tongue and feel unwell.
If you think your child has scarlet fever, take them to your doctor. With antibiotics, they will usually recover quickly. Keep them away from childcare or school until at least 24 hours after starting antibiotic treatment.
What is chickenpox?
Chickenpox is a highly contagious viral infection. It is usually mild, but can lead to serious complications. Vaccination is the best way to protect your child from catching chicken pox.
Chickenpox rash develops as red, itchy spots that turn into fluid-filled blisters. There may be many blisters or just a few. The blisters dry up and form scabs (usually within 5 to 6 days), which then drop off. Your child might feel unwell and have a mild fever. Scratching the spots can cause scars, but you can treat them with calamine lotion to reduce the itch.
The blisters dry up and form scabs (usually within 5 to 6 days), which then drop off. Your child might feel unwell and have a mild fever. Scratching the spots can cause scars, but you can treat them with calamine lotion to reduce the itch.
Take your child to the doctor if their blisters get infected or if your child becomes increasingly unwell.
Children are contagious until all the blisters have dried up. During this time, keep your child home from childcare or school. Try to keep them away from newborn babies, people with a weak immune system. If you are pregnant or trying to get pregnant, stay away from people with chickenpox, as your unborn baby could be affected.
What is psoriasis?
Psoriasis is a long-term condition caused by an overactive immune system. It may develop as only a few dry, red, scaly patches (known as 'plaques') on the skin, or plaques that cover large areas of the body. Psoriasis is not contagious.
Psoriasis can come and go, or it can be a life-long condition.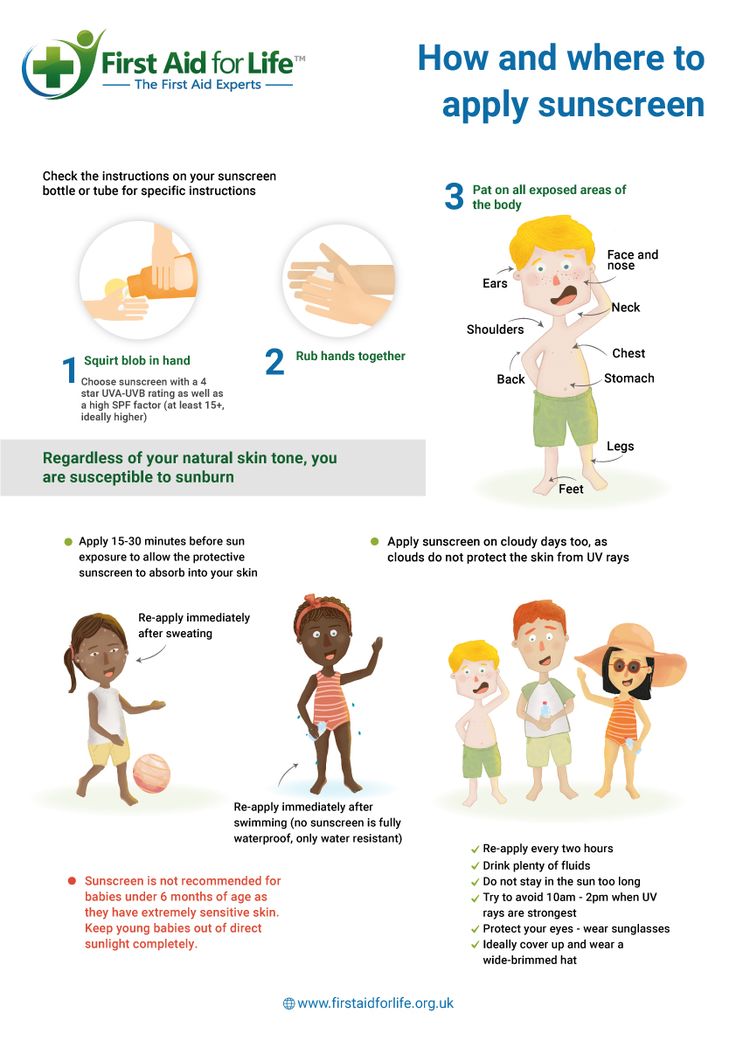 There is no cure, but it can usually be controlled with treatment. Severe psoriasis can be difficult to manage and is associated with other health problems such as Crohn’s disease, diabetes and heart disease.
There is no cure, but it can usually be controlled with treatment. Severe psoriasis can be difficult to manage and is associated with other health problems such as Crohn’s disease, diabetes and heart disease.
If you think your child might have psoriasis, see your doctor. They may refer you to a dermatologist who can help you manage the condition.
What is monkeypox?
Monkeypox was first reported in Australia in May 2022. It is a rare but potentially serious viral illness. The illness usually begins with fever, swollen lymph nodes, headache and muscle, back and joint pain. A rash usually develops 1 to 3 days after the fever begins. The rash tends to be mainly on the face, arms and legs.
The virus is transmitted from person to person through close contact with skin sores, through respiratory droplets (for example, by coughing and sneezing) or through contaminated sheets and towels.
Infants, young children, older people and people with a weak immune system are at risk for developing severe disease.
If your doctor thinks you have monkeypox, they will ask about your symptoms and examine you. They may also send you for tests. Medical experts are currently developing guidelines on the use of vaccines and treatments for monkeypox in Australia.
If you have returned to Australia after travelling overseas to areas with cases of monkeypox and you think you may be at risk, contact a doctor immediately.
Not sure what to do next?
If you are still concerned, check your symptoms with healthdirect’s online Symptom Checker to get advice on when to seek medical attention.
The Symptom Checker guides you to the next appropriate healthcare steps, whether it’s self care, talking to a health professional, going to a hospital or calling triple zero (000).
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Government of Western Australia (Scarlet fever), Public Health Research & Practice (Describing meningococcal disease), Sydney Children’s Hospital Network (Meningococcal infection), The Sydney Children's Hospitals Network (Chickenpox), Australian Government Department of Health (Measles), Australasian College of Dermatologists (A-Z of skin: Psoriasis), Australian Government Department of Health (Monkeypox MPX), Australian Government Department of Health (Chickenpox varicella)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Need more information?
Recognising serious illness in children
Trusted advice on serious symptoms and illnesses in babies and children including high fevers, diabetes, meningitis, and when to seek professional advice.
Read more on Pregnancy, Birth & Baby website
Common childhood rashes
Childhood rashes are common and many disappear without treatment. Learn about symptoms and treatment of childhood rashes, such as eczema, ringworm and impetigo.
Read more on Pregnancy, Birth & Baby website
Childhood rashes - Oral thrush
Oral thrush is a type of fungus infection, very common among babies. It appears as moist, milky-white patches in and around a child's mouth. Usually oral thrush is not serious and can sometimes even go unnoticed.
Read more on Pregnancy, Birth & Baby website
Childhood rashes - MyDr.com.au
Distinguish between the childhood rashes of rubella (German measles), measles, chickenpox and fifth disease ('slapped cheek' disease).
Read more on myDr website
Childhood rashes - Eczema
Eczema is a common chronic skin condition in children. Typically, eczema is characterised by an itchy rash that comes and goes. Eczema is not contagious but does tend to run in families and commonly first appears in early childhood.
Read more on Pregnancy, Birth & Baby website
Measles in children and teenagers | Raising Children Network
Measles can be very serious. Symptoms include a runny nose, fever and rash. Immunisation protects your child, but children can still get measles.
Read more on raisingchildren.net.au website
Serious childhood illnesses: 0-3 years | Raising Children Network
Symptoms of serious illness in babies and young children include severe drowsiness, breathing difficulty, blue skin, seizures, fever and frequent vomiting.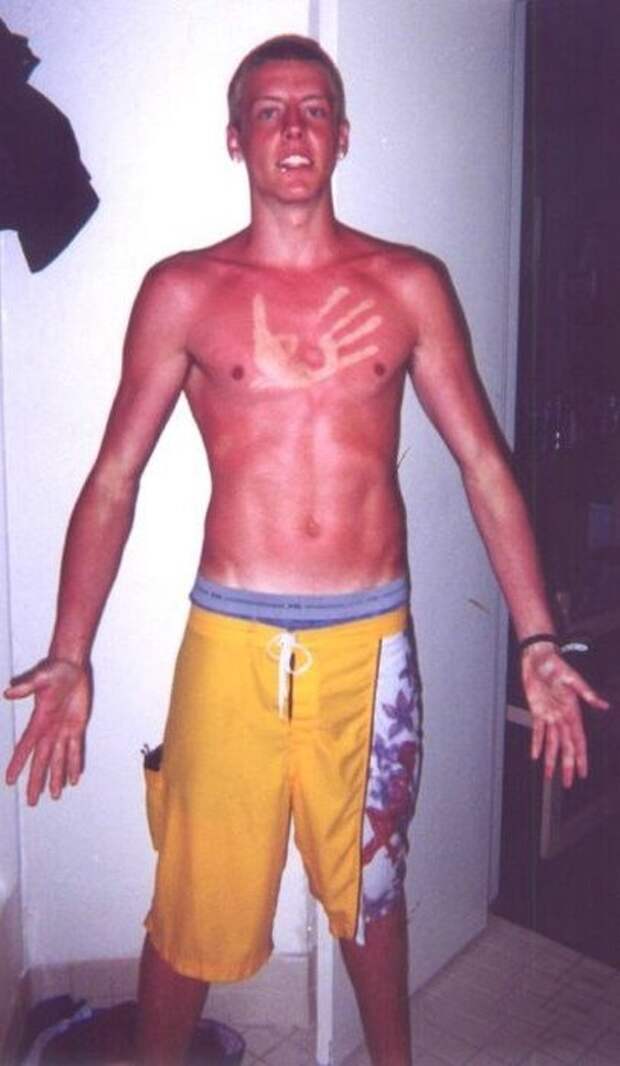
Read more on raisingchildren.net.au website
How to tell if your child is sick
Here is some helpful guidance on how to tell if your child is unwell, common symptoms and childhood illnesses and when you should seek further advice.
Read more on Pregnancy, Birth & Baby website
Hand, foot and mouth disease
Find out what is hand, foot and mouth disease and links to trusted information on its symptoms, diagnosis and treatment.
Read more on Pregnancy, Birth & Baby website
Chickenpox in adults - MyDr.com.au
For those adults who didn't catch chickenpox in childhood, or who haven't been vaccinated, an attack of chickenpox can produce serious, sometimes lethal, complications.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Rash or Redness - Localized
Is this your child's symptom?
- Red or pink rash on one small part of the body (localized)
- Small spots, large spots or solid redness
- Includes redness from skin irritation
Causes of Localized Rash or Redness
- Irritants. A rash in just one spot is usually caused by skin contact with an irritant.

- Plants. Many plants cause skin reactions. Sap from evergreens can cause a red area.
- Pollen. Playing in the grass can cause a pink rash on exposed skin.
- Pet Saliva. Some people get a rash where a dog or cat has licked them.
- Food. Some children get a rash if a food is rubbed on the skin. An example could be a fresh fruit. Some babies get hives around the mouth from drooling while eating a new food.
- Chemicals. Many of the products used in the home can be irritating to the skin.
- Insect Bite. Local redness and swelling is a reaction to the insect's saliva. Can be very large without being an allergy. Kids often get mosquito bites without anyone noticing it.
- Bee Sting. Local redness and swelling is a reaction to the bee's venom. Can be very large without being an allergy.
- Cellulitis. This is a bacterial infection of the skin.
 The main symptom is a red area that keeps spreading. Starts from a break in the skin (such as a scratched insect bite). The red area is painful to the touch.
The main symptom is a red area that keeps spreading. Starts from a break in the skin (such as a scratched insect bite). The red area is painful to the touch. - Other Common Causes. Look at the "See Other Care Guide" section. 8 rashes that you may be able to recognize are listed there. If you suspect one of them, go there. If not, use this guide.
Localized Versus Widespread Rash: How to Decide
- Localized means the rash occurs on one small part of the body. Usually, the rash is just on one side of the body. An example is a rash on 1 foot. Exceptions: athlete's foot can occur on both feet. Insect bites can be scattered.
- Widespread means the rash occurs on larger areas. Examples are both legs or the entire back. Widespread can also be on most of the body surface. Widespread rashes always occur on matching (both) sides of the body. Many viral rashes are on the chest, stomach and back.
- The cause of a widespread rash usually goes through the blood stream.
 Examples are rashes caused by viruses, bacteria, toxins, and food or drug allergies.
Examples are rashes caused by viruses, bacteria, toxins, and food or drug allergies. - The cause of a localized rash usually is just from contact with the skin. Examples are rashes caused by chemicals, allergens, insect bites, ringworm fungus, bacteria or irritants.
- This is why it's important to make this distinction.
Contact Dermatitis
Contact dermatitis is a common cause of a rash in one area. This is especially true of a small rash that will not go away. Contact dermatitis usually starts as raised red spots. It can change to blisters, as in poison ivy. The rash is itchy. Contact dermatitis is an allergic skin rash. The location of the rash may suggest the cause:
- Poison ivy or oak: exposed areas, such as the hands.
- Nickel (metal): anywhere the metal has touched the skin. (Neck from necklaces, earlobe from earrings, or fingers from rings. Stomach from metal snap inside pants, wrist from watch, or face from eyeglass frames.
 )
) - Tanning agents in leather: tops of the feet from shoes or hands from leather gloves
- Preservatives in creams, lotions, cosmetics, sunscreens, shampoos: where applied
- Neomycin in antibiotic ointment: where applied
When to Call for Rash or Redness - Localized
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Purple or blood-colored spots or dots that are not from injury or friction
- Age less than 1 month old and tiny water blisters
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Bright red area or red streak (but not sunburn)
- Rash is very painful
- Fever is present
- Severe itching
- Looks like a boil, infected sore or other infected rash
- Teenager with a rash on the genitals
- Lyme disease suspected (bull's eye rash and tick bite or contact)
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Blisters without a clear cause.
 Exception: Poison Ivy.
Exception: Poison Ivy. - Pimples (Use an antibiotic ointment until seen)
- Rash grouped in a stripe or band
- Peeling fingers
- Rash lasts more than 7 days
- You have other questions or concerns
Self Care at Home
- Mild localized rash or redness
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Localized Rashes
- What You Should Know About Localized Rashes:
- Most new localized rashes are due to skin contact with an irritating substance.

- Here is some care advice that should help.
- Most new localized rashes are due to skin contact with an irritating substance.
- Avoid the Cause:
- Try to find the cause.
- Consider irritants like a plant (such as evergreens or weeds). Also, chemicals (such as solvents or insecticides). Irritants also can include fiberglass or detergents. A new cosmetic or new jewelry (such as nickel) may also be the cause.
- A pet may carry the irritant, as with poison ivy or oak. Also, your child could react directly to pet saliva.
- Review the list of causes for contact dermatitis.
- Do Not Use Soap:
- Wash the red area once with soap to remove any remaining irritants.
- Then, do not use soaps on it. Reason: Soaps can slow healing.
- Cleanse the area when needed with warm water.
- Cold Soaks for Itching:
- Use a cold wet washcloth or soak in cold water for 20 minutes.
- Do this every 3 to 4 hours as needed. This will help with itching or pain.

- Steroid Cream for Itching:
- If the itch is more than mild, use 1% hydrocortisone cream (such as Cortaid). Put it on the rash.
- No prescription is needed.
- Use it 3 times per day.
- Exception: Do not use for suspected ringworm.
- Try Not to Scratch:
- Help your child not to scratch.
- Cut the fingernails short.
- Return to School:
- Children with localized rashes do not need to miss any child care or school.
- What to Expect:
- Most of these rashes go away in 2 to 3 days.
- Call Your Doctor If:
- Rash spreads or gets worse
- Rash lasts for more than 1 week
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 11/05/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Photodermatosis: a common sun allergy
Summer sun dermatitis, often referred to as sun allergy, is the most common form of photodermatosis. This disease is caused by increased sensitivity of the skin to ultraviolet radiation and is caused by exposure to sunlight. This phenomenon is not rare today - about 20% of the population worldwide faces photodermatosis. Allergies show up as small red itchy dots. This usually happens after 12 hours. Relapses are often inevitable. Sun allergies can be more severe: more dots, more itching, and more affected areas.
Sun allergies are very common in women between the ages of 15 and 35. It causes discomfort and negatively affects the appearance, is expressed in the appearance of small red spots that cause intense itching and burning. On the face, these spots usually do not appear, but they are on the neck, shoulders, arms and legs. Other symptoms of photodermatosis: peeling of the skin, rashes in the form of papules or folliculitis (pustules), prolonged pigmentation in the affected areas.
On the face, these spots usually do not appear, but they are on the neck, shoulders, arms and legs. Other symptoms of photodermatosis: peeling of the skin, rashes in the form of papules or folliculitis (pustules), prolonged pigmentation in the affected areas.
Often the symptoms do not appear immediately. Unlike sunburn, photodermatosis can develop only a few hours after returning home (phototoxic reaction), and sometimes even after a few days (photoallergic reaction).
Photodermatosis is caused by ultraviolet rays, especially UVA rays. Their negative impact is increased by deodorants, perfumes, ointments and creams that were applied to sensitive skin before sun exposure. Some substances in perfumes and cosmetics can react with ultraviolet light and cause allergies. This property has, for example, eosin contained in lipstick, and para-aminobenzoic acid, which is part of some sunscreens. Other substances have a similar effect: phenol, retinoids, salicylic, boric and polyunsaturated fatty acids, parsley juice, rose oil, bergamot, musk, St. John's wort and sandalwood.
John's wort and sandalwood.
It is not uncommon for medications to cause symptoms of sun allergy. In particular: barbiturates, antihistamines, cytostatics, oral contraceptives, hormone replacement therapy drugs, sulfonamides, chlorpromazine, certain cardiovascular drugs, certain antibiotics and certain anti-inflammatory drugs. An increased reaction to ultraviolet light is also manifested in the case of a decrease in the protective function of the skin due to additional exposure to it (for example, peeling, cosmetic manipulations). Often the cause of photodermatosis is a violation of the hepatobiliary and gastrointestinal tract.
And there is only one way to solve this problem - to prevent its occurrence. The ideal solution is to avoid the sun or wear protective clothing. If the sun cannot be avoided:
- do not sunbathe between 11.00 – 16.00
- before going to the beach, do not use perfumes and creams containing alcohol
- sunbathe gradually (20-30 minutes a day)
- Use a broad spectrum sunscreen with a strong protection factor (against UVA and UVB rays).
 The first days only on limited areas of the skin. And only after making sure that there is no photodermatosis, when applying these products to certain areas of the skin, use them on all surfaces of the skin.
The first days only on limited areas of the skin. And only after making sure that there is no photodermatosis, when applying these products to certain areas of the skin, use them on all surfaces of the skin. - reapply the cream every two hours
- if it was still not possible to avoid negative effects on the skin, and there is no way to consult a doctor, you can remove the acute manifestations of photodermatosis using cold lotions and special after-sun products containing panthenol. It is better and more effective to seek help from a dermatologist or allergist.
- in the period of exacerbation of allergies, follow a hypoallergenic diet, exclude the intake of alcoholic beverages.
It is important to take every precaution to achieve the best possible result.
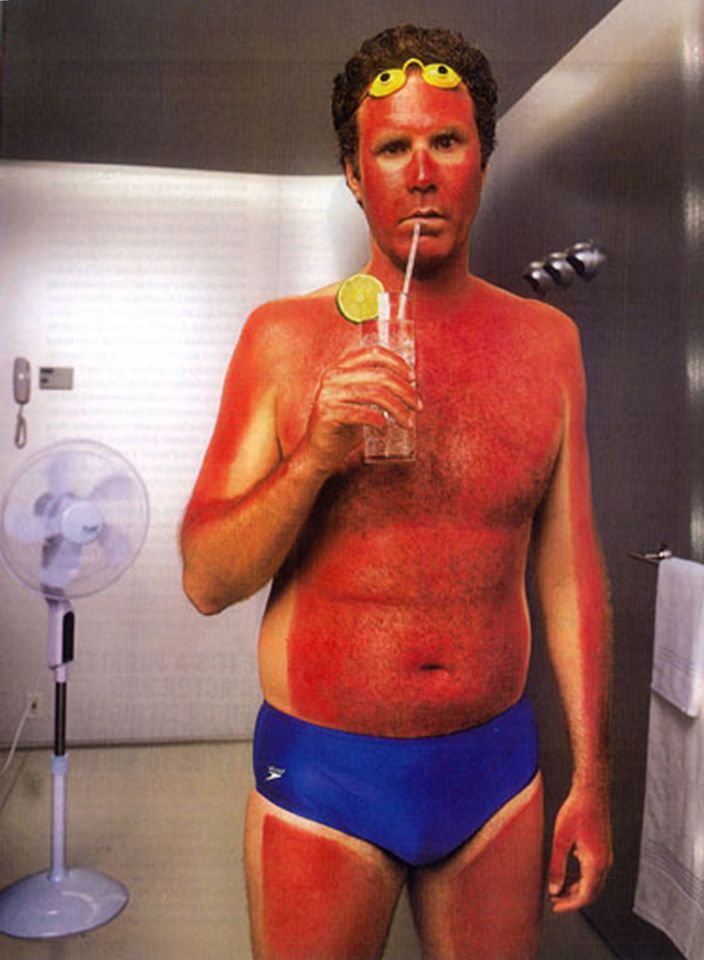
Sunburn symptoms, sunburn treatment folk remedies
It is widely believed that sunburn is just a minor nuisance that is not worth much attention. However, this concept is erroneous, because in addition to discomfort and pain, sunburn can lead to skin cancer. A direct link between sun exposure and the development of malignant melanoma has long been proven.
A direct link between sun exposure and the development of malignant melanoma has long been proven.
What is sunburn?
Sunburn is red, sometimes swollen and painful skin caused by overexposure to the ultraviolet (UV) rays of the sun. Sunburn can range from mild to severe.
The degree depends on the type of skin and the amount of sun exposure. In total, there are 6 types of skin according to the degree of sensitivity.
Types 1 and 2: High sensitivity.
The first type of is blond or redheaded with very fair (pale or milky white) skin (possibly freckled) that never tans. Such people can get burned by being under the midday summer sun for less than half an hour.
Skin type 2 slightly darker, able to get a slight tan, but burns easily if exposed to the sun for a short time.
Types 3 and 4: Medium sensitivity.
Skin type 3 (Central European) - darker than skin type 2. Being in the sun, its owners can get a moderate burn or a light brown tan.
Being in the sun, its owners can get a moderate burn or a light brown tan.
Type four leather olive color, low burn risk. Tans well to medium brown.
Types 5 and 6: Low sensitivity
Type 5 skin dark. Burns are rare, tan is dark.
People with skin type six have very dark skin and never burn.
Sunburn symptoms
Sunburn symptoms appear a couple of hours after exposure to the sun. However, it may take up to 24 hours for the full effect of skin damage to appear. Long-term damage, such as an increased risk of skin cancer, may take years to appear.
They include:
- pain;
- redness of the skin;
- edema;
- blisters;
- nausea;
- chills or fever;
- temperature increase.
The severity of symptoms depends on the degree of skin damage.
Mild sunburn
Mild sunburn is usually accompanied by redness and slight pain and can last three to five days. In the last couple of days, the skin may peel off a little as it regenerates.
In the last couple of days, the skin may peel off a little as it regenerates.
Mild sunburn
Mild sunburn is usually more painful. The skin becomes red, swollen and hot to the touch. It usually takes about a week for complete healing. The skin may then continue to peel off for a few more days.
Severe sunburn
Severe sunburn sometimes requires a visit to a doctor or even a hospital. Painful blisters and very red skin appear. Full recovery may take up to two weeks.
What is the risk of sunburn?
Intense sun exposure that causes sunburn increases the risk of other skin damage and diseases. These include premature aging of the skin (photoaging), precancerous skin lesions, and skin cancer.
Skin photoaging.
Sun exposure causes premature skin aging and wrinkles. It happens like this:
Sunlight destroys the collagen and elastin fibers in the skin, which make it supple and smooth.
Damaged skin loses its ability to regenerate itself.
Premature aging (photoaging) occurs.
Negative effects of UV radiation on the skin of the face:
- Wrinkles.
- Increased pigmentation - this is due to the fact that melanin is distributed unevenly, so it is delivered in excess to some areas.
- Vitiligo is a chronic skin disease. Against the background of the destruction of melanin in the body, the number of melanocytes decreases, the dermis loses its natural pigmentation, and as a result, white spots appear on certain areas of the skin.
- Permanent yellowing of certain areas of the skin.
- The appearance of spider veins on the face.
- Elastosis is the destruction of elastin cells, which are already produced in a minimal amount with age. This leads to a loss of elasticity and firmness of the skin, in other words, the skin sags and becomes flabby.
Premalignant skin lesions.
Premalignant skin lesions appear as rough, scaly patches on sun-damaged areas. They are commonly found on sun-exposed areas of the head, face, neck, and hands of fair-skinned people. These spots can develop into skin cancer. They are also called actinic keratoses and solar keratoses.
Skin cancer.
Sunburn increases the risk of skin cancer, including melanoma. Melanoma is one of the most dangerous malignant human tumors, as it spreads rapidly, metastasizes throughout the body and is poorly treated in the last stages. The main reason for the occurrence is excessive UV radiation, which damages the DNA of skin cells. Errors in the structure of cellular DNA accumulated since childhood disrupt and deplete the skin's sun protection function, increasing the risk of skin cancer in adulthood.
Sunburn is a major risk factor for melanoma, increasing by 50% if a person has had more than 5 severe sunburns in their lifetime.
When should I see a doctor for sunburn?
Seek medical attention if sunburn:
- causes severe swelling;
- does not improve within a few days;
- there are signs of infection in the blisters, such as pain, pus, swelling, and tenderness;
- blisters covering most of the body;
- blisters appear on the face, hands or genitals.
What to do with blisters after sunburn?
- Do not touch the damaged area. Do not attempt to pop the blisters, they will eventually burst on their own. In no case should they be forced to burst ahead of time - there is a risk of infection in the wound.
- If the blister bursts on its own , cover the resulting wound with a bandage to prevent infection. If you think that the infection has already entered the wound, consult a dermatologist.
Signs that indicate infection:
- redness;
- swelling of the wound;
- pain and fever.
Get emergency medical help if you get sunburned and experience:
- Fever.
- Confusion of consciousness.
- Fainting.
- Dehydration.
Sunburn treatment
- Apply after sun. Aloe vera lotion or cream is best for reducing burning sensation and restoring the skin.
- Cooling. A cold compress, ice pack, cold shower or bath will soothe the skin. Do not apply ice directly to your naked body, wrap it in a towel or rag first. Repeat the procedure several times, depending on how severe the burn is.
- Moisturizing. As the edema subsides, skin peeling appears, the purpose of the treatment procedures is to moisturize and accelerate regeneration. The most affordable remedy is panthenol.
- Drink plenty of water. To prevent sun exhaustion and dehydration, you need to drink plenty of water.
- Reduce inflammation.
 Pain medication (Ibuprofen or Aspirin) can be taken to reduce inflammation and pain.
Pain medication (Ibuprofen or Aspirin) can be taken to reduce inflammation and pain.
Avoid sunburn
There are many traditional treatments for sunburn.
Service Doc.ua DOES NOT recommend the following folk remedies for burns:
- Treat burns with sour cream, kefir or curdled milk, applying them to the burnt skin surface.
- Lubricate affected skin with lotion or oil, and margarine.
- Apply to the affected area urine, alcohol, cologne, ointments not intended for the treatment of burns.
The use of such products may lead to deterioration of the condition, as well as infection of the skin.
Is it possible to peel off the skin after a burn?
DO NOT blister or peel skin that is flaky. When the skin rejects the damaged area (flakes), it works to heal itself by forming a new layer of skin underneath. If you peel off the skin before it is ready to be shed, you hinder the renewal process and open the skin to infections.