Pregnancy and yeast infection treatment
Answers to 6 burning questions about yeast infection during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 20, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
Vaginal candidiasis, also known as a yeast infection, can be a real pain. The itching, burning, and discharge can be especially worrisome during pregnancy.
In most cases, though, vaginal yeast infections and most treatment options pose minimal risk to the patient or pregnancy.
After bacterial vaginal infections, yeast infections are the second most common cause of vaginal inflammation, and 75% of women will have at least one in their lifetime. Common symptoms can include redness, itching, or irritation on the external genital area (vulva), an increase in white or tan vaginal discharge, and a burning sensation during urination or intercourse.
There are a range of over-the-counter and prescription treatments, and an Ob/Gyn or gynecologist can help you choose the safest, most effective option during pregnancy.
I’ve invited Meredith McClure, M.D., a UT Southwestern gynecologist, to answer the top questions pregnant and breastfeeding patients ask about yeast infection treatment and prevention.
Meredith McClure, M.D.Q: How common are yeast infections during pregnancy?
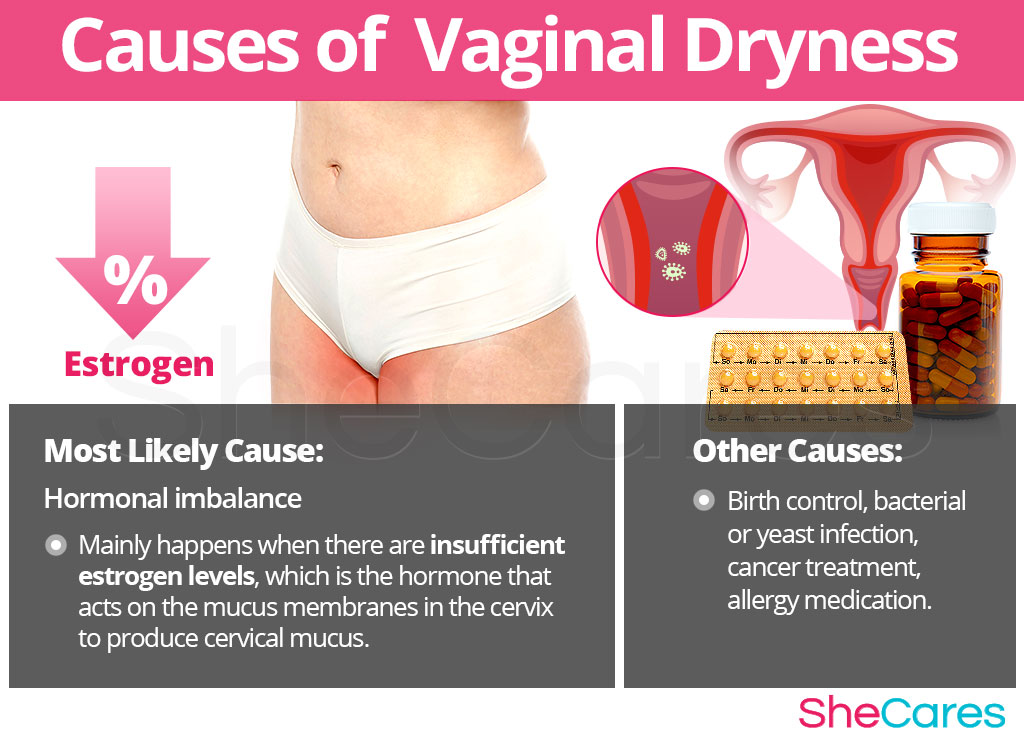
A: Studies have found that 20%-30% of women develop a yeast infection during pregnancy. An increase in the hormone estrogen creates a more hospitable climate for yeast to colonize the vagina because it binds to the protein factor H on the surface of the cells that cause vulvovaginal candidiasis.
Some women are more likely to develop yeast infections due to their genetics. Mutations of several genes can interfere with the immune system’s ability to defend against candida yeast, resulting in recurring infections for some people.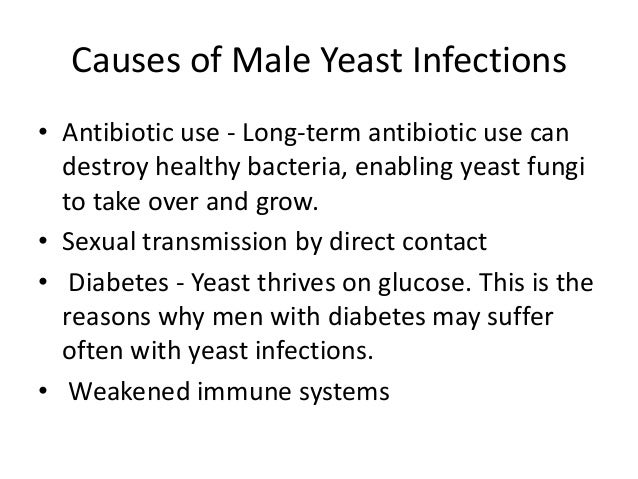 This inherited predisposition is called familial candidiasis.
This inherited predisposition is called familial candidiasis.
Q: Can a yeast infection harm my pregnancy?
A: No. A yeast infection won’t affect your developing baby – that’s why we don’t treat yeast infections that don’t have symptoms. However, most symptomatic yeast infections get worse when left untreated. This means more itching, redness, and inflammation. If the skin becomes cracked or torn from repeated scratching, a skin infection can result. In rare cases, an untreated yeast infection can lead to fatigue, oral thrush, or digestive problems.
Q: Do yeast infections appear throughout pregnancy?
A: Yeast infections can occur any time, but they are most common during the second trimester. Talk with your doctor if you notice signs of a yeast infection while pregnant, even if you have had one before. Some more serious infections have similar symptoms, so your doctor will perform a simple fungal culture swap in the office to check for the presence of yeast.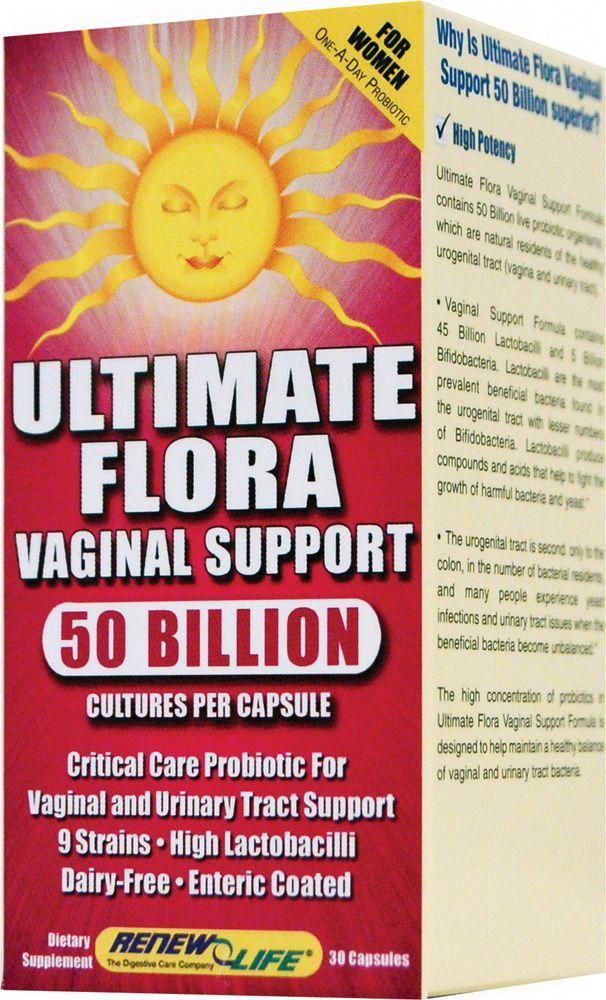
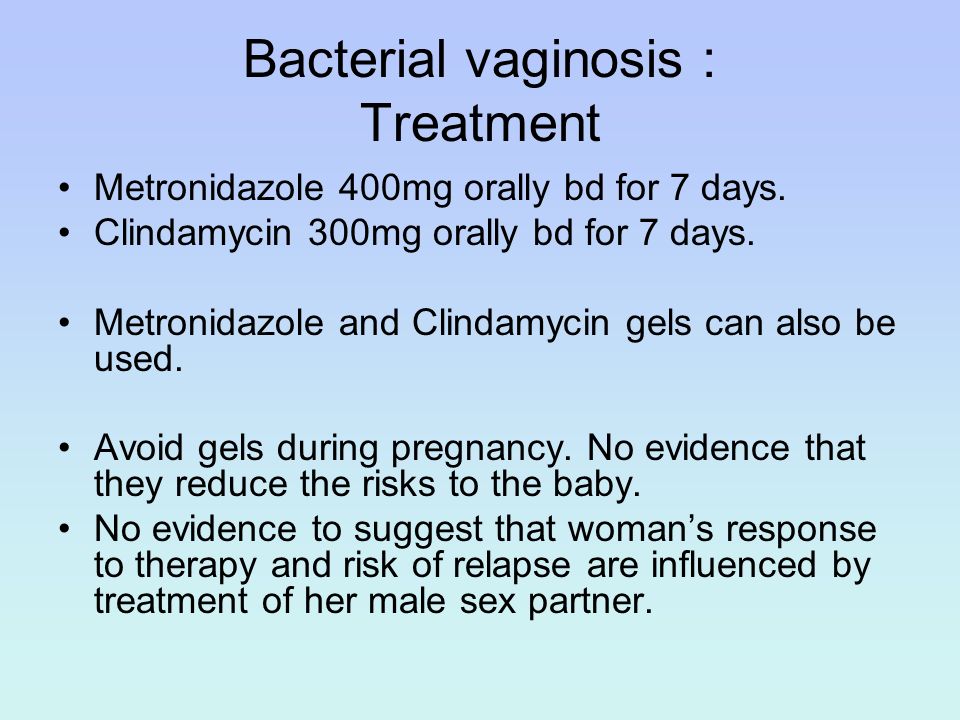
Q: What treatment options are available?
Talk with your doctor about the safest and most effective options for treating yeast infections during pregnancy.A: Topical creams or vaginal suppositories are the recommended yeast infection treatment options during pregnancy or while breastfeeding. Over-the-counter medications such as Miconazole, Clotrimazole, and Terconazole have been shown to eliminate a yeast infection safely and effectively. They are usually applied for three to seven days. It is important to finish the entire course of medication to prevent the infection from coming back. Studies have demonstrated these medications are safe to use during pregnancy.
The oral medication Diflucan (fluconazole) is not recommended for most patients during pregnancy. Though taking a single pill is simpler, quicker, and less messy, some studies suggest fluconazole carries a slightly increased risk of miscarriage, birth defects, or stillbirth, especially at high doses taken over long periods of time.
While the increase is small – approximately 12 incidents per 10,000 births – the convenience of single-pill treatment might not outweigh the risk. However, in the event you have already taken or need to take fluconazole while pregnant, the additional risk at a normal dose is unlikely to pose any problems for your baby.
Q: Are yeast infection treatments safe while breastfeeding?
A: Yeast infections are less common among breastfeeding patients because estrogen levels drop dramatically in the postpartum period, making it hard for yeast to thrive. But if they occur, fluconazole may be taken by women who are breastfeeding as the levels secreted into breast milk are small.
It is possible for a breastfeeding mother and baby to pass thrush, a fungal infection that typically grows in the mouth and throat, back and forth between nipple and mouth. If that happens, both must be treated to stop the infection. Thrush is usually minor and is often caused by the same fungus – and treated with a 7- to 14-day course of the same antifungal medicines – as a yeast infection in the vagina.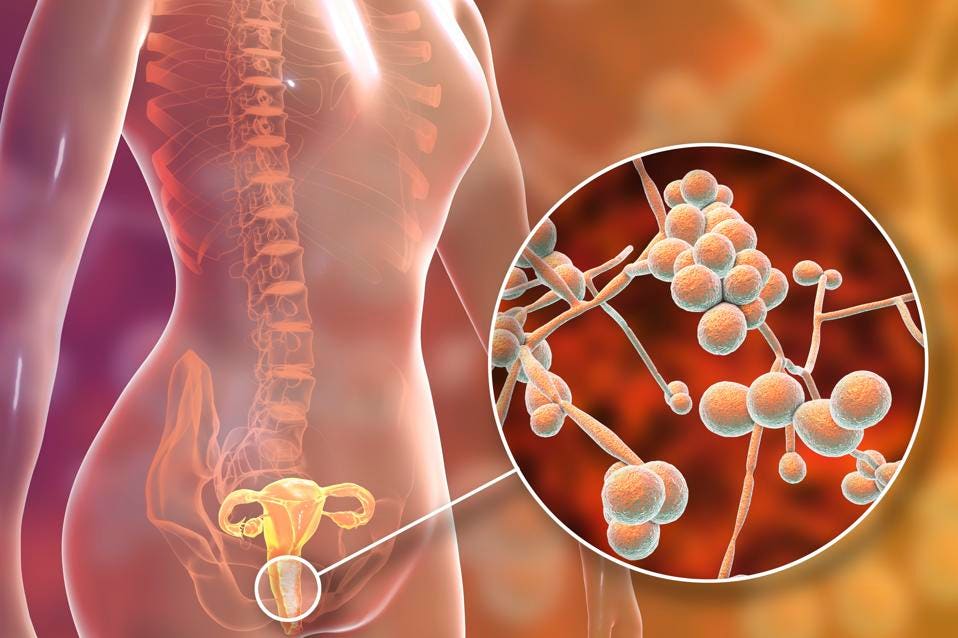
Q: What steps can reduce the risk of yeast infection?
A: During pregnancy and otherwise, take the following precautions:
- Wipe front to back after using the toilet.
- Avoid using scented tampons, pads, and pantyliners.
- Change tampons, pads, and pantyliners often.
- Avoid very hot baths and hot tubs.
- Wear underwear with a cotton lining to promote airflow.
- Do not douche, which removes healthy vaginal bacteria that prevent infection.
- Wear loose fitting clothing.
- Manage your blood sugar if you have diabetes or gestational diabetes.
- Remove wet workout clothes and swimsuits as soon as possible after activities.
If you’re pregnant and notice signs of a yeast infection, discuss treatment options with your doctor so you can eliminate these disruptive symptoms. To request an appointment, call 214-645-8300 or request online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
March 14, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
February 14, 2023
Your Pregnancy Matters
- Melissa Mauskar, M.D.
February 7, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
January 31, 2023
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
- Kyler Elwell Silver, M.D.
January 24, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
January 10, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 20, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 13, 2022
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.
 D.
D.
December 6, 2022
More Articles
Vaginal yeast infections during pregnancy
1. Das Neves J, Pinto E, Teixeira B, Dias G, Rocha P, Cunha T, et al. Local treatment of vulvovaginal candidosis: general and practical considerations. Drugs. 2008;68(13):1787–802. [PubMed] [Google Scholar]
2. Ferrer J. Vaginal candidosis: epidemiological and etiological factors. Int J Gynaecol Obstet. 2000;71(Suppl 1):S21–7. [PubMed] [Google Scholar]
3. Eschenbach DA. Chronic vulvovaginal candidiasis. N Engl J Med. 2004;351(9):851–2. [PubMed] [Google Scholar]
4. Monif GR, Baker DA. Candida albicans. In: Monif GR, Baker DA, editors. Infectious diseases in obstetrics and gynecology. 5th ed. New York, NY: Parthenon Press; 2003. pp. 405–21. [Google Scholar]
5. Baron EJ, Cassell GH, Duffy LB, Eschenbach JR, Greenwood SM, Harvey NE, et al. Laboratory diagnosis of female genital tract infections. In: Baron EJ, editor. Cumulative techniques and procedures in clinical microbiology (Cumitech) 17A. Washington, DC: ASM Press; 1993. pp. 1–28. [Google Scholar]
Laboratory diagnosis of female genital tract infections. In: Baron EJ, editor. Cumulative techniques and procedures in clinical microbiology (Cumitech) 17A. Washington, DC: ASM Press; 1993. pp. 1–28. [Google Scholar]
6. King CT, Rogers PD, Cleary JD, Chapman SW. Antifungal therapy during pregnancy. Clin Infect Dis. 1998;27(5):1151–60. [PubMed] [Google Scholar]
7. Doering PL, Santiago TM. Drugs for treatment of vulvovaginal candidiasis: comparative efficacy of agents and regimens. DICP. 1990;24(11):1078–83. [PubMed] [Google Scholar]
8. Young GL, Jewell D. Topical treatment for vaginal candidiasis (thrush) in pregnancy. Cochrane Database Syst Rev. 2001;4:CD000225. doi: 10.1002/14651858.CD000225. [PubMed] [CrossRef] [Google Scholar]
9. Lee BE, Feinberg M, Abraham JJ, Murthy AR. Congenital malformations in an infant born to a woman treated with fluconazole. Pediatr Infect Dis J. 1992;11(12):1062–4. [PubMed] [Google Scholar]
10. Pursley TJ, Blomquist IK, Abraham J, Andersen HF, Bartley JA.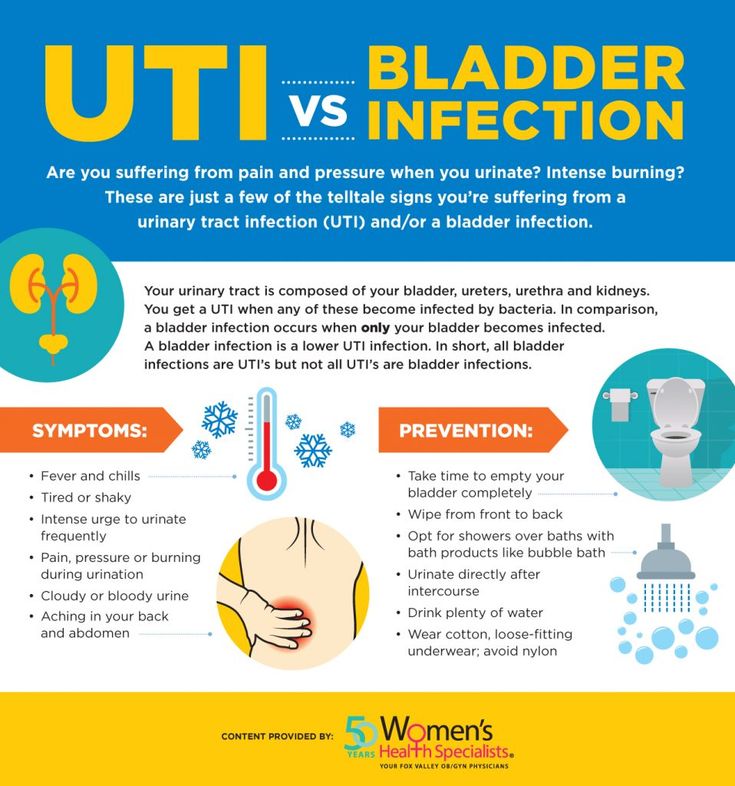 Fluconazole-induced congenital anomalies in three infants. Clin Infect Dis. 1996;22(2):336–40. [PubMed] [Google Scholar]
Fluconazole-induced congenital anomalies in three infants. Clin Infect Dis. 1996;22(2):336–40. [PubMed] [Google Scholar]
11. Nørgaard M, Pedersen L, Gislum M, Erichsen R, Søgaard KK, Schonheyder HC, et al. Maternal use of fluconazole and risk of congenital malformations: a Danish population-based cohort study. J Antimicrob Chemother. 2008;62(1):172–6. Epub 2008 Apr 9. [PubMed] [Google Scholar]
12. Acs N, Bánhidy F, Puhó E, Czeizel AE. Teratogenic effects of vaginal boric acid treatment during pregnancy. Int J Gynaecol Obstet. 2006;93(1):55–6. Epub 2006 Mar 10. [PubMed] [Google Scholar]
13. Fail PA, Chapin RE, Price CJ, Heindel JJ. General, reproductive, developmental and endocrine toxicity of boronated compounds. Reprod Toxicol. 1998;12(1):1–18. [PubMed] [Google Scholar]
14. Pappas PG, Rex JH, Sobel JD, Filler SG, Dismukes WE, Walsh TJ, et al. Guidelines for the treatment of candidiasis. Clin Infect Dis. 2004;38(2):161–89. Epub 2003 Dec 19. [PubMed] [Google Scholar]
15. Oren D, Nulman I, Makhija M, Ito S, Koren G. Using corticosteroids during pregnancy. Are topical, inhaled, or systemic agents associated with risk? Can Fam Physician. 2004;50:1083–5. [PMC free article] [PubMed] [Google Scholar]
Oren D, Nulman I, Makhija M, Ito S, Koren G. Using corticosteroids during pregnancy. Are topical, inhaled, or systemic agents associated with risk? Can Fam Physician. 2004;50:1083–5. [PMC free article] [PubMed] [Google Scholar]
16. Park-Wyllie L, Mazzotta P, Pastuszak A, Moretti ME, Beique L, Hunnisett L, et al. Birth defects after maternal exposure to corticosteroids: prospective cohort study and meta-analysis of epidemiological studies. Teratology. 2000;62(6):385–92. [PubMed] [Google Scholar]
17. Tauscher AE, Fleischer AB, Jr, Phelps KC, Feldman SR. Psoriasis and pregnancy. J Cutan Med Surg. 2002;6(6):561–70. Epub 2002 Oct 9. [PubMed] [Google Scholar]
18. Czeizel AE, Rockenbauer M. Population-based case-control study of teratogenic potential of corticosteroids. Teratology. 1997;56(5):335–40. [PubMed] [Google Scholar]
19. Mygind H, Thulstrup AM, Pedersen L, Larsen H. Risk of intrauterine growth retardation, malformations and other birth outcomes in children after topical use of corticosteroid in pregnancy. Acta Obstet Gynecol Scand. 2002;81(3):234–9. [PubMed] [Google Scholar]
Acta Obstet Gynecol Scand. 2002;81(3):234–9. [PubMed] [Google Scholar]
Infections during pregnancy - prices for diagnosis and monitoring of pregnancy in the clinic "Mother and Child" in Moscow
Every woman who is expecting a baby pays special attention to her health. This is not surprising, because any deviation from the norm or the appearance of any infection can cause the development of serious pathologies in the baby. But there are ailments that expectant mothers are especially common. One of them is thrush or vulvovaginal candidiasis.
Thrush during pregnancy in Moscow:
Clinical hospital MD GROUPClinical hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" Kuntsevo
Clinic "Mother and Child" Savelovskaya Clinic "Mother and Child" South-West Clinic "Mother and Child" Novogireevo Clinic "Mother and Child" Lefortovo
Hide
Thrush and its complications
Thrush in pregnant women is an infectious disease caused by yeast-like fungi of the genus Candida.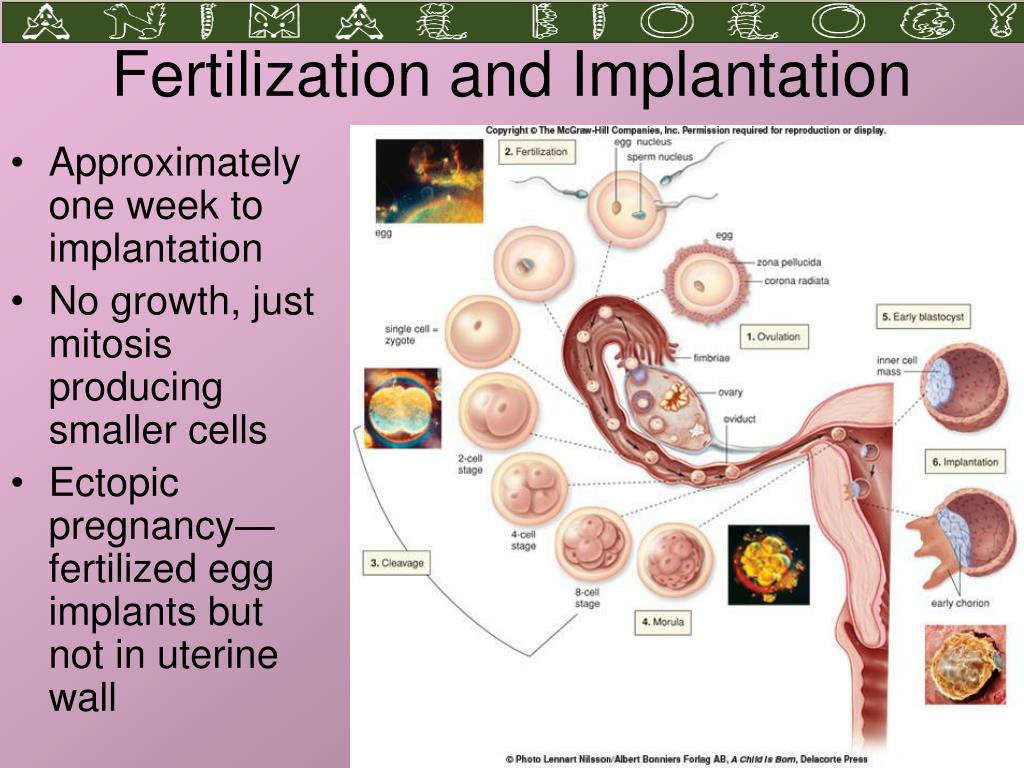 It is worth saying that these microorganisms in small quantities can be present in the vagina and colon of even an absolutely healthy woman. Under certain conditions, active growth of fungi occurs and an inflammatory process develops.
It is worth saying that these microorganisms in small quantities can be present in the vagina and colon of even an absolutely healthy woman. Under certain conditions, active growth of fungi occurs and an inflammatory process develops.
Almost 2/3 of the fair sex at least once in their lives experienced manifestations of thrush. Approximately half of them have relapses of the disease, and in 5% the pathology acquires a chronic relapsing course. But in pregnant women, thrush occurs three times more often than in patients outside of pregnancy. This is due primarily to changes in hormonal status and restructuring of the immune system of the future mother's body. These are exactly the conditions that are necessary for the growth and increase in the number of Candida fungi.
In most cases, thrush is not dangerous for the fetus, but this unpleasant pathology can still cause certain complications. With candidiasis, the risk of termination of pregnancy, premature birth and spontaneous abortion increases. The upward spread of the infectious process can lead to damage to the membranes and leakage of amniotic fluid. All this as a result can cause hypoxia and intrauterine infection of the fetus.
The upward spread of the infectious process can lead to damage to the membranes and leakage of amniotic fluid. All this as a result can cause hypoxia and intrauterine infection of the fetus.
Thrush symptoms
Thrush symptoms:
- moderate or heavy cheesy vaginal discharge;
- white coating on the genitals;
- irritation, itching, burning in the genital area, worse after urination, hygiene, intimacy and at night;
- hyperemia and swelling of the vagina and vulva, the appearance of microcracks on the mucous membrane of the genital organs;
- the appearance of an unpleasant odor.
With a significant spread of the inflammatory process on the surface of the vagina, small and large labia, burgundy vesicles with liquid contents are formed. After the opening of the vesicles, microerosions and crusts are formed. In overweight women, such manifestations can extend to the inguinal and intergluteal folds.
As the disease progresses, the fungus enters the urinary system. The ascending spread of the infection is evidenced by pain, frequent urination, aching pain in the lower abdomen, fever, discomfort and pain during intercourse.
The ascending spread of the infection is evidenced by pain, frequent urination, aching pain in the lower abdomen, fever, discomfort and pain during intercourse.
Causes of pathology development
Despite the fact that candidiasis can be transmitted sexually from an infected partner, the main cause of the development of the disease is considered to be a violation of the immune system and a decrease in the number of lactobacilli. The thing is that during pregnancy, a woman's body is rebuilt, the hormonal status changes, immunity decreases. The microflora of the vagina also changes: the number of lactobacilli, which are necessary to maintain a normal pH level and suppress the growth of pathogenic microorganisms, decreases.
As long as the balance between beneficial and pathogenic microorganisms is maintained, the expectant mother does not experience any discomfort. But as soon as the number of lactobacilli decreases, the process of rapid reproduction of Candida fungi starts. Unpleasant symptoms begin to appear.
Unpleasant symptoms begin to appear.
Another reason for the development of thrush during pregnancy is a decrease in immunity. It should be noted that this is a completely natural process. Without a physiological decrease in immunity, normal gestation is impossible: during the period of expectation of a baby, special substances begin to be synthesized in the woman's body that prevent the formation of antibodies and eliminate the risk of rejection of fetal cells by the mother's immune system. But with a decrease in immunity, more favorable conditions are created for the development of infection and the spread of the inflammatory process. It is these conditions that are optimal for the reproduction of the Candida fungus.
There are other factors that can provoke the development of thrush:
- incorrect or insufficient intimate hygiene;
- wearing synthetic underwear;
- chronic inflammatory diseases that reduce immunity;
- long-term use of antibiotics;
- hypothermia.
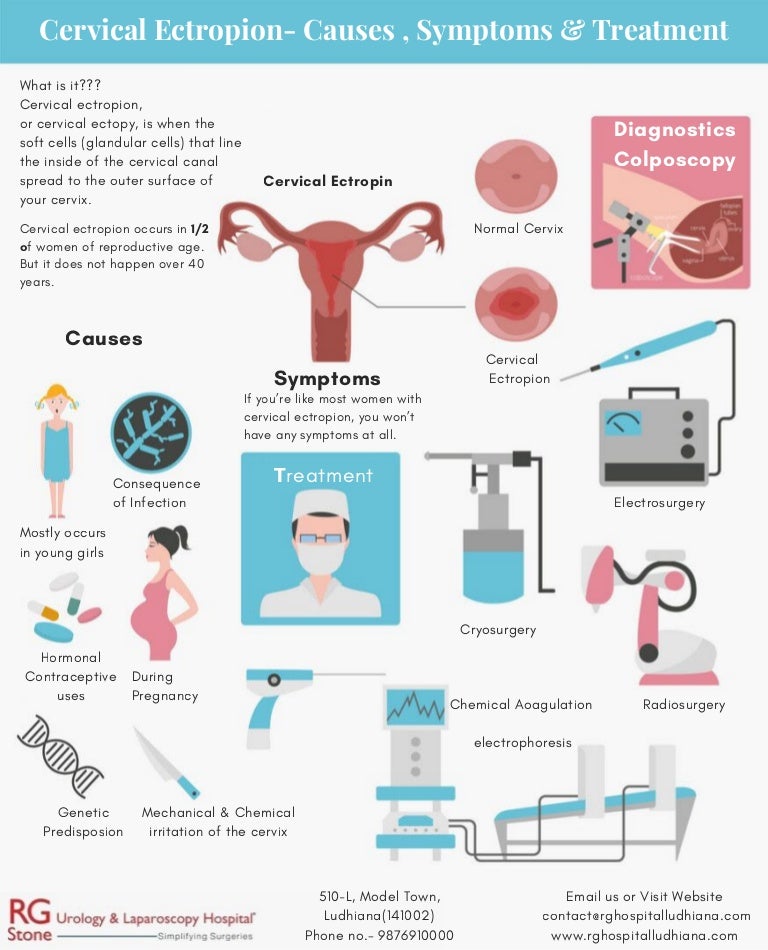
Diagnosis of thrush
The symptoms of thrush are similar to the manifestations of other infectious diseases, so the diagnosis is aimed at determining the causes that caused the anxiety of the pregnant patient. First, a survey is conducted, during which the doctor collects information about the duration and intensity of symptoms. Then an examination is carried out on a chair with mirrors in order to assess the condition of the mucosa. Already by the presence of hyperemia, white plaque, abundant curdled discharge and rash, the doctor can make a preliminary conclusion about the development of candidiasis.
To confirm the diagnosis, a smear is taken for the flora, and PCR diagnostics are also prescribed to differentiate microorganisms.
Treatment of thrush
The main task in the treatment of thrush is to maintain a balance between the therapeutic effect and safety for the fetus. The therapy is based on the use of well-tolerated, non-toxic topical drugs that do not affect the systemic blood flow. Vaginal suppositories are mainly used, thanks to which it is possible to quickly eliminate symptoms. These are polyene antimycotics, imidazoles, triazoles, combined preparations that reduce the activity of yeast-like fungi.
Vaginal suppositories are mainly used, thanks to which it is possible to quickly eliminate symptoms. These are polyene antimycotics, imidazoles, triazoles, combined preparations that reduce the activity of yeast-like fungi.
At the time of treatment, it is recommended to abandon intimate life or use barrier contraceptives. It is also important to strictly follow medical recommendations and adhere to the prescribed therapeutic regimen. Otherwise, it will not be possible to achieve a positive effect from the treatment, and the disease may become chronic.
Prophylaxis
It is impossible to completely exclude the possibility of thrush during pregnancy. However, you can follow the recommendations that will minimize the possible risks. Experts recommend:
- abandon synthetic underwear in favor of natural fabrics;
- observe the rules of intimate hygiene;
- do not use panty liners all the time;
- try not to overcool.
You should also avoid stressful loads and adjust the diet by increasing the amount of fruits, vegetables, dairy products consumed. If before pregnancy a woman has already encountered manifestations of thrush, you should register with a gynecologist as soon as possible.
If before pregnancy a woman has already encountered manifestations of thrush, you should register with a gynecologist as soon as possible.
Make an appointment
services - Thrush during pregnancy
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" KuntsevoClinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" SavelovskayaClinic "Mother and Child" Yugo-ZapadMother and Child Clinic LefortovoMother and Child Clinic Novogireevo
Thrush during pregnancy
By clicking on the send button, I consent to the processing of personal data
Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for recurrent thrush are those pregnant women who have already had a history of thrush episodes
Pregnancy is a special period in a woman's life, the body is rebuilt - the hormonal background changes, the level of progesterone increases, which leads to a decrease in immunity, the level of estrogens rises, and therefore glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida.:max_bytes(150000):strip_icc()/yeast-infections-treatment-3521199-1b83976b404641398aa11374314acd26.jpg)
Lactobacilli are the predominant microorganisms in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli are also involved in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply. These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush.
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and / or vagina, swelling and irritation in the vulva
- vaginal discharge with a "cheesy character", sometimes an unpleasant odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor.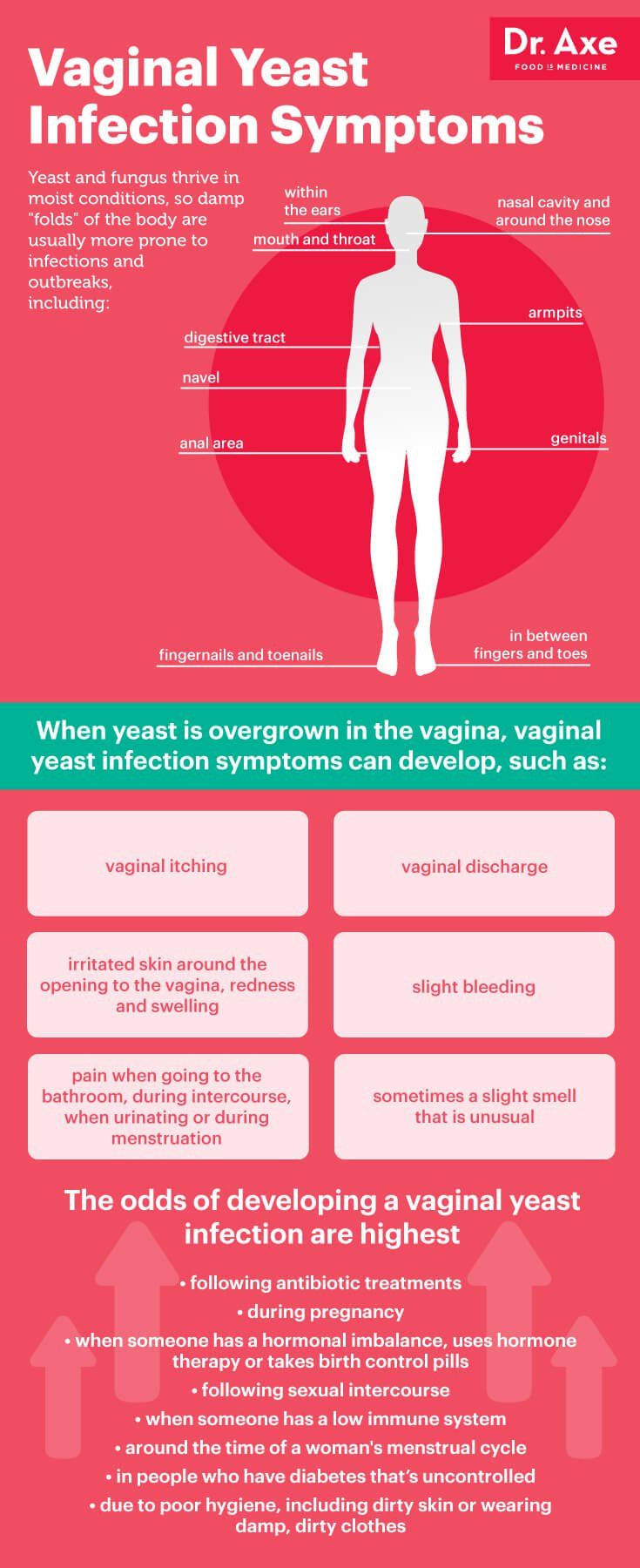
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and experience neither discomfort nor manifestations of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women complications on the course of pregnancy and on the health of the mother and her unborn child. In the treatment of thrush, experts recommend an integrated approach to therapy.
In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosages and regimen.
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® In the treatment of thrush in pregnant womenEcofucin
® is allowed for all pregnancy periods and during lactation 4
Why ecofucin ® 9000 9000 9000 9000 9000 9000 9000 9000 locally in the focus of infection Natamycin + Prebiotic 5 The active substance 7 of the drug Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in the composition of the drug Ecofucin ® helps to restore the vaginal microflora and strengthen local immunity 6 . Efficacy and safety of Ecofucin has been proven by clinical studies Ecofucin promotes faster recovery of patients with thrush. More details For pregnant women Moscow 40 patients For non-pregnant women St. Petersburg 36 patients Clinical cure occurred significantly earlier in the group of patients who used Ecofucin. Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; 1; 28-33 Ecofucin helps to increase the number of own lactobacilli in the vagina and reduce the risk of recurrence of thrush. More details For pregnant women Moscow 40 patients For non-pregnant women St. Petersburg 36 patients Clinical cure occurred significantly earlier in the group of patients who used Ecofucin. Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; 1; 28-33 Method of administration and doses The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually. Additional conditions for effective treatment of thrush are: giving up bad habits, a carbohydrate-restricted diet, wearing underwear made from natural fabrics, etc. It is important to consult a gynecologist in a timely manner and exclude self-treatment. 1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Pharmateka № 9, 2009, p. 64-70. 2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis".