Pregnancy and dieting
Pregnancy and diet - Better Health Channel
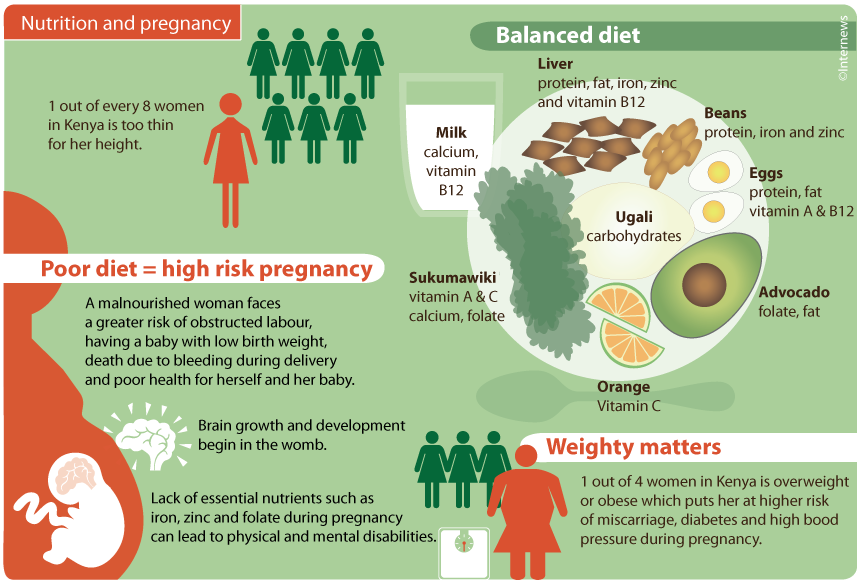
Good nutrition during pregnancy can help to keep you and your developing baby healthy. Your need for certain nutrients (such as iron, iodine and folate) increases when you are pregnant.
A varied diet that includes the right amount of healthy foods from the 5 food groups generally provides our bodies with the vitamins and minerals it needs each day. However, pregnant women may need to take vitamin or mineral supplements during pregnancy (such as folate and vitamin D).
Consult your doctor before taking any supplements. They may recommend that you have a blood test or see a dietitian to review your need to take a supplement. You shouldn’t need to take a vitamin D supplement other than if you have been diagnosed with vitamin D deficiency through a blood test.
Healthy weight gain during pregnancy
Steady weight gain during pregnancy is normal and important for the health of you and your baby. However, it is also important not to gain too much weight.
Excess weight gain during pregnancy can increase your risk of certain health issues including gestational diabetes and high blood pressure in pregnancy. Excess weight gain can also make it difficult to lose weight after pregnancy.
If you are pregnant, a good approach is to eat to satisfy your appetite, and continue to monitor your weight throughout pregnancy. You can talk to your Midwife, GP, Dietitian or Obstetrician about assisting you with monitoring your weight.
Depending on your body mass index (BMI) at the start of your pregnancy, the following weight gain is recommended during pregnancy:
| BMI at start of pregnancy (kg/m2) | Recommended weight gain during pregnancy (kg) |
|---|---|
| < 18.5 (underweight) | 12.5–18.0 |
| 18.5–24.9 (healthy) | 11.5–16.0 |
| 25.0–29.9 (overweight) | 7.0–11.5 |
| > 30 (overweight) | 5.0–9.0 |
If you are overweight, pregnancy is not the time to start dieting or trying to lose weight. Weight gain within these ranges is important to support the growth and development of your baby.
Weight gain within these ranges is important to support the growth and development of your baby.
To maintain an appropriate weight gain during pregnancy, it is important to:
- Choose healthy foods from the 5 food groups.
- Limit discretionary foods and drinks high in saturated fat, added sugars and added salt (such as cakes, biscuits and sugary drinks).
- Remain active during your pregnancy.
Healthy eating for pregnant women
What you eat during pregnancy affects not only your own health and wellbeing and the development of your baby, but there is also substantial evidence that it can have a lasting impact on the health and wellbeing of your child later in life.
Choose a wide variety of healthy foods from the 5 food groups to make sure your and your baby’s nutritional needs are met to support the health and growth of your baby.
You may find that you need to eat more of some foods to ensure key nutrients are obtained, but there is no need to ‘eat for two’.
What to include in your pregnancy diet:
- A variety of fruits and vegetables of different types and colours. Ideally 2 serves of fruit and 5 serves of vegetables every day.
- Increase your intake of grain and cereal foods to 8½ serves a day. Choose mostly wholegrain and high fibre options.
- Select foods high in iron (such as lean red meat or tofu). Iron-rich foods are important for pregnant women. 3½ serves of meat or meat alternatives are recommended.
- Make a habit of drinking milk, eating hard cheese and yoghurt, or calcium-enriched alternatives. Reduced-fat varieties are best. 2½ serves per day are recommended.
- Drink plenty of water
- Limit your intake of foods and drinks high in saturated fat, added sugar and salt to small amounts.
Australian Dietary Guidelines for pregnancy
The Australian Dietary GuidelinesExternal Link recommend these daily servings for pregnant women from the 5 food groups:
| Food group | Serves per day | Example serving size |
|---|---|---|
| Vegetables and legumes/beans | 18 years or under: 5 19–50 years: 5 |
|
| Fruit | 18 years or under: 2 19–50 years: 2 |
Or only occasionally
|
| Grain (cereal) foods, mostly wholegrain and/or high-fibre varieties | 18 years or under: 8 19–50 years: 8½ |
|
| Lean meats and poultry, fish, eggs, tofu, nuts and seeds and legumes/beans | 18 years or under: 3½ 19–50 years: 3½ |
|
| Milk, yoghurt, cheese and/or alternatives, mostly reduced fat | 18 years or under: 3½ 19–50 years: 2½ |
|
*Choose canned foods with no added salt.
Folic acid (folate) and pregnancy
Folate (known as folic acid when added to foods) is a B-group vitamin found in a variety of foods. Folic acid helps protect against neural tube defects in the developing foetus. It is important for pregnant women to make sure they are receiving enough of this important vitamin.
For women who are planning a pregnancy, and during the first 3 months of pregnancy, a daily folic acid supplement of 500 micrograms is recommended, as well as eating foods that are naturally rich in folate or are fortified with folic acid.
Folate in your diet
Excellent food sources of folate include:
- asparagus
- bran flakes
- broccoli
- Brussels sprouts
- chickpeas
- dried beans
- lentils
- spinach.
Very good food sources of folate include:
- cabbage
- cauliflower
- leeks
- oranges
- orange juice
- parsley
- peas
- wheat germ
- wholegrain bread.
Good food sources of folate include:
- hazelnuts
- vegemite
- parsnips
- potato
- salmon
- strawberries
- tomato
- unsalted peanuts
- walnuts.
Although liver is high in folate, it is not recommended for women who are, or could be pregnant, because of its high vitamin A content.
Iron and pregnancy
During pregnancy, a woman’s requirement for iron increases. This is because the developing foetus draws iron from the mother to last it through the first 5 or 6 months after birth.
Iron losses are reduced during pregnancy, because the woman is no longer menstruating. However, this is not enough to offset the needs of the developing foetus. It is important for pregnant women to eat iron-rich foods every day, such as meat, chicken, seafood, dried beans and lentils, and green leafy vegetables.
Animal sources of iron are readily absorbed by the body. Iron from plant sources is not absorbed as easily, but absorption is helped when these foods are eaten together with foods that contain vitamin C (such as oranges). This is important for women who follow a vegetarian diet.
This is important for women who follow a vegetarian diet.
The recommended daily intake (RDI) of iron during pregnancy is 27 mg a day (9 mg a day more than for non-pregnant women). Iron deficiency during pregnancy is common in Australia, and iron supplements may be needed by some women. It is important to discuss your need for supplements with your doctor, as iron can be toxic (poisonous) in large amounts.
Iodine and pregnancy
Iodine is an important mineral needed for the production of thyroid hormone, which is important for growth and development. If you don’t have enough iodine intake during pregnancy, it increases your baby’s risk of mental impairment and congenital hypothyroidismExternal Link (previously known as cretinism).
Foods that are good sources of iodine include:
- seafood
- seaweed (including nori and kelp)
- eggs
- meat
- dairy products.
Iodised salt also includes iodine. It is important to avoid adding salt at the table or in cooking, but if you do, make sure it is labelled iodised.
Due to the re-emergence of iodine deficiency in Australia, iodised salt is now added to all commercially sold bread in Australia and New Zealand, with the exception of organic and unleavened bread.
Pregnant and breastfeeding women have increased iodine requirements. Iodine supplementation of 150 micrograms per day is recommended for women planning a pregnancy, throughout pregnancy and while breastfeeding.
Vitamin D and pregnancy
Vitamin D is essential for your baby’s growth and development and your own health during pregnancy. Vitamin D is important for bone health and for optimal pregnancy outcomes for you and your baby.
We get most of our vitamin D from the sun. Ultraviolet (UV) radiation from the sun produces vitamin D in the skin and is the best natural source of vitamin D. Only a small amount of our vitamin D intake comes from our diet – from foods such as eggs, oily fish, margarine and milks fortified with vitamin D.
Women who are at most risk of vitamin D deficiency:
- have dark coloured skin
- wear covering or concealing clothing for religious or other reasons
- spend much time indoors.
You may need a blood test at the beginning of your pregnancy to assess your vitamin D levels. If so, your doctor (GP) will arrange this. Depending on your results, you might need to take vitamin D supplements. During the winter months, it can be more difficult to obtain enough vitamin D. Consider talking to your GP about your vitamin D levels before pregnancy or early in your pregnancy to make sure you begin pregnancy with optimal vitamin D.
If you are considering taking vitamin D or any other supplements during pregnancy, always discuss it with your GP first. It is not beneficial to take vitamin D supplements if you do not need them.
Multivitamin supplements and pregnancy
Multivitamin supplements may be recommended for some groups of pregnant women, including:
- vegans and vegetarians
- teenagers who may have an inadequate food intake
- substance misusers (of drugs, tobacco and alcohol)
- pregnant women who are already very overweight and who are trying to prevent excessive weight gain.

Always be advised by your GP before taking vitamin or mineral supplements.
Until 2006, Australian dietary recommendations advised increased calcium intake during pregnancy and breastfeeding. This advice has since been revised. Although the baby has a high requirement for calcium during the third trimester of pregnancy (as it starts to develop and strengthen its bones), the mother’s increased capacity to absorb dietary calcium means that there is no need for extra intake.
The recommended dietary intake for non-pregnant women (1,000 mg a day for women aged 19 to 50 years and 1,300 mg a day for adolescents or those aged over 51) remains unchanged during pregnancy and breastfeeding. Dairy foods (such as milk, cheese and yoghurt) and calcium-fortified soy milk are excellent dietary sources of calcium.
The dangers of dieting while pregnant
Some women fear the extra weight gain of pregnancy and may decide to eat sparingly to avoid putting on body fat. Restricted eating or crash dieting in any form while pregnant can seriously compromise your health and that of your baby, and is not recommended during pregnancy.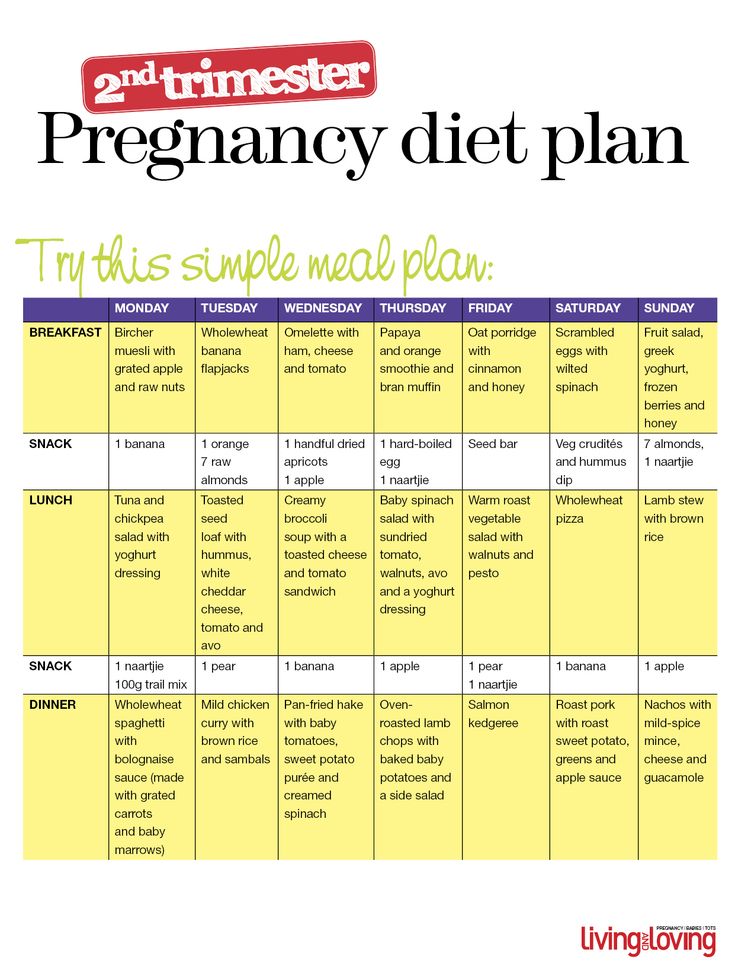
Pregnancy in adolescence
Pregnant adolescents need more of some nutrients than adult women, because they are still growing themselves. Adolescents may give birth to smaller infants, because they are competing with the growing foetus for nutrients.
It is important for pregnant adolescents to make sure they are getting enough iron.
Calcium intake is also important, because young women have not yet reached their peak bone mass, and inadequate calcium intake may increase the risk of osteoporosis developing later in life.
Pregnant adolescents should eat around 3½ serves of milk, yoghurt, cheese or calcium-fortified alternatives each day to make sure they are meeting their calcium needs.
Constipation during pregnancy
Constipation is a common occurrence during pregnancy. To help with constipation, enjoy a wide variety of foods that are high in fibre, such as vegetables, legumes, fruit and wholegrains and drink plenty of water. Being physically active can also help with reducing constipation.
Nausea and vomiting during pregnancy
Nausea and vomiting, especially ‘morning sickness’, are common during pregnancy, particularly in the first trimester.
Some suggestions that may help include:
- Eat some dry bread, biscuits or cereal before getting up in the morning. Get up slowly, avoiding sudden movements.
- Drink liquids between, rather than with, meals to avoid bloating, as this can trigger vomiting.
- Avoid large meals and greasy, highly spiced foods.
- Suck on something sour like a lemon.
- Relax, rest and get into the fresh air as much as possible. Keep rooms well ventilated and odour free.
- Try food and drinks containing ginger, such as ginger tea, as these sometimes relieve nausea.
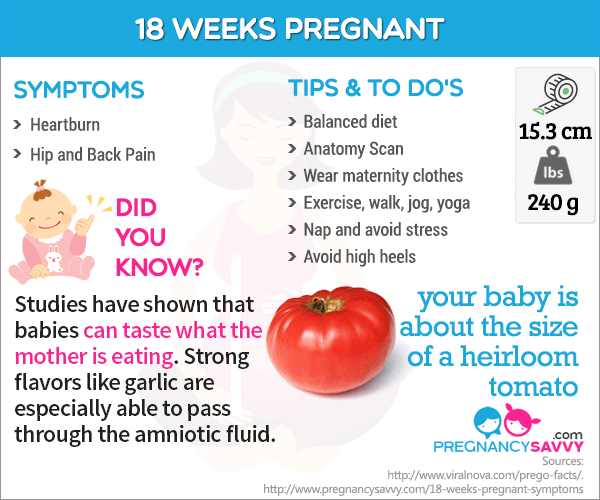
Heartburn and pregnancy
Heartburn is common in pregnancy because, as the baby grows, there is more pressure on the abdomen. Small, frequent meals may help, compared to larger meals.
Try to avoid:
- eating late at night
- bending, lifting or lying down after meals
- excessive consumption of tea or coffee.

You may also like to try sleeping with your bedhead raised a little. You can do this by putting a folded blanket or pillow under your mattress.
Alcohol during pregnancy
There is no known safe level of alcohol consumption for women who are pregnant. Consuming alcohol during pregnancy increases the risk of miscarriage, low birth weight, congenital deformities and effects on the baby’s intelligence.
The Australian guidelines to reduce health risks from drinking alcoholExternal Link recommend that the safest option for pregnant women is not to drink alcohol at all.
If you find it difficult to decrease or stop drinking alcohol during pregnancy talk to:
- your doctor or midwife
- your local community health service
- an alcohol and other drug helpline in your state or territory.
The Australian guidelines to reduce health risks from drinking alcoholExternal Linkprovide more information.
Listeria infection and pregnancy
Listeria infection, or listeriosis, is an illness usually caused by eating food contaminated with bacteria known as Listeria monocytogenes.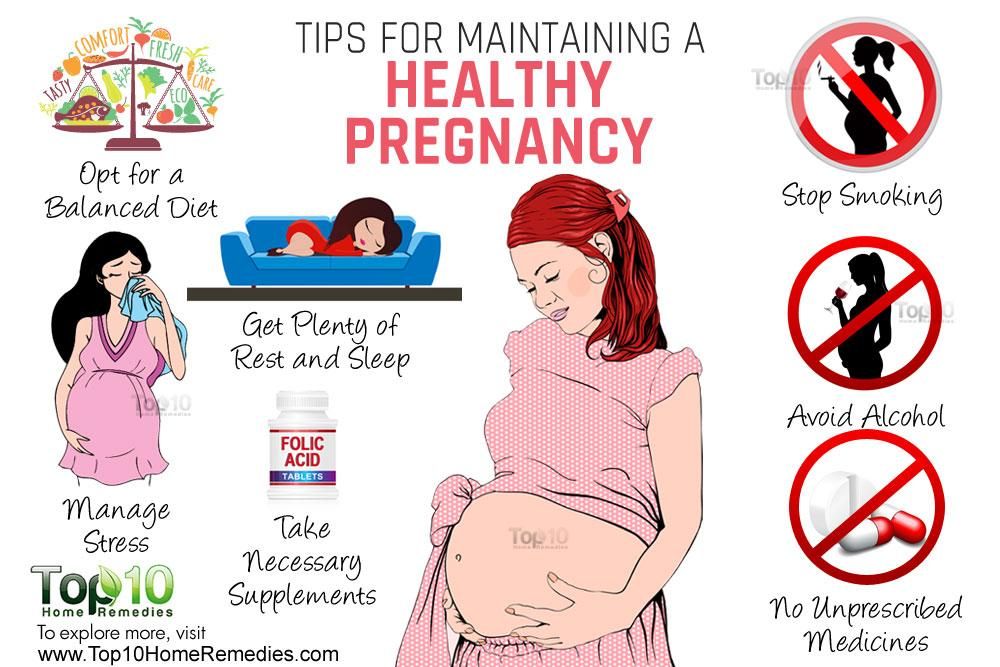 Healthy people may experience no ill-effects from listeria infection at all, but the risks are substantial for pregnant women. The greatest danger is to the unborn baby, with increased risk of miscarriage, stillbirth or premature labour. A listeria infection is easily treated with antibiotics, but prevention is best.
Healthy people may experience no ill-effects from listeria infection at all, but the risks are substantial for pregnant women. The greatest danger is to the unborn baby, with increased risk of miscarriage, stillbirth or premature labour. A listeria infection is easily treated with antibiotics, but prevention is best.
Some foods are more prone to contamination with listeria than others and should be avoided if you are pregnant. They include:
- soft cheeses, such as brie, camembert and ricotta – these are safe if served cooked and hot
- precooked or pre-prepared cold foods that will not be reheated – for example, pre-prepared salads, pâté, quiches and delicatessen meats like ham and salami
- undercooked meat, chilled pre-cooked meats, pâté, meat spread
- raw seafood, such as oysters and sashimi or smoked seafood, such as salmon (canned varieties are safe)
- unpasteurised foods
- pre-prepared or pre-packaged cut fruit and vegetables
- soft-serve ice cream.

The organism that causes listeria infection is destroyed by heat, so properly cooked foods are not a risk.
Salmonella and pregnancy
Salmonella is a cause of food poisoning that can trigger miscarriage. The most likely sources of salmonella are raw eggs and undercooked meat and poultry.
Good food hygiene reduces the risk of infection
Good food hygiene is the best way to reduce the risk of salmonella and listeria infections. Suggestions include:
- Always wash your hands before and after preparing food.
- Keep your kitchen surfaces clean.
- Do not let uncooked food contaminate cooked food.
- Wash fruit, vegetables and salad before eating.
- Cook food thoroughly.
- Keep pets away from kitchen surfaces.
- Wear rubber gloves when handling cat litter trays or gardening.
- Store food at correct temperatures.
Mercury in fish
It is suggested that pregnant women eat 2 to 3 serves of fish every week for their own good health and that of their developing baby. However, pregnant women or women intending to become pregnant within the next 6 months should be careful about which fish they eat. Some types of fish contain high levels of mercury, which can be harmful to the developing foetus.
However, pregnant women or women intending to become pregnant within the next 6 months should be careful about which fish they eat. Some types of fish contain high levels of mercury, which can be harmful to the developing foetus.
When choosing fish, pregnant women should:
- limit to one serve (150 g) per fortnight – billfish (swordfish, broadbill and marlin) and shark (flake), with no other fish eaten in that fortnight
OR - limit to one serve (150 g) per week – orange roughy (deep sea perch) or catfish, with no other fish eaten that week
OR - eat 2 to 3 serves per week – of any other fish or seafood (for example, salmon or tuna).
Note: 150 g is equivalent to approximately 2 frozen crumbed fish portions.
Don’t worry if you’ve had the occasional meal of fish with high levels of mercury. Mercury build-up in the mother’s blood is only a potential problem when that type of fish is eaten regularly.
Where to get help
- Your GP (doctor)
- Midwife
- Obstetrician-gynaecologist
- Dietitians AustraliaExternal Link Tel. 1800 812 942
Pregnancy and diet - Better Health Channel
Good nutrition during pregnancy can help to keep you and your developing baby healthy. Your need for certain nutrients (such as iron, iodine and folate) increases when you are pregnant.
A varied diet that includes the right amount of healthy foods from the 5 food groups generally provides our bodies with the vitamins and minerals it needs each day. However, pregnant women may need to take vitamin or mineral supplements during pregnancy (such as folate and vitamin D).
Consult your doctor before taking any supplements. They may recommend that you have a blood test or see a dietitian to review your need to take a supplement. You shouldn’t need to take a vitamin D supplement other than if you have been diagnosed with vitamin D deficiency through a blood test.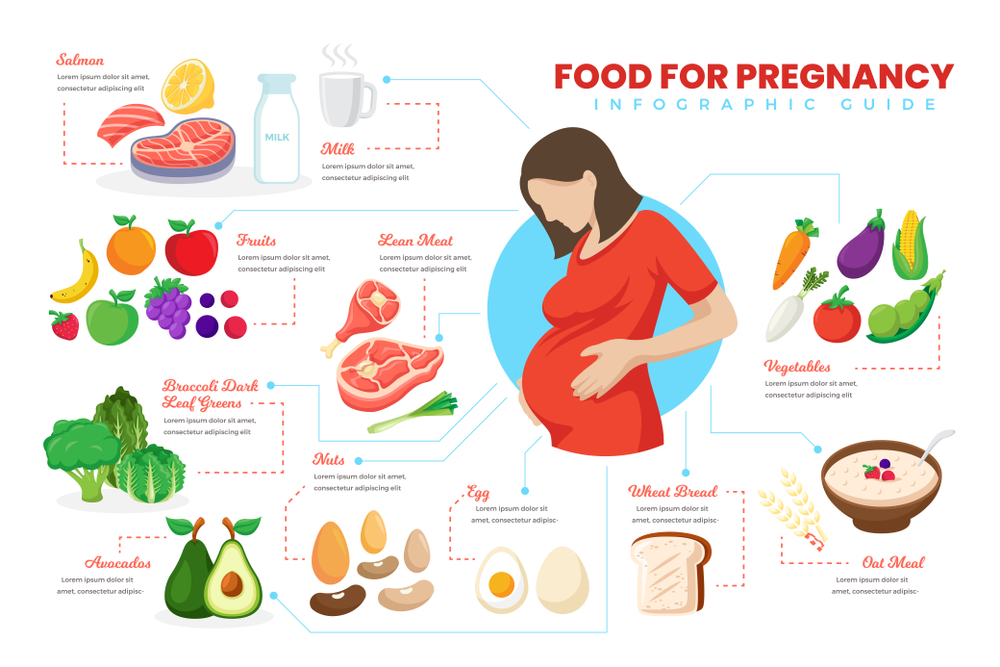
Healthy weight gain during pregnancy
Steady weight gain during pregnancy is normal and important for the health of you and your baby. However, it is also important not to gain too much weight.
Excess weight gain during pregnancy can increase your risk of certain health issues including gestational diabetes and high blood pressure in pregnancy. Excess weight gain can also make it difficult to lose weight after pregnancy.
If you are pregnant, a good approach is to eat to satisfy your appetite, and continue to monitor your weight throughout pregnancy. You can talk to your Midwife, GP, Dietitian or Obstetrician about assisting you with monitoring your weight.
Depending on your body mass index (BMI) at the start of your pregnancy, the following weight gain is recommended during pregnancy:
| BMI at start of pregnancy (kg/m2) | Recommended weight gain during pregnancy (kg) |
|---|---|
| < 18.5 (underweight) | 12. 5–18.0 5–18.0 |
| 18.5–24.9 (healthy) | 11.5–16.0 |
| 25.0–29.9 (overweight) | 7.0–11.5 |
| > 30 (overweight) | 5.0–9.0 |
If you are overweight, pregnancy is not the time to start dieting or trying to lose weight. Weight gain within these ranges is important to support the growth and development of your baby.
To maintain an appropriate weight gain during pregnancy, it is important to:
- Choose healthy foods from the 5 food groups.
- Limit discretionary foods and drinks high in saturated fat, added sugars and added salt (such as cakes, biscuits and sugary drinks).
- Remain active during your pregnancy.
Healthy eating for pregnant women
What you eat during pregnancy affects not only your own health and wellbeing and the development of your baby, but there is also substantial evidence that it can have a lasting impact on the health and wellbeing of your child later in life.
Choose a wide variety of healthy foods from the 5 food groups to make sure your and your baby’s nutritional needs are met to support the health and growth of your baby.
You may find that you need to eat more of some foods to ensure key nutrients are obtained, but there is no need to ‘eat for two’.
What to include in your pregnancy diet:
- A variety of fruits and vegetables of different types and colours. Ideally 2 serves of fruit and 5 serves of vegetables every day.
- Increase your intake of grain and cereal foods to 8½ serves a day. Choose mostly wholegrain and high fibre options.
- Select foods high in iron (such as lean red meat or tofu). Iron-rich foods are important for pregnant women. 3½ serves of meat or meat alternatives are recommended.
- Make a habit of drinking milk, eating hard cheese and yoghurt, or calcium-enriched alternatives. Reduced-fat varieties are best. 2½ serves per day are recommended.
- Drink plenty of water
- Limit your intake of foods and drinks high in saturated fat, added sugar and salt to small amounts.

Australian Dietary Guidelines for pregnancy
The Australian Dietary GuidelinesExternal Link recommend these daily servings for pregnant women from the 5 food groups:
| Food group | Serves per day | Example serving size |
|---|---|---|
| Vegetables and legumes/beans | 18 years or under: 5 19–50 years: 5 |
|
| Fruit | 18 years or under: 2 19–50 years: 2 |
Or only occasionally
|
| Grain (cereal) foods, mostly wholegrain and/or high-fibre varieties | 18 years or under: 8 19–50 years: 8½ |
|
| Lean meats and poultry, fish, eggs, tofu, nuts and seeds and legumes/beans | 18 years or under: 3½ 19–50 years: 3½ |
|
| Milk, yoghurt, cheese and/or alternatives, mostly reduced fat | 18 years or under: 3½ 19–50 years: 2½ |
|
*Choose canned foods with no added salt.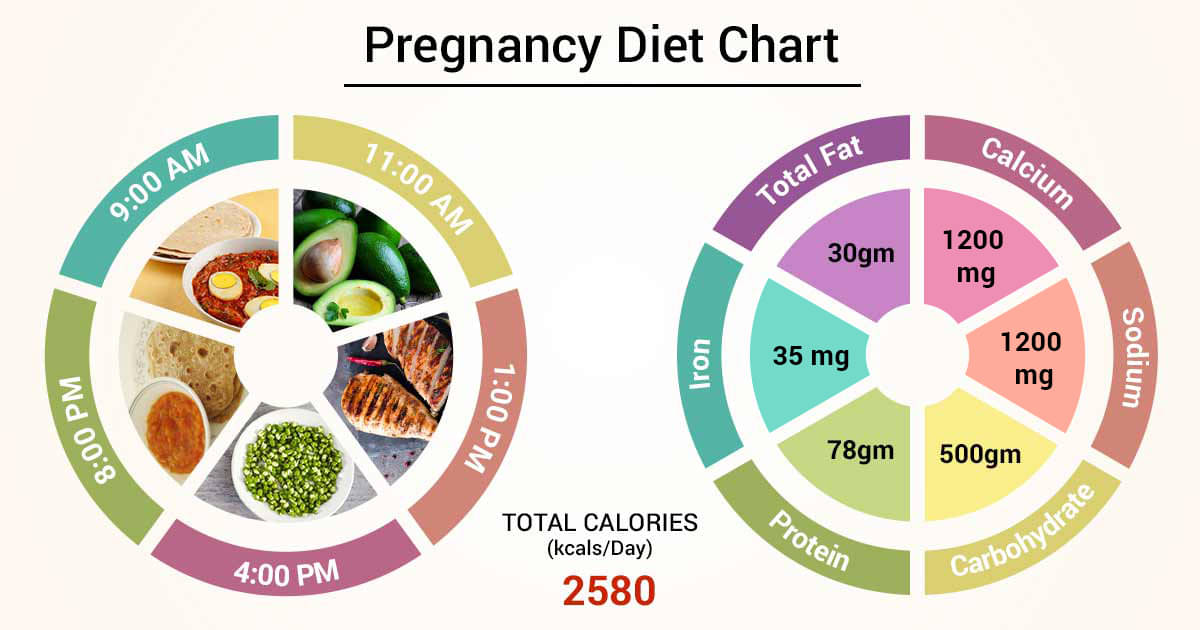
Folic acid (folate) and pregnancy
Folate (known as folic acid when added to foods) is a B-group vitamin found in a variety of foods. Folic acid helps protect against neural tube defects in the developing foetus. It is important for pregnant women to make sure they are receiving enough of this important vitamin.
For women who are planning a pregnancy, and during the first 3 months of pregnancy, a daily folic acid supplement of 500 micrograms is recommended, as well as eating foods that are naturally rich in folate or are fortified with folic acid.
Folate in your diet
Excellent food sources of folate include:
- asparagus
- bran flakes
- broccoli
- Brussels sprouts
- chickpeas
- dried beans
- lentils
- spinach.
Very good food sources of folate include:
- cabbage
- cauliflower
- leeks
- oranges
- orange juice
- parsley
- peas
- wheat germ
- wholegrain bread.

Good food sources of folate include:
- hazelnuts
- vegemite
- parsnips
- potato
- salmon
- strawberries
- tomato
- unsalted peanuts
- walnuts.
Although liver is high in folate, it is not recommended for women who are, or could be pregnant, because of its high vitamin A content.
Iron and pregnancy
During pregnancy, a woman’s requirement for iron increases. This is because the developing foetus draws iron from the mother to last it through the first 5 or 6 months after birth.
Iron losses are reduced during pregnancy, because the woman is no longer menstruating. However, this is not enough to offset the needs of the developing foetus. It is important for pregnant women to eat iron-rich foods every day, such as meat, chicken, seafood, dried beans and lentils, and green leafy vegetables.
Animal sources of iron are readily absorbed by the body. Iron from plant sources is not absorbed as easily, but absorption is helped when these foods are eaten together with foods that contain vitamin C (such as oranges). This is important for women who follow a vegetarian diet.
This is important for women who follow a vegetarian diet.
The recommended daily intake (RDI) of iron during pregnancy is 27 mg a day (9 mg a day more than for non-pregnant women). Iron deficiency during pregnancy is common in Australia, and iron supplements may be needed by some women. It is important to discuss your need for supplements with your doctor, as iron can be toxic (poisonous) in large amounts.
Iodine and pregnancy
Iodine is an important mineral needed for the production of thyroid hormone, which is important for growth and development. If you don’t have enough iodine intake during pregnancy, it increases your baby’s risk of mental impairment and congenital hypothyroidismExternal Link (previously known as cretinism).
Foods that are good sources of iodine include:
- seafood
- seaweed (including nori and kelp)
- eggs
- meat
- dairy products.
Iodised salt also includes iodine. It is important to avoid adding salt at the table or in cooking, but if you do, make sure it is labelled iodised.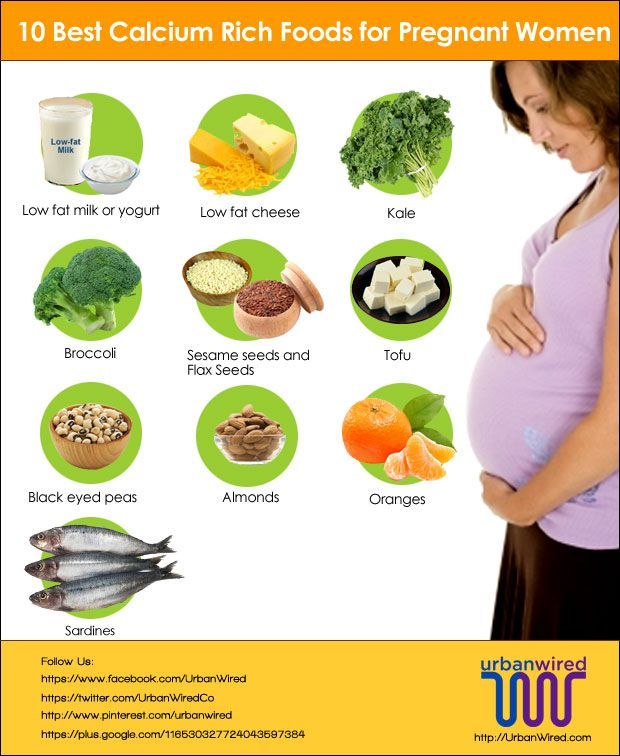
Due to the re-emergence of iodine deficiency in Australia, iodised salt is now added to all commercially sold bread in Australia and New Zealand, with the exception of organic and unleavened bread.
Pregnant and breastfeeding women have increased iodine requirements. Iodine supplementation of 150 micrograms per day is recommended for women planning a pregnancy, throughout pregnancy and while breastfeeding.
Vitamin D and pregnancy
Vitamin D is essential for your baby’s growth and development and your own health during pregnancy. Vitamin D is important for bone health and for optimal pregnancy outcomes for you and your baby.
We get most of our vitamin D from the sun. Ultraviolet (UV) radiation from the sun produces vitamin D in the skin and is the best natural source of vitamin D. Only a small amount of our vitamin D intake comes from our diet – from foods such as eggs, oily fish, margarine and milks fortified with vitamin D.
Women who are at most risk of vitamin D deficiency:
- have dark coloured skin
- wear covering or concealing clothing for religious or other reasons
- spend much time indoors.

You may need a blood test at the beginning of your pregnancy to assess your vitamin D levels. If so, your doctor (GP) will arrange this. Depending on your results, you might need to take vitamin D supplements. During the winter months, it can be more difficult to obtain enough vitamin D. Consider talking to your GP about your vitamin D levels before pregnancy or early in your pregnancy to make sure you begin pregnancy with optimal vitamin D.
If you are considering taking vitamin D or any other supplements during pregnancy, always discuss it with your GP first. It is not beneficial to take vitamin D supplements if you do not need them.
Multivitamin supplements and pregnancy
Multivitamin supplements may be recommended for some groups of pregnant women, including:
- vegans and vegetarians
- teenagers who may have an inadequate food intake
- substance misusers (of drugs, tobacco and alcohol)
- pregnant women who are already very overweight and who are trying to prevent excessive weight gain.

Always be advised by your GP before taking vitamin or mineral supplements.
Until 2006, Australian dietary recommendations advised increased calcium intake during pregnancy and breastfeeding. This advice has since been revised. Although the baby has a high requirement for calcium during the third trimester of pregnancy (as it starts to develop and strengthen its bones), the mother’s increased capacity to absorb dietary calcium means that there is no need for extra intake.
The recommended dietary intake for non-pregnant women (1,000 mg a day for women aged 19 to 50 years and 1,300 mg a day for adolescents or those aged over 51) remains unchanged during pregnancy and breastfeeding. Dairy foods (such as milk, cheese and yoghurt) and calcium-fortified soy milk are excellent dietary sources of calcium.
The dangers of dieting while pregnant
Some women fear the extra weight gain of pregnancy and may decide to eat sparingly to avoid putting on body fat. Restricted eating or crash dieting in any form while pregnant can seriously compromise your health and that of your baby, and is not recommended during pregnancy.
Pregnancy in adolescence
Pregnant adolescents need more of some nutrients than adult women, because they are still growing themselves. Adolescents may give birth to smaller infants, because they are competing with the growing foetus for nutrients.
It is important for pregnant adolescents to make sure they are getting enough iron.
Calcium intake is also important, because young women have not yet reached their peak bone mass, and inadequate calcium intake may increase the risk of osteoporosis developing later in life.
Pregnant adolescents should eat around 3½ serves of milk, yoghurt, cheese or calcium-fortified alternatives each day to make sure they are meeting their calcium needs.
Constipation during pregnancy
Constipation is a common occurrence during pregnancy. To help with constipation, enjoy a wide variety of foods that are high in fibre, such as vegetables, legumes, fruit and wholegrains and drink plenty of water. Being physically active can also help with reducing constipation.
Nausea and vomiting during pregnancy
Nausea and vomiting, especially ‘morning sickness’, are common during pregnancy, particularly in the first trimester.
Some suggestions that may help include:
- Eat some dry bread, biscuits or cereal before getting up in the morning. Get up slowly, avoiding sudden movements.
- Drink liquids between, rather than with, meals to avoid bloating, as this can trigger vomiting.
- Avoid large meals and greasy, highly spiced foods.
- Suck on something sour like a lemon.
- Relax, rest and get into the fresh air as much as possible. Keep rooms well ventilated and odour free.
- Try food and drinks containing ginger, such as ginger tea, as these sometimes relieve nausea.
Heartburn and pregnancy
Heartburn is common in pregnancy because, as the baby grows, there is more pressure on the abdomen. Small, frequent meals may help, compared to larger meals.
Try to avoid:
- eating late at night
- bending, lifting or lying down after meals
- excessive consumption of tea or coffee.

You may also like to try sleeping with your bedhead raised a little. You can do this by putting a folded blanket or pillow under your mattress.
Alcohol during pregnancy
There is no known safe level of alcohol consumption for women who are pregnant. Consuming alcohol during pregnancy increases the risk of miscarriage, low birth weight, congenital deformities and effects on the baby’s intelligence.
The Australian guidelines to reduce health risks from drinking alcoholExternal Link recommend that the safest option for pregnant women is not to drink alcohol at all.
If you find it difficult to decrease or stop drinking alcohol during pregnancy talk to:
- your doctor or midwife
- your local community health service
- an alcohol and other drug helpline in your state or territory.
The Australian guidelines to reduce health risks from drinking alcoholExternal Linkprovide more information.
Listeria infection and pregnancy
Listeria infection, or listeriosis, is an illness usually caused by eating food contaminated with bacteria known as Listeria monocytogenes. Healthy people may experience no ill-effects from listeria infection at all, but the risks are substantial for pregnant women. The greatest danger is to the unborn baby, with increased risk of miscarriage, stillbirth or premature labour. A listeria infection is easily treated with antibiotics, but prevention is best.
Healthy people may experience no ill-effects from listeria infection at all, but the risks are substantial for pregnant women. The greatest danger is to the unborn baby, with increased risk of miscarriage, stillbirth or premature labour. A listeria infection is easily treated with antibiotics, but prevention is best.
Some foods are more prone to contamination with listeria than others and should be avoided if you are pregnant. They include:
- soft cheeses, such as brie, camembert and ricotta – these are safe if served cooked and hot
- precooked or pre-prepared cold foods that will not be reheated – for example, pre-prepared salads, pâté, quiches and delicatessen meats like ham and salami
- undercooked meat, chilled pre-cooked meats, pâté, meat spread
- raw seafood, such as oysters and sashimi or smoked seafood, such as salmon (canned varieties are safe)
- unpasteurised foods
- pre-prepared or pre-packaged cut fruit and vegetables
- soft-serve ice cream.

The organism that causes listeria infection is destroyed by heat, so properly cooked foods are not a risk.
Salmonella and pregnancy
Salmonella is a cause of food poisoning that can trigger miscarriage. The most likely sources of salmonella are raw eggs and undercooked meat and poultry.
Good food hygiene reduces the risk of infection
Good food hygiene is the best way to reduce the risk of salmonella and listeria infections. Suggestions include:
- Always wash your hands before and after preparing food.
- Keep your kitchen surfaces clean.
- Do not let uncooked food contaminate cooked food.
- Wash fruit, vegetables and salad before eating.
- Cook food thoroughly.
- Keep pets away from kitchen surfaces.
- Wear rubber gloves when handling cat litter trays or gardening.
- Store food at correct temperatures.
Mercury in fish
It is suggested that pregnant women eat 2 to 3 serves of fish every week for their own good health and that of their developing baby. However, pregnant women or women intending to become pregnant within the next 6 months should be careful about which fish they eat. Some types of fish contain high levels of mercury, which can be harmful to the developing foetus.
However, pregnant women or women intending to become pregnant within the next 6 months should be careful about which fish they eat. Some types of fish contain high levels of mercury, which can be harmful to the developing foetus.
When choosing fish, pregnant women should:
- limit to one serve (150 g) per fortnight – billfish (swordfish, broadbill and marlin) and shark (flake), with no other fish eaten in that fortnight
OR - limit to one serve (150 g) per week – orange roughy (deep sea perch) or catfish, with no other fish eaten that week
OR - eat 2 to 3 serves per week – of any other fish or seafood (for example, salmon or tuna).
Note: 150 g is equivalent to approximately 2 frozen crumbed fish portions.
Don’t worry if you’ve had the occasional meal of fish with high levels of mercury. Mercury build-up in the mother’s blood is only a potential problem when that type of fish is eaten regularly.
Where to get help
- Your GP (doctor)
- Midwife
- Obstetrician-gynaecologist
- Dietitians AustraliaExternal Link Tel. 1800 812 942
ᐈ Nutrition during pregnancy - Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
Read more
Once again about hormones or a list of must-haves for the week
Read more
Visit to the urologist. For or Against?
Read more
Preservation of reproductive health
Read more
Pregnancy with uterine fibroids
Read more
Practical skills in examining infertile couples
Read more
Pregnancy with endometriosis: a modern view
Read more
Fighting breast cancer
Read more
Varicocele and impaired spermatogenesis
Obstructive obstructive secretory
men
Learn more
Controlled ovarian stimulation protocols (KOS)
More
Miscarriage. What is the reason?
More
Hysteroscopy and its role in the treatment of infertility
More details
Why you cannot get pregnant
More details
How to calculate the sex of a child before conception
More details
Obstruction of the fallopian tubes More details
02 Ovarian hyperstimulation syndrome: a modern view of the problemRead more
Pregnancy with endometriosis - a modern view
Read more
Immunological infertility and the role of antisperm antibodies in it
More
What is cervical pathology?
More details
IVF in the natural cycle: pros and cons
More details
Practical skills in examining infertile couples
More details
Artificial insemination
More details
skin.Read more
Unable to get pregnant. Where to run? Where to begin?
More
What prospective parents need to know (most popular questions)
More
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
Read more
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
Read more
Infertility and cancer: why men should definitely visit a reproductive specialist
Read more
Sex, children, rock and roll: reproductive specialists on what can increase the chances of IVF
Read more
Portrait of a female doctor: 5 signs of good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never. Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
More details
How to plan for health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
More details
Signs, causes and risk factors of miscarriage003
Read more
Reproductive health of adolescent girls: what children and their parents need to know
Read more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More details
Maxim Gapchuk in "Mother and child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
IVF: modern methods and approaches in the treatment of female infertility
Read more
ICSI: male infertility is not a sentence
Read more
advantages over traditional surgery 0003Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: the essence of the method, stages and results
More details
Diagnosis of infertility in men
More details
10 reasons to see an andrologist for a man
More details
Cryotechnologies as a way of family planning
More details
Read more
Monalisa Touch — what kind of technology is this
More
Premature menopause in men: how to recognize and what is dangerous
More
Why visit a gynecologist for preventive examinations
More details
Laser therapy in gynecology: without anesthesia and pain
More details
Outpatient gynecology - timely seeking qualified help
More details
why additional tests are needed after pregnancy and examinationMore details
Causes and prevention of female infertility
More details
One-day surgery: a modern approach to treatment
3
More details
Pregnancy management: to keep the baby healthy and mother's well-being
More details
Pregnancy after IVF: what future parents need to remember
More details
Anomalies of the uterus and their impact on the onset and carrying of pregnancy.
Read more
Scar on the uterus after caesarean section
Read more
The most common mistakes during pregnancy
Read more
Varicose veins and hemorrhoids during pregnancy
More details
Pregnancy planning (lifestyle)
More details
First aid kit for pregnant women during the war
More details
Periods disappeared during the war. What to do?
More details
Freezing of husband's sperm before the war
More details
A visit to a reproductive specialist during the war
More details
I learned that I was pregnant before the war. What to do?
Read more
What does vaginal discharge mean
Read more
Why can't I get pregnant?
Read more
How to get pregnant if you don't ovulate?
Read more
Male Infertility Diagnosis
Read more
When to See a Gynecologist
Read more
Fertility Program Guide
Learn more
cells
Read more
You are given a chance. What you need to know about artificial insemination
More
What causes thrush and why it comes back
More
Myths about egg donation
More
How to prepare for a gynecological examination More
2 Pregnancy during the warRead more
What tests are done during pregnancy and when
Read more
1st, 2nd and 3rd Trimester Prenatal Screenings
More details
Invasive Prenatal Diagnostics
More details
Non-Invasive Prenatal Diagnostics
More details
Bicornuate Pregnancy3
How ovulation is stimulated
More details
Embryo implantation, or what determines the success of IVF
Read more
When is it better to transfer the embryo - on the third or fifth day?
Read more
How to distinguish the onset of labor from a false alarm
Read more
Nutrition for a pregnant woman
So, your plans and decisions to give birth to a child have come true - you are pregnant! But this news causes you a double feeling: - on the one hand, a feeling of joy, and on the other hand, a feeling of certain fear and even fear of unknown trials for your life and the fate of the unborn baby. What will he be like? - healthy, beautiful, happy?...
And this largely depends on the woman herself, on what lifestyle she will lead during pregnancy and, most importantly, how she will eat.
Nutrition of a woman in different periods of pregnancy
The main thing in the menu of a future mother is variety. She should consume foods from all food groups: meat, fish, vegetables and fruits, dairy products, bread and cereals.
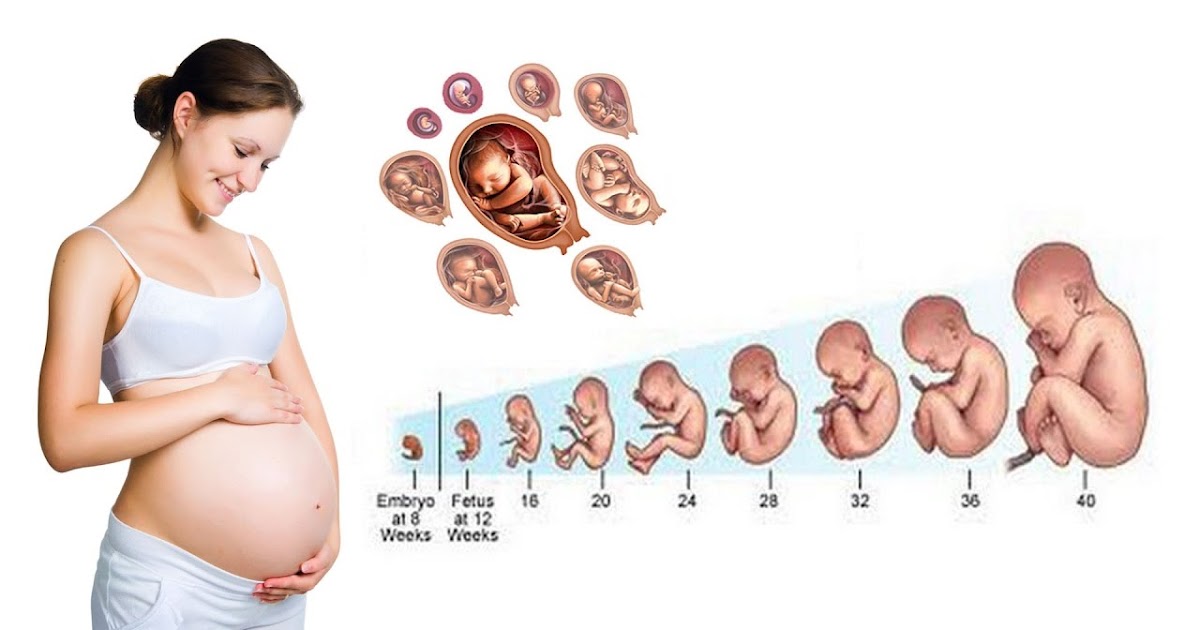
A woman's nutrition during pregnancy can be roughly divided into three periods (trimesters).
If before pregnancy a woman ate normally, felt comfortable, did not experience allergies to any products, then it is not worth changing her diet at an early stage of the first trimester of pregnancy.
During this period, all organs and systems in the child's body are formed, tissues are formed. The body needs complete proteins and vitamins: lean meat (rabbit, chicken, turkey), fish and seafood, dairy products. Be sure to eat rice, fresh or frozen vegetables, seasonal fruits. In the first trimester, many expectant mothers are still working. No matter how difficult it is to control your diet in the workplace, you need to do it - find time for a full breakfast and lunch.
In the first trimester of pregnancy, there is an active restructuring of the body and adaptation to a new state. During this period, it is recommended to switch to a low-calorie diet, which includes more fruits, juices, decoctions of dried fruits, including rose hips. At the very beginning of pregnancy, especially if toxicosis torments, more frequent, but less plentiful meals are recommended.
Always keep a hematogen, a bag of nuts or dried fruit in your pocket to have a snack on the street. If your condition does not allow you to eat regular food, you should pay attention to baby food. Baby products literally save expectant mothers suffering from severe toxicosis. These are boxed cereals, children's curds, cookies and fruit purees.
In the first trimester, special attention must be paid to the quality of products. Gradually abandon sauces, semi-finished products and canned food containing harmful chemical additives. Do not forget that the placenta freely accumulates and passes chemistry. The importance of products containing folic acid is great, without it intensive metabolism is impossible, its deficiency can cause developmental abnormalities. Folic acid is found in greens, nuts, white cabbage and broccoli, beets, legumes, and eggs.
According to nutritionists, the diet of pregnant women should be 300 kcal / day higher than that of non-pregnant women, but in the first trimester there is no need to increase the energy value of the diet at all; in the second trimester, an additional 340 kcal / day is required; in the third trimester - 452 kcal / day. Pregnant women generally get enough calories, and more than 80% of women achieve and even exceed the required weight gain. These extra calories benefit the fetus. An underweight woman should gain 16–20 kg during her entire pregnancy, an overweight woman about 7 kg, and a normal body weight of 11–12 kg.
In the second trimester there are active jumps in the height and weight of the baby and uterus, so the caloric content of the diet needs to be increased. It is desirable to eat more and better. At this time, the need for trace elements increases: iron, magnesium, zinc, selenium, calcium, potassium. The child creates his own "reserve" of trace elements using the mother's resource, which means that the mother should have enough of them for two.
Very often in pregnant women in the second trimester hemoglobin drops, this is a normal physiological phenomenon, if it is not threatening to health. You can increase hemoglobin by eating red meat, chicken, fish, dried fruits, pomegranates, green vegetables and fresh herbs, buckwheat, citrus fruits (oranges, grapefruits, pomelo, lemons), rosehip and berry infusions.
In the second trimester, a pregnant woman should limit the intake of smoked and fried foods, as well as salt in her diet. In no case should you limit the liquid. Pure water is the best drink for a pregnant woman, and water should be consumed up to 2-2.5 liters per day. Water is a natural drink for the body, it does not cause complications and has no contraindications. Edema is caused not by water, but by salt, which we not only add in its pure form, but also consume with canned food, mayonnaise, cheese, and sausage. The absence of salt is not harmful, it is naturally found in many products: vegetables, bread, so the diet will not remain completely without it. Excess salt disrupts metabolism.
During this period, you can increase the calorie content of food. Childbirth must be approached physically strong. It is better to eat meat and fish in the morning, for breakfast and lunch, and for dinner, prepare dairy and vegetable dishes: cheesecakes, stewed vegetables, cottage cheese and vegetable casseroles. It is necessary to minimize the intake of canned food, smoked meats, pickles and marinades, hot spices and fatty foods. Frequent walks in the air, physical activity are recommended.
In the third trimester, it is necessary to reduce the calorie content of foods at the expense of confectionery and flour products, eat less fatty meat, as well as cheese and sour cream.
By the end of this period, many experts advise pregnant women to give up meat altogether in order to increase tissue elasticity and prevent ruptures.
During the entire period of pregnancy, special attention should be paid to the combination of products. If you combine foods wisely, you can ensure more efficient absorption of food. If the food is digested poorly, then this can lead to rotting and fermentation of products and the formation of substances harmful to the body of the mother and child. In addition, the fermentation process is accompanied by gas formation, which can lead to flatulence (bloating) and discomfort. This is especially harmful in the last stages of pregnancy.
Try not to take the first, second and third course at the same time; this overflows the stomach and presses on the fetus, the food is poorly digested and poorly absorbed. Eat little and often. It is not recommended to eat immediately before starting work, a long walk, before charging and immediately after it; it is advisable to rest for 10 minutes before eating.
Eat only when you are hungry, try not to snack on the go. Follow the diet, eat at about the same time.
Proper preparation of food will help to maximize the useful substances contained in the products. Do not overcook food, try not to reheat the same dish several times, it is better to set aside only the portion that will be used. Cook in the most gentle way: baking, steaming, stewing. Avoid frying, boiling in large amounts of water, with this method of processing products, many useful substances are lost. If possible, do not cook for several days at once. Do not use aluminum cookware when cooking. Remember that for a pregnant woman, it is not calories that are important, but the quality of food, its naturalness, primarily a “living cell” (whole cereals, raw vegetables and fruits, fresh meat and dairy products).
What can harm the pregnant woman and the fetus
Smoking and alcohol – quit smoking from the first days of pregnancy, if you have smoked before, avoid "passive" smoking, and do not consume alcoholic beverages in any doses.
Lack of vitamins and microelements in the body - their absence or deficiency can lead to irreparable consequences. So, for example, iodine deficiency can lead to mental retardation of a child, folic acid deficiency - to severe fetal deformities, calcium deficiency - to a violation of the formation of the child's skeleton, iron deficiency - to anemia and a delay in the physical and neuropsychic development of the child. It is necessary to consult a doctor, perhaps he will recommend switching to iodized salt, as well as supplementing your diet with a vitamin-mineral complex and folic acid.
Excess weight is the risk of having a large child, which means the risk of complications during childbirth and the child's tendency to become obese at an older age.