How long can morning sickness last
Morning Sickness: Nausea and Vomiting of Pregnancy
-
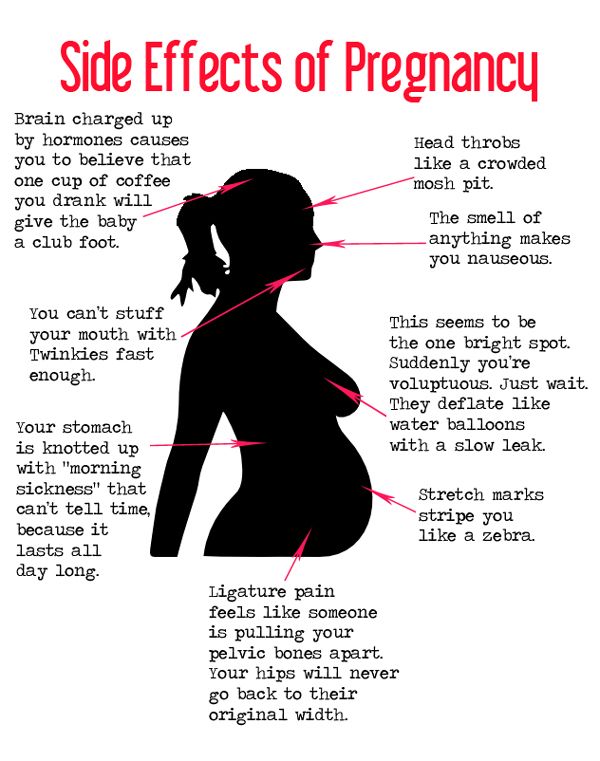
Nausea and vomiting of pregnancy is a common condition. It can occur any time during the day, even though it’s often called “morning sickness.” Nausea and vomiting of pregnancy usually doesn’t harm the fetus, but it can affect your life, including your ability to work or go about your normal everyday activities. There are safe treatment options that can make you feel better and keep your symptoms from getting worse.
-
Nausea and vomiting of pregnancy usually starts before 9 weeks of pregnancy. For most women, it goes away by 14 weeks of pregnancy. For some women, it lasts for several weeks or months. For a few women, it lasts throughout the pregnancy.
-
Some women feel nauseated for a short time each day and might vomit once or twice.
In more severe cases, nausea lasts several hours each day and vomiting occurs more frequently.
-
You should talk with your obstetrician-gynecologist (ob-gyn) or other obstetric care provider if nausea and vomiting of pregnancy affects your life and causes you concern.
-
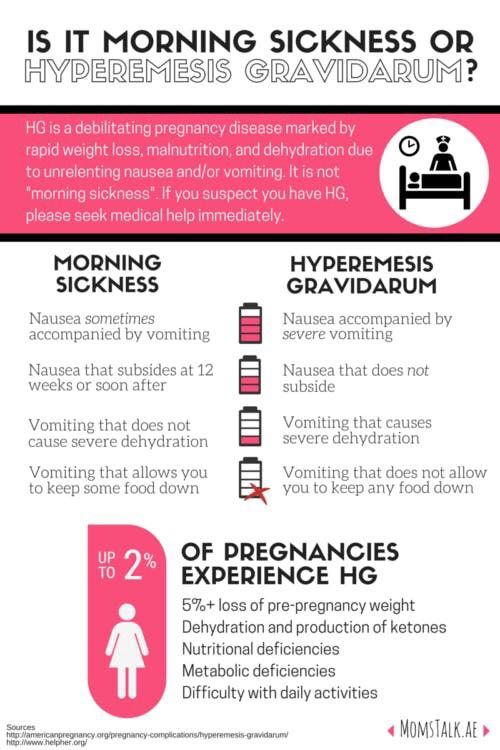
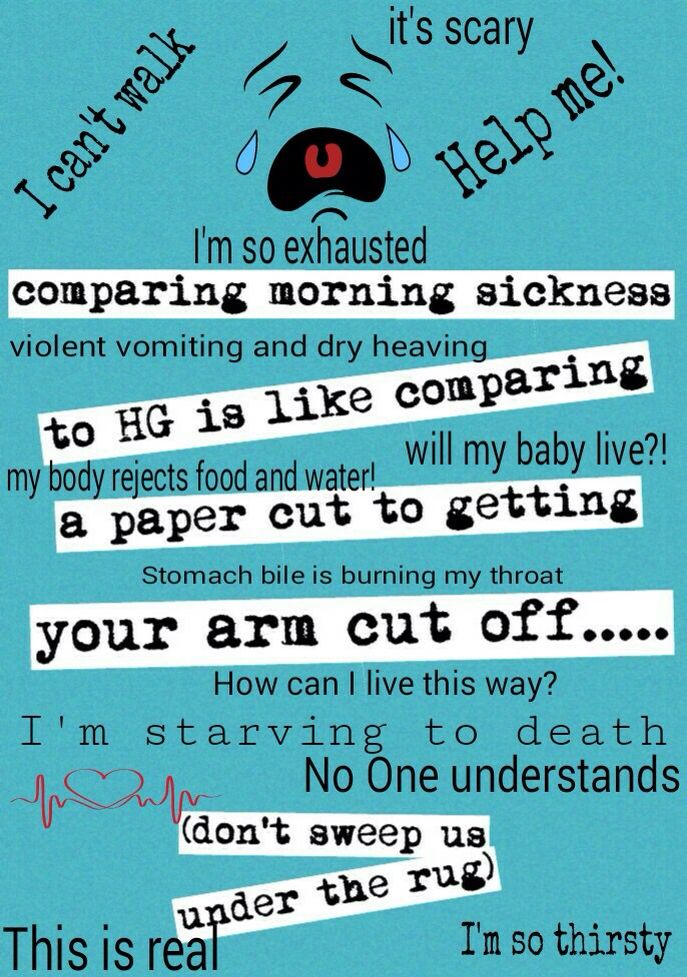
Hyperemesis gravidarum is the term for the most severe form of nausea and vomiting of pregnancy. Hyperemesis gravidarum occurs in up to 3 percent of pregnancies.
-
This condition may be diagnosed when a woman has lost 5 percent of her prepregnancy weight and has other problems related to dehydration, or loss of body fluids (see below).
 Women with hyperemesis gravidarum need treatment, sometimes in a hospital, to stop the vomiting and restore body fluids.
Women with hyperemesis gravidarum need treatment, sometimes in a hospital, to stop the vomiting and restore body fluids. -
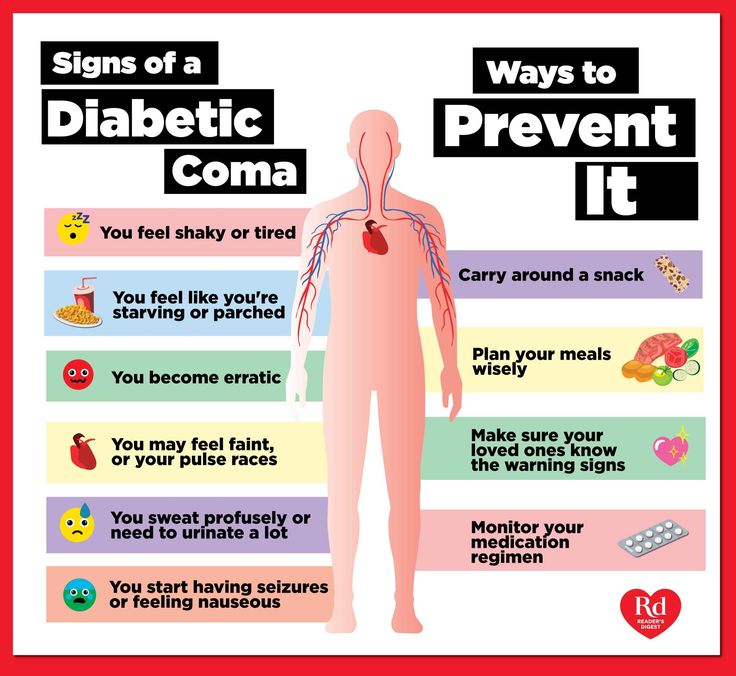
Nausea and vomiting can cause you to lose fluids. If fluids are not replaced, it can lead to dehydration. You should call your ob-gyn or other obstetric care provider if you have the following signs and symptoms of dehydration:
-
You have a small amount of urine that is dark in color.
-
You are unable to urinate.
-
You cannot keep down liquids.
-
You are dizzy or faint when standing up.
-
You have a racing or pounding heartbeat.
-
-
Any of the following can increase the risk of severe nausea and vomiting of pregnancy:
-
Being pregnant with more than one fetus (multiple pregnancy)
-
A previous pregnancy with either mild or severe nausea and vomiting
-
Your mother or sister had severe nausea and vomiting of pregnancy
-
A history of motion sickness or migraines
-
Being pregnant with a female fetus
-
-
Yes, some medical conditions can cause nausea and vomiting during pregnancy.
 These conditions include:
These conditions include:Your ob-gyn or other obstetric care provider might suspect that you have one of these conditions if you have signs or symptoms that usually do not occur with nausea and vomiting of pregnancy. Some of these signs and symptoms include:
-
Nausea and vomiting that occurs for the first time after 9 weeks of pregnancy
-
Abdominal pain or tenderness
-
Fever
-
Headache
-
Enlarged thyroid gland (swelling in the front of the neck)
-
-
This condition usually does not harm your health or your fetus’s health. It also does not mean that your fetus is sick.
-
Nausea and vomiting can become more of a problem if you cannot keep down food or fluids and begin to lose weight.
 When this happens, it sometimes can affect the fetus’s weight at birth.
When this happens, it sometimes can affect the fetus’s weight at birth. -
Weight loss can lead to problems with your thyroid, liver, and fluid balance. Because hyperemesis gravidarum is difficult to treat and can cause health problems, experts recommend early treatment so that it does not become severe.
-
Changes to your diet and lifestyle might help you feel better. These change can include:
-
Yes, take a prenatal vitamin. Studies show that taking a vitamin supplement before and during pregnancy reduces the risk of having severe nausea and vomiting of pregnancy.
-
-
Eat dry toast or crackers in the morning before you get out of bed to avoid moving around on an empty stomach.
-
Eat five or six “mini meals” a day to ensure that your stomach is never empty.
-
Eat frequent bites of foods like nuts, fruits, or crackers.
-
-
Try bland foods. The BRATT diet (bananas, rice, applesauce, toast, and tea) is low in fat and easy to digest. If these foods don’t appeal to you, try others. The goal is to find foods that you can eat and that stay down.
-
Yes, try adding protein to each meal. Good nonmeat sources of protein include:
-
Dairy foods, such as milk, ice cream, and yogurt
-
Nuts and seeds, including butters like almond butter and peanut butter
-
Protein powders and shakes
-
-
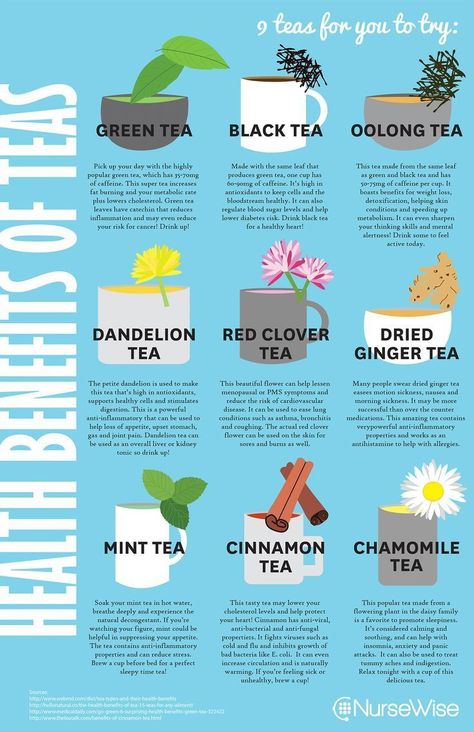
Ginger can help settle your stomach.
 You can try:
You can try: -
Yes, your body needs more water during pregnancy. Drink throughout the day, not just when you are thirsty. Aim for 8 to 12 cups of water a day during pregnancy.
Not drinking fluids can lead to dehydration, which can make nausea worse. If a bad taste in your mouth makes it hard to drink water, chew gum or eat hard candy.
-
Foods or odors that might never have bothered you before might now trigger nausea. Do your best to stay away from them. Use a fan when cooking. Have someone else empty the trash.
-
Frequent vomiting can cause some of your tooth enamel to wear away, due to the acid in your stomach.
 Rinse your mouth with a teaspoon of baking soda dissolved in a cup of water to help neutralize the acid and protect your teeth.
Rinse your mouth with a teaspoon of baking soda dissolved in a cup of water to help neutralize the acid and protect your teeth. -
If diet and lifestyle changes don’t help, or if you have severe nausea and vomiting of pregnancy, you might need medical treatment. Your ob-gyn or other obstetric care provider will first want to know whether your symptoms are due to nausea and vomiting of pregnancy or another medical cause. If other causes are ruled out, you may be able to take certain medications:
-
Vitamin B6 is a safe, over-the-counter treatment that may be tried first for nausea and vomiting of pregnancy.
-
Doxylamine, a medication found in over-the-counter sleep aids, can be added if vitamin B6 alone does not relieve symptoms.
-
A prescription drug that combines vitamin B6 and doxylamine is available.
 Both drugs, taken alone or together, have been found to be safe to take during pregnancy and have no harmful effects on the fetus.
Both drugs, taken alone or together, have been found to be safe to take during pregnancy and have no harmful effects on the fetus.
-
-
“Antiemetic” drugs, which prevent vomiting, may be prescribed for women who aren’t helped by other medications.
-
Many antiemetic drugs have been shown to be safe to use during pregnancy. But others have conflicting or limited safety information. For example, a drug called ondansetron is highly effective in preventing nausea and vomiting, but studies are not clear about its safety for the fetus. Ondansetron also has been linked to heart-rhythm problems in people taking the drug, especially in those who have certain underlying conditions.
-
The decision to use ondansetron and other drugs during pregnancy is based on whether the benefits of these drugs outweigh their potential risks.
 You and your ob-gyn or other obstetric care provider can discuss all of these factors to determine the best treatment for you.
You and your ob-gyn or other obstetric care provider can discuss all of these factors to determine the best treatment for you. -
If your nausea and vomiting are severe or if you have hyperemesis gravidarum, you might need to stay in the hospital until your symptoms are under control.
-
-
Lab tests may be done to check how your liver is working.
-
If you are dehydrated, you may receive fluids and vitamins through an intravenous (IV) line.
-
If your vomiting cannot be controlled, you might need additional medication.
-
If you continue to lose weight, a feeding tube may be recommended to ensure that you and your fetus are getting enough nutrients.

-
-
Dehydration: A condition that happens when the body does not have as much water as it needs.
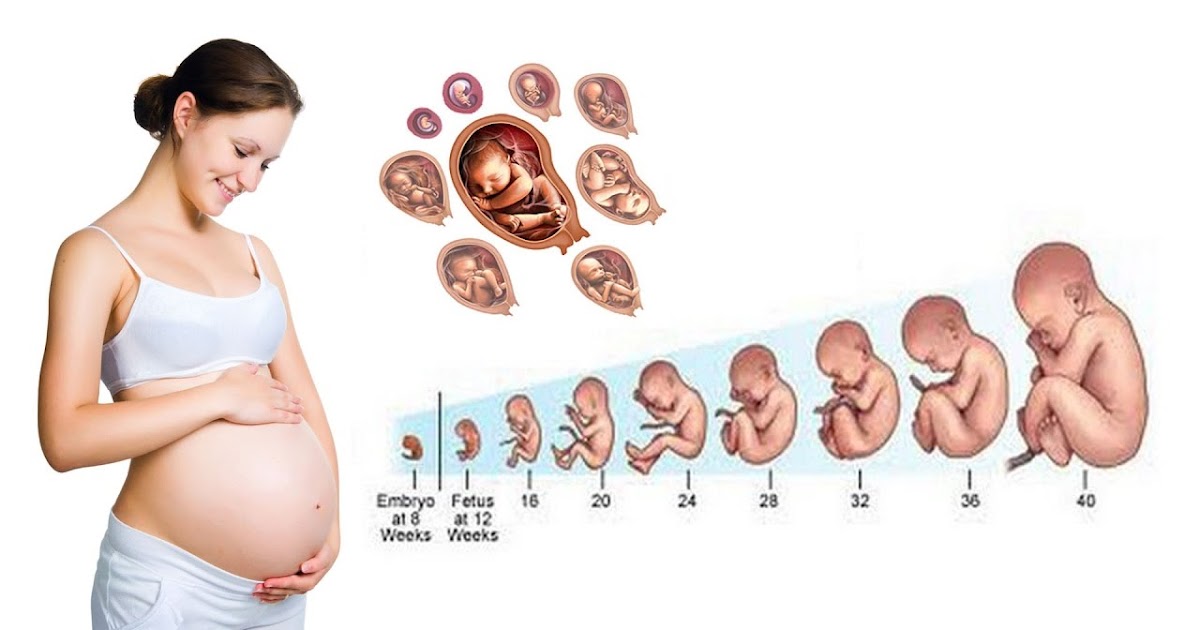
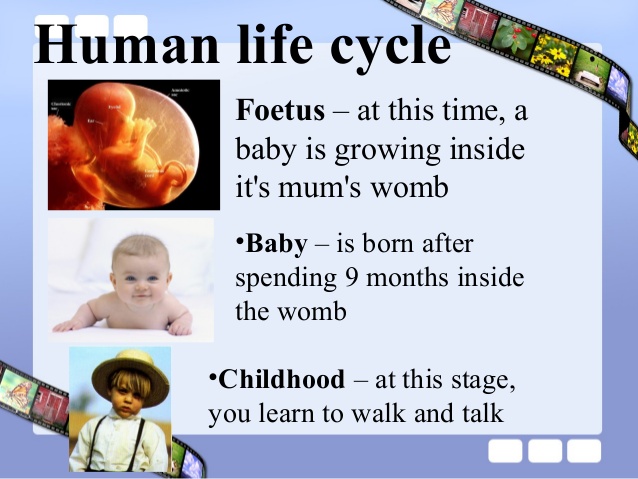
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Hyperemesis Gravidarum: Severe nausea and vomiting during pregnancy that can lead to loss of weight and body fluids.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.
Multiple Pregnancy: A pregnancy where there are 2 or more fetuses.
Nausea and Vomiting of Pregnancy: A condition that occurs in early pregnancy, usually starting before 9 weeks of pregnancy.
Nutrients: Nourishing substances found in food, such as vitamins and minerals.
Obstetric Care Provider: A health care professional who cares for a woman during pregnancy, labor, and delivery.
 These professionals include obstetrician–gynecologists (ob-gyns), certified nurse–midwives (CNMs), maternal–fetal medicine specialists (MFMs), and family practice doctors with experience in maternal care.
These professionals include obstetrician–gynecologists (ob-gyns), certified nurse–midwives (CNMs), maternal–fetal medicine specialists (MFMs), and family practice doctors with experience in maternal care.Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Thyroid Gland: A butterfly-shaped gland located at the base of the neck in front of the windpipe. This gland makes, stores, and releases thyroid hormone, which controls the body’s metabolism and regulates how parts of the body work.
Don't have an ob-gyn? Search for doctors near you.
FAQ126
Published: May 2020
Last reviewed: December 2021
Topics:
Pregnancy Pregnancy Discomforts and Other Concerns
Copyright 2023 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
Morning sickness | March of Dimes
Morning sickness is when you have nausea and vomiting during pregnancy. Even though it’s called morning sickness, it can happen any time of day.
Morning sickness usually starts at about 6 weeks of pregnancy and goes away in the second trimester.
Lots of pregnant women have morning sickness. It usually doesn’t cause harm to you or your baby.
Hyperemesis gravidarum is severe nausea and vomiting that needs treatment (sometimes in a hospital) to help you get better.
If your morning sickness is severe or if it goes into your fourth month of pregnancy, tell your health care provider right away.
What is morning sickness?
Morning sickness (also called nausea and vomiting of pregnancy) is nausea (feeling sick to your stomach) and vomiting that happens in the first few months of pregnancy. Even though it's called morning sickness, it can last all day and happen any time of day.
At least 7 in 10 pregnant women have morning sickness in the first trimester (first 3 months) of pregnancy. It usually starts at about 6 weeks of pregnancy and is at its worst at about 9 weeks. Most women feel better in their second trimester, but some have morning sickness throughout pregnancy. If you have morning sickness, tell your health care provider.
Mild morning sickness doesn’t harm you or your baby. But if nausea and vomiting becomes severe (called hyperemesis gravidarum), it can cause serious problems during pregnancy. You may need to stay in the hospital for treatment.
What is hyperemesis gravidarum?
About 3 in 100 women may have hyperemesis gravidarum. This is extreme, excessive nausea and vomiting during pregnancy. It can cause you to lose weight and become dehydrated (not have enough water in your body). It can start early in pregnancy and last the entire pregnancy. If you have hyperemesis gravidarum, you need treatment to help keep you and your baby safe.
This is extreme, excessive nausea and vomiting during pregnancy. It can cause you to lose weight and become dehydrated (not have enough water in your body). It can start early in pregnancy and last the entire pregnancy. If you have hyperemesis gravidarum, you need treatment to help keep you and your baby safe.
You may be at risk for hyperemesis gravidarum if you:
- Are pregnant for the first time.
- Are pregnant with a girl.
- Are pregnant with multiples (twins, triplets or more). Being pregnant with more than one baby may increase your risk for severe morning sickness because you may have a large placenta and increased pregnancy hormones. The placenta grows in your uterus (womb) and supplies your babies with food and oxygen through the umbilical cord.
- Had mild or severe morning sickness in a previous pregnancy, or your mother or sister had severe morning sickness during pregnancy. Take your family health history to help you find out about health conditions that run in your family.
- Have motion sickness or migraines. A migraine is a severe headache that may make you sensitive to bright lights and sound.
- Are overweight.
- Have trophoblastic disease, a condition that leads to abnormal cell growth in the uterus (womb).
Signs and symptoms of hyperemesis gravidarum include:
- Vomiting more than 3 to 4 times a day
- Vomiting that makes you dizzy or lightheaded
- Vomiting that makes you dehydrated. Signs and symptoms of dehydration include feeling thirsty, dry mouth, a fast heart beat or making little to no urine.
- Losing more than 10 pounds in pregnancy
If you have hyperemesis gravidarum, your provider may treat you with medicine to help relieve your nausea and vomiting. You may need treatment in a hospital with intravenous (also called IV) fluids. IV fluids go through a needle into your vein. They help you stay hydrated and can give you nutrients that you usually get from food. If you continue to lose weight, you may need a feeding tube to make sure you’re getting enough nutrients for you and your baby.
What causes morning sickness?
We don’t know for sure what causes morning sickness. It may be caused by low blood sugar or increased pregnancy hormones. Morning sickness may be worse if you’re stressed or overly tired, if you eat certain foods or if you’re traveling (if you often have motion sickness).
Can you prevent or relieve morning sickness?
Yes. Here’s what you can do to help you feel better and even prevent morning sickness:
- Take a prenatal vitamin before you get pregnant. Talk to your health care provider about which one to take. Sometimes vitamins can upset your stomach, so take it with a snack.
- Keep snacks by your bed. Eat a few crackers before you get up in the morning to help settle your stomach.
- Eat 5 or 6 small meals each day instead of 3 larger meals.
- Eat foods that are low in fat and easy to digest, like cereal, rice and bananas. Don’t eat spicy or fatty foods.
- Eat healthy snacks between meals.
 This can help keep your stomach from being empty and helps prevent nausea. Try snacks that are high in protein, like milk or yogurt.
This can help keep your stomach from being empty and helps prevent nausea. Try snacks that are high in protein, like milk or yogurt. - Drink plenty of fluids, especially water.
- Avoid smells that upset your stomach.
You may have heard about these ways to prevent or relieve morning sickness. Talk to your provider before trying any of these:
- Acupressure and acustimulation (also called electrical nerve stimulation) wristbands. These involve putting pressure on or stimulating certain points of the body (called pressure points) to help prevent nausea.
- Acupuncture. This is a kind of treatment in which thin needles are put into your skin. If you’re thinking about acupuncture to help with morning sickness, tell your provider and find an acupuncturist who is trained to work with pregnant women.
- Ginger. Ginger is an herb (plant) used in cooking and medicine. Ginger ale, tea or candies may help relieve morning sickness.
Even if it’s legal where you live for either personal or medical use, it’s not safe to use marijuana to treat morning sickness. No amount of marijuana has been proven safe to use during pregnancy. If you’re thinking of using marijuana to help with morning sickness, talk to your provider about other treatments that are safer for your baby.
No amount of marijuana has been proven safe to use during pregnancy. If you’re thinking of using marijuana to help with morning sickness, talk to your provider about other treatments that are safer for your baby.
Is there medical treatment for morning sickness?
Yes. If you can’t relieve morning sickness on your own or if you have severe nausea and vomiting of pregnancy, your provider may treat you with these medicines:
- Vitamin B6 and doxylamine. Your provider may treat you with these medicines separately or together. You can get vitamin B6 and doxylamine over-the-counter (OTC), which means you don’t need a prescription for them from your provider. Doxylamine is found in some OTC sleep aids (medicines that help you sleep). Or your provider may prescribe you a medicine that combines them.
- Antiemetic drugs. These are drugs that help prevent vomiting. If Vitamin B6 and doxylamine don’t work, your provider may prescribe an antiemetic drug for you.
 Not all are safe to use during pregnancy, so talk to your provider to make sure the medicine is a good choice for you.
Not all are safe to use during pregnancy, so talk to your provider to make sure the medicine is a good choice for you.
Talk to your provider before you take any medicine during pregnancy, even medicine to help treat morning sickness.
When should you call your health care provider about morning sickness?
For most women, morning sickness is mild and goes away over time. But call your provider if:
- Your morning sickness continues into your 4th month of pregnancy.
- You lose more than 2 pounds.
- Your vomit is brown in color or has blood in it. If so, call your provider right away.
- You vomit more than 3 times a day and can’t keep food or fluids down.
- Your heart beats faster than usual.
- You’re tired or confused.
- You’re making much less urine than usual or no urine at all.
Last reviewed: September, 2020
〚 When will it end? How long does toxicity last? 〛Babystart Official Distributor
January 26, 2020
You feel like you are on a rocking boat when you drive to work, sit in meetings, take your kids to bed. Will it ever end?
Will it ever end?
The good news is that this will most likely end - and relatively soon. Here's what to expect.
Morning sickness usually lasts 6 to 12 weeks with a peak of 8 to 10 weeks. According to an oft-cited study from 2000, 50 percent of women have completed this unpleasant phase by 14 weeks of pregnancy, or around the time they enter their second trimester. The same study showed that 90 percent of women are past morning sickness by 22 weeks.
Although these weeks may seem awfully long, it can be a strange consolation that this means the hormones are doing their job and the baby is thriving. In fact, a 2016 study found that women who had at least one prior pregnancy loss and nausea and vomiting during week 8 were 50 percent less likely to have a miscarriage.
However, it should be noted that this was a correlational study and therefore cannot suggest cause and effect. This means that the opposite is not true: the absence of symptoms does not necessarily mean a higher chance of miscarriage.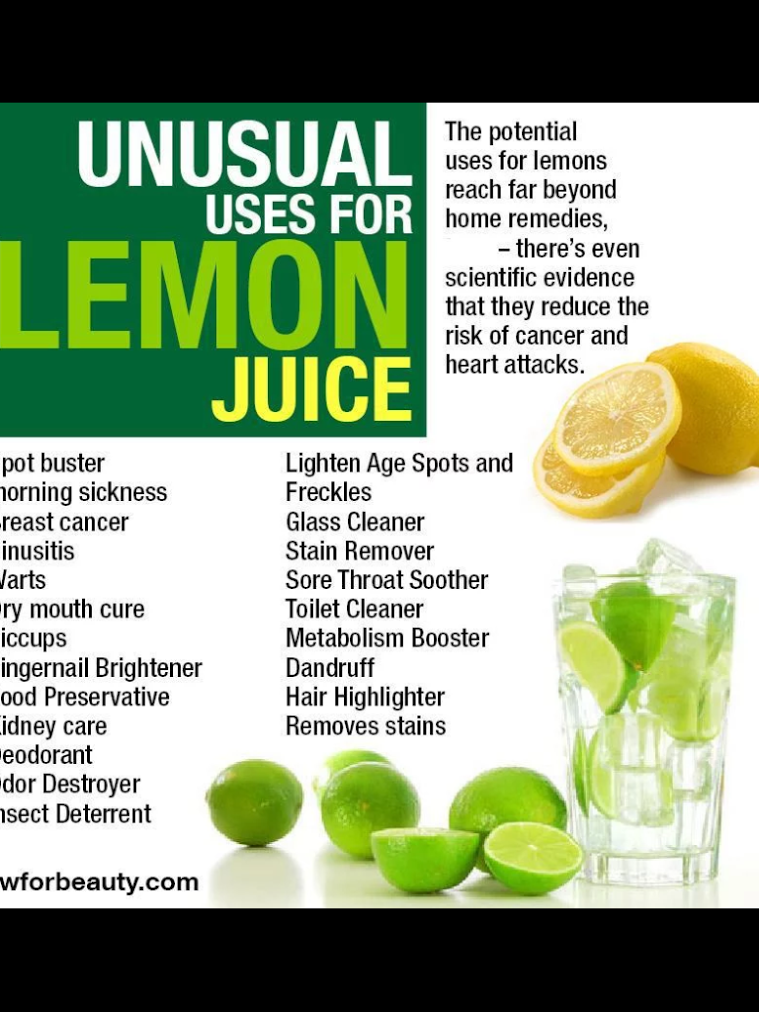
The same study also found that about 80 percent of these women experienced nausea and/or vomiting during the first trimester. So you are not alone, to put it mildly.
How long does morning sickness last?
If you're in the middle of it, you can probably attest to the fact that morning sickness definitely doesn't just happen in the morning. Some people are sick all day, while others struggle during the day or evening.
The term "morning sickness" comes from the fact that after waking up all night without food, you may wake up worse than usual. But only 1.8 percent of pregnant women only get sick in the morning, according to this 2000 study. Some health professionals have begun to name a group of symptoms of NVP, nausea and vomiting during pregnancy.
If you find yourself in the unfortunate group of people who are nauseated all day, you are not alone - and again the symptoms should disappear after the first trimester.
What if I'm still sick after 14 weeks?
If you have morning sickness during pregnancy longer than usual, or if you are vomiting severely, call your doctor.
A condition called Hyperemesis gravidarum occurs in 0.5 to 2 percent of pregnancies. This includes severe and persistent vomiting, which can lead to hospitalization for dehydration.
Women experiencing this condition lose more than 5 percent of their body weight, and it is the second most common reason for pregnant women to stay in the hospital. Most of these rare cases resolve before the 20-week mark, but 22 percent of them persist until the end of the pregnancy.
If you have had it once, you have a higher risk of having it in future pregnancies. Other risk factors include:
- family history of condition
- young age
- first time pregnancy
- twins
- be overweight or obese
What causes morning sickness?
Although the cause is not entirely clear, medical professionals believe that morning sickness is a side effect of human chorionic gonadotropin (hCG), commonly referred to as the "pregnancy hormone.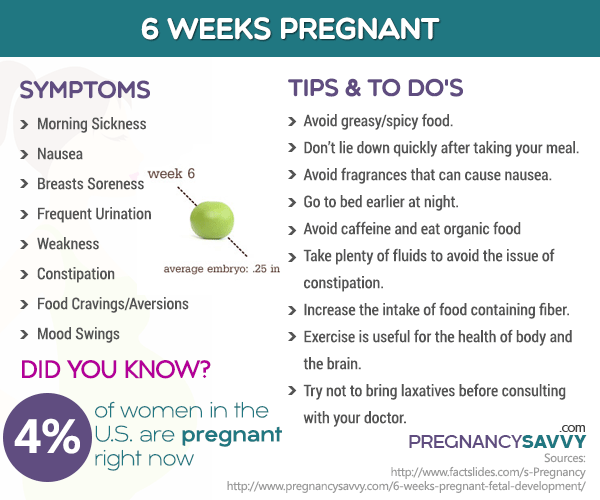 " When the hormone levels rise, as they do in the healthy first trimester of pregnancy, it is thought to cause nausea and vomiting.
" When the hormone levels rise, as they do in the healthy first trimester of pregnancy, it is thought to cause nausea and vomiting.
This theory is further supported by the idea that people who have twins often experience more severe morning sickness.
It is also possible that morning sickness (and food aversion) is a way to protect the child's body from potentially harmful bacteria in food. But, in particular, hCG levels peak towards the end of the first trimester, and then levels off - and even decreases. This is further evidence for the hCG theory, which may also be the cause of these food aversions.
Who is more susceptible to morning sickness?
Some women experience little to no morning sickness, while others are at increased risk of a more severe condition.
Those who are pregnant with twins or more may have more severe symptoms as their hormone levels are higher than a pregnancy with one child.
It may be helpful to ask female family members, such as your mother or sister, about their experience of nausea and vomiting, as this can run in the family.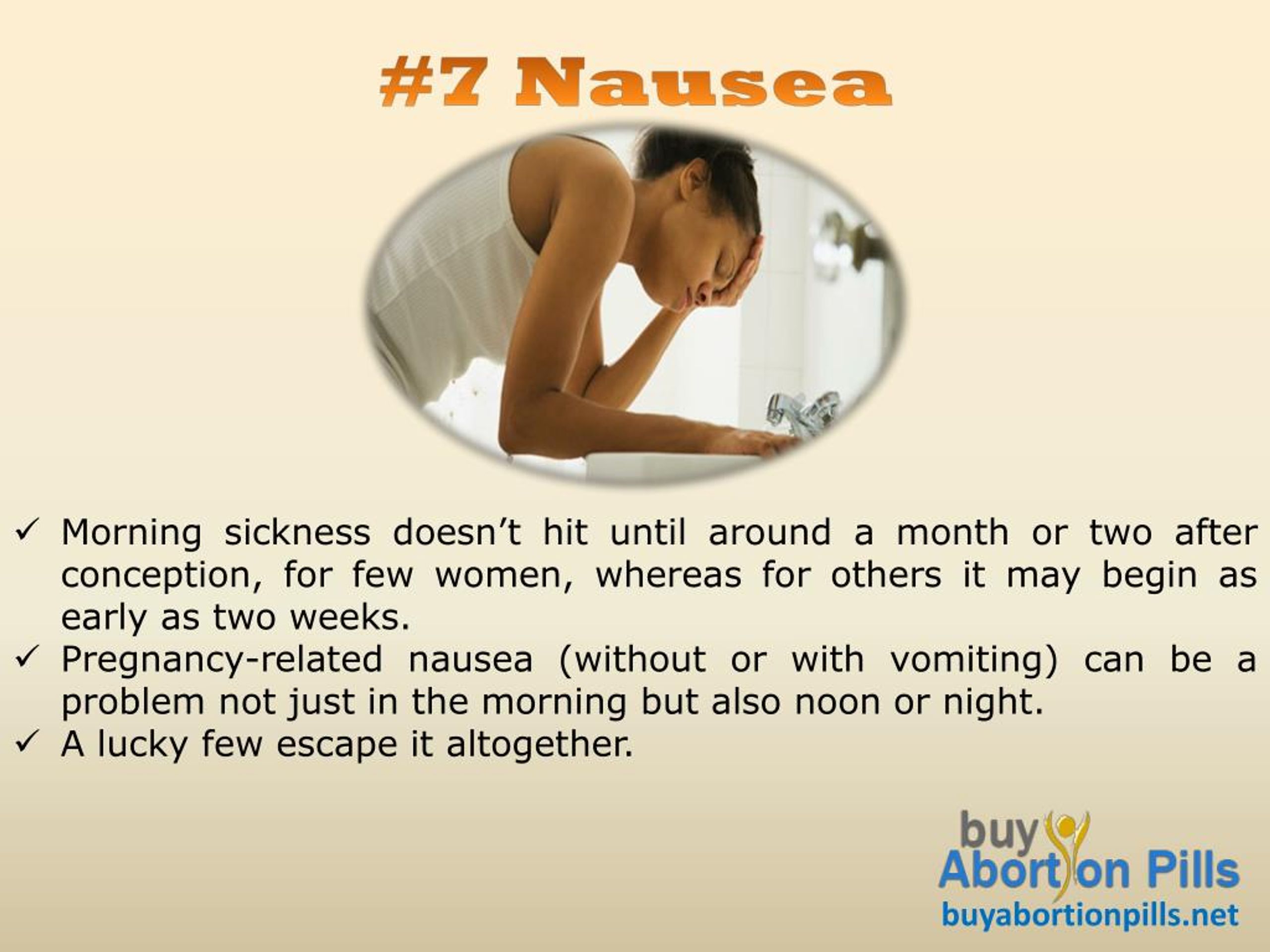 Other risk factors include:
Other risk factors include:
- History of migraine or motion sickness
- previous pregnancy with severe morning sickness
- be a pregnant girl (but don't use the severity of morning sickness to determine your baby's gender!)
How to Manage Morning Sickness
Ironically, food is one of the most recommended ways to help with morning sickness, no matter what time of day you experience it. An empty stomach makes things worse, and even if you don't feel like eating, small meals and snacks can help relieve nausea.
Some people find it helpful to eat soft foods such as toast and crackers. Sip on tea, juice, liquids, and anything else you can drink to stay hydrated. Don't eat right before you go to bed and keep a small snack by your bed to eat as soon as you wake up.
Preventing that empty stomach is the main goal, even if it means finding something small to eat every hour.
We fight against toxicosis - articles from the specialists of the clinic "Mother and Child"
Alexandrova Anna Evgenievna
Embryologist
Clinic "Mother and Child" South-West
rest more
Very often in the first trimester, the expectant mother feels weakness, drowsiness, she wants to lie down to rest, and sometimes she simply does not even have the strength to move. This, of course, is not toxicosis, but if such sensations arise, then they must be indulged so as not to inadvertently provoke another attack of nausea. Get plenty of rest and do not make any sudden movements, because even if you just fail to get up from a chair, you can provoke an attack of nausea.
This, of course, is not toxicosis, but if such sensations arise, then they must be indulged so as not to inadvertently provoke another attack of nausea. Get plenty of rest and do not make any sudden movements, because even if you just fail to get up from a chair, you can provoke an attack of nausea.
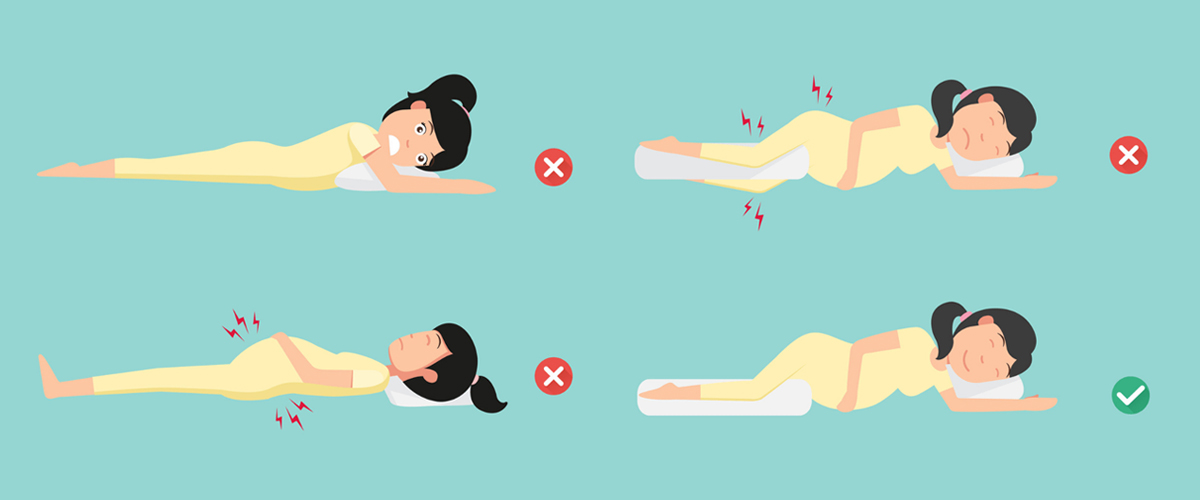
Sleep with the windows open: the air in the bedroom should be fresh and cool. Go to bed on time, do not sit at midnight in front of the TV or at the computer, eliminate all irritating factors: an uncomfortable mattress, blanket, pillow, hard bedding - lack of sleep can respond with morning sickness.
Eat right
Eat fractionally, 5-6 times a day, or even more often, and always in small portions. When you wake up, don't get out of bed right away. One of the most effective methods against toxicosis is breakfast in bed. In the evening, put crackers, yogurt, or any product that you can tolerate well next to your bed. Eat it before you get up, and then lie down for a while. Most likely, morning sickness will either not appear at all, or will be very weak.
Most likely, morning sickness will either not appear at all, or will be very weak.
Usually, in case of toxicosis, it is not recommended to eat fatty, smoked, salty, pickled, drink soda (the usual set of food hazards). But it is likely that some not very healthy product will now be well tolerated, and something from healthy food, on the contrary, will cause nausea. "Pregnant whims" - a cake with herring or pineapples at night - these are the requests of the body that it needs one or another component in food. For example, the desire to chew chalk is a sign of calcium deficiency. So eat what you like and what you want, within reason, of course. And if you don’t feel like something, even if this product is extremely useful and necessary, don’t eat it. If you feel sick from some dish, it means that the body signals you: I don’t need this now!
drink more often
Toxicosis may not be limited to nausea, some may also vomit. This means fluid is lost. Therefore, between meals, drink more often: a sip or two of mineral water or tea with lemon will help to cope with nausea and replenish lost fluids. But drink in small sips. Also, you should not drink food and you should give up soups for a while - a large amount of food drunk and eaten, on the contrary, only provokes nausea and vomiting.
But drink in small sips. Also, you should not drink food and you should give up soups for a while - a large amount of food drunk and eaten, on the contrary, only provokes nausea and vomiting.
breathe fresh air
Outdoor walks are good for everyone, but especially for toxicosis. Firstly, when walking, the blood of the expectant mother and baby is saturated with oxygen, which is very important for health, and secondly, walking calms the nervous system. Together, this helps to reduce the unpleasant symptoms of toxicosis. You need to walk at least two hours a day - but not just along the street, but in the place where the air is really fresh: in the forest, park, square, and best of all outside the city. Before you go out, think over the route: go away from gas-polluted highways, street cafes, food stalls and other "fragrant" places.
eliminate fragrances
Taste and smell preferences change during the first trimester. Now even your favorite perfumes can cause nausea, headaches and allergic reactions. Therefore, put away all fragrant cosmetics that irritate you: perfumes, deodorants, creams, and so on. You will have to stop using your favorite perfume for both your husband and loved ones. Explain to others that this is not a whim, but a temporary measure, very soon everything will return to normal.
Therefore, put away all fragrant cosmetics that irritate you: perfumes, deodorants, creams, and so on. You will have to stop using your favorite perfume for both your husband and loved ones. Explain to others that this is not a whim, but a temporary measure, very soon everything will return to normal.
And do not worry that now you will be left without your usual beauty products. Both the cosmetic store and the pharmacy are full of different creams, tonics, shampoos without fragrance or with a minimal smell.
work with yourself
Psychologists believe that the cause of toxicosis is not only in hormonal changes, but also in the psychological state of a woman. The more a woman experiences, the more anxieties and fears she has, the more pronounced toxicosis can be. Ideally, it is better to limit yourself during pregnancy from any stress. Of course, it’s not always possible to eliminate nervous work or crowding in public transport, but watch less TV, don’t read negative news and various pregnant “horror stories” on the Internet, and don’t react to minor or even major everyday troubles everyone can do. Therefore, if you are worried about toxicosis, create your own comfortable world during pregnancy. If you can’t cope on your own, contact a specialist (psychologist). Toxicosis is really well treated with psychotherapy. The main thing is that the expectant mother should want to get rid of her own anxiety.
Therefore, if you are worried about toxicosis, create your own comfortable world during pregnancy. If you can’t cope on your own, contact a specialist (psychologist). Toxicosis is really well treated with psychotherapy. The main thing is that the expectant mother should want to get rid of her own anxiety.
No matter how unpleasant toxicosis is, it does not last forever. It is necessary to suffer until the beginning or (less often) the middle of the II trimester. And very soon all the unpleasant symptoms of toxicosis will remain in the past!
Make an appointment
to the doctor - Alexandrova Anna Evgenievna
Clinic "Mother and Child" South-West
ICSIECO
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you clarify the cost of services by phone / with the managers of the clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" Savelovskaya Clinic "Mother and Child" » South-WestClinic "Mother and Child" NovogireevoClinic "Mother and Child" Lefortovo
All directionsSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesTreatment roomTelemedicine for adultsTherapeutic studiesUltrasound examinations for adults
01.